Abstract
Hepatocellular carcinoma (HCC) is a common complication in patients with chronic liver disease and leads to significant morbidity and mortality. Liver disease and liver cancer are preventable by mitigating and managing common risk factors, including chronic hepatitis B and C infection, alcohol use, diabetes, obesity, and other components of the metabolic syndrome. The management of patients with HCC requires treatment of the malignancy and adequate control of the underlying liver disease, as preserving liver function is critical for successful cancer treatment and may have a relevant prognostic role independent of HCC management. Hepatologists are the ideal providers to guide the care of patients with HCC as they are trained to identify patients at risk, apply appropriate surveillance strategies, assess and improve residual liver function, evaluate candidacy for transplant, provide longitudinal care to optimize and preserve liver function during and after HCC treatment, survey for cancer recurrence and manage its risk factors, and prevent and treat decompensating events. We highlight the need for a team-based holistic approach to the patient with liver disease and HCC and identify necessary gaps in current care and knowledge.
Keywords: Hepatocellular carcinoma, holistic approach, hepatologist, chronic liver disease, cirrhosis, prevention
Introduction
Hepatocellular carcinoma (HCC), a common and dreaded consequence of liver disease, leads to significant morbidity and mortality worldwide. HCC develops in one-third of patients with cirrhosis, accounts for 80–90% of all primary liver cancers, and is currently the fifth most common cancer worldwide and the third most common cause of cancer-related mortality [1], [2]. In addition to its increasing incidence, there has been a 43% increase in deaths from HCC in the United States between 2000–2016, and the World Health Organization (WHO) predicts over 1 million deaths from liver cancer by 2025 [1]. Current five-year survival for HCC is only 18%, making it the second most lethal cancer [3], [4].
The worldwide increase in HCC incidence is a consequence of several epidemics, all of which are preventable and treatable. Globally, 257 million people are affected by chronic hepatitis B (CHB) and 58 million by chronic hepatitis C (CHC) infection [5], while 280–370 million people suffer from alcohol-use disorder with alcohol-associated liver disease (ALD) affecting 71 million people globally [6]. Obesity and diabetes, the major risk factors for the development of nonalcoholic fatty liver disease (NAFLD, also referred to as metabolic associated fatty liver disease - MAFLD), affect 650 and 578 million people, respectively, with a precipitously rising incidence [7], [8]. These epidemics, coupled with deepening inequities in health care, threaten large sectors of the population with poor access to care, regardless of national wealth per capita.
Management of HCC requires a strong multidisciplinary team, generally consisting of hepatologists with expertise in primary liver cancer and liver transplantation; surgeons with training in transplant, hepatobiliary surgery or surgical oncology; interventional radiologists; diagnostic radiologists; medical oncologists; radiation oncologists; pathologists; palliative care physicians; primary care physicians; psychologists; social workers; nutritionists; nurse navigators; and tumor registrars. The core elements that currently impact staging and treatment options for patients with HCC are based on tumor characteristics (size, location, presence of metastases), specific liver-related risk factors, liver function, and performance status.
We seek to delineate the need for a holistic and team-based approach to the patient with liver disease and hepatocellular carcinoma. The primary providers caring for patients with liver disease and HCC vary by country, ranging from general internal medicine providers to hepatologists trained in advanced liver disease and hepato-oncology. Clinical hepatologists are physicians or advanced providers, who, independently from their primary specialty, spend most of their professional time caring for patients affected by diseases of the liver. Managing patients with HCC and their co-existing liver disease is complex and includes optimizing liver function; evaluating and treating the underlying etiology of liver disease; preventing further hepatotoxicity; managing liver disease decompensation both before and after treatment; assessing eligibility for liver transplantation; and coordinating care among various providers. Therefore, we recommend that hepatologists who are trained in the diagnosis and management of advanced liver disease and liver transplantation and well-versed in all HCC treatment options and their adverse effects and toxicities serve a central role in the backbone of this complex care. These tasks are critical for achieving the best patient outcomes (Figure 1, Table 1). We also strongly emphasize the role of multidisciplinary meetings. We also note the shifting landscape in the etiologies of liver disease, namely NAFLD, and thus recognize the essential expertise of our primary care colleagues, endocrinologists and cardiologists in managing the various metabolic comorbidities and cardiovascular diseases. We also review the evaluation and management process for patients with liver disease and HCC with an emphasis on prevention and treatment strategies.
Figure 1:
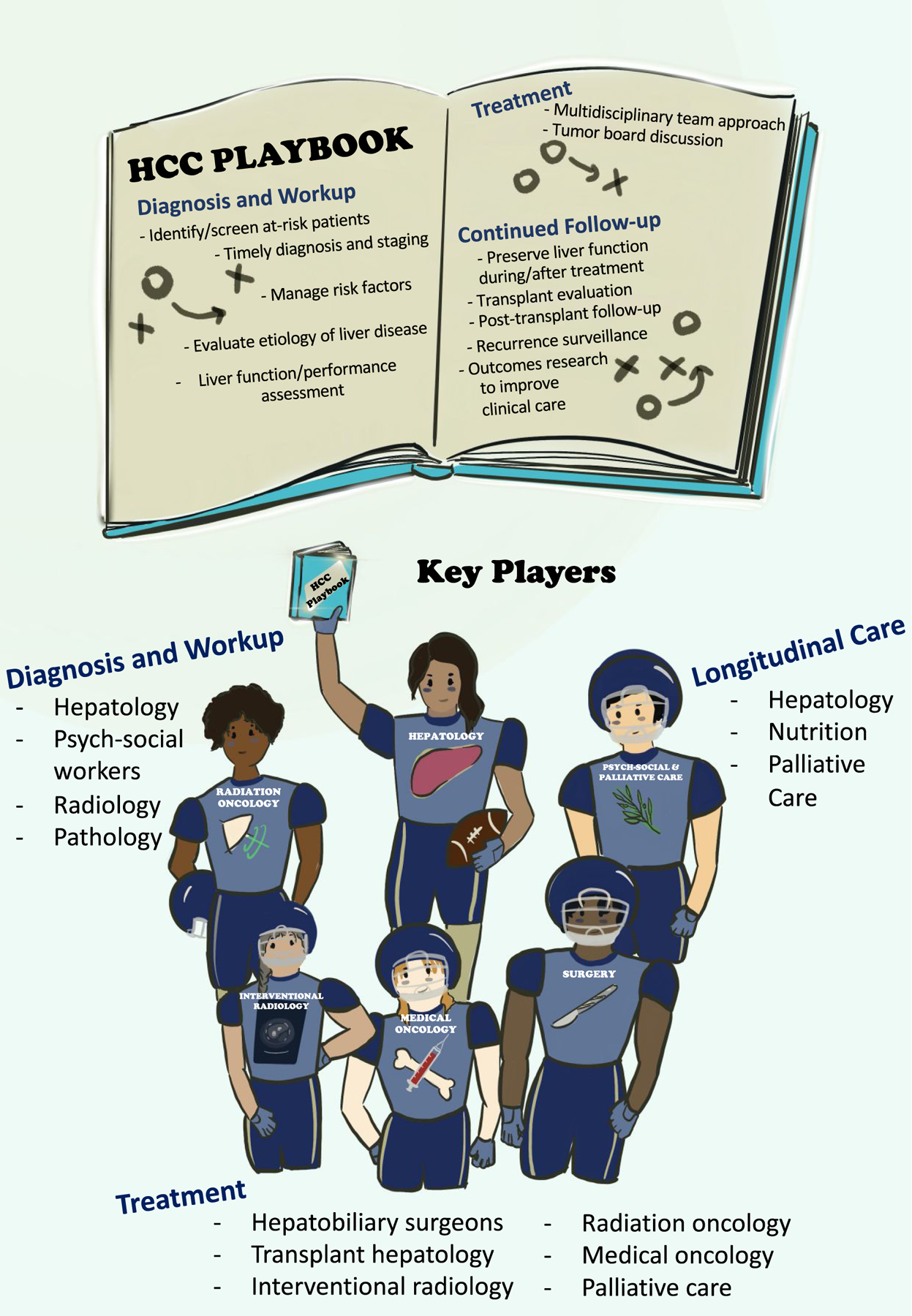
In this figure, we emphasize the central role of the hepatologist in managing patients with hepatocellular carcinoma (HCC) and highlight the primary providers associated with each stage of care. Hepatologists are specialized providers well versed in the understanding and treatment of various forms of chronic liver disease which often coexist and precede the develop of HCC. They are therefore essential to identify high-risk patients to ensure surveillance protocols are implemented to aide in early detection of HCC. Additionally, thorough assessment of risk factors and etiologies of underlying liver disease is imperative, as the majority are either preventable or treatable. Once diagnosed with HCC, hepatologists should work promptly to stage patients and evaluate their underlying liver function and performance status which are critical elements in assessing treatment candidacy. We denote the importance of an integrated, multidisciplinary team approach when it comes to discussing treatment of these complex patients and recommend care management in tertiary centers with experienced providers when possible. After treatment has been implemented, hepatologists are key players for longitudinal care to help manage complications of liver disease, assess for disease recurrence, evaluate for transplant candidacy, and integrate palliative care services when necessary.
