Abstract
Purpose
To examine the relationship between tibial tubercle–trochlear groove (TT-TG) distance and patellar tendon length.
Methods
All healthy athletes who underwent anterior cruciate ligament reconstruction who had a magnetic resonance imaging (MRI) study of the knee on file between July 2018 and June 2019 at a single institution were retrospectively reviewed. Exclusion criteria included patients without an MRI study of the knee on file or with an MRI of insufficient quality precluding reliable calculation of TT-TG and patellar tendon length. MRIs were reviewed to calculate TT-TG, patellar tendon length, and Caton–Deschamps Index (CDI). Patient charts were reviewed to obtain anthropometric characteristics including sex, concomitant injuries, and previous knee procedures as well as age at time of MRI. Spearman correlations were used to assess the relationship between TT-TG, patellar tendon length, and CDI, with regression analysis performed to assess for relationships between TT-TG, patellar tendon length, and patient-specific factors.
Results
Overall, 235 patients (99 female [42.1%], 136 male [57.9%]; mean age: 30.0 years [23.0; 40.0]) were included. Inter-rater reliability between the 2 reviewers was 0.888 for TT-TG, 0.804 for patellar tendon length, and 0.748 for CDI, indicating strong agreement. The correlation between TT-TG and patellar tendon length was 0.021, indicating no true relationship. The correlation between TT-TG and CDI was –0.048 and that of patellar tendon length and CDI was 0.411, indicating a weak positive relationship. Regression analysis found that male sex is strongly correlated with a longer patellar tendon length (odds ratio 2.65, 95% confidence interval 1.33-3.97, P < .001).
Conclusions
In this study, no correlation was found between TT-TG and patellar tendon length or CDI. Male sex was correlated with a longer patellar length.
Level of Evidence
Level III.
The tibial tubercle–trochlear groove (TT-TG) distance is defined as the distance between the center of the trochlear groove and the center of the tibial tubercle as measured on an axial magnetic resonance imaging (MRI) or computed tomography scan. Although the validity and reliability of TT-TG assessment is of some debate due to variation in measurement based on parameters such as knee flexion angle and axial slice orientation, it is a frequently used parameter, and elevated values are an established risk factor for patellar instability.1, 2, 3, 4 In addition, TT-TG distance has been associated with other knee pathologies, including patellofemoral pain syndrome,5 increased osteoarthritis-related structural damage,6 and increased risk of anterior cruciate ligament (ACL) injury.7
Recent reports have suggested that patients undergoing anterior cruciate ligament reconstruction (ACLR) in the presence of elevated TT-TG distances had worse postoperative functional outcome scores compared with those with normal TT-TG distances.8 Furthermore, these suboptimal outcomes are magnified in those patients with elevated TT-TG distances when treated with bone–patellar tendon–bone (BTB) graft, who are reportedly 4 times more likely to have subjective postoperative instability, greater reoperation rates, and more postoperative complications compared with those with normal TT-TG distances.9 These findings could be clinically relevant in ACLR, where the BTB graft is a common autograft used, especially for athletes who participate in contact sports.10
When performing ACLR with BTB graft, it is imperative to estimate the patellar tendon length preoperatively. This helps to preoperatively plan how to set the tibial guide, and if using an allograft, allows the proper tendon length of the BTB allograft to be ordered. However, it is currently unclear what role, if any, TT-TG plays in patellar tendon length. In light of recent associations seen between elevated TT-TG and suboptimal outcomes after ACLR, particularly when using BTB grafts, further understanding of how preoperative TT-TG measurement may be used before ACLR is necessary. Furthermore, by examining the relationship between TT-TG and patellar tendon length, TT-TG may help to optimize surgical planning for ACLR including graft selection (BTB autograft vs allograft or hamstring vs quadriceps), and preparation of alternative fixation devices, such as sutures or bone staples. Therefore, the purpose of this study was to examine the relationship between TT-TG distance and patellar tendon length. The authors hypothesize that greater TT-TG distances will be associated with longer patellar tendon lengths.
Methods
Following institutional review board exemption approval, all skeletally mature patients aged 18 to 50 years who underwent ACLR as identified by Current Procedural Terminology code 29888 between July 2018 and June 2019 and who had either a 1.5-T or 3-T MRI scan on file at a single institution were eligible for analysis. Patients without an MRI scan on file, or whose MRI was of such poor quality that the TT-TG and patellar tendon length could not be reliably calculated were excluded.
