Introduction
Venous thromboembolism is the third most common cardiovascular condition, with an annual incidence estimated at 1 in 1000 persons. 1 Of these, a third present with deep venous thrombosis (DVT), with symptoms including localised pain, swelling and tenderness of the calf or thigh, and signs including erythema and warmth in the affected limb. DVTs may result in devastating complications; more acutely, DVTs can result in pulmonary embolism which is associated with high morbidity and mortality rate. The longer-term sequelae of DVTs include post-thrombotic syndrome (PTS), with chronic limb swelling and ulceration leading to prolonged quality of life impairments.
Of all lower limb DVTs diagnosed on ultrasound, between 30 and 50% may be classified as an isolated distal DVT (IDDVT). 2 IDDVTs refer to thrombosis of the infra-popliteal veins, which include the inter-muscular deep veins (including the posterior tibial, anterior tibial, and peroneal veins) and the calf intra-muscular veins (gastrocnemius and soleal veins). These are usually associated with transient risk factors2,3 and exhibit lower risk for propagation. However, IDDVTs are still associated with the complications discussed above, with a 17% PTS rate, one in 50 developing ulceration after experiencing an IDDVT, 4 and around 5% risk of developing a pulmonary embolism. 5 Appropriate management of IDDVTs is therefore essential to prevent patients from experiencing long-term sequelae stemming from this condition.
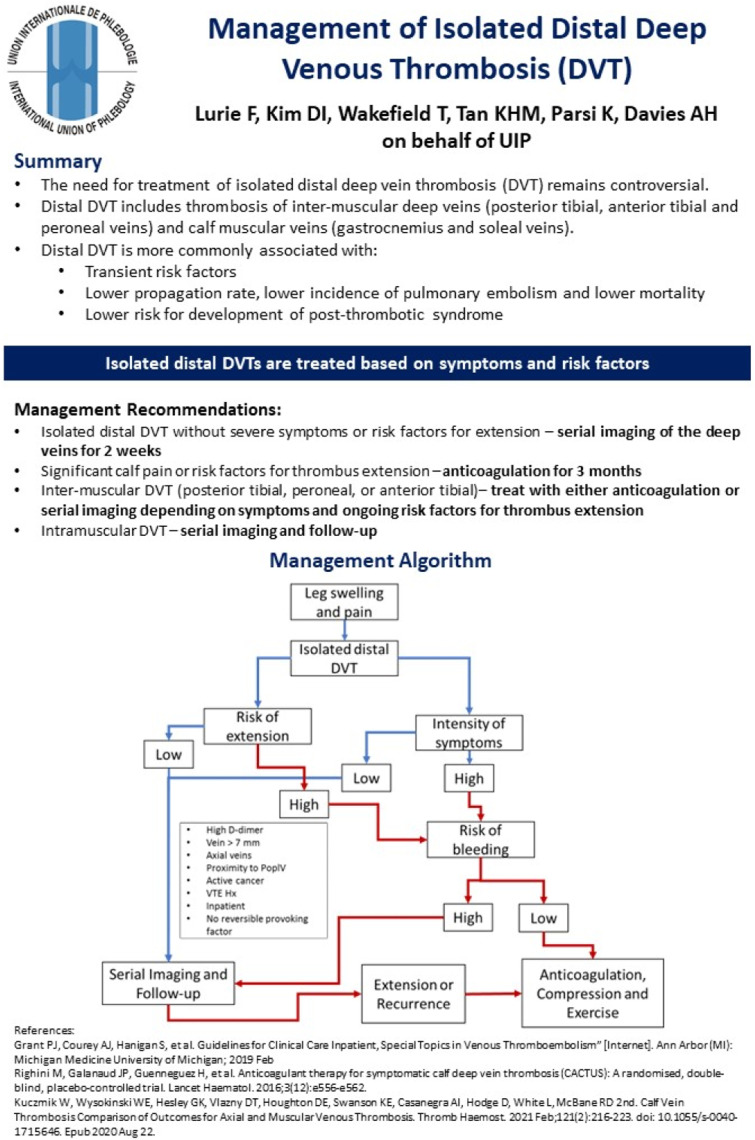
In general, IDDVTs may be treated conservatively with compression and/or serial imaging and observation, or with anticoagulation to help limit proximal extension and recurrence. However, there remains significant debate on selecting the optimal treatment for specific patients presenting with IDDVTs. This article seeks to highlight the management recommendations from the International Union of Phlebology (UIP), identifying characteristics that may help with patient stratification for different treatment options. The accompanying one-page summary also provides a management algorithm that can be followed to help clinicians determine the optimal management plan for patients presenting with IDDVTs (Figure 1).