Table 1.
Holistic approach to the patient with hepatocellular carcinoma
| ‐ Preventative measures to promote “liver health” at all levels: “to inform is to cure” |
| ‐ Recognition of subjects with risk factors for liver disease and aggressive management |
| ‐ Assessment and management of social determinants of health and removal of barriers to care |
| ‐ Early treatment of liver disease to prevent chronicity |
| ‐ Preservation of liver function in patient with cirrhosis and chemoprevention of progression |
| ‐ Oncologic surveillance of patients at risk |
| ‐ Diagnosis of liver cancer and treatment strategy |
| ‐ Team-based multimodal treatment with personalization of care |
| ‐ Establishment of a treatment strategy going beyond the single episode |
| ‐ Management and treatment of comorbidities |
| ‐ Evaluation of potential candidacy for liver transplant |
| ‐ Post-treatment oncologic surveillance |
| ‐ Retreatment of recurrence as needed and feasible, again through a team-based approach |
| ‐ Identifying the transition time to palliative care and participation in palliative care delivery |
Search Strategy for References:
A search of PubMed (https://pubmed.ncbi.nlm.nih.gov) was conducted with the search terms “hepatocellular carcinoma”, “prevention”, “treatment”, and “hepatology” from 2000 until 2021. Papers were also identified through searches of the authors’ own files. Only papers published in English were reviewed. The final reference list was generated on the basis of originality and relevance to the broad scope of this narrative review.
Primary and Secondary Prevention of Hepatocellular Carcinoma
CHB and CHC infections continue to be the major cause of chronic liver disease worldwide. However, in developed countries ALD and NAFLD incidence are on the rise and have become the most relevant risk factors for the development of HCC [2], [9], [10]. These diseases also result in an additional risk effect in patients with chronic viral infection or other known genetic etiologies of chronic liver disease. It has become increasingly more challenging to stratify patients into a distinct liver disease etiology given the presence of multiple comorbid conditions, and therefore a thoughtful and comprehensive evaluation of all possible contributing risk factors is important when evaluating patients with liver disease.
Oncologic surveillance
HCC surveillance protocols are recommended for patients with either known liver disease or known risk factors. One area of controversy is screening for patients with underlying NAFLD/NASH without cirrhosis. Analyses have shown that given the annual HCC incidence rate of <1.5% per year, HCC surveillance in this population is not cost-effective [2], [11], [12]. However, given the ongoing growth in the obesity epidemic with subsequent rise in NAFLD incidence, along with the rising incidence of HCC in NAFLD patients without cirrhosis [13], changes in surveillance guidelines for certain high-risk populations are likely to follow. As discussed by Plaz Torres et al., in NAFLD patients without cirrhosis, advanced fibrosis, diabetes, obesity, older age, male gender, genetic predisposition, and Hispanic ethnicity were significant risk factors for HCC [14], [15]. Future models are needed that account for all known risk factors, including demographics, co-morbidities, environmental factors (air pollution/diet), fibrosis stage, medications, serologic tests, and genetic polymorphisms [16].
It is imperative to start assessing liver cancer risk on an individual basis, as current surveillance guidelines often filter patients into singular categories when, in fact, many patients are affected with multiple comorbidities that lead to liver disease and cancer. For example, studies evaluating liver cancer risk in HCV patients who have successfully achieved sustained virologic response (SVR) have shown that certain comorbid conditions, including diabetes and obesity, are independent risk factors for future development of HCC [17], [18], [19]. Thus, it is essential that hepatologists assess patients holistically when making decisions on the appropriateness and necessity for HCC surveillance.
Unfortunately, despite clear evidence that HCC surveillance is associated with early detection and improved long-term survival, mainly due to a higher rate of treatment with curative approach [20], adherence is low even in high-risk patient populations. Patient factors associated with poor HCC surveillance include poor access to medical care, higher prevalence of comorbidities, etiology of liver disease, and less favorable socioeconomic status [21]. There is also higher prevalence of HCC and disproportionately lower rates of HCC surveillance in non-White ethnic minorities [22]. A recent meta-analysis of surveillance practices in patients with cirrhosis noted surveillance rates of less than 25%, with a significant improvement in surveillance for patients followed by subspecialists [20]. Additional studies have also supported that referral to a hepatologist is associated not only with improved rates of surveillance, but also with improved survival (Table 2) [21, 23–27].
Table 2.
Benefit of Hepatologist Care for Management of HCC
| Study | Study Period | Country | Study population | HCC Outcomes |
|---|---|---|---|---|
| Davila et al | 1994–2002 | United States | 1,873 adults with HCC from the SEER database | HCC surveillance with GI/hepatologist vs. PMD care (OR 2.8, 95% CI 1.73–4.53) |
| Dirchwolf et al | October 2018-October 2019 | Argentina | 301 patients with HCC diagnosis and known risk factors (advanced fibrosis/cirrhosis or chronic hepatitis B with Page-B score ≥10 points) | 98.2% 0f cohort followed by hepatologist underwent surveillance (p<0.001) |
| Serper et al | January 2008 – December 2010 | United States | 3,988 patients from Veterans Administration (128 centers) | Hepatology care within 30-days of HCC diagnosis reduced mortality (HR 0.70; 95% CI 0.63–0.78) |
| Tapper et al | 2001–2015 | United States | 389,257 adults with cirrhosis from Optum database | Hepatology care reduced mortality (0.78 [0.75, 0.80]) |
| Yeo et al | 2007–2016 | United States | 82,427 adults with cirrhosis from Truven Health MarketScan Research Database | HCC surveillance with PMD vs. GI/ID care (OR 0.48, 95% CI 0.46–0.52) |
| Marquardt et al | 2011–2019 | United States | Database of 1.1014 patients with cirrhosis and HCC from Parkland Health and Hospital System and University of Texas Southwestern Medical Center | Risk os screening within 1 year of HCC diagnosis if care provided by GI vs. PCP (OR 12; 95% CI 4.74–30.6) vs. GI+PCP (OR 11.8; 95% CI 4.89–28.5) |
Studies evaluating primary care physician practices note that low rates of HCC surveillance may be due to lack of knowledge of current recommendations or the benefits of surveillance, presence of concerns about the cost of surveillance and inability to effectively communicate with patients about reasons for HCC surveillance, and lastly to the perception that there are more important issues to manage during clinic visits [28]. A particularly interesting challenge for primary care physicians may be the timing of referral for patients with NAFLD to a hepatologist given the ongoing rise in this condition and the susceptibility to HCC in this population. A recent review suggested that patients with diabetes and NAFLD should undergo baseline liver function testing and ultrasonography. It is important to note, however, that in patients with risk factors for NAFLD, a negative ultrasound should not rule out the diagnosis of NAFLD as hepatic fat decreases as hepatic fibrosis increases [29]. Referral to a hepatologist is advised for patients with elevated ALT/AST. If steatosis is noted on ultrasound, non-invasive markers of fibrosis should further stratify patients, and if there are findings of intermediate or advanced fibrosis (FIB-4 ≥ 1.3 or Liver Stiffness Measurement >8kPa), these patients should also be referred to specialty care with hepatology [30]. Additionally, in a joint clinical guideline put out by the European Association for the Study of the Liver, the European Association for the Study of Diabetes and the European Association for the Study of Obesity, for patients with hepatic steatosis and elevated liver chemistries for which significant fibrosis cannot be ruled out, referral to a hepatologist is advised as the next step to aid in assessment of other liver diseases, help gauge disease severity, and make decisions on need for invasive testing such as liver biopsy [31].
Diagnosis of Hepatocellular Carcinoma
HCC is unique in that it is the only clinically significant malignant tumor that does not require histologic examination to establish a diagnosis in patients with known liver cirrhosis and characteristic imaging findings. Diagnosis of HCC in patients with liver cirrhosis has thus been primarily made through non-invasive, contrast-enhanced, multi-phased cross-sectional imaging. The American College of Radiology published guidelines, the Liver Imaging Reporting and Data system (LI-RADS), on how to perform imaging and interpret liver lesions on cross-sectional scans [32]. The distinct vascular pattern that occurs during hepatic carcinogenesis makes this system possible. However, the accuracy of diagnostic imaging depends on the pre-test probability of the disease and thus LI-RADS staging is only validated for patients with cirrhosis. In patients without cirrhosis and those with certain vascular forms of portal hypertension and congenital hepatic fibrosis, HCC diagnosis cannot be made non-invasively and confirmatory biopsy is required [11], [2].
Additionally, although LI-RADS 5 lesions are diagnostic of HCC, biopsy should still be considered for prognostic and therapeutic information. For example, certain histologic findings may help with prognostication, including histotype and grade of differentiation, presence of neurovascular and lymphatic involvement, and expression of certain phenotypic markers. For example, macrotrabecolar massive histotype has a worse prognosis compared to the lymphocyte-rich histotype.
