Abstract
Purpose
To describe a rare case of acquired enophthalmos in a patient with idiopathic orbital inflammatory disease after treatment with systemic corticosteroids.
Observations
Orbital socket contracture produces a non-traumatic enophthalmos and is most frequently reported as a consequence of orbital trauma or metastatic fibrosis. A previously healthy 64-year-old male presented with 3-month history of binocular diplopia and left proptosis, hypoglobus, supraduction deficit, and compressive neuropathy. Imaging techniques showed a left orbital mass; laboratory tests and biopsy of the mass lead to the diagnosis of idiopathic orbital inflammatory disease. Systemic corticosteroids were administered and, surprisingly, the patient developed left enophthalmos with eyelid retraction.
Conclusions and Importance
Although extremely unusual, orbital socket contracture can cause enophthalmos and visual morbidity in patients with idiopathic orbital inflammatory disease treated with corticosteroids.
Keywords: Enophthalmos, Orbital socket contracture, Idiopathic orbital inflammatory disease, Corticosteroids
1. Introduction
Idiopathic Orbital Inflammatory Disease (IOID) is a group of disorders characterised by orbital inflammation,1,2 which usually presents with proptosis, limitation of extraocular movements and pain, and can show different degrees of severity.3 IOID should be considered a diagnosis of exclusion, with evaluation focused on eliminating other causes of orbital disease, such as orbital cellulitis, thyroid eye disease, sarcoidosis, lymphoid tumor, metastasis and rheumatological disorders.4 The prognosis of IOID depends on the tissues affected and the histology.3 It is typically steroid-responsive,2 however, their side effects, relapse rates and lack of response in some cases have resulted in them being partially replaced by immunosuppressive and immunomodulator therapies, in addition to radiotherapy and surgery.3
Enophthalmos is the posterior displacement of the eye within the orbit.5 It is usually secondary to orbital trauma, which can cause expansion of the orbital volume via fractures. Non-traumatic enophthalmos, although uncommon, may be the first manifestation of a local or systemic condition. It may be caused by silent sinus syndrome, silent brain syndrome,6 or malignancy, most notably scirrous breast carcinoma.7 Post inflammatory orbital socket contracture is a cause of non-traumatic enophthalmos and is defined as orbital inflammation with proptosis followed by the development of enophthalmos and radiographic evidence of residual fibrotic changes in the orbit.8
We report an extremely rare case of acquired enophthalmos due to post-inflammatory socket contracture in a patient with IOID treated with corticosteroids.
2. Case-report
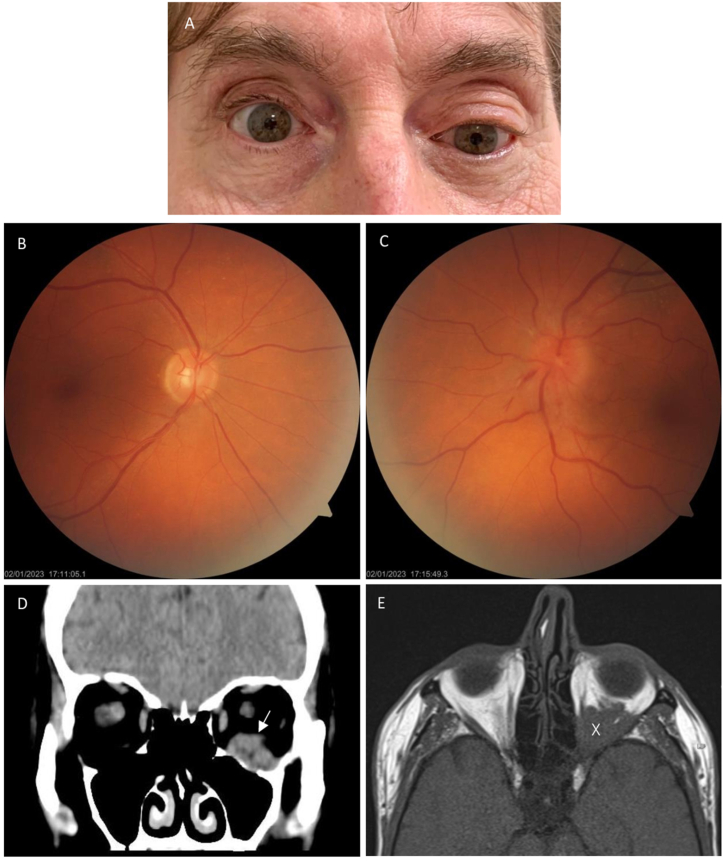
A previously healthy 64-year-old male presented with 3 months history of left proptosis and binocular diplopia. Detailed examination showed hypoglobus and supraduction deficit of the left eye, and 2mm proptosis was demonstrated by Hertel exophthalmometry (15mm in the right eye versus 17mm in the left eye) (Fig. 1A). Visual acuity and colour perception were preserved, but the patient presented a compressive left neuropathy with optic nerve oedema and relative afferent pupillary defect (RAPD) (Fig. 1B and C).
