ABSTRACT
Our study aims to assess the public’s perceptions of respiratory syncytial virus (RSV) and attitudes toward the RSV vaccine and to identify associated factors in China. A nationwide cross-sectional survey conducted using an online platform between August 16 and September 14, 2023. Questions related to socio-demographics, awareness, knowledge, perceptions of susceptibility and severity of RSV, and attitudes toward the RSV vaccine were included in the questionnaire. We used the chi-square test and logistic regression model to explore the associated factors. Overall, 2133 individuals were included in this study. Nearly a quarter of participants (24.3%) indicated that they had never heard of RSV. The proportion of individuals aged over 50 years reporting never having heard of RSV (36.5%) and having a low knowledge level of RSV (55.3%) was significantly higher that of other younger age groups. More than half of individuals (55.7%) exhibited low level of perceptions of susceptibility concerning RSV infection. A total of 68.4% of the participants expressed willingness to receive the RSV vaccine. Younger age was positively associated with a higher willingness to be vaccinated. The most frequent reason for declining the vaccine was “Concern about vaccine’s safety or side effects.” About 60% of individuals considered a price of RSV vaccine below 200 CNY (28 USD) as acceptable. The awareness and perceived susceptibility to RSV infection were limited to the Chinese public. It is necessary to take measures to address the low awareness and knowledge of RSV and acceptability of the RSV vaccine among older adults.
KEYWORDS: Respiratory syncytial virus, perceptions, vaccine, China
Introduction
Respiratory syncytial virus (RSV) is one of the predominant agents of acute lower respiratory infection (ALRI). Individuals infected with RSV typically manifest influenza-like symptoms, such as coughing, runny nose, and sneezing. Infants, young children, and adults aged ≥60 years are at high likelihood of developing severe health problems, such as bronchiolitis, following RSV infection.1,2 No widely adopted specific treatment for RSV is available, and the primary approach for treating ALRI is largely supportive care.3 Currently, the United States has approved two vaccines, Arexvy (GlaxoSmithKline Biologicals, Durham, NC, USA) and AbrysvoTM (Pfizer Inc., New York, NY, USA), formulated for adults aged ≥60 years to prevent RSV. Additionally, the U.S. has authorized two monoclonal antibody (mAb) products, Nirsevimab (AstraZeneca and Sanofi) and Palivizumab (MedImmune), intended for the prevention of RSV in children aged ≤19 months.4 Subsequently, Abrysvo was approved by the U.S. Food and Drug Administration on August 21, 2023, to prevent RSV in infants born to pregnant individuals.5
The burden caused by RSV was severe, and no specific medications existed to treat it; however, the population did not seem to know much about RSV. In South England, 71% of the surveyed pregnant women reported that they had never heard of RSV.6 About 50% of parents of children in France also said they had never heard of RSV.7 Primary healthcare professionals in the United States have paid relatively little attention to the burden of RSV infection in older adults.8 RSV perceptions among the Chinese population remain unclear, posing a challenge in formulating policies aimed at alleviating the health burden associated with the virus. The Chinese National Medical Products Administration has not yet approved the use of preventive products against RSV. Several clinical trials on RSV prevention products are currently underway in China.9 Understanding individuals’ attitudes toward RSV vaccines could provide insights into future RSV-related immunization policy decisions.
Our study was designed to understand the general public’s perceptions of RSV and attitudes toward RSV vaccines. The recommended age for vaccination may change with vaccine accessibility or disease burden, as in the case of the COVID-19 vaccine. A clinical trial of the RSV vaccine was also conducted among healthy adults aged 18–50 years.10 Hence, understanding perceptions about RSV and attitudes toward the RSV vaccine among the general population will serve as overall and valuable inputs for policymakers, enabling them to design robust policies and interventions that closely align with the public’s needs and concerns.
Method
Study design and participants
We performed the nationwide cross-sectional survey using an online questionnaire adminstrated between August 16 and September 14, 2023. The research team generated the questionnaire (simplified Chinese version) through the “Wenjuanxing” platform (https://www.wjx.cn/), and posted and publicized the link to the questionnaire on the social media (WeChat/Weibo) platform. WeChat is a comprehensive, multipurpose messaging, social media, and mobile payment application in China. Weibo is a Chinese microblogging platform, often referred to as “China’s Twitter,” allowing users to share short messages, images, and multimedia. The participants were recruited using convenience sampling.
Prior to questionnaire completion, the participants received information regarding the survey’s purpose and were assured that it did not pose any privacy concerns. The participants were made aware of the voluntary nature of their participation and were free to withdraw from the survey at any point if they experienced discomfort. The questionnaire would only pop up when the participant read the information above and checked the box “agreeing to participate in the survey.” Before submitting the questionnaire, participants reviewed and changed their responses using the back button. We used cookies to prevent participants from accessing the questionnaire more than once. Participants who completed the questionnaire were eligible for compensation for one CNY (0.14 USD, 7.187 CNY = 1 USD). The inclusion criteria for participants were residents of mainland China who aged 18 years or older.
Measures
The questionnaire included a set of general inquiries concerning socio-demographics, comprising age, sex, marital status, education level, occupation, living conditions, annual household income, chronic diseases, self-reported health, and experience of side effects after vaccination. The survey instrument related to perceptions was designed according to the literature.6,11–13 Firstly, we examined the awareness of RSV using one question “Before taking part in this survey, how familiar were you with Respiratory Syncytial Virus (RSV)?” with answers “I have never heard of it,” “I have heard of it, but don’t really know what it is,” “I know some facts about what it is,” and “I have a good understanding about it.”6,11,13 RSV knowledge was tested using seven questions related to the transmission route, symptoms, high-risk susceptible populations, and treatment.12,13 The perceptions of susceptibility and severity of RSV infection were assessed by “How likely do you think you are to get RSV infection?” and “How serious do you think RSV infection is for you?” on a five-point Likert scale.6 We examined attitudes toward the RSV vaccine using the question, “If the RSV vaccine is available in the future, would you be willing to receive it?”. Participants were further asked for reasons for the following: “If you choose ‘Strongly agreement’/‘Agreement,’ why?” and “If you choose ‘Neither agree nor disagree’/‘Disagreement’/‘Strongly disagreement,’ why?”. Finally, we examined which demographic group held the greatest sway over participants’ decisions regarding RSV vaccination and assessed the acceptable price range for the RSV vaccine. Two staff members at the Wuxi Center for Disease Control and Prevention worked on infectious diseases, two researchers specialized in immunization, and one sociologist evaluated the content and face validity of the survey instrument to ensure that the content was coherent, accurate, and understandable. A pilot study (approximately 20 samples) was conducted before the formal distribution. The findings showed that the questions could be successfully understood, and it took approximately two to three minutes to complete the questionnaire.
Statistical analysis
The response rate was calculated as follows: the number of individuals completing the questionnaire/number of individuals visiting the website × 100%. Descriptive statistics were employed for data presentation. To facilitate statistical analysis, responses to the five-point Likert scales were binary coded with reference to previous literature.6,14,15 The answers toward awareness were dichotomously coded where an “I have never heard of it” was categorized as “Never heard,” while other responses were categorized as “Yes.” Each correctly answered knowledge question was assigned one point, whereas an incorrectly answered question received zero points. The total score for the seven questions was computed, and respondents were categorized into one “Knowledge level” variable based on the median score, with scores greater than or equal to the median classified as “High level” and those below as “Low level.” Awareness and knowledge of RSV by socio-demographic characteristics were was compared using a chi-squared test.
