Abstract
Purpose
The study aimed to develop and evaluate a medication diary for patients to report problems with medication use to enable shared-decision making and improve medication adherence.
Methods
Based on a search for existing diaries, a review of the content, and a list of medication self-management problems compiled from previous research, a paper and pencil version of a medication diary was developed. The diary was reviewed for clarity and overall presentation by five healthcare providers and nine patients. Afterwards, user-friendliness was evaluated by 69 patients with polypharmacy discharged from hospital during a quantitative prospective study.
Results
The medication diary consists of several parts: (1) a medication schedule allowing patients to list their medicines, (2) information sheets allowing patients to write down specific medication-related information, (3) a monthly overview to indicate daily whether medication-related problems were experienced, (4) problem sheets elaborating on the problems encountered, (5) space for specific medication-related questions for healthcare providers to facilitate shared-decision making. The review phase resulted in minor textual adjustments and one extra problem in the problem sheet. Most participants, who tested the medication diary for two months, found the diary user-friendly (80%) and easy to fill in (89%). About 40% of participants reported problems with medication use. Half of the patients indicated that the diary can facilitate discussing problems with healthcare providers.
Conclusion
The medication diary offers patients the opportunity to report problems regarding their medication use in a proven user-friendly manner and to discuss these problems with healthcare providers. Reporting and discussing problems with medication use can serve as a first step towards making shared decisions on how to address the problems encountered.
Keywords: Medication self-management, Medication use, Medication errors, Medication safety, Medicines, Patient diary, Evaluation study
1. Introduction
Medication self-management capacity can be defined as “the cognitive and functional ability to self-administer a medication regimen as it has been prescribed” [1]. Self-management of medication entails a diverse set of actions that individuals need to execute effectively to manage their medicines. Knowledge, skills and behaviours are mandatory to correctly take medication and sustain adequate use over time [2]: patients have to be able to obtain medication or fill their prescriptions, know their medicines and comprehend their medication schedule, and should possess functional skills (e.g., recognizing medicines, opening medication packages and choosing the appropriate dose and time of administration) [2,3]. Furthermore, proper self-management of medication requires medication literacy, defined as “the degree to which individuals can obtain, comprehend, communicate, calculate and process patient-specific information about their medications to make informed decisions to safely and effectively use their medications” [4].
Literature highlights that patients commonly face difficulties in self-managing their medicines, impacting both medication adherence and the safe use of medicines [2,[5], [6], [7], [8], [9], [10], [11]]. Medication non-adherence can result, for example, from forgetting to take medicines, being unable to open medication packages or not being able to follow instructions for medication intake [12]. Non-adherence refers to not taking medicines as prescribed [13] which is reported to be the case for about 50% of patients with chronic conditions [14,15]. After hospital discharge, non-adherence to medication is observed in 24% to40% of patients [16,17]. The prevalence of medication errors by community-dwelling patients is estimated between 19 and 59% which is a threat to safe medication use [18]. For older people with complex therapeutic regimens, this prevalence increases to 75% [18].
Patients with polypharmacy are at increased risk of experiencing problems with medication self-management, adherence and safe medication use due to the multitude of medications administered and the higher complexity of their medication schedule [19,20]. Furthermore, patients recently discharged from hospital are more vulnerable to medication-related problems as hospitalisation is often accompanied by several changes in the medication regimen [21,22]. Research showed that 54–82% of patients were unable to name changes in their medication regimen and 55% did not utilize medicines at home as recommended at discharge [[23], [24], [25]]. A systematic review showed that drug-related hospital readmission rates varied from 3% to 64% [26]. Ensuring medication safety in polypharmacy and during transitions of care are priority areas according to the World Health Organisation [27].
To enhance adherence and safe medication use at home, it is important to identify and address difficulties in self-management of medication [28]. To achieve this, healthcare providers need to understand how patients' medication use and self-management proceed at home. Patient involvement, as a cornerstone of patient-centered care and quality of care, is, therefore indispensable [[29], [30], [31]]. Patients, as respected partners in care, should be given the chance to communicate their experiences, problems and needs regarding medication to healthcare providers. In response, healthcare providers can inform patients about different options to deal with the medication-related problems encountered, taking into account patients’ preferences and values. This way, patients and healthcare providers can work together to find the best solution or approach to deal with problems. The process of sharing information and supporting patients to consider options to achieve informed decisions is called shared decision-making [32,33].
A medication diary allowing patients to register problems with medication use in a structured way can help them to discuss these problems with healthcare providers, in order to intervene if necessary and to tailor the pharmacotherapeutic care to the patient's needs. Medication diaries, used in previous research, mainly focus on reporting the extent to which medicines were taken (adherence) [[34], [35], [36], [37]], but do not focus on reporting problems leading to not taking medicines as prescribed. Furthermore, medication diaries are often not evidence-based. Therefore, the main aim of the study was to develop and evaluate a structured medication diary for patients to report problems with medication use to enable shared-decision making and to improve medication adherence.
