Abstract
Background
The integration of acupuncture with intramuscular injection of diclofenac sodium can expedite the onset of analgesia in treating acute renal colic caused by urolithiasis. However, it remains unclear whether acupuncture can accelerate pain relief constantly until complete remission. This study aimed to explore the extent to which acupuncture can expedite the onset time of response or complete pain relief in treating acute renal colic, and the predictive value of patient characteristics for treatment efficacy.
Methods
This secondary analysis utilized data from a prior randomized controlled trial. Eighty patients with acute renal colic were randomly assigned 1:1 to the acupuncture group or the sham acupuncture group. After intramuscular injection of diclofenac sodium, acupuncture or sham acupuncture was delivered to patients. The outcomes included time to response (at least a 50 % reduction in pain) and complete pain relief. Between-group comparison under the 2 events was estimated by Kaplan-Meier methodology. Subgroup analysis was performed utilizing the Cox proportional hazards model.
Results
The median response time and complete pain relief time in the acupuncture group were lower than those in the sham acupuncture group (5 vs 30 min, Log Rank P < 0.001; 20 min vs not observed, Log Rank P < 0.001, respectively). Hazard Ratios (HRs) for response across all subgroups favored the acupuncture group. All HRs for complete pain relief favored acupuncture, expect large stone and moderate pain at baseline. No interaction was found in either event.
Conclusion
Acupuncture can accelerate the response time and complete pain relief time for patients with acute renal colic, with the efficacy universally.
Trial registration
This study has been registered at Chinese Clinical Trial Registry: ChiCTR1900025202.
Key words: Acupuncture, Renal colic, Emergency medicine, Survival analysis
1. Introduction
Urolithiasis, a common pathological condition of the urinary system, exhibits a rising trend in its global incidence.1 Approximately 23.4 % of patients will experience stone-related symptoms within 5 years after a kidney stone diagnosis.2 Acute renal colic manifests as a sudden onset of pain in the lower back or upper abdomen or radiates into the groin, which is the most miserable one among all symptoms.3 In the emergency department, the key to managing acute renal colic is rapid analgesia.4 Nonsteroidal anti-inflammatory drugs (NSAIDs) are the first-line treatment for acute renal colic due to their superior analgesic effect and safety compared to opioids.5,6 However, the use of NSAIDs alone cannot fully address the need in the clinical practice. In a previous study comparing different analgesics in the treatment of acute renal colic, about a third of patients failed to reach halved pain 30 min after an injection of diclofenac or paracetamol.7
As a widely used complementary and alternative therapy,8 acupuncture received much attention in treating acute and chronic pain diseases.9,10 Our initial study revealed that in the context of administering diclofenac sodium via intramuscular injection, adjunctive acupuncture can increase the response rate (50 % reduction in baseline pain score) during the early time points (0, 5, 10, 15, 20, and 30 min) but not during the later time points (45 and 60 min) when compared to sham acupuncture.11 Due to the ceiling effect of response, it remains uncertain whether acupuncture can provide sustained pain relief following the response. In order to provide a comprehensive understanding of acupuncture analgesia, this study supplemented the complete pain relief as an outcome indicator for wide range evaluation. Using an approach in the form of occurrence time and an assessment of the overall effect across all time points rather than individual time points. In addition, patient characteristics, including female and higher baseline pain intensity, were suggested to predict an enhanced acupuncture efficacy.12, 13, 14 Identifying factors that can predict benefits before treatment is meaningful in clinical decision-making, yet these factors were not evaluated in acute renal colic patients treated by acupuncture.
This secondary analysis aimed to explore: (1) the differences between acupuncture and sham acupuncture in pain response time and complete pain relief time; (2) the correlation between patient characteristics and the effect of acupuncture.
2. Methods
2.1. Study design
Details of the initial study have been published.11,15 It was a single-center, sham-controlled, randomized controlled trial conducted in Beijing Hospital of Traditional Chinese Medicine Affiliated to Capital Medical University. All patients came from the emergency department. This study was approved by the ethics committee of the Beijing Hospital of Traditional Chinese Medicine Affiliated to Capital Medical University (2019BL02-025-01) and registered at the Chinese Clinical Trial Registry (ChiCTR1900025202).