Figure 1.
One-page guideline.
Management recommendations
It is recommended that patients presenting with IDDVTs should be stratified based on their symptom burden (high or low burden) and risk factors for proximal extension (Table 1). 6 Two main treatment strategies exist: conservative management with serial imaging and regular follow-up, or anticoagulation together with compression therapy. IDDVT, if presenting without severe symptoms or risk factors for extension, can be managed conservatively. Serial imaging of the deep veins for 2 weeks is recommended, with regular follow-up with a vascular specialist for monitoring. If there are signs of proximal extension or recurrence, the patient will then be started on anticoagulation and compression.
Table 1.
Risk factors for proximal extension of an IDDVT.
| High D-dimer | Active malignancy |
| Vein diameter >7 mm | History of VTE |
| Axial vein involvement | Inpatient admission |
| Proximity to popliteal vein | No reversible provoking factor |
However, should there be significant symptoms such as calf pain or any risk factors for thrombus extension, patients should be further stratified according to their risk of bleeding. If they are deemed to be at low risk of bleeding, 3 months of anticoagulation may be prescribed together with compression therapy. Patients should also be advised to exercise. However, if they are at a high risk of bleeding, it is recommended that clinicians perform serial imaging and follow-up, and only prescribe anticoagulation if there are signs of extension or recurrence on imaging. 7
Management may also be further stratified according to the location of the DVT either in the inter-muscular deep veins or the intra-muscular veins. It is recommended that intra-muscular IDDVTs can be managed with serial imaging and follow-up alone. Inter-muscular IDDVTs (in the posterior tibial, peroneal, or anterior tibial veins) may be managed with either anticoagulation or serial imaging depending on patients’ symptoms and risk factors for thrombus extension as detailed above.
Discussion
This article provides a one-page clinical practice guideline summarising the clinical management of IDDVT. It is part of a series of publications for the UIP One-Page Guidelines which are aimed at ensuring that patients with venous disease receive timely and appropriate care based on current best evidence and expert consensus.
Despite the frequency of IDDVTs encountered in clinical practice, the current evidence remains sparse and there remains controversy regarding whether IDDVTs require treatment at all. This stems from studies showing low risks of proximal extension and high rates of complete resolution without anticoagulant treatment, 8 and low risks of developing valvular insufficiency at late follow-up. 9 However, few studies have directly observed the effects of treatment in confirmed IDDVTs. For example, the more recent CACTUS trial showed no significant impact of therapeutic anticoagulation for proximal extension or thromoboembolism rates related to IDDVTs, but increased risk of bleeding. This trial, however, was underpowered due to early trial termination. The lack of trials directly comparing the various treatment modalities represents a gap in the literature that should be addressed urgently.
This one-page guideline has recommended that high-risk or highly symptomatic patients receiving anticoagulation should continue treatment for at least 3 months, which is consistent with the guidelines from the American College of Chest Physicians. 10 Studies have however used varying protocols ranging from 6 weeks to 3 months, with a meta-analysis suggesting reduction in recurrence rates when comparing patients who received more than 6 weeks of anticoagulant therapy to those who received 6 weeks only. 11 Optimal duration of anticoagulation, in view of the potential bleeding risks (as observed in the CACTUS trial 7 ), needs to be clarified further to maximise therapeutic benefits for patients without significantly increasing their risks.
