Highlights
-
•
Cancer screenings decreased sharply immediately after the onset of the pandemic.
-
•
In FY2021, only endoscopic screening recovered to more than the pre-pandemic levels.
-
•
Despite some recovery, other cancer screening has not reached pre-pandemic levels.
-
•
It is crucial to monitor cancer mortality and increase screening participation.
Keywords: Cancer Screening, Population-based Cancer Screening, COVID-19, SARS-CoV-2, Coronavirus Disease, Cancer Prevention
Abstract
Objectives
The impact of the coronavirus disease (COVID-19) pandemic on cancer screening has become a global concern; compared with pre-pandemic levels, the number of individuals who underwent population-based cancer screening in Japan decreased by 10–30% in fiscal year (FY)2020. Therefore, it is important to monitor subsequent changes in the number of participants.
Methods
This descriptive study analysed data from a national database to determine changes from 2017 to 2021 in the number of people screened for gastric cancer (upper gastrointestinal [UGI] series or endoscopy), colorectal cancer (faecal immunochemical test), lung cancer (chest X-ray), breast cancer (mammography), and cervical cancer (Pap smear).
Results
Compared with the pre-pandemic period (FY 2017–2019), the number of participants in screening programmes in FY2021 decreased maximally for the gastric cancer UGI series (2.8 million to 2.2 million; −23.3 %), followed by those for lung cancer (7.9 million to 7.3 million; −8.2 %), colorectal cancer (8.4 million to 7.8 million; −7.3 %), breast cancer (3.1 million to 3.0 million; −4.5 %), and cervical cancer (4.3 million to 4.1 million; −3.2 %). Conversely, the number of people screened for endoscopic gastric cancer screening increased (1.0 million to 1.2 million; +13.1 %).
Conclusions
The number of participants, which decreased sharply immediately after the onset of the COVID-19 pandemic, recovered only slightly in FY2021 and did not return to pre-pandemic levels yet, except for endoscopic gastric cancer screening. Therefore, the impact of this decline in participation in cancer-detection programmes and changes in mortality should be monitored carefully.
1. Introduction
The coronavirus disease (COVID-19) pandemic that spread to Japan in March 2020 has affected cancer screening as the number of participants of population-based screenings in Japan decreased by 10 %–30 % during the pandemic (Machii and Takahashi, 2023). The following programs are endorsed by the Ministry of Health, Labour and Welfare (MHLW) as of 15 June 2023 for population-based cancer screening in Japan: biennial gastric cancer screening via upper gastrointestinal series (UGI) or endoscopy for individuals aged 50 and above, with an annual UGI alternative for those 40 and above; annual faecal immunochemical test (FIT) for colorectal cancer and chest x-ray for lung cancer for individuals aged 40 and above; biennial mammography for breast cancer and Pap smear for cervical cancer for females aged 40 and 20 and above, respectively. Population-based cancer screening can be categorised by screening systems into mass screening and individual screening. Local governments (1737 municipalities in Japan) set limits on the number of participants for each screening type according to the screening capacity, and the residents in the target group are free to choose either type of screening. Community health centres and large-scale facilities conduct mass screenings, and participants gather there at a date and time designated by local governments. On the other hand, individual screenings are conducted by clinics contracted by local governments, and participants choose a facility from a list of medical institutions provided by the local government and book their own tests. The number of participants for these screenings is compiled into the MHLW national database and published on the departmental website after 2 years (Ministry of Health, 2023a, Ministry of Health, 2023b). On the MHLW database, the data, including the total number of participants, are organised by fiscal year (FY) and include the total number of participants by local government (47 prefectures, with 1737 municipalities within each prefecture), sex, age, and screening type (mass or individual screening).
A previous study showed that the number of people screened for all five cancers decreased in FY2020 as compared to that in FY 2017–2019, and the rate of change was greater for mass screening (−34.3 % to − 14.2 %) than for individual screening (−26.0 % to − 2.2 %) (Machii and Takahashi, 2023). When evaluated by cancer type, the number of participants for UGI-based screening for gastric cancer decreased maximally during the observation period. These are speculated to be mainly attributable to the government declaration of a state of emergency issued from 7 April to 25 May 2020 for almost all municipalities. During that period, a state of emergency was declared for all local governments in 47 prefectures from 16 April 2020, to 13 May 2020 (Cabinet Secretariat, 15 June 2023). Local governments under a state of emergency were asked by the MHLW to cancel or postpone mass screenings but were allowed to conduct individual screenings after taking sufficient measures to prevent infection. By the end of FY2020, a state of emergency was declared from 8 January to 21 March 2021, for up to 11 prefectures where the spread of the new coronavirus infection rapidly increased (Cabinet Secretariat, 15 June 2023). During this time, the MHLW's guidance regarding restrictions on cancer screenings remained unchanged. Although these restrictions from the MHLW were not legally forced, the announcement may have significantly reduced the number of participants in the UGI-based screening, which has the highest percentage of mass screening among all participants. A decline in the rate of cancer screening can adversely affect cancer diagnosis and increase cancer mortality (Bakouny et al., 2021, Chen et al., 2021, Gathani et al., 2021); therefore, it is important to restore participation in cancer screening.