2. Materials and methods
2.1. Stage 1: Development of the medication diary
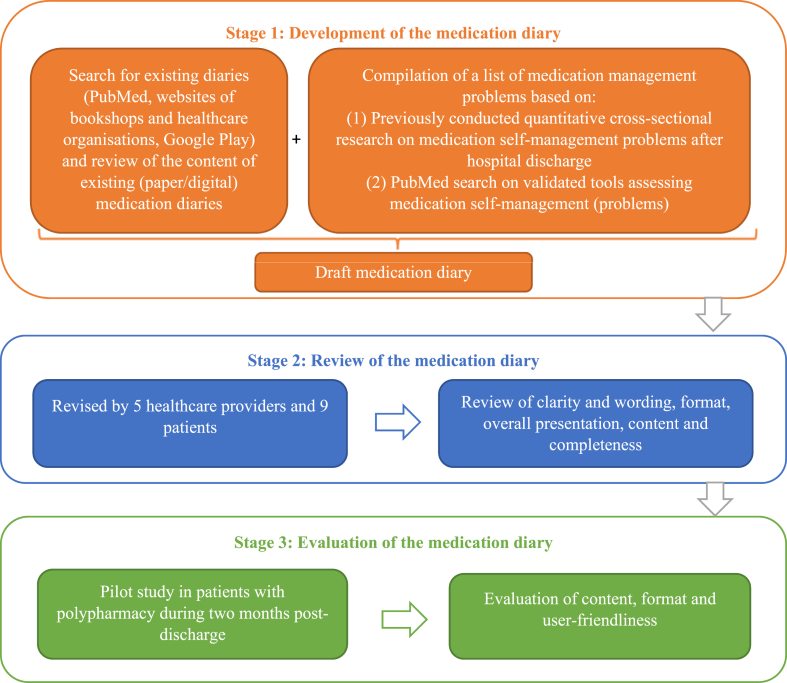
As shown in Fig. 1, several actions were undertaken during the first stage of developing the medication diary. First, a PubMed search was conducted to identify research articles on the development, evaluation or utilization of medication diaries. The following search strategy was used: ((("medication diar*") OR ("medicine diar*")) OR (("patient diary") AND ("medication"))). Articles published until November 1, 2021 in English, French or Dutch were eligible. To assess the relevance of the search results, the title and abstract were screened. Articles were included if the abstract reported on the development, evaluation or use of a medication diary in adult patients. Afterwards, the full text was reviewed to assess the content of the medication diary used and the extent to which diaries offer patients an evidence-based structure for reporting medication-related problems. Supplementary file 1 presents the selection process and results. Additionally, websites of bookshops and websites of healthcare organisations (i.e., hospitals) were hand-searched. Digital medication diaries were searched via Google Play, using the Dutch and English terms for medication diary. Diaries were mainly intended for the registration of medicines and medicine intake. None of the diaries provided a list of medication self-management problems to be reported.
Fig. 1.
Flowchart of the methodology.
Hence, a list of problems in medication self-management was derived from previous research as a basis for developing the diary. In this context, a cross-sectional study on the prevalence of medication self-management problems post-discharge was employed to pinpoint the difficulties faced by polypharmacy patients [38]. The study results indicated that patients face many problems in managing their medications, averaging four problems after hospital discharge. These problems included difficulties to obtain medication, a lack of medication-taking abilities and a lack of medication knowledge [38]. Subsequently, to finalise the list of problems, PubMed was searched for literature reviews that evaluated instruments for assessing medication management problems. For this purpose, the following search strategy was used: (("medication management") AND ("assessment") AND ("instrument") AND (("review") OR ("Review" [Publication Type]))). The search yielded 10 records, but only four of them consisted of reviews on instruments assessing medication management problems [[39], [40], [41], [42]]. The content of the different instruments included in the reviews was examined, and the medication management problems assessed in the instruments were listed.
Based on reviewing existing diaries and the list of potential problems with medication, a draft version of the diary was developed by the authors. Afterwards, a graphic designer from the University of Antwerp was consulted to determine the diary's design. The format, colour, font and text size were discussed considering readability and user-friendliness.
2.2. Stage 2: Review of the medication diary
The draft of the medication diary was reviewed for clarity and wording, format, overall presentation, content and completeness. Two hospital pharmacists, a physician and two nurses, employed in both university and regional hospitals, as well as nine patients with polypharmacy (i.e., taking five or more chronic medicines daily), reviewed the medication diary. Healthcare providers were selected based on their knowledge of hospital medication management and their role in direct patient care. Feedback was provided verbally.
2.3. Stage 3: Evaluation of the medication diary
As part of a larger prospective descriptive study on the feasibility and validity of different methods measuring medication adherence, the medication diary was pilot tested by patients. This article will not report a detailed analysis of the feasibility and validity of the different measurement methods. This report focuses on evaluating the content, format and user-friendliness of the medication diary.
