Abstract
Introduction
This scoping review aims to highlight key social determinants of health associated with breast cancer screening behavior in United States women aged ≥40 years old, identify public and private databases with SDOH data at city, state, and national levels, and share lessons learned from United States based observational studies in addressing SDOH in underserved women influencing breast cancer screening behaviors.
Methods
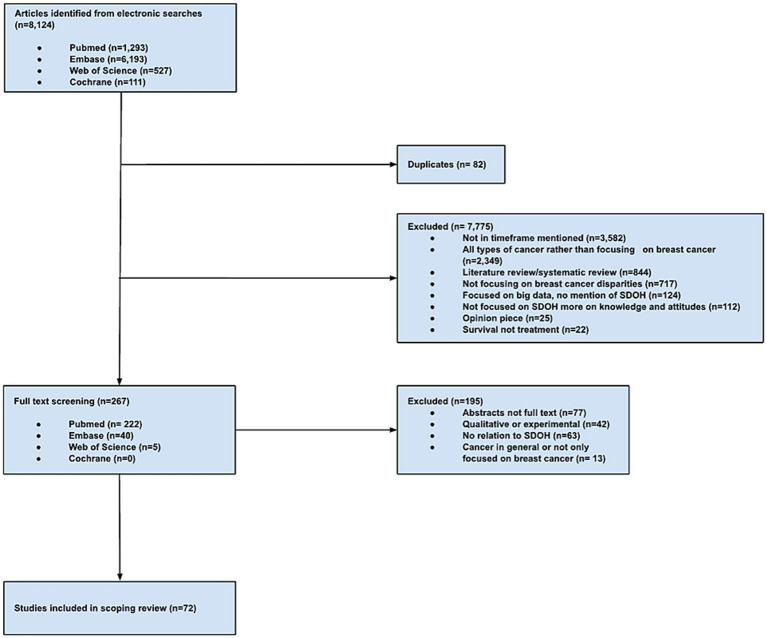
The Arksey and O’Malley York methodology was used as guidance for this review: (1) identifying research questions; (2) searching for relevant studies; (3) selecting studies relevant to the research questions; (4) charting the data; and (5) collating, summarizing, and reporting results.
Results
The 72 included studies were published between 2013 and 2023. Among the various SDOH identified, those related to socioeconomic status (n = 96) exhibited the highest frequency. The Health Care Access and Quality category was reported in the highest number of studies (n = 44; 61%), showing its statistical significance in relation to access to mammography. Insurance status was the most reported sub-categorical factor of Health Care Access and Quality.
Discussion
Results may inform future evidence-based interventions aiming to address the underlying factors contributing to low screening rates for breast cancer in the United States.
Keywords: social determinants of health, breast cancer screening, mammography, health inequities, underserved women, United States
Introduction
The social determinants of health (SDOH) are factors outside of the realm of medicine that impact health outcomes and quality of life on a daily basis (1). According to the World Health Organization (WHO), SDOH are defined as “the conditions in which people are born, grow, work, live, and age, and the wider set of forces and systems shaping the conditions of daily life (1).” These determinants of health can be divided into five categories: economic stability, education access and quality, health care access and quality, neighborhood and built environment, and social and community context (2). While factors within each of these categories can individually impact a different facet of a person’s health, these categories often also work collectively to create facilitators and barriers to healthy behaviors and health outcomes (1–3). Such SDOH play a significant role in creating new and worsening existing healthcare disparities and may exhibit a stronger influence on health and well-being than the care received by providers and healthcare organizations (4).
One of the most influential roles of SDOH lies within the realm of equitable access to cancer care (4–7). Specifically, when considering breast cancer, there is significant evidence that supports the influence of SDOH on screening. Despite the presence of innovative screening and treatment strategies, breast cancer remains the second most common type of cancer and is a leading cause of disability and mortality in the United States (8). Breast cancer screening, through mammography and clinical breast examination, is the method of primary prevention that is recommended by the United States Preventive Service Task Force (9). However, research studies showed that health disparities persist, as minority women within the United States are less likely to take advantage of breast cancer screening methods (10–14). Though these studies assessed primarily the role of race and ethnicity on breast cancer screening behaviors, they all found that reported associations were mediated by other SDOH such as quality of health care, education, family income, and health insurance (11–14). Hence, there is a need to explore and understand which determinants act as significant influential factors contributing to low breast cancer screening behaviors. This scoping review aims to highlight key SDOH associated with breast cancer screening behavior in United States women aged ≥40 years old, identify public and private databases with SDOH data at city, state, and national levels, and share lessons learned from United States based observational studies in addressing SDOH in underserved women influencing breast cancer screening behaviors. Findings can guide researchers, physicians, and community workers in improving accessibility, affordability, and quality of breast cancer screening opportunities through culturally competent strategies tailored to satisfy the needs of the at-risk female population group.
Methods
The review team consisted of a multidisciplinary team of health professionals with extensive knowledge on the role of SDOH in minority populations. The Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) was utilized as a reference checklist for the sections of this study (15). The Arksey and O’Malley (16) York methodology was used as guidance for this review. This framework employs five steps: (1) identifying research questions; (2) searching for relevant studies; (3) selecting studies relevant to the research questions; (4) charting the data; and (5) collating, summarizing, and reporting results (16). These methods ensure transparency, permits replicability of the search strategy, and increases the reliability of study findings.
Step 1: identifying research questions
Three research questions were used for this scoping review: (1) What are the major SDOH hindering breast cancer screening in United States women aged > = 40?; (2) What were the major databases/data sources used to capture SDOH data to assess its influence on breast cancer screening behaviors in United States women?; and (3) What are the lessons learned for future recommendations to address SDOH in underserved women at-risk for the disease?
Step 2: searching for relevant articles
Keywords and MeSH terms were developed in collaboration with a research librarian (MK) who is an expert in scoping review protocols. Search terms included: breast cancer, breast cancer screening, mammography, race/ethnicity, education level, income, housing instability, insurance coverage, language preferences, health equity, health disparities, and medically underserved communities, among others. Four electronic databases (PubMed, Embase, Web of Science, and Cochrane) were selected due to their breadth and focus on psychosocial and behavioral aspects of chronic illnesses. These databases were searched to identify peer-reviewed literature from primary data sources, secondary data sources, and case reports. The review of the literature was completed over a period of 3 months, from January 2023 to March 2023. The screening of these articles was carried out by senior author (LS) and co-authors (VJ, DL, GO, YZ, SB, AM, SD, MR, and DD).
Inclusion criteria
The articles that were included were peer-reviewed observational studies, published in English between 2013 and 2023 that focused on the SDOH, including race/ethnicity, employment, education, food security, insurance status, housing, and access to quality healthcare. These observational studies specifically focused on assessing the significance of the role of SDOH in creating health inequities in breast cancer screenings, particularly for women who are 40 years or older, and are at-risk or have been diagnosed with breast cancer. The ≥40 years old age cut-off was selected based on the American Cancer Society recommended guidelines for screening, which highlight that (1) women between 40 and 44 have the option to start screening with a mammogram every year; (2) women 45–54 should get mammograms every year; and (3) women 55 and older can switch to a mammogram every other year, or they can choose to continue yearly mammograms (17).
Exclusion criteria
Excluded studies encompass narrative, scoping, and systematic reviews, as well as qualitative, descriptive, and experimental studies. Additionally, articles were excluded if they did not focus on SDOH as influential factors of breast cancer screening behavior, were assessing knowledge and attitudes rather than exploring SDOH as influencing factors of breast cancer screening, were discussing interventions addressing low breast cancer screening rates and associated disparities that might be related to SDOH, were focusing on survival and mortality rather than screening, and were looking at guideline adherence rather than breast cancer screening behavior itself. Datasets with data collected prior to 2005 were not included in the review.
Step 3: selecting studies relevant to the research questions
All co-authors (VJ, DL, GO, YZ, SB, AM, SD, MR, and DD) extracted, summarized, and tabulated the data from relevant studies. The senior author (LS) reviewed all tabulated data for accuracy and to resolve any discrepancies. Summary tables included an evidence table (Table 1) describing study characteristics, types of SDOH, and outcomes. Types of SDOH were first listed and then categorized based on Healthy People 2030 into five categories: Economic Stability, Education Access and Quality, Health Care Access and Quality, Neighborhood and Built Environment, and Social and Community Context (18). The Healthy People 2030 is a set of science-based objectives with targets to monitor progress and motivate and focus action (18). The Healthy People 2030 first introduced SDOH objectives in 2010, following the World Health Organization’s (WHO) call to address SDOH to maintain health and quality of life (18). The five categories listed reflect the social conditions and environments that are shaped by a wider set of forces and influence behavioral outcomes (18).
Table 1.
Study characteristics.
| Article # | Primary Author/Year | Study design | Sample size | Study population | Age range | Study purpose | Type of SDOH | SDOH category based on HP 2030 | Association between SDOH and Outcome (Significant/non-significant)* | Type of methodology/Analysis used |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Agenor et al. (2020) | Cross-sectional study | n = 45,031 | National Health Interview Survey Female Respondents | 40–75 years old | To examine odds in receiving a mammogram in relationship to sexual orientation across racial/ethnic groups | Race/Ethnicity | Social and community context | Significant | Adjusted Wald tests, Logistic regression |
| Sexual orientation | Social and community context | Significant | ||||||||
| 2 | Agrawal et al. (2021) | Cross-sectional study | n = 919 | African American church going women from Houston, Texas | 40–86 years old | To examine factors associated with adherence to the National Comprehensive Cancer Network breast cancer screening guidelines | Race/Ethnicity | Social and community context | Significant | T-test, Chi-square, Logistic regression |
| 3 | Alabdullatif et al. (2022) | Cross-sectional study | n = 94,290 | National Health Interview Survey female respondents | ≥40 years old | To examine the association between IT based health care communication and mammography utilization as modified by race/ethnicity/age | Race/Ethnicity | Social and community context | Significant | Logistic regression, Trend analysis |
| Age | ||||||||||
| 4 | Alatrash et al. (2021) | Cross-sectional study | n = 316 | Muslim and Christian Arab American Women from Jordan, Lebanon, and Egypt | ≥40 years old | To examine associations of sociodemographic characteristics with perceived benefits and barriers to mammogram screening | Race/Ethnicity | Social and community context | Significant | Fishers exact test, Bonferroni post hoc test, Chi-square test, and OR test |
| 5 | Anderson et al. (2014) | Cross-sectional study | n = 138 | Central cancer registry data linked to Medicare claims from three Appalachian states (Pennsylvania, Ohio, and Kentucky) | ≥65 years old | To examine the relationship of an area-based measure of breast cancer screening and geographic area deprivation on the incidence of later stage breast cancer across a diverse region of Appalachia | Economic status | Economic stability | Significant | Exploratory spatial data analysis, multivariate regression, and linear regression |
| Insurance status | Health care access and quality | Significant | ||||||||
| 6 | Asgary et al. (2014) | Cross-sectional study | n = 100 | Homeless women that received services at Barbara Kleinman Shelter in Brooklyn and Bowery Residence Committee’s Safe Haven at least three times between 2010 and 2012 | 50–74 years old | To evaluate and compare rates and predictors of mammograms in homeless and low-income domicile patients | Income | Economic stability | Non-significant | T-test, Multivariable logistic regression |
| Insurance status | Health care access and quality | Non-significant | ||||||||
| Housing | Neighborhood and built environment | Non-significant | ||||||||
| Race | Social and community context | Non-significant | ||||||||
| Age | Social and community context | Non-significant | ||||||||
| Access to provider counseling | Health care access and quality | Significant | ||||||||
| History of mental illness | Social and community context | Non-significant | ||||||||
| Substance/alcohol abuse | Social and community context | Non-significant | ||||||||
| HIV status | Social and community context | Non-significant | ||||||||
| 7 | Ayanian et al. (2013) | Cross-sectional study | n = 577,316 | Medicaid beneficiaries in 2009 | 65–69 years old | To examine use of mammography in relation to race/ethnicity in Medicare health maintenance organizations, PPO, and traditional Medicare | Income | Economic stability | Significant | Logistic regression |
| Insurance status | Health care access and quality | Significant | ||||||||
| Race/Ethnicity | Social and community context | Significant | ||||||||
| Area of residence | Neighborhood and built environment | Significant | ||||||||
| 8 | Balazy et al. (2019) | Retrospective Cohort study | n = 1,057 | Single institution women undergoing breast radiotherapy from 2012 to 2017 | 56–60 years old | To examine whether non-English speaking patients present at a later stage than their respective English-speaking counterparts and whether language is associated with mammographic screening | Language | Social and community context | Significant | Ordinal logistic regression, Trend analysis |
| Race/Ethnicity | Social and community context | Significant | ||||||||
| Age | Social and community context | Significant | ||||||||
| 9 | Beaber et al. (2016) | Cohort study | n = 3,413 | Women from Geisel School of Medicine and Brigham and Women’s Hospital primary care networks from 2011 to 2013 | ≥40 years old | To evaluate factors influencing when women begin screening after turning 40 years of age within a network of primary care practices | Race/Ethnicity | Social and community context | Non-significant | Kaplan–Meier cumulative incidence, Cox proportional hazards regression |
| Access to healthcare providers | Health care access and quality | Significant | ||||||||
| Health insurance | Health care access and quality | Significant | ||||||||
| Household income | Economic stability | Significant | ||||||||
| Zip code | Neighborhood and built environment | Significant | ||||||||
| 10 | Beaber et al. (2019) | Cohort study | n = 51,241 | 10 PROSPR sites with women receiving first mammograms in 2011 | 50–74 years old | To evaluate multilevel predictors of non-adherence among screened women | Age | Social and community context | Significant | Logistic regression, Multivariable analysis |
| Race/Ethnicity | Social and community context | Significant | ||||||||
| Zip code | Neighborhood and built environment | Non-significant | ||||||||
| Median income | Economic stability | Non-significant | ||||||||
| 11 | Calo et al. (2016) | Cross-sectional study | n = 1,541 | Participants of 2010 Houston Survey and contextual data from United States Census | 40–74 years old | To evaluate associations between area level socioeconomic measures and mammography screening among a racially and ethnically diverse sample of women in Texas | Age | Social and community context | Significant | Chi-square test, Two level random intercept regression model, Bivariate analysis, and Multivariable analyses |
| Insurance | Health care access and quality | Significant | ||||||||
| Income | Economic stability | Significant | ||||||||
| Education | Education access and quality | Significant | ||||||||
| Race/Ethnicity | Social and community context | Significant | ||||||||
| Housing | Neighborhood and built environment | Significant | ||||||||
| 12 | Castaneda et al. (2014) | Cross-sectional study | n = 208 | Survey through UCSD health system | ≥40 years old | To examine factors associated with mammography screening utilization among middle-aged Latinas | Age | Social and community context | Significant | Exploratory factor analysis, Logistic regression |
| Income | Economic stability | Significant | ||||||||
| Education | Education access and quality | Significant | ||||||||
| Language | Social and community context | Significant | ||||||||
| Race/Ethnicity | Social and community context | Significant | ||||||||