Included patients’ MRI scans were reviewed by 2 independent trained research assistants (E.E.J., R.W.P.). All MRIs were either 1.5- or 3-Tesla strength and included both sagittal and axial planes. They were performed in a standard fashion with patients in the supine position, using an 8-channel knee coil with the knee in slight flexion with an average knee flexion angle (KFA) of 20.78°. The scanning protocol included coronal, sagittal, and axial imaging with axial T2 fat-saturated imaging obtained in all cases. Axial images were obtained within the following technical parameter range: fast spin echo, repetition time of 175 to 8,531 milliseconds, echo time of 14 to 120 milliseconds, field of view of 140 to 180, and slice thickness between 2.5 and 4 mm.
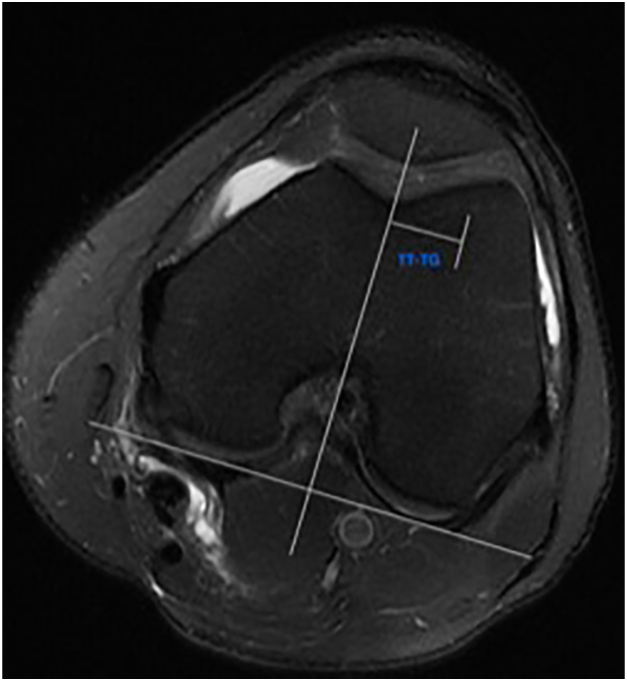
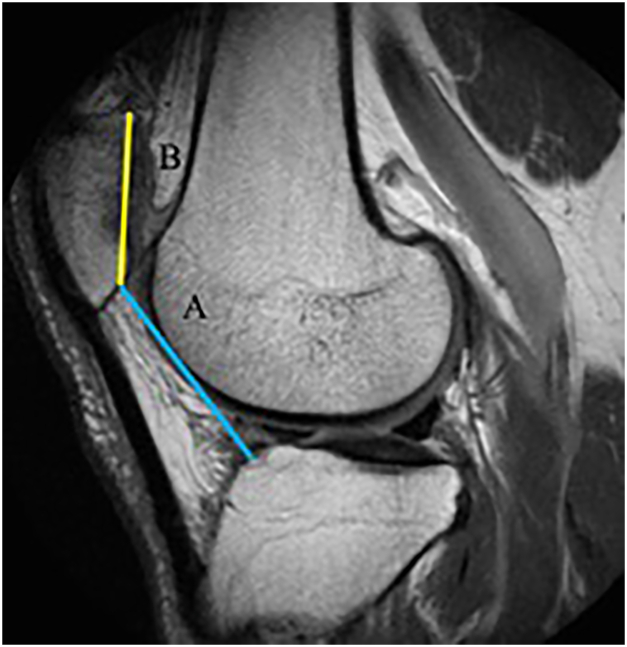
All MRI scans were reviewed to calculate the TT-TG, patellar tendon length, KFA, and Caton–Deschamps Index (CDI) measurements. The TT-TG was measured on axial images where the center of the trochlear groove and tibial tubercle were defined and the distance between the 2 points was calculated (Fig 1).11,12 Patellar tendon length was measured on sagittal images by measuring the inferior border of the patella to the tibial tuberosity insertion of the tendon.13 To measure CDI on MRI, the technique described by Askenberger et al.14 was used. This technique determines CDI by using the sagittal slice showing the greatest length of the patella to determine patellar height (Fig 2). Patient charts were reviewed to obtain anthropometric characteristics including sex, body mass index (BMI), age at MRI, time between injury and MRI, as well as presence of concomitant knee pathology and any previous history of knee injury or surgery in the affected knee.