Fig. 1.
A) Left proptosis and inferior displacement of the globe before treatment with systemic corticosteroids. B) Normal fundoscopy of the right eye. C) Left optic disc oedema. D) Coronal CT without contrast showed a soft-tissue density mass on the floor of the left orbit (white arrow). E) Axial T1-weighted MRI showed left proptosis and an ill-defined mass in the left orbit (white X) involving the intra and extraconal compartments.
Laboratory tests did not support a specific diagnosis, including thyroid disease, sarcoidosis, granulomatosis with polyangiitis (GPA), Crohn's disease, rheumatoid arthritis, systemic lupus erythematosus, and infection. The CT and MRI (Fig. 1D and E) revealed a space-occupying lesion in the left orbit and ruled out orbital fractures. Due to the compressive neuropathy, 1-g intravenous methylprednisolone daily was initiated in theatre just after the biopsy of the mass was taken. The biopsy was performed with a transconjunctival approach through the lower eyelid and a sample of tissue occupying the inferior orbit was taken. Macroscopically, the lesion was pink and friable, it had a soft consistency and no capsule, and the surrounding bone was found intact, without erosions or notches. Histology results showed the presence of a chronic inflammatory infiltrate comprising aggregates of small lymphocytes without nuclear atypia (Fig. 2A), and the immunophenotype of the lymphoid cells revealed predominance of T cells (Fig. 2B), with presence of abundant B cells (Fig. 2C), concordant with polyclonality, and consistent with IOID.
Fig. 2.
A) Hematoxylin and eosin stained slides showed aggregates of small lymphocytes without nuclear atypia. B) The immunophenotype of the lymphoid cells revealed predominance of T cells (CD3), C) with presence of abundant B cells (CD20), concordant with polyclonality.
Once lymphoproliferative diseases were excluded, oral 1mg/kg prednisone was started with a slow taper over 8 weeks. Surprisingly, 10 days after initiating treatment, the patient complained about a sensation of a sunken left eye and exophthalmometry revealed 3mm enophthalmos (15mm in the right eye versus 12mm in the left eye), orbital fat atrophy and superior left eyelid retraction (Fig. 3A,B,C). The patient was in orthotropia in primary position, but he had binocular diplopia in extreme left gaze. MRI showed orbital fat atrophy (Fig. 3D).
Fig. 3.
A-C) Photographs showing deep superior sulcus and enophthalmos of the left eye after steroid treatment. D) Axial T2-weighted MRI showed atrophy of the soft tissues in the left orbit (white X), causing left enophthalmos.
3. Discussion
Non-traumatic enophthalmos has three main pathogenic mechanisms: structural changes in the bony orbit (silent sinus syndrome); orbital fat atrophy (age-related process or a lipodystrophy/scleroderma); and retraction secondary to fibrosis of the extraocular muscles or connective tissues (metastasis or post inflammatory).5
Enophthalmos caused by posterior traction secondary to fibrosis is most frequently reported as a result of orbital trauma or metastasis.8 To our knowledge, there are only a few cases of orbital socket contracture after an acute inflammatory disease. After conducting a literature review on the December 14, 2023 utilizing PubMed, Google Scholar, SCOPUS and EMBASE using the key words (IOID OR OID OR (Idiopathic AND orbital AND inflammatory AND disease) OR (orbital AND inflammatory AND disease)) AND (enophthalmos OR (non AND traumatic AND enophthalmos) OR (socket AND contracture)) AND (Steroids OR corticosteroids), we found only one case of IOID which developed abrupt unilateral enophthalmos after steroid therapy9 and one other case of enophthalmos as a consequence of the resolution of an IOID treated with radiation therapy.10 Talar-Williams et al. presented 6 cases of orbital socket contracture in patients with GPA during the treatment course of active inflammatory orbital disease with systemic immunosuppressants. Secondly, there are two publications of acquired enophthalmos in patients with lupus erythematosus after treatment with prednisolone.11,12
Systemic corticosteroids are currently considered first-line therapy for IOID and over 75% of patients show dramatic improvement.13 Undesirable ocular side effects of the use of systemic corticosteroids include glaucoma, cataract and herpetic corneal infection.14 However, orbital socket contracture has been rarely described.
In our case, a 64-year-old male with IOID received high-dose steroid treatment before enophthalmos and eyelid retraction appeared. Ocular motility improved after treatment, but the patient continued to have a mild restriction in extreme left gaze. We cannot exclude the possibility that our therapy with corticosteroids contributed to fat atrophy, but no local corticosteroid injection or other systemic treatment was administered, and no fat atrophy was observed in the contralateral orbit or elsewhere. Therefore, we conclude that his acquired enophthalmos occurred as a sequela of the acute inflammatory component of the orbital disease, and the residual fibrosis may be responsible for the contracture of the soft tissues within the orbit.8
4. Conclusion
Acquired enophthalmos due to orbital socket contracture in a patient with IOID occurred after treatment with systemic corticosteroids. The orbital socket contracture, presumably caused by orbital fibrosis, led to enophthalmos, eyelid retraction and restrictive ophthalmopathy. Orbital socket contracture, rarely reported as a complication of IOID treated with corticosteroids, can be an important cause of enophthalmos and visual morbidity. Further studies should be carried out to evaluate its prevalence and sequelae.
