Abstract
Complex congenital heart disease is often accompanied by extracardiac manifestations; , the significance of genitourinary involvement remains unclear. We present 3 patients with palliated complex congenital heart disease and with pregnancies complicated by premature delivery who were found to have congenital uterine anomalies that may have contributed to their obstetrical complications.
Key Words: adult congenital heart disease, congenital uterine anomalies, Fontan, heterotaxy, müllerian anomalies, single ventricle
Graphical abstract
Congenital uterine anomalies (CUAs), also known as müllerian anomalies, are a known risk factor for obstetrical complications such as premature delivery and miscarriage.1 Complex congenital heart disease (CCHD), such as heterotaxy and single-ventricle disease, is often accompanied by extracardiac manifestations; however, the exact correlation and significance of genitourinary involvement remain unclear. We present a case series of 3 patients with palliated CCHD who had pregnancies complicated by premature delivery and were subsequently found to have CUAs that may have contributed to their obstetrical complications.
Learning Objectives
-
•
To understand the association of extracardiac anatomical malformations, such as CUAs, in CCHD.
-
•
To appreciate how CUAs may augment obstetrical risk in patients with CCHD.
-
•
To consider screening patients with CCHD who are undergoing prepregnancy counseling for CUAs with pelvic MRI.
Case 1
A 32-year-old G1P0000 woman with a history of congenitally corrected transposition of the great arteries with a restrictive ventricular septal defect and pulmonary valve stenosis status post hemi-Mustard baffle, a Rastelli-type left ventricle-to- aorta tunnel, a bidirectional Glenn procedure, and a right ventricle-to-pulmonary artery 28-mm conduit homograft, type 1 diabetes managed with an insulin pump, and atrial fibrillation status post ablation presented at 35 weeks’ gestation with preterm premature rupture of the membranes and preeclampsia with severe features, and ultimately failed induction necessitating emergency cesarean delivery. At the time of delivery, she was found to have a bicornuate uterus. She had an unremarkable postpartum course. She later had 2 further pregnancies; both deliveries were premature but were otherwise uncomplicated.
Case 2
A 27-year-old G2P0010 woman with a history of tricuspid atresia status post lateral tunnel Fontan procedure at age 2 years, coarctation of the aorta status post- stent placement at age 17 years, atrial septal defect, fenestration closure at age 21 years after a thrombotic stroke, and Fontan-associated liver disease with high-grade fibrosis (F3) presented at 32 weeks’ gestation with loss of fetal movement and was found to have nonreassuring fetal heart tones necessitating emergency cesarean delivery. At the time of delivery, she was found to have a bicornuate uterus. The hysterotomy incision inadvertently involved a portion of her abnormal septum and complicated her initial postpartum course with postpartum hemorrhage; however, she ultimately returned to her cardiac baseline.
Case 3
A 24-year-old G3P0020 woman with a history of heterotaxy with asplenia and right atrial appendage isomerism, hypoplastic left heart syndrome, double-outlet right ventricle, and interrupted inferior vena cava status post Kawashima-type Fontan procedure, Fontan-associated liver disease with high-grade fibrosis (F3), and 2 previous miscarriages, presented at 23 weeks’ gestation with concern for shortened cervical length and uterine didelphys. She was initially managed expectantly until she went into preterm labor at 28 weeks with concern for footling breech presentation, necessitating emergency cesarean delivery. At the time of delivery, she was found actually to have bicornuate uterus. Her postpartum course was notable for postpartum depression but was otherwise uncomplicated.
