Abstract
Human immunodeficiency virus remains a global public health problem. Despite efforts to determine the prevalence of non-adherence to ART and its predictors in Ethiopia, various primary studies presented inconsistent findings. Therefore, this review aimed to determine the pooled prevalence of non-adherence to ART and identify its predictors. We have searched PubMed, Google Scholar and Web of Science databases extensively for all available studies. A weighted inverse-variance random-effects model was used to compute the overall non-adherence to ART. The pooled prevalence of non-adherence to ART was 20.68% (95% CI: 17.74, 23.61); I2 = 98.40%; p < 0.001). Educational level of primary school and lower [AOR = 3.5, 95%CI: 1.7, 7.4], taking co-medications [AOR = 0.45, 95%CI: 0.35, 0.59], not using memory aids [AOR = 0.30, 95%CI: 0.13, 0.71], depression [AOR = 2.0, 95%CI: 1.05, 3.79], comorbidity [AOR = 2.12, 95%CI: 1.16, 3.09), under-nutrition [AOR = 2.02, 95%CI: 1.20, 3.43], not believing on ART can control HIV [AOR = 2.31, 95%CI: 1.92, 2.77], lack of access to health facilities [AOR = 3.86, 95%CI: 1.10, 13.51] and taking ART pills uncomfortably while others looking [AOR = 5.21, 95%CI: 2.56, 10.53] were significantly associated with non-adherence to anti-retroviral therapy. The overall pooled prevalence of non-adherence to ART was considerably high in Ethiopia. Educational status, taking co-medications, not using memory aids, depression, comorbidity, under nutrition, not believing on anti-retroviral therapy controls HIV, lack of access to health facilities and taking ART pills uncomfortably were independent predictors of non-adherence to ART in Ethiopia. Therefore, healthcare providers, adherence counselors and supporters should detect non-adherence behaviors and patients’ difficulties with ART early, and provide intensive counseling to promote adherence.
Supplementary Information
The online version contains supplementary material available at 10.1007/s10461-023-04252-4.
Keywords: Non-adherence to ART; Predictors; Ethiopia, Meta-analysis
Introduction
Human immunodeficiency virus/acquired immunodeficiency syndrome (HIV/AIDS) remains a major global public health problem [1–10]. As of 2021, it is estimated that 38.4 million people across the globe are living with HIV. In the same year, about 1.5 million new cases were recorded, and there were 650,000 deaths related to HIV/AIDS [11, 12]. Of this, the highest burden (60–90%) was accounted for developing countries including Ethiopia [2, 13, 14]. According to the Ethiopian Demographic and Health Survey (EDHS), 2016 report, the prevalence of HIV among the adult population was estimated to be 1.18% [15]. The World Health Organization (WHO) global disease burden, 2016 also reported that 768,040 people were living with HIV, 39,140 new cases, and 28,650 HIV/AIDS-related deaths in Ethiopia [16].
HIV/AIDS not only upset individuals’ health, but also influences the families, communities, sectors and the development of the nation [14, 17–19]. The introduction of anti-retroviral therapy (ART) was a crucial turning point in the history of HIV infection, and the gradual evolution of the infection into a chronic and non-fatal condition [20]. The primary goal of ART is to achieve and sustain viral suppression [20–22]. The initial challenge in combating HIV/AIDS epidemic was access to anti-retroviral (ARV) drugs [2, 23, 24].
However, increasing the production and decreasing the cost of ARV drugs intensively have facilitated the scaling-up of ART programs worldwide [23, 24]. The Joint United Nations Programme on HIV/AIDS set the 95-95-95 targets in order to combat the spread of HIV. By the year 2030, it is aimed that 95% of all people living with HIV (PLWH) will be aware of their HIV status. Additionally, 95% of those who are diagnosed with HIV will receive antiretroviral therapy [25, 26].
ART is recommended for all patients irrespective of their CD4 cell count, WHO staging and clinical status (test and treat strategy) [27, 28]. Early initiation and strict adherence to ART are important in the reduction of the progression of the virus through suppression of viral load and increase the level of cluster of differentiation 4 (CD4) cells count. This improves the survival and quality of life of the patient, increases productivity and decreases the incidence of opportunistic infections [5, 29, 30]. It is also believed that ART prevents the chance of HIV transmission by suppressing the viral load in infected individuals [31–33].
Adherence to ART is the patient’s ability to follow treatment plan by taking the correct dose of medications (≥ 95% of the prescribed doses) at prescribed time, frequencies (schedule) and following dietary instructions [9, 18, 34, 35]. It is strongly correlated with suppression of the disease and reduction of morbidity and mortality rates among people living with HIV [36–38], and the clinical outcomes of ART mainly depends on the adherence of patients to ART [19].
However, it often poses a special challenge and requires commitment from both the patient and the healthcare team [1, 39]. Non-adherence to ART is a major reason for treatment failure [35, 40, 41]. Ethiopia has implemented various strategies to enhance adherence to ART. These include transforming a fee-based ART program into a free one in 2005, decentralizing services to lower level health facilities and private hospitals and offering capacity building for service providers on counseling aspects [6, 42]. However, ensuring adherence to ART remains a major challenge in the country [6, 43].
Despite many efforts to determine the prevalence of non-adherence to ART and its predictors among adult people living with HIV in Ethiopia, various primary studies presented inconsistent findings and showed epidemiological variations ranging from 3% [2] to 61% [44]. Therefore, this review aimed to determine the pooled prevalence of non-adherence to ART and identify its predictors.
Methods
Reporting and Registration Protocol
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist [45] was used to report the results of this systematic review and meta-analysis (Supplemental Table 1). The review protocol was registered with Prospero database: (PROSPERO, 2023: CRD42023429516).
Databases and Search Strategy
We have extensively searched PubMed, Google Scholar, Web of Science databases for all available primary studies reporting non-adherence to ART and its predictors in Ethiopia using the following search terms and phrases: (ʺNon-adherenceʺ [MeSH term] OR ʺAdherenceʺ [MeSH term] OR ʺPrevalenceʺ [MeSH term]) AND (ʺAnti-retroviral therapyʺ [MeSH term]) AND (ʺPredictorsʺ [MeSH term] OR ʺAssociated factorsʺ [MeSH term] OR ʺRisk factorsʺ [MeSH term] OR ʺDeterminantsʺ [MeSH term]) AND ʺEthiopiaʺ. The search string was developed using ʺANDʺ and ʺORʺ Boolean Operators. Moreover, a manual search of the reference lists of included studies was also performed. The searched studies were published between 2007 and 2023 in Ethiopia and published in English.
Eligibility Criteria
All observational (cross-sectional, case-control and retrospective cohort) studies that were conducted among adult (age ≥ 18 years old) people living with HIV and which have reported the prevalence of non-adherence to ART and/or at least one associated factor of non-adherence to ART and written in English were included in the review. However, citations without abstracts, full texts, anonymous reports, editorials, systematic reviews and meta-analyses and qualitative studies were excluded from the review.
Study Selection
All the retrieved studies were exported to EndNote version 7 reference manager and the duplicated studies were removed. Initially, two independent reviewers (TM and SD) screened the titles and abstracts, followed by the full-text reviews to determine the eligibility of each study. The disagreement between the two reviews was solved through discussion.
Data Extraction
Two independent reviewers (TM and SZ) have extracted the data using a structured Microsoft excel data extraction form. Whenever variations were observed in the extracted data, the phase was repeated. While the discrepancies between the data extractors were continued, the third reviewer (AS) was involved. The name of the first author and year of publication, region, study area, study design, sample size, response rate and effect size of the included primary studies were extracted.
Primary Outcome Measure of Interest
The primary outcome of interest was prevalence of non-adherence to ART among adult people living with HIV in Ethiopia, which was determined by dividing the total number of non-adherents by the total number of study participants.
Operational Definitions of Variables
Non-adherence to ART is the condition of missing doses completely, not following the information given by the health care providers and taking drugs inappropriately [9, 18, 34, 35].
Data Analysis
STATA version 17 statistical software was used to analyze all the statistical analyses. A weighted inverse-variance random-effects model [46] was used to compute the overall non-adherence to ART and determine the impact of its predictors.
The presence of publication bias was checked by observing the symmetry of the funnel plot, and Egger’s test with a p-value of < 0.05 was also employed to determine a significant publication bias [47]. The percentage of total variation across studies due to heterogeneity was assessed using I2 statistics [48]. The values of I2 25,50 and 75% represented low, moderate and high heterogeneity respectively [48].
A p-value of I2 statistic < 0.05 was used to declare a significant heterogeneity [49, 50]. To identify the influence of a single study on the overall meta-analysis, sensitivity analysis was performed. A forest plot was used to estimate the effect of independent factors on the outcome variable and a measure of association at 95%CI was reported. The Odds Ratio (OR) was the most frequently reported measure of association in the eligible primary studies. When the included primary studies provided Risk Ratio results rather than ORs, we used Epi-Info along with descriptive statistics to convert these statistics to ORs.
To estimate the pooled OR effect, either a fixed-effects or a random-effects model is used. A fixed-effects model is used if all the included studies used comparable methodology and were from identical populations, whereas a random-effects model is used when the included studies used different methodologies and sampled from different populations. In our review, the included primary studies used different methodologies and drawn from several independent populations. Thus, a random-effects model was used for this study.