| 13 | Cataneo et al. (2022) | Cross-sectional study | n = 22,825 | LEP and English-speaking female participants who filled the NHIS survey in 2015 | 40–75 years old | To evaluate the impact of limited language proficiency in screening for breast cancer | Language | Social and community context | Significant | Linear regression, Chi-square test, and Stepwise multivariate regression analysis |
| Income | Economic stability | Significant | ||||||||
| Insurance | Health care access and quality | Significant | ||||||||
| Access to primary care providers | Health care access and quality | Significant | ||||||||
| Race/Ethnicity | Social and community context | Significant | ||||||||
| 14 | Chandak et al. (2019) | Retrospective cross-sectional study | n = 7,673 | Women diagnosed with breast cancer between 2008 and 2012 as noted in the Nebraska Cancer Registry | 40–70 years old | To examine rural–urban differences in access to breast cancer screening in a predominantly rural Midwestern state in the United States | Geographic location | Neighborhood and community context | Significant | Spatial analysis, Hot spot analysis |
| Access to mammography facilities | Health care access and quality | Significant | ||||||||
| Age | Social and community context | Significant | ||||||||
| 15 | Christensen et al. (2023) | Retrospective cross-sectional study | n = 457,476 | 5% sample of American Indian and White women receiving Medicare fee-for-service in AZ, CA, NY, MX, OK, and WA | 40–89 years old | To examine the impact of urbanicity and income on receiving mammography for American Indian women compared with that for White women | Race | Social and community context | Significant | Multivariable logistic regression analysis, Linear regression |
| Income | Economic stability | Significant | ||||||||
| Neighborhood | Neighborhood and built environment | Significant | ||||||||
| 16 | Clark et al. (2017) | Cohort study | n = 48,234 | Women who received digital breast tomosynthesis (DBT) from 22 primary care centers in the Dartmouth-Brigham and Women’s Hospital Population-based Research Optimizing Screening through Personalized Regimens research center (PROSPR) | 49–65 years old | To examine DBT trends and estimated associations with insurance type | Insurance type | Health care access and quality | Significant | Descriptive statistics, Repeated measures analysis using generalized estimating equations (GEE) |
| Zip code | Neighborhood and built environment | Non-significant | ||||||||
| Race | Social and community context | Non-significant | ||||||||
| Neighborhood household income | Neighborhood and built environment/Economic stability | Non-significant | ||||||||
| Age | Social and community context | Non-significant | ||||||||
| 17 | Clarke et al. (2019) | Cross-sectional study | n = 29,951 | Women who participated in the 2005, 2008, 2010, 2013, and 2015 National Health Interview Survey | 50–74 years old | To present national estimates of mammography screening among women by nativity, birthplace, and percentage of lifetime living in the United States (U.S.) | Birthplace | Neighborhood and built environment | Non-significant | Descriptive Statistics, Two-sided t tests |
| Citizenship | Social and community context | Non-significant | ||||||||
| Length of time in the United States | Social and community context | Non-significant | ||||||||
| Age | Social and community context | Non-significant | ||||||||
| Race/Ethnicity | Social and community context | Non-significant | ||||||||
| Educational attainment | Education access and quality | Non-significant | ||||||||
| Poverty status | Economic stability | Non-significant | ||||||||
| Health insurance | Health Care Access and Quality | Non-Significant | ||||||||
| 18 | Davis et al. (2017) | Cross-sectional study | n = 758 | Patients presenting to radiology department for routine screening mammography from December 2016 to February 2017 | > 40 years old | To clarify why late screening might occur in an at-risk population | Race/Ethnicity | Social and community context | Significant | Descriptive statistics, Univariate logistic regression, and Multivariate logistic regression |
| Age | Social and community context | Significant | ||||||||
| Employment status | Economic stability | Significant | ||||||||
| Income | Economic stability | Significant | ||||||||
| Insurance status | Health care access and quality | Significant | ||||||||
| Access to mammography | Health care access and quality | Significant | ||||||||
| Education level | Education access and quality | Significant | ||||||||
| 19 | Dong et al. (2022) | Case–control study | n = 33,537 | Patients diagnosed with invasive breast cancer from the Ohio Cancer Incidence Surveillance System between 2010 and 2017 | 40–64 years old | To examine whether there were reductions in geospatial disparities in advanced stage breast cancer at diagnosis in Ohio after Medicaid expansion | Area of residence | Neighborhood and built environment | Significant | Space–time scan statistic in SaTScan |
| Household income | Economic stability | Significant | ||||||||
| Medicaid coverage | Health care access and quality | Significant | ||||||||
| Education level | Education access and quality | Significant | ||||||||
| Household vehicle availability | Economic stability/Social and community context | Significant | ||||||||
| Insurance coverage | Health care access and quality | Significant | ||||||||
| 20 | Duggan et al. (2019) | Cross-sectional study | n = 240 | Residents of two adjacent rural counties in Lower Yakima Valley in eastern Washington state who self-identify as Latina or Non-Latina white | ≥40 years old | To examine county-level difference, stratified by ethnicity, of predictor of breast-screening utilization in rural underserved communities | Race/Ethnicity | Social and community context | Non-significant | Multivariate logistic regression |
| Education level | Education access and quality | Significant | ||||||||
| Income | Economic stability | Non-significant | ||||||||
| County of residence | Neighborhood and built environment | Significant | ||||||||
| Access to clinic | Health care access and quality | Significant | ||||||||
| Age | Social and community context | Significant | ||||||||
| 21 | Elkin et al. (2014) | Cross-sectional study | n = 1,749 | Adult women attending mammography facilities certified by the FDA under the Mammography Quality Standards Act (MQSA) in six states in 2011 | ≥ 40 | To survey certified mammography facilities in CA, CT, GA, IA, NM, and NY regarding wait times for next available screening, availability of evening and weekend appointments and digital mammography, and insurance copayment requirements | Access to mammography facilities | Health care access and quality | Significant | Chi-square tests |
| Insurance copayments | Health care access and quality | Significant | ||||||||
| 22 | Fedewa et al. (2016) | Cross-sectional study | n = 18,459 | Women aged ≥40 years from the 2008 and 2013 National Health Interview Surveys | ≥ 40 years old | To examine changes in nationwide mammography prevalence and physician recommendation among younger (≥ 40) and older (≥ 75) women by insurance and SES before and after the 2009 USPSTF BC screening guidelines | Insurance status | Health care access and quality | Significant (for younger women) | Chi-square tests, Logistic regression models |
| Income | Economic stability | Significant (for younger women) | ||||||||
| Age | Social and community context | Significant (for younger women) | ||||||||
| Race/Ethnicity | Social and community context | Significant (for younger women) | ||||||||
| Birthplace | Neighborhood and built environment | Significant (for younger women) | ||||||||
| Education | Education access and quality | Significant (for younger women) | ||||||||
| 23 | Flores et al. (2018) | Cohort study | n = 9,575 | Women who underwent screening mammography in 2005 at Harvard Medical School’s main campus and all affiliated community imaging sites | 50–64 years old | To evaluate the association between PCP, contact and longitudinal adherence with screening mammography guidelines over a 10-year period across different racial/ethnic groups | Race/Ethnicity | Social and community context | Non-significant | Generalized estimating equations, Logistic regression, Linear regression, and Wald chunk tests |
| Age | Social and community context | Non-significant | ||||||||
| Primary language | Social and community context | Non-significant | ||||||||
| Insurance status | Health care access and quality | Significant | ||||||||
| Level of primary care physician interaction | Health care access and quality | Significant | ||||||||
| 24 | Guo et al. (2019) | Cohort study | n = 3,911 | African American participants of the Study on Women’s Health Across the Nation (SWAN) | 45–63 years old | To analyze economic, social, and psychological factors associated with African American women’s adherence to the recommended breast cancer screening guidelines during their mid-age period | Age | Social and community context | Significant | Multinomial logistic regression |
| Quality of life | Social and community context | Significant | ||||||||
| Employment | Economic stability | Significant | ||||||||
| Education | Education access and quality | Significant | ||||||||
| Family income | Economic stability | Significant | ||||||||
| Access to healthcare provider | Health care access and quality | Significant | ||||||||
| Transportation access | Neighborhood and built environment | Significant | ||||||||
| 25 | Henderson et al. (2015) | Cohort study | n = 256,470 | Black and white female patients enrolled in the Carolina Mammography Registry from 2005 to 2010 | ≥ 40 years old | To determine if digital screening mammography performs equally well in black and white women | Race | Social and community context | Non-significant | Computed mammography sensitivity, specificity, and positive predictive value (PPV1), random effects logistic regression model, and Chi-square test |
| Education level | Education access and quality | Non-significant | ||||||||
| Rural/urban area of residence | Neighborhood and built environment | Non-significant | ||||||||
| Age | Social and community context | Non-significant | ||||||||
| 26 | Henderson et al. (2020) | Cross-sectional study | n = 393,430 | Women ages ≥40 years receiving screening mammography across three Breast Cancer Surveillance Consortium registries from 2012 to 2017 | ≥ 40 years old | To evaluate barriers to receiving health care, focusing on caretaker responsibilities, health insurance and cost, and transportation | Age | Social and community context | Significant | Chi-square tests, Multivariate logistic regression, and Wald test |
| Race/Ethnicity | Social and community context | Significant | ||||||||
| Education | Education access and quality | Significant | ||||||||
| Family/Personal history of breast cancer | Social and community context | Significant | ||||||||
| Income | Economic stability | Significant | ||||||||
| Health insurance costs | Health care access and quality | Significant | ||||||||
| Internet access | Neighborhood and built environment | Significant | ||||||||
| Local unemployment rate | Economic stability | Significant | ||||||||
| English language proficiency | Social and community context/education access and quality | Significant | ||||||||
| 27 | Henry et al. (2014) | Cross-sectional study | n = 5,197 | Women who received mammography from 2008 to 2010 according to the Utah Behavioral Risk Factor Surveillance System | 40–74 years old | To investigate possible pre-disposing and enabling factors associated with nonadherence to screening guidelines among Utah women 40 years and older using survey data from the Utah Behavioral Risk Factor Surveillance System (BRFSS) | Health care access | Health care access and quality | Non-significant | Descriptive statistics, Bivariate analysis, Wald chi-square tests, and Multivariable logistic regression models |
| Age | Social and community context | Significant | ||||||||
| Health insurance | Health care access and quality | Significant | ||||||||
| Income | Economic stability | Significant | ||||||||
| Having a regular physician | Health care access and quality | Significant | ||||||||
| Travel time to nearest facility | Neighborhood and built environment | Non-significant | ||||||||
| 28 | Hong et al. (2018) | Cross-sectional study | n = 196 | Korean American women residing in the Chicago metropolitan area | 50–74 years old | To identify the relationship between perceived discrimination, trust, and breast cancer screening adherence specifically among Korean American (KA) women | Perceived discrimination | Social and community context | Non-significant | Multiple logistic regressions, Firth logistic regressions |
| Trust in health care providers/health care systems | Social and community context | Significant | ||||||||
| Cultural beliefs | Social and community context | Non-significant | ||||||||
| 29 | Hubbard et al. (2016) | Cohort study | n = 49,775 | Medicare-enrolled women who underwent a screening mammogram within a registered Breast Cancer Surveillance Consortium (BCSC) program | 66–75 years old | To investigate the sociodemographic factors influencing adherence to screening mammography among older women | Age | Social and community context | Significant | Multivariable logistic regression, Cox proportional hazards regression, and Kaplan–Meier curves |
| Income | Economic stability | Significant | ||||||||
| Education | Education access and quality | Significant | ||||||||
| Health Literacy | Education access and quality | Significant | ||||||||
| Access to healthcare | Health care access and quality | Significant | ||||||||
| Diversity index | Social and community context | Significant | ||||||||
| Public transportation expenditures | Neighborhood and built environment | Significant | ||||||||
| 30 | Jena et al. (2017) | Cohort study | n = 95,661 | Women with individual-subscriber or employer-supplemented MA insurance provided through Kaiser | ≥65 years old | To examine the impact of eliminating cost sharing for screening mammography on mammography rates | Age | Social and community context | Significant | Propensity score method, Multivariate logistic regression |
| Race/Ethnicity | Social and community context | Non-significant | ||||||||
| Insurance status | Health care access and quality | Significant | ||||||||
| Neighborhood socioeconomic status | Social and community context/Economic stability | Non-significant | ||||||||
| 31 | Jensen et al. (2022) | Cross-sectional study | n = 2,065 | Low-income, uninsured, or under-insured women in West Texas who were served by the Access to Breast Care for West Texas (ABC4WT) program | 40–49 years old | To identify sociodemographic barriers and determinants for breast cancer screenings, as well as screening outcomes, in low-income, uninsured, or under-insured communities in West Texas | Age | Social and community context | Non-significant | Pearson’s Chi-square test, T-tests, and Multivariate logistic regression analysis |
| Race/Ethnicity | Social and community context | Non-significant | ||||||||
| Monthly income | Economic stability | Non-significant | ||||||||
| County of residence | Social and community context | Non-significant | ||||||||
| 32 | Jin et al. (2019) | Cross-sectional study | n = 303 | Korean American women in the Atlanta metropolitan area | 50–80 years old | To investigate the factors linked to mammography screening among Korean American women in the state of Georgia, United States | Health literacy | Education access and quality | Significant | Pearson Chi-square, T-tests, Multiple logistic regression |
| Health beliefs | Social and community context | Significant | ||||||||
| Education | Education access and quality | Significant | ||||||||
| Age | Social and community context | Significant | ||||||||
| Income | Economic stability | Significant | ||||||||
| Insurance status | Health care access and quality | Significant | ||||||||
| 33 | Johnson et al. (2021) | Case–control study | n = 3,271 | Idaho residents with ductal carcinoma in situ or invasive breast cancer | 50–64 years old | To assess the time from breast cancer diagnosis to treatment for women enrolled in Idaho’s Women’s Health Check (WHC) Program compared to other female Idaho residents with breast cancer | Socioeconomic status | Economic stability | Non-significant | Chi-square statistics, Stratified Wilcoxon (Van Elteren) tests, Quantile regression |
| Age | Social and community context | Non-significant | ||||||||
| Race/Ethnicity | Social and community context | Non-significant | ||||||||
| Census trace poverty | Economic Stability | Non-significant | ||||||||
| 34 | Kadivar et al. (2016) | Cross-sectional study | n = 4,249 | Hispanic and non-Hispanic United States-born white women who participated in the National Assessment of Adult Literacy | ≥40 years old | To investigate the connection between functional health literacy and mammography utilization among Hispanic women, in comparison to non-Hispanic White women in the United States | Health literacy | Education access and quality | Significant | Chi-square test, MML probit regression model |