2.2. Participant
Participants were included if they: (1) aged 18–75; (2) diagnosed with acute renal colic by X-ray or ultrasound within 24 h; (3) scored 4 or higher for pain intensity on visual analog scale (VAS) .16 Key exclusion criteria included receipt of analgesia within 6 h, allergy to diclofenac sodium, morphine, or anisodamine, serious cardiovascular or digestive diseases and pregnancy or lactation.
2.3. Randomization and blinding
Eighty acute renal colic patients in the emergency department were randomly assigned 1:1 to the acupuncture group or the sham acupuncture group. The random number sequence was generated via SAS 9.4 by an independent statistician. Opaque envelopes were utilized to ensure that the allocation remains concealed. Patients, outcome evaluators, and statistical analysts were blinded to the assignment, while acupuncturists were not.
2.4. Procedure
After baseline evaluation and randomization, all patients received 50 mg/2 mL of diclofenac sodium (Guangdong Bangmin Pharmaceutical Co, LTD) intramuscular injection. Immediately thereafter, patients received either acupuncture or sham acupuncture for 30 min. Bilateral Yaotongdian (EX-UE 7) were selected for the acupuncture group, wherein 4 needles were inserted to a depth of 8–10 mm. After needling, the needles were twirled, lifted and thrusted for 30 s to achieve De qi. Two nonacupoints on each arm were selected for the sham acupuncture group, which were penetrated shallowly (1–2 mm) without manipulation. The nonacupoints consisted of 16 points that were distinct from the actual acupoints and were determined to be devoid of any analgesic efficacy. These nonacupoints were randomly assigned to 8 subgroups, and one subgroup was randomly selected for each patient. This complex setup of nonacupoints was used to prevent treatment effect in the sham acupuncture group.17 Both interventions were administered by licensed acupuncture therapists who possess a minimum 5-year experience. If the patient scored higher than 8 on VAS at 60 min after needling, rescue analgesia of 0.1 mg/kg intravenous morphine (Northeast Pharmaceutical Group Shenyang First Pharmaceutical Co, Ltd) and 10 mg intramuscular racanisodamine (TianJin KingYork Pharmaceutical Co, Ltd) was administered.
2.5. Endpoints
The outcomes of this secondary analysis were time to response and complete pain relief. Response was defined as a reduction in VAS score by 50 % from the baseline, while complete pain relief was defined as achieving a VAS score of 0. The VAS is a visual analogue-based subjective rating scale ranging from 0 to 10, with higher scores representing more severe pain.16 Time points of evaluation were 0, 5, 10, 15, 20, 30, 45, and 60 min after manipulation.
2.6. Statistical analysis
Statistical analysis was conducted using SPSS 20.0 software. Intention-to-treat principles were applied, and all patients who underwent randomization were included in the analysis. Non-normal distributed continuous variables were expressed as median (interquartile range) [M (IQR)]. Counting data were expressed as frequencies. Cumulative incidence curves were generated by the Kaplan-Meier method, with the response or complete pain relief difined as the endpoints. Differences between groups were analyzed by log-rank test. Subgroup analysis was performed according to gender, age, body mass index (BMI), stone size and baseline pain level. Age (< 60 years, youth and middle age; ≥ 60 years, old age), BMI18 (< 24, normal or underweight; ≥ 24, overweight or obese), stone size19 (≤ 5 mm, small; > 5 mm, large) and baseline pain level20 (4 ≤ VAS < 7, moderate; VAS ≥ 7, severe) were transformed into categorical variables. Hazard ratios (HRs) and interaction P values were computed from a Cox proportional hazards model, with the group difined as a covariate. All statistical tests were two-sided, with P < 0.05 considered statistically significant. No data imputation was necessary, as there was no missing data in the initial study.
3. Results
A total of 80 patients were randomly assigned to the acupuncture group (n = 40) and sham acupuncture group (n = 40). All patients completed the trial with no dropouts or missing data. The demographic and baseline variables were comparable between groups, with no significant difference other than BMI (P = 0.02). Demographic and baseline data are presented in Table 1.