Fig 1.
Tibial tubercle–trochlear groove (TT-TG) distance measured on MRI (left). TG was measured in the center of the TG at the most proximal axial image with a complete cartilaginous trochlea. TT is indicated by a reference line and was measured at the most distal aspect of the patellar tendon insertion. (MRI, magnetic resonance imaging.)
Fig 2.
CDI measurement from sagittal MRI containing the greatest length of the patella. The CDI equals the distance from the distal aspect of the patellar articular cartilage to the anterosuperior corner of the tibial joint surface (blue line: A), divided by the length of the cartilaginous articular surface (yellow line: B). (CDI, Caton–Deschamps Index; MRI, magnetic resonance imaging.)
KFA Assessment
KFA was measured in accordance with that described by Summers et al.,15 in which the angle was measured where the patella appeared the largest in longitudinal dimension and from there moving to the slice where both the anterior and posterior cortex of the proximal tibia and distal femur were visible. Using our institutional Picture Archiving and Communication Systems, lines were drawn on the proximal anterior cortex of the tibia and distal anterior cortex of the femur, and the angle tool was used to ultimately determine the KFA. Manó et al.16 concluded that a similar means of measurement can determine the radiographic flexion angle within 2 degrees of accuracy compared with the true KFA.
Statistics
Both Shapiro–Wilks and Kolmgrov–Smirnov tests were run to assess normality. Comparisons between groups were calculated by performing t-tests for parametric continuous data and Mann–Whitney U tests for nonparametric continuous data. Parametric continuous data are presented as mean ± standard deviation. Nonparametric continuous data are presented as median [first quartile; third quartile]. Categorical data are presented as n (%), and P values were calculated with either χ2 or Fisher exact tests. Inter-rater reliability was assessed by calculating intraclass correlation coefficients (ICCs) for continuous data. The ICC scores and kappa values were interpreted as follows based on recommendations from Cohen: a score of 0 to 0.20 indicates no to slight reliability, 0.21 to 0.40 as fair reliability, 0.41 to 0.60 indicates moderate reliability, 0.61 to 0.80 indicates substantial reliability, and a score of 0.81 to 1.00 indicates a strong reliability.17 Inter-rater reliability was evaluated for TT-TG, patellar tendon length, and CDI. The relationship between TT-TG, patellar tendon length, and CDI were assessed by calculating Spearman correlations. Multiple linear regression analyses with assessment for multicollinearity were performed in order to assess the relationship between TT-TG and patellar tendon length as the dependent outcome based on patient demographic information. The threshold for significance was set to P < .05. All statistical analyses were done using R Studio (Version 4.1.2; R Foundation for Statistical Computing Vienna, Austria).
Results
Baseline and Demographic Data
Ninety-nine female and 136 male patients met inclusion criteria for analysis at a mean age at MRI of 30.0 years old [23.0, 40.0]. The mean BMI was 26.6 [23.7, 29.9]. Baseline anthropometric and injury-related data for the cohort are shown in Table 1. Radiographic parameters and measurements for the cohort are demonstrated in Table 2.
Table 1.
Baseline Patient Data
| N = 235 | |
|---|---|
| Sex | |
| Female, n (%) | 99 (42.1%) |
| Male | 136 (57.9%) |
| Laterality | |
| Left | 130 (55.3%) |
| Right | 105 (44.7%) |
| Age at MRI, y | 30.0 [23.0; 40.0] |
| BMI | 26.6 [23.7; 29.9] |
| Height, inches | 68.0 [65.0; 70.75] |
NOTE. Results reported as N (Percentage of study cohort); median [first quartile; third quartile].
BMI, body mass index; MRI, magnetic resonance imaging.
Table 2.
Demographic and Radiographic Parameters
| Demographic or Radiographic Parameter | Value |
|---|---|
| Concomitant pathology |
|
| Presence of previous knee injuries or surgery |
|
| Time from injury to MRI, d | 6.5 days |
| Knee flexion angle, ° | 20.78° |
| TT-TG, mm | 11.0 (3.85) |
| Patellar tendon length, mm | 48.0 (5.23) |
| Patella To tibia distance, mm | 32.5 (4.72) |
| Articular cartilage distance, mm | 31.2 (3.18) |
| CDI, mm/mm | 1.03 (0.15) |
NOTE. Results reported as N (standard deviation).