In relation to responses concerning perceptions of susceptibility, responses of “Extremely unlikely,” “Unlikely,” and “Neutral/not sure” were aggregated into the category “Low perception,” while “Likely” and “Extremely likely” were grouped into “High perception.” In terms of responses regarding perceptions of severity, answers, such as “Not at all,” “Slightly,” and “Somewhat,” were amalgamated into the “Low perception” group, while “Moderately” and “Extremely” were consolidated under “High perception.” The responses to attitudes toward the RSV vaccine were binary coded such that a “Strongly agreement” or “Agreement” was coded as “Yes,” while other responses were coded as “No.” We used the univariate and multivariate logistic regression model to explore the factors associated with perceptions of susceptibility and severity of RSV infection (“Low perception” as reference) and willingness to vaccinate against RSV (“No” as reference). The crude and adjusted odds ratio (OR) and 95% confidence interval (CI) were calculated. We included significant variables in the univariate analysis into the multivariate analysis. The responses marked as “unclear” for variables, including having chronic diseases and experiencing side effects due to vaccination, were excluded from the logistic regression analysis. We also explored the reasons toward the willingness and refusal to receive the RSV vaccine at different levels of awareness, knowledge, and perceptions of the susceptibility and severity of RSV infection. All analyses were performed using the R software. A two-sided p value of < .05 was considered statistically significant. We provided the Checklist for Reporting Results of Internet E-Surveys (CHERRIES) in the Appendix.16
Ethics
The study was approved by the Ethics Committee of the Wuxi Centre for Disease Control and Prevention (2022No7).
Results
A total of 2359 questionnaires were collected, of which 226 were incomplete. All the completed questionnaires were included in the analysis. Overall, 2133 individuals were included in the study (Table 1), with a response rate of 63.5% (2133/3359). The participants were located in all 31 provincial-level administrative divisions of Mainland China (Table A1). The majority of the participants (42.7%) fell within the age range of 18 to 30 years and 53.3% were female. A substantial majority, specifically 73.3%, had college or equivalent educational qualifications. Among the participants, 24.3% indicated that they had never heard of RSV. It was found that 36.5% of individuals aged >50 years reported never having heard of RSV, which was significantly higher than that in other age groups (Table A2). About half of the respondents (44.3%) believed that they were at risk of contracting RSV, and 59.8% perceived RSV infection to be somewhat serious. A total of 68.4% of the participants expressed willingness to receive the RSV vaccine when available.
Table 1.
Characteristics of participants.
| Characteristics | No. (%)(N = 2133) |
|---|---|
| Age group, years | |
| 18–≤30 | 911 (42.7) |
| 31–≤40 | 817 (38.3) |
| 41–≤50 | 290 (13.6) |
| >50 | 115 (5.4) |
| Sex | |
| Male | 996 (46.7) |
| Female | 1137 (53.3) |
| Marital status | |
| Unmarried | 1398 (65.5) |
| Married | 698 (32.7) |
| Divorce | 37 (1.7) |
| Education level | |
| Junior high school or below | 125 (5.9) |
| High school graduate or equivalent | 180 (8.4) |
| Undergraduate or equivalent | 1564 (73.3) |
| Postgraduate or above | 264 (12.4) |
| Occupation | |
| Healthcare-related | 732 (34.3) |
| Others | 1401 (65.7) |
| Living with children aged ≤6 years or old adults aged ≥60 years | |
| Yes | 1314 (61.6) |
| No | 819 (38.4) |
| Annual household income | |
| <50,000 CNY | 198 (9.3) |
| 50,000–≤149,999 CNY | 879 (41.2) |
| 150,000–≤299,999 CNY | 746 (35.0) |
| ≥300,000 CNY | 310 (14.5) |
| Having chronic diseases | |
| Yes | 266 (12.5) |
| No | 1780 (83.5) |
| Unclear | 87 (4.1) |
| Self-reported health | |
| Very poor | 27 (1.3) |
| Poor | 80 (3.8) |
| Neutral | 974 (45.7) |
| Well | 811 (38.0) |
| Very well | 241 (11.3) |
| Experiencing side effects following previous vaccination | |
| Yes | 163 (7.6) |
| No | 1859 (87.2) |
| Unclear | 111 (5.2) |
| Awareness of RSV | |
| I have never heard of it | 518 (24.3) |
| I have heard of it, but don’t really know what it is | 856 (40.1) |
| I know some facts about what it is | 689 (32.3) |
| I have a good understanding about RSV | 70 (3.3) |
| Perceptions of susceptibility of RSV infection | |
| Extremely unlikely | 63 (3.0) |
| Unlikely | 186 (8.7) |
| Neutral/not sure | 939 (44.0) |
| Likely | 846 (39.7) |
| Extremely likely | 99 (4.6) |
| Perceptions of severity of RSV infection | |
| Not at all | 51 (2.4) |
| Slightly | 312 (14.6) |
| Somewhat | 1276 (59.8) |
| Moderately | 419 (19.6) |
| Extremely | 75 (3.5) |
| If the RSV vaccine is available in the future, would you be willing to receive it? | |
| Strongly disagreement | 25 (1.2) |
| Disagreement | 107 (5.0) |
| Neither agree nor disagree | 542 (25.4) |
| Agreement | 1119 (52.5) |
| Strongly agreement | 340 (15.9) |
*50,000 CNY was equal to 6957 USD; 150,000 CNY was equal to 20,871 USD; and 300,000 CNY was equal to 41,742 USD.
About a quarter of the participants (22.5%) demonstrated a lack of awareness concerning the modes of transmission associated with RSV (Figure 1). Nearly 30% of the respondents did not know that infants, young children, and the elderly were at high risk of RSV infection. A total of 22.4% of the participants held the belief that specific drugs for the treatment of RSV infections were presently available. The median total score for the knowledge-related questions was 6.00. More than half of adults (55.3%) aged >50 years exhibited low level of knowledge of RSV, which was significantly higher than that in other age groups (Table A3).
Figure 1.
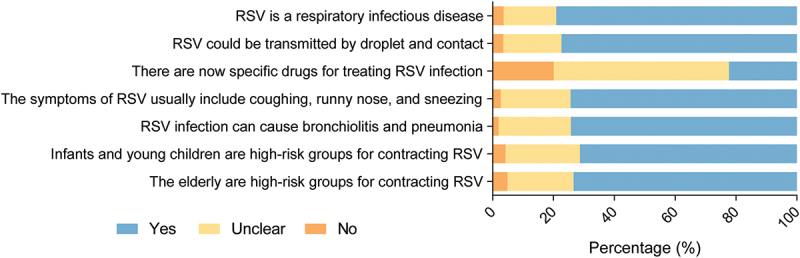
Knowledge of RSV among participants.
Age, education level, occupation, annual household income, awareness of RSV, and knowledge level were significantly associated with perceptions of susceptibility to RSV infection in Table 2. Higher educational attainment displayed a positive association with increased susceptibility perceptions. Compared to participants who had never heard of RSV, those who were aware of RSV were more likely to perceive themselves as susceptible to RSV infection. Participants with a high level of knowledge about RSV demonstrated an increased likelihood of perceiving susceptibility to RSV infection (adjusted OR: 1.572, 95% CI: 1.288–1.919, p < .001).
Table 2.