Table 1.
Demographic and baseline data.
| Variable | Participants, no. (%) |
P valuea | |
|---|---|---|---|
| Acupuncture (n = 40) | Sham acupuncture (n = 40) | ||
| Gender | >0.99 | ||
| Male | 33 (82.5) | 33 (82.5) | |
| Female | 7 (17.5) | 7 (17.5) | |
| Age | 0.58 | ||
| Youth and middle age (< 60 y) | 33 (82.5) | 31 (77.5) | |
| Old age (≥ 60 y) | 7 (17.5) | 9 (22.5) | |
| BMI | 0.02 | ||
| Normal or underweight (< 24 kg/m2) | 10 (25) | 20 (50) | |
| Overweight or obese (≥ 24 kg/m2) | 30 (75) | 20 (50) | |
| Stone size | >0.99 | ||
| Small (≤ 5 mm) | 29 (72.5) | 29 (72.5) | |
| Large (> 5 mm) | 11 (27.5) | 11 (27.5) | |
| Pain level | 0.23 | ||
| Moderate (4 ≤ VAS < 7) | 10 (25.0) | 15 (37.5) | |
| Severe (VAS ≥ 7) | 30 (75.0) | 25 (62.5) | |
Abbreviations: BMI, body mass index, calculated as weight in kilograms divided by height in meters squared; VAS, visual analog scale, range from 1 to 10, with higher scores indicating worse pain.
P values are based on χ2 tests.
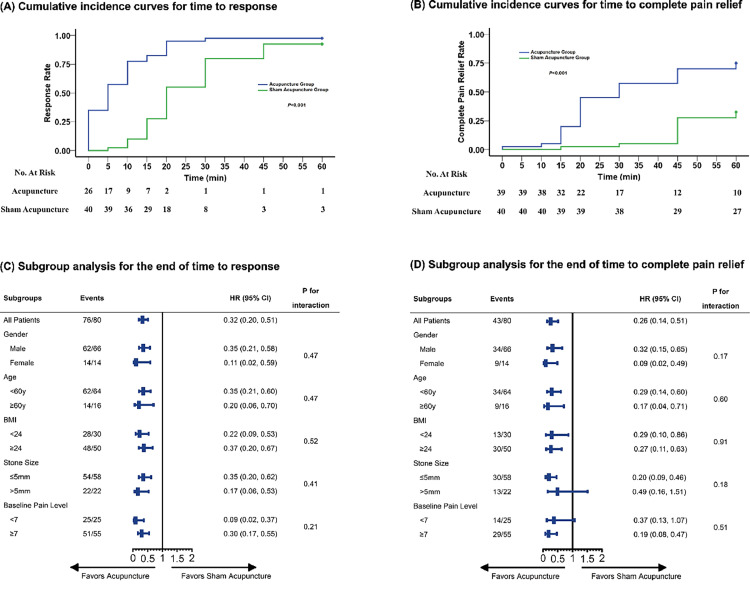
The median (IQR) time to response in the acupuncture group (5 [0, 10] min) was shorter than that in the sham acupuncture group (20 [15, 30] min; χ2 = 32.28, Log Rank P < 0.001). Within 15 min, 33 patients in the acupuncture group and 11 in the sham acupuncture group achieved the response event, with the numbers increasing to 39 and 37, respectively, at 60 min. The cumulative incidence curves for response are illustrated in Fig. 1A.
Fig. 1.
Cumulative incidence curves for time to (A) response and (B) complete pain relief; subgroup analysis for the end of (C) response and (D) complete pain relief.
In terms of complete pain relief time, a shorter median time was observed in the acupuncture group (30 [20, 60] min) than the sham acupuncture group (- [45,-] min; χ2 = 21.03, Log Rank P < 0.001). Within 15 min, 8 patients in the acupuncture group and 1 in the sham acupuncture group achieved the complete pain relief event, with the numbers increasing to 30 and 13, respectively, at 60 min. Fig. 1B depicts the cumulative incidence curves for complete pain relief.