2.3.1. Participants
Using consecutive sampling, patients were recruited out of two Belgian hospitals at two geriatric, four internal and five surgical wards between January and March 2022. During this period, all eligible patients who were willing to participate in the study were included. Patients’ eligibility was evaluated by a hospital ward nurse who served as a liaison between the researchers and the patients. Hospitalised patients had to meet the following criteria: (1) aged ≥18 years, (2) taking five or more chronic medicines at discharge (i.e., polypharmacy), (3) being discharged towards home and (4) being Dutch-speaking. Exclusion criteria consisted of: (1) being not responsible for own medication administration at home, (2) incapable of giving consent to participate in the study, (3) having a neuropsychiatric diagnosis of dementia.
As the evaluation of the content, format and user-friendliness of the medication diary is descriptive in nature, no power analysis was conducted. However, as part of the larger prospective descriptive study, the sample size was determined, based on the expected correlation between the different methods measuring medication adherence (r = 0.3), a power of 0.80 and a type I error rate of 0.05. The sample size determined was 84 patients.
2.3.2. Data collection
Between January and June 2022, data were collected on the day of hospital discharge (i.e., the moment of inclusion) and two months post-discharge. Patients willing to participate in the study were administered a questionnaire on socio-demographic data (e.g., age, gender, educational level,..) and medication management (e.g., number of medicines, use of medication aids, …) for descriptive purposes. At the time of discharge, patients received instructions on using the medication diary for two months (±60 days). Teaching patients how to use the diary was performed by two nurse researchers, one in each participating hospital. For this purpose, the written instructions presented in the diary itself (see supplementary file 2 or 3) were discussed with the patient, and additional explanations were given if necessary. Patients received a printout of their medication scheme which was pasted or transcribed into the diary by the nurse.
During two months post-discharge, patients were asked to record (changes in) their medication scheme and to indicate whether they experienced any problems concerning their medication use. If so, patients were asked to fill in a structured problem sheet indicating the medication-related problems encountered. To determine whether the completion of the diary went well (i.e., whether patients experienced any difficulties in completing the diary or had any questions about the diary) and to gather information on dropouts (i.e., patients not completing/using the diary), patients were contacted by telephone at weeks 1, 3 and 5 after hospital discharge.
Two months post-discharge, a home visit was conducted where a self-developed questionnaire was administered. Statements and multiple-choice questions were used to assess the user-friendliness of the medication diary. Statements could be answered using a 4-point Likert scale (1 = strongly disagree to 4 = strongly agree). In an open-ended question, patients were asked whether items should be added or removed (See supplementary file 4).
Telephone calls and home visits were performed by three nurse researchers. To ensure uniformity among data collectors, the content of the telephone calls and the administration of the survey during the home visit was discussed in a meeting before the start of the study. Regular online and live meetings throughout the process of data-collection were performed.
2.3.3. Data analysis
The data analysis was conducted using the Statistical Package for the Social Sciences (SPSS) version 28. Frequency distributions were used to describe discontinuous data. The mean value and standard deviation were used for the description of continuous data with a normal distribution, whereas for non-normally distributed data, the range and median were used. The normality of the distribution was tested using Z-scores. Descriptive statistics were used to describe changes needed to make the medication diary more user-friendly. Drop-out rates and reasons were described. Drop-outs were excluded for analysis.
2.4. Translation of the diary
To facilitate publication, a native English speaker from the University of Antwerp's language institute (Linguapolis) translated the Dutch version of the medication diary into English. The translator was not engaged in this study or any prior research on this topic.
3. Results
3.1. Stage 1: Development
The paper and pencil version of the medication diary consists of several parts.
-
1)
The medication schedule allows patients to list their (non-)prescribed medicines. Patients can indicate the name, indication, dosing frequency, quantity, time of administration and administration route for each medicine. Changes in the medication schedule, such as stopping or starting medication therapy, can be indicated.
-
2)
The information sheets allow patients to write down specific information, such as common side effects or precautions for each medicine.
-
3)
In the monthly overview, patients can indicate daily whether they experienced problems taking medicines. To reduce the burden of completing the diary, a deliberate choice was made to focus solely on reporting problems with medication use, and not to indicate every medication intake.
-
4)
In case of problems, patients can fill in a structured problem sheet indicating the problems they were experiencing. Problems in the problem sheet are divided into categories: (1) problems with obtaining medicines (i.e., medicines out of stock, forgot to collect medicines from the pharmacy, cannot afford medicines, no refill prescription available), (2) side-effects, (3) problems with medication use (wrong dose, wrong time, wrong administration route, forgot to take medicines, administration problems), (4) problems with medication packages (problems with opening or storage), (5) other problems. Patients can indicate with which medicine they experienced problems (all or specific ones) and whether they took any action to address the problem (e.g., contact with the general practitioner, pharmacist, …).
-
5)
Shared-decision making: Patients can write down specific questions for their general practitioner or another care provider, new medication instructions, appointments with healthcare providers concerning their medicines, …
In collaboration with the graphic designer of Antwerp University, an A5-sized medication diary was chosen so it can be easily carried by a patient in a handbag or backpack. The Calibri Font was used since a sans-serif font is more readable. To make the medication diary visually appealing and enhance clarity, tabs were used in different colours for each part of the medication diary. The complete medication diary, both in Dutch and English, was added as a supplementary file (see supplementary material 2 and 3).