| Income | Economic stability | Significant | ||||||||
| Age | Social and community context | Significant | ||||||||
| Medical insurance | Health care access and quality | Significant | ||||||||
| Race/Ethnicity | Social and community context | Significant | ||||||||
| 35 | Kempe et el. (2013) | Retrospective cohort study | n = 47,946 | Medically insured women who had not undergone a mammogram in the past 24 months | 52–69 years old | To identify the various factors such as race/ethnicity, socioeconomic characteristics, and health status of women who were not screened for breast cancer in an insured population | Age | Social and community context | Significant | Poisson regression models |
| Race/Ethnicity | Social and community context | Significant | ||||||||
| Language preference | Social and community context | Significant | ||||||||
| Insurance | Health care access and quality | Significant | ||||||||
| Primary care encounters | Health care access and quality | Significant | ||||||||
| Specialty encounters | Health care access and quality | Significant | ||||||||
| 36 | Khaliq et al. (2015) | Cross-sectional study | n = 250 | Hospitalized women | 50–75 years old | To explore the sociodemographic and clinical factors associated with non-adherence to breast cancer screening among hospitalized women | Race | Social and community context | Non-significant | Logistic regression, Unpaired t-test, and Chi square tests |
| Education | Education access and quality | Significant | ||||||||
| Annual household income | Economic stability | Significant | ||||||||
| Access to primary care physician | Health care access and quality | Significant | ||||||||
| Age | Social and community context | Non-significant | ||||||||
| 37 | Kim et al. (2019) | Retrospective cross-sectional study | n = 127,298 | Females participating in the American Community Survey and Robert Wood Johnson Foundation 500 | 50–74 years old | To evaluate disparities in city-level screening mammography utilization and to identify factors that may impact urban screening utilization | Zip Code/Geography | Neighborhood and built environment | Significant | Mann–Whitney U test, Tukey–Kramer multiple comparison correction, and Spearman rank correlation |
| Health insurance | Healthcare access and quality | Significant | ||||||||
| Median income level | Economic stability | Significant | ||||||||
| Poverty | Economic stability | Significant | ||||||||
| Race | Social and community context | Significant | ||||||||
| 38 | Kim et al. (2022) | Cross-sectional study | n = 497,600 | Females across the United States who participated in the Behavioral Risk Factor Surveillance System in 2012, 2014, 2016, and 2018 | 50–74 years old | To explore the association between diabetes and mammography screening and whether the association varied between racial, ethnic, and geographical groups | Age | Social and community context | Significant | Logistic regression models |
| Race | Social and community context | Significant | ||||||||
| Ethnicity | Social and community context | Significant | ||||||||
| Employment | Economic stability | Significant | ||||||||
| Education | Education access and quality | Significant | ||||||||
| Zip Code/Geography | Neighborhood and built environment | Significant | ||||||||
| Median income level | Economic stability | Significant | ||||||||
| Health care coverage | Healthcare access and quality | Significant | ||||||||
| 39 | Komenaka et al. (2015) | Cross-sectional study | n = 1,664 | All female patients seen in the Maricopa Medical Center Breast Clinic in Phoenix, Arizona | ≥40 years old | To investigate the relationship of health literacy and screening mammography | Age | Social and community context | Significant | Two-sample t test, Fisher’s exact test, and Logistic regression analysis |
| Race | Social and community context | Significant | ||||||||
| Ethnicity | Social and community context | Significant | ||||||||
| Education | Education access and quality | Significant | ||||||||
| Employment status | Economic stability | Significant | ||||||||
| Insurance status | Healthcare access and quality | Significant | ||||||||
| English as primary language | Social and community context | Significant | ||||||||
| 40 | Kosog et al. (2020) | Retrospective cross-sectional study | n = 1,161 | Female patients from a single FQHC in a major metropolitan city (Chicago, IL) | 50–74 years old | To identify an association between sociodemographic factors and breast cancer screening adherence in FQHC patients including the homeless | Age | Social and community context | Non-significant | Multivariate logistic regression |
| Ethnicity | Social and community context | Non-significant | ||||||||
| Primary insurance policy | Healthcare access and quality | Significant | ||||||||
| Homelessness status | Economic stability | Significant | ||||||||
| Language | Social and community context | Non-significant | ||||||||
| Race | Social and community context | Non-significant | ||||||||
| 41 | Lapeyrouse et al. (2017) | Cross-sectional study | n = 304 | Female Latina participants in 2009–2010 ecological household study | >40 years old | To investigate whether differences in ever having a mammogram exist between Latina border residents by health insurance status, to determine whether those Latinas who reported ever having a mammogram vary by healthcare system, and to investigate the ranking of cost, trust, and familiarity as primary reasons for solely seeking health care in the United States or Mexico | Acculturation | Social and community context | Significant | Frequency statistics, Two-proportion z-test, Binary logistic regression, T-tests, and Chi squared tests |
| Age | Social and community context | Significant | ||||||||
| Ethnicity | Social and community context | Significant | ||||||||
| Education | Education access and quality | Non-significant | ||||||||
| Income | Economic stability | Non-significant | ||||||||
| Health insurance status | Healthcare access and quality | Significant | ||||||||
| 42 | Lawson et al. (2021) | Retrospective cohort study | n = 7,047 | Females diagnosed with breast cancer in Western Washington state | 40–74 years old | To determine factors associated with receipt of screening mammography by insured women before breast cancer diagnosis, and subsequent outcomes | Age | Social and community context | Significant | Multivariable logistic regression analysis, Univariable logistic regression models, Kaplan Meier estimator, Log rank test, and Cox proportional hazards model |
| Race | Social and community context | Significant | ||||||||
| Ethnicity | Social and community context | Significant | ||||||||
| Zip Code/Geography | Neighborhood and built environment | Significant | ||||||||
| Socioeconomic Disadvantage | Economic stability | Significant | ||||||||
| 43 | Lee et al. (2016) | Cross-sectional study | n = 799,467 | Females who had mammograms performed across five BCSC regional facilities from 2011 to 2012 | ≥40 years old | To compare on-site availability of advanced breast imaging services between imaging facilities serving vulnerable patient populations and those serving non-vulnerable populations | Race | Social and community context | Non-significant | Adjusted log binomial generalized estimating equations |
| Ethnicity | Social and community context | Non-significant | ||||||||
| Household income | Economic stability | Non-significant | ||||||||
| Rural/Urban residence, zip code | Neighborhood and built environment | Non-significant | ||||||||
| Education | Education access and quality | Non-significant | ||||||||
| Access to mammography facilities | Healthcare access and quality | Non-significant | ||||||||
| 44 | Lee et al. (2017) | Cross-sectional study | n = 168 | Korean American females in the Midwest | 40–79 years old | To investigate breast cancer screening rates and its associated factors in Korean-American immigrant women | Age | Social and community context | Significant | Hierarchical logistic regression analysis |
| Race | Social and community context | Significant | ||||||||
| Ethnicity | Social and community context | Significant | ||||||||
| Healthcare accessibility | Healthcare access and quality | Significant | ||||||||
| Income | Economic stability | Significant | ||||||||
| Education | Education access and quality | Significant | ||||||||
| Language | Social and community context | Significant | ||||||||
| Health care literacy | Healthcare access and quality | Significant | ||||||||
| 45 | Lee et al. (2021) | Cross-sectional study | n = 2,313,118 | Females attending Breast Cancer Surveillance Consortium affiliated imaging facilities | 40–89 years old | To determine women’s access to and use of DBT screening based on race/ethnicity, educational attainment, and income | Access to DBT | Healthcare access and quality | Significant | Descriptive statistics, Log-binomial regression models, and three-step generalized estimated equations |
| Race | Social and community context | Significant | ||||||||
| Ethnicity | Social and community context | Significant | ||||||||
| Educational attainment | Education access and quality | Significant | ||||||||
| Income | Economic stability | Significant | ||||||||
| 46 | Li et al. (2020) | Cross-sectional study | n = 12,639 (NHIS) | Civilian noninstitutionalized women living in United States households | 40–74 years old | To identify factors and related inconsistencies associated with mammography use in the entirety of the United States population, as well as between black and white subgroups | Age | Social and community context | Significant | RF analysis; Logistic regression |
| Family education | Education access and quality | Significant (NHIS)/Non-Significant (BRFSS) | ||||||||
| Family annual income | Economic stability | Significant | ||||||||
| n = 169,116 (BRFSS) | Women with telephone access in the United States | Number of children at home | Social and community context | Significant | ||||||
| Race (Black) | Social and community context | Significant | ||||||||
| n = 181,755 (total) | Women in the United States without a history of breast cancer | Marital status | Social and community context | Mixed | ||||||
| Health insurance status | Health care access and quality | Significant | ||||||||
| Region | Neighborhood and built environment | Significant | ||||||||
| 47 | Luo et al. (2021) | Cohort | n = 33,320 | Female Medicare beneficiaries with an initial diagnosis of breast cancer from 2006 through 2014 in the SEER-Medicare database | 67–74 years old | To evaluate the contributions of each tumor biology (histologic grade and hormone receptor status) and healthcare (screening mammography use and time delay from mammography to diagnostic biopsy) factor to racial disparity at breast cancer stage-at-diagnosis between African American and white patients | Race | Social and community context | Significant | Probabilistic graph modeling (PGM) using naïve Bayesian network (NBN)-based contribution analysis |
| 48 | Molina et al. (2016) | Cross-sectional study | n = 536 | Federally qualified health center (FQHC)-based group of United States-based Latinas in western Washington State who have not obtained a mammogram in the past 2 years | 42–74 years old | To assess the role of four neighborhood characteristics in knowledge-, psychocultural-, and economic-based barriers to mammography use among Latinas | Block group-level socioeconomic deprivation concentration | Neighborhood and built environment/Education access and quality/Economic stability | Non-significant | Multinomial regression models |
| Neighborhood socioeconomic-based segregation | Neighborhood and built environment/Economic stability | Significant | ||||||||
| Neighborhood Latino-based concentration | Neighborhood and built environment/Social and community context | Significant | ||||||||
| Neighborhood Latino-based segregation | Neighborhood and built environment/Social and community context | Significant | ||||||||
| Economic | Economic stability/Health care access and quality | Significant | ||||||||
| 49 | Monsivais et al. (2022) | Cohort study | n = 34,588 | Female patients of a large health care network in Washington State who had completed a mammogram between January 1 and December 31 in 2017 or 2018 but did not have a mammogram in the following year | ≥50 years old | To assess whether racial and socioeconomic inequities in breast cancer screening widened during the COVID-19 pandemic | Age | Social and community context | Significant | Multivariable logistic regression models |
| Insurance status | Health care access and quality | Significant | ||||||||
| Race or ethnicity | Social and community context | Significant | ||||||||
| Rural or urban residence | Neighborhood and built environment | Significant | ||||||||
| 50 | Nair et al. (2022) | Cohort study | n = 19,292 | BSPAN program participants who had at least one mammogram between 2012 and 2019 | 40–64 years old | To assess prevalence and correlates of baseline adherence, and longitudinal adherence to screening mammograms using data from the longitudinal BSPAN program | Age | Social and community context | Non-significant | Multivariable logistic regression models; multivariable Cox proportional hazards model; chi-square; independent samples t-test; and sensitivity analysis |
| Race or ethnicity | Social and community context | Non-significant | ||||||||
| Marital status | Social and community context | Significant | ||||||||
| Urbanization | Neighborhood and built environment | Non-significant | ||||||||
| Proximity to metro | Neighborhood and built environment | Non-significant | ||||||||
| Rural | Neighborhood and built environment | Non-significant | ||||||||
| Language preference | Social and community context | Significant | ||||||||
| Literacy | Education access and quality | Significant | ||||||||
| Years lived in the United States | Social and community context | Significant | ||||||||
| 51 | Onega et al. (2018) | Cross-sectional study | n = 46,944 | Women visiting one of the 15 primary care practices included in the Dartmouth-Hitchock regional network (in NH) and women’s Hospital primary care network (greater Boston) | 40–89 years old | To examine the effect of PCP, practice, and health system-level characteristics and processes on the breast cancer screening metrics of overall percent screened and percent screening past age 75 | Race or ethnicity | Social and community context | Significant | Generalized linear mixed effects regression models; variance components analysis |
| Insurance status | Health care access and quality | Significant | ||||||||
| Age | Social and community context | Significant | ||||||||
| 52 | Oviedo et al. (2022) | Cross-sectional study | n = 157 | Women without a history of breast disease who self-identified as Filipino living in the United States, recruited through the national officers of the Philippine Nurses Association of America | ≥40 years old | To determine factors that influence mammogram adherence in Filipino American women using Andersen’s Behavioral Health Model of Services for Vulnerable Populations as the conceptual framework | Breast cancer literacy | Education access and quality | Non-significant | Andersen’s Behavioral Health Model of Services for Vulnerable Populations; logistics regression models; adjusted odds ratios |
| Sociocultural deterrents | Social and community context | Non-significant | ||||||||
| Cultural beliefs | Social and community context | Non-significant | ||||||||
| Years lived in the United States | Social and community context | Non-significant | ||||||||
| 53 | Padela et al. (2015) | Cross-sectional study | n = 240 | Self-identified Muslim, English-speaking women recruited from 11 CIOGC-affiliated mosques and Muslim organization sites in Greater Chicago | >40 years old | To assess relationships between several religion-related factors and breast cancer screening in a group of Chicago-based Muslim women | Religiosity | Social and community context | Significant | Bivariate testing (ex. unadjusted odds ratios) and multivariate logistic regression models |
| Perceived religious discrimination in healthcare | Social and community context | Significant | ||||||||
| Age | Social and community context | Significant | ||||||||
| Years of residence in the United States | Social and community context | Significant | ||||||||
| Ethnicity | Social and community context | Non-significant | ||||||||
| 54 | Paranjpe et al. (2022) | Retrospective cross-sectional study | n = 7,990 | Civilian, noninstitutionalized Asian and non-Hispanic white women who completed the National Health Interview Survey | ≥40 years old | To determine whether breast cancer screening practices were different between Asian and non-Hispanic white women in a national population-based study | Race | Social and community context | Significant | Taylor series linearization methods; Wald chi-square tests; and Multivariable logistic regression |
