Abstract
Urban refugees may be disproportionately affected by socio-environmental stressors that shape alcohol use, and this may have been exacerbated by additional stressors in the COVID-19 pandemic. This multi-method study aimed to understand experiences of, and contextual factors associated with, alcohol use during the pandemic among urban refugee youth in Kampala, Uganda. We conducted a cross-sectional survey (n = 335), in-depth individual interviews (IDI) (n = 24), and focus groups (n = 4) with urban refugee youth in Kampala. We also conducted key informant interviews (n = 15) with a range of stakeholders in Kampala. We conducted multivariable logistic regression analyses with survey data to examine socio-demographic and ecosocial (structural, community, interpersonal) factors associated with ever using alcohol and alcohol misuse. We applied thematic analyses across qualitative data to explore lived experiences, and perceived impacts, of alcohol use. Among survey participants (n = 335, mean age= 20.8, standard deviation: 3.01), half of men and one-fifth of women reported ever using alcohol. Among those reporting any alcohol use, half (n = 66, 51.2 %) can be classified as alcohol misuse. In multivariable analyses, older age, gender (men vs. women), higher education, and perceived increased pandemic community violence against women and children were associated with significantly higher likelihood of ever using alcohol. In multivariable analyses, very low food security, relationship status, transactional sex, and lower social support were associated with increased likelihood of alcohol misuse. Qualitative findings revealed: (1) alcohol use as a coping mechanism for stressors (e.g., financial insecurity, refugee-related stigma); and (2) perceived impacts of alcohol use on refugee youth health (e.g., physical, mental). Together findings provide insight into multi-level contexts that shape vulnerability to alcohol mis/use among urban refugee youth in Kampala and signal the need for gender-tailored strategies to reduce socio-environmental stressors.
Keywords: Alcohol use, Alcohol misuse, COVID-19, Urban refugee, Informal settlements, Uganda, Food insecurity
1. Background
Alcohol is a leading burden of disease risk factor across the globe, increasing premature death risk among those aged 15–48 (Stanaway et al., 2018). Refugees may experience increased susceptability to alcohol use; a systematic review of research on substance use among refugees indicated that social insecurities tied to refugee status further the harmful consequences of substance use (Saleh et al., 2023). Additional barriers exist for refugees and displaced persons living in low and middle-income countries (LMIC) where the burden of alcohol-use related harm is greater (Loring, 2014) and an estimated 1 % of persons with a substance use disorder receive minimally adequate treatment (Degenhardt et al., 2017). Yet alcohol use is understudied with refugee adolescents and youth in LMIC (Horyniak et al., 2016). This is a notable knowledge gap, as there were 108.5 million forcibly displaced persons at the end of 2022, with the overwhelming majority—76 %—hosted in LMIC ((UNHCR) 2023). Over one-third of forcibly displaced persons—41 %—are children and youth under 18 years old ((UNHCR) 2023). Forcibly displaced youth in LMIC are faced with unique challenges that impact their mental health and well-being, including exposure to psychosocial stressors such as trauma, violence, poverty, and social marginalization before, during, and post-migration (Frounfelker et al., 2020). Stressful life experiences and living conditions may contribute to substance use-related coping among refugee youth (Saleh et al., 2023). This may have worsened in the COVID-19 pandemic when many of these stressors—including poverty—were exacerbated alongside elevated worry, loneliness, and anxiety among refugee persons globally (World Health Organization 2020). A systematic review, not youth specific, noted trends in increased alcohol use during the pandemic across various global contexts, yet no studies included were from Africa or LMIC humanitarian settings (Roberts et al., 2021). Another systematic review with youth reported increased mental health issues in the pandemic—yet studies also did not include refugees or African contexts (Nearchou et al., 2020). Scant research has examined alcohol use in the pandemic among urban refugee youth in LMIC who are at the nexus of refugee and youth pandemic-related health disparities.
Urbanization is increasing at a rapid rate among refugees globally, whereby more than 60 % of refugees and 80 % of internally displaced persons (IDP) reside in urban environments (Muggah and Abdenur, 2018; Park, 2019). These trends are salient in Kampala, Uganda that is home to approximately 133,887 urban refugees. Harmful alcohol use among urban refugees is common; one study in Mbarara city, Uganda, found a prevalence of 43% among adults (Bahati et al., 2023). In Kampala, 27 % of urban refugees are between 15 and 24 years old (UNHCR 2022), and many live in slums and informal settlements (Sabila and Silver, 2020), contexts often characterized by social and health disparities (Lancet, 2017; Ezeh et al., 2017; Lilford et al., 2017). Substance use is common among youth in urban Uganda; one study found that over 70 % of youth aged 12–24 in Kampala had ever used a substance, and nearly 40 % of them used regularly (UNODC 2022). Approximately one-third of youth aged 12–18 living in slums in Kampala reported alcohol consumption within the past 12 months before the COVID-19 pandemic, half of whom reported problem drinking patterns (Swahn et al., 2020). Due to shared social and physical geographies of persons living in slums that produce neighbourhood effects that shape community-level health (Ezeh et al., 2017; Lilford et al., 2017), it is plausible that these alcohol consumption trends among non-refugees in Kampala's slums could be similarly experienced by refugee youth living in the same environments. Among urban refugee youth in Kampala, depression was consistently high both before and after the COVID-19 pandemic declaration and associated with social-ecological stressors such as food insecurity, violence exposure, and low social support—signaling the chronicity of both depression and its associated stressors (Logie et al., 2022). Yet “insufficient attention has been paid to mental health and non-communicable diseases in stressful slum environments” (p. 547)(Ezeh et al., 2017) at large, and this is true also regarding urban refugee youth. Research on risk factors for non-communicable diseases (NCD) such as alcohol misuse with refugees has largely focused on rural refugee camps/settlements (Horyniak et al., 2016; Ezard et al., 2011) that have different social geographies than urban contexts.
The pandemic exacerbated inequities such as gender inequality, state fragility, food instability, and lack of social protection in LMIC (Banati et al., 2020). A World Health Organization survey with over 30,000 refugees and migrants from 170 countries noted that 20 % reported increased drug and alcohol use (World Health Organization 2020). There were noted increases in alcohol use in the pandemic among general populations of youth, including in Canada (Gohari et al., 2022; Gohari et al., 2023), the United States (Rehm et al., 2020), Switzerland (Zysset et al., 2022), and LMIC such as India and Kenya (McClarty et al., 2022). Displaced adolescents in Ethiopia and Lebanon also reported alcohol use as an escape from the pressures of the pandemic (Banati et al., 2020). The socio-economic impacts of the COVID-19 pandemic may have affected the mental health of refugees in LMIC, such as Uganda (World Health Organization 2020; Matovu et al., 2021). Prior to the COVID-19 pandemic, 44 % of the Ugandan refugee population were living in poverty (The World Bank 2021). By November of 2020, poverty rates among refugees increased to 52 %, with 89 % of households reporting lost income since the pandemic (The World Bank 2021).
Yet even before the pandemic, evidence suggests that refugee youth may use substances as a coping mechanism for stressful experiences such as displacement, abuse, and neglect in contexts such as Serbia (Vasic et al., 2021) and Kenya (Im and George, 2022). To illustrate, searching for social protection, strategies to cope with past trauma, and effects from intergenerational trauma trajectories were identified as potential pathways to substance use for urban refugee youth in pre-pandemic Kenya (Im and George, 2022). While findings suggest that refugee youth may engage in alcohol-related stress coping (Saleh et al., 2023; Frounfelker et al., 2020; Connor and Hall, 2015; Greene and Kane, 2020), scant research has examined substance use during the pandemic among refugee youth in LMIC (Saleh et al., 2023; Frounfelker et al., 2020; Connor and Hall, 2015; Greene and Kane, 2020). Better understanding alcohol use experiences among urban refugee youth in the COVID-19 pandemic can inform research and health promotion strategies.
Given the added socio-environmental stressors during COVID-19, there is a need to understand how urban refugee youth in LMIC may engage with alcohol use to cope with pandemic-related stressors. To address these knowledge gaps, this study aims to explore experiences of, and contextual factors associated with, alcohol use during COVID-19 among urban refugee youth in Kampala, Uganda.
2. Theoretical framework
This study was informed by Krieger's ecosocial approach (Krieger, 2001; Krieger, 2012; Krieger, 1994) that conceptualizes the social patterning of health by interlinked social, cultural and ecological forces. Specifically, social and ecological contexts are embodied through complex pathways across the life-course that are multi-level (e.g., structural, community), spatio-temporal (e.g., spanning time and place), and include exposure to hazardous economic, social, and environmental conditions, including social trauma (Krieger, 2012).