In FY2021, prefectures experiencing a rapid rise in new coronavirus infections were intermittently subject to state of emergency declarations from 25 April to 30 September (Cabinet Secretariat, 15 June 2023). Consequently, in 21 of the 47 prefectures, a state of emergency was declared at least once during these periods. Throughout this time, the MHLW's guidance concerning restrictions on cancer screenings remained consistent with the previous year's. To the best of our knowledge, no nationwide survey has yet been conducted to ascertain local government compliance with the MHLW's guidance or to determine the criteria used for cancelling or resuming screenings. With regard to public behaviour during the state of emergency, the targets of restrictions on going out were different in FY2020 and FY2021. At the beginning of FY2021 (April 2021), the MHLW announced that going out to participate in cancer screening was not subject to restrictions.
This study investigated the changes in Japanese population-based cancer screening between the period before the COVID-19 pandemic and that after the pandemic period (FY2021) based on national data.
2. Methods
2.1. Data sources
Based on the data available in a national database (Ministry of Health, 2023a, Ministry of Health, 2023b), we identified the total number of participants by country, prefectures, and designated city from FY2017 to FY2021. The pre-pandemic period was defined as FY 2017–2019 (April 2017 to March 2020). The subjects of analysis were the five types of cancer screening recommended by the MHLW; in these data, gastric cancer screening was aggregated separately by UGI and endoscopy. Therefore, six screening types in total were available for analysis. Furthermore, the number of participants with each cancer type was identified according to sex, age group, and screening type (mass or individual screening).
As this study used publicly available open-source data, the research did not require informed consent. No ethical review by the National Cancer Center was required. As it is currently impossible to calculate the actual cancer screening rate in Japan, which has been explained in the limitations section, we reported the statistics based on the number of participants in the analyses.
2.2. Descriptive statistics
The number of participants in each year was summarised according to the national total, sex, age group, and type of screening. The percentage change in the number of participants in each screening during the pandemic period (FY2020 and FY2021), relative to the control period (FY2017–2019), was calculated as follows:
Percentage change in participants = [Number of participants in FY2020 or FY2021 − Average number of participants in the past 3 years] / Average number of participants in the past 3 years.
Considering the possibility of fluctuations in the number of participants during FY 2017–2019, a sensitivity analysis was performed as follows.
Percentage change in participants = [Number of participants in FY2020 or FY2021 − Number of participants in FY2019] / Number of participants in FY2019.
The percentage change in the number of participants for FY2021 and FY2020 was calculated as follows:
Percentage change in participant number = [Number of participants in FY2021 − Number of participants in FY2020) / Number of participants in FY 2020.
To estimate the number of municipalities that provided cancer screenings to residents, the number of municipalities with at least one participant in cancer screening was counted.
2.3. Comparison between 21 prefectures, where a state of emergency was declared, and other prefectures of changes in the number of participants
The percentage changes (FY2021 vs. FY 2017–2019, FY2021 vs. FY2020) were compared between the 21 prefectures that declared a state of emergency in FY 2021 and the other 26 prefectures where no such emergency was declared. The percentage changes of participants in municipalities with extremely small populations were not stable (changes in one person have a large impact on the results); therefore, percentage changes at the prefecture level were compared. The Shapiro–Wilk normality test was performed on the rates of change in these two groups. The intergroup differences were compared using the Student’s t-test, for normally distributed measures and the Mann–Whitney U test for non-normally distributed measures. A p < 0.01 was considered significant. SPSS ver20 (IBM SPSS Statistics) was used for statistical analysis.
3. Results
Table 1a and Table 1b) shows the number of participants in FY2021 and FY2020 and the average number of participants in the previous 3 years in subgroups stratified by sex, age group, and screening type. Supplementary Table 1a shows the number of participants in FY 2017–2019. Regardless of sex, age group, or type of screening, the number of participants in FY2021 increased from FY2020 for all five cancer screenings.
Table 1a.
. Numbers and percentage changes of participants in gastric cancer screening programmes in Japan during fiscal years 2017–2021.