| Insurance status | Healthcare access and quality | Significant | ||||||||
| Education | Education access and quality | Significant | ||||||||
| Family income | Economic stability | Significant | ||||||||
| Place of Birth in United States | Neighborhood and built environment | Significant | ||||||||
| 55 | Patel et al. (2014) | Cross-sectional study | n = 334 | Low-income African American women in Nashville, Chattanooga, and Memphis | ≥ 40 years old | To examine socio-demographic factors that influence decision to use mammography and other breast cancer screenings in low-income African Americans and examine differences in obstacles to screening by geographic region | Age | Social and community context | Non-significant | Chi-square test, Binary logistic regression model |
| City of residence | Neighborhood and built environment | Significant | ||||||||
| BMI | Healthcare access and quality | Significant | ||||||||
| Annual household income | Economic stability | Significant | ||||||||
| Health insurance status | Healthcare access and quality | Non-significant | ||||||||
| Transportation access | Neighborhood and built environment | Significant | ||||||||
| Medical visits in the Past 12 months | Neighborhood and built environment | Non-significant | ||||||||
| Education | Education access and quality | Non-significant | ||||||||
| Employment status | Economic stability | Non-significant | ||||||||
| 56 | Ryu et al. (2013) | Cross-sectional study | n = 1,596 | Immigrant women in five Asian-American ethnic groups participating in the 2009 California Health Interview Survey | 40–70 years old | To compare rates of screening mammography among immigrant women in five Asian-American ethnic groups in California, and ascertain the extent to which differences in mammography rates among these groups are attributable to differences in known correlates of cancer screening | Age | Social and community context | Non-significant | Wald chi-square design-adjusted test of independence, Multiple logistic regression, Predicted probabilities |
| English proficiency | Social and community context | Non-significant | ||||||||
| Educational attainment | Education access and quality | Significant | ||||||||
| Ethnicity | Social and community context | Significant | ||||||||
| Income | Economic stability | Non-significant | ||||||||
| Current health insurance | Healthcare access and quality | Significant | ||||||||
| 57 | Sabatino et al. (2016) | Cross-sectional study | n = 1,429 (2010) | Female Medicare beneficiaries without breast cancer history between 2010 and 2013 | 65–74 years old | To examine whether mammography use increased after elimination of Medicare cost sharing for screening mammography and whether changes varied for different groups of women | Age | Social and community context | Significant | Pearson Wald F test, Multivariable logistic regression |
| Race | Social and community context | Non-significant | ||||||||
| Ethnicity | Social and community context | Significant | ||||||||
| Birthplace | Neighborhood and built environment | Non-significant | ||||||||
| n = 2,152 (2013) | Income | Economic stability | Non-significant | |||||||
| Access to Care | Healthcare access and quality | Significant | ||||||||
| Type of health insurance | Healthcare access and quality | Significant | ||||||||
| Number of provider visits | Healthcare access and quality | Significant | ||||||||
| 58 | Schommer et al. (2023) | Retrospective cross-sectional study | n = 781 | Breast cancer female patients from Seton Medical Center Austin tumor registry between March 1, 2019 and March 2, 2021 | 40–70 years old | To explore the relationship between COVID-19 (before and after) and stage distribution, time-to-intervention, and insurance status of patients presenting with breast cancer in the Austin local cancer center | Age | Social and community context | Significant | Descriptive statistics, Chi-square test, Fisher exact test, unpaired T-test, Wilcoxon signed-rank test, Multinomial Logistic regression, Two-tailed Wald test |
| Sex | Social and community context | Non-significant | ||||||||
| Race | Social and community context | Significant (Pre and Post COVID) | ||||||||
| Ethnicity | Social and community context | Significant (Pre and Post COVID) | ||||||||
| Insurance status | Healthcare access and quality | Significant | ||||||||
| Time from breast cancer diagnosis to first treatment | Healthcare access and quality | Significant | ||||||||
| 59 | Sealy-Jefferson et al. (2019) | Cross-sectional study | n = 7,120 | Racially/ethnically diverse post-menopausal women from the Women’s Health Initiative Survey (1993–2014) | 50–79 years old | To examine whether rural–urban residence was associated with stage at breast cancer diagnosis among large well-defined racially/ethnically diverse cohort of postmenopausal women | Age | Social and community context | Significant | Univariable logistic regression, Multivariable logistic regression |
| Race | Social and community context | Non-significant | ||||||||
| Ethnicity | Social and community context | Non-significant | ||||||||
| Education | Education access and quality | Non-significant | ||||||||
| Rural/Urban Residence, Zip Code | Neighborhood and built environment | Non-significant | ||||||||
| Social Strain | Social and community context | Non-significant | ||||||||
| Health insurance status | Health care access and quality | Non-significant | ||||||||
| Social Support | Social and community context | Non-significant | ||||||||
| 60 | Selove et al. (2016) | Retrospective cohort Study | n = 4,476 | Non-Hispanic Black and White non-HMO Medicare women, who resided in United States, who had a mammogram, biopsy, and breast cancer diagnosis during 2005–2008 | 65–84 years old | Examine the length of critical intervals between abnormal mammogram and breast cancer treatment within a large cohort of Medicare beneficiaries varying by age, race, and medical comorbidities | Age | Social and community context | Significant | Cox proportional hazard models, Logistic regression models |
| Race | Social and community context | Non-significant | ||||||||
| Ethnicity | Social and community context | Non-significant | ||||||||
| Physical comorbidities | Healthcare access and quality | Significant | ||||||||
| 61 | Shon et al. (2019) | Cross-sectional study | n = 3,710 | Immigrant Asian women who filled the 2005,2007, 2009, and 2011 California Health Interview Survey | ≥40 years old | To examine significant predictors of never having a mammogram among Chinese, Vietnamese, and Korean immigrant women living in California and age 40 years and older and to explore whether relationships between enabling components and acculturation components and odds of never having a mammogram vary across Chinese, Vietnamese, and Korean immigrant women | Ethnicity | Social and community context | Non-significant | Bivariate analysis (Chi-square or ANOVA), Multivariate logistic regression |
| Age | Social and community context | Significant | ||||||||
| Education | Education access and quality | Non-significant | ||||||||
| Federal poverty level | Economic stability | Non-significant | ||||||||
| Age | Social and community context | Non-significant | ||||||||
| Employment | Economic stability | Non-significant | ||||||||
| English proficiency | Social and community context | Non-significant | ||||||||
| Years lived in the United States | Neighborhood and built environment | Non-significant | ||||||||
| Insurance type | Healthcare access and quality | Non-significant | ||||||||
| Number of Physician Visits in the past 12 months | Healthcare access and quality | Significant | ||||||||
| Number of Chronic Illnesses | Healthcare Access and Quality | Non-significant | ||||||||
| 62 | Spada et al. (2021) | Retrospective cross-sectional study | n = 35,735 | Female breast cancer patients registered in the Pennsylvania Cancer Registry | 50–64 and 68–74 | To determine if increased access to health insurance following the Affordable Care Act (ACA) resulted in an increased proportion of early-stage breast cancer diagnosis among women in Pennsylvania, particularly minorities, rural residents, and those of lower socioeconomic status | Health Insurance Access | Healthcare access and quality | Non-significant | T-tests; Multivariable logistic regression models; Difference-in-differences analysis |
| Area Deprivation Index | Neighborhood and built environment | Non-significant | ||||||||
| Race | Social and community context | Significant (for 68–74) | ||||||||
| Ethnicity | Social and community context | Significant (for 68–74) | ||||||||
| Area of Residence | Neighborhood and built environment | Non-significant | ||||||||
| PCP Density | Healthcare access and quality | Non-significant | ||||||||
| 63 | Tangka et al. (2017) | Cross-sectional study | n = 3,821,084 | Medicaid-insured women in the United States from 2006 to 2008 | 40–64 years old | To assess racial/ethnic and geographic disparities in the use of breast cancer screening | Race | Social and community context | Significant | Regression models; Generalized Estimating Equations (GEE) |
| Ethnicity | Social and community context | Significant | ||||||||
| State of residence | Neighborhood and built environment | Significant | ||||||||
| 64 | Thomas et al. (2018) | Retrospective cohort study | n = 14,651 | Medicaid-insured women (not dual enrolled) in California who received treatment in the specialty mental health care system and have filled least one antipsychotic prescription | 48–67 years old | To examine mammogram disparities for those with severe mental illness and the contribution of psychosocial factors to mammogram use among women with severe mental illness | Healthcare access and utilization | Healthcare access and quality | Significant | Poisson models with robust standard errors |
| Health insurance status | Healthcare access and quality | Significant | ||||||||
| Race | Social and community context | Significant | ||||||||
| Ethnicity | Social and community context | Significant | ||||||||
| County of residence | Neighborhood and built environment | Non-significant | ||||||||
| Age | Social and community context | Non-significant | ||||||||
| 65 | Tran et al. (2019) | Cross-sectional study | n = 482,360 | U.S. female survey participants in the 2012, 2014, or 2016 Breast and Cervical Cancer-Screening module of the Behavioral Risk Factor Surveillance System (BRFSS) survey | ≥ 40 years old | To explore urban–rural disparities in United States breast cancer screening practices at the national, regional, and state levels | Area of residence (urban/suburban/rural) | Neighborhood and built environment | Significant | Binary logistic regression models |
| Age | Social and community context | Significant | ||||||||
| Race | Social and community context | Significant | ||||||||
| Education | Education access and quality | Significant | ||||||||
| Healthcare coverage | Healthcare access and quality | Significant | ||||||||
| Healthcare access and utilization | Healthcare access and quality | Significant | ||||||||
| 66 | Vang et al. (2020) | Cross-sectional study | n = 518 | Medically underserved women in NYC | ≥40 years old | To examine the relationship between language preference and screening mammogram adherence | Ethnicity | Social and community context | Significant | Descriptive statistics (Chi-square tests and Fisher’s exact tests), Bivariate analyses and multiple logistic regressions |
| Age | Social and community context | Significant | ||||||||
| Race | Social and community context | Significant | ||||||||
| Education | Education access and quality | Significant | ||||||||
| Lack of sufficient healthcare coverage | Healthcare access and quality | Significant | ||||||||
| Language | Social and community context | Significant | ||||||||
| 67 | Virk-Baker et al. (2013) | Cross-sectional study | n = 406,602 | White and Black women in fee-for-service Medicare plans from 203 United States counties with highest risk of breast cancer deaths | 65–74 years old | To assess the uptake of breast cancer screening in women 65–74 years old from counties with most of the breast cancer deaths in Black older women | Race | Social and community context | Non-significant | Logistic regression |
| Comorbid conditions | Healthcare access and quality | Non-significant | ||||||||
| Age | Social and community context | Non-significant | ||||||||
| Education | Education access and quality | Non-significant | ||||||||
| ER utilization | Healthcare access and quality | Non-significant | ||||||||
| Economic status | Economic stability | Non-significant | ||||||||
| 68 | Wang et al. (2018) | Cross-sectional study | n = 8,347 | Patients cared by Accountable Care Organizations (ACO) clinics in rural Nebraska with average risk of breast cancer | 50–74 years old | To understand the adherence to the biennial breast cancer screening guideline by rural women with average risk for breast cancer | Age | Social and community context | Significant | Descriptive statistics, Multiple logistic regression, Spearman correlations, and Generalized estimating equation method |
| Gender | Social and community context | Significant | ||||||||
| Race | Social and community context | Significant | ||||||||
| Ethnicity | Social and community context | Significant | ||||||||
| Insurance status | Healthcare access and quality | Significant | ||||||||
| Preferred language | Social and community context | Significant | ||||||||
| Travel time to clinic | Healthcare access and quality | Significant | ||||||||
| County poverty rate | Economic stability | Significant | ||||||||
| County uninsured rate | Healthcare access and quality | Significant | ||||||||
| Race/Ethnicity composition of county | Social and community context | Significant | ||||||||
| 69 | Wiese et al. (2023) | Retrospective study | n = 73,718 | Female population in the United States with limited accessibility to mammography (living more than 20-min drive time to nearest mammography facility) | 45–84 years old | To evaluate the travel-time based geographic accessibility to mammography facilities at the census tract level by urban–rural status in continuous US from 2006 to 2022 | Rural vs. Urban/Suburban Setting | Neighborhood and built environment | Non-significant | Descriptive statistics, Regression analysis |
| Accessibility to screening facility | Healthcare access and quality | Non-significant | ||||||||
| 70 | Wilcox et al. (2016) | Cross-sectional study | n = 697 | Randomly sampled households with at least one female tenant selected through 20 United States census tracts with Haitian population | ≥40 years old | To identify the correlation between race/ethnicity and annual mammogram compliance | Age | Social and community context | Significant | Binary logistic regression; Chi-square tests |
| Race | Social and community context | Significant | ||||||||
| Ethnicity | Social and community context | Significant | ||||||||
| Education level | Education access and quality | Significant | ||||||||
| Preferred language | Social and community context | Significant | ||||||||
| Poverty status | Economic stability | Significant | ||||||||
| Employment status | Economic stability | Significant | ||||||||
| Insurance coverage | Healthcare access and quality | Significant | ||||||||
| Provider visits | Healthcare access and quality | Significant | ||||||||
| 71 | Wilkerson et al. (2023) | Retrospective cohort study | n = 738 | Female patients who underwent treatment for BC at a quaternary care academic medical center or affiliate zonal hospital | 40–45 years old | To discover if the majority of Black women are diagnosed with breast cancer on their first mammogram and to determine if the connection between patient demographics and primary findings of breast cancer are of importance for preventative care | Age | Social and community context | Significant | Chi-square test; multivariate logistic regression; Wilcoxon rank-sum test |
| Race | Social and community context | Significant | ||||||||
| BMI | Healthcare access and quality | Significant | ||||||||
| Insurance coverage | Healthcare access and quality | Significant | ||||||||
| 72 | Wu et al. (2021) | Retrospective cohort study | n = 1,044 | Visually impaired women enrolled in fee-for service Medicare | 65–72 years old | To assess whether receiving breast cancer screenings are similar for women w/wo visual impairment | Age | Social and community context | Significant | Chi-square test; Multivariable conditional logistic regression |
| Race | Social and community context | Significant | ||||||||
| Environment | Neighborhood and built environment | Significant | ||||||||
| Insurance coverage | Healthcare access and quality | Significant | ||||||||
| Urbanization | Neighborhood and built environment | Significant |
*Statistical significance was assessed based on the p value (p < 0.05).