ACLR, anterior cruciate ligament reconstruction; BMI, body mass index; CDI, Caton-Deschamps Index; LCL, lateral collateral ligament; MCL, medial collateral ligament; MRI, magnetic resonance imaging; TT-TG, tibial tubercle–trochlear groove distance.
Inter-rater Reliability
The inter-rater reliability between the 2 reviewers were assessed by calculating intraclass correlation coefficients for TT-TG, patellar tendon length, and CDI index. The TT-TG measurements demonstrated strong agreement (ICC = 0.888), as did the patellar tendon length measurements (ICC = 0.804), and the CDI measurements (ICC = 0.748, Table 3).
Table 3.
ICC Values
| Variable | ICC Value | Agreement |
|---|---|---|
| TT-TG, mm | 0.888 | Strong agreement |
| Patellar tendon length, mm | 0.804 | Strong agreement |
| Patella to tibia distance, mm | 0.895 | Strong agreement |
| Articular cartilage distance, mm | 0.803 | Strong agreement |
| CDI, mm/mm | 0.748 | Strong agreement |
CDI, Caton-Deschamps Index; ICC, intraclass correlation coefficient; TT-TG, tibial tubercle–trochlear groove distance.
Correlation Between TT-TG, Patellar Tendon Length, and Patient-Specific Factors
The correlation between TT-TG and patellar tendon length was 0.021, indicating no true relationship. The correlation between TT-TG and CDI was –0.048, indicating no true relationship. The relationship between patellar tendon length and CDI was 0.411, indicating a weak positive relationship. In addition, there was no true relationship found between age, KFA, time from injury to MRI, or patient height and TT-TG, as demonstrated in Table 4, and there was no significant difference in mean TT-TG distance between female (10.7 mm) and male patients (11.2 mm, P = .232).
Table 4.
Relationship Between TT-TG and Age, KFA, Time From Injury to MRI, and Patient Height
| Variable | Correlation Value | Relationship |
|---|---|---|
| Age | 0.017 | No true relationship |
| KFA | –0.140 | No true relationship |
| Time from injury to MRI | –0.114 | No true relationship |
| Patient height | 0.135 | No true relationship |
KFA, knee flexion angle; MRI, magnetic resonance imaging; TT-TG, tibial tubercle–trochlear groove distance.
Regression Analysis
Regression analysis showed no true relationships with the dependent outcome of TT-TG as represented in Table 5. However, when evaluating patellar tendon length, male sex was a factor associated with increased length (estimate: 2.65; 95% confidence interval 1.33-3.97, P < .001; Table 6).
Table 5.
Regression Analysis in Which TT-TG Is the Dependent Outcome
| Variable | Beta Estimate (95% CI) | P Value |
|---|---|---|
| Age | –0.01 (–0.06 to 0.04) | .665 |
| BMI | 0.06 (–0.04 to 0.16) | .209 |
| Sex: male | 0.56 (–0.45 to 1.57) | .275 |
| Laterality: right | –1.16 (–2.17 to 0.16) | .024 |
BMI, body mass index; CI, confidence interval; TT-TG, tibial tubercle–trochlear groove distance
Table 6.
Regression Analysis in Which Patellar Tendon Length Is the Dependent Outcome
| Variable | Beta Estimate (95% CI) | P Value |
|---|---|---|
| Age | –0.07 (–0.14 to 0.002) | .056 |
| BMI | –0.06 (–0.19 to 0.07) | .388 |
| Sex: male | 2.65 (1.13-3.97) | <.001 |
| Laterality: right | 0.54 (–0.78 to 1.85) | .424 |
NOTE. P-value in bold represents statistical significance, <.05.
BMI, body mass index; CI, confidence interval.