Results
Search Results
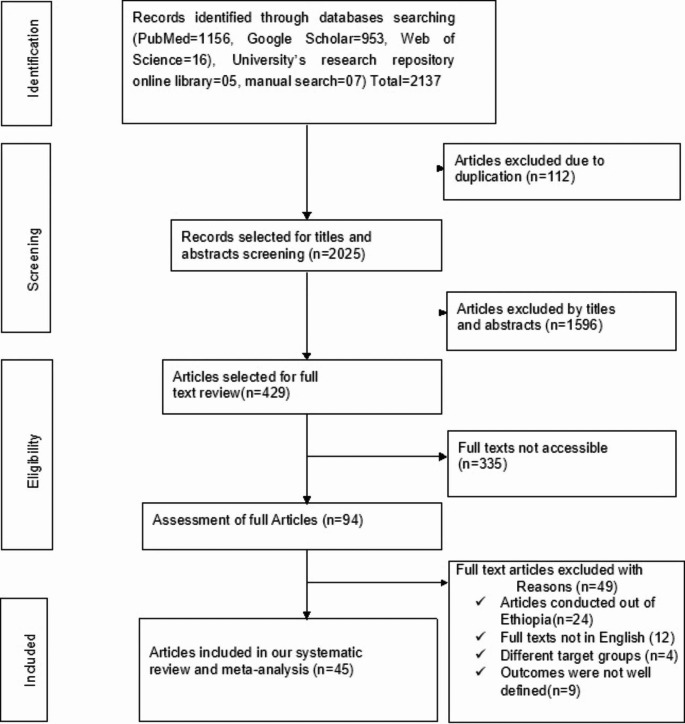
The search strategy retrieved a total of 2137 studies from PubMed (n = 1156), Google Scholar (n = 953), Web of Science (n = 16), manual search (n = 7) and University’s research repository online library (n = 5) studies. After carefully removing irrelevant studies based on their titles and abstracts (n = 1596) and duplicated studies (n = 112), a total of 429 studies were selected for full-text review.
Afterward, full-text reviews were conducted, resulting in the removal of 335 studies due to lack of complete texts. Then, 94 studies were assessed for full articles review and 49 studies were excluded (their full texts not written in English, conducted outside of Ethiopia, different target groups and the outcomes not well defined). Finally, 45 studies were found relevant to determine the prevalence of non-adherence to ART and identify its predictors. We traced the PRISMA flow chart [51] to show the selection process from initially identified records to finally included studies (Fig. 1).
Fig. 1.
PRISMA flow chart showing the studies selection process, 2023
Characteristics of the Included Studies
The forty-two studies [1–3, 5, 6, 8–10, 18, 19, 27, 29, 34, 43, 44, 52–78], two studies [79, 80] and one study [35] were conducted using cross-sectional, retrospective cohort and case-control studies respectively. Regarding geographical region, fourteen studies were conducted in Oromia [2, 3, 9, 18, 27, 44, 52, 57, 59, 64, 69, 76, 77, 79], eleven studies in Amhara [1, 6, 19, 56, 61, 66–68, 73, 75, 78], ten studies in Southern nations nationalities [5, 10, 34, 35, 43, 53, 55, 60, 62, 72], two studies in Addis Ababa [8, 44], two studies in Tigray [58, 80], one study in Oromia and Southern nations nationalities [54], one study in Harari and Dire Dawa [63] and one study was conducted in each Benishangul Gumuz [71], Somali [74], Harari [29], and Sidama region [65]. The total sample size of the included studies was 36,317, where the smallest sample size was 81 in Southern nations and nationalities and the largest sample size was also 19,525 in Tigray region health research institute. The prevalence of non-adherence to ART was obtained from forty-four included primary studies [1–3, 5, 6, 8–10, 18, 19, 27, 29, 34, 43, 44, 52–80], while the data regarding the predictors of non-adherence to ART were obtained from the thirty-five studies [1, 2, 5, 6, 8, 18, 19, 27, 29, 35, 44, 53–55, 57–61, 63–69, 71–74, 76–80], with a response rate ranges from 87 to 100% (Table 1).
Table 1.
General characteristics of the included studies
| ID | Author [Year] | Study area | Study design | Sample size | Prevalence (95% CI) | Quality |
|---|---|---|---|---|---|---|
| 1. | Abera A et al. [2015] | Oromia | CS | 221 | 36.19(29.9, 42.5) | Low risk |
| 2. | Alagaw A et al. [2013] | SNNP | CS | 357 | 25.6(21.1, 30.1) | Low risk |
| 3. | Amberbir A et al. [2008] | Oromia | Cohort | 400 | 5.7(3.4, 8.0) | Low risk |
| 4. | Angelo AT et al. [2021] | SNNP | CS | 329 | 16.7(12.7, 20.7) | Low risk |
| 5. | Assefa N et al. [2021] | A. A | CS | 422 | 61(56.4, 65.7) | Low risk |
| 6. | Awel M et al. [2007] | Oromia | CS | 459 | 17(13.6, 20.4) | Low risk |
| 7. | Aychiluhm SB et al. [2021] | Amhara | CS | 310 | 17.4(13.2, 21.6) | Low risk |
| 8. | Beyene KA et al. [2009] | Oromia + SNNP | CS | 422 | 6.9(4.5, 9.3) | Low risk |
| 9. | Billoro BB et al. [2018] | SNNP | CS | 265 | 43.8(37.8, 49.8) | Low risk |
| 10. | Bitew BD et al. [2014] | SNNP | Case-control | 462 | Not applicable | Low risk |
| 11. | Chaka TE et al. [2016] | Oromia | CS | 1,631 | 3(2.2, 3.8) | Low risk |
| 12. | Debito T et al. [2014] | SNNP | CS | 341 | 21.4(17.1, 25.8) | Low risk |
| 13. | Demas Z et al. [2022] | Oromia | CS | 385 | 30.6(26.0, 35.2) | Low risk |
| 14. | Demeke B et al. [2014] | Amhara | CS | 130 | 10(4.8, 15.2) | Low risk |
| 15. | Demessie R et al. [2014] | A. A | CS | 350 | 20.9(16.6, 25.2) | Low risk |
| 16. | Desta AA et al. [2020] | Tigray | Cohort | 19,525 | 5.16(4.9, 5.5) | Low risk |
| 17. | Dibaba D et al. [2021] | Oromia | CS | 445 | 10.2(7.4, 13.0) | Low risk |
| 18. | Ejigu M et al. [2020] | Oromia | CS | 284 | 19(14.4, 23.6) | Low risk |
| 19. | Ejigu SH et al [2014] | Oromia | CS | 271 | 21.1(16.2, 26.0) | Low risk |
| 20. | Gebregziabher TT et al. [2020] | Tigray | CS | 339 | 25.4(20.8, 30.0) | Low risk |
| 21. | Hassen A et al. [2018] | Oromia | CS | 352 | 26.4(21.8, 31.0) | Low risk |
| 22. | Hebo SH et al. [2019] | SNNP | CS | 355 | 32.23(27.4, 37.1) | Low risk |
| 23. | Hussen HS et al. [2019] | SNNP | CS | 391 | 32.23(27.6, 36.9) | Low risk |
| 24. | Jima F et al. [2018] | Amhara | CS | 160 | 14.4(9.0, 19.8) | Low risk |
| 25. | Kassahun TB et al. [2018] | Oromia | CS | 321 | 27.7(22.8, 32.6) | Low risk |
| 26. | Koyra HC et al. [2018] | SNNP | CS | 320 | 32(27.0, 37.1) | Low risk |
| 27. | Letta S et al. [2016] | Harari + Dire D | CS | 620 | 15(12.2, 17.8) | Low risk |
| 28. | Markos E et al. [2008] | Sidama | CS | 291 | 25.8()20.8, 30.8 | Low risk |
| 29. | Mengistie A et al. [2018] | Amhara | CS | 352 | 5(2.7, 7.3) | Low risk |
| 30. | Mitku H et al. [2013] | Harari | CS | 239 | 13(8.7, 17.3) | Low risk |
| 31. | Mitku AA et al. [2016] | Amhara | CS | 224 | 10.3(6.3, 14.3) | Low risk |
| 32. | Mohammed M et al. [2023] | Amhara | CS | 394 | 33.2(28.6, 37.9) | Low risk |
| 33. | Molla AA et al. [2018] | Amhara | CS | 440 | 11.8(8.8, 14.8) | Low risk |
| 34. | Negash E et al. [2016] | Oromia | CS | 383 | 10.7(7.6, 13.8) | Low risk |
| 35. | Nigusso FT et al. [2020] | B/Gumuz | CS | 390 | 39.7(34.8, 44.6) | Low risk |
| 36. | Reta H et al. [2017] | SNNP | CS | 81 | 11(4.2, 17.8) | Low risk |
| 37. | Rike M et al. [2021 | SNNP | CS | 370 | 19.7(15.7, 23.8) | Low risk |
| 38. | Tadesse S et al. [2014 | Amhara | CS | 647 | 14.7(12.0, 17.4) | Low risk |
| 39. | Tesfay S et al. [2022] | Somali | CS | 373 | 23.1(18.8, 27.4) | Low risk |
| 40. | Tessema B et al. [2010] | Amhara | CS | 504 | 17.3(14.0, 20.6) | Low risk |
| 41. | Tiyou A et al. [2010] | Oromia | CS | 319 | 27.6(22.7, 32.5) | Low risk |
| 42. | Tsega B et al. [2015] | Amhara | CS | 351 | 19.1(15.0, 23.2) | Low risk |
| 43. | Yadeta AD et al. [2016] | Oromia | CS | 326 | 33.74(28.6, 38.9) | Low risk |
| 44. | Zeleke AB et al. [2012] | Oromia | CS | 334 | 6.29(3.7, 8.9) | Low risk |
| 45. | Zewude SB et al. [2022] | Amhara | CS | 432 | 18.5(14.8, 22.2) | Low risk |
Abbreviations: AA, Addis Ababa; B/Gumuz, Benishangul Gumuz; CS, cross-sectional; Dire D, Dire Dawa;SNNP,Southern nations, nationalities and peoples
Quality Appraisal of the Included Studies
Two independent reviewers (TM and SD) appraised the quality of the included studies ,and scored for the validity of results. The quality of each study was evaluated using the Joanna Briggs Institute (JBI) quality appraisal criteria [81]. Forty-two studies [1–3, 5, 6, 8–10, 18, 19, 27, 29, 34, 43, 44, 52–78], two studies [79, 80] and one study [35] were appraised using JBI checklist for cross-sectional, cohort and case-control studies respectively.