3.2. Stage 2: Review
After a review of the clarity and wording of the medication diary by healthcare providers and patients, some minor textual adjustments were made based on their feedback. Only one extra problem category was suggested which was added to the structured problem sheet: ‘I cannot read or understand all the information about my medication.‘. The other problems were considered appropriate for inclusion in the diary by healthcare providers and patients and were, therefore, retained. The format and overall presentation required no changes according to the evaluators (i.e., healthcare providers and patients).
3.3. Stage 3: Evaluation
3.3.1. Research population
Of the 85 patients willing to fill in the diary during two months post-discharge, 69 patients completed the study (18.8% dropout). Reasons for dropout are shown in Supplementary file 5. The mean age of the participants was 68.9 years [SD 8.8] and 73% (n = 50) were men. The majority (69%, n = 43) had at least a higher secondary education level. Participants took on average seven different medicines at discharge [SD 2.5]. Participants’ characteristics are shown in Table 1.
Table 1.
Sample characteristics.
| Characteristics (n = 69) | |
|---|---|
| Age in years, mean [SD, min – max] | 68.9 [8.8, 43–86] |
| Gender (male), % (n) | 72.5 (50) |
| Highest level of education, % (n) | |
| No education | 5.8 (4) |
| Primary education | 4.3 (3) |
| Lower secondary education | 20.3 (14) |
| Higher secondary education | 31.8 (22) |
| Higher vocational education | 18.8 (13) |
| Bachelor's degree | 14.5 (10) |
| University (master's degree/PhD) | 4.3 (3) |
| Number of chronic medicines at discharge, mean [SD, min – max] | 7.2 [2.5, 5–15] |
| Number of medication changes during two months post-dischargea, mean [SD, min – max] | 1 [0–12] |
| Use of medication aids (yes), % (n) | 61.8 (42) |
Patient-reported SD = standard deviation, min = minimum, max = maximum, PhD = Doctor of Philosophy.
3.3.2. Use of the medication diary
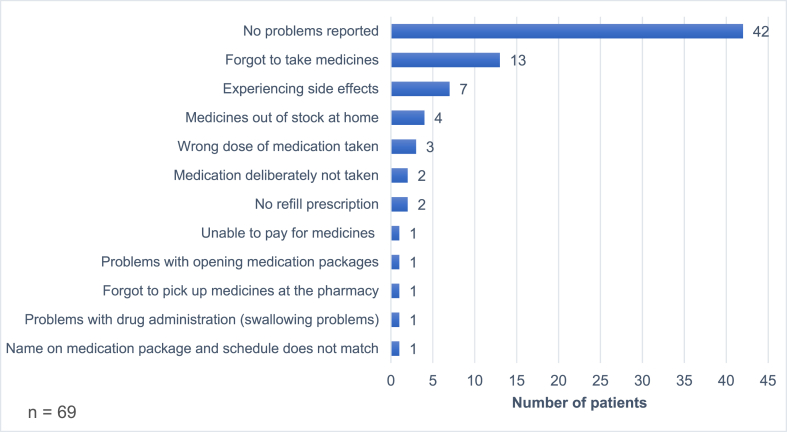
About 85.5% of participants (n = 59) wrote their medicines in the diary's medication schedule, while 11.6% (n = 8) stuck a copy of their medication schedule in the diary. Only 2.9% (n = 2) did not fill in the medication schedule. Medication-related information was added to the information sheets by 28% of participants (n = 19). All patients, except one, indicated in the monthly overview whether they were experiencing problems with medication. Approximately 40% of the participants (n = 28) reported problems with their medication intake in the problem sheets over two months. Forgetting to take medicines was reported by most patients, followed by experiencing side effects and not having medicines in stock at home (Fig. 2). Nineteen percent (n = 13) wrote down questions for healthcare providers, appointments with healthcare providers or new medication instructions.
Fig. 2.
Problems reported in the medication diary.
3.3.3. Evaluation of the content, format and user-friendliness of the medication diary
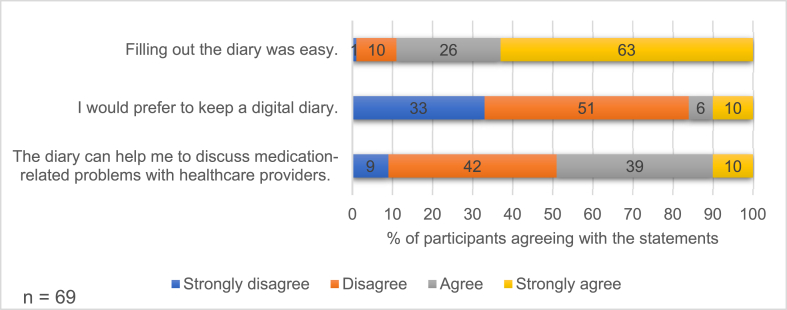
Most participants (89%, n = 61) indicated that filling in the diary over two months was easy. Half of the participants (49%, n = 34) reported that the medication diary could help them discuss problems regarding medication use with healthcare providers such as the general practitioner, pharmacist, home nurse, … Only 16% (n = 11) of the participants would prefer to keep a digital diary (Fig. 3).