Factors associated with perceptions of susceptibility of RSV infection.
| Variables | Univariate analysis |
Multivariate analysis |
||
|---|---|---|---|---|
| OR | P value | OR | P value | |
| Age group, years (18–≤30 as reference) | ||||
| 31–≤40 | 1.010 (0.829–1.230) | .921 | 1.015 (0.823–1.251) | .890 |
| 41–≤50 | 0.791 (0.597–1.048) | .102 | 0.844 (0.623–1.143) | .273 |
| >50 | 0.494 (0.316–0.774) | .002 | 0.589 (0.362–0.957) | .033 |
| Sex (Male as reference) | ||||
| Female | 0.918 (0.768–1.097) | .347 | NA | NA |
| Marital status (Unmarried as reference) | ||||
| Married | 1.017 (0.841–1.231) | .860 | NA | NA |
| Divorce | 1.598 (0.788–3.240) | .194 | NA | NA |
| Education level (Junior high school or below as reference) | ||||
| High school graduate or equivalent | 2.358 (1.300–4.276) | .005 | 1.959 (1.063–3.611) | .031 |
| Undergraduate or equivalent | 4.648 (2.809–7.691) | <.001 | 2.974 (1.754–5.044) | <.001 |
| Postgraduate or above | 4.104 (2.361–7.135) | <.001 | 2.328 (1.284–4.220) | .005 |
| Occupation (Others as reference) | ||||
| Healthcare-related | 1.753 (1.454–2.113) | <.001 | 1.306 (1.059–1.610) | .013 |
| Living with children aged ≤6 years or old adults aged ≥60 years (No as reference) | ||||
| Yes | 1.113 (0.927–1.337) | .253 | NA | NA |
| Annual household income (CNY) (<50,000 as reference) | ||||
| 50,000–≤149,999 | 1.788 (1.261–2.536) | .001 | 1.393 (0.959–2.025) | .082 |
| 150,000–≤299,999 | 2.351 (1.652–3.347) | <.001 | 1.681 (1.145–2.467) | .008 |
| ≥300,000 | 1.560 (1.048–2.323) | .029 | 1.194 (0.771–1.848) | .426 |
| Chronic diseases (Yes as reference) | ||||
| No | 1.072 (0.821–1.400) | .610 | NA | NA |
| Self-reported health (Very poor as reference) | ||||
| Poor | 1.684 (0.638–4.444) | .292 | NA | NA |
| Neutral | 1.509 (0.639–3.564) | .348 | NA | NA |
| Well | 1.924 (0.814–4.548) | .136 | NA | NA |
| Very well | 1.296 (0.533–3.150) | .568 | NA | NA |
| Experiencing side effects following previous vaccination (Yes as reference) | ||||
| No | 0.790 (0.571–1.093) | .154 | NA | NA |
| Awareness of RSV (“I have never heard of it” as reference) | ||||
| I have heard of it, but don’t really know what it is | 1.626 (1.272–2.078) | <.001 | 1.377 (1.064–1.783) | .015 |
| I know some facts about what it is | 3.138 (2.437–4.041) | <.001 | 2.184 (1.656–2.881) | <.001 |
| I have a good understanding about RSV | 2.900 (1.727–4.873) | <.001 | 1.947 (1.127–3.366) | .017 |
| Knowledge level (Low level as reference) | ||||
| High level | 2.148 (1.788–2.581) | <.001 | 1.572 (1.288–1.919) | <.001 |
NA: Not applicable; the OR >1 indicated that the presence of the factor was associated with an increased likelihood of the high level of perceptions to susceptibility of RSV infection.
The multivariate analysis results revealed significant correlations between perceptions of the severity of RSV infection with age, occupation, presence of chronic diseases, side effects after vaccination, and awareness of RSV (Table 3). Specifically, older age was negatively associated with a higher perception of severity. Participants who were related to healthcare occupations had a lower likelihood of perceiving the severity of RSV infection than those who were not (adjusted OR: 0.514, 95% CI: 0.398–0.662, p < .001). Furthermore, participants who were aware of RSV, as opposed to those who had never heard of it, demonstrated a greater tendency to perceive the severity of the RSV infection.
Table 3.
Factors associated with perceptions of severity of RSV infection.
| Variables | Univariate analysis |
Multivariate analysis |
||
|---|---|---|---|---|
| OR | P value | OR | P value | |
| Age group, years (18–≤30 as reference) | ||||
| 31–≤40 | 0.664 (0.528–0.835) | <.001 | 0.664 (0.519–0.851) | .001 |
| 41–≤50 | 0.550 (0.389–0.778) | .001 | 0.633 (0.441–0.908) | .013 |
| >50 | 0.505 (0.293–0.869) | .014 | 0.551 (0.311–0.976) | .041 |
| Sex (Male as reference) | ||||
| Female | 0.754 (0.612,0.928) | .008 | 0.829 (0.667–1.031) | .092 |
| Marital status (Unmarried as reference) | ||||
| Married | 1.151 (0.924–1.435) | .209 | NA | NA |
| Divorce | 1.313 (0.601–2.869) | .494 | NA | NA |
| Education level (Junior high school or below as reference) | ||||
| High school graduate or equivalent | 1.234 (0.698–2.179) | .470 | NA | NA |
| Undergraduate or equivalent | 1.177 (0.743–1.864) | .488 | NA | NA |
| Postgraduate or above | 0.701 (0.402–1.222) | .210 | NA | NA |
| Occupation (Others as reference) | ||||
| Healthcare-related | 0.644 (0.513–0.809) | <.001 | 0.514 (0.398–0.662) | <.001 |
| Living with children aged ≤6 years or old adults aged ≥60 years (No as reference) | ||||
| Yes | 1.352 (1.087–1.683) | .007 | 1.237 (0.976–1.566) | .078 |
| Annual household income (CNY) (<50,000 as reference) | ||||
| 50,000–≤149,999 | 1.214 (0.810–1.820) | .348 | 1.127 (0.738–1.721) | .581 |
| 150,000–≤299,999 | 1.556 (1.037–2.333) | .033 | 1.463 (0.955–2.241) | .081 |
| ≥300,000 | 0.924 (0.575–1.487) | .746 | 0.980 (0.596–1.611) | .937 |
| Having chronic diseases (Yes as reference) | ||||
| No | 0.498 (0.376–0.660) | <.001 | 0.449 (0.324–0.622) | <.001 |
| Self-reported health (Very poor as reference) | ||||
| Poor | 0.617 (0.240–1.582) | .315 | 0.625 (0.227–1.719) | .363 |
| Neutral | 0.312 (0.137–0.707) | .005 | 0.440 (0.180–1.076) | .072 |
| Well | 0.393 (0.173–0.892) | .026 | 0.543 (0.219–1.346) | .187 |
| Very well | 0.417 (0.177–0.979) | .045 | 0.534 (0.210–1.362) | .189 |
| Experiencing side effects following previous vaccination (Yes as reference) | ||||
| No | 0.639 (0.450–0.907) | .012 | 0.678 (0.461–0.997) | .048 |
| Awareness of RSV (“I have never heard of it” as reference) | ||||
| I have heard of it, but don’t really know what it is | 2.154 (1.592–2.913) | <.001 | 2.114 (1.540–2.901) | <.001 |
| I know some facts about what it is | 1.911 (1.399–2.611) | <.001 | 2.257 (1.611–3.162) | <.001 |
| I have a good understanding about RSV | 2.365 (1.322–4.232) | .004 | 2.978 (1.571–5.645) | .001 |
| Knowledge level (Low level as reference) | ||||
| fHigh level | 1.147 (0.930–1.415) | .200 | NA | NA |
NA: Not applicable; the OR >1 indicated that the presence of the factor was associated with an increased likelihood of the high level of perceptions of severity of RSV infection.
In the multivariate analysis (Table 4), age, educational level, living conditions, self-reported health, side effects after vaccination, awareness of RSV, and perceptions of susceptibility and severity were associated with willingness toward the RSV vaccination. Adults aged >50 years were more likely to refuse to vaccinate against RSV than those aged 18–30 years. Individuals living with children aged ≤6 years or adults aged ≥60 years were more willing to receive RSV vaccination (adjusted OR: 1.407, 95% CI: 1.118–1.770, p = .004). Participants who did not experience side effects after vaccination previously were more likely to show willingness to vaccinate against RSV (adjusted OR: 2.440, 95% CI: 1.669–3.566, p < .001). High perception of susceptibility (adjusted OR: 2.079, 95% CI: 1.647–2.624, p < .001) and severity (adjusted OR: 4.019, 95% CI: 2.863–5.642, p < .001) of RSV infection were positively associated with willingness to RSV vaccination.
Table 4.