The ecosocial approach's focus on spatiotemporal pathways is particularly relevant for understanding alcohol use among urban refugee youth in Uganda who largely live in slums and informal settlements (Sabila and Silver, 2020), environments characterized by elevated exposure to poverty, stigma, marginalization, and infectious diseases (Ezeh et al., 2017; Lilford et al., 2017) The ecosocial approach focus on social trauma and hazardous living conditions across the life-course is also pertinent to research with refugee youth, who are exposed to trauma and violence during migration journeys and upon resettlement (Silove et al., 2017; Crankshaw et al., 2017) and are in a sensitive life course developmental period shaped by less developed coping strategies, lower self-efficacy, and reduced social power (Earnshaw et al., 2022). Informed by this ecosocial approach (Krieger, 2001; Krieger, 1994) and prior studies with urban refugee youth in Kampala (Logie et al., 2022), we explored multi-level factors linked with alcohol use in the pandemic, including at structural (e.g., food insecurity), community (e.g., violence, social support), and interpersonal (e.g., transactional sex) levels.
3. Materials and methods
3.1. Study setting and study methods
This multi-methods study uses cross-sectional data collected as part of an embedded COVID-19 study (Kukaa Salama) within the parent cohort study, the Tushirikiane HIV self-testing randomized control trial (RCT) conducted with refugee adolescent youth in Kampala, Uganda (Logie et al., 2021). The intervention and primary outcomes for Tushirikiane (Logie et al., 2021, 2023) and Kukaa Salama (Logie et al., 2021, 2023) have been described elsewhere. We use cross-sectional data in this analysis at a timepoint (February to March 2022) that included measurement of the variables of interest, namely alcohol use and COVID-19 stressors. Eligibility included 16–24-year-old youth who: spoke one of the study languages (English, French, Swahili, Luganda, Kinyarwanda, Kirundi), had access to a mobile phone, and lived in one of five of Kampala's informal settlements (Kabalagala, Kansanga, Katwe, Nsambya, and Rubaga), and identified as a refugee or who had parents who identified as refugees. We hired and trained 12 refugee youth aged 16–24 living in informal settlements as peer navigators (PN) who used peer-driven and convenience sampling to recruit participants.
3.2. Quantitative data collection and analyses
Cross-sectional data for these analyses were collected from February 2022 to March 2022 via a standardized tablet-based questionnaire in five study languages based on the participant's preferences (English, French, Swahili, Kinyarwanda or Kirundi,) and administered by trained research assistants using the secure tablet-based application SurveyCTO (Dobility, Cambridge, USA).
3.2.1. Survey measures
Outcome variables: Outcome variables included: 1) ever using alcohol and 2) alcohol misuse. To assess alcohol use ever, participants were asked if they ever consumed alcohol with single-item question with a binary (yes/no) response option. Alcohol misuse was assessed with the C.A.G.E. (Cutting down, Annoyed by Criticism, Guilty feeling, Eye-openers) scale (Cronbach's α = 0.75), a four-item scale with response options of Yes (scored 1) and No (scored 0) (Williams, 2014). A total score of 2 or higher is considered clinically significant alcohol misuse (Williams, 2014; Malet et al., 2005; Asadollahi et al., 2023).
Exposure variables: Socio-demographic information was collected including gender, age, education level, and employment status. At the structural level, we assessed food insecurity using the six-item short form of the U.S. Household Food Security Survey Module (Blumberg et al., 1999). (Cronbach's α = 0.78). Six items were used, with response options of ‘Yes (1)’ or ‘No (0)’. The sum of these items ranges from 0 to 6. A score of 0–1 was coded as high/marginal food security, 2–4 was coded as low food security, and 5–6 was coded as very low food security.
At the community level, we assessed increased perceived violence in the community using the following three questions, each with a binary response (yes/no): “Since COVID-19 lockdown have you seen an increase in violence against a) women, b) men and/or c) children?” We also measured social support using the eight-item Modified Medical Outcomes Study Social Support Survey (mMOS-SS), which assesses instrumental and emotional support (Moser et al., 2012). The scale is rated on a 5-point Likert type ranging from 5 (strongly agree) to 1 (strongly disagree). The total score was converted into a final score (ranging from 0 to 100), with higher scores reflecting higher social support (Cronbach alpha coefficient was 0.89 in this study).
At the interpersonal level we assessed relationship status (no current partner, dating one partner/married and casual dating/multiple partners), and recent transactional sex, assessed with binary (yes/no) item: “In the past 3 months, have you had sex in exchange for any of this food, gifts, money, place to live, alcohol and drugs?”
3.2.2. Quantitative data management and analyses
Statistical analyses were performed with Stata software version 14.2 (StataCorp, College Station, TX). Descriptive statistics were used to summarize the study participants' characteristics. Associations between exposure variables and each alcohol use outcome variable were assessed using logistic regression analyses. We selected exposure variables informed by the ecosocial framework (Krieger, 2001) discussed in the preceding theoretical framework section that included structural (e.g., food insecurity), community (e.g., violence, social support), and interpersonal (e.g., transactional sex) level variables. Multivariate logistic regression analyses examined associations between exposure variables and the two outcome variables, adjusting for age and gender. Multivariable logistic regression analyses were conducted using exposure variables that showed significant associations in bivariate analyses. Individuals identifying as transgender (n = 4) were included in the descriptive analysis (Table 1) but excluded from regression analysis due to the small sample size. Results from the logistic regression analyses are presented as odds ratios (OR) and adjusted odds rations (aOR) with 95 % confidence intervals (CIs), and the level of statistical significance was set at p < 0.05.
Table 1.
Socio-demographic characteristics of this sample of urban refugee youth participants in Kampala, Uganda, stratified by gender (n = 335).
| Variable | N (%), or mean (standard deviation [SD]) |
Young women | Young men | P-value* |
|---|---|---|---|---|
| Socio-demographic variables | ||||
| Age, years (Range: 16–27) | 20.8 (3.0) | 20.4 (2.8) | 21.0 (3.2) | 0.056 |
| Place of birthn=10 missing | 0.641 | |||
| Democratic Republic of Congo | 253 (77.8%) | 122 (77.2 %) | 129 (79.1 %) | |
| Burundi | 34 (10.5 %) | 17 (10.8 %) | 16 (9.8 %) | |
| Uganda | 14 (4.3%) | 9 (5.7%) | 5 (3.1%) | |
| OthersA | 24 (7.4%) | 10 (6.3%) | 13 (8.0%) | |
| Length of time in Uganda | 0.874 | |||
| < 5 years | 107 (31.9%) | 51 (32.3 %) | 56 (32.4 %) | |
| 6–10 years | 142 (42.4 %) | 65 (41.1 %) | 75 (43.3 %) | |
| >10 years | 86 (25.7 %) | 42 (26.6 %) | 42 (24.3 %) | |
| Employment | ||||
| Employed/student | 188 (56.1) | 95 (60.1) | 90 (52.1) | 0.138 |
| Unemployed | 147 (43.9) | 63 (39.9) | 83 (47.9) | |
| Highest level of educationn=12 missing | 0.047* | |||
| Less than secondary school | 150 (46.4) | 82 (53.9 %) | 67 (40.1 %) | |
| Some secondary school | 131 (40.6) | 53 (34.9 %) | 76 (45.5 %) | |
| Secondary school or higher | 42 (13.0) | 17 (11.2 %) | 24 (14.4 %) | |
| Structural level factors | ||||
| Food securityn=3 missing | 0.769 | |||
| High or marginal | 27 (8.2) | 12 (7.7 %) | 14 (8.2 %) | |
| Low | 106 (31.9) | 53 (34.0 %) | 52 (30.2 %) | |
| Very low | 109 (59.9) | 91 (58.3 %) | 106 (61.6 %) | |
| Community level factor | ||||
| Increased violence in community in the pandemic | ||||
| Against womenn=9 missing | 0.492 | |||
| No | 180 (55.2 %) | 81 (53.3 %) | 99 (58.2 %) | |
| Yes | 146 (44.8 %) | 71 (46.7 %) | 71 (41.8 %) | |
| Against menn=13 missing | 0.079 | |||
| No | 229 (71.1 %) | 111(75.0 %) | 117(68.8 %) | |
| Yes | 93 (28.9 %) | 37 (25.0 %) | 53 (31.2 %) | |
| Against childrenn=6 missing | 0.529 | |||
| No | 182 (55.3 %) | 86 (55.8 %) | 95 (55.6 %) | |
| Yes | 147 (44.7 %) | 68 (44.2 %) | 76 (44.4 %) | |
| Social support (range: 0–100) | 58.5 (21.3) | 58.1 (20.8) | 59.2 (21.8) | 0.664 |
| Interpersonal level factors | ||||
| Relationship status | 0.004* | |||
| No current partner | 133 (39.8) | 77 (48.7) | 55 (32.0) | |
| Dating one partner/married | 154 (46.1) | 66 (41.8) | 86 (50.0) | |
| Casual dating/multiple partners | 47 (14.1) | 15 (9.5) | 31 (18.0) | |
| Have children (young parenthood) | 0.002* | |||
| No | 298 (89.2) | 132 (83.5) | 162 (94.2) | |
| Yes | 36 (10.8) | 26 (16.5) | 10 (5.8) | |
| Transactional sex in past 3-months | 0.264 | |||
| No | 83 (79.1) | 24 (75.0 %) | 59 (84.3 %) | |
| Yes | 22 (20.9) | 8 (25.0 %) | 11 (15.7 %) | |
| Alcohol use | ||||
| Ever used alcohol | <0.001* | |||
| No | 207(61.8) | 122 (77.2) | 85 (49.1) | |
| Yes | 128 (38.2) | 36 (22.8) | 88 (50.9) | |
| Alcohol misuse as assessed with C.A.G.E.B | 0.052 | |||
| No | 63 (48.8) | 22 (62.9) | 41 (43.6) | |
| Yes | 66 (51.2) | 13 (37.1) | 53 (56.4) | |
Note: SD, standard deviation; OtherA: (Kenya, South Sudan, Rwanda, Tanzania, and Somalia). B: C.A.G.E. (Cutting down, Annoyed by Criticism, Guilty feeling, Eye-openers) scale. A total CAGE score of 2 or higher is considered clinically significant alcohol misuse. *p < 0.05.