| Screening type | FY2017–2019, mean (%) | FY2020 | FY 2021 | Percentage changeFY2020 vs FY2017–2019 | Percentage changeFY2021 vs FY2017–2019 | Percentage changeFY2021 vs FY2020 | |
|---|---|---|---|---|---|---|---|
| Gastric cancer (UGI) | |||||||
| Total | 2,819,623 | 1,910,660 | 2,163,137 | −32.2 | −23.3 | 13.2 | |
| Sex | Male | 1,248,063 (44.3) | 863,923 (45.2) | 972,188 (44.9) | −30.8 | −22.1 | 12.5 |
| Female | 1,571,561 (55.7) | 1,046,737 (54.8) | 1,190,949 (55.1) | −33.4 | −24.2 | 13.8 | |
| Age, years | 40–49 | 411,252 (14.6) | 280,183 (14.7) | 323,332 (14.9) | −31.9 | −21.4 | 15.4 |
| 50–59 | 392,302 (13.9) | 273,295 (14.3) | 326,351 (15.1) | −30.3 | −16.8 | 19.4 | |
| 60–69 | 895,957 (31.8) | 549,058 (28.7) | 599,408 (27.7) | −38.7 | −33.1 | 9.2 | |
| 70–79 | 910,524 (32.3) | 659,832 (34.5) | 741,594 (34.3) | −27.5 | −18.6 | 12.4 | |
| ≥80 | 209,588 (7.4) | 148,292 (7.8) | 172,452 (8.0) | −29.2 | −17.7 | 16.3 | |
| Type of screening | Mass screening | 2,125,243 (75.4) | 1,396,841 (73.1) | 1,623,255 (75.0) | −34.3 | −23.6 | 16.2 |
| Individual screening | 694,380 (24.6) | 513,819 (26.9) | 539,882 (25.0) | −26.0 | −22.2 | 5.1 | |
| Gastric cancer (endoscopy) | |||||||
| Total | 1,017,519 | 926,423 | 1,150,879 | −9.0 | 13.1 | 24.2 | |
| Sex | Male | 430,091 (42.3) | 399,968 (43.2) | 488,141 (42.4) | −7.0 | 13.5 | 22.0 |
| Female | 587,428 (57.7) | 526,455 (56.8) | 662,738 (57.6) | −10.4 | 12.8 | 25.9 | |
| Age, years | 50–59 | 147,649 (14.5) | 150,602 (16.3) | 194,056 (16.9) | 2.0 | 31.4 | 28.9 |
| 60–69 | 321,590 (31.6) | 265,170 (28.6) | 323,175 (28.1) | −17.5 | 0.5 | 21.9 | |
| 70–79 | 416,677 (41.0) | 386,812 (41.8) | 475,107 (41.3) | −7.2 | 14.0 | 22.8 | |
| ≥80 | 131,603 (12.9) | 123,839 (13.4) | 158,541 (13.8) | −5.9 | 20.5 | 28.0 | |
| Type of screening | Mass screening | 18,437 (1.8) | 15,822 (1.7) | 19,760 (1.7) | −14.2 | 7.2 | 24.9 |
| Individual screening | 999,082 (98.2) | 910,601 (98.3) | 1,131,119 (98.3) | −8.9 | 13.2 | 24.2 | |
UGI, upper gastrointestinal series; FY, fiscal year.
Table 1b.
. Numbers and percentage changes of participants in cancer screening programmes for colorectal cancer, lung cancer, breast cancer, and cervical cancer in Japan during fiscal years 2017–2021.
| Screening type | FY2017–2019, mean (%) | FY2020 | FY 2021 | Percentage changeFY2020 vs FY2017–2019 | Percentage changeFY2021 vs FY2017–2019 | Percentage changeFY2021 vs FY2020 | |
|---|---|---|---|---|---|---|---|
| Colorectal cancer (FIT) | |||||||
| Total | 8,424,776 | 7,298,673 | 7,810,826 | −13.4 | −7.3 | 7.0 | |
| Sex | Male | 3,321,617 (39.4) | 2,893,898 (39.6) | 3,086,347 (39.5) | −12.9 | −7.1 | 6.7 |
| Female | 5,103,159 (60.6) | 4,404,775 (60.4) | 4,724,479 (60.5) | −13.7 | −7.4 | 7.3 | |
| Age, years | 40–49 | 856,762 (10.2) | 693,443 (9.5) | 750,797 (9.6) | −19.1 | −12.4 | 8.3 |
| 50–59 | 953,545 (11.3) | 816,647 (11.2) | 910,127 (11.7) | −14.4 | −4.6 | 11.4 | |
| 60–69 | 2,368,211 (28.1) | 1,802,854 (24.7) | 1,867,805 (23.9) | −23.9 | −21.1 | 3.6 | |
| 70–79 | 3,086,488 (36.6) | 2,874,921 (39.4) | 3,053,174 (39.1) | −6.9 | −1.1 | 6.2 | |
| ≥80 | 1,159,770 (13.8) | 1,110,808 (15.2) | 1,228,923 (15.7) | −4.2 | 6.0 | 10.6 | |
| Type of screening | Mass screening | 3,569,051 (42.4) | 2,787,198 (38.2) | 3,100,545 (39.7) | −21.9 | −13.1 | 11.2 |
| Individual screening | 4,855,726 (57.6) | 4,511,475 (61.8) | 4,710,281 (60.3) | −7.1 | −3.0 | 4.4 | |
