Abstract
Prostatic condyloma acuminata is a rarely encountered clinical manifestation primarily linked to low-risk subtypes of human papillomavirus (HPV), such as HPV-6 and HPV-11. Unlike the more common anogenital presentation, prostatic condyloma acuminata remains an infrequent phenomenon, necessitating a nuanced approach to diagnosis and management. We present a case report involving a 68-year-old patient with an intricate medical history, where the discovery of prostatic condyloma acuminata presented diagnostic challenges and clinical intricacies.
Keywords: Prostatic condyloma, Condyloma acuminata, HPV infection
1. Introduction
Prostatic condyloma acuminata, predominantly associated with low-risk HPV subtypes (HPV-6 and HPV-11), is a rare clinical presentation. It is distinct from the typical anogenital location of HPV-induced genital warts. In this report, we explore the clinical, diagnostic, and therapeutic aspects of prostatic condyloma acuminata.
2. Case presentation
A 68-year-old patient, with a history of diabetes, hypertension, and a coronary artery condition requiring stent placement, presented to our emergency department with fever and left-sided lower back pain, related to an idiopathic retroperitoneal fibrosis, which encases both ureters, that led to left-sided ureterohydronephrosis.
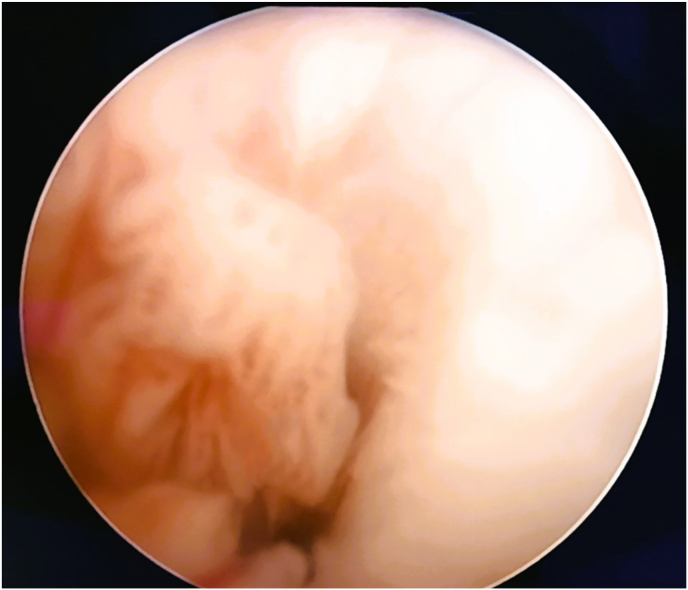
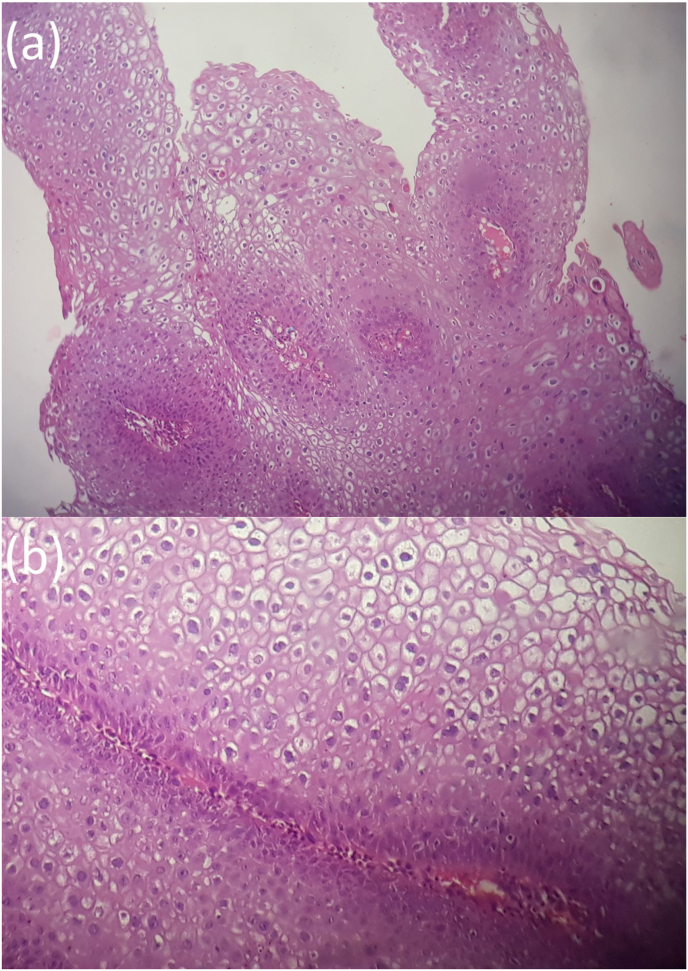
An emergency double J stent placement has been performed. Upon introducing the cystoscope, the entire urethra displayed multiple fringed, papillary-like processes (Fig. 1). These lesions were biopsied. The histopathological examination identified exophytic papillary fragments, with squamous epithelium displaying significant acanthosis. Some superficial cells exhibited koilocytosis with binucleation and a perinuclear clear halo. These findings were indicative of urethral condylomata acuminata (Fig. 2). The identification of the high-risk HPV viral genome was conducted using conventional PCR targeting a short, 67 base pair region specific to the HPV genome and the CYP2C8 gene, which is also specific to HPV.
Fig. 1.
Intraoperative photograph of an endoscopic view of the prostatic urethra covered with multiple fringed, papillary-like processes.
Fig. 2.
a: Papillary squamous lesion with parakeratosis (x 100). b: The squamous epithelium shows numerous koilocytes (x 200).
During the course of the patient's treatment, he developed urinary distension and renal insufficiency due to prostatic hypertrophy. Patient history revealed minimal prior urinary symptoms. A transurethral resection of the prostate was performed. The histopathological examination of the prostate chips revealed the same features as observed in the urethral biopsies of prostatic condyloma acuminata, in addition to fibromyoglandular hyperplasia without signs of malignancy.