Histologic findings may play a major role in defining more aggressive tumors, which can guide early transplant referral and possible initiation of adjuvant systemic therapies. Even though a single driver mutation leading to oncogenesis in HCC has not been identified, multiple studies have shown that a significant portion of HCCs may have genetic alterations identified via sequencing platforms that could be targeted by drugs currently approved by the FDA [33], [34]. For example, one study found that mutations that activated the PI3K-mTOR pathway were associated with poor outcomes in sorafenib-treated patients, and the mutations predicted to activate the WNT pathway were associated with innate resistance to immune checkpoint inhibitors [35]. Further, patients who are immune checkpoint inhibitor non responders often harbor NT/β-catenin mutations (i.e., immune-cold tumors), and may instead respond to lenvatinib treatment as these types of HCCs have a high FGFR4 expression [36]. Further studies are needed, but these early findings suggest the utility of genomic profiling of tumors to guide treatment decisions [34].
Advancements in systemic therapeutic options and multiple ongoing biomarker-driven studies may ultimately make tissue sampling of all imaging-confirmed HCCs the standard of care. Additionally, appropriate diagnosis of other primary liver cancers such as cholangiocarcinoma or mixed hepato-cholangiocarcinoma (cHCC-CCA) often requires tissue confirmation. For example, mass forming intrahepatic cholangiocarcinoma (ICCA) is the most common subtype of ICCA and can often present with similar radiographic characteristics to HCC, including arterial enhancement and washout. Lack of tissue confirmation leads to misdiagnosis and inappropriate treatment in these cases [37]. Combined hepato-cholangiocarcinoma is a very rare (0.75% of all primary liver cancers) heterogenous tumor with a significantly worse prognosis compared to HCC alone. There are no clear validated treatments, either locoregional or systemic for cHCC-CCA, however the mainstay of treatment is resection whenever feasible [38]. Radiographic diagnosis alone can misclassify cHCC-CCA as HCC in up to 54% of cases, and studies have shown that the combination of imaging with biopsy can improve sensitivity and specificity up to 60% and 82%, respectively [39]. Interestingly, a recent multi-center analysis found superior outcomes for liver transplantation over resection, regardless of tumor burden in patients with cHCC-CCA, and in patients within Milan criteria, overall survival was similar to patients with HCC alone [40]. Though this is a single study with need for further prospective trials to confirm the findings, these results emphasize the need for appropriate diagnosis to guide optimal treatment strategies.
Overall, given the aforementioned information, it is reasonable to conclude that a liver biopsy might be routinely performed not only in masses with atypical features, but also in all patients with imaging concerning for LI-RADS 4 and 5 lesions, whenever feasible and safe.
“Liquid biopsy” entails the analysis of tumor components that have been released into the bloodstream or other bodily fluids. These components include circulating tumor cells, methylated nucleic acids (cell-free DNA and RNA), and extracellular vesicles [41], [42]. This area holds great promise for the early detection of HCC, prediction of treatment response, and assessment of resistance patterns and clonal tumor evolution [42]. It may serve of particular importance in assessing treatment response in patients on systemic therapy to avoid unnecessary toxicity in those unlikely to respond. To date, there are a variety of trials investigating methylation profiling from plasma DNA and mutations in circulating tumor DNA for early detection of HCC along with comparative trials using liquid biomarkers against standard surveillance (ultrasound +/− AFP) [43]. Given the ease and simplicity of obtaining samples, the implementation of liquid biopsy could markedly increase adherence to surveillance in high-risk populations.
Another important facet of care during the diagnostic stage of this disease is the recognition of the significant psychological burden placed upon our patients. Graf et al. recently published a systematic review assessing the extent of psychological burden on patients suffering from hepatobiliary cancers and found that a substantial percentage of patients suffer from depressive symptoms, anxiety, and reduced health-related quality of life in almost all areas. They found that psycho-oncological intervention was associated with increased survival rate, potentially related to reduced stress and improvement in immune function, as well as more proactive health behaviors and increased compliance during follow-up [44]. This highlights the importance of early involvement and referral to psychology and social work specialists.
Staging of Hepatocellular Carcinoma
There are a variety of staging systems that have been proposed for HCC [45]. None of these systems are universally accepted, but the one that is most widely utilized is the Barcelona Clinic Liver Cancer (BCLC) system which has been validated in European, American, and Asian populations. The BCLC staging system has passed the test of time and has proven to be very helpful as it considers not only tumor burden, but also underlying liver function and patient performance status, and is able to provide treatment recommendations based on prognostic subclasses [46].
However, as new treatment paradigms evolve, there are increasingly gray areas. For example, studies show that in selected patients, indication for surgical resection may be expanded beyond BCLC recommendations [47]. There is controversy surrounding the treatment of intermediate and advanced stage (BCLC Stage B and C) patients, as these stages encompass a very heterogenous population with a wide range of outcomes after treatment, suggesting that subclassification is urgently needed for better treatment guidance [48]. There have been a multitude of proposed subclassifications for Stage B and Stage C patients to better prognosticate and guide treatment decisions [46],[49].
For Stage C patient subclassification, the extent of vascular invasion, degree of extrahepatic spread (regional lymph nodes versus distal metastases), and performance status have been used to improve prognostication. BCLC stage C patients represent a heterogeneous population, where stage determinants (i.e. macrovascular invasion, extra-hepatic spread, and performance Status >1) have different prognostic meaning, and where even extent of macro-vascular invasion identifies two sub-populations with different potential therapeutic approach and survival [50]. Notably, studies have found excellent outcomes with the use of curative therapies, including surgical resection, in those patients with minimal vascular invasion limited to subsegmental branches [48]. Transarterial radioembolization (TARE) and transarterial chemoembolization (TACE) may also be effective in some of these cases [51]. Additionally, with advancements in systemic therapies, namely immunotherapy, various clinical trials are evaluating the efficacy of combining locoregional techniques with systemic treatments and the utility of immunotherapy in the adjuvant setting [52].
There are also concerns that the CTP score may not be ideal for assessing liver function because of provider subjectivity when assessing severity of ascites and encephalopathy. The albumin-bilirubin score (ALBI) has been proposed as a better and more objective scoring method and has now been incorporated into the most recent update of the BCLC staging system [46], [53]. For these reasons, it is quite common for treatment decisions to veer from current guidelines. For example, one study by Alahmadi et al. evaluated compliance with current AASLD guidelines and found that only about 50% of an institution’s multidisciplinary tumor board recommendations were actually adherent to guidelines [54]. This sheds light on the complexity involved in treatment decisions and again enforces the vital role of a hepatologist in thoroughly evaluating and optimizing patients’ liver function and performance status to facilitate the best treatment approaches. In real life, the BCLC staging system is an important guiding principle, but treatment allocation should be decided during multidisciplinary tumor board conferences, as there is compelling evidence from clinical practice that a multidisciplinary evaluation of patients may lead to therapeutic decisions different from those identified in the BCLC algorithm [55].
In response, the BCLC staging system was recently revised (2022 update) and now addresses prior shortcomings, including further subclassification of BCLC Stage B patients according to tumor burden and liver function, with clarification of both liver function and performance status. Liver function in compensated patients is now further stratified by ALBI scores along with AFP, whereas performance status is now defined as being related to symptoms from malignancy, not pre-existing comorbidities. Treatment decisions are also further expanded into a “Treatment Stage Migration” section in which a patient’s clinical profile may shift them to receive therapy for more advanced stages of liver cancer and an “Untreatable Progression” section in which patients remain in their initial BCLC stages but have failed therapy and thus should consider therapies corresponding to more advanced stages. The latter two sections again highlight the importance of individualized patient evaluation [46].
Tumor Board Discussion and Multidisciplinary Treatment Options of Hepatocellular Carcinoma
The treatment of HCC involves a multidisciplinary discussion, and it has been shown that this collaborative approach to disease management leads to improved survival in patients with HCC [56]. Studies have also found that the use of a multidisciplinary approach increases patient referrals for treatment, increases both curative and palliative treatments, and improves both patient and team member experiences [57], [58]. There is evidence that survival is increased in patients whose therapeutic decisions are discussed in a multidisciplinary tumor board (MTB), and this evidence is generated increasingly by studies in which the minority of patients received BCLC stage-concordant treatment [59]. Once again, these findings highlight how the hepatologist should play a role in identifying more subtle clinical nuances that may deviate from the proposed treatment algorithms and introduce the concept of treatment selection according to therapeutic hierarchy rather than stage hierarchy [60].
Given the complexity of this disease and the growing variety of treatment options, patients with HCC should be evaluated in a multidisciplinary care center with experienced, specialized physicians. Hepatologists play a vital role during multidisciplinary discussions, as they offer unbiased care options given their indirect role in oncologic treatment. They also are well-versed in understanding their patients’ liver function and performance status which again plays a critical role in decision making. They can also identify active risk factors for HCC recurrence and liver disease progression which may impart important clinical decision making such as early referral for liver transplant evaluation. Most patients will undergo sequential treatments with different approaches during their disease course due to changes in tumor characteristics and underlying liver function. Hepatologists are critical for longitudinal care to best represent the holistic patient profile.