Thus, among the forty-two cross-sectional studies, thirty-four studies scored seven of eight questions, 87.5% (low risk), five studies scored six of eight questions, 75% (low risk), and the remaining three studies also scored five of eight questions, 62.5% (low risk). Likewise, among the two cohort studies, one study scored eight of ten questions, 80% (low risk), and the second study also scored seven of ten questions, 70% (low risk). Moreover, one case-control study was appraised and scored eight of ten questions (Supplemental Table 2).
Studies were deemed to be of low risk when they scored 50% or higher on the quality assessment indicators. After conducting a thorough quality appraisal, we determined that the primary studies included in our analysis displayed a high level of reliability in their methodological quality scores. The cross-sectional studies scored between 5 and 7 out of a total of 8 points, while the cohort and case-control studies scored between 7 and 8 out of a total of 10 points. Thus, all included studies [1–3, 5, 6, 8–10, 18, 19, 27, 29, 34, 35, 43, 44, 52–80] had high quality.
Risk of Bias Assessment
The assessment tool [82] was used to assess the risk of bias. It consists of ten items that assess four areas of bias: internal validity and external validity. Items 1–4 evaluate selection bias, non-response bias and external validity. Items 5–10 assess measure bias, analysis-related bias, and internal validity. Accordingly, of the total of the forty-five included studies, thirty-nine studies scored eight of ten questions and the six studies also scored seven of ten questions. Studies were classified as ʺlow riskʺ if eight and above of ten questions received a ʺYesʺ, as ʺmoderate riskʺ if six to seven of ten questions received a ʺYesʺ and as ʺhigh riskʺ if five or lower of ten questions received a ʺYesʺ. Therefore, all included studies [1–3, 5, 6, 8–10, 18, 19, 27, 29, 34, 35, 43, 44, 52–80] had low risk of bias (high quality) (Supplemental Table 3).
Meta-Analysis
Non-Adherence to Anti-Retroviral Therapy
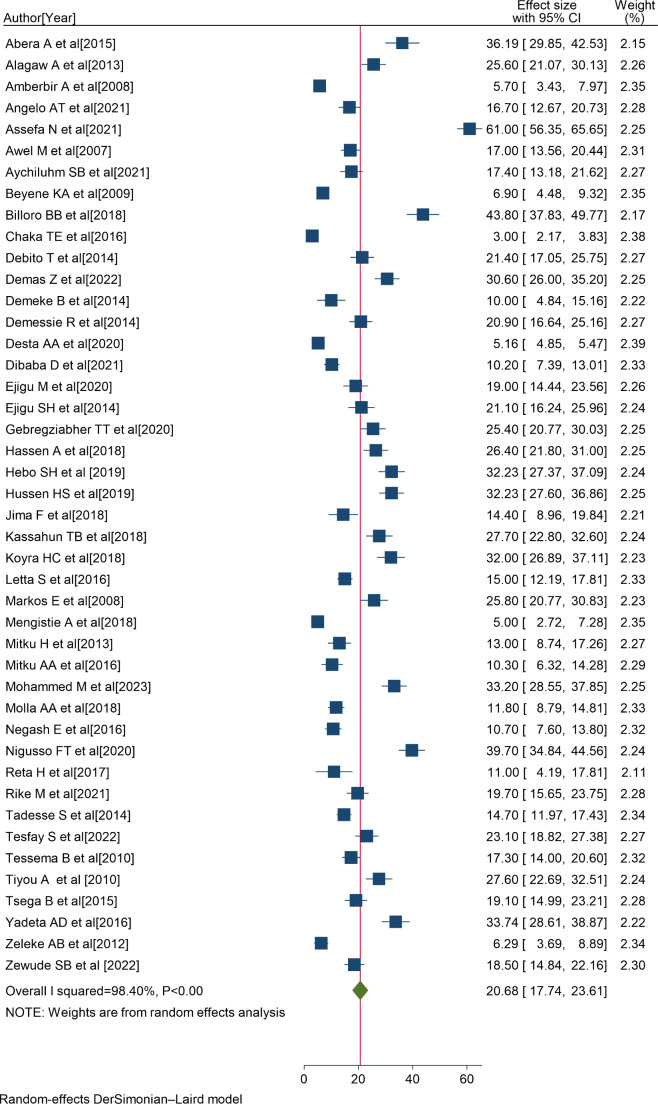
Consequently, 45 eligible primary studies [1–3, 5, 6, 8–10, 18, 19, 27, 29, 34, 35, 43, 44, 52–80] were included in the final meta-analysis. In Ethiopia, the prevalence of non-adherence to ART ranges from 3% in Oromia [2] to 61% in Addis Ababa [44], and the overall pooled prevalence of non-adherence to ART was 20.68% (95% CI:17.74, 23.61); I2 = 98.40%; P < 0.001) (Fig. 2).
Fig. 2.
Forest plot showing the pooled non-adherence to ART in Ethiopia, 2023
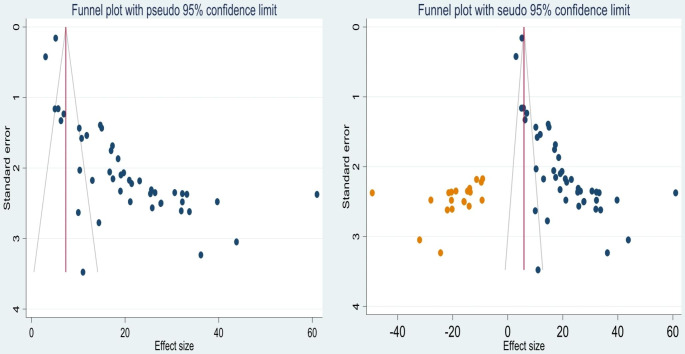
Publication Bias
The asymmetry of the included primary studies on the funnel plot suggests the presence of publication bias (Fig. 3a), and the p-value of Egger’s regression test (P < 0.001) also indicated the presence of publication bias. Hence, we have done trim and fill analysis to manage the publication bias (Fig. 3b).
Fig. 3.
Funnel plot showing the publication bias of non-adherence to ART before adjustment a and after adjustment with trim and fill analysis b in Ethiopia, 2023
Investigation of Heterogeneity
The percentage of I2 statistics of the forest plot indicates a marked heterogeneity among the included studies (I2 = 98.40%, P < 0.001) (Fig. 2). Hence, sensitivity analysis and sub-group analysis were performed to minimize the heterogeneity.