There was an increase in the likelihood of response in the acupuncture group compared to the sham acupuncture group (HR, 0.32; 95 % CI, 0.20–0.51; Fig. 1C). HRs for response across all subgroups favored the acupuncture group (Fig. 1C), including male, female, youth and middle age, old age, normal or underweight, overweight or obese, small stone, large stone, moderate baseline pain level and severe baseline pain level. No significant result was found in the interaction P values.
For complete pain relief, results in the overall study population also favored acupuncture group (HR, 0.26; 95 % CI, 0.14–0.51; Fig. 1D). Subgroup analysis showed that, with the exception of the large stone and moderate baseline pain level subgroups, the male, female, youth and middle age, old age, normal or underweight, overweight or obese, small stone and severe baseline pain level subgroups favored the acupuncture group (Fig. 1D). No interaction was observed according to the interaction P values.
A sensitivity analysis was conducted to assess the impact of subgroup classification methods. The median values of age (47 years), BMI (24.6 kg/ m2), stone size (4 mm) and baseline VAS score (8) were established as boundary criteria for subgroup classification. Results of the sensitivity analysis were provided in the Supplement 1 and Supplement 2. All subgroups favored the acupuncture group in both events, with no interaction detected.
4. Discussion
The findings of this study indicated that the incorporation of acupuncture rather than sham acupuncture into intramuscular diclofenac sodium reduced the time required for patients with acute renal colic to achieve halved pain or painlessness. Moreover, the application of acupuncture exhibited favorable results across the majority of subgroups. These findings reinforced the evidence for the utilization of acupuncture as a complementary therapy in the management of acute renal colic.
With an intramuscular injection of diclofenac sodium, the median time to response and complete pain relief was much shorter in the acupuncture group (5 min/30 min) than in the sham acupuncture group (20 min/longer than 60 min). Despite acupuncture as a standalone intervention can provide pain relief for acute renal colic,21,22 it elicits superior effects at initial time points but inferior to diclofenac or acetaminophen at long-term time point.23 The varied onset times and analgesic intensities may contribute to different pathways. The analgesic effect of NSAIDs, for instance, diclofenac, mainly contributes to the inhibition of cyclooxygenase −1 and −2 and peripheral prostaglandins,24 which exhibits a delayed onset but persists for a prolonged duration. The analgesic mechanism of acupuncture involves neurotransmitters such as opioid peptide, glutamate, and calcium adenosine.25 These nerve conductions exhibit prompt onset but quickly fade. Therefore, this study suggests that the combination of acupuncture and NSAIDs can align with the need of clinical practice.
In pain disorders, the stratified care model needs evidence from clinical studies in order to provide the most appropriate therapy to a particular patient.26 Subgroup analysis presented favorable HRs for acupuncture in most subgroups, with no interaction across all subgroups. Patients with large stone size or moderate baseline pain intensity did not appear to derive a clear benefit from acupuncture for complete pain relief event, but no interaction was detected. These was possibly attributed to the limited events observed (8/7 in the acupuncture group and 5/7 in the sham acupuncture group). As the sensitivity analysis supported the efficacy for complete pain relief in these 2 subgroups, for this study alone, the efficacy of acupuncture for acute pain is considered universal.
In this study, a time-to-event analysis was employed. The time-to-event analysis allows for an overall comparison, rather than individual time points, also taking into account the patients who have not reached the endpoint at the end of the follow-up period.27 The 2 events used, response and complete pain relief, were both recommended and verified.5,28 A point-to-point evaluation approach was opted in most studies, that is, group comparisons at each evaluation time point. This design increases the probability of type I error due of multiple comparisons. In certain prior investigations, the difference in pain scores between groups was assessed.22,23 Since pain scores exhibit sensitivity in the assessment of acute pain, significant deviations may not always correspond with clinical significance. Consequently, overestimations of efficacy may occur, limit the utility for clinical practice. For improving the interpretation, dichotomous outcomes were recommended.28,29 The response, often defined as a 50 % reduction in pain score, represents a common dichotomous outcome in pain research.7,21,30 However, due to a ceiling effect, relying solely on response as an outcome has limitations in assessing between-group differences post-response. Our initial report failed to find an advantage of acupuncture at 45 and 60 min, as both groups exhibited high response rates early in the assessment. In this current secondary analysis, we confirmed that acupuncture can provide continuous analgesic effect until complete pain relief, rather than merely expediting the onset of analgesia. The use of rescue analgesia was not included in the analysis due to its occurrence in only one patient (acupuncture group).