For healthcare providers, this article and summary document should highlight the complexity of management of IDDVTs. All healthcare staff members, including emergency medicine practitioners and vascular specialists, that are likely to encounter a patient with an IDDVT should be aware of the need for individualised risk assessment and targeted management, with appropriate escalation of therapies applied when required. This is in line with national and international guidelines and further reinforced by the management algorithm provided in this one-page guideline. This will facilitate the urgent assessment and interventions indicated in this population of patients.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Guarantor: Professor Alun Davies on behalf of the UIP.
Contributorship: K.P. and A.H.D. conceptualised the design of the short report and one-page guideline.
F.L., D-I.K., and T.W. contributed to the literature review and formulation of the recommendations.
M.T. contributed to the formatting and layout of the one-page guideline (Figure 1) and wrote the initial draft of the short report.
All authors reviewed the short report prior to submission.
ORCID iDs
Matthew Tan https://orcid.org/0000-0002-5789-0353
Kurosh Parsi https://orcid.org/0000-0003-0630-8877
Alun H Davies https://orcid.org/0000-0001-5261-6913
References
- 1.Heit JA. Epidemiology of venous thromboembolism. Nat Rev Cardiol 2015; 12(8): 464–474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kesieme E, Kesieme C, Jebbin N, et al. Deep vein thrombosis: a clinical review. Hematol Res Rev 2011: 59–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Grant PJ, Courey AJ, Hanigan S, et al. Guidelines for clinical care inpatient, special topics in venous thromboembolism” [Internet]. Ann Arbor, MI: Michigan Medicine University of Michigan, 2019. [PubMed] [Google Scholar]
- 4.Turner BR, Thapar A, Jasionowska S, et al. Systematic review and meta-analysis of the pooled rate of post-thrombotic syndrome after isolated distal deep venous thrombosis. Eur J Vasc Endovasc Surg. 2022; 65: 291–295. [DOI] [PubMed] [Google Scholar]
- 5.Spencer FA, Kroll A, Lessard D, et al. Isolated calf deep vein thrombosis in the community setting: the Worcester Venous Thromboembolism study. J Thromb Thrombolysis 2012; 33(3): 211–217. [DOI] [PubMed] [Google Scholar]
- 6.Kuczmik W, Wysokinski WE, Hesley GK, et al. Calf Vein Thrombosis Comparison of Outcomes for Axial and Muscular Venous Thrombosis. Thromb Haemostasis 2021; 121(2): 216–223. Epub 2020 Aug 22. DOI: 10.1055/s-0040-1715646. [DOI] [PubMed] [Google Scholar]
- 7.Righini M, Galanaud JP, Guenneguez H, et al. Anticoagulant therapy for symptomatic calf deep vein thrombosis (CACTUS): A randomised, double-blind, placebo-controlled trial. Lancet Haematol 2016; 3(12): e556–e562. [DOI] [PubMed] [Google Scholar]
- 8.Palareti G, Cosmi B, Lessiani G, et al. Evolution of untreated calf deep-vein thrombosis in high risk symptomatic outpatients: the blind, prospective CALTHRO study. Thromb Haemostasis 2010; 104(11): 1063–1070. [DOI] [PubMed] [Google Scholar]
- 9.McLafferty RB, Moneta GL, Passman MA, et al. Late clinical and hemodynamic sequelae of isolated calf vein thrombosis. J Vasc Surg 1998; 27(1): 50–57. [DOI] [PubMed] [Google Scholar]
- 10.Stevens SM, Woller SC, Kreuziger LB, et al. Antithrombotic therapy for VTE disease: second update of the CHEST guideline and expert panel report. Chest 2021; 160(6): e545–608. [DOI] [PubMed] [Google Scholar]
- 11.Franco L, Giustozzi M, Agnelli G, et al. Anticoagulation in patients with isolated distal deep vein thrombosis: a meta‐analysis. J Thromb Haemostasis 2017; 15(6): 1142–1154. [DOI] [PubMed] [Google Scholar]