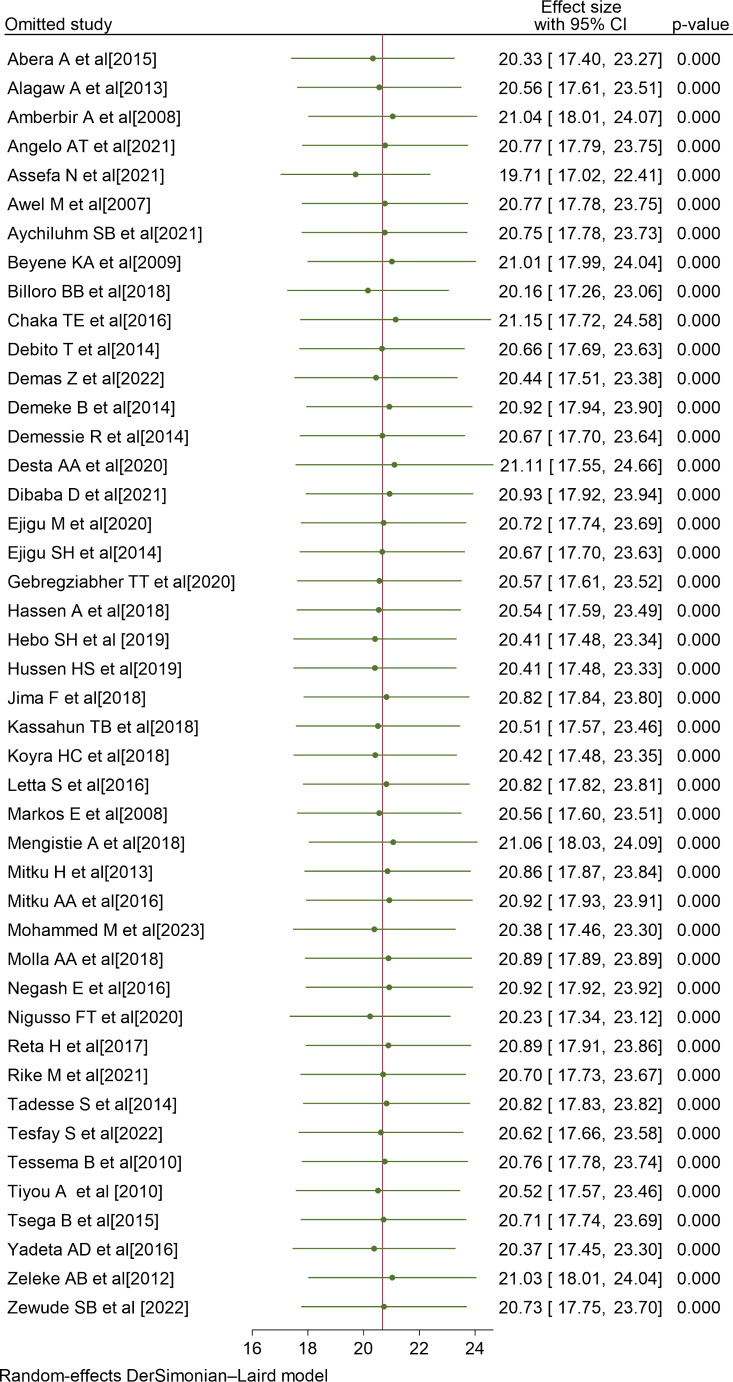
Sensitivity Analysis
To determine the influence of a particular study on the overall meta-analysis, we conducted a sensitivity analysis. The forest plot showed that the estimate from a single study is closer to the combined estimate, which implied the absence of a single study effect on the overall pooled estimate. Thus, it has been demonstrated that a solitary study has no significant impact on the overall outcome of the meta-analysis (Fig. 4).
Fig. 4.
Sensitivity analysis of non-adherence to ART in Ethiopia, 2023
Sub-group Analysis by the Sample Size
The sample size sub-group analysis showed the higher pooled prevalence of non-adherence to ART with <350 sample sizes [21.63, 95%CI: 17.10, 26.15, I2= 94.55%, P<0.001] followed by ≥350 sample sizes [19.94, 95%CI: 16.35, 23.52, I2= 98.70%, P<0.001] (Table 2).
Table 2.
Subgroup analysis of non-adherence to ART in Ethiopia, 2023
| Variables | Outcome | Subgroup | No. of studies | Model | Prevalence (95%CI) |
I2 | P-value |
|---|---|---|---|---|---|---|---|
| Sample size | ART non-adherence | ≥ 350 | 25 | Random | 19.94(16.35, 23.52) | 98.70% | 0.00 |
| < 350 | 20 | Random | 21.63(17.10, 26.15) | 94.55% | 0.00 | ||
| Study period | ART non-adherence | ≥ 2018 | 23 | Random | 24.70(18.65, 30.74) | 98.91% | 0.00 |
| < 2018 | 22 | Random | 16.74(12.96, 20.53) | 97.08% | 0.00 |
Sub-group analysis by the Study Period
The pooled prevalence of non-adherence to ART in studies conducted before the year 2018 was 16.74 [95%CI: 12.96, 20.53, I2 = 97.08%, P < 0.001], which was lower than the studies conducted in the year 2018 and later [24.70, 95% CI: 18.65, 30.74; I2 = 98.91%; P < 0.001] (Table 2). Based on the sub-group analyses, it appears that the heterogeneity of this study may be attributed to differences in sample sizes and study periods among the primary studies that were included.
Predictors of Non-Adherence to ART
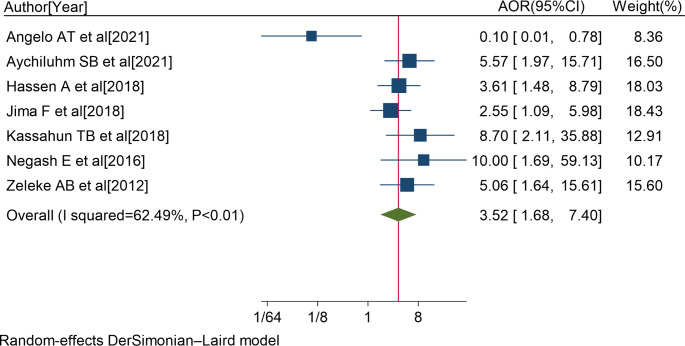
In the review, seven studies [5, 19, 52, 54, 59, 61, 64] reported that educational level of primary school and lower was significantly associated with non-adherence to ART. The pooled AOR of non-adherence to ART for patients with educational level of primary school and below was 3.52 (95%CI: 1.68, 7.40; I2 = 62.49%; P < 0.01) (Fig. 5).
Fig. 5.
Forest plot of the adjusted odds ratios with corresponding 95% CIs of studies on the association of educational level of primary school and lower and non-adherence to ART. The midpoint and the length of each segment indicated an AOR and a 95% CI; and the diamond shape showed the combined AOR of all studies
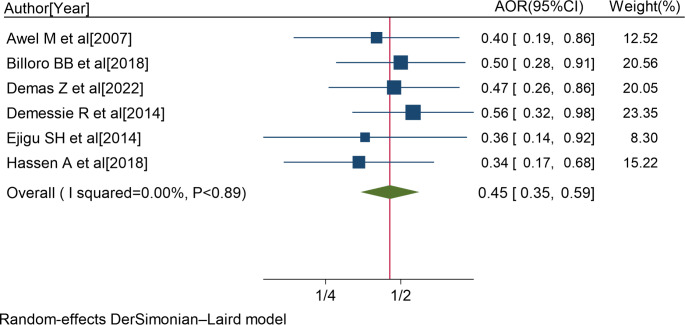
Six studies [8, 18, 34, 57, 59, 64] showed a significant association between taking co-medications and non-adherence to ART. The pooled AOR of non-adherence to ART for patients with co-medications was 0.45 (95%CI: 0.35, 0.59; I2 = 0.00%; P < 0.89) (Fig. 6).
Fig. 6.
Forest plot of the adjusted odds ratios with corresponding 95% CIs of studies on the association of co-medications and non-adherence to ART. The midpoint and the length of each segment indicated an AOR and a 95% CI; and the diamond shape showed the combined AOR of all studies
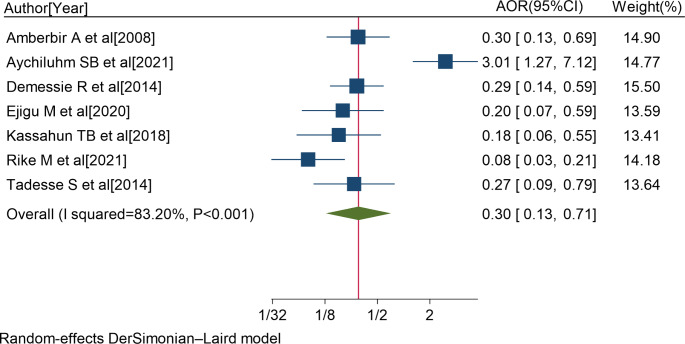
Seven studies [6, 8, 27, 62, 72, 73, 79] also reported a significant association between not using memory aids and non-adherence to ART. The pooled AOR of non-adherence to ART for patients who were not using memory aids was 0.30 (95%CI: 0.13, 0.71; I2 = 83.20%; P < 0.001) (Fig. 7).
Fig. 7.
Forest plot of the adjusted odds ratios with corresponding 95% CIs of studies on the association of not using memory aids and non-adherence to ART. The midpoint and the length of each segment indicated an AOR and a 95% CI; and the diamond shape showed the combined AOR of all studies
Six studies [19, 44, 53, 58, 60, 79] showed a significant association between depression and non-adherence to ART. The pooled AOR of non-adherence to ART for patients with depression was 2.0 (95%CI: 1.05, 3.79).
Three studies [5, 62, 83] reported a significant association between comorbidity and non-adherence to ART. The pooled AOR of non-adherence to ART for patients with comorbidity was 2.12 (95%CI: 1.16, 3.09).
Three studies [35, 69, 71] also showed a significant association between under-nutrition and non-adherence to ART. The pooled AOR of non-adherence to ART for patients with under-nutrition was 2.02 (95%CI: 1.20, 3.43).
Three studies [55, 57, 64] also showed a significant association between not believing on ART controls HIV and non-adherence to ART. The pooled AOR of non-adherence to ART for patients who didn’t belief that ART controls HIV was 2.31 (95%CI: 1.92, 2.77).