The present study has several limitations. Firstly, as a post hoc analysis, no sample size calculation was conducted for current outcomes, resulting in a possible lack of power. Secondly, the 60-min follow-up period may be inadequate to observe the end of complete pain relief, particularly in the sham acupuncture group. Within 60 min, 75 % (30/40) of patients in the acupuncture group, compared to 32.5 % (13/40) in the sham acupuncture group, achieved this event. Although constrained by the total observations, according to the trends in Fig. 1B, we estimated that it may not compromise the assessment of acupuncture efficacy. Future studies can extend the follow-up time to obtain accurate quartile times for the sham acupuncture group, thus improving the stability of conclusions.
The efficacy of acupuncture in treating acute renal colic is long-lasting and universal. Despite the promising results, it is important to treat the conclusion cautiously, as further investigation with larger samples and longer follow-up is required to confirm their validity.
CRediT authorship contribution statement
Xue-Zhou Wang: Conceptualization, Software, Formal analysis, Writing – original draft. Cun-Zhi Liu: Validation, Writing – review & editing, Supervision, Project administration, Funding acquisition. Li-Qiong Wang: Methodology, Formal analysis, Writing – original draft. Zhi-Cheng Qu: Investigation, Writing – review & editing. Ying Cao: Investigation, Writing – review & editing. Shi-Yan Yan: Methodology, Investigation, Writing – review & editing. Jing-Wen Yang: Investigation, Writing – review & editing. Jian-Feng Tu: Conceptualization, Writing – review & editing, Supervision.
Acknowledgments
Declaration of competing interest
The authors declare that they have no conflicts of interest.
Funding
This study was supported by The National Science Fund for Distinguished Young Scholars (No.81825024). The funder has no role in design, data collection, analysis or interpretation.
Ethical statement
This study was approved by the ethics committee of the Beijing Hospital of Traditional Chinese Medicine Affiliated with Capital Medical University (2019BL02-025-01). All participants provided informed consent.
Data availability
The data sets generated during and/or analyzed during the current study are not publicly available due to protection of participants’ privacy but are available from the corresponding author on reasonable request.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.imr.2024.101021.
Supplement 1. Sensitivity analysis for the response event.
Supplement 2. Sensitivity analysis for the complete pain relief event.
Supplement 3. CONSORT checklist.
Appendix. Supplementary materials
References
- 1.Thongprayoon C, Krambeck AE. Rule AD. Determining the true burden of kidney stone disease. Nat Rev Nephrol. 2020;16(12):736–746. doi: 10.1038/s41581-020-0320-7. [DOI] [PubMed] [Google Scholar]
- 2.Li X, Zhu W, Lam W, Yue Y, Duan H, Zeng G. Outcomes of long-term follow-up of asymptomatic renal stones and prediction of stone-related events. BJU Int. 2019;123(3):485–492. doi: 10.1111/bju.14565. [DOI] [PubMed] [Google Scholar]
- 3.Bultitude M, Rees J. Management of renal colic. BMJ. 2012;345:e5499. doi: 10.1136/bmj.e5499. [DOI] [PubMed] [Google Scholar]