Curative Therapies for Hepatocellular Carcinoma
Curative options remain focused on liver transplantation, surgical resection, and ablative techniques. In patients with early-stage disease, surgical resection is ideal if tumor burden is segmentally localized and if the patient has stable liver function and performance status without evidence of clinically significant portal hypertension (CSPH), defined as a hepatic vein pressure gradient (HVPG)>10mmHg. For the most accurate assessment of portal hypertension, HVPG measurements can be done to stratify more precisely those that may be high risk for surgery [61]. Non-invasive markers, including bilirubin > 1mg/dL and platelet count of ≤100,000/mL, have also been suggested by EASL and AASLD as surrogate markers of portal hypertension. Studies have shown that in experienced centers, patients with moderate portal hypertension have competitive survival outcomes, and thus a variety of factors including liver function, tumor size, and required extent of hepatectomy must also be accounted for prior to excluding a patient from resection [62]. The increasing use of minimally invasive surgery has further expanded surgical indications. In a recent editorial by Romagnoli et al., patients were considered ideal candidates for surgical resection if they were ≤75 years of age with excellent performance status (ECOG 0), minimal medical comorbidities, a single tumor ≥3cm in size located peripherally or exophytically without vascular invasion, and no evidence of cirrhosis or portal hypertension. Ablation alone or as a bridge to liver transplantation is favored in patients with cirrhosis, especially if portal hypertension is present [63]. It is worth noting that the majority of trials comparing resection and ablation were based out of East Asia where the majority of patients had chronic hepatitis B, many of whom were non-cirrhotic. It is hard to generalize those findings in the Western world where many patients have NAFLD and operative risk is substantially higher due to added cardiovascular risk factors such as obesity, diabetes, and hyperlipidemia. It has been suggested that for very early stage disease (tumor size <2cm), ablation provides similar outcomes to resection while remaining more cost effective [64], and thus can be considered first line therapy [2].
With advances in interventional techniques, including the use of portal vein embolization as a means of inducing hypertrophy in the future liver remnant (FLR), liver resection can now be offered to a wider range of patients and can improve survival after a major hepatectomy [65]. Another technique that can be used for a similar purpose is lobar TARE, which simultaneously treats the tumor and leads to hypertrophy of the FLR [66]. The use of liver resection in patients with tumor thrombus is another method under investigation. One study from the Liver Cancer Study Group of Japan demonstrated that surgical resection offered better survival outcomes compared to non-surgical treatment when the tumor thrombus was limited to the first-order branch of the portal vein (PV1) [67]. However, due to lack of direct comparisons of resection and systemic treatments, the benefit of this approach remains unclear [2]. Of note, the 5-year recurrence rate following resection remains high at 70%, thus surveillance must continue. Liver transplant is the preferred treatment option for patients with more advanced liver disease or with clinically significant portal hypertension for whom surgical resection would be too high risk. This topic will be discussed further.
Non-Curative Loco-Regional and Systemic Therapies
Non-curative, or palliative treatment options for HCC include TACE, TARE, and stereotactic body radiation therapy (SBRT). Major societies do not recommend one form of locoregional therapy over others, and often the decisions are made based on tumor location and experience and expertise of each center. Often, they are used sequentially, after thorough discussion at MTB.
Systemic therapy is perhaps the most exciting emerging topic in the field of HCC. After a decade of negative clinical trials, several new drugs have surfaced with clinical efficacy for the treatment of HCC. The tyrosine kinase inhibitors (TKIs) sorafenib and lenvatinib were the agents approved initially for first line treatment, however as of May 2020, the combination of atezolizumab (PD-L1 inhibitor) with bevacizumab (VEGF inhibitor) was found to increase survival significantly compared to sorafenib (HR 0.58, 95% CI 0.42–0.79, p<0·001) [68]. This combination is advised as first line, unless contraindicated, in which case, either of the two first line TKIs may be considered. Given the risk of GI bleeding with bevacizumab, upper endoscopy is currently advised by the American Society of Clinical Oncology [69] to evaluate variceal status as a prerequisite for this new first line combination. It is important to emphasize that the presence of varices indicates the presence of CSPH and more advanced liver disease, independent of the presence of HCC, and these patients require a hepatologist’s attention due to the risk of hepatic decompensation. Maintenance of liver function is essential to maintain eligibility for antitumor treatments that will prolong overall survival. Second line agents include the TKIs regorafenib and cabozantinib, the VEGF-inhibitor ramucirumab (if AFP is >400ng/dL), and immune checkpoint inhibitors nivolumab or pembrolizumab. The HIMALAYA trial, a phase 3 randomized, open-label, multicenter study using a single priming dose of the CTLA-4 inhibitor tremelimumab in combination with a PD-L1 inhibitor durvalumab, showed superior overall survival (HR 0.78; 96% CI, 0.65–0.92; p=0.0035) and favorable benefit-risk profile compared to sorafenib and is currently pending FDA approval as a novel, first-line therapy [70].
Patient Selection and Side Effects of Therapy:
Currently, the BCLC 2022 guidelines recommend systemic therapy for patients with advanced stage (BCLC C) disease, patients with intermediate (BCLC B) disease with diffuse, infiltrative, extensive bi-lobar involvement, or patients that either do not respond to locoregional therapy or are not candidates for locoregional therapy and thus fall into the treatment stage migration category [46]. Use of systemic therapy as either adjuvant or neoadjuvant treatment will be discussed in the next section.
While we note that most therapies are approved for well compensated (CTP A) disease, a recent multi-center study on the safety of atezolizumab and bevacizumab in patients with impaired liver function (CTP B status) demonstrated tolerability in this population and also demonstrated there was no correlation between the presence of varices at pre-treatment endoscopy and the development of bleeding [71]. It is important to note that the initial phase III trial excluded patients with history of autoimmune disease, immune deficiency, significant cardiovascular disease within 3 months of the study treatment, untreated or incompletely treated varices, history of malignancy (other than HCC) within 5 years, co-infection of hepatitis B and C (HBV and HCV), and poorly controlled hypertension, among others. Thus, special attention needs to be given when considering use of these medications in patients with any of these conditions.
Adverse effects (AEs) of TKIs, including hand-foot syndrome (also known as palmar-plantar erythrodysesthesia), are most often seen with the use of regorafenib, affecting up to 53% of patients. This results in altered sensation, stiffness, pain, erythema, and hyperkeratosis and can be treated with emollients, topical corticosteroids and ultimately dose reduction or drug cessation in severe circumstances. Additional AEs include diarrhea, hypertension, fatigue, nausea/vomiting, and increased risk of bleeding [72]. AEs of immunotherapy tend to be dose dependent for CTLA-4 inhibitors but not for PD-1 or PD-L1 inhibitors. The most common target organs associated with immune-related AEs (irAEs) include the skin, GI tract, endocrine glands, and the liver at 44%, 35%, 6% and 5%, respectively. Documented symptoms include rash, pruritus, diarrhea, appetite changes, hepatitis, colitis, hypophysitis, fatigue, asthenia, thyroid issues, dry mouth, arthralgias, adrenal insufficiency, edema, constipation, pneumonitis, hypertension, pyrexia, infusion reaction, epistaxis, alopecia, and palmar-plantar erythrodysesthesia. An additional risk is also the reactivation of HBV and thus effective antiviral therapy before and during ICI treatment is recommended. For skin reactions, treatment generally consists of topical steroids and anti-histamines for mild grade 1–2 reactions to intravenous steroids for higher grade or life-threatening toxicities. GI toxicities vary from diarrhea to life-threatening colitis with potential for perforation and peritonitis. Grading of colitis requires endoscopic evaluation, and treatment varies from systemic corticosteroids to other immunosuppressive therapies, including anti-TNF treatments such as infliximab. Liver toxicities are graded as follows: grade 1 (AST/ALT ≤3× ULN), grade 2 (AST/ALT 3–5× ULN), grade 3 (ALT/AST 5–20× ULN) and grade 4 (ALT/AST>20× ULN). Histologically there is pan-lobular hepatitis and bile duct injury, central vein endotheliitis and sinusoidal lymphohistiocytic infiltrates. Treatment consists of steroid therapy and withdrawal of treatment for grade 2 toxicity or higher. More severe cases may require addition of other immunosuppressive agents, including mycophenolate mofetil (MMF), azathioprine, cyclosporine, tacrolimus, anti-thymocyte globulin, tocilizumab and plasma exchange. Thyroid dysfunction does not generally require stopping therapy but focuses on treatment of hypothyroidism with thyroid supplementation and/or use of beta-blockers for management of symptomatic hyperthyroidism. For treatment of more rare irAEs, including pneumonitis, myocarditis, neurologic complications including myasthenia gravis or Guillain-Barre syndrome, the mainstay of therapy is again corticosteroids with the possible addition of stronger immunosuppressants, including anti-TNF therapy, anti-thymocyte globulin, MMF, intravenous immunoglobulin, or plasma exchange [73]. Given the complexity and range of significant adverse effects associated with new lines of therapy, we also encourage multidisciplinary discussions between providers for appropriate diagnosis and management. As outlined by Londoño et al, developing a coordinated strategy through multidisciplinary efforts involving health professionals specialized in each organ system involved can help to not only understand the pathogenesis of these irAEs, but also assure the best personalized care [74].