Discussion
As has been increasingly recognized, patients with CCHD phenotypes that were previously not survivable into adulthood are now able to undergo a variety of complex palliative surgical procedures that have dramatically improved their survival. With this improvement has come an increasing number of patients with CCHD who desire pregnancy and a search to characterize their risk and likelihood of success so we may best counsel them. Although guidelines are robust with regard to their recommendations for cardiac work-up and treatment, there is little about extracardiac manifestations that are common with these patients and may affect their ability to both achieve pregnancy and carry it to term.2,3
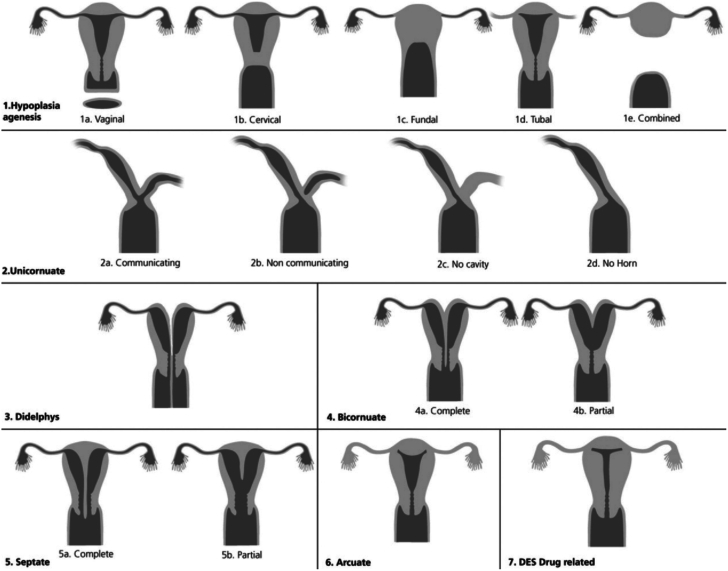
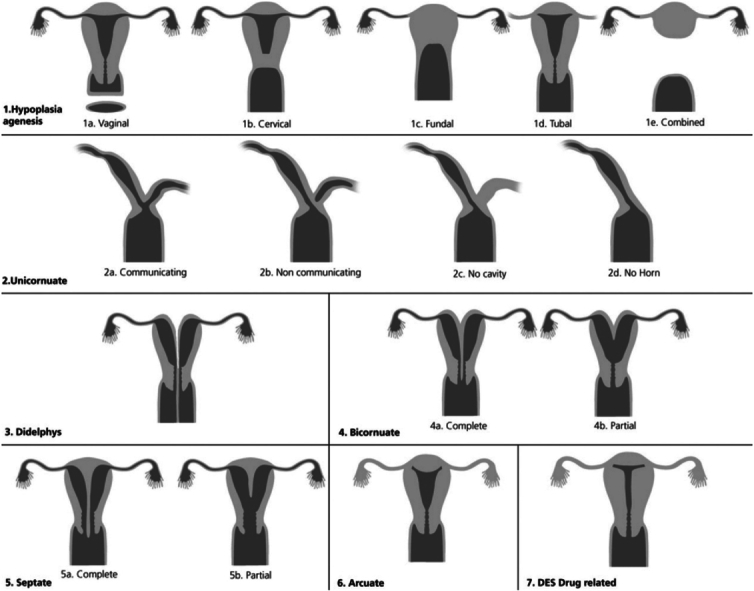
CUAs, also known as müllerian duct anomalies, are a wide spectrum of anatomical malformations of the uterus. The underlying pathophysiology involves disruption of the normal embryologic development of the uterus somewhere in the process of differentiation, migration, unification, and canalization of the müllerian duct system. Although there is no universally accepted classification system for CUAs, the 2021 American Society for Reproductive Medicine classification system is the accepted standard in the United States and divides these anomalies on this embryologic basis while accounting for the wide variety of manifestations (Figure 1).4,5 Each subtype carries different obstetrical considerations (Table 1).1 CUAs are best evaluated by magnetic resonance imaging (MRI) because it can define both external and internal contours of the uterus; however, CUAs are often first suspected on the basis of pelvic ultrasound or, as in 2 of our cases, found at the time of delivery.6 Furthermore, CUAs may complicate cesarean delivery, thus adding further risk to already complicated deliveries and even damage to an already anatomically malformed uterus, as seen in case 2.
Figure 1.
Spectrum of Congenital Uterine Anomalies
Congenital uterine anomalies (CUAs) can be categorized into the following broad categories on the basis of the timing of disruption of normal embryologic development of the Müllerian ducts. This figure actually simplifies many of the anomalies, which were further delineated in the 2021 American Society for Reproductive Medicine guidelines, as referenced in the text. Reprinted with permission from Behr et al5. DES = diethylstilbestrol.
Table 1.
Obstetrical Complications of Congenital Uterine Anomalies
| Area of Embryologic Disruption | Congenital Uterine Anomaly | Obstetrical Complications |
|---|---|---|
| Hypoplasia/agenesis | — | Infertility |
| Unification | Unicornuate | Miscarriage, prematurity, fetal malpresentation, ectopic pregnancy |
| Bicornuate | Miscarriage, prematurity, and fetal malpresentation | |
| Didelphys | Prematurity | |
| Canalization | Septate | Miscarriage, prematurity, and fetal malpresentation |
| Arcuate | Second trimester pregnancy loss, fetal malpresentation |
The most common association of CUAs is with renal malformations, most commonly unilateral renal agenesis or multicystic dysplastic kidney.6 Only 1 recent case series has looked specifically at the association between CUAs and CCHD, by presenting 8 patients with a majority single ventricle or transposition patients with unification defects.7 No larger studies exist that describe the prevalence of CUAs in persons with congenital heart disease, nor are there any studies looking at the compounded obstetrical risk that having both may conditions carry. Although one may hypothesize an association between genetic syndromes and the concomitant presence of CUA and CCHD, none of our 3 patients had an identified genetic syndrome. It may be reasonable to offer genetic counseling and consider genetic testing for these patients, as noted in the 2018 American Heart Association and American College of Cardiology guideline for management of adults with congenital heart disease, because this may be missed in patients with CCHD where it is not phenotypically apparent.8
In the most recent systemic review on pregnancy outcomes in patients with a Fontan circulation, Garcia Ropero et al9 showed that there was a high incidence of miscarriages, prematurity, and intrauterine growth restriction. These investigators wrote that this is “driven by a combination of factors, including placental insufficiency, intrinsic morphological uterine abnormalities, and adverse hemodynamics related to the Fontan circulation”9; however no dedicated studies have looked at the prevalence of CUAs in these patients. Other subtypes of CCHD such as heterotaxy do not have as robust studies on obstetrical outcomes, although similar complications can be expected for similar reasons. In our cases, determining which factors affected their premature deliveries to what extent is difficult given the known association of premature delivery with their forms of CCHD. In all 3 cases, limitations in cardiac output augmentation were compounded by placental abnormalities that have been shown to be associated with CCHD.10 Furthermore, although CUAs are known risk factors for prematurity and miscarriage, there may also be a yet undefined disruption in postnatal uterine development in patients with prolonged or profound cyanosis that may affect the ability of the uterus to carry pregnancy, as well as increase the risk of complications such as postpartum hemorrhage.