Discussion
In contrast to the initial study hypothesis, the results of the present study, in which MRI was used to assess TT-TG, patellar tendon length, and CDI in ACL-deficient knees, showed no true relationship between these parameters. Thus, TT-TG does not appear to be a useful preoperative indicator of patellar tendon length and likely does not hold substantial value in preoperatively templating BTB graft sizes, although there remain substantial limitations with assessment of TT-TG, as these values can be heavily influenced by KFA, which can further be affected by factors such as previous surgeries and concomitant pathology. Thus, further work must be performed in order to better standardize knee flexion angles and optimize MRI protocols for assessment of TT-TG.
There is literature to suggest associations between elevated TT-TG distance and risk of primary ACL rupture7,9 as well as persistent instability and greater rate of reoperation, particularly with the use of BTB grafts,9 necessitates a critical evaluation of the potential contributing factors. The potential relationship between patellar tendon length, BTB grafts, and TT-TG distance and specifically how these variables collectively could impact ACL surgery are not clearly defined but certainly must be explored. One such factor could lie within the relationship between TT-TG distance and the true, anatomic length of the patellar tendon (the length of the patellar tendon in situ), which is not a perfectly sagittal structure and therefore is not as easily or accurately measured on a sagittal MRI as might be believed. Based on simple trigonometric rationale, a greater TT-TG distance (adjacent value) should correlate with a longer patellar tendon length (hypotenuse). Such interest in patellar tendon length before ACLR could relate to prevention of graft–tunnel mismatch, which is believed to occur in as many as 26% of ACLR procedures using BTB grafts, resulting in extrusion of the tibial bone plug leading to suboptimal “time-zero” bone-to-bone fixation of the tibial bone plug.18 However, perhaps a simpler explanation for the findings of Paul et al.9 and others could simply stem from the potential role for radiographic technique, concomitant injuries, previous surgery, and other anthropometric variables seen in the ACL-injured patient to impact radiographic TT-TG measurements. Izadpanah et al.19 demonstrated a variation in measured TT-TG of greater than 35% based on knee flexion angles during MRI alone. By controlling for factors such as KFA and concomitant knee pathology in the present study, we sought to identify potential confounders and further explain the findings by Paul et al.9 However, the present study did not implicate any particular patient or injury-specific factors and thus we must remain critical and rigorous in our attempt to gain further understanding of such relationships.
Anthropometric studies have sought to identify morphometric data from MRI in order to establish correlations between patellar tendon length, patient sex, and patient height to better template BTB grafts preoperatively.20 Through an MRI-based study, Brown et al.21 identified a strong correlation between patient height and intra-articular length of the ACL. Interestingly, however, they showed no correlation between patient height or intra-articular length of the ACL and patellar tendon length. This comes in contrast to studies by Goldstein et al.22 and a cadaveric study by Denti et al.23 in which there actually was a correlation between patient height and patellar tendon length. Finally, Navali et al.24 determined that patellar tendon length is an exception in human anthropometry, noting no strong correlation between patient height and patellar tendon length. Thus, the ability to reliably identify patients at risk for graft–tunnel mismatch using MRI could offer some value to ACL surgeons, although the most useful parameters are not yet clearly defined.
Despite its importance in patellofemoral kinematics, TT-TG is highly variable among patients and often has little association with patient size, sex, or other demographic factors. When assessing TT-TG and its potential relationship to patient height, Dornacher et al.25 determined that there was very poor correlation between TT-TG and patient height and concluded that TT-TG is an individualized, patient-specific parameter. Interestingly, our study did find that male sex has weak correlation with TT-TG and a strong positive correlation with patellar tendon length. This contrasts to the findings of Campbell et al.,26 in which their MRI-based study demonstrated that female patients were found to have significantly longer patellar tendon lengths than male patients. However, Goldstein et al.22 reported that patient height had a strong correlation with patellar tendon lengths, but male sex was instead associated with longer patellar tendon length. The results of the present study are consistent with the findings of Goldstein et al.,22 in which patient sex could be considered for preoperative estimation of a patient’s patellar tendon length; however, further study is needed in order to validate this recommendation.