While TKIs have been shown to be safe and effective in the post-transplant setting, further understanding of the risks of immunotherapy and organ rejection is required before this therapy will be accepted in in the post-transplant setting. It should be noted that there are case reports of successful treatment with immunotherapy in the post-transplant setting [75], albeit with a high incidence of rejection. While the use of immunotherapy in the post-transplant setting remains controversial, there has been more focus on the safety of these therapies as down-staging techniques in potential liver transplant recipients, especially as HCC is the indication for 20% of transplants performed in the United States. The majority of evidence is from small case series and case reports but has overall demonstrated that with an appropriate washout period these classes of medications do not result in increased risk of rejection in the post-transplant setting [76], [77]. Given the favorable reports thus far, the National Liver Review Board recently updated its guidance to support immunotherapy as a down-staging or bridging therapy and in their recent policy update endorsed this treatment does not preclude consideration for HCC exception points[78]. We anticipate future randomized clinical trials assessing this topic [79].
Systemic therapy is most often prescribed by medical oncologists, but disciplines of prescribing physicians vary between institutions and countries. One large retrospective study by Kaplan et al. looked at non-oncologist compared to oncologist prescribers of sorafenib and found similar survival outcomes in patients with HCC, suggesting that physicians with expertise in the management of HCC can safely and effectively administer systemic therapy [80]. Ultimately, which providers will prescribe systemic therapy for HCC will be based on provider comfort, expertise, and institutional organization and support. Evidence is also accumulating of possible differential responses to systemic treatment based on the etiologies of liver disease [81], further emphasizing the need for a thorough and expert assessment of liver disease in these patients.
Combination and Adjuvant Therapy
The combined use of various systemic agents and adjuvant systemic therapies after either surgical or locoregional therapies are areas of intense research. Prior evidence has shown no survival benefit with adjuvant systemic therapy, and currently EASL and AASLD do not recommend the use of adjuvant therapy following successful resection or ablation [82], [2]. Studies that have looked at adjuvant systemic therapy after non-curative locoregional treatments in cases of intermediate stage HCC have not met their primary endpoints [83]. However, it should be noted that only sorafenib has been studied as adjuvant therapy and there are over 25 phase 3 trials currently underway evaluating optimal combinations of other medications – we eagerly await these results [79], [52].
Liver Transplantation
Transplant is considered a curative therapy for unresectable HCC and is often the first line treatment in those with more advanced liver disease or those in whom surgical resection would be too high risk. The decision as to which patients would make ideal transplant candidates is complex and requires a multidisciplinary discussion. Various factors must be meticulously reviewed, including underlying liver function, medical comorbidities, tumor burden, and risk factors for HCC recurrence. There are some patients with compensated liver disease who are ultimately well controlled with locoregional treatments, and as liver transplantation is not without risks and associated morbidity, we again emphasize the need for appropriate evaluation of risks and benefits when considering transplant candidacy.
Indications for transplant and priority assigned during disease progression is a moving target and varies by country. In the US, a patient considered for liver transplant must fall within Milan (United Network for Organ Sharing, UNOS T2) criteria, meaning one tumor ≤5cm, or up to three tumors, none >3cm. If the tumor burden exceeds these criteria, the patient can be down-staged with treatment and, if successful, the patient may qualify for MELD exception points if they meet down-staging criteria (one tumor >5cm and ≤8cm; two or three tumors each >3cm and ≤5cm with total tumor diameter of ≤8cm; OR four or five lesions each <3cm and total tumor diameter of ≤8cm). If the patient has exceeded these downstaging criteria, the center can appeal to the National Liver Review Board (NLRB) to be listed with MELD exception points after successful downstaging. It is worth noting that a common challenge faced by potential transplant candidates is very early HCC (one tumor that is <2cm in size, UNOS T1 criteria), as this does not qualify for MELD exception points. From an oncologic point of view, cancers should be treated earlier, and no randomized trials exist comparing observation versus immediate treatment for T1 lesions. The AASLD currently recommends observation for T1 HCC in patients with cirrhosis, but the risks and benefits of delaying treatment in patients with otherwise preserved liver function must be discussed at length with the patient. Additionally, in liver transplant candidates within Milan criteria, bridging treatment of HCC is advised to prevent progression and subsequent dropout from the waiting list [11]. It must be noted that about 50% of patients referred for transplant are ultimately deemed ineligible, and of those listed, about 20% will die or be delisted while waiting for a transplant. Thus, hepatologists must work closely with these patients to control the HCC with bridging therapies and to manage their underlying liver disease to optimize their chances of successful liver transplantation [84].
In 2020, the Scientific Registry of Transplant Recipients noted that 10.9% of new waiting list registrations were in patients with a primary diagnosis of HCC. HCC remains the third most common cause for transplant but has declined further to only 12.6% likely reflecting ongoing effects from the policy change implemented by UNOS in 2015 to reduce disparity in organ access between HCC and non-HCC patients and to improve geographic variation in transplant rates for those listed with HCC. Given the delay in acquiring exception points, early identification of potential transplant candidates is of critical importance [85]. For example, one study that compared time from the first diagnosis of HCC to liver transplant noted a 60% increased risk in HCC recurrence at 5-years post-transplant when wait times exceeded 18 months [86]. Most recently and effective as of July 26, 2022, the NLRB made a change to their policy to note that patients who initially had T2 disease treated with either resection or locoregional therapy who developed a new T1 or T2 lesion more than 6 months, but less than 60 months following treatment, and for whom a transplant program is requesting an initial exception are eligible to receive MELD score exception without a 6-month delay period. We thus anticipate changes in the percentage of patients undergoing liver transplant for HCC-related indications in the future [87].
Post-treatment Care and Recurrence
Care of patients with HCC should not be limited to the treatment of the tumor(s). Patients must continue to follow closely with their hepatologists during and after HCC treatment given the risk of hepatic decompensation, their most important competing risk of death. Hepatic decompensation is the major driver of mortality in patients with HCV and successfully treated early HCC, once again highlighting how long-term preservation of liver function results in lower HCC-related mortality [88]. Furthermore, surveillance for HCC recurrence is essential to ensure early identification so that patients can be treated with curative intent and remain within Milan to be considered for potential liver transplantation. It is generally felt that after liver transplant, the recurrence rate is around 10–20%, while after resection and ablation the rate rises to about 70% within 5 years [11]. Most societies give loose recommendations to screen every 3 months for at least the first year after curative therapies with liver resection and ablation. Though no clear protocols exist for surveillance after liver transplant, over 70% of recurrences are observed within the first two years post-transplant with a median time to recurrence of 20.5 months. Therefore, most clinicians recommend surveillance every 3–6 months for the first 2–3 years post-transplant [89], [11]. Certain factors can help stratify those at higher risk of recurrence, including tumor size >3cm, microvascular invasion, tumor differentiation, and serum AFP. Hepatologists must closely review tumor biology and phenotype when deciding how aggressive screening strategies should be post-resection and post-transplant [90], [79]. As discussed earlier, ongoing attention to risk factor modification is an extremely important part of post-treatment care and tertiary HCC prevention as well. Although the evidence is not yet strong enough to guide practice, data from nested studies suggest that the use of aspirin, metformin, SGLT-2 inhibitors, GLP-1 agonists or statins may confer some degree of chemoprevention [91–97]. Additionally, nutritional management is essential for liver health and hepatocarcinogenesis. Maintaining a healthy BMI and avoiding diets high in simple sugars and carbohydrates to better control diabetes and HLD can prevent development and progression of NAFLD. Malnutrition and sarcopenia, which are common findings in patients with chronic liver disease, are independent negative prognostic factors in HCC. Sarcopenia can independently predict HCC-related mortality after various therapies and early recognition and intervention through nutritional support in conjunction with physical exercise can improve prognosis [98].
Palliative Care
Hepatologists must also exercise clinical judgement as to the need and timing for integrating palliative care. Palliative care reduces patient and family suffering, healthcare utilization, and improves survival in those with cancer or any life-limiting illness. It is prudent for patients and their care givers to be offered early referral to palliative care specialists. The timing of palliative care referral depends on the center expertise in managing patients with end-stage liver disease. Palliative care in HCC patients can be integrated at various stages of liver cancer, as the focus is to assist with symptom management, advance care planning, psychosocial support, and care coordination [99]. It is often a misconception that referral to palliative care is equivalent to “end of life care”, and this “stigma” should be dissolved to provide comprehensive care to our patients. Hospice services should be offered to patients at the end of life, based on clinical judgement. Hepatologists are best able to judge these needs as they closely monitor liver function, which may decline because of, or independently of HCC. For example, a recent study noted that the MELD-Na score can be used as an objective measure to identify patients with a significant risk of 6-month mortality, and a score of 28 or higher may prompt consideration of hospice to improve value-based health care in patients with no transplant options [100]. These decisions usually require multi-disciplinary discussions between treating providers but should be considered long after involving palliative care, and when the focus becomes comfort, rather than cancer treatment. Currently, EASL recommends that patients with BCLC D HCC who are not liver transplant candidates receive palliative care, including pain and nutritional support [2], [101].