Significance of associations between breast cancer screening as an outcome and identified SDOH were reported (Table 1). Table 2 included a list of databases from where the data was accessed, the availability status of the data (public/private), and the geographical level from where the data was extracted. Basic qualitative content analysis was carried out to identify similar themes in future directions across studies highlighted in Table 3. The three phases of qualitative content analysis for the results of primary qualitative research described by Elo and Kyngas (19) were applied: (i) preparation, (ii) organizing, and (iii) reporting.
Table 2.
Database availability status and characteristics.
| Primary Author/Year | Database/Data source | Publicly available (yes/no) | City/State/National level |
|---|---|---|---|
| Agenor et al. (2020) | National Health Interview Survey (2013–2017) | Yes | National |
| Agrawal et al. (2021) | Surveys conducted at Three Texas Churches | No | State |
| Alabdullatif et al. (2022) | National Health Interview Survey (2011–2018) | Yes | National |
| Alatrash et al. (2021) | Surveys conducted primarily in Arab American mosques and churches | No | City |
| Anderson et al. (2014) | National Program of Cancer Registries | Yes | State |
| Asgary et al. (2014) | EHRs from shelter-based clinics of Lutheran Family Health Centers | No | City |
| Ayanian et al. (2013) | Medicare beneficiary summary file | Yes | National |
| Balazy et al. (2019) | EHRs from Stanford Health | No | City |
| Beaber et al. (2016) | EHRs from Dartmouth-Hitchcock Health System and Brigham and Women’s Hospital | No | City |
| Beaber et al. (2019) | EHRs from 10 PROPSR research medical facilities | No | National |
| Calo et al. (2016) | United States Census Bureau and Health of Houston Survey | Yes | City |
| Castaneda et al. (2014) | Survey from UCSD patients 2007–2008 | No | City |
| Cataneo et al. (2019) | National Health Interview Survey (2015) | Yes | National |
| Chandak et al. (2019) | Nebraska Cancer Registry (2008–2012) | Yes | State |
| Christensen et al. (2023) | Medicare Beneficiary Summary File | No | State |
| Clark et al. (2017) | 2013 US Census American Community Survey | Yes | State |
| Clark et al. (2019) | National Health Interview Survey (2005, 2008, 2010, 2013, 2015) | Yes | National |
| Davis et al. (2017) | Surveys conducted at the radiology department of the University of Arizona College of Medicine | No | State |
| Dong et al. (2022) | Ohio Cancer Incidence Surveillance System (OCISS) | No | State |
| Duggan et al. (2019) | Surveys conducted at grocery stores, religious organizations, and community events | Yes | County |
| Elkin et al. (2014) | FDA’s searchable online database of facilities | Yes | State |
| Fedewa et al. (2016) | National Health Interview Survey (2013) | No | National |
| Flores et al. (2018) | Institution’s Research Patient Data Registry, MagView, Burtonsville, Maryland | No | City |
| Guo et al. (2019) | Study of Women’s Health Across the Nation (SWAN) | No | National |
| Henderson et al. (2015) | Carolina Mammography Registry (CMR) | No | State |
| Henderson et al. (2020) | Breast Cancer Surveillance Consortium (BCSC), a National Cancer Institute (NCI)-funded network of mammography registries across the United States. | No | National |
| Henry et al. (2014) | The 2008 and 2010 Utah Behavioral Risk Factor Surveillance System | No | State |
| Hong et al. (2017) | Questionnaires | No | City Level |
| Hubbard et al. (2016) | Breast Cancer Surveillance Consortium (BCSC) | Yes | National Level |
| Jena et al. (2017) | Kaiser Permanente MA plans | No | State level |
| Jensen et al. (2022) | Access to Breast Care for West Texas (ABC4WT) | No | State level |
| Jin et al. (2019) | Self-report survey questionnaires | No | State level |
| Johnson et al. (2021) | Cancer Data Registry of Idaho (CDRI) | Yes | State level |
| Kadivar et al. (2016) | National Assessment of Adult Literacy (NAAL) | Yes | National Level |
| Kempe et el. (2013) | Kaiser Permanente Colorado (KPCO) | No | State level |
| Khaliq et al. (2015) | Bedside interviews | No | City |
| Kim et al. (2019) | American Community Survey and Robert Wood Johnson Foundation 500 Cities Project with data from Behavioral Risk Factor Surveillance System | Yes | City |
| Kim et al. (2022) | Cross sectional data from 2012, 2014, 2016, and 2018 Behavioral Risk Factor Surveillance System | Yes | National |
| Komenaka et al. (2015) | Maricopa Medical Center Breast Clinic data | No | City |
| Kosog et al. (2019) | FQHC Electronic Medical Record | No | City |
| Lapeyrouse et al. (2017) | 2009–2010 Ecological Household Study on Latino Border Residents in El Paso County, TX | No | City |
| Lawson et al. (2021) | Insurance enrollment data from regional commercial insurers and Medicare liked with records from the Cancer Surveillance System from 2007–2018 | No | State and National |
| Lee et al. (2016) | Breast Cancer Surveillance Consortium | Yes | National |
| Lee et al., 2017 | Baseline data from mobile phone program “mMammogram” | No | State/Regional |
| Lee et al. (2021) | Breast Cancer Surveillance Consortium | Yes | National |
| Li et al. (2020) | 2016 National Health Interview Survey | Yes | National |
| 2016 Behavioral Risk Factor Surveillance System | Yes | National | |
| Luo et al. (2021) | SEER Medicare | Yes | National |
| Molina et al. (2016) | 2011–2014 Fortaleza Latina! | Yes | State |
| Monsivais et al. (2022) | Patient data from MultiCare health system, a large state-wide, non-profit healthcare system with 230 clinics and hospitals across Washington State | No | State |
| Nair et al. (2022) | 2012–2019 electronic health record data for BSPAN program participants | Yes | State |
| Onega et al. (2018) | PROSPR research centers including the primary care populations of the Dartmouth-Hitchock regional network (in NH) and the Brigham and Women’s Hospital primary care network (in greater Boston) | Yes | National |
| Oviedo et al. (2022) | Self-administered, web-based surveys sent through the PI’s network of friends and through the national officers of the Philippine Nurses Association of America and further through snowball recruitment | No | National |
| Padela et al. (2015) | Self-administered surveys given to participants at sites affiliated with the Council of Islamic Organizations of Greater Chicago (CIOGC) in the Chicago metro area | No | City |
| Paranjpe et al. (2022) | 2015 National Health Interview Survey | Yes | National |
| Patel et al. (2014) | Meharry CNP Community Survey Database | No | State |
| Ryu et al. (2013)* | 2009 California Health Interview Survey | Yes | State |
| Sabatino et al. (2016) | National Health Interview Survey Data | Yes | National |
| Schommer et al. (2023) | Seton Medical Center Austin Tumor Registry | No | City |
| Sealy-Jefferson et al. (2019) | Women’s Health Initiative Program (WHI) | No | National |
| Selove et al. (2016) | Center for Medicare and Medicaid Services (CMS) | No | National |
| Shon et al. (2019) | California Health Interview Survey data | Yes | State |
| Spada et al. (2021) | Pennsylvania Cancer Registry | Yes | State |
| Tangka et al. (2017) | Fee-for-service claims and encounter data from Centers for Medicare and Medicaid Services | No | National |
| Thomas et al. (2018) | California Medicaid (Medi-Cal) Administrative, Pharmacy, and Billing Systems | No | State |
| Client and Service Information System | |||
| Tran et al. (2019) | Behavioral Risk Factor Surveillance System surveys (BRFSS) | Yes | National |
| Vang et al. (2020) | Participants of breast health education programs at various communities and faith-based organizations in MU areas of NYC | No | City |
| Virk-Baker et al. (2013) | Medicare claims data for outpatient procedures, physician visits and inpatient stays from 2001–2006 | Yes | National |
| Wang et al. (2018) | Clinic EMRs and provider surveys from an ACO organization | No | State |
| Secondary data obtained from Area Health Resource File administered by Health Resources and Services Administration | |||
| Wiese et al. (2023) | US FDA, BRFSS | Yes | National |
| Wilcox et al. (2016) | US Department of Health | Yes | State |
| Wilkerson et al. (2023) | U.S Department of Health | Yes | National |
| CDC | |||
| Prevention and National Cancer Institute | |||
| JNCI | |||
| Wu et al. (2021) | Medicare database | No | National |
| Clinical Modification (ICD-9-CM) billing codes | |||
| Current Procedural Terminology (CPT) | |||
| Healthcare Common Procedure Coding System (HCPCS) | |||
| Young et al. (2020) | FDA’s mammography facility database | Yes | State |
| American Community Survey US Census Rural -Urban community (RUCA) codes |
*For one control variable, county-level PCP data were obtained across the state from a different database: Area Health Resources Files.
Table 3.
Lessons learned identified from thematic analysis across included studies.
| Lessons learned themes |
|
Step 4 and 5: charting the data and collation, summarization, and reporting of results
Study characteristics were tabulated for primary author/year, study design, sample size, study population, age range, study purpose, type of SDOH, SDOH category based on HP 2030, association between SDOH and outcome (significant/non-significant), and type of methodology/analysis used for data analysis (Table 1). Identified databases were tabulated by primary author/year, database/data source, public availability, and city/state/national level (Table 2). Each database was stratified based on availability (publicly available/not publicly available) and location (city/state/national level). Lessons learned from each relevant study were highlighted in Table 3.
Results
The initial study extraction resulted in 8,124 articles from PubMed (n = 1,293), EMBASE (n = 6,193), Web of Science (n = 527), and Cochrane (n = 111). Studies were excluded due to publication outside of the timeframe (n = 7,775), discussion of all types of cancer rather than focusing on breast cancer (n = 2,349), being a literature review or systematic review (n = 884), lack of focus on breast cancer disparities (n = 717), focusing on big data or no mention of SDOH (n = 124), focusing more on knowledge and attitudes rather than SDOH (n = 112), being an opinion piece or an editorial (n = 25), or emphasizing survival as an outcome rather than treatment (n = 22). Duplicate studies were also excluded (n = 82 from PubMed, n = 60 from EMBASE, n = 20 from Web of Science, and n = 2 from Cochrane). A total of 267 studies met the inclusion criteria from PubMed (n = 222), EMBASE (n = 40), and Web of Science (n = 5). An additional 195 studies were excluded after a full study review due to being an abstract and not a full text (n = 77), having a qualitative or experimental study design (n = 42), having no relation to SDOH (n = 63), and discussing cancer types in general rather than narrowing it down to breast cancer (n = 13). A total of 72 studies were retained for analysis (Figure 1).
Figure 1.
PRISMA-ScR flow chart of study selection process.
The 72 included studies were published between 2013 and 2023. About half of the studies (58%) were published in 2018 or later (n = 42). Study designs included cross-sectional studies (n = 45); cohort studies (n = 18); and case–control studies (n = 9). Sample size ranged from n = 100 to n = 3,821,084 female adults with breast cancer while the age of this target population ranged from 40 to 89 years old (Table 1).
Priority populations
Priority populations who were actively involved (or targeted) in implementation activities were ethnically diverse female patients diagnosed with breast cancer including African American women; Muslim and Christian Arab American; Haitian women; Filipino women; and Korean American women. Another set of studies focused on women from programs, such as women from Geisel School of Medicine (n = 3,413), from the BSPAN program (n = 19,292), women who underwent mammography in Harvard Medical School (n = 9,575), female patients from a single institution undergoing breast radiotherapy (n = 1,057), presenting to radiology department (n = 758), mammogram facilities (n = 1,749), and at a quaternary care academic medical center (n = 738) (Table 1).
Additional studies focused on the characteristics of the women, such as women who have individual subscribers or employer supplemented (n = 95,661), are Medicaid-insured and Medicare fee-for service (n = 11), are insured but have not undergone mammogram in 24 months (n = 47,946), have no history of breast cancer (n = 181,755), have telephone access (n = 169,116), homeless women (n = 100), hospitalized women (n = 250), are medically underserved (n = 518), and have limited accessibility to mammogram (n = 73,718) (Table 1).
Classification of SDOH factors influencing breast cancer screening behavior based on the healthy people 2030 categories
An examination of SDOH influential factors of breast cancer screening was conducted, focusing on their classification into Healthy People 2030 categories (20). Among the various SDOH identified, those related to socioeconomic status (n = 96) exhibited the highest frequency (Table 1). Specifically, factors such as income (n = 32), education level (n = 29), employment status (n = 8), birthplace/citizenship (n = 5), acculturation/years lived in the United States (n = 5), marital status (n = 2), social support (n = 2), and number of children (n = 1) were among the key elements. Access to healthcare (n = 75) emerged as a significant theme, with subcategories like insurance status (n = 33), accessibility of healthcare services and providers (n = 18), insurance coverage (n = 8), access to mammography facilities (n = 5), insurance copayments (n = 2), time from breast cancer diagnosis to first treatment (n = 1), travel time to clinic (n = 1), and county uninsured rate (n = 1) also being identified. Race/Ethnicity (n = 79), age (n = 52), sex/gender (n = 2), and sexual orientation (n = 1) were additional factors reported. Language-related SDOH (n = 21) were observed 21 times, encompassing language proficiency/preferred language (n = 15) and health literacy (n = 6). Furthermore, location (n = 30), transportation (n = 5), housing (n = 3), county poverty rate (n = 2), internet access (n = 1), area deprivation index (n = 1), diversity index (n = 1), cultural and religious beliefs (n = 4), perceived discrimination (n = 2), health beliefs (n = 1), and trust in health care providers/systems (n = 1) were also cited. Finally, health-related factors (n = 9) that were reported include comorbidities and chronic illnesses (n = 3), BMI (n = 2), medical/family history of breast cancer (n = 1), history of mental illness (n = 1), HIV status (n = 1), and substance/alcohol abuse (n = 1) (Table 1). Among the Healthy People 2030 categories, Social and Community Context (n = 177) emerged as the most prevalent, with a striking 177 occurrences of SDOH. Following closely behind were Healthcare Access and Quality (n = 80), Economic Stability (n = 56), Neighborhood and Built Environment (n = 46), and Education Access and Quality (n = 36) (Table 1).