Limitations
This study has limitations. The validity of the present study relies on whether or not the TT-TG can accurately and reproducibly be calculated. There are many reports describing 30° as optimal KFA for determination of TT-TG measurements due to the effect of knee flexion on tibial external rotation.19,27,28 Furthermore, Suomalainen et al.29 suggested that TT-TG decreased by 0.29 mm every degree of knee flexion, which would suggest that our mean KFA of 20° may overestimate TT-TG by approximately 2.9 mm. However, this study drew conclusions based on measurements in only 13 adolescent patients. In our study, we performed TT-TG measurements in accordance with the commonly used strategy described by Schoettle et al.30 and believe that our mean KFA of 20° is within the “slight knee flexion” recommended by Izadpanah et al.19 and is appropriate, given potential for patellar instability due to elevated TT-TG occurring between 20 and 30° of knee flexion. Furthermore, formal regression analysis demonstrated no true relationship between KFA and TT-TG in this much larger cohort than that analyzed by Suomalainen et al.29 Similarly, when accounting for concomitant injuries and/or previous surgeries, an attempt at control of any potential confounding factors was made and did not demonstrate meaningful effect on this study’s findings. Additionally, many consider the intra-articular distance of the ACL, not the patellar tendon length, as the most integral parameter to when attempting to mitigate graft-tunnel mismatch. However, the ACL is an obliquely oriented structure that cannot be easily measured with a single sagittal image31 or requires complex formulas for accurate measurement32; therefore, identifying more easily measured structures such as patellar tendon length and TT-TG would be a more reproducible source of information if a correlation did exist. In addition, accurate preoperative knowledge of patellar tendon length affords the surgeon with valuable information that may indicate the need for longer tibial tunnels, rotation of the graft, or other strategies necessary to circumvent graft-tunnel mismatch. Third, the MRIs reviewed in this study were in ACL-deficient cases. ACL deficiency can be a source of quad atrophy and patellar tracking changes ultimately affecting patellar tendon length24,33; however, these changes are believed to take place over the course of several months, whereas MRIs performed in our patients were performed in the acute setting within a few weeks of injury. Fourth, the data from this study stem from a single center in one geographic region. Although there is substantial heterogeneity in our cohort with respect to sex, race, and BMI, the anthropometric results of this study may not be generalizable to other geographic regions.
Conclusions
In this study, no correlation was found between TT-TG and patellar tendon length or CDI. Male sex was correlated with a longer patellar length.
Disclosure
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests: B.J.E. reports the following conflicts: American Academy of Orthopaedic Surgeons, American Orthopaedic Society for Sports Medicine, and American Shoulder and Elbow Surgeons: board or committee member; Arthrex: paid consultant, research support; DePuy, a Johnson & Johnson Company: research support; Linvatec: research support; PLoS One: editorial or governing board; and Smith & Nephew and Stryker: research support. All other authors (E.E.J., W.L.J., B.K., R.M., R.W.P., M.R.) declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
References
- 1.Arendt E.A., Askenberger M., Agel J., Tompkins M.A. Risk of redislocation after primary patellar dislocation: A clinical prediction model based on magnetic resonance imaging variables. Am J Sports Med. 2018;46:3385–3390. doi: 10.1177/0363546518803936. [DOI] [PubMed] [Google Scholar]
- 2.Christensen T.C., Sanders T.L., Pareek A., Mohan R., Dahm D.L., Krych A.J. Risk factors and time to recurrent ipsilateral and contralateral patellar dislocations. Am J Sports Med. 2017;45:2105–2110. doi: 10.1177/0363546517704178. [DOI] [PubMed] [Google Scholar]