Factors associated with willingness to receive the RSV vaccination.
| Variables | Univariate analysis |
Multivariate analysis |
||
|---|---|---|---|---|
| OR | P value | OR | P value | |
| Age group, years (18–≤30 as reference) | ||||
| 31–≤40 | 0.637 (0.512–0.792) | <.001 | 0.674 (0.501–0.906) | .009 |
| 41–≤50 | 0.571 (0.424–0.769) | <.001 | 0.682 (0.466–0.999) | .049 |
| >50 | 0.518 (0.336–0.800) | .003 | 0.685 (0.408–1.151) | .153 |
| Sex (Male as reference) | ||||
| Female | 0.865 (0.712–1.050) | .143 | NA | NA |
| Marital status (Unmarried as reference) | ||||
| Married | 1.372 (1.109–1.698) | .004 | 1.200 (0.880–1.635) | .249 |
| Divorce | 0.600 (0.296–1.219) | .158 | 0.630 (0.285–1.392) | .253 |
| Education level (Junior high school or below as reference) | ||||
| High school graduate or equivalent | 0.737 (0.432–1.256) | .262 | 0.516 (0.287–0.928) | .027 |
| Undergraduate or equivalent | 0.934 (0.606–1.441) | .758 | 0.494 (0.302–0.806) | .005 |
| Postgraduate or above | 0.514 (0.315–0.837) | .008 | 0.278 (0.160–0.485) | <.001 |
| Occupation (Others as reference) | ||||
| Healthcare-related | 0.919 (0.751–1.124) | .409 | NA | NA |
| Living with children aged ≤6 years or old adults aged ≥60 years (No as reference) | ||||
| Yes | 1.327 (1.089–1.615) | .005 | 1.407 (1.118–1.770) | .004 |
| Annual household income (CNY) (<50,000 as reference) | ||||
| 50,000–≤149,999 | 1.379 (0.971–1.956) | .072 | NA | NA |
| 150,000–≤299,999 | 1.243 (0.873–1.770) | .227 | NA | NA |
| ≥300,000 | 0.786 (0.530–1.165) | .230 | NA | NA |
| Having chronic diseases (Yes as reference) | ||||
| No | 0.998 (0.747–1.333) | .990 | NA | NA |
| Self-reported health (Very poor as reference) | ||||
| Poor | 1.269 (0.499–3.232) | .617 | 1.610 (0.558–4.646) | .379 |
| Neutral | 1.683 (0.745–3.805) | .211 | 2.493 (0.976–6.371) | .056 |
| Well | 2.298 (1.014–5.211) | .046 | 2.859 (1.115–7.329) | .029 |
| Very well | 2.962 (1.253–6.999) | .013 | 3.805 (1.432–10.109) | .007 |
| Experiencing side effects following previous vaccination (Yes as reference) | ||||
| No | 1.903 (1.368–2.646) | <.001 | 2.440 (1.669–3.566) | <.001 |
| Awareness of RSV (“I have never heard of it” as reference) | ||||
| I have heard of it, but don’t really know what it is | 2.161 (1.696–2.754) | <.001 | 1.682 (1.291–2.192) | .001 |
| I know some facts about what it is | 2.747 (2.121–3.558) | <.001 | 1.979 (1.475–2.654) | <.001 |
| I have a good understanding about RSV | 4.304 (2.199–8.423) | <.001 | 2.825 (1.360–5.867) | .005 |
| Knowledge level (Low level as reference) | ||||
| High level | 1.499 (1.235–1.821) | <.001 | 1.205 (0.959–1.512) | .109 |
| Perceptions of susceptibility (Low perception as reference) | ||||
| High perception | 2.680 (2.177–3.300) | <.001 | 2.079 (1.647–2.624) | <.001 |
| Perceptions of severity (Low perception as reference) | ||||
| High perception | 4.940 (3.599–6.781) | <.001 | 4.019 (2.863–5.642) | <.001 |
NA: Not applicable; the OR >1 indicated that the presence of the factor was associated with an increased likelihood of willingness to receive the RSV vaccination.
The most frequently cited reason for accepting the RSV vaccine was “Worried about the risk of RSV infection,” followed by “Protecting the people you are around” as the second most common reason (Figure 2). The most prevalent reason for refusing the RSV vaccine was “Concern about vaccine’s safety or side effects,” with “I want to wait because this is a new vaccine” being the second most cited reason. Among individuals with low awareness, low knowledge, or low perception of susceptibility, the most common reason for willingness remained as “Worried about the risk of RSV infection” (Figures A1–A3). “RSV infection could be quite severe” was the most prevalent reason for willingness among individuals with a high perception of severity (Figure A4).
Figure 2.
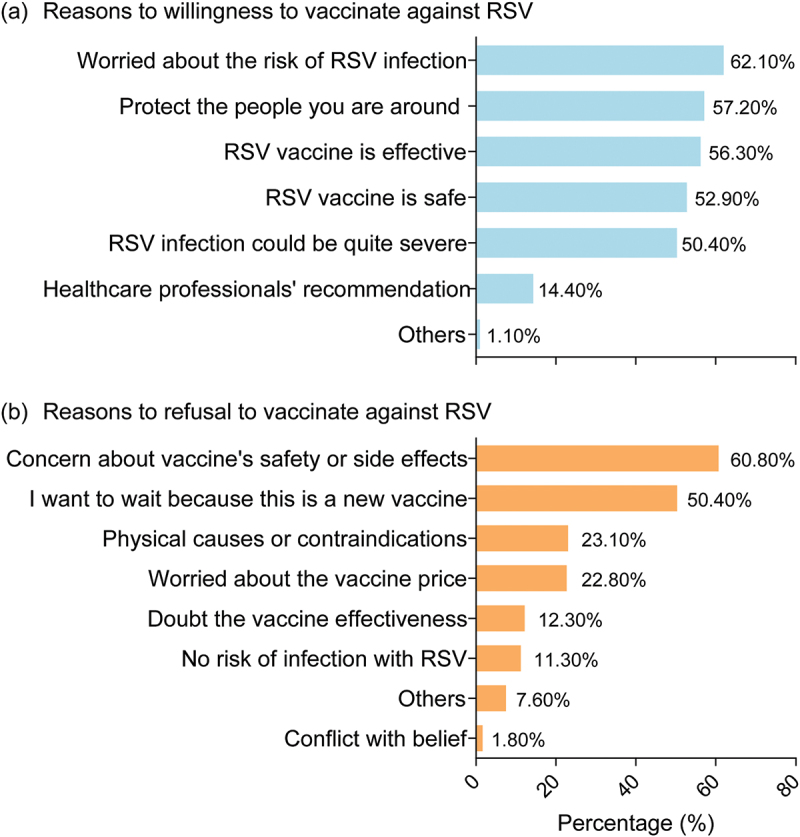
Reasons for willingness and refusal to vaccinate against RSV.
Regarding population influencing the decision to vaccinate against RSV, 44.7% of participants identified the recommendations from healthcare professionals in tertiary hospitals as the most impactful (Figure 3). Regarding the acceptable price range for the RSV vaccine, 60.01% of individuals considered a price below 200 CNY (28 USD) as acceptable, while only 2.81% considered a price below 3000 CNY (417 USD) to be acceptable.
Figure 3.
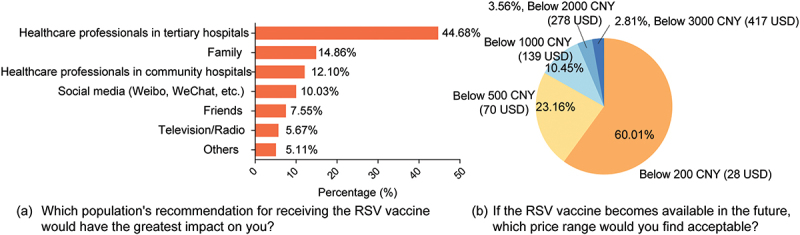
Main information sources for decision-making and acceptable prices for RSV vaccine.