In total analyses, transgender participants were included but, in the gender stratified analyses, transgender participants were not included due to insufficient sample size.
3.3. Qualitative data collection and analyses
The qualitative data collection was conducted from March to November 2021 at community collaborators' agencies in Kampala and at key informant workplaces. With refugee youth aged 16–24, we conducted four focus groups, two with men and two with women, and split by age (16–20 and 21–24). We also conducted 24 in-depth individual interviews with refugee youth recruited by peer navigators from the quantitative survey, purposively sampled to include gender and age diversity. We conducted 15 key informant (KI) interviews with government officials, community-based refugee agencies, and community leaders with experience working with, or offering services to, urban refugees in Kampala. Study collaborators purposively sampled KI from their professional networks. Local researchers were trained to facilitate the collection of qualitative data with the assistance of a translator as needed. The interviews and focus groups were conducted in French, Swahili, Kinyarwanda or Kirundi, audio recorded then translated and transcribed verbatim into English.
The purpose of the qualitative data collection was to understand COVID-19 stressors, and coping strategies, among urban refugee youth in Kampala during the pandemic. This included questions on stressors and related mental health challenges, and adaptative and maladaptive coping strategies, and alcohol use was a probe in both exploring mental health and stress coping strategies. Interview and focus group guides were developed in collaboration with community partners and piloted with the PN. Questions such as “What are some ways that adolescents in your community cope with feeling worried, bad or sad?” and “What are some of the challenges that adolescents face in being healthy in the [COVID-19] pandemic?” were posed to initiate discussions of alcohol and substance use. Research ethics approval was received by the University of Toronto and Mildmay Uganda, the Uganda National Council for Science & Technology. Informed verbal consent was obtained from all participants.
3.3.1. Qualitative and mixed-methods analyses
We conducted team based analysis, whereby five researchers coded transcripts using the Dedoose cloud-based platform (SocioCultural Research Consultants, LA, USA); this approach engages multiple analysts and facilitates group-based coding and collaboration while helping to mitigate individual bias (Giesen and Roeser, 2020). Each transcript was coded by two team members and in cases of a coding discrepancy, a different team member was engaged in reviewing the transcript, examining any coding differences, and resolved the discrepancy. Qualitative data was analyzed using a thematic analysis approach (Braun and Clarke, 2006; Attride-Stirling, 2001) due to its benefits of being theoretically flexible and conducive to inductive analyses to identify emergent themes as well as deductive analyses informed by the ecosocial approach (Krieger, 2001).
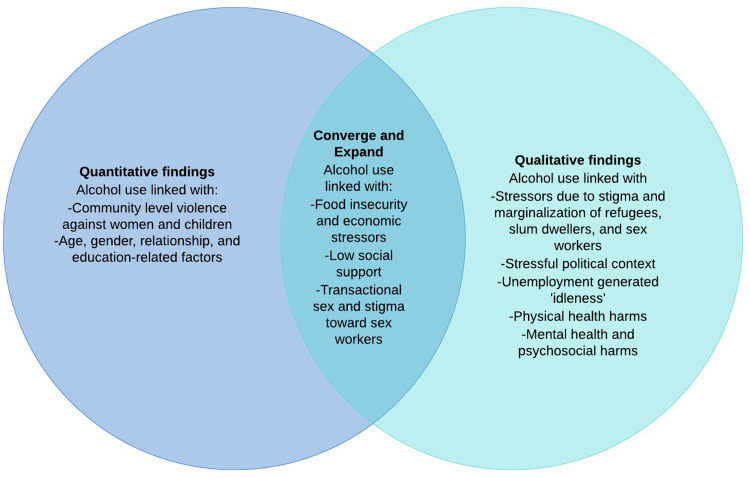
To explore and visually represent convergence and divergence of quantitative and qualitative findings, we developed a summative joint display that depicts divergence/convergence by method (Creswell, 2013; McCrudden et al., 2021). This mixed-methods analysis aims to enhance understanding of meaningful findings and methodological insights that shed light on different perspectives of the issue. In our case, the specific dimensions for which we can compare qualitative and quantitative data is an exploration of ecosocial factors associated with alcohol use among urban refugee youth in the pandemic. As we are analyzing cross-sectional survey data, we are not able to include a comparative analysis with qualitative findings regarding the perceived health and psychosocial impacts of alcohol use as that would necessitate longitudinal survey data which we did not have as C.A.G.E. scores were not collected longitudinally.
4. Results
4.1. Quantitative findings
The characteristics of the survey sample (n = 335, mean age and standard deviation [SD]= 20.8 [3.01]; young men: n = 173; 51.6 %; young women: n = 158; 47.2 %) are presented in Table 1. Over half of participants (n = 207, 61.8 %) reported ever using alcohol, which was significantly higher among men than women (n = 88; 50.9 % among men vs. n = 36; 22.8 % among women, p < 0.001). The frequency of alcohol misuse was calculated among participants who reported ever using alcohol; half of whom can be classified as reporting alcohol misuse per C.A.G.E. scoring guidelines (n = 66, 51.2 %). There was higher alcohol misuse among young men than young women, but this was not statistically significant (56.4% vs 37.1 %; p = 0.052).
Multivariable regression analyses results for ever using alcohol use and alcohol misuse are shown in Table 2. Ever using alcohol was associated with socio-demographic (gender, age, education) and community-level (increased community violence) variables. In multivariable analyses, older age (adjusted Odds Ratio [aOR]=1.30; 95 % Confidence Interval [CI]: 1.19–1.42; p < 0.001), gender (men vs. women) (aOR=3.43; 95 % CI: 2.07–5.68; p < 0.001), higher education (secondary school or higher vs. less than secondary) (aOR=2.90; 95 % CI: 1.29–6.52, p = 0.01), perceived increased pandemic community violence against women (aOR=2.76; 95 % CI: 1.63–4.68; p < 0.001), and perceived increased pandemic community violence against children (aOR=2.18; 95 % CI: 1.31–3.65; p = 0.003) were associated with increased odds of ever using alcohol.
Table 2.
Univariable and multivariable regression models for ever using alcohol and alcohol misuse among this sample of urban refugee youth participants in Kampala, Uganda (n = 335).
| Variable | Alcohol ever use (N = 331) |
Alcohol misuse (N = 128) |
||||||
|---|---|---|---|---|---|---|---|---|
| Crude OR (95 % CI) | P-Value | Adjusted ORa (95 % CI) | P-Value | Crude OR (95 % CI) | P-Value | Adjusted ORa (95 % CI) | P-Value | |
| Socio-demographic variables | ||||||||
| Age | 1.31 (1.20, 1.42) | <0.001* | 1.30 (1.19, 1.42) | <0.001* | 1.02 (0.89, 1.16) | 0.747 | 1.03 (0.91, 1.18) | 0.627 |
| Gender | ||||||||
| Men (Ref=women) | 3.51 (2.18, 5.65) | <0.001* | 3.43 (2.07, 5.68) | <0.001* | 2.19 (0.99, 4.86) | 0.054 | 2.23 (1.00, 4.96) | 0.05 |
| Length of time in Uganda | ||||||||
| <5 years | Ref | Ref | ||||||
| 6–10 years | 0.83 (0.49, 1.39) | 0.472 | 0.76 (0.34, 1.70) | 0.505 | ||||
| >10 years | 0.87 (0.48, 1.57) | 0.664 | 0.54 (0.22, 1.34) | 1.182 | ||||
| Employment | ||||||||
| Employed/student | Ref | Ref | ||||||
| Unemployed | 1.04 (0.66, 1.62) | 0.874 | 1.42 (0.71, 2.85) | 0.320 | ||||
| Highest level of education | ||||||||
| Less than secondary | Ref | Ref | ||||||
| Some secondary | 1.66(1.01, 2.74) | 0.045 | 0.81 (0.45, 1.46) | 0.484 | 1.12 (0.51, 2.46) | 0.770 | ||
| Secondary school or higher | 4.60 (2.21, 9.60) | <0.001* | 2.90 (1.29, 6.52) | 0.010* | 1.20 (0.47, 3.07) | 0.698 | ||
| Structural level factors | ||||||||
| Food security | ||||||||
| High or marginal | Ref | Ref | Ref | |||||
| Low | 0.69(0.27, 1.72) | 0.422 | 2.11(0.37,11.86) | 0.399 | 2.06 (0.36, 11.95) | 0.418 | ||
| Very low | 1.46 (0.62, 3.44) | 0.383 | 6.17(1.24,30.78) | 0.026* | 6.24 (1.22, 32.02) | 0.028* | ||
| Community level factors | ||||||||
| Increased community violence in the pandemic (Ref. No increased violence) | ||||||||
| Against women | 2.20 (1.39, 3.49) | 0.001* | 2.76 (1.63, 4.68) | <0.001* | 0.77 (0.38, 1.56) | 0.468 | ||
| Against men | 1.54 (0.94, 2.53) | 0.090 | 1.28 (0.60, 2.71) | 0.524 | ||||
| Against children | 1.84 (1.17, 2.90) | 0.008* | 2.18 (1.31, 3.65) | 0.003* | 0.99 (0.50, 1.99) | 0.998 | ||
| Social support | 0.99 (0.98, 1.00) | 0.074 | 0.99(−0.51, 0.07) | 0.163 | 0.98 (0.96, 1.00) | 0.060 | 0.97 (0.96, 0.99) | 0.029* |
| Interpersonal level factors | ||||||||
| Relationship status | ||||||||
| Dating one partner/married | Ref | Ref | Ref | Ref | ||||
| No current partner | 0.35 (0.21, 0.59) | <0.001* | 0.64 (0.36, 1.16) | 0.145 | 0.95(0.39, 2.31) | 0.910 | 1.07 (0.43, 2.70) | 0.881 |
| Casual dating/multiple partners | 1.76 (0.90, 3.42) | 0.099 | 1.87 (0.91, 3.84) | 0.088 | 3.38 (1.37, 8.34) | 0.008* | 3.42 (1.37, 8.58) | 0.009* |
| Have children (young parenthood) | ||||||||
| Yes (vs. no) | 1.59 (0.79, 3.18) | 0.194 | 1.16 (0.51, 2.62) | 0.722 | 1.25 (0.46, 3.40) | 0.662 | 1.96 (0.62, 6.20) | 0.253 |
| Transactional sex in past 3-months | ||||||||
| Yes (vs. no) | 1.22 (0.44, 3.34) | 0.700 | 4.57(1.13,18.43) | 0.033* | 4.53 (1.11, 18.51) | 0.036* | ||
Note: OR-odds ratio; CI-confidence interval. aAdjusted for age and gender. *p < 0.05.