Two studies [34, 64] reported a significant association between lack of access to health facilities and non-adherence to ART. The pooled AOR of non-adherence to ART for patients with lack of access to health facilities was 3.86 (95%CI: 1.10, 13.51).
Two studies [1, 72] showed a significant association between taking ART pills uncomfortably while others looking and non-adherence to ART. The pooled AOR of non-adherence to ART for patients taking ART pills uncomfortably while others looking was 5.21 (95%CI: 2.56, 10.53).
Thus, PLWH with educational level of primary school and lower were 3.5 times more likely to have non-adherence to ART compared with those with educational level of secondary school and above.
Likewise, PLWH who were taking co-medications were 2.2 times more likely to develop non-adherence to ART than PLWH who didn’t take co-medications.
Those PLWH who were not using memory aids were also 3.3 times more likely to have non-adherence to ART compared to PLWH who were using memory aids.
In this study, adult PLWH with depression were 2 times more likely to develop non-adherence to ART than those who didn’t have depression.
Similarly, PLWH with comorbidity were 2.1 times more likely to develop non-adherence to ART than PLWH without comorbidity.
Besides, PLWH with under-nutrition (BMI < 18.5 Kg/m2) were 2 times more likely to have non-adherence to ART compared to those without under-nutrition.
PLWH who didn’t believe on ART can control HIV were 2.3 times more likely to have non-adherence to ART than those who believed that ART controls HIV.
Additionally, PLWH with lack of access to health facilities were 3.9 times more likely to develop non-adherence to ART than those who had access to health facilities. Moreover, PLWH who were taking ART pills uncomfortably while others looking were 5.2 times more likely to develop non-adherence to ART than their counterparts.
Discussion
This review aimed to determine the overall pooled prevalence of non-adherence to ART and its predictors in Ethiopia. In this study, the overall pooled prevalence of non-adherence to ART was 20.68% (95% CI: 17.74, 23.61; I2 = 98.40%; p < 0.001), which was higher than the study findings conducted in India (12.4%) [84], Vietnam (11.5%) [85], Kenya (18%) [86], Indonesia (18.5%) [87], Orlu of Nigeria (17.1%) [14], Monze and Nyimba districts of Zambia (16.5%) [88], and Kasama district of Zambia (18%) [89].
But the finding was lower than the study findings conducted in Senegal (24.6%) [90], Northwest province of Zambia (27%) [91], China (28%) [92], Cameroon (37.78%) [7], Nepal (40%) [93], South Nigeria (40.1%) [94] and Benin city, Nigeria (41.9%) [95]. This discrepancy could be due to differences in study settings, methodologies, health care delivery systems across settings and the existence of socio-cultural variations [6].
Furthermore, the finding of this study reported that adult PLWH with educational level of primary school and lower were 3.5 times more likely to have non-adherence to ART than those with educational level of secondary school and above. This finding was consistent with the study finding conducted in Cameroon [7] and Vietnam [85]. It is possible that the low level of education among individuals also leads to a low level of awareness about HIV and its treatment. Consequently, the non-adherence to ART may be high [5].
According to the findings of this study, PLWH who were taking co-medications were also 2.2 times more likely to develop non-adherence to ART than PLWH who didn’t take co-medications. Patients who take co-medications may experience perceived side effects, which could lead them to skip or miss their ART regimens [96].
It has been found that not using memory aids is a significant predictor of non-adherence to ART. People living with HIV who do not use memory aids are 3.3 times more likely to have non-adherence to ART compared to those who do use memory aids. The finding was in line with a study conducted in Vietnam [97]. One way to make it easier for patients to remember when to take their medication is by using memory aids [98].
The finding of this study also showed that Adult PLWH with depression were 2 times more likely to have non-adherence to ART than those who didn’t have depression. This might be explained as patients become depressed, they would be hopeless and in turn, they might skip or miss to take their regular ART regimens. This finding supports the role of HIV/AIDS counselors in screening for depression and providing treatment when appropriate, either directly or through collaboration with the mental health professionals [53].
Similarly, the finding indicated that PLWH with comorbidity were 2.1 times more likely to develop non-adherence to ART than PLWH without comorbidity. The possible reason might be explained as patients with comorbid diseases could be tired and limit them from taking ART regimens regularly [5].
Besides, PLWH with under-nutrition were 2 times more likely to have non-adherence to ART compared to those without under-nutrition. This finding is consistent with studies conducted in Zambian and Uganda [99, 100]. Patients with low nutritional status could have reduced immunity, posing the patients to be suffered from frequent opportunistic infections. This can affect drug metabolism, absorption and efficacy of drugs, potentially leading to non-adherence to ART [101].
Similarly, PLWH who didn’t belief that ART can control the virus were 2.3 times more likely to be non-adherent to ART compared to those who believed ART can control the virus. It might be explained that this false belief could encourage patients to cease taking ART regimens [102].
Additionally, PLWH who don’t have access to health facilities are nearly four times more likely to struggle with adherence to antiretroviral therapy (ART) compared to those who do have access to health facilities. This finding is supported with a study conducted in Ghana [103]. PLWH who were willing to take ART could became non-adherent because of difficulties in reaching the treatment centers due to unexpected transport and other strikes; long travel distance; geographical difficulty including lack of transportation services in many remote areas; and the seasonal deterioration of poorer roads during the rainy season [104].
Moreover, PLWH who were taking ART pills uncomfortably while others looking were 5.2 times more likely to develop non-adherence to ART than their counterparts. This finding was congruent with a study finding conducted in Addis Ababa [105]. Patients may be uncomfortable while taking ART pills in front of others due to fear of stigma from disclosing their HIV status to the family, colleagues, and the community. This could lead to non-adherence to ART [106].
Strength and Limitation of the Study
This review is the first study to combine the results of multiple studies conducted in Ethiopia, providing stronger evidence on non-adherence to ART and the factors predicting it. The study also included many study participants (n = 36,317) exceeding the sample sizes of the primary studies included. While all the studies are of good quality, it should be noted that the majority of the studies analyzed were cross-sectional. Moreover, the study couldn’t perform a sub-group analysis depending on the study setting and design.
Conclusions
The overall pooled prevalence of non-adherence to ART was considerably high in Ethiopia. The review has revealed that primary school and lower, taking co-medications, not using memory aids, depression, comorbidity, under-nutrition, not believing on ART controls HIV, lacking access to health facilities and taking ART pills uncomfortably while others looking were independent predictors of non-adherence to ART in Ethiopia. Therefore, healthcare providers, adherence counselors and supporters should detect non-adherence behaviors and patients’ difficulties with ART early, and provide intensive counseling and manage the difficulties appropriately to promote adherence and improve the treatment outcome.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Abbreviations
- AIDS
Acquired Immunodeficiency Syndrome
- AOR
Adjusted Odds Ratio
- ART
Anti-Retroviral Therapy
- ARV
Anti-Retro Viral
- BMI
Body Mass Index
- CD4
Cluster of Differentiation 4
- CI
Confidence Interval
- EDHS
Ethiopian Demographic and Health Survey
- HIV
Human Immunodeficiency Virus
- JBI
Joanna Briggs Institute
- OR
Odds Ratio
- PLWH
People Living With HIV
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- USA
United States of America
- WHO
World Health Organization
Author’ Contributions
TM has generated the idea of this review, and SD, BM, SZ, WN and AS contributed to data collection and statistical analysis. TM wrote the first draft of this manuscript. AK, BB, GK, GN, HA, YT, SA and DK also revised the manuscript. All authors took their responsibility for the accuracy of the analysis and the contents of the review. Finally, all authors read and approved the final version of the manuscript.
Funding
Not applicable.
Data Availability
All necessary data and supplementary materials were included in the manuscript.
Declarations
Ethics Approval and Consent to Participate
Not applicable because no primary data were collected.
Consent for Publication
Not applicable.