| Lung cancer (chest x-ray) | |||||||
| Total | 7,918,697 | 6,593,528 | 7,267,464 | −16.7 | −8.2 | 10.2 | |
| Sex | Male | 3,198,703 (40.4) | 2,679,184 (40.6) | 2,940,332 (40.5) | −16.2 | −8.1 | 9.7 |
| Female | 4,719,994 (59.6) | 3,914,344 (59.4) | 4,327,132 (59.5) | −17.1 | −8.3 | 10.5 | |
| Age, years | 40–49 | 710,592 (9.0) | 556,306 (8.4) | 629,521 (8.7) | −21.7 | −11.4 | 13.2 |
| 50–59 | 778,708 (9.8) | 639,820 (9.7) | 738,390 (10.2) | −17.8 | −5.2 | 15.4 | |
| 60–69 | 2,189,666 (27.7) | 1,571,519 (23.8) | 1,670,868 (23.0) | −28.2 | −23.7 | 6.3 | |
| 70–79 | 3,010,602 (38.0) | 2,684,477 (40.7) | 2,936,181 (40.4) | −10.8 | −2.5 | 9.4 | |
| ≥80 | 1,229,129 (15.5) | 1,141,406 (17.3) | 1,292,504 (17.8) | −7.1 | 5.2 | 13.2 | |
| Type of screening | Mass screening | 4,409,525 (55.7) | 3,163,019 (48.0) | 3,662,599 (50.4) | −28.3 | −16.9 | 15.8 |
| Individual screening | 3,509,172 (44.3) | 3,430,509 (52.0) | 3,604,865 (49.6) | −2.2 | 2.7 | 5.1 | |
| Breast cancer (mammography) | |||||||
| Total | 3,100,533 | 2,565,900 | 2,959,985 | −17.2 | −4.5 | 15.4 | |
| Age, years | 40–49 | 879,936 (28.4) | 727,345 (28.3) | 796,157 (26.9) | −17.3 | −9.5 | 9.5 |
| 50–59 | 681,034 (22.0) | 586,869 (22.9) | 693,769 (23.4) | −13.8 | 1.9 | 18.2 | |
| 60–69 | 835,959 (27.0) | 633,753 (24.7) | 719,148 (24.3) | −24.2 | −14.0 | 13.5 | |
| 70–79 | 607,644 (19.6) | 530,876 (20.7) | 639,056 (21.6) | −12.6 | 5.2 | 20.4 | |
| ≥80 | 95,960 (3.1) | 87,057 (3.4) | 111,855 (3.8) | −9.3 | 16.6 | 28.5 | |
| Type of screening | Mass screening | 1,495,147 (48.2) | 1,105,214 (43.1) | 1,326,522 (44.8) | −26.1 | −11.3 | 20.0 |
| Individual screening | 1,605,385 (51.8) | 1,460,686 (56.9) | 1,633,463 (55.2) | −9.0 | 1.7 | 11.8 | |
| Cervical cancer (Pap smear) | |||||||
| Total | 4,260,272 | 3,767,370 | 4,124,877 | −11.6 | −3.2 | 9.5 | |
| Age, years | 20–29 | 380,885 (8.9) | 397,995 (10.6) | 398,993 (9.7) | 4.5 | 4.8 | 0.3 |
| 30–39 | 781,530 (18.3) | 702,443 (18.6) | 710,242 (17.2) | −10.1 | −9.1 | 1.1 | |
| 40–49 | 939,360 (22.0) | 831,412 (22.1) | 895,419 (21.7) | −11.5 | −4.7 | 7.7 | |
| 50–59 | 722,492 (17.0) | 655,134 (17.4) | 759,430 (18.4) | −9.3 | 5.1 | 15.9 | |
| 60–69 | 800,719 (18.8) | 618,666 (16.4) | 695,494 (16.9) | −22.7 | −13.1 | 12.4 | |
| 70–79 | 551,198 (12.9) | 484,993 (12.9) | 569,620 (13.8) | −12.0 | 3.3 | 17.4 | |
| ≥80 | 84,088 (2.0) | 76,727 (2.0) | 95,679 (2.3) | −8.8 | 13.8 | 24.7 | |
| Type of screening | Mass screening | 1,195,295 (28.1) | 856,012 (22.7) | 1,032,518 (25.0) | −28.4 | −13.6 | 20.6 |
| Individual screening | 3,064,977 (71.9) | 2,911,358 (77.3) | 3,092,359 (75.0) | −5.0 | 0.9 | 6.2 | |
FIT, faecal immunochemical test; FY, fiscal year.
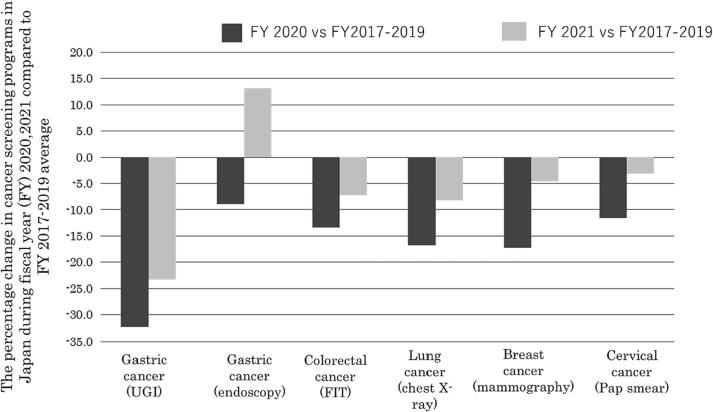
Fig. 1 shows the percentage changes in the pandemic period (FY 2020–2021) compared with those in the pre-pandemic period (FY 2017–2019). The participants of screening programmes in FY2021 decreased maximally for the gastric cancer UGI series (2.8 million to 2.2 million; −23.3 %), followed by those for lung cancer (7.9 million to 7.3 million; −8.2 %), colorectal cancer (8.4 million to 7.8 million; −7.3 %), breast cancer (3.1 million to 3.0 million; −4.5 %), and cervical cancer (4.3 million to 4.1 million; −3.2 %). Conversely, the number of individuals who underwent endoscopic gastric cancer screening increased (1.0 million to 1.2 million; +13.1 %).