Discussion
Our study has demonstrated one-quarter of individuals (518/2133) who reported that they had never heard of RSV, while 55.7% (1188/2133) and 76.8% (1639/2133) exhibited low levels of perceptions of susceptibility and severity of RSV infection, respectively. More than 30% (674/2133) of the participants expressed reluctance to receive an RSV vaccine. The most frequent reason for accepting the RSV vaccine was “Worried about the risk of RSV infection,” while the primary reason for declining the vaccine was “Concern about vaccine’s safety or side effects.” It was also found that the acceptable price of the RSV vaccine was relatively low.
The Health Belief Model (HBM) has served as a valuable framework for elucidating shifts in health-related behaviors and their continuance since the 1950s.17 Perceived susceptibility and severity of a disease are two of the six domains within the HBM. Elevated perceptions of disease risk tend to foster positive health behaviors. The levels of perceived susceptibility to and severity of RSV infection in our study were not high. Among the factors analyzed, occupation emerged as a significant influencing factor. Interestingly, individuals involved in healthcare occupations demonstrated elevated perceptions of susceptibility but concurrently displayed diminished perceptions of severity compared to those who did not. This phenomenon could be linked to the absence of routine laboratory tests to diagnose RSV infections, potentially influencing the perception of severity among healthcare professionals.8 Physicians might prioritize their attention toward the severe health complications associated with RSV, such as bronchiolitis and pneumonia, while downplaying the role of the virus as an etiological agent in these conditions. Due to their extensive experience in dealing with various diseases and witnessing more severe conditions, it is possible that healthcare professionals perceive RSV infection as less prominent and, hence, do not consider it a significantly severe condition.
In a survey of 5627 parents from eight countries, the rate of parental acceptance of the mAb products for their infants ranged from 43% in France to 72% in China.7 In Jordan, 70% of surveyed young females were willing to vaccinate against RSV during pregnancy.18 Furthermore, 40% of pregnant women in England indicated a high likelihood of accepting the vaccine if it is routinely recommended.6 Concerning about vaccine’s safety or side effects was the most frequent reasons to refuse the RSV vaccine. This aligns with the prevalent reasons for vaccine refusal observed in previous studies, including those related to COVID-19 and monkeypox vaccines.11,19 Existing evidence has demonstrated the safety of vaccines including Arexvy and AbrysvoTM, with acceptable safety profiles.20,21 Our study revealed that 3/5 of the participants deemed a price below 200 CNY (28 USD) as acceptable. AbrysvoTM was priced at 219.72 USD and Arexvy was priced at 198.396 USD, representing a higher cost in comparison to other vaccines such as influenza or pneumococcal vaccines.22 High price of RSV vaccine might be a barrier to its adoption. Zeevat et al. found that the justifiable RSV vaccine price was 50.03 EUR (389 CNY) in the Netherlands and 109.74 GBP (980 CNY) in the United Kingdom.23 Further investigations in China are warranted to determine a reasonable price that can achieve cost-effectiveness while considering its potential impact on vaccine hesitancy.
Adults aged ≥60 years were identified as a high-risk population because they were highly likely to develop serious complications from RSV infection.24 Our study revealed that older adults were more likely to have reduced awareness and knowledge of RSV and to refuse the RSV vaccine. Previous studies found that a negative correlation between older age and higher vaccine confidence and higher vaccination rates.25,26 According to Yang et al., within the context of the “3Cs” framework driving vaccine hesitancy (confidence, complacency, and convenience), confidence played a more significant role in influencing vaccine hesitancy among older adults.27 Their study identified a positive association between lower socioeconomic status and higher vaccine hesitancy.27 Vaccine hesitancy in older adults could also be explained by limited access to relevant information or lack of social support.26,28 Utilizing the influence of healthcare professionals in tertiary hospitals could potentially serve as a strategy to mitigate RSV vaccine hesitancy and increase vaccine uptake when RSV vaccines are introduced in China. It is advisable to conduct ongoing assessments of older adults’ attitudes toward RSV vaccines in the future to provide valuable insights for policy formulation and decision-making.
Our study has a few limitations. Firstly, using a convenience sampling method and web-based survey may constrain the representativeness of the surveyed sample and, subsequently, the generalizability of the findings. The presence of selection bias was possible, because of the high proportion of education level and economic status and the low proportion of older adults among participants, which may lead to an overestimation of the level of awareness and knowledge of RSV among the general population. Additionally, individuals unfamiliar with RSV might have been less motivated to participate in the questionnaire. Actual public awareness and knowledge of RSV may be even lower. Second, caution should be exercised when interpreting willingness to receive the RSV vaccine. There was a gap between the willingness to be vaccinated and the final act of vaccination. Participants may tend to express a willingness toward vaccinations to conform to socially acceptable norms, a phenomenon known as social desirability bias. Third, we tested RSV-related knowledge using seven questions and specific terms, such as bronchiolitis, which might not provide a full picture of the public’s knowledge of RSV. Future research should consider adding knowledge-related items and ensuring their comprehensibility when investigating populations’ knowledge of RSV. For example, the public can distinguish RSV from other viruses that cause acute respiratory infections. Fourth, the categorization of perception into high or low which related to perceived susceptibility and severity aimed to capture the spectrum of subjective risk assessments among participants. The classification of participants into “low perception” did not inherently label their perception as right or wrong. Finally, the perceptions and attitudes, influenced by various factors, may vary over time.
Conclusions
Our findings have underscored the lack awareness and perceived susceptibility to RSV infection among the Chinese public. A notable proportion (approximately one-third) showed refusal to vaccinated against RSV. Our study also indicated that the acceptable price of the RSV vaccine was relatively low. It is necessary to take measures to address the limited awareness of RSV and acceptability of the RSV vaccine among older adults.
Supplementary Material
Acknowledgments
This work was supported by AIR@InnoHK administered by Innovation and Technology Commission; Medical Development discipline Foundation of Wuxi [grant number FZXK2021010]. WBW was supported by Shanghai Municipal Science and Technology Major Project [grant number ZD2021CY001]. The sponsor and funder had no role in the study design, data collection, analysis, interpretation of data, writing, or in the decision to submit the article for publication.
Appendix.
Table A1.
Distributions of respondents’ locations.
| Province | No. (%) (N = 2133) |
|---|---|
| Anhui | 38 (1.78) |
| Beijing | 33 (1.55) |
| Chongqing | 136 (6.38) |
| Fujian | 75 (3.52) |
| Gansu | 19 (0.89) |
| Guangdong | 174 (8.16) |
| Guangxi | 37 (1.73) |
| Guizhou | 5 (0.23) |
| Hainan | 4 (0.19) |
| Hebei | 60 (2.81) |
| Heilongjiang | 32 (1.50) |
| Henan | 51 (2.39) |
| Hubei | 46 (2.16) |
| Hunan | 36 (1.69) |
| Inner Mongolia | 14 (0.66) |
| Jiangsu | 687 (32.21) |
| Jiangxi | 44 (2.06) |
| Jilin | 19 (0.89) |
| Liaoning | 34 (1.59) |
| Ningxia | 8 (0.38) |
| Qinghai | 23 (1.08) |
| Shaanxi | 22 (1.03) |
| Shandong | 168 (7.88) |
| Shanghai | 124 (5.81) |
| Shanxi | 35 (1.64) |
| Sichuan | 42 (1.97) |
| Tianjin | 5 (0.23) |
| Tibet | 1 (0.05) |
| Xinjiang | 6 (0.28) |
| Yunnan | 19 (0.89) |
| Zhejiang | 136 (6.38) |
Table A2.