Fig. 3.
Overall evaluation of the medication diary.
After filling in the medication diary for two months, 80% of participants (n = 55) indicated that no changes were needed to make the diary more user-friendly. The remaining participants indicated that user-friendliness could be increased and provided the following suggestions: smaller size (n = 4), more structure (n = 3), less structure (n = 3), more space for free text notes (n = 3), less extensive problem sheets (n = 2), larger font size (n = 1), more space for comments in the monthly overview for example to report parameters such as blood pressure (n = 1), provide columns in the medication schedule (morning, afternoon, evening) to indicate the time of intake (n = 1), smaller columns in the monthly overview (n = 1), fewer problem sheets (n = 1). Only 9% (n = 6) indicated that items should be added and/or removed from the diary. Two participants suggested adding a page for parameters such as blood pressure measurements, one suggested adding space for contact details of important persons (e.g., general practitioner) and another suggested adding examples of how to fill in the diary. The information sheets could be removed according to three participants. Furthermore, two participants indicated that a monthly overview covering one year is sufficient, and therefore, the dual monthly overview could be removed. One participant suggested deleting the problem sheets because s/he did not experience any problems.
4. Discussion
To our knowledge, this is the first study developing a paper and pencil version of a medication diary that can serve as a resource for reporting problems concerning medication self-management and medication use. A search in PubMed did not yield any research papers focusing on the development or evaluation of a medication diary at all. The research articles found used the medication diaries as a method for data collection and were mostly intended for monitoring medication intake. Our diary is unique because it focuses on problems in various stages of the medication self-management process (i.e., obtaining medication, understanding medication related-information, medication administration, monitoring side effects, …) and not solely on medication intake. The diary guides patients by offering an evidence-based structure since scientific research into medication self-management problems experienced by patients was used in the development. Furthermore, the diary offers the possibility to record actions taken by the patient in case of problems. This can give healthcare professionals insight into how patients deal with problems and determine whether additional support is needed.
During the development, the opinion of, not only healthcare providers but also patients as potential users of the medication diary was considered. A minority of patients (20%) did suggestions to make the diary more user-friendly. However, those suggestions were very diverse and dependent on the individual. For example, one participant wanted more structure in the diary while another wanted less structure. It is difficult to tailor the medication diary to each individual need or preference. No fundamental changes were made to the diary at the end of the pilot test, as the majority found the diary user-friendly and did not consider any changes necessary. We should acknowledge that there is an overrepresentation of male respondents in our sample, who may have a different opinions about the medication diary than women.
The researchers chose to develop a medication diary on paper instead of a digital version since paper is more accessible to an older population. In Belgium, only half of the people aged 65 or over have a smartphone and only 42% have a tablet [43]. We certainly want to reach the older population, given their heightened vulnerability to difficulties in managing their medicines as a result of the cognitive and physical decline that is part of the aging process [44]. Furthermore, aging raises the likelihood of polypharmacy, which, in turn is related to medication-related problems [45]. The results of our study showed that the paper and pencil version was a good choice, since only 16% would prefer to keep a digital diary. However, making the diary available both digitally (via an application) and on paper could be of added value. It will allow patients to make a choice that suits their preferences.
The diary is mainly intended for those who experience problems with their medication. However, in this study, a large proportion of patients (60%) reported no problems during two months. These results are inconsistent with previous research. A study on medication self-management problems after hospital discharge in geriatric patients showed that about 90% encountered at least one problem in medication management [38]. Another study in community-dwelling adults (65+) showed that 70% of patients experienced one or more medication management problems [46]. However, these results relate only to older patients (≥65 years), who are more vulnerable to problems in medication management because of physical and cognitive decline [44]. In the present study, the diary was evaluated in a population of adult patients (18+) with an age varying between 43 and 86 years which may explain the lower percentage of problems encountered. Nevertheless, we should wonder whether they did not experience any problems or did not want to report problems. We must be aware that registering, reporting or discussing problems regarding medication use always requires a certain level of willingness and effort from the patient. Not experiencing problems or not wanting to communicate problems could explain why only half of the participants indicated that the diary has the potential to help them discuss problems with caregivers.
Furthermore, we should be aware that self-reported data in the medication diary may be subject to errors and social desirability bias. Errors in the medication scheme, for example, were minimised, since the nurse involved in the study, wrote or stuck an up-to-date scheme in the diary at discharge. However, we cannot guarantee the correctness of the schedule two months post-discharge as we did not have access to the medication list after a patient's discharge. This should be considered a limitation of the study. To minimise the risk of incorrect data, patients were advised to have any changes in their medication noted by the general practitioner or to request a new printout if changes occurred.
