ABSTRACT
One-lung ventilation is indicated during thoracic surgery for visualization and exposure of surgical site. It is achieved with bronchial blockers, double-lumen endobronchial tube, single-lumen endotracheal tubes and Univent tube for infants and children. Fibreoptic bronchoscope is required for placing and confirming the correct position of these tubes. We report a perioperative management of safe conduct of one lung ventilation for a 6-year child undergoing left lower lobe lobectomy through C-MAC video laryngoscope guided two single lumen tubes in limited resource settings where paediatric-sized fibreoptic bronchoscope is unavailable.
Keywords: Lobectomy, one-lung ventilation, pediatric anesthesia
INTRODUCTION
One-lung ventilation (OLV) is essential for adequate visualization and exposure of surgical site during thoracic surgery. It is achieved with bronchial blockers, double-lumen endobronchial tubes (DLT), single-lumen endotracheal tubes (ETT), and the Univent tube for infants and children.[1] Fiber optic bronchoscope is required for placing and confirming the correct position of these tubes. The objective of this report is to describe perioperative management of safe conduct of one-lung ventilation with two endotracheal tubes to a child in limited resource settings where pediatric-sized fiber optic bronchoscope (FOB) is unavailable.
CASE HISTORY
A six-year-old female weighing 16 kgs was presented to the cardiothoracic and vascular surgery outpatient department with complaints of recurrent episodes of cough with blood-tinged sputum for 2 years. She had a history of multiple hospital admissions for it and was managed medically. She did not have any other specific complaints. On examination, she was hemodynamically stable, and facial anomaly and retrognathia were not detected. Chest auscultation revealed crepitations and decreased air entry in the lower lobe of the left lung. Her blood investigations were reported to be within normal limits. Chest X-ray showed multiple small cystic lesions in the lower lobe of the left lung. Computed tomography (CT) pulmonary angiography findings were suggestive of congenital lobar pulmonary sequestrations of the left lung. Diameter of the trachea, right bronchus, and left bronchus was measured to be 13 mm, 8 mm, and 6 mm, respectively, on CT. Left lower lobe lobectomy was planned. Informed written consent form was obtained from patient’s mother for publication.
After the pre-anesthetic assessment, she was shifted to the operation theater, American Society of anaesthesiologists (ASA) standard monitors non-invasive blood pressure, electrocardiogram, pulse oximetry was attached. Twenty G intravenous catheter was secured in the right and left upper limbs. Baseline parameters were noted. After preoxygenation, general anesthesia was induced as per standard technique with 2 μg/kg of fentanyl and 2 mg/kg of propofol. Neuromuscular blockade was achieved with 0.1 mg/kg of vecuronium with sevoflurane 2.5% to maintain adequate anesthetic depth for laryngoscopy and intubation. C-MAC video laryngoscope was used to place a 4.5-mm ID micro-cuff ETT (Tube A) into the trachea and pushed it forward to the right bronchus after assessing the tracheal and bronchial dimensions from the CT scan because a pediatric-sized fiber optic bronchoscope was not available in our institute. Its correct position at bronchial level was confirmed by set of alternative techniques, viz. auscultation showing air entry in the right side of lungs and no air entry in the left lung, presence of capnography with adequate delivery of tidal volume within normal peak pressure range and C-arm X-ray. The right lung was ventilated with ventilatory settings of tidal volume 80 ml, respiratory rate 16, and PEEP 4 for which delivered tidal volume was 70–72 ml with right lung isolation.
Again, under C-MAC guidance, a smaller-sized cuffed ETT of 3.5 mm ID (Tube B) was placed into the trachea. The position of tubes was reconfirmed with auscultation, ultrasonography, and C-arm X-ray [Figure 1]. Throat pack was placed to prevent any leaks. The bronchial tube was connected to the ventilator. The tracheal tube was connected to a Jackson–Rees circuit, and an adjusting pressure limit valve was regulated to provide continuous positive airway pressure (CPAP) of 2–4 cm H2O to the operating lung. The patient was positioned on the right lateral. Anesthesia was continued with oxygen and sevoflurane to maintain a minimum alveolar concentration (MAC) of 1 and SpO2 of ≥96%. Peak pressure, end tidal CO2, and delivered tidal volume were monitored continuously. Intermittent dosage of fentanyl, paracetamol, and left erector spinae plane block under ultrasound guidance was performed with 10 ml of 0.25% bupivacaine for analgesia. Arterial blood gas was done every hour to check for electrolyte parameters and oxygenation status. Left lobectomy was done, and the lung lower lobe was excised. The procedure was well-tolerated by the child for 4 h, after which she was changed to a supine position and the ETTs were replaced with a single 6 mm ETT and bilateral lung ventilation was resumed. She was shifted to pediatric intensive care unit and extubated after 3 h. Analgesia was continued with paracetamol, transferred to the ward the next day with stable hemodynamic, and oral feed was resumed. She was discharged on the third day and advised for follow-up.
Figure 1.