Fig. 1.
The percentage change in the number of screening participants during the pandemic (FY2020 and FY2021) as compared to the FY2017–2019 average.
With regard to the screening type during the observation period, the proportion of participants in mass screening was the highest for UGI (>70 %), followed by lung cancer (48.0–55.7 %), breast cancer (43.1–48.2 %), colorectal cancer (38.2–42.4 %), cervical cancer (22.7–28.1 %), and endoscopy (<2%). In gastric cancer screening (UGI and endoscopy) in FY2021, the number of those who underwent UGI decreased from FY 2017–2019 for both screening types (−23.6 % for mass screening, −22.2 % for individual screening), whereas the number of those who underwent endoscopic screening increased for both screening types (+7.2 % for mass screening, +13.2 % for individual screening). In other cancer screening, the number of participants in mass screenings in FY2021 decreased from FY 2017–2019 (percentage change as − 16.9 % to − 11.3 %), and the number of those for individual screenings was similar to the pre-pandemic levels (percentage change: −3.0 % to + 2.7 %). In terms of the sex-stratified analyses for gastric, colorectal, and lung cancers, the number of female participants consistently remained 1.2–1.5 times higher than that of male participants during the observation period. The increasing and decreasing trends in the number of participants were similar in both sexes. In terms of age groups, most participants were in their 70 s (gastric, colon, and lung cancers) and 40 s (breast and cervical cancers) in all FY. Compared to FY2017–2019, there was an increase in the number of participants from the following age groups: All age groups for endoscopy: 80 years and older for colorectal cancer screening and lung cancer screening, 50 s and 70 years and older for breast cancer screening; and 20 s, 50 s, and ≥ 70 years for cervical cancer screening.
Table 2 shows the results of the sensitivity analysis. During FY2017–2019, the number of UGI patients who underwent gastric cancer screening decreased from 3.0 million to 2.6 million; however, the number of endoscopies increased from 0.9 to 1.1. In other cancer screenings, there was almost no change in the number of participants: 8.5 million to 8.4 million (colorectal cancer), 7.9 million and 7.9 million (lung cancer), 3.1 million and 3.1 million (breast cancer), and 4.3 million to 4.2 million (cervical cancer). Compared with FY2019, the participants of screening programmes in FY2021 decreased maximally for the gastric cancer UGI series (−16.4 %), followed by those for lung cancer (−7.6 %), colorectal cancer (−6.5 %), breast cancer (−4.8 %), and cervical cancer (−2.4 %). Conversely, the number of those who underwent endoscopic gastric cancer screening increased (+3.6 %).
Table 2.
Numbers and percentage changes of participants in colorectal, lung, breast and cervical cancer screening programmes in Japan during fiscal years 2017–2021.
| FY 2017 | FY 2018 | FY 2019 | FY 2017–2019, mean. | FY 2021 | Percentage change (FY2021 vs. FY2017–2019) | Percentage change (FY2021 vs. FY2019) | |
|---|---|---|---|---|---|---|---|
| Gastric cancer (UGI) | 3,040,310 | 2,831,769 | 2,586,791 | 2,819,623 | 2,163,137 | −23.3 | −16.4 |
| Gastric cancer (endoscopy) | 898,528 | 1,042,753 | 1,111,277 | 1,017,519 | 1,150,879 | 13.1 | 3.6 |
| Colorectal cancer (FIT) | 8,471,498 | 8,448,671 | 8,354,160 | 8,424,776 | 7,810,826 | −7.3 | −6.5 |
| Lung cancer (chest X-ray) | 7,941,580 | 7,945,305 | 7,869,206 | 7,918,697 | 7,267,464 | −8.2 | −7.6 |
| Breast cancer (mammography) | 3,081,788 | 3,111,009 | 3,108,801 | 3,100,533 | 2,959,985 | −4.5 | −4.8 |
| Cervical cancer (Pap smear) | 4,289,730 | 4,265,870 | 4,225,216 | 4,260,272 | 4,124,877 | −3.2 | −2.4 |
FIT, faecal immunochemical test; FY, fiscal year; UGI, upper gastrointestinal series;
Table 3 shows the number of municipalities with at least one participant in cancer screening during the observation period. For mass screenings, the number of such municipalities decreased during the pandemic (FY2020) and increased to almost pre-pandemic levels in FY2021. In particular, the fluctuation was maximal in UGI mass screening: 1653 (95.2 %) to 1660 (95.6)% in FY 2017–––2019, 1588 (91.4 %) in FY2020, and 1642 (94.5 %) in FY2021. For endoscopy (individual screening), the number of applicable municipalities increased consistently from 481 (27.7 %) to 842 (48.5 %) regardless of the pandemic period. For other cancer screenings, the number of applicable municipalities remained almost constant during the observation period.
Table 3.