Awareness of RSV by socio-demographics.
| Characteristics | Awareness of RSV |
P value | |
|---|---|---|---|
| Never heard, No. (%) | Yes, No. (%) | ||
| Age group, years | <.001 | ||
| 18–≤30 | 187 (20.5) | 724 (79.5) | |
| 31–≤40 | 196 (24.0) | 621 (76.0) | |
| 41–≤50 | 93 (32.1) | 197 (67.9) | |
| >50 | 42 (36.5) | 73 (63.5) | |
| Sex | .184 | ||
| Male | 255 (25.6) | 741 (74.4) | |
| Female | 263 (23.1) | 874 (76.9) | |
| Marital status | .056 | ||
| Unmarried | 341 (24.4) | 1057 (75.6) | |
| Married | 162 (23.2) | 536 (76.8) | |
| Divorce | 15 (40.5) | 22 (59.5) | |
| Education level | .014 | ||
| Junior high school or below | 45 (36.0) | 80 (64.0) | |
| High school graduate or equivalent | 47 (26.1) | 133 (73.9) | |
| Undergraduate or equivalent | 363 (23.2) | 1201 (76.8) | |
| Postgraduate or above | 63 (23.9) | 201 (76.1) | |
| Occupation | <.001 | ||
| Healthcare-related | 76 (10.4) | 656 (89.6) | |
| Others | 442 (31.5) | 959 (68.5) | |
| Living with children aged ≤6 years or old adults aged ≥60 years | .016 | ||
| Yes | 296 (22.5) | 1018 (77.5) | |
| No | 222 (27.1) | 597 (72.9) | |
| Annual household income (CNY) | <.001 | ||
| <50,000 | 73 (36.9) | 125 (63.1) | |
| 50,000–≤149,999 | 190 (21.6) | 689 (78.4) | |
| 150,000–≤299,999 | 157 (21.0) | 589 (79.0) | |
| ≥300,000 | 98 (31.6) | 212 (68.4) | |
| Having chronic diseases | .005 | ||
| Yes | 63 (23.7) | 203 (76.3) | |
| No | 421 (23.7) | 1359 (76.3) | |
| Unclear | 34 (39.1) | 53 (60.9) | |
| Self-reported health | <.001 | ||
| Very poor | 9 (33.3) | 18 (66.7) | |
| Poor | 25 (31.3) | 55 (68.8) | |
| Neutral | 287 (29.5) | 687 (70.5) | |
| Well | 151 (18.6) | 660 (81.4) | |
| Very well | 46 (19.1) | 195 (80.9) | |
| Experiencing side effects following previous vaccination | .001 | ||
| Yes | 38 (23.3) | 125 (76.7) | |
| No | 437 (23.5) | 1422 (76.5) | |
| Unclear | 43 (38.7) | 68 (61.3) | |
Table A3.
Knowledge of RSV by socio-demographics.
| Characteristics | Knowledge of RSV |
P value | |
|---|---|---|---|
| Low level, No. (%) | High level, No. (%) | ||
| Age group, years | .012 | ||
| 18–≤30 | 446 (49.0) | 465 (51.0) | |
| 31–≤40 | 349 (42.7) | 468 (57.3) | |
| 41–≤50 | 124 (42.8) | 166 (57.2) | |
| >50 | 62 (53.9) | 53 (46.1) | |
| Sex | .001 | ||
| Male | 497 (49.9) | 499 (50.1) | |
| Female | 484 (42.6) | 653 (57.4) | |
| Marital status | <.001 | ||
| Unmarried | 600 (42.9) | 798 (57.1) | |
| Married | 364 (52.1) | 334 (47.9) | |
| Divorce | 17 (45.9) | 20 (54.1) | |
| Education level | <.001 | ||
| Junior high school or below | 94 (75.2) | 31 (24.8) | |
| High school graduate or equivalent | 103 (57.2) | 77 (42.8) | |
| Undergraduate or equivalent | 690 (44.1) | 874 (55.9) | |
| Postgraduate or above | 94 (35.6) | 170 (64.4) | |
| Occupation | <.001 | ||
| Healthcare-related | 232 (31.7) | 500 (68.3) | |
| Others | 749 (53.5) | 652 (46.5) | |
| Living with children aged ≤6 years or old adults aged ≥60 years | .881 | ||
| Yes | 606 (46.1) | 708 (53.9) | |
| No | 375 (45.8) | 444 (54.2) | |
| Annual household income (CNY) | <.001 | ||
| <50,000 | 122 (61.6) | 76 (38.4) | |
| 50,000–≤149,999 | 408 (46.4) | 471 (53.6) | |
| 150,000–≤299,999 | 293 (39.3) | 453 (60.7) | |
| ≥300,000 | 158 (51.0) | 152 (49.0) | |
| Having chronic diseases | <.001 | ||
| Yes | 134 (50.4) | 132 (49.6) | |
| No | 783 (44.0) | 997 (56.0) | |
| Unclear | 64 (73.6) | 23 (26.4) | |
| Self-reported health | .022 | ||
| Very poor | 18 (66.7) | 9 (33.3) | |
| Poor | 42 (52.5) | 38 (47.5) | |
| Neutral | 468 (48.0) | 506 (52.0) | |
| Well | 347 (42.8) | 464 (57.2) | |
| Very well | 106 (44.0) | 135 (56.0) | |
| Experiencing side effects following previous vaccination | .008 | ||
| Yes | 89 (54.6) | 74 (45.4) | |
| No | 831 (44.7) | 1028 (55.3) | |
| Unclear | 61 (55.0) | 50 (45.0) | |
| Awareness of RSV | <.001 | ||
| I have never heard of it | 348 (67.2) | 170 (32.8) | |
| I have heard of it, but don’t really know what it is | 430 (50.2) | 426 (49.8) | |
| I know some facts about what it is | 188 (27.3) | 501 (72.7) | |
| I have a good understanding about RSV | 15 (21.4) | 55 (78.6) | |
Figure A1.
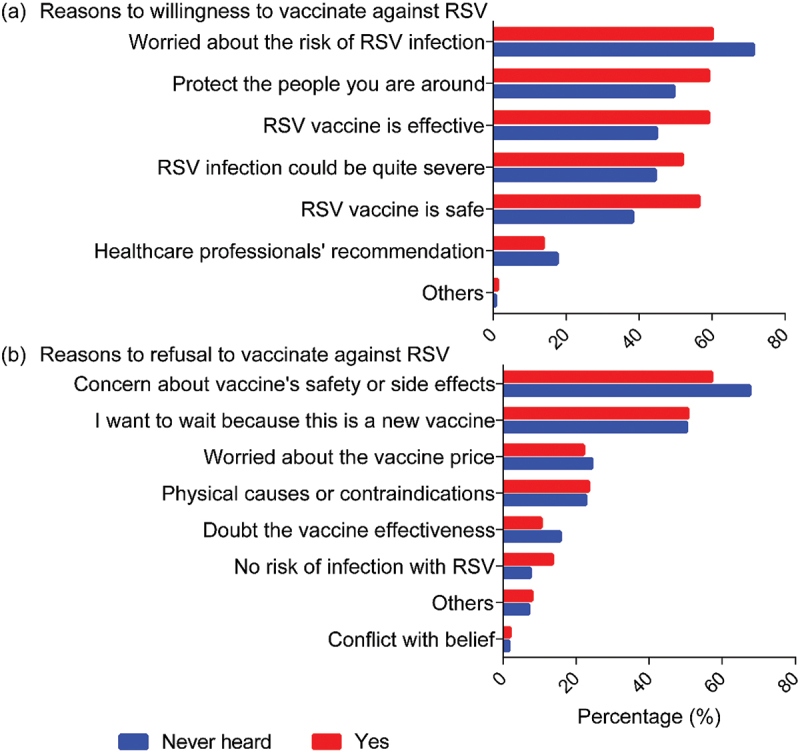
Reasons for willingness and refusal to vaccinate against RSV by level of awareness.
Figure A2.