Alcohol misuse assessed with C.A.G.E (Cutting down, Annoyed by Criticism, Guilty feeling, Eye-openers) scale. A total CAGE score of 2 or higher is considered clinically significant alcohol misuse.
Adjusting for age and gender, greater odds of alcohol misuse were associated with structural (food insecurity), community (social support), interpersonal (casual dating/ having multiple partners, recent transactional sex) level variables. Participants with very low food security had more than 6-fold higher odds of alcohol misuse than food secure participants (aOR=6.24; 95 % CI: 1.22–32.02; p = 0.028). Higher social support was associated with lower odds of alcohol misuse (aOR: 0.97; 95 % CI: 0.96–0.99; p = 0.029). Relationship status (casual dating/multiple partners vs. married/one partner) was associated with 3-fold higher odds of alcohol misuse (aOR = 3.42, 95 % CI = 1.37–8.58; p = 0.009). In addition, recent transactional sex was associated with 4.5-fold higher odds of reporting alcohol misuse (aOR = 4.53, 95 % CI = 1.11–18.51; p = 0.036).
4.2. Qualitative findings
Key informant interviews (n = 15) included men (n = 7) and women (n = 8) and represented healthcare professionals, youth advocates, government workers, counsellors, and community organization leaders. Focus group refugee youth participants (n = 24, age range =16–24) included men (n = 12) and women (n = 12) who resided in one of five informal settlements in Kampala (Kabalagala n = 1, Kasanga n = 9, Katwe n = 3, Nsambya n = 5, Rubaga n = 6). In-depth interviews were conducted with refugee youth (n = 24, age range =16–24, mean age [SD] =20.6 [2.2]) from DR Congo (n = 14), Burundi (n = 8), South Sudan (n = 1) and Rwanda (n = 1). Amongst in-depth individual interview (IDI) participants, half were men (n = 12) and the other half women (n = 12).
Qualitative findings revealed two overarching themes: (1) alcohol use as a coping mechanism for ecosocial stressors; and (2) perceived impacts of alcohol use on refugee youth health and wellbeing.
4.2.1. Alcohol use as a coping mechanism for ecosocial stressors
While alcohol use was discussed as a coping strategy, two subthemes included using alcohol as a coping strategy for (i) financial insecurity and lack of opportunities, and (ii) intersecting stigmas and contextual stressors.
4.2.1.1. Alcohol use to cope with financial stress and lack of opportunities
Participants described how the COVID-19 pandemic exacerbated financial, food, and water insecurity, which increased stress within the community and, in turn, contributed to alcohol-related coping for young people in informal settlements of Kampala. As described by a refugee young woman:
COVID has affected people psychologically and financially…people thought a lot about how they were going to live, what are we going to eat? Where to find rent? Clothing… It was stressful. (23-year-old, refugee young woman, in-depth individual interview [IDI] ID #13)
Participants emphasized that financial insecurity, particularly due to COVID-19-related unemployment, was a major driver of increased stress and contributed to alcohol mis/use among young refugees. Interviewees noted that stress due to financial insecurity and coping via alcohol consumption is a cycle whereby increased alcohol use may reduce motivation and opportunities for employment, which in turn can lead to further alcohol consumption. As described by a refugee young man:
There is no job and that is why people started drinking there… here in Uganda, you have the cheapest alcohol…you can easily buy it. Instead of searching for a job, people will just look for where to ask for five hundred shillings and buy alcohol. (16–20-year-old refugee young man, focus group [FG] participant)
Consequently, COVID-19 negatively impacted refugee youth mental health. As a key informant described:
Drugs have become common, some of them have started smoking weed, drinking “kavera” high concentrated alcohol… they don't know what they will eat, where they will sleep, where they will work from… even if you talk to them and advise them, they don't follow you. (Key informant individual in-depth (IDI), ID #1, man, refugee support group director)
Other refugee youth highlighted that the alcohol use was often habitual and a consequence of a lack of opportunities that resulted in increased ‘idleness’:
In my area, you will find very young people, looking for something to do for their lives. Like learning opportunities, school… but they are in alcohol and other drugs because they don't have anything to do. That hurts me a lot… and when you want to [go to] church, it is also challenging because we have to pay transport every time we are going there, and because of that, young people don't go to church. (21–24-year-old refugee young woman, FG participant)
These narratives also suggested that COVID-19 increased idleness within the community due to lockdown-related unemployment and school closures, which magnified refugee stress and in turn increased alcohol use. A refugee young woman discussed how this ‘idleness’ affected youth:
Many people changed their behaviour. Some of them started smoking marijuana and drinking alcohol because they did not have a place to go, churches and schools were closed, and they end up doing bad things… COVID-19 changed their way of living. (16-year-old refugee young woman, IDI, ID #18)
This was corroborated by another refugee young woman who highlighted that increased substance use during COVID-19 was a coping mechanism for idleness:
The issue of alcohol and drugs have especially come out during this COVID period when all youths were home with nothing to do…. Both boys and girls have engaged in drinking and taking weed. (16–20-year-old refugee young woman, FG participant)
4.2.1.2. Alcohol use to cope with intersecting stigmas and contextual stressors
Participants noted that many young refugees face stigma, discrimination, and stress during the refugee journey and throughout resettlement. For example, some participants identified that the discrimination experienced by refugee sex workers can lead to increased use of alcohol or other substances as a coping strategy. A key informant commented on the impacts of such stigma:
You are fearing what people will be saying, at the end of the day you start harming yourself or resort in alcohol or drug abuse trying to forget, or even by trying to cope. Some girls go into prostitution, mostly unwillingly. When they cannot survive in that profession, they go back to alcohol and drug abuse to forget what they have been in. Unfortunately, some of them also develop drug dependency. (Key informant IDI, ID#13, man, refugee serving organization)
Interviewees indicated that the COVID-19 pandemic worsened pre-existing discrimination that adolescent refugees in Uganda faced, exacerbating unemployment and isolation due to reduced community activities from social distancing measures. A key informant expanded on the influence of refugee-related stigma on alcohol use and noted that:
[A refugee may need] drugs and alcohol to see how he can get through the day… It will always affect their mental health… We have lost about 49 people who are really traumatized due to drugs and alcohol, because of discrimination for general non-assistance to refugees. There is continuing general discrimination, not everyone listens to you, cannot feel you, and they discriminate against you, so it affects your mental health. In our community that's what we are seeing for adolescent refugees in Uganda. When they are not assisted, they are ready to go take alcohol, drugs then after that they are affected by mental health. If someone is discriminated against, he has nothing to do, to eat, no work, he is affected by mental health. He begins to ask himself the question if he exists in life. (Key informant IDI, ID #3, man, refugee youth advocate)
The Ugandan political climate was also identified as stressful and contributing to alcohol and substance use among young refugees. Some participants identified substance use as a coping mechanism to combat discomfort during election-related violence:
The politics of Uganda also contributed a lot to alcohol and drug use. You remember, when these elections were going to take place, youth would take weed to feel courageous and brave. So, when the soldiers came, they would not fear, because they were drugged. We have so many challenges as refugee youth that we are facing in the country. (16–20-year-old refugee young woman, FG participant)
Additionally, others discussed how the structural system of the country does not often prioritize slum and informal settlement communities where many refugees reside, in turn increaseing substance use in these regions. This neglect of slums and subsequent social and health challenges was illustrated by a key informant: “The government does not control the slums, so, slums are rejected by the government and that is where there are a lot of bad things happening: there are a lot of diseases, tuberculosis, drug addicts, mental health problems because that's where there are a lot of cheaper drugs and cheaper alcohol.” (Key informant IDI, ID #9, man, LGBTQ refugee serving organization)
4.2.2. Perceived impacts of alcohol use on refugee youth health and wellbeing
Two subthemes regarding health and wellbeing impacts of alcohol use on refugee youth health and wellbeing include perceived physical health impacts, and perceived mental health and psychosocial impacts.