Competing Interests
All authors have declared no conflicts of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Tsega BSB, Shewamene Z. Determinants of non-adherence to antiretroviral therapy in adult hospitalized patients, Northwest Ethiopia. Patient Prefer Adherence. 2015;9:373–80. doi: 10.2147/PPA.S75876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chaka TE, Abeya SG, Adlo AM, Abebe TW, Hamuse SD, Lencha MT. Antiretroviral therapy: level of adherence and its determinants among patients on treatment in different health facilities. A Cross Sectional Study in Oromia Regional State, Ethiopia. J AIDS Clin Res. 2016;7(11):1–7. doi: 10.4172/2155-6113.1000629. [DOI] [Google Scholar]
- 3.Abera A, Fenti B, Tesfaye T, Balcha F. Factors influencing adherence to antiretroviral therapy among people living with HIV/AIDS at ART Clinic in Jimma University teaching hospital, Southwest Ethiopia. J Pharma Reports. 2015;1(101):2. [Google Scholar]
- 4.Alemu K, Likisa J, Alebachew M, Temesgen G, Tesfaye G, Dinsa H. Adherence to highly active antiretroviral therapy and predictors of non-adherence among pediatrics attending Ambo Hospital ART Clinic, West Ethiopia. J HIV AIDS Infect Dis. 2014;2:1–7. [Google Scholar]
- 5.Angelo AT, Alemayehu DS. Adherence and its associated factors among adult HIV-infected patients on antiretroviral therapy in South Western Ethiopia, 2020. Patient preference and adherence. Feb. 2021;12:299–308. doi: 10.2147/PPA.S298594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Aychiluhm SB, Tadesse AW, Urmale Mare K, Melaku MS, Ibrahim IM, Ahmed O, Ebrahim OA, Wagris M, Menber Y, Kassa AM. Level of non-adherence and its associated factors among adults on first-line antiretroviral therapy in Amhara Regional State, Ethiopia. PLoS ONE. 2021;16(8):e0255912. doi: 10.1371/journal.pone.0255912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Buh A, Deonandan R, Gomes J, Krentel A, Oladimeji O, Yaya S. Prevalence and factors associated with HIV treatment non-adherence among people living with HIV in three regions of Cameroon: a cross-sectional study. PLoS ONE. 2023;18(4):e0283991. doi: 10.1371/journal.pone.0283991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Demessie R, Mekonnen A, Amogne W, Shibeshi W. Knowledge and adherence to antiretroviral therapy among adult people living with HIV/AIDS at Tikur Anbessa Specialized Hospital, Ethiopia. Int J Basic Clin Pharmacol. 2014;3(2):320–0. [Google Scholar]
- 9.Dibaba D, Kajela G, Chego M, Ermeko T, Zenbaba D, Hailu S, Kasim J, Abdulkadir A. Antiretroviral treatment adherence level and associated factors among adult HIV-positive patients on both HIV/AIDS care models: comparative study in selected hospitals of Western Ethiopia, 2019. HIV/AIDS-Research and Palliative Care. 2021 Dec 15:1067–78. [DOI] [PMC free article] [PubMed]
- 10.Reta H. Adherence to Antiretroviral Therapy and Associated Factors among Adult People Living With Hiv/Aids: The Case of Yergalem Health Center, Southern, Ethiopia (Doctoral Dissertation, St. Mary’s University).
- 11.HIV/AIDS JUNPo, Global HIV. & AIDS statistics-2020 fact sheet. Online. http://www.unaids.org/en/resources/fact-sheet. 2020.
- 12.Towers GJ, Zuliani-Alvarez L. pandemic HIV. 2020.
- 13.Velloza J, Kemp CG, Aunon FM, Ramaiya MK, Creegan E, Simoni JM. Alcohol use and antiretroviral therapy non-adherence among adults living with HIV/AIDS in sub-saharan Africa: a systematic review and meta-analysis. AIDS Behav. 2020;24:1727–42. doi: 10.1007/s10461-019-02716-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nwokorie IC, Ezeama MC, Nwanjo HU. Adherence to highly active antiretrovial therapy among patients receiving treatment in Imo State University Teaching, Hospital, Orlu, Nigeria. World Sci News. 2021;161:90–110. [Google Scholar]
- 15.Csace I. Ethiopia demographic and health survey 2016. Addis Ababa, Ethiopia, and Rockville. Maryland, USA: CSA and ICF; 2016. p. 2016. [Google Scholar]
- 16.Fullman N, Barber RM, Abajobir AA, Abate KH, Abbafati C, Abbas KM, Abd-Allah F, Abdulkader RS, Abdulle AM, Abera SF, Aboyans V. Measuring progress and projecting attainment on the basis of past trends of the health-related Sustainable Development Goals in 188 countries: an analysis from the global burden of Disease Study 2016. The Lancet. 2017;390(10100):1423–59. doi: 10.1016/S0140-6736(17)32336-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Azagew AW, Mekonnen CK, Ferede AJ, Yazew KG, Tezera ZB. Adherence to highly active antiretroviral therapy and its Association with Serostatus Disclosure among people living with HIV in Ethiopia: A Systematic Review and Meta-Analysis.
- 18.Demas Z, Gebremariam A, Kebede A, Ayele L. Adherence to Antiretroviral Treatment and Associated factors among Seropositive People Received Treatment in Jimma Town Public Health Facilities, Ethiopia. J Int Association Providers AIDS Care. 2022;21:23259582221121096. doi: 10.1177/23259582221121096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Molla AA, Gelagay AA, Mekonnen HS, Teshome DF. Adherence to antiretroviral therapy and associated factors among HIV positive adults attending care and treatment in University of Gondar Referral Hospital, Northwest Ethiopia. BMC Infect Dis. 2018;18(1):1–8. doi: 10.1186/s12879-018-3176-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Babo YD, Alemie GA, Fentaye FW. Predictors of first-line antiretroviral therapy failure amongst HIV-infected adult clients at Woldia Hospital, Northeast Ethiopia. PLoS ONE. 2017;12(11):e0187694. doi: 10.1371/journal.pone.0187694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.World Health Organization. Consolidated guidelines on the use of antiretroviral Drugs for treating and preventing HIV Infection: recommendations for a public health approach. World Health Organization; 2016. [PubMed]
- 22.Palmisano L, Vella S. A brief history of antiretroviral therapy of HIV Infection: success and challenges. Ann Ist Super Sanita. 2011;47(1):44–8. doi: 10.4415/ANN_11_01_10. [DOI] [PubMed] [Google Scholar]
- 23.World Health Organization. The use of antiretroviral therapy. WHO Regional Office for South-East Asia; 2002.
- 24.World Health Organization. Antiretroviral therapy for HIV Infection in adults and adolescents: recommendations for a public health approach-2010 revision. World Health Organization; 2010. [PubMed]
- 25.HIV/AIDS JUNPo. Fast-track: ending the AIDS epidemic by 2030. Geneva: Joint United Nations Programme on HIV. AIDS. 2014:1–36.
- 26.HIV/AIDS, JUNPo, Organization WH. 2008 report on the global AIDS epidemic: World Health Organization; 2008.
- 27.Ejigu M, Desalegn Z, Mulatu B, Mosisa G. Adherence to combined antiretroviral therapy and associated factors among people living with HIV attending Nekemte Specialized Hospital, Oromia, Ethiopia: a cross-sectional study. HIV/AIDS (Auckland NZ) 2020;12:97. doi: 10.2147/HIV.S239995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Janelle J, Orrick J, Sherman EM. ARV Therapy in Adults & Adolescents. 2020.
- 29.Mitiku H, Abdosh T, Teklemariam Z. Factors affecting adherence to antiretroviral treatment in harari national regional state, eastern Ethiopia. Isrn Aids. 2013;2013:960954. doi: 10.1155/2013/960954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Steel G, Nwokike J, Joshi M. Development of a multi-method tool to measure ART adherence in resource-constrained settings: the South Africa experience. RPM Plus. 2007;6.
- 31.Fuge TG, Tsourtos G, Miller ER. Factors affecting optimal adherence to antiretroviral therapy and viral suppression amongst HIV-infected prisoners in South Ethiopia: a comparative cross-sectional study. AIDS Res Therapy. 2022;19(1):1–4. doi: 10.1186/s12981-022-00429-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kato M, Granich R, Bui DD, Tran HV, Nadol P, Jacka D, Sabin K, Suthar AB, Mesquita F, Lo YR, Williams B. The potential impact of expanding antiretroviral therapy and combination prevention in Vietnam: towards elimination of HIV transmission. Journal of acquired immune deficiency syndromes (1999). 2013;63(5):e142. [DOI] [PMC free article] [PubMed]
- 33.Tanser F, Barnighausen T, Grapsa E, Zaidi J, Newell ML. High coverage of ART associated with decline in risk of HIV acquisition in rural KwaZulu-Natal, South Africa. Science. 2013;339(6122):966–71. doi: 10.1126/science.1228160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Billoro B, Mamo G, Jarso H. Adherence to antiretroviral therapy and associated factors among HIV infected patients in Nigist Eleni Mohammed Memorial General Hospital, Hossana, Southern Ethiopia. J AIDS Clin Res. 2018;9(774):2. [Google Scholar]
- 35.Bitew BD, Berehane Y, Getahun EA, Abyu DM. Determinants of none-adherence to antiretroviral therapy among HIV-infected adults in Arba Minch General Hospital, Gamo Gofa Zone, Southern Ethiopia: a case control study. Am J Health Res. 2014;2(2):234–40. doi: 10.11648/j.ajhr.20140205.13. [DOI] [Google Scholar]
- 36.Kioko MT, Pertet AM. Factors contributing to antiretroviral drug adherence among adults living with HIV or AIDS in a Kenyan rural community. Afr J Prim Health Care Family Med. 2017;9(1):1–7. doi: 10.4102/phcfm.v9i1.1343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Conway C. The role of adherence to antiretroviral therapy in the management of HIV Infection. JAIDS J Acquir Immune Defic Syndr. 2007;45:14–8. doi: 10.1097/QAI.0b013e3180600766. [DOI] [PubMed] [Google Scholar]
- 38.Gulick RM. Antiretroviral treatment 2010: progress and controversies. Journal of acquired immune deficiency syndromes (1999). 2010;55(Suppl 1):S43. [DOI] [PMC free article] [PubMed]
- 39.World Health Organization. Progress on global access to HIV antiretroviral therapy: a report on 3 by 5 and beyond, March 2006.