Database access and characteristics
Databases with the highest number of occurrences include data from the National Health Interview Survey (n = 8) [over a range of years from 2005 to 2018], the Breast Cancer Surveillance Consortium (n = 4), and the United States Department of Health (n = 2). Other databases used include the National Program of Cancer Registries, the National Assessment of Adult Literacy, and SEER Medicare. Of the 74 databases used, 47% (n = 35) are publicly available. The databases are available at the city (n = 16), county (n = 1), state (n = 28), and national (n = 30) levels (Table 2).
Significance of association between SDOH factors and access to mammography and treatment opportunities
The Health Care Access and Quality category was reported in the highest number of studies (n = 44; 61%), showing its statistical significance in relation to access to mammography. Insurance status was the most reported sub-categorical factor of Health Care Access and Quality with n = 36 (50%) articles supporting this finding. A total of n = 42 (58%) studies showed statistical significance in the social and community context category, with the highest subcategories being age and ethnicity with n = 46 (63%) and n = 40 (55%) articles denoting their significance, respectively. Language was the third highest with n = 11 (15%) studies highlighting its significance as an influential factor of screening behavior. Further, n = 28 (38%) studies exhibited statistical significance under the Economic Stability category, with income level being the most common sub-categorical indicator emphasized in n = 20 (27%) studies. Next, the Neighborhood and Built Environment category showed statistical significance in n = 18 (25%) articles, with zip code or geographic location being reported as the strongest sub-categorical indicator in n = 15 studies (20%). Moreover, n = 24 (33%) articles showed statistical significance in Education Access and Quality as strong indicators of mammography rate, with the highest level of education completed acting as the strongest sub-categorical factor in n = 24 (33%) articles (Table 1).
The methodology used across the included studies to communicate statistical data were reported as: logistic regression (n = 63), descriptive statistics (n = 23), chi-square tests (n = 20), T-tests (n = 13), linear regression (n = 9), multivariate analyses (n = 9), Wald tests (n = 8), Generalized estimating equations (n = 7), Spatial analysis (n = 7), Cox proportional hazards regression (n = 5), Kaplan–Meier cumulative incidence (n = 3), Sensitivity analysis (n = 2), Trend analysis (n = 2), and Z tests (n = 1) (Table 1).
Lessons learned
Using the three phases of qualitative content analysis delineated by Elo and Kyngas (19), qualitative themes were identified. First, data relevant to lessons learned was collected from each of the included studies in the preparation stage (Phase I) (Supplementary material 1). Second, lessons learned were organized into bullet points and tabulated by primary author to compare data across studies and explore emerging themes (Phase 2) (Supplementary material 1). Major themes were then highlighted in Table 3 (Phase III).
Many of the studies demonstrated a strong association between a lack of health insurance and a lower rate of breast cancer screening (21–25). Ethnic minority women, with the exception of those identifying as Asian, had a lower likelihood of being screened, and Black women experienced a higher risk of diagnosis upon first screening (25–29). While few studies analyze the effect of sexual orientation on breast cancer screening, initial insights reveal there are significant differences in mammography between bisexual, lesbian, and heterosexual women regardless of racial/ethnic groups (30). In considering religious values, fatalism-emphasizing religions were associated with less screening adherences and maintenance of modesty did not prove a significant limitation for women receiving mammograms (31–33). Economic factors present limitations as both high levels of poverty and impoverished rural regions were associated with lower screening rates (27, 32, 34–37). Improving patient-provider communication, addressing perceived discrimination, and improving trust in the health care system is necessary to improve screening rates across all demographics (38–42). Additionally, structural efforts to improve health insurance coverage, language proficiency, and transportation services could be beneficial (20–110). These steps will need to involve the local community to develop community-tailored educational campaigns to reinforce the importance of establishing yearly mammogram screenings (Table 3) (22, 34, 46, 49, 54, 55, 70, 76, 80, 86).
Discussion
The purpose of this scoping review was to identify the major SDOH acting as influential factors of breast cancer screening in United States women aged ≥ 40 years old. The analysis of the 72 included studies can inform which SDOH categories to focus on when designing evidence-based interventions for more effective and sustained positive behavior and health outcomes among United States women at-risk of breast cancer.
SDOH factors and healthy people 2030 categories
Of the classifications of SDOH by Healthy People 2030, the Social and Community Context Category was the most prevalent across the included studies (n = 177). However, when looking at the most frequently cited SDOH influential factors of breast cancer screening behaviors, those related to socioeconomic status exhibited the highest frequency. Such factors included income (n = 32), education level (n = 29), employment status (n = 8), birthplace/citizenship (n = 5), acculturation/years lived in the United States (n = 5), marital status (n = 2), social support (n = 2), and number of children (n = 1). Other highly reported factors include insurance status (n = 33) under the Healthcare Access and Quality category, as well as race/ethnicity (n = 79) and age (n = 52) under the Social and Community Context Category.
There is evidence to show the significance of the relationship between socioeconomic factors and breast cancer screening. Over 30 different interventions that address SDOH increased breast cancer screening rates by 12.3% (93). Social determinants such as poverty, lack of education, neighborhood disadvantage, residential segregation, racial discrimination, lack of social support, and social isolation have shown in numerous studies to play a role in the breast cancer stage at diagnosis (94, 95). Gomez et al. (94) highlighted in their review that social and built environments have been shown to factor into cancer diagnoses in 82% of 34 reviewed articles published since 2010, including breast cancer (96). Studies have found that, not only do these factors have a significant association with breast cancer screening individually, but they also work dynamically to impact screening and treatment for breast cancer (97).
Low affordability and healthcare accessibility profoundly impact breast cancer screening, leading to lower adherence in female patients. For instance, Medicaid patients who are required to pay co-payments for preventative services as well as for recommended follow-up visits are less likely to pursue such preventative services and mammograms are included in lost care (96). Co-payments of more than $10 have been associated with reduced rates of mammograms (97). Furthermore, a study investigating breast cancer screening among young military women revealed that, when removing cost and access barriers to obtaining a breast mammography, first-time screening rates were 90% (98). Similar results have been noted when patients were provided free mammograms in underserved areas. The Building Relationships and Initiatives Dedicated to Gaining Equality (BRIDGE) Healthcare Clinic, a free clinic offered by the University of South Florida, provided patients free mammograms and noted that about 84.5% of patients utilized these services (99).
Significance of associations between SDOH factors and breast cancer screening and treatment
The majority of the studies reported a significant association between the SDOH factors under each of the five Healthy People 2030 categories. Insurance status was the most reported sub-categorical factor of Health Care Access and Quality with n = 36 (50%) articles supporting this finding. Insurance status often determines whether patients seek mammography services as they often become costly without robust coverage (93). Despite stable mammography rates among women in the United States between the years 2000 and 2015, women who report being uninsured consistently have the lowest rates of mammography at 35.3% (100).
Moreover, a total of n = 42 (58%) studies showed statistical significance in the social and community context category, with the highest subcategories being age and ethnicity with n = 46 (63%) and n = 40 (55%) articles denoting their significance, respectively. Health disparities in the United States have been consistently associated with delayed screening, which then contributes to higher mortality rates among both Hispanic and Black populations (28). Inequities also exist in mammography rates between patients of different sexual orientations (111). White, bisexual women had significantly lower mammography rates than White, heterosexual women, while mammography rates were significantly higher for bisexual, Black women than for heterosexual, Black women (102).
Income (n = 20; 27%) strongly influences mammography rates since women with estimated household incomes greater than $38,100 have been found to have rates of repeat mammography higher than those of women below $25,399 (109). In addition to household income, food security acts as another influential factor of mammography rates. When patients are forced to choose between feeding their families and pursuing preventative care, mammography becomes more of a luxury than lifesaving care (110). Women facing food insecurity have shown a 54% lower likelihood of obtaining mammography (110).
Language (n = 11; 15%) and availability of translation services, health literacy, and culture also play a strong role in mammography rates since many women with limited English proficiency seek mammography care and receive abnormal results (103). Appropriate, timely follow-up in the correct language is imperative to proper care provision; however, a lack of translation services worsens the language barrier between these patients and their healthcare providers, delaying care (101). Clinics with a patient population that is majority non-English speaking also experience greater follow-up delays than those with a minority of non-English speakers due to language barriers (103). The lower a patient’s health literacy, the less likely they are to undergo up-to-date breast cancer screening according to official guidelines (104, 105). The cultural and religious beliefs in fatalism have also been continuously found to be associated with lower mammography rates, whereby women with the highest beliefs in fatalism had the lowest breast cancer screening rates (106, 107).
Finally, Education Access and Quality sub-categories were significant indicators of mammography rate, with the highest level of education completed acting as the strongest sub-categorical factor in n = 24 (33%) articles. A systematic review by Damiani et al. (109) showed that United States women with the highest level of education were more likely to screen for breast cancer, with a 36% higher rate of adherence to national screening guidelines compared to women with lower levels of education. This finding holds health professionals and community outreach efforts accountable in ensuring that the local patient population is aware of the importance of and has access to breast cancer screening measures (109, 110).
Availability of public databases
Of the 74 databases used, only 47% (n = 35) were publicly available. There is a need to establish more widely accessible databases encompassing a routine collection of data on the SDOH to allow for the examination of additional evidence on exiting associations between SDOH and health outcomes. These databases could also inform the development and implementation of longitudinal and experimental studies at the county, city, and national levels to decrease health disparities exacerbated by SDOH factors.
Strengths and limitations
Despite the importance of this study in guiding and informing the development and implementation of future SDOH-oriented evidence-based interventions for breast cancer screening, findings need to take into consideration this study’s limitations. First, despite a comprehensive search of the literature in psychosocial databases compatible with the topic at hand, this review did not include gray literature and did not encompass tracing of reference lists in included studies. Second, it also was limited to observational studies to explore SDOH factors acting as factors based on statistical tests looking at significance of reported associations. These observational studies also widely varied in reported sample sizes, ranging from 100 participants to a population of 4 million. Therefore, although statistical significance was reported across different studies, effect sizes, power, and external validity varied greatly. Future systematic reviews should assess the rigor and quality of analysis carried out, evaluate recruitment efforts and data collection methods, and critique analytical tests carried out to account for the difference in sample sizes. Third, the mesh terms included as many technical words and keywords relevant to the SDOH as possible but might have inadvertently omitted some key words due to the continuously evolving and changing definitions related to SDOH. However, the help of an expert research librarian mitigated the impact of this concern by imposing rigor in implemented scoping review protocols when developing the search strategy for this review. Fourth, formal assessment of the methodology and quality of the evidence was beyond the scope of this study and relied on the reported statistical tests to assess significance. Follow-up systematic reviews would help with addressing this limitation by focusing specifically on the analytical proportion of each study. Fifth, although various categorizations exist for SDOH such as the WHO and CDC categories, the Healthy People 2030 taxonomy was adopted for use as it is the most recently updated classification encompassing a wide range of SDOH. Future studies should compare these taxonomies by feasibility, usability, and importance for a more valid and systematic approach to SDOH categorization.
Conclusion
This scoping review describes major SDOH acting as significant influential factors of breast cancer screening behaviors among United States women aged ≥40 years old who are at-risk of the disease. Results may inform future evidence-based interventions aiming to address the underlying factors contributing to low screening rates for breast cancer in the United States. Efforts to integrate SDOH within the different components of intervention planning, implementation, and sustainability are widely gaining recognition, particularly in underserved communities, due to their substantial influence on everyday behaviors.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
VJ: Conceptualization, Data curation, Methodology, Writing – original draft. DL: Conceptualization, Data curation, Methodology, Writing – original draft. GO: Conceptualization, Data curation, Methodology, Writing – original draft. YZ: Conceptualization, Data curation, Methodology, Writing – original draft. SB: Conceptualization, Data curation, Methodology, Writing – original draft. AM: Conceptualization, Data curation, Methodology, Writing – original draft. SD: Conceptualization, Data curation, Methodology, Writing – original draft. MR: Conceptualization, Data curation, Methodology, Writing – original draft. DD: Methodology, Writing – original draft. MK: Methodology, Software, Writing – review & editing. LS: Conceptualization, Investigation, Methodology, Project administration, Supervision, Validation, Writing – review & editing.
Funding Statement
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2024.1354717/full#supplementary-material
References
- 1.World Health Organization (2014). World conference on social determinants of health: case studies on social determinants. Available at: http://www.who.int/sdhconference/resources/case_studies/en/
- 2.Office of Disease Prevention and Health Promotion (n.d.). Social determinants of health. Healthy people 2030. U.S. Department of Health and Human Services. Available at: https://health.gov/healthypeople/priority-areas/social-determinants-health
- 3.Krause TM, Schaefer C, Highfield L. The association of social determinants of health with health outcomes. Am J Manag Care. (2021) 27:e89–96. doi: 10.37765/ajmc.2021.88603, PMID: [DOI] [PubMed] [Google Scholar]
- 4.Agency for Healthcare Research and Quality (2021). 2021 National Healthcare Quality and Disparities Report: Executive Summary. [PubMed]
- 5.Liu D, Schuchard H, Burston B, Yamashita T, Albert S. Interventions to reduce healthcare disparities in cancer screening among minority adults: a systematic review. J Racial Ethn Health Disparities. (2021) 8:107–26. doi: 10.1007/s40615-020-00763-1, PMID: [DOI] [PubMed] [Google Scholar]
- 6.Zavala VA, Bracci PM, Carethers JM, Carvajal-Carmona L, Coggins NB, Cruz-Correa MR, et al. Cancer health disparities in racial/ethnic minorities in the United States. Br J Cancer. (2021) 124:315–32. doi: 10.1038/s41416-020-01038-6, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ward E, Jemal A, Cokkinides V, Singh GK, Cardinez C, Ghafoor A, et al. Cancer disparities by race/ethnicity and socioeconomic status. CA Cancer J Clin. (2004) 54:78–93. doi: 10.3322/canjclin.54.2.78 [DOI] [PubMed] [Google Scholar]
- 8.Mathers C, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. (2006) 3:e442. doi: 10.1371/journal.pmed.0030442, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.U.S. Preventive Services Task Force (2016). Breast cancer screening final recommendations. Available at: http://screeningforbreastcancer.org/ (Accessed May 26, 2023).