4.2.2.3. Perceived physical health-related impacts of alcohol use among refugee youth
Participants described situations in which alcohol misuse resulted in physical harm to refugees themselves. A key informant from the Ministry of Health identified that: “Alcohol and substance use kills adolescents. You find adolescents in bad conditions: they have lost weight because they do not eat, they are malnourished, swollen cheeks, their hair has turned in yellow…” (Key informant IDI, ID #10, woman, healthcare provider [doctor])
Participants also mentioned the negative impacts of alcohol misuse on sexual health among youth refugees: “[Alcohol misuse] has brought diseases. [Adolescent refugees] are prone to getting STDs [sexually transmitted diseases], so, at time, they may not know the impact of drinking, probably… if someone is drunk, they may not think of having protected sex, such things are very dangerous to their health.” (Key informant IDI, ID #12, woman, healthcare provider [nurse]) Others also emphasized the risks of alcohol misuse on physical safety. A key informant described: “What is sad is that some of [the refugees] are very young and you find them drinking spirits from morning to evening. During lockdown, on top of cases of food shortage, we also had cases of rape.” (Key informant IDI, ID #5, man, refugee youth serving agency)
4.2.2.4. Perceived mental health and psychosocial impacts of alcohol use
Mental and psychosocial health impacts consistently emerged as a harmful outcome of alcohol use and misuse. Participants suggested that, although some youth refugees use alcohol for stress coping, persistent alcohol use can harm mental health: “The more the intake of alcohol and drugs increase, the more mental health problems increase in the community. As you know, alcohol and drugs affect you a lot mentally.” (Key informant IDI, ID #7, woman, refugee youth serving agency)
Others indicated that alcohol misuse could contribute to disconnection from families and community violence. A young refugee man noted that:
Using those things that “attack” the brain like alcohol, weed; some of these people don't support their families as requested. After using alcohol, your brain does not work, you get into violence in the community for no reason which only brings trouble… that's the side effect when you start alcohol and drugs when you are still young. (21–24-year-old refugee young man, FG participant)
A key informant reinforced the potential connection between alcohol misuse and risks of violence:
When there is too much alcohol and drug abuse, there is delinquency and when there is delinquency the youth become violent, they do things that are against the law and when we say delinquency that means we have a big number of people who are involved in crimes. (Key informant IDI, ID#14, man, refugee youth peer navigator)
4.3. Mixed-methods findings
Fig. 1 illustrates findings regarding ecosocial factors associated with alcohol use in the pandemic among urban refugee youth that emerged from quantitative and qualitative methods, including where the findings overlap and where they diverge. For instance, quantitative results reveal associations between alcohol use and the structural level domain of food insecurity; qualitative findings expand on this to shed light into other structural level drivers of alcohol use, including food insecurity but also financial stress at large, water insecurity, and unemployment—and related with unemployment, the concept of ‘idleness’.
Fig. 1.
Ecosocial factors associated with alcohol use in the COVID-19 pandemic among urban refugee youth in Kampala, Uganda.
While quantitative results reveal associations between community level stressors linked with alcohol use such as increased pandemic community violence against women and children and reduced social support, the community level variables raised in the qualitative data offer insight into intersecting stigmas that target multiple, interlocking social categories that urban refugee youth in Kampala may occupy, including refugee, ‘slum-dweller’, and sex worker. While qualitative narratives do not directly discuss reduced social support as a driver of increased alcohol use, they do mention social support in two ways. First, substance use may reduce the ability of youth to access and benefit from social support that is being offered to them. Second, poverty may exacerbate barriers to accessing social support, such as not having transportation funds to attend church.
Finally, at the interpersonal level, quantitative findings revealed recent transactional sex was associated with alcohol use, and qualitative findings expand on this to reveal that refugee youth engaged in transactional sex may “go back to alcohol and drug abuse to forget what they have been in”, suggesting transactional sex may be a stressful working condition. We did not explore identical questions with qualitative and quantitative research methods, hence there was also divergence in findings. A unique insight revealed in qualitative findings was refugee-related stressors, stigma, and the stressful political context that involved election-related violence that possibly exacerbated prior traumas. The summative joint display (Fig. 1) illustrates the benefits of employing both qualitative and quantitative approaches to more fulsomely understand urban refugee youth alcohol use in the pandemic.
5. Discussion
Our study identified a high frequency of ever using alcohol (61.8 %), and alcohol misuse (51.2 %), during the pandemic in this sample of refugee youth in Kampala. Quantitative findings revealed socio-demographic (older age, gender [men], higher education) and community-level factors—increased pandemic community violence—associated with ever using alcohol. We identified structural (food insecurity), community (low social support), and interpersonal (relationship status, recent transactional sex) level factors associated with alcohol misuse. Qualitative findings provide additional insight into the ways that alcohol was used as a coping mechanism for myriad ecosocial stressors, and its perceived impacts on health and wellbeing, among refugee youth. Together, findings signal the relevance of an ecosocial approach to understanding the ways that hazardous social environments shape pandemic alcohol use among urban refugee youth in Kampala and can inform contextually tailored health promotion strategies.
Our findings build on and expand prior research on alcohol use among urban refugee youth. It is not possible to directly compare the alcohol mis/use frequency we documented among refugee youth in this study with non-refugee youth living in Kampala's slums due to our study's non-random sampling, different measurement approaches, and COVID-19 pandemic timeframe, but it appears that alcohol use frequency may be similar among our sample compared with non-refugee youth in a pre-pandemic study that reported 31 % consumed alcohol in the past 12-months and 15 % reported ≤3 drinks per week (Swahn et al., 2020). Our findings also align with prior work in Kampala with urban refugee youth that used a singular question on alcohol use frequency, finding one-fifth reported frequent alcohol use (≥3 times week) that was associated with transactional sex, multiple sex partners, and recent intimate partner violence (Logie et al., 2022). We build on this study by using a validated alcohol misuse measure (C.A.G.E.) (Williams, 2014), focusing on the pandemic timeframe, assessing food insecurity, and including qualitative methods.
Our findings corroborate previous research on stressful life events and discrimination as motivations for increased alcohol use (Keyes et al., 2011; Choi et al., 2014; Kamulegeya et al., 2020; Corbin et al., 2013) For instance, prior research found that stress was a key motivator for heavy episodic drinking among university students in Uganda (Kamulegeya et al., 2020). Our qualitative findings corroborate this and suggest that alcohol mis/use may serve as a stress coping mechanism for refugee youth. We extend this literature on alcohol-related stress coping to urban refugee youth and to refugee-related and pandemic-related stressors (e.g., unemployment, idleness, refugee-related stigma, political stressors). Participants emphasized the cycle between alcohol mis/use and mental health challenges, corroborating research on relationships between adolescent alcohol use, stressors, and psychosocial conditions (Keyes et al., 2012; McHugh, 2019). Our findings have implications for tailored interventions to address these multi-level concerns specific to refugee youth in informal settlements in Kampala; stress-coping interventions can take into consideration the complexity of stressors and cultural and linguistic needs (Posselt et al., 2014).
Our findings that food insecurity was associated with alcohol misuse corroborates prior research that similarly identified links between food insecurity and alcohol use in African contexts such as Benin (Ragetlie et al., 2021), South Africa (Eaton et al., 2014; Dewing et al., 2013; Eaton et al., 2014), Mozambique (Wainberg et al., 2018), and Tanzania (Parcesepe et al., 2019). Both our qualitative and quantitative findings point to food insecurity as a stressor linked with alcohol use with urban refugee youth. Considering the high food insecurity prevalence in our study, and the fact that most forcibly displaced persons globally are hosted in countries with acute food insecurity (UNHCR 2021), it is critical to better understand associations between food insecurity and alcohol mis/use with urban refugee youth. Strategies that address social determinants of health such as food insecurity could in turn have positive ripple effects on health promotion, including reducing problematic alcohol use (Turner et al., 2022; Whittle et al., 2019).
We also found an association between alcohol use and community-level violence against women and children in the pandemic. This corroborates research on the impact of COVID-19 on women's health in Wakiso, Uganda, which also noted an association between alcohol use and violence against women (Miller et al., 2022). A pre-pandemic systematic review on substance use with forced migrants also reported associations between alcohol use and increased sexual and gender-based violence and child neglect (Horyniak et al., 2016). This requires further investigation in longitudinal studies to understand causality. For instance, do refugee youth use alcohol to mitigate the stress of living in a hazardous context with increased community violence, and/or does refugee youths’ alcohol use contribute to this increased community violence?