Municipalities with at least one participant in cancer screening out of all 1,737 municipalities in Japan.
| Screening Type | FY 2017 N (%) | FY 2018 N (%) | FY 2019 N (%) | FY 2020 N (%) | FY 2021 N (%) | |
|---|---|---|---|---|---|---|
| Gastric cancer (UGI) | Total | 1712 (98.6) | 1713 (98.6) | 1713 (98.6) | 1678 (96.6) | 1711 (98.5) |
| Mass screening | 1660 (95.6) | 1659 (95.5) | 1653 (95.2) | 1588 (91.4) | 1642 (94.5) | |
| Individual screening | 661 (38.1) | 675 (38.9) | 687 (39.6) | 696 (40.1) | 711 (40.9) | |
| Gastric cancer (endoscopy) | Total | 533 (30.7) | 691 (39.8) | 780 (44.9) | 809 (46.6) | 896 (51.6) |
| Mass screening | 70 (4.0) | 72 (4.1) | 86 (5.0) | 90 (5.2) | 91 (5.2) | |
| Individual screening | 481 (27.7) | 644 (37.1) | 725 (41.7) | 754 (43.4) | 842 (48.5) | |
| Colorectal cancer (FIT) | Total | 1736 (99.9) | 1736 (99.9) | 1737 (100.0) | 1727 (99.4) | 1737 (100.0) |
| Mass screening | 1604 (92.3) | 1614 (92.9) | 1616 (93.0) | 1569 (90.3) | 1604 (92.3) | |
| Individual screening | 927 (53.4) | 952 (54.8) | 977 (56.2) | 984 (56.6) | 1011 (58.2) | |
| Lung cancer (chest X-ray) | Total | 1688 (97.2) | 1690 (97.3) | 1697 (97.7) | 1680 (96.7) | 1700 (97.9) |
| Mass screening | 1622 (93.4) | 1623 (93.4) | 1630 (93.8) | 1585 (91.2) | 1624 (93.5) | |
| Individual screening | 661 (38.1) | 686 (39.5) | 708 (40.8) | 719 (41.4) | 754 (43.4) | |
| Breast cancer (mammography) | Total | 1727 (99.4) | 1729 (99.5) | 1729 (99.5) | 1727 (99.4) | 1727 (99.4) |
| Mass screening | 1612 (92.8) | 1617 (93.1) | 1616 (93.0) | 1557 (89.6) | 1606 (92.5) | |
| Individual screening | 1391 (80.1) | 1397 (80.4) | 1404 (80.8) | 1398 (80.5) | 1417 (81.6) | |
| Cervical cancer (Pap smear) | Total | 1735 (99.9) | 1735 (99.9) | 1736 (99.9) | 1735 (99.9) | 1735 (99.9) |
| Mass screening | 1493 (86.0) | 1490 (85.8) | 1490 (85.8) | 1424 (82.0) | 1478 (85.1) | |
| Individual screening | 1545 (88.9) | 1551 (89.3) | 1551 (89.3) | 1550 (89.2) | 1562 (89.9) |
FIT, faecal immunochemical test; FY, fiscal year; UGI, upper gastrointestinal series;
Table 4 shows the distribution of the total number of participants and the percentage change (FY2021 vs FY2017 − 2019) in the 21 prefectures wherein a state of emergency was declared in FY2021 (endemic areas) and other prefectures. The median values and interquartile range of the percentage change in endemic areas and the other areas for each cancer screening were as follows, and no significant difference was observed between the two areas: −24.9 (10.7), −21.2 (10.0), p = 0.12 for UGI; 20.5 (70.2), 19.2 (69.8), p = 0.59 for endoscopy, −7.5 (6.0), −7.4 (4.9), p = 0.86 for colorectal cancer, −9.0 (8.8), −10.5 (11.2), p = 0.85 for lung cancer, −4.4 (5.6) and − 6.0 (8.3), p = 0.36 for breast cancer, and − 2.5 (7.9), −6.9 (7.2), p = 0.03 for cervical cancer. Furthermore, there was no significant difference in the percentage change from FY2020 to FY2021 between the regions that had declared a state of emergency and other regions (Supplementary Table 2).
Table 4.
Distribution of cancer screening participants (percentage change) in areas subjected to the state of emergency declaration in FY2021 (Endemic areas, n = 21) and other areas (n = 26).
| Screening type | Areas | FY 2017–2019, mean | FY2021 | Percentage change (FY2021 vs. FY 2017–2019) | p-value |
|---|---|---|---|---|---|
| Median (25th percentile, 75th percentile) | Median (25th percentile, 75th percentile) | Median (25th percentile, 75th percentile) | |||
| Gastric cancer (UGI) | Endemic | 82,772 (35502, 123793) | 64,742 (28136, 87180) | −24.9 (−29.6, −18.9) | 0.12 ** |
| Other | 28,606 (15377, 51201) | 21,849 (11209, 39863) | −21.2 (−25.8, −15.8) | ||
| Gastric cancer (endoscopy) | Endemic | 23,465 (6486, 56913) | 29,187 (12859, 60899) | 20.5 (5.3, 75.5) | 0.59** |
| Other* | 5474 (2450, 20217) | 6099 (2852, 18496) | 19.2 (−1.8, 68.0) | ||
| Colorectal cancer (FIT) | Endemic | 185,020 (133223, 446379) | 175,105 (122438, 416885) | −7.5 (−11.4, −5.4) | 0.86 *** |
| Other | 79,412 (62104, 124358) | 72,571 (56753, 120379) | −7.4 (−11.2, −6.3) | ||
| Lung cancer (chest x-ray) | Endemic | 199,367 (143448, 414157) | 176,212 (128508, 400498) | −9.0 (−13.9, −5.1) | 0.85*** |
| Other | 80,419 (54418, 113225) | 69,141 (51383, 103728) | −10.5 (−16.4, −5.2) | ||
| Breast cancer (mammography) | Endemic | 89,985 (60491, 156044) | 89,049 (56956, 145279) | −4.4 (−7.5, −1.9) | 0.36 *** |
| Other | 31,822 (24737, 43234) | 29,122 (22754, 41428) | −6.0 (−9.6, −1.3) | ||
| Cervical cancer (Pap smear) | Endemic | 113,119 (76936, 228974) | 117,118 (71314, 224200) | −2.5 (−6.8, 1.1) | 0.03 ** |
| Other | 39,837 (34147, 51579) | 36,126 (30479, 49381) | −6.9 (−9.9, −2.7) |
FIT, faecal immunochemical test; FY, fiscal year; UGI, upper gastrointestinal series;
*n = 25; One prefecture was excluded from the analysis because endoscopic screening was not provided in FY2017–2019.