- 40.Mbuagbaw L, Thabane L, Ongolo-Zogo P, Yondo D, Noorduyn S, Smieja M, Dolovich L. Trends and determining factors associated with adherence to antiretroviral therapy (ART) in Cameroon: a systematic review and analysis of the CAMPS trial. AIDS Res Therapy. 2012;9:1–0. doi: 10.1186/1742-6405-9-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wakibi SN, Ng’ang’a ZW, Mbugua GG. Factors associated with non-adherence to highly active antiretroviral therapy in Nairobi, Kenya. AIDS Res Therapy. 2011;8(1):1–8. doi: 10.1186/1742-6405-8-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Batuka J, Yakobsen I. Meeting Targets and Maintaining Epidemic Control (EPIC) Project. Decentralized distribution of antiretroviral therapy through the private sector: a strategic guide for scale up. 2019.
- 43.Hussen Hebo STGK, Abiso Erango M. Factors affecting levels of antiretroviral drug adherence among adult patient living with HIV in Public Health Facilities of Arba Minch Town, Southern Ethiopia: using cumulative Logit Model. J Adv Med Med Res. 2019:1–9.
- 44.Assefa N. Factors Influencing Adherence to Antiretroviral Therapy (ART) Among Adult People Living With HIV/AIDS In Saris, Kality and Akaki Health Centers, Addis Ababa, Ethiopia (Doctoral Dissertation, St. Mary’s University).
- 45.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int J Surg. 2021;88:105906. doi: 10.1016/j.ijsu.2021.105906. [DOI] [PubMed] [Google Scholar]
- 46.DerSimonian R, Kacker R. Random-effects model for meta-analysis of clinical trials: an update. Contemp Clin Trials. 2007;28(2):105–14. doi: 10.1016/j.cct.2006.04.004. [DOI] [PubMed] [Google Scholar]
- 47.Peters JL, Sutton AJ, Jones DR, Abrams KR, Rushton L. Comparison of two methods to detect publication bias in meta-analysis. JAMA. 2006;295(6):676–80. doi: 10.1001/jama.295.6.676. [DOI] [PubMed] [Google Scholar]
- 48.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–60. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Borenstein M, Hedges LV, Higgins JP, Rothstein HR. A basic introduction to fixed-effect and random‐effects models for meta‐analysis. Res Synthesis Methods. 2010;1(2):97–111. doi: 10.1002/jrsm.12. [DOI] [PubMed] [Google Scholar]
- 50.Jp H. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:589–624. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 51.Stovold E, Beecher D, Foxlee R, Noel-Storr A. Study flow diagrams in Cochrane systematic review updates: an adapted PRISMA flow diagram. Syst Reviews. 2014;3:1–5. doi: 10.1186/2046-4053-3-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Zeleke AB. Factors That Influence Adherence To Antiretroviral Therapy Among Adults at Nekemte Referral Hospital In Ethiopia (Doctoral dissertation, University of South Africa).
- 53.Alagaw A, Godana W, Taha M, Dejene T. Factors associated with antiretroviral treatment adherence among adult patients in wolaita soddo hospital. J Trop Dis. 2013 Dec 13.
- 54.Beyene KA, Gedif T, Gebre-Mariam T, Engidawork E. Highly active antiretroviral therapy adherence and its determinants in selected hospitals from south and central Ethiopia. Pharmacoepidemiol Drug Saf. 2009;18(11):1007–15. doi: 10.1002/pds.1814. [DOI] [PubMed] [Google Scholar]
- 55.Debito T, Deyno S. Rate and predictors of adherence to antiretroviral therapy among clients on antiretroviral therapy at TEPI health center, south-west Ethiopia. Sci Technol Arts Res J. 2014;3(3):93–8. doi: 10.4314/star.v3i3.15. [DOI] [Google Scholar]
- 56.Demeke B, Chanie T. Adherence to antiretroviral therapy and associated factors among patients living with HIV/AIDS in Dessie Referral Hospital, Northern Ethiopia. Int J Pharm Sci Res. 2014;5(9):572–81. [Google Scholar]
- 57.Ejigu SH, Rike WA, Angamo MT. Medication adherence and associated factors among patients on highly active antiretroviral therapy in Nekemte Hospital, Ethiopia. Gazi Med J. 2014;20(3):199–208. doi: 10.5455/GMJ-30-153681. [DOI] [Google Scholar]
- 58.Gebreagziabher TT, Woldemariam GT. Antiretroviral treatment adherence and determinant factors among adult people infected with human immunodeficiency virus in eastern tigray general hospitals, Northern Ethiopia, 2019. HIV/AIDS-Research and Palliative Care. Sep. 2020;30:497–505. doi: 10.2147/HIV.S273917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Hassen A, Mohammed Y. Antiretroviral therapy adherence level and associated factors among HIV/AIDS patients in jimma zone government health facilities, ART clinics, South-West Ethiopia. Int J Multicultural Multireligious Underst. 2019;5(5):331–41. doi: 10.18415/ijmmu.v5i5.535. [DOI] [Google Scholar]
- 60.Koyra HC. Adherence to antiretroviral therapy among adult persons living with HIV/AIDS in Southern Ethiopia. Int J Virol AIDS. 2018;5(038):10–23937. [Google Scholar]
- 61.Jima F, Tatiparthi R. Prevalence of nonadherence and its associated factors affecting on HIV adults follow-up at antiretroviral therapy clinic in Batu Hospital, Eastern Ethiopia. Indian J Sexually Transmitted Dis AIDS. 2018;39(2):91–7. doi: 10.4103/ijstd.IJSTD_37_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kassahun TB, Zalalem KB. Barriers of adherence to antiretroviral therapy among HIV/AIDS infected persons in Nekemte referral hospital, East Wollega, Oromia Regional State, Western Ethiopia, 2017. J AIDS HIV Res. 2018;10(5):64–76. doi: 10.5897/JAHR2018.0462. [DOI] [Google Scholar]
- 63.Letta S, Demissie A, Oljira L, Dessie Y. Factors associated with adherence to antiretroviral therapy (ART) among adult people living with HIV and attending their clinical care, Eastern Ethiopia. BMC Int Health Hum Rights. 2015;15(1):1–7. doi: 10.1186/s12914-015-0071-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Awel M. Antiretroviral Treatment Adherence and Its Determinants among People Living With HIV/AIDS on Highly Active Antiretroviral Therapy at Two Hospitals in Oromiya Regional State, Ethiopia, 2006 (Doctoral dissertation, Addis Ababa University).
- 65.Markos E, Worku A, Davey G. Adherence to ART in PLWHA and Yirgalem hospital, South Ethiopia. Ethiop J Health Dev. 2008;22(2):174–9. [Google Scholar]
- 66.Mengistie A, Birhane A, Tesfahun E. Assessment of adherence to antiretroviral therapy among adult people living with HIV/AIDS in North East, Ethiopia. BioRxiv. 2018 Dec 10:492330.
- 67.Mitku AA, Alelign T. Factors Associated with adherence to antiretroviral therapy of HIV/AIDS patients in North Shoa Zone Hospitals and Health Centers, Ethiopia. Ng-Journal of Social Development. 2016;5(5):192–204. [Google Scholar]
- 68.Mohammed AY, Ahmed MB, Tefera TB. Assessment of factors affecting art adherence among people living with human immune virus in bale robe hospital, South East Ethiopia. Am J Public Health. 2015;3(2):60–7. [Google Scholar]
- 69.Negash E, Wakgari N, Wasie B, Edris M, Bekele G. Adherence to antiretroviral therapy and its associated factors among HIV positive patients in Nekemte public health institutions, West Ethiopia. HIV & AIDS Review. 2016;15(3):116 – 21.
- 70.Negesa L, Demeke E, Mekonnin W. Adherence to antiretroviral therapy and factors affecting among people living with HIV/AIDS and taking antiretroviral therapy, Dire Dawa Town, Eastern Ethiopia. J Infect Dis Treat. 2017;3(1):5. [Google Scholar]
- 71.Nigusso FT, Mavhandu-Mudzusi AH. Magnitude of non-adherence to antiretroviral therapy and associated factors among adult people living with HIV/AIDS in Benishangul-Gumuz Regional State, Ethiopia. PeerJ. 2020;8:e8558. doi: 10.7717/peerj.8558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Rike M, Loha E, Kassa A. Adherence to antiretroviral treatment among Adult People Living with HIV/AIDS attending highly active antiretroviral therapy at Adare Hospital, Southern Ethiopia. Ethiop J Health Dev. 2021;35(2).
- 73.Tadesse S, Tadesse A, Wubshet M. Adherence to antiretroviral treatment and associated factors among people living with HIV/AIDS in Northwest Ethiopia. J Trop Dis Public Health. 2014 Oct 3.