The patient is currently on low-dose corticosteroids. A follow-up CT scan is scheduled for three months from now to determine the further management of his retroperitoneal fibrosis. As for the urethral condylomatosis, post-transurethral resection of the prostate, the patient no longer experiences urinary symptoms and reports a high degree of satisfaction with his voiding.
3. Discussion
Condyloma acuminata, commonly known as genital warts, is a well-known viral infection, mainly associated with the genital and anal regions. It usually manifests itself as soft, fleshy warts that are easily visible and identifiable. In rare cases, however, the condition may present differently, as in the case of prostatic-accumulated-condyloma.1
Prostatic condyloma acuminata, commonly known as genital warts, is an infrequent clinical presentation within the prostate. This condition is primarily associated with the human papillomavirus (HPV), specifically the low-risk subtypes such as HPV-6 and HPV-11. While HPV-related genital warts are more commonly observed in the anogenital area, their presence within the prostate is considered rare. HPV can spread locally from the genital or anal areas to nearby tissues. If a person has genital warts on or near the urethra, there is a possibility of the virus spreading to the prostate, which is in close proximity. In this discussion, we explore the clinical significance, diagnostic challenges, and management considerations related to prostatic condyloma acuminata.2
One of the key clinical implications of prostatic condyloma acuminata is its potential association with HPV infection. Genital warts caused by HPV are a well-recognized sexually transmitted infection, and their presence within the prostate raises questions about the mechanisms of viral transmission and the implications for prostate health. Understanding the prevalence and clinical impact of prostatic condyloma acuminata is essential for both patients and healthcare providers.
Diagnosing prostatic condyloma acuminata can be challenging due to its rare occurrence and the fact that it is often asymptomatic. The condition may be discovered incidentally during prostate examinations for unrelated reasons, such as prostate cancer screenings. Imaging studies, including transrectal ultrasound (TRUS), may reveal nodular lesions within the prostate, which can prompt further investigation. Histopathological examination of prostate biopsies, including the presence of characteristic koilocytes and viral particles, is necessary for definitive diagnosis. Additionally, molecular techniques such as PCR can be employed to confirm the presence of HPV DNA in prostate tissues.3
The management of prostatic condyloma acuminata should be approached cautiously. In many cases, the warts may regress spontaneously, and the primary goal of treatment is often to alleviate associated symptoms, if present. Options include surveillance, topical treatments, or, in rare cases, surgical intervention. Given the potential for complications and the lack of standardized guidelines, a personalized treatment plan should be developed, taking into account the patient's overall health and preferences 1.