**Endemic areas vs. other areas using the Mann–Whitney U test.
***Endemic areas vs. other areas using the Student's t-test.
4. Discussion
Compared with FY2017–2019 (before the COVID-19 pandemic), the number of participants in population-based screening in Japan in FY2021 decreased by 3–25 %, except for endoscopy, which increased by approximately 15 %. Although the number of participants in FY2021 rose by 7 % to 24 % compared to FY2020, levels did not revert to pre-pandemic norms, with the exception of endoscopic screening for gastric cancer. By screening type, participant numbers in mass screenings fluctuated more than those in individual screenings throughout the observation period. Specifically, mass screenings saw a decline of approximately 21–34 % from pre-pandemic levels in FY2020 (2–26 % for individual screenings) and rebounded by only 11–21 % in FY2021 (4–12 % for individual screenings). One plausible explanation for the significant downturn in mass screenings in FY2020 is that all local governments were subjected to a state of emergency declaration and many consequently curtailed or suspended the screening period, following guidance from the MHLW. Unlike individual screenings carried out at medical institutions, mass screenings elevate infection risk due to close proximity among participants and necessitate enhanced infection prevention measures, such as maintaining social distance and health checks. Prior to the pandemic, mass screenings typically involved hundreds of participants, and it is likely that few local governments had these measures in place; thus, the MHLW's directive was deemed reasonable. The principal reason for the substantial recovery in mass screenings in FY2021 appears to be the reduced number of local governments under a state of emergency, allowing many to extend the screening period or increase daily capacity. Moreover, even those local governments still under a state of emergency, but having implemented infection control measures may have resumed screenings on their own accord. This hypothesis is supported by the fact that the number of municipalities with at least one participant for mass screening (i.e., the number of municipalities that offered mass screening) in FY2021 has increased to almost pre-pandemic levels (Table 3). However, the number of participants has not fully recovered in FY2021, which may be due to the limits set by municipalities on the number of participants that could be included in mass screenings. Another reason for the increase in the number of participants in FY2020–2021 is a change in patient awareness due to the announcement by the mass media of a decrease in the screening rates, the Japanese Ministry of Health, Labour and Welfare announcement of no restriction on venturing out for cancer screening even during a state of emergency (April 2021), the start of vaccination against the coronavirus (from February 2021), and the end of the state of emergency (September 2021) (Cabinet Secretariat, 2023). Nevertheless, the main reason for this assumption is unclear, and more detailed research is needed on the participants' motives in this regard. Although the mechanisms underlying fluctuations in the number of participants during the pandemic are not yet fully understood, infection prevention measures and encouragement for the public to participate in cancer screening should be swiftly implemented under the state of emergency to avoid a reduction in screening participants in a potential future pandemic.
Worldwide, there have been few reports on the impact of the COVID-19 pandemic on cancer screening beyond 2021. In the United States and Brazil, breast, cervical, and prostate cancer screening rates declined significantly in 2020 and did not recover to 2019 levels even in 2021 (Oakes et al., 2023, Antonini et al., 2023). Another US report found that colorectal cancer screening rates in 2021 exceeded those in 2019 (Star et al., 2023). The main reason for this increase is the increased use of home screening kits. Furthermore, an increase in endoscopic screening has been reported in South Korea (Lee et al., 2022), which was attributable to the fact that those who did not participate in gastric cancer screening in 2020 were afraid of getting stomach cancer, and shifted to the endoscopic screening option, which is more reliable than UGI for early detection of gastric cancer.
Although UGI was on a downward trend even before the pandemic in Japan, endoscopy has shown an increasing trend, except in FY2020. Possible reasons for this increase include the increased number of municipalities that have started offering endoscopic screening to residents after the introduction of the gastroscopic screening programme in Japan in 2016, especially for individualised screening (Table 3).