Next Steps
While it is exciting that the field of HCC has started to shift dramatically, due to changes in risk factors, global prevalence, and treatment options, it also brings with it multiple areas that still need further investigation. Below is a summary of the areas in which strong evidence is still lacking and which we anticipate fluidity in clinical practice in the coming years:
Screening: The shifting paradigm in risk factors, namely the obesity epidemic, has challenged our true understanding of who to screen for HCC. Given the rise in non-cirrhotic HCC that extends beyond those with chronic viral infections, we anticipate future studies outlining those at sufficient risk to warrant surveillance. Additionally, this similar population poses challenges for optimal screening/surveillance techniques as ultrasonography poses limitations in those with central obesity. Paradigm shifts in screening, such as the use of abbreviated MRI, liquid biopsy, and/or novel biomarkers are foreseeable in the future.
Treatment: Given the novelty of immunotherapy, we still lack a true understanding as to the appropriate timeline when to initiate systemic therapy. There are many Phase 3 trials assessing the use of immunotherapy not only in unique combinations, but as adjuvant and neoadjuvant treatments in patients of all stages of disease. Additionally, it is important to note that our first line therapy is atezolizumab and bevacizumab and that future trials will need to compare outcomes not only in survival but also in safety and risk-profiles for this combination as opposed to sorafenib, which may become a more outdated therapy as time progresses. Lastly, we need further studies assessing treatment outcomes in those with NAFLD-associated HCC as our ability to generalize data mostly from Asian-based populations is challenging, and we need to continue to understand the safety of various systemic therapies in patients with impaired liver function.
Transplant: Due to changes in the OPTN/NLRB policies, HCC exception points are more challenging to obtain. We note the policy-related decline in liver transplant for the indication of HCC and the challenges inherent in setting policy with an incomplete understanding of who will successfully go on to transplant and how to best bridge patients to ensure they do not fall off the waitlist. Again, we note that based on preliminary data, immunotherapy may be safe in potential liver transplant recipients, and identifying the populations for whom wait list drop out and disease progression is highest is critical.
Conclusion
The landscape of HCC management has drastically changed in recent years and the pace of innovation is acutely accelerating. We have outlined here that it takes a team to manage patients with liver cancer, and that hepatologists remain the quarterbacks as they play a critical role in evaluating underlying liver disease, educating, and preventing further hepatic decompensation, coordinating chemopreventive strategies, determining candidacy for liver transplantation, and treating liver cancer. Treatment of liver cancer cannot be separated from treatment of the underlying liver disease. Oncologic-focused hepatologists are experts in various liver diseases as well as liver malignancies, and their intimate understanding of their patients’ underlying etiologies makes them the optimal arbiters of a tailored HCC treatment plan and a coordinated, holistic long-term management plan. Advances must be made to improve and implement surveillance of HCC in high-risk populations, with a particular focus on ethnic minorities. Improved education of both patients and providers is critical in this movement. Given the changes in risk factors and treatments, we must also work towards curating comprehensive outcome studies to better guide surveillance strategies and treatment approaches, considering cost-analysis and quality of life measures as key factors in decision making. As the physicians who follow patients with HCC longitudinally, hepatologists are the ideal providers to collect these clinical and patient-reported outcomes and ensure that overall treatment strategy promotes patient-centered care. This remains an exciting time in the field of hepatology, and we eagerly await the results of the various clinical trials dedicated to improving HCC treatment outcomes.
Key Points:
The management of liver cancer is complicated by underlying liver disease. While many guidelines incorporate severity of liver disease, there are other nuances related to liver disease and its interplay with cancer management that need to be considered.
Evolving diagnostic tools and therapies for all stages of HCC challenge our prior treatment paradigms and make translation of evidence into daily practice more complex.
The care of patients with HCC goes beyond cancer treatment. Identification of the risk factors, preservation and optimization of liver function, and comprehensively addressing the needs of the patient, are the framework for sound treatment.
Hepatologists, as physicians trained in the evaluation, diagnosis, and management of liver disease, including evaluation of transplant candidacy, should be involved along the continuum of care of these complex patients.
We present the hepatologist’s “real life” playbook for a team-based holistic and individualized approach to the management of patients with liver disease and hepatocellular carcinoma.
Financial Support:
This project was supported in part by the Yale Liver Center award NIH P30 DK034989 Molecular and Translational core. Additional disclosures per Dr. Giannini include Advisory board membership and lecture fees from AstraZeneca, EISAI, MSD, Roche. Disclosures per Dr. Colombo include Advisory committee membership for Merck, Roche, Novartis, Bayer, BMS, Gilead Sciences, Tibotec, Vertex, Janssen Cilag, Achillion, Lundbeck, GSK, GenSpera, AbbVie, Alfa Wasserman, Intercept COST, Target HCC, Exelixis, Galapagos and speaking and teaching engagements for Tibotec, Roche, Novartis, Bayer, BMS, Gilead Sciences, Vertex, Merck, Janssen, AbbVie.
Footnotes
Conflict of Interest
There are no further personal or financial disclosures.
Declaration of Interest
This project was supported in part by the Yale Liver Center award NIH P30 DK034989 Clinical -Translational core.
Data Availability Statement:
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study
References
- 1.International Agency for Research on Cancer: World Health Organization. Liver Source: Globocan 2018 June 2020]; Available from: https://gco.iarc.fr/today/data/factsheets/cancers/11-Liver-fact-sheet.pdf.
- 2.EASL Clinical Practice Guidelines: Management of hepatocellular carcinoma. J Hepatol, 2018. 69(1): p. 182–236. [DOI] [PubMed] [Google Scholar]
- 3.JQ X, Trends in liver cancer mortality among adults aged 25 and over in the United States, 2000–2016. 2018, NCHS Data Brief [PubMed]
- 4.Jemal A, et al. Annual Report to the Nation on the Status of Cancer, 1975–2014, Featuring Survival. JNCI: Journal of the National Cancer Institute, 2017. 109(9). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Prevention, C.f.D.C.a. Global Viral Hepatitis: Millions of People are Affected [cited January 2021; Available from: https://www.cdc.gov/hepatitis/global/index.htm.
- 6.Asrani SK, et al. Reducing the Global Burden of Alcohol-Associated Liver Disease: A Blueprint for Action. Hepatology, 2021. 73(5): p. 2039–2050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Organization WH Obestiy and overweight January 2021]; Available from: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight.