Overall, these cases are hypothesis generating for an underappreciated association between CCHD and CUAs. It may be reasonable to consider uterine imaging for CUAs, ideally with MRI, as part of prepregnancy planning and risk stratification in patients with CCHD who desire pregnancy, especially if there is a history of spontaneous abortions, as was the case with 2 of our patients. Further research is needed to better describe the prevalence of CUAs with CCHD and identify more specific associations that may allow for better pregnancy counseling as more patients from this group continue to age and become of child-bearing potential.
Funding Support and Author Disclosures
The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Footnotes
Ada Stefanescu Schmidt, MD, served as Guest Associate Editor for this paper. James L. Januzzi, MD, served as Guest Editor-in-Chief for this paper.
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
References
- 1.Chan Y.Y., Jayaprakasan K., Tan A., Thornton J.G., Coomarasamy A., Raine-Fenning N.J. Reproductive outcomes in women with congenital uterine anomalies: a systematic review. Ultrasound Obstet Gynecol. 2011;38(4):371. doi: 10.1002/uog.10056. [DOI] [PubMed] [Google Scholar]
- 2.Lindley K.J., Merz N.B., Asgar A.W., et al. Management of women with congenital or inherited cardiovascular disease from pre-conception through pregnancy and postpartum: JACC focus seminar 2/5. J Am Coll Cardiol. 2021;77(14):1778–1798. doi: 10.1016/j.jacc.2021.02.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Canobbio M.M., Warnes C.A., Aboulhosn J., et al. Management of pregnancy in patients with complex congenital heart disease: a scientific statement for healthcare professionals from the American Heart Association. Circulation. 2017;135:e50–e87. doi: 10.1161/CIR.0000000000000458. [DOI] [PubMed] [Google Scholar]
- 4.Pfeifer S.M., Attaran M., Goldstein J., et al. ASRM müllerian anomalies classification 2021. Fertil Steril. 2021;116(5):1238–1252. doi: 10.1016/j.fertnstert.2021.09.025. [DOI] [PubMed] [Google Scholar]
- 5.Behr S.C., Courtier J.L., Qayyum A. Imaging of müllerian duct anomalies. Radiographics. 2012;32:E233–250. doi: 10.1148/rg.326125515. [DOI] [PubMed] [Google Scholar]
- 6.Robbins J.B., Broadwell C., Chow L.C., Parry J.P., Sadowski E.A. Müllerian duct anomalies: embryological development, classification, and MRI assessment. J Magn Reson Imaging. 2015;41(1):1–12. doi: 10.1002/jmri.24771. [DOI] [PubMed] [Google Scholar]
- 7.Farahzad M.M., Quint E.H., Smith Y.R., Dendrinos M.L., Rosen M.W., O’Brien K.E. Müllerian anomalies among individuals with congenital heart disease – should we be screening? J Pediatr Adolesc Gynecol. 2023;36:224–230. [Google Scholar]
- 8.Stout K.K., Daniels C.J., Aboulhosn J.A., et al. 2018 AHA/ACC guideline for the management of adults with congenital heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2019;73(12):e81–e192. doi: 10.1016/j.jacc.2018.08.1029. [DOI] [PubMed] [Google Scholar]
- 9.Garcia Ropero A., Baskar S., Roos Hesselink J.W., et al. Pregnancy in women with a Fontan circulation: a systematic review of the literature. Circ Cardiovasc Qual Outcomes. 2018;11 doi: 10.1161/CIRCOUTCOMES.117.004575. [DOI] [PubMed] [Google Scholar]
- 10.Wu F., Quade B., Carreon C., et al. Placental findings in pregnancies complicated by maternal cardiovascular disease. JACC Adv. 2022;1(1) doi: 10.1016/j.jacadv.2022.100008. [DOI] [PMC free article] [PubMed] [Google Scholar]