- 4.Afshar K, Jafari S, Marks AJ, Eftekhari A, MacNeily AE. Nonsteroidal anti-inflammatory drugs (NSAIDs) and non-opioids for acute renal colic. Cochrane Database Syst Rev. 2015;(6) doi: 10.1002/14651858.CD006027.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pathan SA, Mitra B, Cameron PA. A systematic review and meta-analysis comparing the efficacy of nonsteroidal anti-inflammatory drugs, opioids, and paracetamol in the treatment of acute renal colic. Eur Urol. 2018;73(4):583–595. doi: 10.1016/j.eururo.2017.11.001. [DOI] [PubMed] [Google Scholar]
- 6.Knoedler JJ, Lieske JC. Non-steroidal anti-inflammatory drugs for renal colic. Lancet. 2016;387(10032):1971–1972. doi: 10.1016/S0140-6736(16)00745-5. [DOI] [PubMed] [Google Scholar]
- 7.Pathan SA, Mitra B, Straney LD, Afzal MS, Anjum S, Shukla D, et al. Delivering safe and effective analgesia for management of renal colic in the emergency department: a double-blind, multigroup, randomised controlled trial. Lancet. 2016;387(10032):1999–2007. doi: 10.1016/S0140-6736(16)00652-8. [DOI] [PubMed] [Google Scholar]
- 8.Barnes PM, Bloom B, Nahin RL. Complementary and alternative medicine use among adults and children: united States, 2007. Natl Health Stat Re. 2008;(12):1–23. [PubMed] [Google Scholar]
- 9.Vickers AJ, Linde K. Acupuncture for chronic pain. JAMA. 2014;311(9):955–956. doi: 10.1001/jama.2013.285478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Coutaux A. Non-pharmacological treatments for pain relief: TENS and acupuncture. Joint Bone Spine. 2017;84(6):657–661. doi: 10.1016/j.jbspin.2017.02.005. [DOI] [PubMed] [Google Scholar]
- 11.Tu JF, Cao Y, Wang LQ, Shi GX, Jia LC, Liu BL, et al. Effect of adjunctive acupuncture on pain relief among emergency department patients with acute renal colic due to urolithiasis: a randomized clinical trial. JAMA Netw Open. 2022;5(8) doi: 10.1001/jamanetworkopen.2022.25735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Witt CM, Schützler L, Lüdtke R, Wegscheider K, Willich SN. Patient characteristics and variation in treatment outcomes: which patients benefit most from acupuncture for chronic pain. Clin J Pain. 2011;27(6):550–555. doi: 10.1097/AJP.0b013e31820dfbf5. [DOI] [PubMed] [Google Scholar]
- 13.Witt CM, Vertosick EA, Foster NE, Lewith G, Linde K, MacPherson H, et al. The effect of patient characteristics on acupuncture treatment outcomes: an individual patient data meta-analysis of 20,827 chronic pain patients in randomized controlled trials. Clin J Pain. 2019;35(5):428–434. doi: 10.1097/AJP.0000000000000691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sherman KJ, Cherkin DC, Ichikawa L, Avins AL, Barlow WE, Khalsa PS, et al. Characteristics of patients with chronic back pain who benefit from acupuncture. BMC Musculoskelet Disord. 2009;10:114. doi: 10.1186/1471-2474-10-114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cao Y, Tu JF, Shi GX, Wang LQ, Jia LC, Li B, et al. Acupuncture as adjunctive therapy for acute renal colic caused by urinary calculi: study protocol for a randomized controlled trial. Trials. 2021;22(1):652. doi: 10.1186/s13063-021-05600-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hjermstad MJ, Fayers PM, Haugen DF, Caraceni A, Hanks GW, Loge JH, et al. Studies comparing Numerical Rating Scales, Verbal Rating Scales, and Visual Analogue Scales for assessment of pain intensity in adults: a systematic literature review. J Pain Symptom Manage. 2011;41(6):1073–1093. doi: 10.1016/j.jpainsymman.2010.08.016. [DOI] [PubMed] [Google Scholar]
- 17.Wang LP, Zhang XZ, Guo J, Liu HL, Zhang Y, Liu CZ, et al. Efficacy of acupuncture for migraine prophylaxis: a single-blinded, double-dummy, randomized controlled trial. Pain. 2011;152(8):1864–1871. doi: 10.1016/j.pain.2011.04.006. [DOI] [PubMed] [Google Scholar]