This study has two main limitations, as mentioned previously (Machii and Takahashi, 2023). First, this study compared the total number of screenings between different years and did not account for age standardisation, though changes in the size or age structure of the population between FY2017 and FY2021 could have influenced the results. Currently, in Japan, there is no system for identifying the exact number of people who are eligible for population-based screening, and it is impossible to accurately calculate the cancer screening rate based on the actual measurements. Therefore, the number of participants, instead of the eligible population, was used in this study. Second, not all of the changes in the number of cancer screening participants from before the pandemic to FY2020 and FY2021 may be due to the pandemic. Even before the pandemic, gastric X-ray examinations had decreased significantly, and gastroendoscopy examinations had increased significantly. Other cancer screenings had increased or decreased slightly before the pandemic. Third, changes in the number of participants in the workplace-based screenings were not assessed because of the lack of a publicly available database. Differences in pandemic impacts should be assessed based on data from large screening sites covering both population-based and workplace-based screening. In the future, Japanese cancer national screening programmes should be integrated and a comprehensive database should be constructed to improve cancer screening.
5. Conclusion
The number of participants, which decreased sharply immediately after the onset of the pandemic, recovered only slightly in FY2021 and did not return to the pre-pandemic levels, except for endoscopic screening for gastric cancer. There are concerns that decreasing the number of people receiving medical examinations during the pandemic will delay cancer diagnosis and increase cancer deaths. Therefore, it is necessary to carefully monitor the mortality rate and take measures to increase the number of people participating in screening.
This study was supported by the Japanese Health and Labor Sciences Research Grant (2023, HT, 23EA1001).
6. Data statement
These data were derived from resources available in the public domain as follows: Portal Site of Official Statistics of Japan website (https://www.e-stat.go.jp/, https://www.e-stat.go.jp/en/node).
CRediT authorship contribution statement
Ryoko Machii: Conceptualization, Data curation, Formal analysis, Methodology, Project administration, Validation, Visualization, Writing – original draft, Writing – review & editing. Hirokazu Takahashi: Writing – review & editing, Project administration, Funding acquisition. Jin Miyazawa: Data curation, Writing – review & editing. Tomio Nakayama: Writing – review & editing, Supervision.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.pmedr.2024.102649.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
Data availability
Data will be made available on request.
References
- Antonini M., Pinheiro D.J.P.D.C., Matos A.B.T.M.B., Ferraro O., Mattar A., Okumura L.M., Lopes R.G.C., Real J.M. Impact of the COVID-19 pandemic on the breast cancer early diagnosis program in Brazil. Prev. Med. Rep. 2023;32 doi: 10.1016/j.pmedr.2023.102157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bakouny Z., Paciotti M., Schmidt A.L., Lipsitz S.R., Choueiri T.K., Trinh Q.D. Cancer screening tests and cancer diagnoses during the COVID-19 pandemic. JAMA Oncol. 2021;7:458–460. doi: 10.1001/jamaoncol.2020.7600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen R.C., Haynes K., Du S., Barron J., Katz A.J. Association of cancer screening deficit in the United States with the COVID-19 pandemic. JAMA Oncol. 2021;7:878–884. doi: 10.1001/jamaoncol.2021.0884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gathani T., Clayton G., MacInnes E., Horgan K. The COVID-19 pandemic and impact on breast cancer diagnoses: What happened in England in the first half of 2020. Br. J. Cancer. 2021;124:710–712. doi: 10.1038/s41416-020-01182-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee, K., Suh, M., Jun, J.K., Choi, K.S., 2022. Impact of the COVID-19 pandemic on gastric cancer screening in South Korea: Results from the Korean national cancer screening survey (2017–2021). J. Gastric Cancer. 22, 264–272. Doi: 10.5230/jgc.2022.22.e36. [DOI] [PMC free article] [PubMed]
- Machii, R., Takahashi, H., 2023. Japanese cancer screening programs during the COVID-19 pandemic: Changes in participation between 2017–2020. Cancer Epidemiol. 82, 102313. Doi: 10.1016/j.canep.2022.102313. [DOI] [PMC free article] [PubMed]
- Ministry of Health, Labour and Welfare. Guideline for population based cancer screening program. https://www.mhlw.go.jp/bunya/kenkou/gan_kenshin.html (in Japanese) (Cited 2023 15 June).
- Ministry of Health, Labour and Welfare. Report on Regional Public Health Services and Health Promotion, Services Portal Site of Official Statistics of Japan Website. https://www.e-stat.go.jp/stat-search/files?page=1&toukei=00450025&kikan=00450&tstat=000001030884 (in Japanese) (Cited 2023 15 June).
- Oakes, A.H., Boyce, K., Patton, C., Jain, S., 2023. Rates of routine cancer screening and diagnosis before vs after the COVID-19 pandemic. JAMA Oncol. 9, 145–146. https://doi: 10.1001/jamaoncol.2022.5481. [DOI] [PMC free article] [PubMed]
- Cabinet Secretariat. Covid-19 information and resources. https://corona.go.jp/news/news_20200421_70.html (in Japanese) (Cited 2023 15 June).
- Star, J., Bandi, P., Siegel, R.L., Han, X., Minihan, A., Smith, R.A., Jemal, A., 2023. Cancer screening in the United States during the second year of the COVID-19 pandemic. J. Clin. Oncol., JCO2202170. https://doi: 10.1200/JCO.22.02170. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data will be made available on request.