Most patients found the diary user-friendly and easy to fill in. However, only a limited proportion of patients actively used all elements of the medication diary. For example, only 19 patients filled out the information sheets. Furthermore, more than half of the participants have not completed the problem sheets as they did not experience medication-related problems. Consequently, we have to be cautious about conclusions regarding the user-friendliness of the diary. It is desirable to have the diary used by a larger sample of patients experiencing problems. In this regard, it would be recommended to assess whether patients experience medication self-management problems using validated tools [39,40,46].
4.1. Study limitations
First of all, only one database was searched for existing medication diaries. Therefore it is possible that not all existing diaries were identified. Secondly, the questionnaire evaluating user-friendliness and the medication diary itself relies on self-reported data, which may be subjective to social desirability bias. Thirdly, the medication diary was pilot tested by a small sample of patients, and only a limited number of participants utilized all components of the diary. Lastly, there was an overrepresentation of male respondents in our study. Both the small sample size and the lack of gender equality may limit the generalisability of the results.
4.2. Clinical relevance
Good communication between patients and healthcare providers is crucial for optimal drug treatment [[47], [48], [49]]. On the one hand, it is important that medication therapy can be aligned with the patient's needs, experiences and goals. On the other hand, healthcare providers need to know how the patient's use of medicines proceeds.
This medication diary offers the possibility of registering problems with medicines, making it easier to discuss problems with general practitioners, pharmacists, nurses or other healthcare providers. This enables healthcare providers to intervene if necessary and to tailor the pharmacotherapeutic care to the patient's needs.
5. Conclusions
The developed medication diary can potentially serve as a supportive tool for patients to report their problems regarding medication management. The user-friendliness of the diary was demonstrated. The medication diary has the potential to help discuss problems regarding medication management with healthcare providers. However, self-reporting problems related to medication requires a certain willingness from the patient.
Funding
Laura Mortelmans was supported by the Research Foundation Flanders through grant 11L0522 N. The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Arega is sponsor of the Scientific Arega Chair at the University of Antwerp. A yearly gift allows its members to plan and execute research activities with the aim to improve quality of care and quality of life for patients with polypharmacy. Tinne Dilles is holder of the scientific chair. There are no contracts with Arega on research activities. Arega has no influence on the research program or the research projects. The Scientific Arega Chair financed the production of the diary in function of the pilot test.
Ethical approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval for part 3 of the study (i.e., the evaluation of the medication diary in patients with polypharmacy) was granted by the Ethics Committee of The Antwerp University Hospital (registration number B3002021000224). All participants received information on the purpose, design and execution of the study. Written informed consent was given by all study participants.
Availability of data and material
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
CRediT authorship contribution statement
Laura Mortelmans: Writing – original draft, Visualization, Project administration, Methodology, Investigation, Funding acquisition, Formal analysis, Conceptualization. Tinne Dilles: Writing – review & editing, Supervision, Methodology, Funding acquisition, Conceptualization.
Declaration of competing interest
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests: Laura Mortelmans reports financial support was provided by Research Foundation Flanders. Tinne Dilles reports a relationship with Arega that includes: funding grants. If there are other authors, they declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
We would like to thank Ann Roelant for designing the medication diary. Furthermore, we would like to thank Jana Van Dingenen and Marjan De Graef for supporting data collection in stage 3 of the study.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.heliyon.2024.e26127.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Maddigan S.L., et al. Predictors of older adults' capacity for medication management in a self-medication program: a retrospective chart review. J. Aging Health. 2003;15(2):332–352. doi: 10.1177/0898264303251893. [DOI] [PubMed] [Google Scholar]