Furthermore, it's important to consider the public health aspect of prostatic condyloma acuminata. The presence of HPV in the prostate may have implications for sexual partners and the potential transmission of the virus.4 Healthcare professionals should counsel patients on safe sexual practices and HPV vaccination as a preventive measure.5
In the realm of medical intricacies, one may encounter the enigmatic Condyloma acuminata, which has the propensity to manifest as singular, papillary growths nestled within the prostatic urethra. Remarkably, there may be an absence of any discernible lesions on the external genitalia, confounding both clinical observations and historical evidence. This peculiarity is an area where the realms of urology and pathology converge, demanding keen vigilance.
This uncommon condition can pose diagnostic challenges, as benign conditions may mimic malignant ones, such as urothelial or squamous carcinoma. The complexity is exacerbated when considering factors like urethral instrumentation and immunosuppression, which increase the likelihood of this atypical presentation. Differentiating between these neoplasms is crucial, as it determines distinct prognosis and treatment paths.
4. Conclusion
In summary, prostatic condyloma acuminata, a rare condition associated with low-risk HPV subtypes, presents unique clinical challenges. Diagnosing it can be intricate, often occurring incidentally during unrelated examinations. Treatment should be personalized, focusing on symptom relief. The public health dimension involves potential HPV transmission. Healthcare providers should emphasize safe practices and vaccination. This case underscores the need for vigilance in differentiating this rare condition from more serious neoplasms, as accurate diagnosis guides treatment and prognosis.
Consent
Signed consent was obtained from the patient.
CRediT authorship contribution statement
Houssem Aouini: Writing – original draft, Software, Resources, Conceptualization. Sami Chebbi: Writing – review & editing, Writing – original draft, Project administration, Data curation, Conceptualization. Bilel Saidani: Writing – review & editing, Software, Methodology, Conceptualization. Ahlem Blel: Validation, Resources, Methodology, Investigation. Marouene Chakroun: Validation, Project administration, Methodology, Conceptualization. Mohamed Riadh Ben Slama: Visualization, Validation, Conceptualization.
Declaration of competing interest
The authors declare that there are no conflicts of interest regarding the publication of this article.
References
- 1.Zayko M.O., Velilla R.E., Shurbaji M.S. Condyloma acuminata presenting as isolated papillary lesions in the prostatic urethra. Am J Case Rep. 2018 Dec 22;19:1522–1525. doi: 10.12659/AJCR.911682. PMID: 30578409; PMCID: PMC6320550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Scheinfeld N. 2017 Jan 4. Condylomata Acuminata (Anogenital Warts) in Adults: Epidemiology, Pathogenesis, Clinical Features, and Diagnosis. UpToDate. [Google Scholar]
- 3.Sarier M., Ozel E., Duman I., Yuksel Y., Demirbas A. HPV type 45-positive condyloma acuminata of the bladder in a renal transplant recipient. Transpl Infect Dis. 2017 Apr;19(2) doi: 10.1111/tid.12667. Epub 2017 Mar 16. PMID: 28100036. [DOI] [PubMed] [Google Scholar]
- 4.Skerlev M., Ljubojevic S. Posebnosti genitalnih infekcija humanim papiloma virusom u muskaraca [The specifities of the HPV-genital infections in males] Med Glas. 2010 Aug;7(2):89–95. Croatian. PMID: 21258302. [PubMed] [Google Scholar]
- 5.Sumino Y., Mimata H., Nomura Y. Urethral condyloma acuminata following urethral instrumentation in an elderly man. Int J Urol. 2004 Oct;11(10):928–930. doi: 10.1111/j.1442-2042.2004.00920.x. PMID: 15479306. [DOI] [PubMed] [Google Scholar]