- 3.Dejour H., Walch G., Nove-Josserand L., Guier Ch. Factors of patellar instability: An anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc. 1994;2:19–26. doi: 10.1007/BF01552649. [DOI] [PubMed] [Google Scholar]
- 4.Frings J., Balcarek P., Tscholl P., Liebensteiner M., Dirisamer F., Koenen P. Conservative versus surgical treatment for primary patellar dislocation. Dtsch Arztebl Int. 2020;117:279–286. doi: 10.3238/arztebl.2020.0279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tahmasebi M.N., Aghaghazvini L., Mirkarimi S.S., Zehtab M.J., Sheidaie Z., Sharafatvaziri A. The influence of tibial tuberosity–trochlear groove distance on development of patellofemoral pain syndrome. Arch Bone Jt Surg. 2019;7:46–51. [PMC free article] [PubMed] [Google Scholar]
- 6.Haj-Mirzaian A., Guermazi A., Hakky M., et al. Tibial tuberosity to trochlear groove distance and its association with patellofemoral osteoarthritis-related structural damage worsening: Data from the osteoarthritis initiative. Eur Radiol. 2018;28:4669–4680. doi: 10.1007/s00330-018-5460-9. [DOI] [PubMed] [Google Scholar]
- 7.Saper M.G., Popovich J.M., Fajardo R., Hess S., Pascotto J.L., Shingles M. The relationship between tibial tubercle–trochlear groove distance and noncontact anterior cruciate ligament injuries in adolescents and young adults. Arthroscopy. 2016;32:63–68. doi: 10.1016/j.arthro.2015.06.036. [DOI] [PubMed] [Google Scholar]
- 8.Shen X., Xiao J., Yang Y., et al. Multivariable analysis of anatomic risk factors for anterior cruciate ligament injury in active individuals. Arch Orthop Trauma Surg. 2019;139:1277–1285. doi: 10.1007/s00402-019-03210-x. [DOI] [PubMed] [Google Scholar]
- 9.Paul R.W., Johnson E.E., Hall A., et al. Comparison of post-operative outcomes following anterior cruciate ligament reconstruction between patients with vs. without elevated tibial tubercle–trochlear groove (TT–TG) distance. Knee Surg Sports Traumatol Arthrosc. 2023;31:2446–2453. doi: 10.1007/s00167-022-07191-0. [DOI] [PubMed] [Google Scholar]
- 10.Erickson B.J., Harris J.D., Fillingham Y.A., et al. Anterior cruciate ligament reconstruction practice patterns by NFL and NCAA football team physicians. Arthroscopy. 2014;30:731–738. doi: 10.1016/j.arthro.2014.02.034. [DOI] [PubMed] [Google Scholar]
- 11.Brady J.M., Rosencrans A.S., Shubin Stein B.E. Use of TT-PCL versus TT-TG. Curr Rev Musculoskelet Med. 2018;11:261–265. doi: 10.1007/s12178-018-9481-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Erickson B.J., Nguyen J., Gasik K., Gruber S., Brady J., Shubin Stein B.E. Isolated medial patellofemoral ligament reconstruction for patellar instability regardless of tibial tubercle–trochlear groove distance and patellar height: Outcomes at 1 and 2 years. Am J Sports Med. 2019;47:1331–1337. doi: 10.1177/0363546519835800. [DOI] [PubMed] [Google Scholar]
- 13.Chang C.B., Seong S.C., Kim T.K. Preoperative magnetic resonance assessment of patellar tendon dimensions for graft selection in anterior cruciate ligament reconstruction. Am J Sports Med. 2009;37:376–382. doi: 10.1177/0363546508324971. [DOI] [PubMed] [Google Scholar]
- 14.Askenberger M., Bengtsson Moström E., Ekström W., et al. Operative repair of medial patellofemoral ligament injury versus knee brace in children with an acute first-time traumatic patellar dislocation: A randomized controlled trial. Am J Sports Med. 2018;46:2328–2340. doi: 10.1177/0363546518770616. [DOI] [PubMed] [Google Scholar]
- 15.Summers H.K.C., Picken S., Al-Dadah O. Inter- and intra-rater reliability of knee flexion angle measurements on X-ray and MRI. Ann Joint. 2022;7 doi: 10.21037/aoj-22-2. 34-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Manó S., Pálinkás J., Kiss L., Csernátony Z. The influence of lateral knee X-ray positioning on the accuracy of full extension level measurements: An in vitro study. Eur J Orthop Surg Traumatol. 2012;22:245–250. [Google Scholar]
- 17.McHugh M.L. Interrater reliability: The kappa statistic. Biochem Med (Zagreb) 2012;22:276–282. [PMC free article] [PubMed] [Google Scholar]
- 18.Shaffer B., Gow W., Tibone J.E. Graft-tunnel mismatch in endoscopic anterior cruciate ligament reconstruction: A new technique of intraarticular measurement and modified graft harvesting. Arthroscopy. 1993;9:633–646. doi: 10.1016/s0749-8063(05)80499-2. [DOI] [PubMed] [Google Scholar]