- 18.Steering Committee . international diabetes institute; Melbourne: 2000. The Asia pacific perspective: Redefining Obesity and Its Treatment. [Google Scholar]
- 19.Yallappa S, Amer T, Jones P, Greco F, Tailly T, Somani BK, et al. Natural history of conservatively managed ureteral stones: analysis of 6600 patients. J Endourol. 2018;32(5):371–379. doi: 10.1089/end.2017.0848. [DOI] [PubMed] [Google Scholar]
- 20.Hawker GA, Mian S, Kendzerska T, French M. Measures of adult pain: visual Analog Scale for Pain (VAS Pain), Numeric Rating Scale for Pain (NRS Pain), McGill Pain Questionnaire (MPQ), Short-Form McGill Pain Questionnaire (SF-MPQ), Chronic Pain Grade Scale (CPGS), Short Form-36 Bodily Pain Scale (SF-36 BPS), and Measure of Intermittent and Constant Osteoarthritis Pain (ICOAP) Arthritis Care Res (Hoboken). 2011;63(11):S240–S252. doi: 10.1002/acr.20543. Suppl. [DOI] [PubMed] [Google Scholar]
- 21.Beltaief K, Grissa MH, Msolli MA, Bzeouich N, Fredj N, Sakma A, et al. Acupuncture versus titrated morphine in acute renal colic: a randomized controlled trial. J Pain Res. 2018;11:335–341. doi: 10.2147/JPR.S136299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lee YH, Lee WC, Chen MT, Huang JK, Chung C, Chang LS. Acupuncture in the treatment of renal colic. J Urol. 1992;147(1):16–18. doi: 10.1016/s0022-5347(17)37121-5. [DOI] [PubMed] [Google Scholar]
- 23.Kaynar M, Koyuncu F, Buldu İ, Tekinarslan E, Tepeler A, Karatağ T, et al. Comparison of the efficacy of diclofenac, acupuncture, and acetaminophen in the treatment of renal colic. Am J Emerg Med. 2015;33(6):749–753. doi: 10.1016/j.ajem.2015.02.033. [DOI] [PubMed] [Google Scholar]
- 24.Hoy SM. Diclofenac sodium bolus injection (Dyloject(TM)): a review in acute pain management. Drugs. 2016;76(12):1213–1220. doi: 10.1007/s40265-016-0619-7. [DOI] [PubMed] [Google Scholar]
- 25.Qiao L, Guo M, Qian J, Xu B, Gu C, Yang Y. Research advances on acupuncture analgesia. Am J Chin Med. 2020;48(2):245–258. doi: 10.1142/S0192415X20500135. [DOI] [PubMed] [Google Scholar]
- 26.Foster NE, Hill JC, O'Sullivan P, Hancock M. Stratified models of care. Best Pract Res Clin Rheumatol. 2013;27(5):649–661. doi: 10.1016/j.berh.2013.10.005. [DOI] [PubMed] [Google Scholar]
- 27.Schober P, Vetter TR. Survival analysis and interpretation of time-to-event data: the tortoise and the hare. Anesth Analg. 2018;127(3):792–798. doi: 10.1213/ANE.0000000000003653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cooper SA, Desjardins PJ, Turk DC, Dworkin RH, Katz NP, Kehlet H, et al. Research design considerations for single-dose analgesic clinical trials in acute pain: IMMPACT recommendations. Pain. 2016;157(2):288–301. doi: 10.1097/j.pain.0000000000000375. [DOI] [PubMed] [Google Scholar]
- 29.McQuay HJ, Derry S, Eccleston C, Wiffen PJ, Moore AR. Evidence for analgesic effect in acute pain—50 years on. Pain. 2012;153(7):1364–1367. doi: 10.1016/j.pain.2012.01.024. [DOI] [PubMed] [Google Scholar]
- 30.Pan M, Lan Y, Wang Z. Wrist-ankle acupuncture has a positive effect on chronic pain: a systematic review and meta-analysis. Acupunct Herb Med. 2023;3(1):7–19. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data sets generated during and/or analyzed during the current study are not publicly available due to protection of participants’ privacy but are available from the corresponding author on reasonable request.