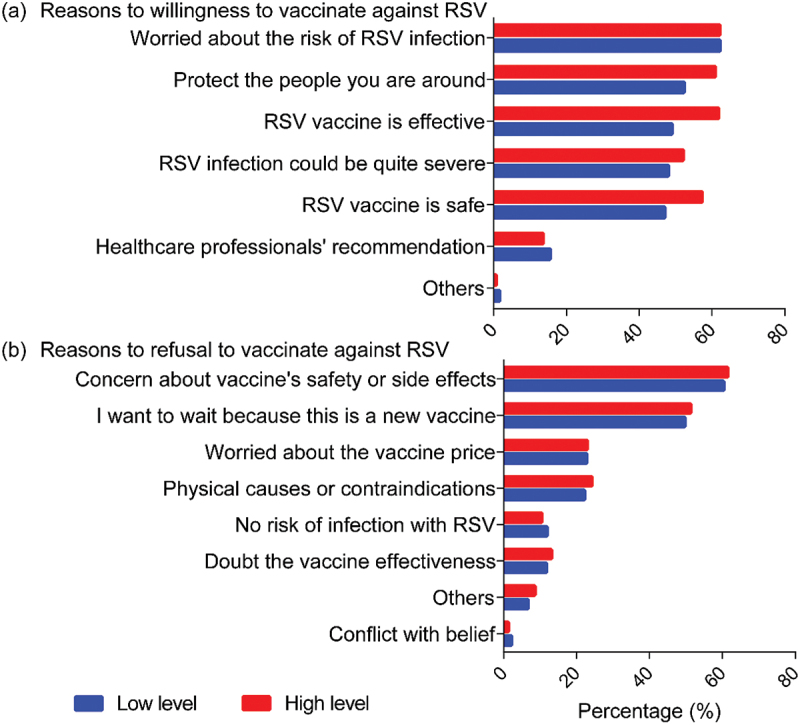
Reasons for willingness and refusal to vaccinate against RSV by level of knowledge.
Figure A3.
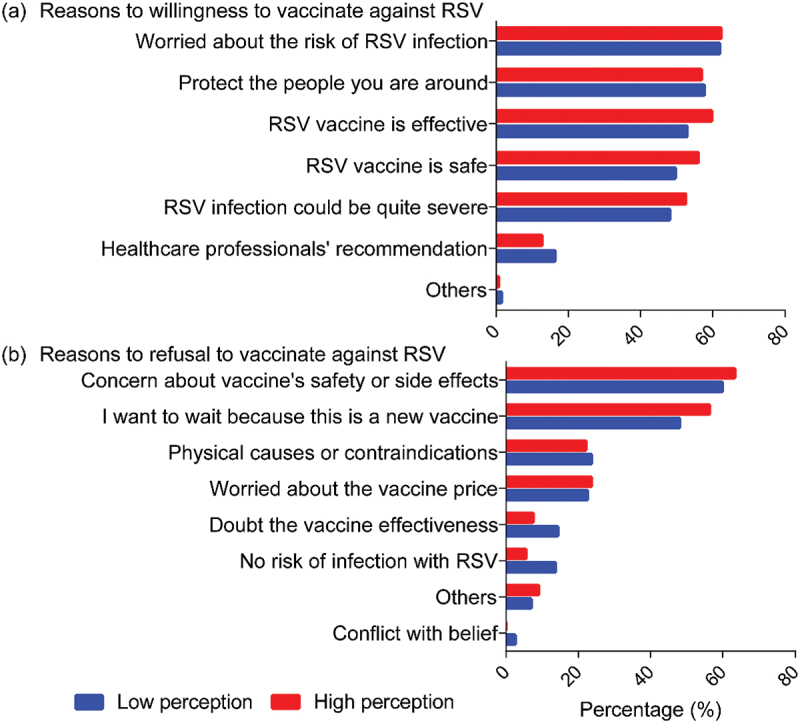
Reasons for willingness and refusal to vaccinate against RSV by level of perceptions of susceptibility.
Figure A4.
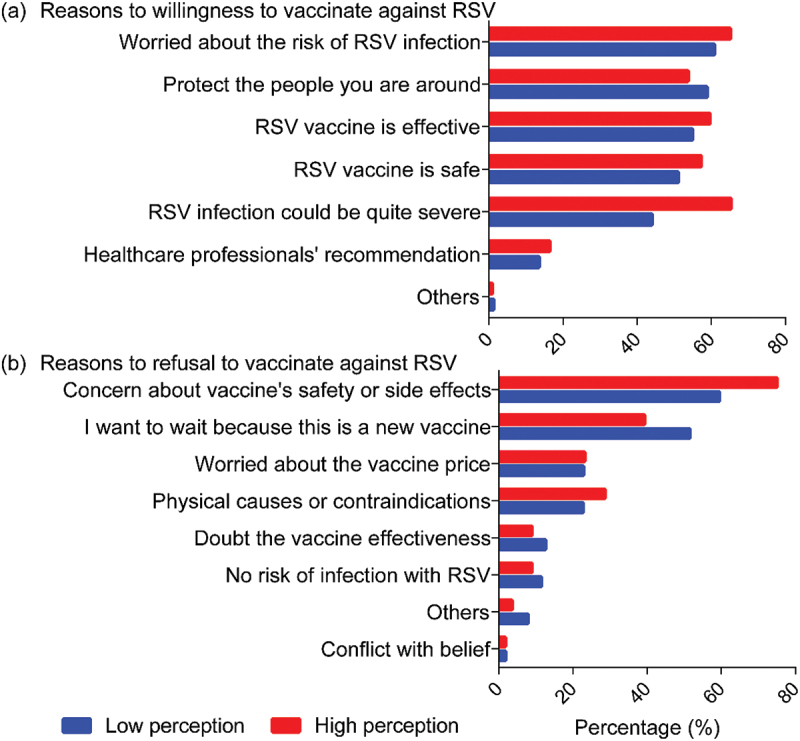
Reasons for willingness and refusal to vaccinate against RSV by level of perceptions of severity.
Funding Statement
The work was supported by the Medical Development discipline Foundation of Wuxi [FZXK2021010]; Innovation and Technology Commission [AIR@InnoHK]; Shanghai Municipal Science and Technology Major Project [ZD2021CY001].
Disclosure statement
No potential conflict of interest was reported by the author(s).
CRediT authorship contribution statement
QW: Conceptualization, Data curation, Formal Analysis, Writing original draft, Writing review & editing, Methodology, Visualization. SXX: Conceptualization, Investigation, Methodology, Writing original draft, Funding acquisition. LQY: Methodology, Writing original draft. Lan L: Methodology, Writing original draft. MY: Investigation. XWW: Investigation. YS: Investigation. WBW: Supervision, Funding acquisition. Leesa L: Conceptualization, Supervision, Writing review & editing, Funding acquisition.
Data availability statement
Data may be available from the corresponding author on reasonable request depending on the policy and procedures of the institutions that participate in the consortiums.
Supplementary material
Supplemental data for this article can be accessed on the publisher’s website at https://doi.org/10.1080/21645515.2024.2310916
References
- 1.Li Y, Wang X, Blau DM, Caballero MT, Feikin DR, Gill CJ, Madhi SA, Omer SB, Simões EAF, Campbell H, et al. Global, regional, and national disease burden estimates of acute lower respiratory infections due to respiratory syncytial virus in children younger than 5 years in 2019: a systematic analysis. Lancet. 2022;399(10340):2047–14. doi: 10.1016/S0140-6736(22)00478-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Savic M, Penders Y, Shi T, Branche A, Pirçon JY.. Respiratory syncytial virus disease burden in adults aged 60 years and older in high-income countries: a systematic literature review and meta-analysis. Influenza Other Respir Viruses. 2023;17(1):e13031. doi: 10.1111/irv.13031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Munro APS, Martinón-Torres F, Drysdale SB, Faust SN. The disease burden of respiratory syncytial virus in infants. Curr Opin Infect Dis. 2023;36(5):379–384. doi: 10.1097/QCO.0000000000000952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention . Respiratory Syncytial Virus (RSV) immunizations. [accessed 2023 Sept 26]. https://www.cdc.gov/vaccines/vpd/rsv/index.html.