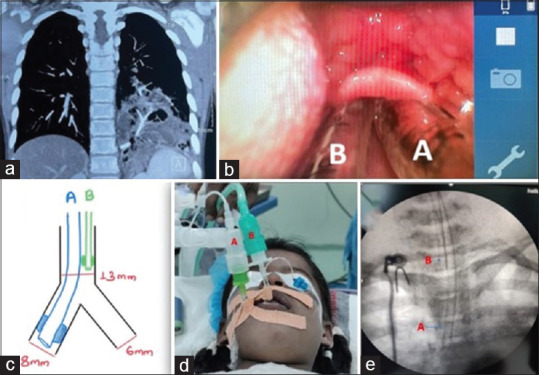
(a) CT lung showing lobar pulmonary sequestrations of the left lung, (b) C-MAC video laryngoscope image of two endotracheal tubes at the level of the epiglottis, (c) schematic diagram of the position of tubes within the airway, (d) (tube A) 4.5 mm ID micro-cuff endotracheal tube in the right bronchus, (tube B) 3.5 mm ID cuffed endotracheal tube in trachea, (e) C-ARM image confirming the position of Tube A in right bronchus and tube B in the trachea
DISCUSSION
Endobronchial intubation is one of the common approaches for one-lung ventilation among pediatric patients, but there is a chance of an improper seal, an inadequate collapse, and an inability to deliver CPAP to the operative lung.[2] 26Fr-sized double-lumen endobronchial tube is the smallest tube available and is used for isolating lung of children ≥8 years or ≥25 kgs. Lung separation is often achieved with the use of single-lumen endotracheal tube and a FOB-assisted bronchial blockers in children as DLTs are too large to be used in them. One-lung ventilation also creates a large intrapulmonary shunt as the non-ventilated lung is perfused without oxygenation. CPAP is essential to operative lung to avoid hypoxemia whenever OLV is desired for a prolonged duration. Hence, we placed another tube to deliver continuous CPAP and for passage of suctioning to the operative lung. Two tubes allowed for independent lung ventilation of the lungs.[3,4] Patients with chronic lung disease of the operative lung typically tolerate single-lung ventilation due to chronically decreased perfusion, and thus, the intrapulmonary shunt fraction is small. Tubes were selected based on CT measurements with consideration that the inner diameter of trachea (13 mm) is less than the sum of the outer diameter of tube A (6.2 mm) and tube B (5.3 mm). ET tube was pushed forward to the right bronchus to ensure the ventilation of the right lung primarily without any leaks and the right bronchus had a large diameter than left hence could accommodate larger size ET tube required for adequate ventilation. Right bronchus has smaller margin of safety as compared to the left bronchus; hence, a multimodal approach via ultrasonography, capnograph, and auscultations was performed for ensuring the correct placement of the endobronchial tube. The operating left lung was provided CPAP alone. It was not ventilated like the right lung as independent ventilation might cause asynchrony among both lungs predisposing to risk of mediastinal shift. Limitation of single-lung ventilation is that there is a little possibility of contamination of the normal lung in the setting of infection and hemorrhage. Hence, additional ETT facilitated frequent suctioning. Tube position was rechecked after changing the patient position to left lateral, and proper ventilation was ensured prior proceeding for surgery. Oxygenation and ventilation status were monitored through arterial blood gas. Lung protective strategy was ensured for ventilating right lung with tidal volume of 4–5 ml/kg and maintaining plateau pressure less than 30 cm H2O. However, we suggest to rule out the presence of subglottic stenosis before planning to place 2 ETT with its feature of biphasic stridor, dyspnea, air hunger and suprasternal, intercostal, and diaphragmatic retractions. Computed tomography (CT) and magnetic resonance imaging (MRI) are helpful in establishing its diagnosis and locating the exact site and length of the stenotic segment along the airway.[5] Fiber optic bronchoscope guided small size single ETT is required in such conditions.
CONCLUSIONS
Although fiber optic bronchoscope guided technique remains the gold standard for airway management for one-lung ventilation in pediatric. Two endotracheal tubes can be safely used for one-lung ventilation in children in case of its unavailability as an alternative with detailed assessment and formulating plans for perioperative management.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Fabila TS, Menghraj SJ. One lung ventilation strategies for infants and children undergoing video assisted thoracoscopic surgery. Indian J Anaesth. 2013;57:339–44. doi: 10.4103/0019-5049.118539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Templeton TW, Piccioni F, Chatterjee D. An update on one-lung ventilation in children. Anesth Analg. 2021;132:1389–99. doi: 10.1213/ANE.0000000000005077. [DOI] [PubMed] [Google Scholar]
- 3.Letal M, Theam M. Paediatric lung isolation. BJA Educ. 2017;17:57–62. [Google Scholar]
- 4.Paquet C, Karsli C. Technique of lung isolation for whole lung lavage in a child with pulmonary alveolar proteinosis. Anesthesiology. 2009;110:190–2. doi: 10.1097/ALN.0b013e318190bda2. [DOI] [PubMed] [Google Scholar]
- 5.Aravena C, Almeida FA, Mukhopadhyay S, Ghosh S, Lorenz RR, Murthy SC, et al. Idiopathic subglottic stenosis: A review. J Thorac Dis. 2020;12:1100–11. doi: 10.21037/jtd.2019.11.43. [DOI] [PMC free article] [PubMed] [Google Scholar]