- 2.Bailey S.C., Oramasionwu C.U., Wolf M.S. Rethinking adherence: a health literacy-informed model of medication self-management. J. Health Commun. 2013;18(Suppl 1):20–30. doi: 10.1080/10810730.2013.825672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kripalani S., et al. Deficits in communication and information transfer between hospital-based and primary care physicians: implications for patient safety and continuity of care. JAMA. 2007;297(8):831–841. doi: 10.1001/jama.297.8.831. [DOI] [PubMed] [Google Scholar]
- 4.Pouliot A., et al. Defining and identifying concepts of medication literacy: an international perspective. Res. Soc. Adm. Pharm. 2018;14(9):797–804. doi: 10.1016/j.sapharm.2017.11.005. [DOI] [PubMed] [Google Scholar]
- 5.Spiers M.V., Kutzik D.M., Lamar M. Variation in medication understanding among the elderly. Am. J. Health Syst. Pharm. 2004;61(4):373–380. doi: 10.1093/ajhp/61.4.373. [DOI] [PubMed] [Google Scholar]
- 6.Davis T.C., et al. Low literacy impairs comprehension of prescription drug warning labels. J. Gen. Intern. Med. 2006;21(8):847–851. doi: 10.1111/j.1525-1497.2006.00529.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Davis T.C., et al. Literacy and misunderstanding prescription drug labels. Ann. Intern. Med. 2006;145(12):887–894. doi: 10.7326/0003-4819-145-12-200612190-00144. [DOI] [PubMed] [Google Scholar]
- 8.Kripalani S., et al. Predictors of medication self-management skill in a low-literacy population. J. Gen. Intern. Med. 2006;21(8):852–856. doi: 10.1111/j.1525-1497.2006.00536.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mackey L.M., et al. Self-management skills in chronic Disease management: what role does health literacy have? Med. Decis. Making. 2016;36(6):741–759. doi: 10.1177/0272989x16638330. [DOI] [PubMed] [Google Scholar]
- 10.Dijkstra N.E., et al. Medication self-management: considerations and decisions by older people living at home. Res. Soc. Adm. Pharm. 2020 doi: 10.1016/j.sapharm.2020.09.004. [DOI] [PubMed] [Google Scholar]
- 11.Sino C.G., et al. Medication management capacity in relation to cognition and self-management skills in older people on polypharmacy. J. Nutr. Health Aging. 2014;18(1):44–49. doi: 10.1007/s12603-013-0359-2. [DOI] [PubMed] [Google Scholar]
- 12.Cross A.J., et al. Interventions for improving medication-taking ability and adherence in older adults prescribed multiple medications. Cochrane Database Syst. Rev. 2020;5(5) doi: 10.1002/14651858.CD012419.pub2. Cd012419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vrijens B., et al. A new taxonomy for describing and defining adherence to medications. Br. J. Clin. Pharmacol. 2012;73(5):691–705. doi: 10.1111/j.1365-2125.2012.04167.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sabate E. World Health Organization; Geneva, Switzerland: 2003. Adherence to Long-Term Therapies: Evidence for Action. [Google Scholar]
- 15.Zelko E., Klemenc-Ketis Z., Tusek-Bunc K. Medication adherence in elderly with polypharmacy living at home: a systematic review of existing studies. Mater. Soc. Med. 2016;28(2):129–132. doi: 10.5455/msm.2016.28.129-132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mitchell B., Chong C., Lim W.K. Medication adherence 1 month after hospital discharge in medical inpatients. Intern. Med. J. 2016;46(2):185–192. doi: 10.1111/imj.12965. [DOI] [PubMed] [Google Scholar]
- 17.Fallis B.A., et al. Primary medication non-adherence after discharge from a general internal medicine service. PLoS One. 2013;8(5) doi: 10.1371/journal.pone.0061735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mira J.J., et al. A systematic review of patient medication error on self-administering medication at home. Expet Opin. Drug Saf. 2015;14(6):815–838. doi: 10.1517/14740338.2015.1026326. [DOI] [PubMed] [Google Scholar]
- 19.Aggarwal P., Woolford S.J., Patel H.P. Multi-morbidity and polypharmacy in older people: challenges and opportunities for clinical practice. Geriatrics. 2020;5(4):85. doi: 10.3390/geriatrics5040085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Marcum Z.A., Gellad W.F. Medication adherence to multidrug regimens. Clin. Geriatr. Med. 2012;28(2):287–300. doi: 10.1016/j.cger.2012.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bagge M., et al. Older people's experiences of medicine changes on leaving hospital. Res. Soc. Adm. Pharm. 2014;10(5):791–800. doi: 10.1016/j.sapharm.2013.10.005. [DOI] [PubMed] [Google Scholar]
- 22.Harris C.M., et al. What happens to the medication regimens of older adults during and after an acute hospitalization? J. Patient Saf. 2013;9(3):150–153. doi: 10.1097/PTS.0b013e318286f87d. [DOI] [PubMed] [Google Scholar]
- 23.Ziaeian B., et al. Medication reconciliation accuracy and patient understanding of intended medication changes on hospital discharge. J. Gen. Intern. Med. 2012;27(11):1513–1520. doi: 10.1007/s11606-012-2168-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pasina L., et al. Medication non-adherence among elderly patients newly discharged and receiving polypharmacy. Drugs Aging. 2014;31(4):283–289. doi: 10.1007/s40266-014-0163-7. [DOI] [PubMed] [Google Scholar]
- 25.Schoonover H., et al. Predicting potential postdischarge adverse drug events and 30-day unplanned hospital readmissions from medication regimen complexity. J. Patient Saf. 2014;10(4):186–191. doi: 10.1097/pts.0000000000000067. [DOI] [PubMed] [Google Scholar]