- 19.Izadpanah K., Weitzel E., Vicari M., et al. Influence of knee flexion angle and weight bearing on the tibial tuberosity–trochlear groove (TTTG) distance for evaluation of patellofemoral alignment. Knee Surg Sports Traumatol Arthrosc. 2014;22:2655–2661. doi: 10.1007/s00167-013-2537-5. [DOI] [PubMed] [Google Scholar]
- 20.Janani G., Lakshmi S., Prakash A., et al. Preoperative templating of bone–patellar tendon–bone graft for anterior cruciate ligament reconstruction: A morphometry-based graft harvest method. Clin Orthop Surg. 2022;14 doi: 10.4055/cios21167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Brown J.A., Brophy R.H., Franco J., et al. Avoiding allograft length mismatch during anterior cruciate ligament reconstruction: patient height as an indicator of appropriate graft length. Am J Sports Med. 2007;35:986–989. doi: 10.1177/0363546506298584. [DOI] [PubMed] [Google Scholar]
- 22.Goldstein J.L., Verma N., McNickle A.G., Zelazny A., Ghodadra N., Bach B.R. Avoiding mismatch in allograft anterior cruciate ligament reconstruction: Correlation between patient height and patellar tendon length. Arthroscopy. 2010;26:643–650. doi: 10.1016/j.arthro.2009.09.012. [DOI] [PubMed] [Google Scholar]
- 23.Denti M., Bigoni M., Randelli P., et al. Graft–tunnel mismatch in endoscopic anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 1998;6:165–168. doi: 10.1007/s001670050093. [DOI] [PubMed] [Google Scholar]
- 24.Navali A.M., Jafarabadi M.A. Is there any correlation between patient height and patellar tendon length? Arch Bone Jt Surg. 2015;3:99–103. [PMC free article] [PubMed] [Google Scholar]
- 25.Dornacher D., Reichel H., Kappe T. Does tibial tuberosity–trochlear groove distance (TT–TG) correlate with knee size or body height? Knee Surg Sports Traumatol Arthrosc. 2016;24:2861–2867. doi: 10.1007/s00167-015-3526-7. [DOI] [PubMed] [Google Scholar]
- 26.Campbell A.L., Caldwell J.M.E., Yalamanchili D., et al. Effect of patient height and sex on the patellar tendon and anterior cruciate ligament. Orthop J Sports Med. 2021;9 doi: 10.1177/23259671211003244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zilber S., Goutallier D. Preoperative planning of tibial tubercle medialisation according to the trochlear groove angle. Orthop Traumatol Surg Res. 2019;10:129–131. doi: 10.1016/j.otsr.2018.09.020. [DOI] [PubMed] [Google Scholar]
- 28.Krishnan H., Eldridge J.D., Clark D., Metcalfe A.J., Stevens J.M., Mandalia V. Tibial tuberosity-trochlear groove distance: Does it measure up? Bone Joint Open. 2022;3:268–274. doi: 10.1302/2633-1462.33.BJO-2021-0107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Suomalainen J.S., Regalado G., Joukainen A., et al. Effects of knee flexion and extension on the tibial tuberosity–trochlear groove (TT–TG) distance in adolescents. J Exp Ortop. 2018;5:31. doi: 10.1186/s40634-018-0149-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Schoettle P.B., Zanetti M., Seifert B., Pfirrmann C.W.A., Fucentese S.F., Romero J. The tibial tuberosity–trochlear groove distance; a comparative study between CT and MRI scanning. Knee. 2006;13:26–31. doi: 10.1016/j.knee.2005.06.003. [DOI] [PubMed] [Google Scholar]
- 31.Van Zyl R., Van Schoor A.N., Du Toit P.J., et al. The association between anterior cruciate ligament length and femoral epicondylar width measured on preoperative magnetic resonance imaging or radiograph. Arthrosc Sports Med Rehabil. 2020;2:e23–e31. doi: 10.1016/j.asmr.2019.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rosso F., Rossi R., Faletti R., Cantivalli A., Blonna D., Bonasia D.E. Transepicondylar distance measured on MRI can predict the length of the graft required for different anterior cruciate ligament reconstruction (ACLR) techniques useful for revision surgery. J Orthop Traumatol. 2022;23:50. doi: 10.1186/s10195-022-00670-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Van de Velde S.K., Gill T.J., DeFrate L.E., Papannagari R., Li G. The effect of anterior cruciate ligament deficiency and reconstruction on the patellofemoral joint. Am J Sports Med. 2008;36:1150–1159. doi: 10.1177/0363546508314404. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.