- 10.Coughlin SS, Uhler RJ, Richards T, Wilson KM. Breast and cervical cancer screening practices among Hispanic and non-Hispanic women residing near the United States-Mexico border, 1999–2000. Fam Commun Health. (2003) 26:130–9. doi: 10.1097/00003727-200304000-00006, PMID: [DOI] [PubMed] [Google Scholar]
- 11.Jones AR, Caplan LS, Davis MK. Racial/ethnic differences in the self-reported use of screening mammography. J Community Health. (2003) 28:301–16. doi: 10.1023/a:1025451412007 [DOI] [PubMed] [Google Scholar]
- 12.Rodriguez MA, Ward LM, Perez-Stable EJ. Breast and cervical cancer screening: impact of health insurance status, ethnicity, and nativity of Latinas. Ann Fam Med. (2005) 3:235–41. doi: 10.1370/afm.291, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lantz PM, Mujahid M, Schwartz K, Janz NK, Fagerlin A, Salem B, et al. The influence of race, ethnicity, and individual socioeconomic factors on breast cancer stage at diagnosis. Am J Public Health. (2006) 96:2173–8. doi: 10.2105/AJPH.2005.072132, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Abraido-Lanza AF, Chao MT, Gammon MD. Breast and cervical cancer screening among Latinas and non-Latina whites. Am J Public Health. (2004) 94:1393–8. doi: 10.2105/AJPH.94.8.1393, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. (2018) 169:467–73. doi: 10.7326/M18-0850, PMID: [DOI] [PubMed] [Google Scholar]
- 16.Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. (2005) 8:19–32. doi: 10.1080/1364557032000119616 [DOI] [Google Scholar]
- 17.American Cancer Society . ACS breast cancer screening guidelines. Cancer.org. (2023). Available at: https://www.cancer.org/cancer/types/breast-cancer/screening-tests-and-early-detection/american-cancer-society-recommendations-for-the-early-detection-of-breast-cancer.html (Accessed January 16, 2024).
- 18.Office of Disease Prevention and Health Promotion (2023). Social determinants of health. Health.gov. Available at: https://health.gov/healthypeople/objectives-and-data/social-determinants-health (Accessed August 15, 2023).
- 19.Elo S, Kyngäs H. The qualitative content analysis process. J Adv Nurs. (2008) 62:107–15. doi: 10.1111/j.1365-2648.2007.04569.x [DOI] [PubMed] [Google Scholar]
- 20.Henderson LM, O’Meara ES, Haas JS, Lee CI, Kerlikowske K, Sprague BL, et al. The role of social determinants of health in self-reported access to health care among women undergoing screening mammography. J Women's Health. (2020) 29:1437–46. doi: 10.1089/jwh.2019.8267, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Beaber EF, Tosteson ANA, Haas JS, Onega T, Sprague BL, Weaver DL, et al. Breast cancer screening initiation after turning 40 years of age within the PROSPR consortium. Breast Cancer Res Treat. (2016) 160:323–31. doi: 10.1007/s10549-016-3990-x, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jin SW, Lee HY, Lee J. Analyzing factors of breast cancer screening adherence among Korean American women using Andersen’s behavioral model of healthcare services utilization. Ethn Dis. (2019) 29:427–34. doi: 10.18865/ed.29.s2.427, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kosog K, Earle M, Stellon E, Nolan C, Wainwright MK, Webb T, et al. Identifying an association between socio-demographic factors and breast cancer screening adherence in a federally qualified health Centre sample in the United States. A retrospective, cross-sectional study. Health Soc Care Commun. (2020) 28:1772–9. [DOI] [PubMed] [Google Scholar]
- 24.Kempe KL, Larson RS, Shetterley S, Wilkinson A. Breast cancer screening in an insured population: whom are we missing? Perm J. (2013) 17:38–44. doi: 10.7812/TPP/12-068, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Selove R, Kilbourne B, Fadden MK, Sanderson M, Foster M, Offodile R, et al. Time from screening mammography to biopsy and from biopsy to breast cancer treatment among black and white, women medicare beneficiaries not participating in a health maintenance organization. Womens Health Issues. (2016) 26:642–7. doi: 10.1016/j.whi.2016.09.003, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wilcox ML, Acuña JM, Ward-Peterson M, Alzayed A, Alghamdi M, Aldaham S. Racial/ethnic disparities in annual mammogram compliance among households in little Haiti, Miami-Dade County, Florida: an observational study. Medicine. (2016) 95:e3826. doi: 10.1097/md.0000000000003826, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wilkerson AD, Obi M, Ortega C, Sebikali-Potts A, Wei W, Pederson HJ, et al. Young black women may be more likely to have first mammogram cancers: a new perspective in breast cancer disparities. Ann Surg Oncol. (2023) 30:2856–69. doi: 10.1245/s10434-022-12995-y, PMID: [DOI] [PubMed] [Google Scholar]
- 28.Agénor M, Pérez AE, Tabaac AR, Bond KT, Charlton BM, Bowen DJ, et al. Sexual orientation identity disparities in mammography among White, black, and Latina US women. LGBT Health. (2020) 7:312–20. doi: 10.1089/lgbt.2020.0039, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Alatrash M. Determinants of breast cancer screening in three Arab American women subgroups. J Transcult Nurs. (2021) 32:749–56. doi: 10.1177/10436596211008215 [DOI] [PubMed] [Google Scholar]
- 30.Jensen B, Khan H, Layeequr RR. Sociodemographic determinants in breast cancer screening among uninsured women of West Texas. Medicina. (2022) 58:1–12. doi: 10.3390/medicina58081010, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Anderson RT, Yang T-C, Matthews SA, Camacho F, Kern T, Mackley HB, et al. Breast cancer screening, area deprivation, and later-stage breast cancer in Appalachia: does geography matter? Health Serv Res. (2014) 49:546–67. doi: 10.1111/1475-6773.12108, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hong HC, Ferrans CE, Park C, Lee H, Quinn L, Collins EG. Effects of perceived discrimination and trust on breast cancer screening among Korean American women. Womens Health Issues. (2018) 28:188–96. doi: 10.1016/j.whi.2017.11.001, PMID: [DOI] [PubMed] [Google Scholar]
- 33.Agrawal P, Chen TA, McNeill LH, Acquati C, Connors SK, Nitturi V, et al. Factors associated with breast cancer screening adherence among church-going African American women. Int J Environ Res Public Health. (2021) 18:8494. doi: 10.3390/ijerph18168494, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Onega T, Tosteson TD, Weiss J, Haas JS, Goodrich M, DiFlorio R, et al. Multi-level influences on breast cancer screening in primary care. J Gen Intern Med. (2018) 33:1729–37. doi: 10.1007/s11606-018-4560-1, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dong W, Rose J, Kim U, Cooper GS, Tsui J, Koroukian SM. Medicaid expansion associated with reduction in geospatial breast cancer stage at diagnosis disparities. J Public Health Manag Pract. (2022) 28:469–77. doi: 10.1097/PHH.0000000000001514, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Henderson LM, Benefield T, Nyante SJ, Marsh MW, Greenwood-Hickman MA, Schroeder BF. Performance of digital screening mammography in a population-based cohort of black and white women. Cancer Causes Control. (2015) 26:1495–9. doi: 10.1007/s10552-015-0631-3, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Patel K, Kanu M, Liu J, Bond B, Brown E, Williams E, et al. Factors influencing breast cancer screening in low-income African Americans in Tennessee. J Community Health. (2014) 39:943–50. doi: 10.1007/s10900-014-9834-x, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Johnson CJ, Morawski BM, Hobbs L, Lewis D, Cariou C, Rycroft RK. Time from breast cancer diagnosis to treatment among Idaho’s National Breast and cervical Cancer early detection program population, 2011-2017. Cancer Causes Control. (2021) 32:667–73. doi: 10.1007/s10552-021-01407-3, PMID: [DOI] [PubMed] [Google Scholar]
- 39.Khaliq W, Aamar A, Wright SM. Predictors of non-adherence to breast cancer screening among hospitalized women. PLoS One. (2015) 10:e0145492. doi: 10.1371/journal.pone.0145492, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lee CI, Bogart A, Germino JC, Goldman LE, Hubbard RA, Haas JS, et al. Availability of advanced breast imaging at screening facilities serving vulnerable populations. J Med Screen. (2016) 23:24–30. doi: 10.1177/0969141315591616, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Virk-Baker MK, Martin MY, Levine RS, Wang X, Nagy TR, Pisu M. Mammography utilization among black and White Medicare beneficiaries in high breast cancer mortality US counties. Cancer Causes Control. (2013) 24:2187–96. doi: 10.1007/s10552-013-0295-9, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wiese D, Islami F, Henry KA. Changes in geographic accessibility to mammography by state and rural-urban status, United States, 2006-2022. J Natl Cancer Inst. (2023) 115:337–40. doi: 10.1093/jnci/djac217, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Oviedo AD. Mammogram adherence among Filipino American women. J Immigr Minor Health. (2022) 24:639–44. doi: 10.1007/s10903-021-01223-6, PMID: [DOI] [PubMed] [Google Scholar]
- 44.Nair RG, Lee SJC, Berry E, Argenbright KE, Tiro JA, Skinner CS. Long-term mammography adherence among uninsured women enrolled in the breast screening and patient navigation (BSPAN) program. Cancer Epidemiol Biomarkers Prev. (2022) 31:77–84. doi: 10.1158/1055-9965.EPI-21-0191, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Alabdullatif N, Arrieta A, Dlugasch L, Hu N. The impact of IT-based healthcare communication on mammography screening utilization among women in the United States: National Health Interview Survey (2011-2018). Int J Environ Res Public Health. (2022) 19:12737. doi: 10.3390/ijerph191912737, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Asgary R, Garland V, Sckell B. Breast cancer screening among homeless women of new York City shelter-based clinics. Womens Health Issues. (2014) 24:529–34. doi: 10.1016/j.whi.2014.06.002, PMID: [DOI] [PubMed] [Google Scholar]
- 47.Ayanian JZ, Landon BE, Zaslavsky AM, Newhouse JP. Racial and ethnic differences in use of mammography between Medicare advantage and traditional Medicare. J Natl Cancer Inst. (2013) 105:1891–6. doi: 10.1093/jnci/djt333, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Balazy KE, Benitez CM, Gutkin PM, Jacobson CE, von Eyben R, Horst KC. Association between primary language, a lack of mammographic screening, and later stage breast cancer presentation. Cancer. (2019) 125:2057–65. doi: 10.1002/cncr.32027, PMID: [DOI] [PubMed] [Google Scholar]
- 49.Beaber EF, Sprague BL, Tosteson ANA, Haas JS, Onega T, Schapira MM, et al. Multilevel predictors of continued adherence to breast cancer screening among women ages 50-74 years in a screening population. J Women's Health. (2019) 28:1051–9. doi: 10.1089/jwh.2018.6997, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Calo WA, Vernon SW, Lairson DR, Linder SH. Area-level socioeconomic inequalities in the use of mammography screening: a multilevel analysis of the health of Houston survey. Womens Health Issues. (2016) 26:201–7. doi: 10.1016/j.whi.2015.11.002, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Castañeda SF, Malcarne VL, Foster-Fishman PG, Davidson WS, Mumman MK, Riley N, et al. Health care access and breast cancer screening among Latinas along the California-Mexican border. J Immigr Minor Health. (2014) 16:670–81. doi: 10.1007/s10903-013-9938-x, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Cataneo JL, Meidl H, Ore AS, Raicu A, Schwarzova K, Cruz CG. The impact of limited language proficiency in screening for breast cancer. Clin Breast Cancer. (2023) 23:181–8. doi: 10.1016/j.clbc.2022.11.008, PMID: [DOI] [PubMed] [Google Scholar]
- 53.Chandak A, Nayar P, Lin G. Rural-urban disparities in access to breast cancer screening: a spatial clustering analysis: disparities in breast cancer screening. J Rural Health. (2019) 35:229–35. doi: 10.1111/jrh.12308, PMID: [DOI] [PubMed] [Google Scholar]
- 54.Christensen EW, Pelzl CE, Patel BK, Carlos RC, Rula EY. Urbanicity, income, and mammography-use disparities among American Indian women. Am J Prev Med. (2023) 64:611–20. doi: 10.1016/j.amepre.2023.01.013, PMID: [DOI] [PubMed] [Google Scholar]
- 55.Clark CR, Tosteson TD, Tosteson ANA, Onega T, Weiss JE, Harris KA, et al. Diffusion of digital breast tomosynthesis among women in primary care: associations with insurance type. Cancer Med. (2017) 6:1102–7. doi: 10.1002/cam4.1036, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Clarke TC, Endeshaw M, Duran D, Saraiya M. Breast cancer screening among women by nativity, birthplace, and length of time in the United States. Natl Health Stat Rep. (2019) 129:1–15. [PubMed] [Google Scholar]
- 57.Davis J, Liang J, Petterson MB, Roh AT, Chundu N, Kang P, et al. Risk factors for late screening mammography. Curr Probl Diagn Radiol. (2019) 48:40–4. doi: 10.1067/j.cpradiol.2017.10.014 [DOI] [PubMed] [Google Scholar]
- 58.Duggan C, Molina Y, Carosso E, Ibarra G, Thompson B. County of residence and screening practices among Latinas and non-Latina whites in two rural communities. Ethn Dis. (2019) 29:31–8. doi: 10.18865/ed.29.1.31, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Elkin EB, Paige Nobles J, Pinheiro LC, Atoria CL, Schrag D. Changes in access to screening mammography, 2008-2011. Cancer Causes Control. (2013) 24:1057–9. doi: 10.1007/s10552-013-0180-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Fedewa SA, de Moor JS, Ward EM, DeSantis CE, Goding Sauer A, Smith RA, et al. Mammography use and physician recommendation after the 2009 U.S. preventive services task force breast cancer screening recommendations. Am J Prev Med. (2016) 50:e123–31. doi: 10.1016/j.amepre.2015.10.010, PMID: [DOI] [PubMed] [Google Scholar]
- 61.Flores EJ, López D, Miles RC, Glover M, 4th, Lehman CD, Harvey HB, et al. Impact of primary care physician interaction on longitudinal adherence to screening mammography across different racial/ethnic groups. J Am Coll Radiol. (2019) 16:908–14. doi: 10.1016/j.jacr.2018.12.020, PMID: [DOI] [PubMed] [Google Scholar]