- 74.Tesfay S, Dingeta T. Level of ART Adherence and Associated Factors During Covid-19 Pandemic Era in Public Hospitals of Jigjiga City Eastern Ethiopia (Doctoral Dissertation, Haramaya University). [DOI] [PMC free article] [PubMed]
- 75.Tessema B, Biadglegne F, Mulu A, Getachew A, Emmrich F, Sack U. Magnitude and determinants of nonadherence and nonreadiness to highly active antiretroviral therapy among people living with HIV/AIDS in Northwest Ethiopia: a cross-sectional study. AIDS Res Therapy. 2010;7(1):1–8. doi: 10.1186/1742-6405-7-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Tiyou A, Belachew T, Alemseged F, Biadgilign S. Predictors of adherence to antiretroviral therapy among people living with HIV/AIDS in resource-limited setting of southwest Ethiopia. AIDS Res Therapy. 2010;7(1):1–0. doi: 10.1186/1742-6405-7-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Yadeta AD, Chaka EE. Predictors of art adherence among people living with human immune virus attending treatment at hospitals in West Shewa Zone, Oromia Region, Ethiopia, 2015. J Health Med Nurs. 2016;29:1–7. [Google Scholar]
- 78.Zewude SB, Ajebe TM. Magnitude of optimal adherence and predictors for a low level of adherence among HIV/AIDS-infected adults in South Gondar Zone, Northwest Ethiopia: a multifacility cross-sectional study. BMJ open. 2022;12(1):e056009. doi: 10.1136/bmjopen-2021-056009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Amberbir A, Woldemichael K, Getachew S, Girma B, Deribe K. Predictors of adherence to antiretroviral therapy among HIV-infected persons: a prospective study in Southwest Ethiopia. BMC Public Health. 2008;8:1–9. doi: 10.1186/1471-2458-8-265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Desta AA, Kidane KM, Woldegebriel AG, Ajemu KF, Berhe AA, Zgita DN, Teweldemedhn LW, Woldegebriel LL, Bezabih NM, Woldearegay TW. Level of adherence and associated factors among HIV-infected patients on antiretroviral therapy in Northern Ethiopia: retrospective analysis. Patient preference and adherence. 2020 Sep 3:1585–94. [DOI] [PMC free article] [PubMed]
- 81.Peters M, Godfrey C, McInerney P, Soares C, Khalil H, Parker D. The Joanna Briggs Institute reviewers’ manual 2015: methodology for JBI scoping reviews. 2015.
- 82.Hoy D, Brooks P, Woolf A, Blyth F, March L, Bain C, Baker P, Smith E, Buchbinder R. Assessing risk of bias in prevalence studies: modification of an existing tool and evidence of interrater agreement. J Clin Epidemiol. 2012;65(9):934–9. doi: 10.1016/j.jclinepi.2011.11.014. [DOI] [PubMed] [Google Scholar]
- 83.Mohammed M, Abeje G, Kebede N, Mohammed T, Ahmed K. Second-line antiretroviral therapy adherence and associated factors among adults living with HIV in Dessie City administration public hospitals. Northeast Ethiopia; 2021.
- 84.Saha R, Saha I, Sarkar AP, Das DK, Misra R, Bhattacharya K, Roy RN, Bhattacharya A. Adherence to highly active antiretroviral therapy in a tertiary care hospital in West Bengal, India. Singapore Med J. 2014;55(2):92. doi: 10.11622/smedj.2014021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Le PM, Nguyen PT, Nguyen HV, Bui DH, Vo SH, Nguyen NV, Nguyen TV, Tran AT, Le AD, Ha NM, Dao AT. Adherence to highly active antiretroviral therapy among people living with HIV and associated high-risk behaviours and clinical characteristics: a cross-sectional survey in Vietnam. Int J STD AIDS. 2021;32(10):911–8. doi: 10.1177/09564624211002405. [DOI] [PubMed] [Google Scholar]
- 86.MOMANYI ZK. Factors associated with the Prevalence of Non Adherence to Antiretroviral Therapy among HIV Positive Patients in Kibra Slums, Nairobi, Kenya (Doctoral dissertation, JKUAT COHES).
- 87.Suryana K, Suharsono H, Antara IG. Factors associated with adherence to anti-retroviral therapy among people living with HIV/AIDS at Wangaya hospital In Denpasar, Bali, Indonesia: a Cross-Sectional Study. HIV/AIDS-Research and Palliative Care. 2019 Nov 19:307 – 12. [DOI] [PMC free article] [PubMed]
- 88.Musenge EM, Kaonga R, Sitali DP, Zimba J. Adherence to antiretroviral therapy among people living with HIV and AIDS in Monze and Nyimba districts of Zambia.
- 89.Mzyece P. Factors that affect adherence to antiretroviral therapy in Kasama district. Int J Multi-Disciplinary Res. 2018.
- 90.Sow¹- PG, Coume M, Ka O, Gaye A, Vinekar V. Determinants of medication adherence among people living with HIV/AIDS in Senegal.
- 91.Mbewe R. Factors Associated with Adherence to Haart of Plwha in Chavuma District, North-Western Province, Zambia (Doctoral Dissertation, Cavendish University).
- 92.Bronia M. Actors That Lead to Non-Adherence to Anti-Retroviral Therapy Among HIV Infected Adults at Chilenje First Level Hospital in Lusaka District (Doctoral Dissertation).
- 93.Sharma B, Joshi K. Treatment adherence of antiretroviral therapy among people living with HIV/AIDS. J Chitwan Med Coll. 2016;6(3):56–61. doi: 10.3126/jcmc.v6i3.16701. [DOI] [Google Scholar]
- 94.Oku AO, Owoaje ET, Ige OK, Oyo-Ita A. Prevalence and determinants of adherence to HAART amongst PLHIV in a tertiary health facility in south Nigeria. BMC Infect Dis. 2013;13:1–9. doi: 10.1186/1471-2334-13-401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Patrick OE, John EA. Adherence of HIV/AIDS patients to antiretroviral therapy in a tertiary health facility in Benin City. Afr J Pharm Pharmacol. 2008;2(7):145–52. [Google Scholar]
- 96.Mukui IN, Ng’ang’a L, Williamson J, Wamicwe JN, Vakil S, Katana A, Kim AA. Rates and predictors of non-adherence to antiretroviral therapy among HIV-positive individuals in Kenya: results from the second Kenya AIDS indicator survey, 2012. PLoS ONE. 2016;11(12):e0167465. doi: 10.1371/journal.pone.0167465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Xuan Tran B, Thanh Nguyen L, Hoang Nguyen N, Van Hoang Q. Determinants of antiretroviral treatment adherence among HIV/AIDS patients: a multisite study. Global Health Action. 2013;6(1):19570. doi: 10.3402/gha.v6i0.19570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Axelsson JM, Hallager S, Barfod TS. Antiretroviral therapy adherence strategies used by patients of a large HIV clinic in Lesotho. J Health Popul Nutr. 2015;33:1–9. doi: 10.1186/s41043-015-0026-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Cantrell RA, Sinkala M, Megazinni K, Lawson-Marriott S, Washington S, Chi BH, Tambatamba-Chapula B, Levy J, Stringer EM, Mulenga L, Stringer JS. A pilot study of food supplementation to improve adherence to antiretroviral therapy among food insecure adults in Lusaka, Zambia. Journal of acquired immune deficiency syndromes (1999). 2008;49(2). [DOI] [PMC free article] [PubMed]
- 100.Daniel M, Mazengia F, Birhanu D. Nutritional status and associated factors among adult HIV/AIDS clients in Felege Hiwot Referral Hospital, Bahir Dar, Ethiopia. Sci J Public Health. 2013;1(1):24–31. doi: 10.11648/j.sjph.20130101.14. [DOI] [Google Scholar]
- 101.Franke M, Murray M, Muñoz M, Hernández-Díaz S, Sebastián J, Atwood S, et al. Food insufficiency is a risk factor for suboptimal antiretroviral therapy adherence among HIV-infected adults in urban Peru. AIDS Behav. 2011;15:1483–9. doi: 10.1007/s10461-010-9789-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Talam N, Gatongi P, Rotich J, Kimaiyo S. Adherence to antiretroviral drug therapy by adult patients attending HIV/AIDS clinic at a Kenyan tertiary helath institution. East Afr Med J. 2009;86(5). [DOI] [PubMed]
- 103.Obirikorang C, Selleh P, Abledu J, Fofie C. Predictors of adherence to antiretroviral therapy among HIV/AIDS patients in the upper west region of Ghana. Isrn Aids. 2013;2013. [DOI] [PMC free article] [PubMed]
- 104.Protopopescu C, Raffi F, Roux P, Reynes J, Dellamonica P, Spire B, et al. Factors associated with non-adherence to long-term highly active antiretroviral therapy: a 10 year follow-up analysis with correction for the bias induced by missing data. J Antimicrob Chemother. 2009;64(3):599–606. doi: 10.1093/jac/dkp232. [DOI] [PubMed] [Google Scholar]
- 105.Abdissa A. Determinant factors affecting adherence to antiretroviral therapy among HIV infected patients in Addis Ababa. University of South Africa; 2013.
- 106.Biressaw S, Abegaz WE, Abebe M, Taye WA, Belay M. Adherence to antiretroviral therapy and associated factors among HIV infected children in Ethiopia: unannounced home-based pill count versus caregivers’ report. BMC Pediatr. 2013;13:1–9. doi: 10.1186/1471-2431-13-132. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All necessary data and supplementary materials were included in the manuscript.