- 5.U.S. FOOD & DRUG . FDA approves first vaccine for pregnant individuals to prevent RSV in infants. [accessed 2023 Sept 26].https://www.fda.gov/news-events/press-announcements/fda-approves-first-vaccine-pregnant-individuals-prevent-rsv-infants.
- 6.Wilcox CR, Calvert A, Metz J, Kilich E, MacLeod R, Beadon K, Heath PT, Khalil A, Finn A, Snape MD, et al. Attitudes of pregnant women and healthcare professionals toward clinical trials and routine implementation of antenatal vaccination against respiratory syncytial virus: a multicenter questionnaire study. Pediatr Infect Dis J. 2019;38(9):944–951. doi: 10.1097/INF.0000000000002384. [DOI] [PubMed] [Google Scholar]
- 7.Lee Mortensen G, Harrod-Lui K. Parental knowledge about respiratory syncytial virus (RSV) and attitudes to infant immunization with monoclonal antibodies. Expert Rev Vaccines. 2022;21(10):1523–1531. doi: 10.1080/14760584.2022.2108799. [DOI] [PubMed] [Google Scholar]
- 8.Hurley LP, Allison MA, Kim L, O’Leary ST, Crane LA, Brtnikova M, Beaty BL, Allen KE, Poser S, Lindley MC, et al. Primary care physicians’ perspectives on respiratory syncytial virus (RSV) disease in adults and a potential RSV vaccine for adults. Vaccine. 2019;37(4):565–570. doi: 10.1016/j.vaccine.2018.12.031. [DOI] [PubMed] [Google Scholar]
- 9.Center for drug evaluation. Implied permission for clinical trials. [accessed 2023 Sept 26]. https://www.cde.org.cn/main/xxgk/listpage/4b5255eb0a84820cef4ca3e8b6bbe20c.
- 10.Schmoele-Thoma B, Zareba AM, Jiang Q, Maddur MS, Danaf R, Mann A, Eze K, Fok-Seang J, Kabir G, Catchpole A, et al. Vaccine efficacy in adults in a respiratory syncytial virus challenge study. N Engl J Med. 2022;386(25):2377–2386. doi: 10.1056/NEJMoa2116154. [DOI] [PubMed] [Google Scholar]
- 11.Wang B, Peng X, Li Y, Fu L, Tian T, Liang B, Sun Y, Chen Y, Wu X, Liu Q, et al. Perceptions, precautions, and vaccine acceptance related to monkeypox in the public in China: a cross-sectional survey. J Infect Public Health. 2023;16(2):163–170. doi: 10.1016/j.jiph.2022.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Riccò M, Ferraro P, Peruzzi S, Zaniboni A, Ranzieri S. Respiratory syncytial virus: knowledge, attitudes and beliefs of general practitioners from North-Eastern Italy (2021). Pediatr Rep. 2022;14(2):147–165. doi: 10.3390/pediatric14020021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wendlandt R, Cowling BJ, Chen Y, Havers F, Shifflett P, Song Y, Zhang R, Iuliano D, Xu C, Yu H, et al. Knowledge, attitudes and practices related to the influenza virus and vaccine among older adults in Eastern China. Vaccine. 2018;36(19):2673–2682. doi: 10.1016/j.vaccine.2018.03.052. [DOI] [PubMed] [Google Scholar]
- 14.Lazarus JV, Ratzan SC, Palayew A, Gostin LO, Larson HJ, Rabin K, Kimball S, El-Mohandes A. A global survey of potential acceptance of a COVID-19 vaccine. Nat Med. 2021;27(2):225–228. doi: 10.1038/s41591-020-1124-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sumner KM, Duca LM, Arriola CS, Neyra J, Soto G, Romero C, Tinoco Y, Nogareda F, Matos E, Chavez V, et al. Knowledge, attitudes, and practices associated with frequent influenza vaccination among healthcare personnel in Peru, 2016–2018. Vaccine. 2023;14:100314. Published 2023 May 12. doi: 10.1016/j.jvacx.2023.100314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Eysenbach G. Improving the quality of web surveys: the checklist for reporting results of internet E-Surveys (CHERRIES). J Med Internet Res. 2004;6(3):e34. doi: 10.2196/jmir.6.3.e34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Karen G, Barbara KR, Viswanath K. Health behavior and health education: theory, research, and practice. 4th ed. San Francisco (CA): Jossey-Bass; 2008. [Google Scholar]
- 18.Kherfan T, Sallam M. Prospective attitudes towards Respiratory Syncytial Virus (RSV) vaccination: validation of a survey instrument among young females in Jordan pending vaccine Authorization. Vaccines (Basel). 2023;11(8):1386. doi: 10.3390/vaccines11081386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wang Q, Yang L, Jin H, Lin L. Vaccination against COVID-19: a systematic review and meta-analysis of acceptability and its predictors. Prev Med. 2021;150:106694. doi: 10.1016/j.ypmed.2021.106694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kampmann B, Madhi SA, Munjal I, Simões EAF, Pahud BA, Llapur C, Baker J, Pérez Marc G, Radley D, Shittu E, et al. Bivalent prefusion F vaccine in pregnancy to prevent RSV Illness in Infants. N Engl J Med. 2023;388(16):1451–1464. doi: 10.1056/NEJMoa2216480. [DOI] [PubMed] [Google Scholar]
- 21.Melgar M, Britton A, Roper LE, Talbot HK, Long SS, Kotton CN, Havers FP. Use of respiratory syncytial virus vaccines in older adults: recommendations of the advisory committee on immunization practices – United States, 2023. MMWR Morb Mortal Wkly Rep. 2023;72(29):793–801. doi: 10.15585/mmwr.mm7229a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Centers for Disease Control and Prevention. CDC Vaccine Price List . [accessed 2023 Sept 26]. https://www.cdc.gov/vaccines/programs/vfc/awardees/vaccine-management/price-list/index.html.
- 23.Zeevat F, Luttjeboer J, Paulissen JHJ, van der Schans J, Beutels P, Boersma C, Postma MJ, Nair H, Campbell H, Openshaw P, et al. Exploratory analysis of the economically justifiable price of a hypothetical RSV vaccine for older adults in the Netherlands and the United Kingdom. J Infect Dis. 2022;226(Suppl 1):S102–S109. doi: 10.1093/infdis/jiab118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Centers for Disease Control and Prevention . RSV prevention. [accessed 2023 Sept 26]. https://www.cdc.gov/rsv/about/prevention.html.
- 25.de Figueiredo A, Simas C, Karafillakis E, Paterson P, Larson HJ. Mapping global trends in vaccine confidence and investigating barriers to vaccine uptake: a large-scale retrospective temporal modelling study. Lancet. 2020;396(10255):898–908. doi: 10.1016/S0140-6736(20)31558-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wang G, Yao Y, Wang Y, Gong J, Meng Q, Wang H, Wang W, Chen X, Zhao Y. Determinants of COVID-19 vaccination status and hesitancy among older adults in China. Nat Med. 2023;29(3):623–631. doi: 10.1038/s41591-023-02241-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yang L, Ji L, Wang Q, Yang G, Xiu S, Cui T, Shi N, Zhu L, Xu X, Jin H, et al. Understanding drivers of vaccine hesitancy during the COVID-19 pandemic among older adults in Jiangsu Province, China: cross-sectional survey. JMIR Form Res. 2023;7:e39994. doi: 10.2196/39994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zhang D, Zhou W, Poon PK, Kwok KO, Chui TW, Hung PHY, Ting BYT, Chan DCC, Wong SYS. Vaccine resistance and hesitancy among older adults who live alone or only with an older partner in community in the early stage of the fifth wave of COVID-19 in Hong Kong. Vaccines (Basel). 2022;10(7):1118. doi: 10.3390/vaccines10071118. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data may be available from the corresponding author on reasonable request depending on the policy and procedures of the institutions that participate in the consortiums.