5. Patient consent
Consent to publish this case report has been obtained from the patient.
Funding
No funding or grant support.
CRediT authorship contribution statement
Sonia Peñarrocha-Oltra: Writing – review & editing, Writing – original draft. Marta Balboa Miró: Writing – review & editing. Marta Pérez-López: Writing – review & editing, Supervision. Nuria Ibáñez Flores: Writing – review & editing, Supervision.
Declaration of competing interest
The following authors have no financial disclosures: SPO, MBM, MPL, NIF.
Authorship: All authors attest that they meet the current ICMJE criteria for Authorship.
Acknowledgements
None.
References
- 1.Jacobs D., Galetta S. Diagnosis and management of orbital pseudotumor. Curr Opin Ophthalmol. 2002;13(6):347–351. doi: 10.1097/00055735-200212000-00001. [DOI] [PubMed] [Google Scholar]
- 2.Swamy B.N., McCluskey P., Nemet A., et al. Idiopathic orbital inflammatory syndrome: Clinical features and treatment outcomes. Br J Ophthalmol. 2007;91(12):1667–1670. doi: 10.1136/bjo.2007.124156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rachwani-Anil R., Zamorano-Martín F., Rocha-de-Lossada C., et al. Orbital inflammatory disease. Arch Soc Esp Oftalmol. 2022;97(2):89–99. doi: 10.1016/j.oftale.2021.05.001. [DOI] [PubMed] [Google Scholar]
- 4.Jacobs D., Galetta S. Diagnosis and management of orbital pseudotumor. Curr Opin Ophthalmol. 2002;13(6):347–351. doi: 10.1097/00055735-200212000-00001. [DOI] [PubMed] [Google Scholar]
- 5.Athanasiov P.A., Prabhakaran V.C., Selva D. Non-traumatic enophthalmos: a review. Acta Ophthalmol. 2008;86(4):356–364. doi: 10.1111/j.1755-3768.2007.01152.x. [DOI] [PubMed] [Google Scholar]
- 6.Chang J.R., Gruener A.M., McCulley T.J. Orbital disease in Neuro-Ophthalmology. Neurol Clin. 2017;35(1):125–144. doi: 10.1016/j.ncl.2016.08.011. [DOI] [PubMed] [Google Scholar]
- 7.Mourits M.P., Saeed P., Kloos R.J.H.M. [Enophthalmos as a first sign of breast cancer] Ned Tijdschr Geneeskd. 2015;159:A9114. [PubMed] [Google Scholar]
- 8.Talar-Williams C., Sneller M.C., Langford C.A., Smith J.A., Cox T.A., Robinson M.R. Orbital socket contracture: a complication of inflammatory orbital disease in patients with Wegener's granulomatosis. Br J Ophthalmol. 2005;89(4):493–497. doi: 10.1136/bjo.2004.050039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kakimaru A. A case of idiopathic orbital inflammation with abrupt unilateral enophthalmos caused by steroid therapy. Neuro Ophthalmol Jpn. 2006:467–473. Published online. [Google Scholar]
- 10.Prabhu R.S., Kandula S., Liebman L., et al. Association of Clinical response and Long-term Outcome Among patients with biopsied orbital pseudotumor receiving modern radiation therapy. Int J Radiat Oncol Biol Phys. 2013;85(3):643–649. doi: 10.1016/j.ijrobp.2012.06.033. [DOI] [PubMed] [Google Scholar]
- 11.Park K.R., Seo M.R., Ryu H.J., Chi M.J., Baek H.J., Choi H.J. Acquired enophthalmos with systemic lupus erythematosus. Lupus. 2016;25(1):88–92. doi: 10.1177/0961203315600245. [DOI] [PubMed] [Google Scholar]
- 12.Kao T.Y., Yoon M.K., McCulley T.J., Ruben B.S., Hwang T.N. Acquired enophthalmos in lupus erythematosus profundus. J Neuro Ophthalmol. 2010;30(1):64–66. doi: 10.1097/WNO.0b013e3181c25698. [DOI] [PubMed] [Google Scholar]
- 13.Secretariat M.A. Optical coherence tomography for age-related macular degeneration and diabetic macular edema: an evidence-based analysis. Ont Health Technol Assess Ser. 2009;9(13):1–22. [PMC free article] [PubMed] [Google Scholar]
- 14.Le Moli R., Baldeschi L., Saeed P., Regensburg N., Mourits M.P., Wiersinga W.M. Determinants of liver damage associated with intravenous methylprednisolone pulse therapy in Graves' ophthalmopathy. Thyroid. 2007;17(4):357–362. doi: 10.1089/thy.2006.0267. [DOI] [PubMed] [Google Scholar]