In addition, findings highlight the association between transactional sex and alcohol use, a relationship identified in previous studies in South Africa (Magni et al., 2015) and Uganda (Miller et al., 2021). Researchers suggest that sex workers may be more exposed to alcohol through their work (Magni et al., 2015; Miller et al., 2021), including South African findings on transactional sex in exchange for alcohol (Watt et al., 2012). From our qualitative findings, the stigma faced by sex workers emerged as an added stressor that may contribute to alcohol use, substantiating previous findings that describe stigma as a mediator of the relationship between transactional sex and substance use (Benoit et al., 2015).
In sum, our study signals the salience of an ecosocial conceptual framework (Krieger, 2001; Krieger, 2012; Krieger, 1994) for documenting multi-level (structural, community, interpersonal) hazardous environments that produce stress and in turn shape alcohol mis/use outcomes—in this case, alcohol mis/use was patterned by larger social inequities such as food insecurity, community violence, low social support, and marginalization of transactional sex. Our findings also point to the importance of applying intersectional (Crenshaw, 1991), gender-based analyses (Tannenbaum et al., 2016). An intersectional stigma lens posits that the interplay of belonging to multiple, marginalized social categories—in our case, stigma and devaluation of refugees, slum-dwellers, and sex workers—shapes access to power, resources and opportunities (Crenshaw, 1991; Sievwright et al., 2022). Our finding on gender differences in alcohol mis/use reflects prior work with this population that noted refugee young men were twice as likely to report frequent alcohol use than refugee young women (Logie et al., 2022). How gender norms, gender relations, and institutionalized gender—the “social norms that define, reproduce, and often justify different expectations and opportunities for men and women” (p. 3) (Tannenbaum et al., 2016)—shape urban refugee young men's stress coping strategies, alcohol use motivation, and social interactions, warrant further attention.
5.1. Strengths and limitations
There are study limitations. These include the non-random sample that precludes generalizing findings to larger populations, and the cross-sectional analysis does not allow inferences of causality between ecosocial factors and alcohol use. Social desirability bias may have led to underreporting alcohol use and other stigmatized factors such as transactional sex. To mitigate this challenge, we engaged twelve refugee youth peer navigators, diverse in age, gender, and country of origin, to recruit peers across five different informal settlements. Single-item measures of community violence in the pandemic, used to reduce participant burden, could be strengthened with validated scales. The quantitative cohort study focused on HIV risks and not alcohol (although alcohol was assessed as an HIV risk factor), and while the qualitative study focused on COVID-19 stressors and stress-coping at large—inclusive of alcohol use—alcohol was also not the specific focus. This is a limitation as an alcohol-focused study could have more deeply explored frequency, type, and contexts of alcohol use. There is potentially a bias that participants enrolling in the parent HIV study may be more likely to use alcohol due to its associations with interlinked HIV vulnerabilities (Logie et al., 2022) than those not interested in such a study.
Despite these limitations, our research fills knowledge gaps by addressing calls for research with refugee youth on both COVID-19 health impacts (Gautham et al., 2021) and on alcohol use at large (Horyniak et al., 2016). Our findings can inform strengths-based, harm-reduction focused, contextually tailored initiatives to address alcohol misuse with urban refugee youth in Kampala. For instance, Bernays et al.’s study with mobile youth in Uganda and South Africa co-designed a theoretically informed harm reduction intervention with mobile youth that included peer support, drop-in centres, local adult community champions, and sustained support over time (Bernays et al., 2023). Similar co-design processes hold promise in addressing larger contexts of alcohol mis/use with urban refugee youth.
6. Conclusion
This research signals the importance of addressing the hazardous social environments—including food insecurity, economic precarity, stigma, and violence—that shape alcohol mis/use. Multi-level strategies can include a focus on individual-level coping mechanisms, yet need to be accompanied by initiatives to reduce structural and community-level inequities in order to optimize health and wellbeing among urban refugee youth in Kampala.
CRediT authorship contribution statement
Carmen H. Logie: Formal analysis, Investigation, Methodology, Project administration, Resources, Supervision, Writing – original draft, Writing – review & editing. Moses Okumu: Funding acquisition, Investigation, Supervision, Writing – review & editing. Zerihun Admassu: Formal analysis, Methodology, Writing – original draft, Writing – review & editing. Frannie MacKenzie: Project administration, Supervision, Writing – original draft, Writing – review & editing. Lauren Tailor: Investigation, Writing – original draft, Writing – review & editing. Jean-Luc Kortenaar: Data curation, Investigation, Project administration, Supervision, Writing – review & editing. Amaya Perez-Brumer: Funding acquisition, Methodology, Writing – review & editing. Rushdia Ahmed: Writing – review & editing. Shamilah Batte: Investigation, Project administration, Writing – review & editing. Robert Hakiza: Conceptualization, Funding acquisition, Investigation, Project administration, Supervision, Writing – review & editing. Daniel Kibuuka Musoke: Funding acquisition, Investigation, Methodology, Project administration, Supervision, Writing – review & editing. Brenda Katisi: Investigation, Project administration, Supervision, Writing – review & editing. Aidah Nakitende: Investigation, Methodology, Project administration, Supervision, Writing – review & editing. Robert-Paul Juster: Funding acquisition, Methodology, Writing – review & editing. Marie-France Marin: Funding acquisition, Methodology, Writing – review & editing. Peter Kyambadde: Conceptualization, Funding acquisition, Investigation, Methodology, Resources, Writing – review & editing.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
Funding
The study was funded by Grand Challenges Canada with additional support by Canadian Institutes of Health Research (CIHR), International Development Research Centre (IDRC), and the University of Toronto School of Cities Urban Challenge Fund. Logie was also supported by Canada Research Chairs and Canada Foundation for Innovation. Funders played no role in study design.
Acknowledgments
We acknowledge all of the peer navigators and participants, as well as collaborating agencies: Young African Refugees for Integral Development (YARID), Ugandan Ministry of Health, Office of the Prime Minister, Most At Risk Populations Initiative (MARPI), and International Research Consortium (Kampala).
References
- Asadollahi A., Kaveh M.H., Saberi L.F., Karimi M., Ahmad N. Psychometric properties of the CAGE questionnaire amongst middle-aged and older adults in Khuzistan province of Iran. J. Cross-Cult Gerontol. 2023;38:97–109. doi: 10.1007/s10823-023-09470-w. [DOI] [PubMed] [Google Scholar]
- Attride-Stirling J. Thematic networks: an analytic tool for qualitative research. Qual. Res. 2001;1:385–405. [Google Scholar]
- Bahati R., Ashaba S., Sigmund C.D., Rukundo G.Z., Ainamani H.E. Gender differences in substance use and associated factors among urban refugees in Uganda. Eur. J. Psychotraumatol. 2023;14:2238583. doi: 10.1080/20008066.2023.2238583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Banati P., Jones N., Youssef S. Intersecting Vulnerabilities: the Impacts of COVID-19 on the Psycho-emotional Lives of Young People in Low- and Middle-Income Countries. Eur. J. Dev. Res. 2020;32:1613–1638. doi: 10.1057/s41287-020-00325-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benoit C., McCarthy B., Jansson M. Stigma, sex work, and substance use: a comparative analysis. Sociol. Health Illn. 2015;37:437–451. doi: 10.1111/1467-9566.12201. [DOI] [PubMed] [Google Scholar]
- Bernays S., Lanyon C., Tumwesige E., Aswiime A., Ngwenya N., Dlamini V., et al. This is what is going to help me’: developing a co-designed and theoretically informed harm reduction intervention for mobile youth in South Africa and Uganda. Glob. Public Health. 2023;18 doi: 10.1080/17441692.2021.1953105. [DOI] [PubMed] [Google Scholar]
- Blumberg S.J., Bialostosky K., Hamilton W.L., Briefel R.R. The effectiveness of a short form of the Household Food Security Scale. Am. J. Public Health. 1999;89:1231–1234. doi: 10.2105/ajph.89.8.1231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braun V., Clarke V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006;3:77–101. [Google Scholar]