- 26.El Morabet N., et al. Prevalence and preventability of drug-related hospital readmissions: a systematic review. J. Am. Geriatr. Soc. 2018;66(3):602–608. doi: 10.1111/jgs.15244. [DOI] [PubMed] [Google Scholar]
- 27.World Health Organization . World Health Organization; Geneva: 2017. Medication without Harm - Global Patient Safety Challenge on Medication Safety. [Google Scholar]
- 28.LeBlanc R.G., Choi J. Optimizing medication safety in the home. Home Healthc. Nurse. 2015;33(6):313–319. doi: 10.1097/nhh.0000000000000246. [DOI] [PubMed] [Google Scholar]
- 29.Baker A. Crossing the quality chasm: a new health system for the 21st century. BMJ. 2001;323(7322):1192. doi: 10.1136/bmj.323.7322.1192. [DOI] [PubMed] [Google Scholar]
- 30.American geriatrics society expert panel on person-centered care, person-centered care: a definition and essential elements. J. Am. Geriatr. Soc. 2016;64(1):15–18. doi: 10.1111/jgs.13866. [DOI] [PubMed] [Google Scholar]
- 31.Coulter A. What do patients and the public want from primary care? Bmj. 2005;331(7526):1199–1201. doi: 10.1136/bmj.331.7526.1199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Elwyn G., et al. Implementing shared decision making in the NHS. BMJ. 2010;341:c5146. doi: 10.1136/bmj.c5146. [DOI] [PubMed] [Google Scholar]
- 33.Coulter A., Collins A. King's Fund; London: 2011. Making Shared Decision-Making a Reality; p. 621. [Google Scholar]
- 34.van Berge Henegouwen M.T., van Driel H.F., Kasteleijn-Nolst Trenité D.G. A patient diary as a tool to improve medicine compliance. Pharm. World Sci. 1999;21(1):21–24. doi: 10.1023/a:1008627824731. [DOI] [PubMed] [Google Scholar]
- 35.Sidiropoulos P., et al. Correlation of patient preferences to treatment outcomes in patients with rheumatoid arthritis treated with tumour necrosis factor inhibitors in Greece. Clin. Rheumatol. 2020;39(12):3643–3652. doi: 10.1007/s10067-020-05171-8. [DOI] [PubMed] [Google Scholar]
- 36.McCarthy D.M., et al. A multifaceted intervention to improve patient knowledge and safe use of opioids: results of the ED EMC(2) randomized controlled trial. Acad. Emerg. Med. 2019;26(12):1311–1325. doi: 10.1111/acem.13860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Heard K., et al. Accuracy of the structured medication history assessment tool (MedHAT) compared with recorded real-time medication use. Pharmacotherapy. 2016;36(5):496–504. doi: 10.1002/phar.1750. [DOI] [PubMed] [Google Scholar]
- 38.Mortelmans L., et al. What happens after hospital discharge? Deficiencies in medication management encountered by geriatric patients with polypharmacy. Int. J. Environ. Res. Publ. Health. 2021;18(13):7031. doi: 10.3390/ijerph18137031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Badawoud A.M., et al. Measuring medication self-management capacity: a scoping review of available instruments. Drugs Aging. 2020;37(7):483–501. doi: 10.1007/s40266-020-00764-z. [DOI] [PubMed] [Google Scholar]
- 40.Advinha A.M., Lopes M.J., de Oliveira-Martins S. Assessment of the elderly's functional ability to manage their medication: a systematic literature review. Int. J. Clin. Pharm. 2017;39(1):1–15. doi: 10.1007/s11096-016-0409-z. [DOI] [PubMed] [Google Scholar]
- 41.Farris K.B., Phillips B.B. Instruments assessing capacity to manage medications. Ann. Pharmacother. 2008;42(7):1026–1036. doi: 10.1345/aph.1G502. [DOI] [PubMed] [Google Scholar]
- 42.Elliott R.A., Marriott J.L. Standardised assessment of patients' capacity to manage medications: a systematic review of published instruments. BMC Geriatr. 2009;9:27. doi: 10.1186/1471-2318-9-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Vlaanderen Statistiek. Mediabezit. 2022 https://www.vlaanderen.be/statistiek-vlaanderen/media-en-mediagebruik/mediabezit [Google Scholar]
- 44.Barnett K., et al. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet. 2012;380(9836):37–43. doi: 10.1016/s0140-6736(12)60240-2. [DOI] [PubMed] [Google Scholar]
- 45.Fried T.R., et al. Health outcomes associated with polypharmacy in community-dwelling older adults: a systematic review. J. Am. Geriatr. Soc. 2014;62(12):2261–2272. doi: 10.1111/jgs.13153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Orwig D., Brandt N., Gruber-Baldini A.L. Medication management assessment for older adults in the community. Gerontol. 2006;46(5):661–668. doi: 10.1093/geront/46.5.661. [DOI] [PubMed] [Google Scholar]
- 47.Parker L., et al. Medications and doctor–patient communication. Australian Journal for General Practitioners. 2021;50:709–714. doi: 10.31128/AJGP-05-21-5973. [DOI] [PubMed] [Google Scholar]
- 48.Ryan R., et al. Interventions to improve safe and effective medicines use by consumers: an overview of systematic reviews. Cochrane Database Syst. Rev. 2014;2014(4) doi: 10.1002/14651858.CD007768.pub3. Cd007768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Australian Commission on Safety and Quality in Health Care . ACSQHC; Sydney: 2020. Medication without Harm - WHO Global Patient Safety Challenge - Australia's Response. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.