- 8.Saeedi P, et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: Results from the International Diabetes Federation Diabetes Atlas, 9th edition. Diabetes Research and Clinical Practice, 2019. 157. [DOI] [PubMed] [Google Scholar]
- 9.Kim HS and El-Serag HB, The Epidemiology of Hepatocellular Carcinoma in the USA. Curr Gastroenterol Rep, 2019. 21(4): p. 17. [DOI] [PubMed] [Google Scholar]
- 10.Garuti F, et al. The changing scenario of hepatocellular carcinoma in Italy: an update. Liver Int, 2021. 41(3): p. 585–597. [DOI] [PubMed] [Google Scholar]
- 11.Marrero JA, et al. Diagnosis, Staging, and Management of Hepatocellular Carcinoma: 2018 Practice Guidance by the American Association for the Study of Liver Diseases. Hepatology, 2018. 68(2): p. 723–750. [DOI] [PubMed] [Google Scholar]
- 12.Singal AG, Lim JK, and Kanwal F, AGA Clinical Practice Update on Interaction Between Oral Direct-Acting Antivirals for Chronic Hepatitis C Infection and Hepatocellular Carcinoma: Expert Review. Clinical Liver Disease, 2020. 15(6): p. 211–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Piscaglia F, et al. Clinical patterns of hepatocellular carcinoma in nonalcoholic fatty liver disease: A multicenter prospective study. Hepatology, 2016. 63(3): p. 827–38. [DOI] [PubMed] [Google Scholar]
- 14.Plaz Torres MC, et al. Surveillance for Hepatocellular Carcinoma in Patients with Non-Alcoholic Fatty Liver Disease: Universal or Selective? Cancers (Basel), 2020. 12(6). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ioannou GN, et al. Models estimating risk of hepatocellular carcinoma in patients with alcohol or NAFLD-related cirrhosis for risk stratification. Journal of Hepatology, 2019. 71(3): p. 523–533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ioannou GN, Epidemiology and risk-stratification of NAFLD-associated HCC. Journal of Hepatology, 2021. 75(6): p. 1476–1484. [DOI] [PubMed] [Google Scholar]
- 17.Rinaldi L, et al. Risk of Hepatocellular Carcinoma after HCV Clearance by Direct-Acting Antivirals Treatment Predictive Factors and Role of Epigenetics. Cancers, 2020. 12(6): p. 1351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Degasperi E, et al. Factors Associated With Increased Risk of De Novo or Recurrent Hepatocellular Carcinoma in Patients With Cirrhosis Treated With Direct-Acting Antivirals for HCV Infection. Clin Gastroenterol Hepatol, 2019. 17(6): p. 1183–1191.e7. [DOI] [PubMed] [Google Scholar]
- 19.Meringer H, Shibolet O, and Deutsch L, Hepatocellular carcinoma in the post-hepatitis C virus era: Should we change the paradigm? World J Gastroenterol, 2019. 25(29): p. 3929–3940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wolf E, et al. Use of Hepatocellular Carcinoma Surveillance in Patients With Cirrhosis: A Systematic Review and Meta-Analysis. Hepatology, 2021. 73(2): p. 713–725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Davila JA, et al. Use of surveillance for hepatocellular carcinoma among patients with cirrhosis in the United States. Hepatology, 2010. 52(1): p. 132–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.White DL, et al. Incidence of Hepatocellular Carcinoma in All 50 United States, From 2000 Through 2012. Gastroenterology, 2017. 152(4): p. 812–820.e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dirchwolf M, et al. Failure in all steps of hepatocellular carcinoma surveillance process is frequent in daily practice. Ann Hepatol, 2021. 25: p. 100344. [DOI] [PubMed] [Google Scholar]
- 24.Serper M, et al. Association of Provider Specialty and Multidisciplinary Care With Hepatocellular Carcinoma Treatment and Mortality. Gastroenterology, 2017. 152(8): p. 1954–1964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tapper EB, et al. The Quality and Outcomes of Care Provided to Patients with Cirrhosis by Advanced Practice Providers. Hepatology (Baltimore, Md.), 2020. 71(1): p. 225–234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yeo YH, et al. Surveillance of patients with cirrhosis remains suboptimal in the United States. Journal of Hepatology, 2021. 75(4): p. 856–864. [DOI] [PubMed] [Google Scholar]
- 27.Marquardt P, et al. Hepatocellular Carcinoma Screening Process Failures in Patients with Cirrhosis. Hepatol Commun, 2021. 5(9): p. 1481–1489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.McGowan CE, et al. Suboptimal surveillance for and knowledge of hepatocellular carcinoma among primary care providers. Clin Gastroenterol Hepatol, 2015. 13(4): p. 799–804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dyson JK, Anstee QM, and McPherson S, Non-alcoholic fatty liver disease: a practical approach to diagnosis and staging. Frontline Gastroenterology, 2014. 5(3): p. 211–218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Khandelwal R, et al. Non-alcoholic fatty liver disease in diabetes: When to refer to the hepatologist? World Journal of Diabetes, 2021. 12(9): p. 1479–1493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.EASL-EASD-EASO Clinical Practice Guidelines for the management of non-alcoholic fatty liver disease. J Hepatol, 2016. 64(6): p. 1388–402. [DOI] [PubMed] [Google Scholar]
- 32.American College of Radiology. Liver Reporting & Data System v2018 November 2021]; Available from: https://www.acr.org/Clinical-Resources/Reporting-and-Data-Systems/LI-RADS
- 33.Schulze K, et al. Exome sequencing of hepatocellular carcinomas identifies new mutational signatures and potential therapeutic targets. Nat Genet, 2015. 47(5): p. 505–511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Harding JJ, et al. Prospective Genotyping of Hepatocellular Carcinoma: Clinical Implications of Next-Generation Sequencing for Matching Patients to Targeted and Immune Therapies. Clin Cancer Res, 2019. 25(7): p. 2116–2126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pinyol R, Sia D, and Llovet JM, Immune Exclusion-Wnt/CTNNB1 Class Predicts Resistance to Immunotherapies in HCC. Clin Cancer Res, 2019. 25(7): p. 2021–2023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yamauchi M, et al. Tumor Fibroblast Growth Factor Receptor 4 Level Predicts the Efficacy of Lenvatinib in Patients With Advanced Hepatocellular Carcinoma. Clin Transl Gastroenterol, 2020. 11(5): p. e00179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ni T, et al. Different MR features for differentiation of intrahepatic mass-forming cholangiocarcinoma from hepatocellular carcinoma according to tumor size. The British journal of radiology, 2018. 91(1088): p. 20180017–20180017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gigante E, et al. New insights into the pathophysiology and clinical care of rare primary liver cancers. JHEP Reports, 2021. 3(1): p. 100174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gigante E, et al. Combining imaging and tumour biopsy improves the diagnosis of combined hepatocellular-cholangiocarcinoma. Liver International, 2019. 39(12): p. 2386–2396. [DOI] [PubMed] [Google Scholar]
- 40.Dageforde LA, et al. Multi-Center Analysis of Liver Transplantation for Combined Hepatocellular Carcinoma-Cholangiocarcinoma Liver Tumors. J Am Coll Surg, 2021. 232(4): p. 361–371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Di Tommaso L, et al. Role of liver biopsy in hepatocellular carcinoma. World journal of gastroenterology, 2019. 25(40): p. 6041–6052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.von Felden J, et al. Liquid biopsy in the clinical management of hepatocellular carcinoma. Gut, 2020. 69(11): p. 2025–2034. [DOI] [PubMed] [Google Scholar]
- 43.Clinicaltrials.gov. NIH U.S. National Library of Medicine August 2022. December 2021]; Available from: https://clinicaltrials.gov/ct2/results?cond=Hepatocellular+Carcinoma&term=Liquid+biopsy&cntry=&state=&city=&dist=.
- 44.Graf J and Stengel A, Psychological Burden and Psycho-Oncological Interventions for Patients With Hepatobiliary Cancers-A Systematic Review. Front Psychol, 2021. 12: p. 662777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Maida M, et al. Staging systems of hepatocellular carcinoma: a review of literature. World J Gastroenterol, 2014. 20(15): p. 4141–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Reig M, et al. BCLC strategy for prognosis prediction and treatment recommendation: The 2022 update. Journal of Hepatology, 2022. 76(3): p. 681–693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Torzilli G, et al. A snapshot of the effective indications and results of surgery for hepatocellular carcinoma in tertiary referral centers: is it adherent to the EASL/AASLD recommendations?: an observational study of the HCC East-West study group. Ann Surg, 2013. 257(5): p. 929–37. [DOI] [PubMed] [Google Scholar]
- 48.Golfieri R, et al. Patients with Barcelona Clinic Liver Cancer Stages B and C Hepatocellular Carcinoma: Time for a Subclassification. Liver Cancer, 2019. 8(2): p. 78–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kim JH, et al. New intermediate-stage subclassification for patients with hepatocellular carcinoma treated with transarterial chemoembolization. Liver International, 2017. 37(12): p. 1861–1868. [DOI] [PubMed] [Google Scholar]
- 50.Giannini EG, et al. Patients with advanced hepatocellular carcinoma need a personalized management: A lesson from clinical practice. Hepatology, 2018. 67(5): p. 1784–1796. [DOI] [PubMed] [Google Scholar]
- 51.Prince D, et al. Management of patients with intermediate stage hepatocellular carcinoma. Therapeutic advances in medical oncology, 2020. 12: p. 1758835920970840–1758835920970840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Foerster F and Galle PR, The Current Landscape of Clinical Trials for Systemic Treatment of HCC. Cancers, 2021. 13(8): p. 1962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Johnson PJ, et al. A nssessment of liver function in patients with hepatocellular carcinoma: A new evidence-based approach - The albi grade. Journal of Clinical Oncology, 2015. 33(6): p. 550–558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Alahmadi A, et al. Utility of multidisciplinary tumor board (MTB) in the management of hepatocellular cancer (HCC). Annals of Oncology, 2016. 27: p. vi238. [Google Scholar]