- Choi K.W., Watt M.H., MacFarlane J.C., Sikkema K.J., Skinner D., Pieterse D., et al. Drinking in the context of life stressors: a multidimensional coping strategy among South African Women. Subst. Use Misuse. 2014;49:66–76. doi: 10.3109/10826084.2013.819365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connor J.P., Hall W. Alcohol burden in low-income and middle-income countries. Lancet. 2015;386:1922–1924. doi: 10.1016/S0140-6736(15)00236-6. [DOI] [PubMed] [Google Scholar]
- Corbin W.R., Farmer N.M., Nolen-Hoekesma S. Relations among stress, coping strategies, coping motives, alcohol consumption and related problems: a mediated moderation model. Addict. Behav. 2013;38:1912–1919. doi: 10.1016/j.addbeh.2012.12.005. [DOI] [PubMed] [Google Scholar]
- Crankshaw T.L., Voce A., Butler L.M., Darbes L., Medicine H., Building G.C., et al. Expanding the relationship context for couple-based HIV prevention: elucidating women's perspectives on non-traditional sexual partnerships. Soc. Sci. Med. 2017;166:169–176. doi: 10.1016/j.socscimed.2016.08.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crenshaw K. Mapping the margins: intersectionality, identity politics, and violence against women of color. Stanford. Law Rev. 1991;43:1241. [Google Scholar]
- Creswell J.W. Qualitative, quantitative, and mixed methods approaches. Res. Des. 2013:1–26. [Google Scholar]
- Degenhardt L., Glantz M., Evans-Lacko S., Sadikova E., Sampson N., Thornicroft G., et al. Estimating treatment coverage for people with substance use disorders: an analysis of data from the World Mental Health Surveys. World Psychiatry. 2017;16:299–307. doi: 10.1002/wps.20457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dewing S., Tomlinson M., Le Roux I.M., Chopra M., Tsai A.C. Food insecurity and its association with co-occurring postnatal depression, hazardous drinking, and suicidality among women in peri-urban South Africa. J. Affect. Disord. 2013;150:460–465. doi: 10.1016/j.jad.2013.04.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Earnshaw V.A., Watson R.J., Eaton L.A., Brousseau N.M., Laurenceau J.-P., Fox A.B. Integrating time into stigma and health research. Nat. Rev. Psychol. 2022;1(4):236–247. doi: 10.1038/s44159-022-00034-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eaton L.A., Cain D.N., Pitpitan E.V., Carey K.B., Carey M.P., Mehlomakulu V., et al. Exploring the relationships among food insecurity, alcohol use, and sexual risk taking among men and women living in South African townships. J. Prim. Prev. 2014;35:255–265. doi: 10.1007/s10935-014-0346-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eaton L.A., Pitpitan E.V., Kalichman S.C., Sikkema K.J., Skinner D., Watt M.H., et al. Food insecurity and alcohol use among pregnant women at alcohol-serving establishments in South Africa. Prev. Sci. 2014;15:309–317. doi: 10.1007/s11121-013-0386-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ezard N., Oppenheimer E., Burton A., Schilperoord M., MacDonald D., Adelekan M., et al. Six rapid assessments of alcohol and other substance use in populations displaced by conflict. Confl. Health. 2011;5:1. doi: 10.1186/1752-1505-5-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ezeh A., Oyebode O., Satterthwaite D., Chen Y.-F., Ndugwa R., Sartori J., et al. The history, geography, and sociology of slums and the health problems of people who live in slums. The Lancet. 2017;389:547–558. doi: 10.1016/S0140-6736(16)31650-6. [DOI] [PubMed] [Google Scholar]
- Frounfelker R.L., Miconi D., Farrar J., Brooks M.A., Rousseau C., Betancourt T.S. Mental health of refugee children and youth: epidemiology, interventions, and future directions. Annu. Rev. Public Health. 2020;41:159–176. doi: 10.1146/annurev-publhealth-040119-094230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gautham I., Albert S., Koroma A., Banu S. Impact of COVID-19 on an Urban Refugee population. Health Equity. 2021;5:718–723. doi: 10.1089/heq.2020.0148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giesen L., Roeser A. Structuring a team-based approach to coding qualitative data. Int. J. Qual. Methods. 2020;19 [Google Scholar]
- Gohari M.R., Varatharajan T., MacKillop J., Leatherdale S.T. Examining the Impact of the COVID-19 Pandemic on youth Alcohol Consumption: longitudinal Changes From Pre-to Intra-pandemic Drinking in the COMPASS Study. J. Adolesc. Health. 2022;71:665–672. doi: 10.1016/j.jadohealth.2022.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gohari M.R., Varatharajan T., Patte K.A., MacKillop J., Leatherdale S.T. The intersection of internalizing symptoms and alcohol use during the COVID-19 pandemic: a prospective cohort study. Prev. Med. 2023;166 doi: 10.1016/j.ypmed.2022.107381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greene M.C., Kane J.C. In: Child Adolesc Fam Refug Ment Health Glob Perspect [Internet] Song SJ, Ventevogel P, editors. Springer International Publishing; Cham: 2020. Substance Use Among Refugee and Conflict-Affected Children and Adolescents; pp. 179–194. [cited 2023 Sep 25]Available from: [DOI] [Google Scholar]
- Horyniak D., Melo J.S., Farrell R.M., Ojeda V.D., Strathdee S.A. Epidemiology of substance use among forced migrants: a global systematic review. PLoS ONE. 2016:11. doi: 10.1371/journal.pone.0159134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Im H., George N. It hurts so much to live for nothing”: lived experiences of substance use among refugee youth in displacement. Int. J. Ment. Health Addict. 2022;20:1671–1686. [Google Scholar]
- Kamulegeya L.H., Kitonsa P.J., Okolimong E., Kaudha G., Maria S., Nakimuli-Mpungu E. Prevalence and associated factors of alcohol use patterns among university students in Uganda. Pan. Afr. Med. J. 2020;37:339. doi: 10.11604/pamj.2020.37.339.21136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keyes K.M., Hatzenbuehler M.L., Hasin D.S. Stressful life experiences, alcohol consumption, and alcohol use disorders: the epidemiologic evidence for four main types of stressors. Psychopharmacol. (Berl) 2011;218:1–17. doi: 10.1007/s00213-011-2236-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keyes K.M., Hatzenbuehler M.L., Grant B.F., Hasin D.S. Stress and alcohol: epidemiologic evidence. Alcohol Res. Curr. Rev. 2012;34:391–400. [PMC free article] [PubMed] [Google Scholar]
- Krieger N. Epidemiology and the web of causation: has anyone seen the spider? Soc. Sci. Med. 1994;39:887–903. doi: 10.1016/0277-9536(94)90202-x. [DOI] [PubMed] [Google Scholar]
- Krieger N. Theories for social epidemiology in the 21st century: an ecosocial perspective. Int. J. Epidemiol. 2001:30. doi: 10.1093/ije/30.4.668. [DOI] [PubMed] [Google Scholar]
- Krieger N. Methods for the scientific study of discrimination and health: an ecosocial approach. Am. J. Public Health. 2012;102:936–944. doi: 10.2105/AJPH.2011.300544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lancet T. Health in slums: understanding the unseen. Lancet. 2017;389:478. doi: 10.1016/S0140-6736(17)30266-0. [DOI] [PubMed] [Google Scholar]
- Lilford R.J., Oyebode O., Satterthwaite D., Melendez-Torres G.J., Chen Y.-F., Mberu B., et al. Improving the health and welfare of people who live in slums. The Lancet. 2017;389:559–570. doi: 10.1016/S0140-6736(16)31848-7. [DOI] [PubMed] [Google Scholar]
- Logie C., Okumu M., Hakiza R., Kibuuka Musoke D., Berry I., Mwima S., et al. Mobile Health–Supported HIV Self-Testing Strategy Among Urban Refugee and Displaced Youth in Kampala, Uganda: protocol for a Cluster Randomized Trial (Tushirikiane, Supporting Each Other) JMIR. Res. Protoc. 2021;10:e26192. doi: 10.2196/26192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Logie C.H., Okumu M., Berry I., Hakiza R., Kibuuka Musoke D., Kyambadde P., et al. Kukaa Salama (Staying Safe): study protocol for a pre/post-trial of an interactive mHealth intervention for increasing COVID-19 prevention practices with urban refugee youth in Kampala, Uganda. BMJ Open. 2021:11. doi: 10.1136/bmjopen-2021-055530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Logie C.H., Berry I., Okumu M., Loutet M., McNamee C., Hakiza R., et al. The prevalence and correlates of depression before and after the COVID-19 pandemic declaration among urban refugee adolescents and youth in informal settlements in Kampala, Uganda: a longitudinal cohort study. Ann. Epidemiol. 2022;66:37–43. doi: 10.1016/j.annepidem.2021.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Logie C.H., Okumu M., Malama K., Mwima S., Hakiza R., Kiera U.M., et al. Examining the substance use, violence, and HIV and AIDS (SAVA) syndemic among urban refugee youth in Kampala, Uganda: cross-sectional survey findings. BMJ Glob. Health. 2022;7 doi: 10.1136/bmjgh-2021-006583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Logie C.H., Okumu M., Berry I., Hakiza R., Baral S.D., Musoke D.K., et al. Findings from the Tushirikiane mobile health (mHealth) HIV self-testing pragmatic trial with refugee adolescents and youth living in informal settlements in Kampala. Uganda J. Int. AIDS Soc. 2023;26:e26185. doi: 10.1002/jia2.26185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Logie C.H., Okumu M., Berry I., Kortenaar J.-L., Hakiza R., Musoke D.K., et al. Kukaa Salama (Staying Safe): a pre-post trial of an interactive informational mobile health intervention for increasing COVID-19 prevention practices with urban refugee youth in Uganda. Int. Health. 2023:ihad051. doi: 10.1093/inthealth/ihad051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loring B. World Health Organization; 2014. Alcohol and Inequities: Guidance for Addressing Inequities in Alcohol-Related Harm. [Google Scholar]