- 62.Guo Y, Cheng TC, Yun LH. Factors associated with adherence to preventive breast cancer screenings among middle-aged African American women. Soc Work Public Health. (2019) 34:646–56. doi: 10.1080/19371918.2019.1649226, PMID: [DOI] [PubMed] [Google Scholar]
- 63.Henry KA, McDonald K, Sherman R, Kinney AY, Stroup AM. Association between individual and geographic factors and nonadherence to mammography screening guidelines. J Women's Health. (2014) 23:664–74. doi: 10.1089/jwh.2013.4668, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Hubbard RA, O’Meara ES, Henderson LM, Hill D, Braithwaite D, Haas JS, et al. Multilevel factors associated with long-term adherence to screening mammography in older women in the U.S. Prev Med. (2016) 89:169–77. doi: 10.1016/j.ypmed.2016.05.034, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Jena AB, Huang J, Fireman B, Fung V, Gazelle S, Landrum MB, et al. Screening mammography for free: impact of eliminating cost sharing on cancer screening rates. Health Serv Res. (2017) 52:191–206. doi: 10.1111/1475-6773.12486, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Kim E, Moy L, Gao Y, Hartwell CA, Babb JS, Heller SL. City patterns of screening mammography uptake and disparity across the United States. Radiology. (2019) 293:151–7. doi: 10.1148/radiol.2019190647, PMID: [DOI] [PubMed] [Google Scholar]
- 67.Kim SE, Bachorik AE, Bertrand KA, Gunn CM. Differences in breast cancer screening practices by diabetes status and race/ethnicity in the United States. J Women's Health. (2022) 31:848–55. doi: 10.1089/jwh.2021.0396, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Komenaka IK, Nodora JN, Hsu C-H, Martinez ME, Gandhi SG, Bouton ME, et al. Association of health literacy with adherence to screening mammography guidelines. Obstet Gynecol. (2015) 125:852–9. doi: 10.1097/aog.0000000000000708, PMID: [DOI] [PubMed] [Google Scholar]
- 69.Lapeyrouse LM, Miranda PY, Morera OF. Heyman JM, Balcazar HG. Healthcare use and mammography among Latinas with and without health insurance near the US-Mexico border. J Racial Ethn Health Disparities. (2017) 4:282–7. doi: 10.1007/s40615-016-0227-y, PMID: [DOI] [PubMed] [Google Scholar]
- 70.Lee HY, Lee MH, Jang YJ, Lee DK. Breast cancer screening disparity among Korean American immigrant women in Midwest. Asian Pac J Cancer Prev. (2017) 18:2663–7. doi: 10.22034/APJCP.2017.18.10.2663, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Lee CI, Zhu W, Onega T, Henderson LM, Kerlikowske K, Sprague BL, et al. Comparative access to and use of digital breast tomosynthesis screening by women’s race/ethnicity and socioeconomic status. JAMA Netw Open. (2021) 4:e2037546. doi: 10.1001/jamanetworkopen.2020.37546 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Li L, Ji J, Besculides M, Bickell N, Margolies LR, Jandorf L, et al. Factors associated with mammography use: a side-by-side comparison of results from two national surveys. Cancer Med. (2020) 9:6430–51. doi: 10.1002/cam4.3128, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Luo Y, Carretta H, Lee I, LeBlanc G, Sinha D, Rust G. Naïve Bayesian network-based contribution analysis of tumor biology and healthcare factors to racial disparity in breast cancer stage-at-diagnosis. Health Inf Sci Syst. (2021) 9:35. doi: 10.1007/s13755-021-00165-5, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Molina Y, Plascak JJ, Patrick DL, Bishop S, Coronado GD, Beresford SAA. Neighborhood predictors of mammography barriers among US-based Latinas. J Racial Ethn Health Disparities. (2017) 4:233–42. doi: 10.1007/s40615-016-0222-3, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Monsivais P, Amiri S, Robison J, Pflugeisen C, Kordas G, Amram O. Racial and socioeconomic inequities in breast cancer screening before and during the COVID-19 pandemic: analysis of two cohorts of women 50 years +. Breast Cancer. (2022) 29:740–6. doi: 10.1007/s12282-022-01352-2, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Padela AI, Murrar S, Adviento B, Liao C, Hosseinian Z, Peek M, et al. Associations between religion-related factors and breast cancer screening among American Muslims. J Immigr Minor Health. (2015) 17:660–9. doi: 10.1007/s10903-014-0014-y, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Paranjpe A, Zheng C, Chagpar AB. Disparities in breast cancer screening between Caucasian and Asian American women. J Surg Res. (2022) 277:110–5. doi: 10.1016/j.jss.2022.03.032, PMID: [DOI] [PubMed] [Google Scholar]
- 78.Sabatino SA, Thompson TD, Guy GP, de Moor JS, Tangka FK. Mammography use among medicare beneficiaries after elimination of cost sharing. Med Care. (2016) 54:394–9. doi: 10.1097/mlr.0000000000000495, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Schommer L, Mikulski MF, Goodgame B, Brown KM. Racial disparities in breast cancer presentation and diagnosis in COVID-era Central Texas. J Surg Res. (2023) 288:79–86. doi: 10.1016/j.jss.2023.02.021, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Sealy-Jefferson S, Roseland ME, Cote ML, Lehman A, Whitsel EA, Mustafaa FN, et al. Rural-urban residence and stage at breast cancer diagnosis among postmenopausal women: the Women’s health initiative. J Women's Health. (2019) 28:276–83. doi: 10.1089/jwh.2017.6884, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Shon E-J, Townsend AL. Predictors of never having a mammogram among Chinese, Vietnamese, and Korean immigrant women in the U.S. PLoS One. (2019) 14:e0224505. doi: 10.1371/journal.pone.0224505, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Spada NG, Geramita EM, Zamanian M, van Londen GJ, Sun Z, Sabik LM. Changes in disparities in stage of breast cancer diagnosis in Pennsylvania after the affordable care act. J Women's Health. (2021) 30:324–31. doi: 10.1089/jwh.2020.8478, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Tangka FK, Subramanian S, Mobley LR, Hoover S, Wang J, Hall IJ, et al. Racial and ethnic disparities among state Medicaid programs for breast cancer screening. Prev Med. (2017) 102:59–64. doi: 10.1016/j.ypmed.2017.06.024, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Thomas M, James M, Vittinghoff E, Creasman JM, Schillinger D, Mangurian C. Mammography among women with severe mental illness: exploring disparities through a large retrospective cohort study. Psychiatr Serv. (2018) 69:48–54. doi: 10.1176/appi.ps.201600170, PMID: [DOI] [PubMed] [Google Scholar]
- 85.Tran L, Tran P. US urban-rural disparities in breast cancer-screening practices at the national, regional, and state level, 2012-2016. Cancer Causes Control. (2019) 30:1045–55. doi: 10.1007/s10552-019-01217-8, PMID: [DOI] [PubMed] [Google Scholar]
- 86.Vang S, Margolies LR, Jandorf L. Screening mammogram adherence in medically underserved women: does language preference matter? J Cancer Educ. (2022) 37:1076–82. doi: 10.1007/s13187-020-01922-y, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Wang H, Gregg A, Qiu F, Kim J, Chen B, Wan N, et al. Breast cancer screening for patients of rural accountable care organization clinics: a multi-level analysis of barriers and facilitators. J Community Health. (2018) 43:248–58. doi: 10.1007/s10900-017-0412-x, PMID: [DOI] [PubMed] [Google Scholar]
- 88.Wu AM, Morse AR, Seiple WH, Talwar N, Hansen SO, Lee PP, et al. Reduced mammography screening for breast cancer among women with visual impairment. Ophthalmology. (2021) 128:317–23. doi: 10.1016/j.ophtha.2020.07.029, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Kadivar H, Kenzik KM, Dewalt DA, Huang I-C. The association of English functional health literacy and the receipt of mammography among Hispanic women compared to non-Hispanic U.S.-born white women. PLoS One. (2016) 11:e0164307. doi: 10.1371/journal.pone.0164307, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Ryu SY, Crespi CM, Maxwell AE. What factors explain disparities in mammography rates among Asian-American immigrant women? A population-based study in California. Womens Health Issues. (2013) 23:e403–10. doi: 10.1016/j.whi.2013.08.005, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Korn AR, Walsh-Bailey C, Correa-Mendez M, DelNero P, Pilar M, Sandler B, et al. Social determinants of health and US cancer screening interventions: A systematic review. CA Cancer J Clin. (2023) 73:461–79. doi: 10.3322/caac.21801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Coughlin SS. Social determinants of breast cancer risk, stage, and survival. Breast Cancer Res Treat. (2019) 177:537–48. doi: 10.1007/s10549-019-05340-7 [DOI] [PubMed] [Google Scholar]
- 93.Alcaraz KI, Wiedt TL, Daniels EC, Yabroff KR, Guerra CE, Wender RC. Understanding and addressing social determinants to advance cancer health equity in the United States: a blueprint for practice, research, and policy. CA Cancer J Clin. (2020) 70:31–46. doi: 10.3322/caac.21586, PMID: [DOI] [PubMed] [Google Scholar]
- 94.Gomez SL, Shariff-Marco S, DeRouen M, Keegan TH, Yen IH, Mujahid M, et al. The impact of neighborhood social and built environment factors across the cancer continuum: current research, methodological considerations, and future directions. Cancer. (2015) 121:2314–30. doi: 10.1002/cncr.29345, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Williams AD, Moo TA. The impact of socioeconomic status and social determinants of health on disparities in breast Cancer incidence, treatment, and outcomes. Curr Breast Cancer Rep. (2023) 15:30–6. doi: 10.1007/s12609-023-00473-7 [DOI] [Google Scholar]
- 96.Sabik LM, Vichare AM, Dahman B, Bradley CJ. Co-payment policies and breast and cervical cancer screening in Medicaid. Am J Manag Care. (2020) 26:69–74. doi: 10.37765/ajmc.2020.42395, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Trivedi AN, Rakowski W, Ayanian JZ. Effect of cost sharing on screening mammography in Medicare health plans. N Engl J Med. (2008) 358:375–83. doi: 10.1056/NEJMsa070929, PMID: [DOI] [PubMed] [Google Scholar]
- 98.Amin A, Shriver CD, Henry LR, Lenington S, Peoples GE, Stojadinovic A. Breast cancer screening compliance among young women in a free access healthcare system. J Surg Oncol. (2008) 97:20–4. doi: 10.1002/jso.20895, PMID: [DOI] [PubMed] [Google Scholar]
- 99.Koç H, O’Donnell O, Van Ourti T. “Conclusion: In the absence of a universal screening program in the U.S., determinants of access—income, insurance coverage and receipt of medical advice—appear to drive the education disparities in screening mammography.” (2018) Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6163342/
- 100.White A, Thompson TD, White MC, Sabatino SA, de Moor J, Doria-Rose PV, et al. Cancer screening test use—United States, 2015. MMWR Morb Mortal Wkly Rep. (2017) 66:201–6. doi: 10.15585/mmwr.mm6608a1, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Tsapatsaris A, Babagbemi K, Reichman MB. Barriers to breast cancer screening are worsened amidst COVID-19 pandemic: a review. Clin Imaging. (2022) 82:224–7. doi: 10.1016/j.clinimag.2021.11.025, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Karliner LS, Ma L, Hofmann M, Kerlikowske K. Language barriers, location of care, and delays in follow-up of abnormal mammograms. Med Care. (2012) 50:171–8. doi: 10.1097/MLR.0b013e31822dcf2d, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Sentell TL, Tsoh JY, Davis T, Davis J, Braun KL. Low health literacy and cancer screening among Chinese americans in California: a cross-sectional analysis. BMJ Open. (2015) 5:e006104. doi: 10.1136/bmjopen-2014-006104, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Baccolini V, Isonne C, Salerno C, Giffi M, Migliara G, Mazzalai E, et al. The association between adherence to cancer screening programs and health literacy: a systematic review and meta-analysis. Prev Med. (2022) 155:106927. doi: 10.1016/j.ypmed.2021.106927, PMID: [DOI] [PubMed] [Google Scholar]
- 105.Liang W, Wang JH, Chen M-Y, Feng S, Lee M, Schwartz MD, et al. Developing and validating a measure of Chinese cultural views of health and cancer. Health Educ Behav. (2008) 35:361–75. doi: 10.1177/1090198106294893 [DOI] [PubMed] [Google Scholar]
- 106.Molaei-Zardanjani M, Savabi-Esfahani M, Taleghani F. Fatalism in breast cancer and performing mammography on women with or without a family history of breast cancer. BMC Womens Health. (2019) 19:116. doi: 10.1186/s12905-019-0810-6, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Barton MB, Moore S, Shtatland E, Bright R. The relation of household income to mammography utilization in a prepaid health care system. J Gen Intern Med. (2001) 16:200–3. doi: 10.1111/j.1525-1497.2001.00228.x, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Mahmood A, Kedia S, Dillon PJ, Kim H, Arshad H, Ray M. Food security status and breast cancer screening among women in the United States: evidence from the health and retirement study and health care and nutrition study. Cancer Causes Control. (2023) 34:321–35. doi: 10.1007/s10552-023-01667-1, PMID: [DOI] [PubMed] [Google Scholar]
- 109.Damiani G, Basso D, Acampora A, Bianchi CB, Silvestrini G, Frisicale EM, et al. The impact of level of education on adherence to breast and cervical cancer screening: evidence from a systematic review and meta-analysis. Prev Med. (2015) 81:281–9. doi: 10.1016/j.ypmed.2015.09.011, PMID: [DOI] [PubMed] [Google Scholar]
- 110.Khalil S, Hatch L, Price CR, Palakurty SH, Simoneit E, Radisic A, et al. Addressing breast Cancer screening disparities among uninsured and insured patients: a student-run free clinic initiative. J Community Health. (2020) 45:501–5. doi: 10.1007/s10900-019-00767-x, PMID: [DOI] [PubMed] [Google Scholar]
- 111.Lawson MB, Lee CI, Hippe DS, Chennupati S, Fedorenko CR, Malone KE, et al. Receipt of screening mammography by insured women diagnosed with breast cancer and impact on outcomes. J Natl Compr Cancer Netw. (2021) 19:1156–64. doi: 10.6004/jnccn.2020.7801, PMID: [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.