- 55.Leoni S, et al. Adherence to AASLD guidelines for the treatment of hepatocellular carcinoma in clinical practice: experience of the Bologna Liver Oncology Group. Dig Liver Dis, 2014. 46(6): p. 549–55. [DOI] [PubMed] [Google Scholar]
- 56.Yopp AC, et al. Establishment of a multidisciplinary hepatocellular carcinoma clinic is associated with improved clinical outcome. Ann Surg Oncol, 2014. 21(4): p. 1287–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Taylor C, et al. Multidisciplinary team working in cancer: what is the evidence? BMJ, 2010. 340: p. c951. [DOI] [PubMed] [Google Scholar]
- 58.Siddique O, et al. The importance of a multidisciplinary approach to hepatocellular carcinoma. J Multidiscip Healthc, 2017. 10: p. 95–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Sinn DH, et al. Multidisciplinary approach is associated with improved survival of hepatocellular carcinoma patients. PLoS One, 2019. 14(1): p. e0210730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Vitale A, et al. Treatment of Hepatocellular Carcinoma in the Precision Medicine Era: From Treatment Stage Migration to Therapeutic Hierarchy. Hepatology, 2020. 72(6): p. 2206–2218. [DOI] [PubMed] [Google Scholar]
- 61.Stremitzer S, et al. Value of hepatic venous pressure gradient measurement before liver resection for hepatocellular carcinoma. Br J Surg, 2011. 98(12): p. 1752–8. [DOI] [PubMed] [Google Scholar]
- 62.Cucchetti A, et al. Is portal hypertension a contraindication to hepatic resection? Annals of Surgery, 2009. 250(6): p. 922–928. [DOI] [PubMed] [Google Scholar]
- 63.Romagnoli R, Mazzaferro V, and Bruix J, Surgical resection for hepatocellular carcinoma: Moving from what can be done to what is worth doing. Hepatology, 2015. 62(2): p. 340–342. [DOI] [PubMed] [Google Scholar]
- 64.Cucchetti A, et al. Cost-effectiveness of hepatic resection versus percutaneous radiofrequency ablation for early hepatocellular carcinoma. Journal of hepatology, 2013. 59. [DOI] [PubMed] [Google Scholar]
- 65.Shindoh J, CW DT, and Vauthey JN, Portal vein embolization for hepatocellular carcinoma. Liver Cancer, 2012. 1(3–4): p. 159–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Theysohn JM, et al. Hepatic volume changes after lobar selective internal radiation therapy (SIRT) of hepatocellular carcinoma. Clin Radiol, 2014. 69(2): p. 172–8. [DOI] [PubMed] [Google Scholar]
- 67.Kokudo T, et al. Survival benefit of liver resection for hepatocellular carcinoma associated with portal vein invasion. Journal of Hepatology, 2016. 65(5): p. 938–943. [DOI] [PubMed] [Google Scholar]
- 68.Finn RS, et al. Atezolizumab plus Bevacizumab in Unresectable Hepatocellular Carcinoma. New England Journal of Medicine, 2020. 382(20): p. 1894–1905. [DOI] [PubMed] [Google Scholar]
- 69.Gordan JD, et al. Systemic Therapy for Advanced Hepatocellular Carcinoma: ASCO Guideline. Journal of Clinical Oncology, 2020. 38(36): p. 4317–4345. [DOI] [PubMed] [Google Scholar]
- 70.Abou-Alfa GK, et al. Tremelimumab plus Durvalumab in Unresectable Hepatocellular Carcinoma. NEJM Evidence, 2022. 1(8): p. EVIDoa2100070. [DOI] [PubMed] [Google Scholar]
- 71.D’Alessio A, et al. Preliminary evidence of safety and tolerability of atezolizumab plus bevacizumab in patients with hepatocellular carcinoma and Child-Pugh A and B cirrhosis: A real-world study. Hepatology, 2022. [DOI] [PMC free article] [PubMed]
- 72.Wai Ling Khoo TS, R.A., Olynyk JK, Tyrosine Kinase Inhibitors in the Treatment of Hepatocellular Carcinoma, JEE T-P, Editor. 2019, Codon Publications. [PubMed] [Google Scholar]
- 73.Cui TM, et al. Adverse Effects of Immune-Checkpoint Inhibitors in Hepatocellular Carcinoma. Onco Targets Ther, 2020. 13: p. 11725–11740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Londoño MC and Reig M, Multidisciplinary Clinical Approach to Cancer Patients with Immune-Related Adverse Events Induced by Checkpoint Inhibitors. Cancers (Basel), 2020. 12(11). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Morales RE, et al. Safety and efficacy of ipilimumab to treat advanced melanoma in the setting of liver transplantation. J Immunother Cancer, 2015. 3: p. 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Tabrizian P, Florman SS, and Schwartz ME, PD-1 inhibitor as bridge therapy to liver transplantation? Am J Transplant, 2021. 21(5): p. 1979–1980. [DOI] [PubMed] [Google Scholar]
- 77.Qiao Z. y., et al. Neoadjuvant Programmed Cell Death 1 (PD-1) Inhibitor Treatment in Patients With Hepatocellular Carcinoma Before Liver Transplant: A Cohort Study and Literature Review. Frontiers in Immunology, 2021. 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.OPTN. Review of National Liver Review Board (NLRB) Diagnoses and Update to Alcohol Associated Diagnoses 2022; Available from: https://optn.transplant.hrsa.gov/media/bidemby1/policy-notice_liver_nlrb_ald_diagnoses.pdf.
- 79.Llovet JM, et al. Trial Design and Endpoints in Hepatocellular Carcinoma: AASLD Consensus Conference. Hepatology. n/a(n/a) [DOI] [PubMed]
- 80.Kaplan DE, et al. Sorafenib prescribed by gastroenterologists and hepatologists for hepatocellular carcinoma: A retrospective, multi-institutional cohort study. Medicine, 2018. 97(4): p. e9757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Pfister D, et al. NASH limits anti-tumour surveillance in immunotherapy-treated HCC. Nature, 2021. 592(7854): p. 450–456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Heimbach JK, et al. AASLD guidelines for the treatment of hepatocellular carcinoma. Hepatology, 2018. 67(1): p. 358–380. [DOI] [PubMed] [Google Scholar]
- 83.Bteich F and Di Bisceglie AM, Current and Future Systemic Therapies for Hepatocellular Carcinoma. Gastroenterol Hepatol (N Y), 2019. 15(5): p. 266–272. [PMC free article] [PubMed] [Google Scholar]
- 84.Mazzarelli C, et al. Palliative care in end-stage liver disease: Time to do better? Liver Transplantation, 2018. 24(7): p. 961–968. [DOI] [PubMed] [Google Scholar]
- 85.Kwong AJ EN, Kim WR, Lake JR, Smith JM, Schladt DP, Skeans MA, Foutz J, Gauntt K, Cafarella M, Snyder JJ, Israndi AK, Kasiske BL. OPTN/SRTR 2020. Annual Data Report: Liver Available from: 10.1111/ajt.16978. [DOI] [PubMed]
- 86.Mehta N, et al. Wait Time of Less Than 6 and Greater Than 18 Months Predicts Hepatocellular Carcinoma Recurrence After Liver Transplantation: Proposing a Wait Time “Sweet Spot”. Transplantation, 2017. 101(9): p. 2071–2078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Guidance to Liver Transplant Programs and the National Liver Review Board for Adult MELD Exceptions for Hepatocellular Carcinoma (HCC) 2022; Available from: https://optn.transplant.hrsa.gov/media/gqlnhrtn/20200804_nlrb_adult_hcc_guidance.pdf?j=599912&sfmc_sub=135482566&l=5025_HTML&u=25851997&mid=100001876&jb=7.
- 88.Cabibbo G, et al. Hepatic decompensation is the major driver of death in HCV-infected cirrhotic patients with successfully treated early hepatocellular carcinoma. J Hepatol, 2017. 67(1): p. 65–71. [DOI] [PubMed] [Google Scholar]
- 89.Gabutti A, et al. Hepatocellular Carcinoma Recurrence After Liver Transplantation. Oncology (Williston Park), 2020. 34(3). [PubMed] [Google Scholar]
- 90.Filgueira NA, Hepatocellular carcinoma recurrence after liver transplantation: Risk factors, screening and clinical presentation. World J Hepatol, 2019. 11(3): p. 261–272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Sahasrabuddhe VV, et al. Nonsteroidal anti-inflammatory drug use, chronic liver disease, and hepatocellular carcinoma. J Natl Cancer Inst, 2012. 104(23): p. 1808–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Simon TG, et al. Association of Aspirin with Hepatocellular Carcinoma and Liver-Related Mortality. New England Journal of Medicine, 2020. 382(11): p. 1018–1028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Del Barco S, et al. Metformin: multi-faceted protection against cancer. Oncotarget, 2011. 2(12): p. 896–917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Tseng CH, Metformin and risk of hepatocellular carcinoma in patients with type 2 diabetes. Liver Int, 2018. 38(11): p. 2018–2027. [DOI] [PubMed] [Google Scholar]
- 95.Singh S, et al. Statins are associated with a reduced risk of hepatocellular cancer: a systematic review and meta-analysis. Gastroenterology, 2013. 144(2): p. 323–32. [DOI] [PubMed] [Google Scholar]
- 96.Tsan YT, et al. Statins and the risk of hepatocellular carcinoma in patients with hepatitis B virus infection. J Clin Oncol, 2012. 30(6): p. 623–30. [DOI] [PubMed] [Google Scholar]
- 97.Plaz Torres MC, et al. Diabetes medications and risk of HCC. Hepatology n/a(n/a). [DOI] [PMC free article] [PubMed]
- 98.Perisetti A, et al. Sarcopenia in hepatocellular carcinoma: Current knowledge and future directions. World J Gastroenterol, 2022. 28(4): p. 432–448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Woodrell CD, et al. Palliative Care for People With Hepatocellular Carcinoma, and Specific Benefits for Older Adults. Clin Ther, 2018. 40(4): p. 512–525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Brown C, Aksan N, and Muir AJ, MELD-Na Accurately Predicts 6-Month Mortality in Patients With Decompensated Cirrhosis: Potential Trigger for Hospice Referral. J Clin Gastroenterol, 2021. [DOI] [PMC free article] [PubMed]
- 101.Tandon P, et al. AGA Clinical Practice Update on Palliative Care Management in Cirrhosis: Expert Review. Clinical Gastroenterology and Hepatology, 2021. 19(4): p. 646–656.e3. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study