- Magni S., Christofides N., Johnson S., Weiner R. Alcohol use and transactional sex among women in South Africa: results from a nationally representative survey. PLoS ONE. 2015;10 doi: 10.1371/journal.pone.0145326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malet L., Schwan R., Boussiron D., Aublet-Cuvelier B., Llorca P.-M. Validity of the CAGE questionnaire in hospital. Eur. Psychiatry J. Assoc. Eur. Psychiatr. 2005;20:484–489. doi: 10.1016/j.eurpsy.2004.06.027. [DOI] [PubMed] [Google Scholar]
- Matovu J.K.B., Kabwama S.N., Ssekamatte T., Ssenkusu J., Wanyenze R.K. COVID-19 Awareness, Adoption of COVID-19 Preventive Measures, and Effects of COVID-19 lockdown among adolescent boys and young men in Kampala, Uganda. J. Community Health. 2021;46:842–853. doi: 10.1007/s10900-021-00961-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McClarty L., Lazarus L., Pavlova D., Reza-Paul S., Balakireva O., Kimani J., et al. Socioeconomic burdens of the COVID-19 pandemic on LMIC populations with increased HIV vulnerabilities. Curr. HIV/AIDS Rep. 2022;19:76–85. doi: 10.1007/s11904-021-00591-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCrudden M.T., Marchand G., Schutz P.A. Joint displays for mixed methods research in psychology. Methods Psychol. 2021;5 [Google Scholar]
- McHugh R. Alcohol Use Disorder and Depressive Disorders. Alcohol Res. Curr. Rev. 2019;40(1) doi: 10.35946/arcr.v40.1.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller A.P., Pitpitan E.V., Nabukalu D., Nalugoda F., Nakigozi G., Kigozi G., et al. Transactional Sex, Alcohol Use and Intimate Partner Violence Against Women in the Rakai Region of Uganda. AIDS Behav. 2021;25:1144–1158. doi: 10.1007/s10461-020-03069-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller A.P., Mugamba S., Bulamba R.M., Kyasanku E., Nkale J., Nalugoda F., et al. Exploring the impact of COVID-19 on women's alcohol use, mental health, and experiences of intimate partner violence in Wakiso, Uganda. PLoS ONE. 2022;17 doi: 10.1371/journal.pone.0263827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moser A., Stuck A.E., Silliman R.A., Ganz P.A., Clough-Gorr K.M. The eight-item modified medical outcomes study social support survey: psychometric evaluation showed excellent performance. J. Clin. Epidemiol. 2012;65:1107–1116. doi: 10.1016/j.jclinepi.2012.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muggah, R. Abdenur, A.E. 2018 Refugees and the city: the twenty-first-century front lineWorld Refugee Council Research Paper #2. World Refugee Council: Centre for International Governance Innovation. Waterloo, Canada. vi to 18. https://www.cigionline.org/static/documents/documents/WRC%20Research%20Paper%20no.2.pdf.
- Nearchou F., Hennessy E., Flinn C., Niland R., Subramaniam S.S. Exploring the impact of covid-19 on mental health outcomes in children and adolescents: a systematic review. Int. J. Environ. Res. Public Health. 2020:17. doi: 10.3390/ijerph17228479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parcesepe A.M., Nash D., Tymejczyk O., Reidy W., Kulkarni S.G., Elul B. Gender differences and psychosocial factors associated with problem drinking among adults enrolling in HIV Care in Tanzania. AIDS Behav. 2019;23:1612–1622. doi: 10.1007/s10461-018-2340-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park B.H. The power of cities. Power Cities. 2019;8–11.
- Posselt M., Galletly C., De Crespigny C., Procter N. Mental health and drug and alcohol comorbidity in young people of refugee background: a review of the literature. Ment. Health Subst. Use Dual. Diagn. 2014;7(1):19–30. [Google Scholar]
- Ragetlie R., Hounkpatin W.A., Luginaah I. Community perceptions of gendered alcohol misuse in a food insecure context: the case of northwestern Benin. Soc. Sci. Med. 2021;280 doi: 10.1016/j.socscimed.2021.114016. [DOI] [PubMed] [Google Scholar]
- Rehm J., Kilian C., Ferreira-Borges C., Jernigan D., Monteiro M., Parry C.D.H., et al. Alcohol use in times of the COVID 19: implications for monitoring and policy. Drug. Alcohol Rev. 2020;39:301–304. doi: 10.1111/dar.13074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts A., Rogers J., Mason R., Siriwardena A.N., Hogue T., Whitley G.A., et al. Alcohol and other substance use during the COVID-19 pandemic: a systematic review. Drug. Alcohol Depend. 2021;229 doi: 10.1016/j.drugalcdep.2021.109150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sabila S., Silver I. Cities as partners: the case of Kampala. Forced. Migr. Rev. 2020;63:41–43. [Google Scholar]
- Saleh E.A., Lazaridou F.B., Klapprott F., Wazaify M., Heinz A., Kluge U. A systematic review of qualitative research on substance use among refugees. Addiction. 2023;118:218–253. doi: 10.1111/add.16021. [DOI] [PubMed] [Google Scholar]
- Sievwright K.M., Stangl A.L., Nyblade L., Lippman S.A., Logie C.H., Veras M.A., de S.M., et al. An Expanded Definition of Intersectional Stigma for Public Health Research and Praxis. Am. J. Public Health. 2022;112:S356–S361. doi: 10.2105/AJPH.2022.306718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silove D., Ventevogel P., Rees S. The contemporary refugee crisis: an overview of mental health challenges. World Psychiatry. 2017;16:130–139. doi: 10.1002/wps.20438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stanaway J.D., Afshin A., Gakidou E., Lim S.S., Abate D., Abate K.H., et al. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018:392. doi: 10.1016/S0140-6736(18)32225-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swahn M.H., Culbreth R., Salazar L.F., Tumwesigye N.M., Jernigan D.H., Kasirye R., et al. The prevalence and context of alcohol use, problem drinking and alcohol-related harm among youth living in the slums of Kampala, Uganda. Int. J. Environ. Res. Public Health. 2020:17. doi: 10.3390/ijerph17072451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tannenbaum C., Greaves L., Graham I.D. Why sex and gender matter in implementation research. BMC. Med. Res. Methodol. 2016;16:145. doi: 10.1186/s12874-016-0247-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The World Bank Monitoring Social and Economic Impacts of COVID-19 on Refugees in Uganda: Results from the High-Frequency Phone Survey; Washington, DC; 2021. [Google Scholar]
- Turner V.E., Demissie Z., Sliwa S.A., Clayton H.B. Food insecurity and Its association with alcohol and other substance use among high school students in the United States. J. Sch. Health. 2022;92:177–184. doi: 10.1111/josh.13118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- UNHCR. Global trends in forced displacement. 2021.
- UNHCR. Uganda - Refugee Statistic June 2022 - Kampala. 2022 p. 2022–2022.
- UNHCR UNHC for R. Figures at a glance | UNHCR US. 2023.
- UNODC . UNODC; 2022. Rapid Assessment of Substance Use and Associated Health and Social Services in Selected Relief and Humanitarian (Refugee) Settings and Situations: Assessment Report Uganda. [Google Scholar]
- Vasic J., Grujicic R., Toskovic O., Pejovic Milovancevic M. Mental health, alcohol and substance use of refugee youth. front psychiatry [Internet]. 2021 [cited 2023 Sep 25];12. Available from: https://www.frontiersin.org/articles/10.3389/fpsyt.2021.713152. [DOI] [PMC free article] [PubMed]
- Wainberg M., Oquendo M.A., Peratikos M.B., Gonzalez-Calvo L., Pinsky I., Duarte C.S., et al. Hazardous alcohol use among female heads-of-household in rural Mozambique. Alcohol Fayettev N. 2018;73:37–44. doi: 10.1016/j.alcohol.2018.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watt M.H., Aunon F.M., Skinner D., Sikkema K.J., Kalichman S.C., Pieterse D. Because he has bought for her, he wants to sleep with her”: alcohol as a currency for sexual exchange in South African drinking venues. Soc. Sci. Med. 2012;74 doi: 10.1016/j.socscimed.2011.12.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whittle H.J., Sheira L.A., Frongillo E.A., Palar K., Cohen J., Merenstein D., et al. Longitudinal associations between food insecurity and substance use in a cohort of women with or at risk for HIV in the United States. Addiction. 2019;114:127–136. doi: 10.1111/add.14418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams N. The CAGE questionnaire. Occup. Med. 2014;64:473–474. doi: 10.1093/occmed/kqu058. [DOI] [PubMed] [Google Scholar]
- World Health Organization . World Health Organization; Geneva: 2020. ApartTogether survey: Preliminary Overview of Refugees and Migrants Self-Reported Impact of COVID-19. [Google Scholar]
- Zysset A., Volken T., Amendola S., Von Wyl A., Dratva J. Change in alcohol consumption and binge drinking in university students during the early COVID-19 pandemic. Front. Public Health. 2022;10 doi: 10.3389/fpubh.2022.854350. [DOI] [PMC free article] [PubMed] [Google Scholar]