Abstract
Objective
Visual arts-based exposure and training are effective tools to enhance medical education. The visual arts can increase emotional intelligence and critical thinking skills. This study, conducted at Georgetown University School of Medicine (GUSoM) and the National Gallery of Art (NGA) in Washington, DC, was designed to measure the effect of a visual arts elective course on medical students’ self-perception of their communication skills.
Methods
This 6-week course involved lessons at the NGA and GUSoM for16 second-year medical students. The intervention students were age and gender-matched to14 second-year medical student control participants who took different elective courses. Prior to and following the intervention, the participants completed the Communication Skills Attitude Scale (CSAS). Statistical analysis was performed with either the 2-sided t-test or 2-sided Wilcoxon rank-sum test.
Results
There were no statistically significant differences in the presurvey scores between the groups. However, there were 6 CSAS questions in the postsurveys that had statistically significant differences between the 2 groups. Within each group, there were also numerous statistically significant differences between their presurvey and postsurvey responses, with positive changes occurring in the intervention group (IG) and primarily negative changes occurring in the control group (CG). The NGA course improved the self-perception of communication skills, with students reporting stronger views on the importance of communication skills in teamwork and patient rapport. The CG, on the other hand, did not have as many improved perceptions of communication skills and had stronger opinions regarding not needing the ability to communicate well to be a good physician.
Conclusion
This study indicates that medical student communication skills can benefit from exposure to visual arts activities and experiences. Future physicians must become effective communicators, and this study paves the way for research investigating the relationship between visual arts education and the development of a physician's communication skills.
Keywords: Medical curriculum, visual arts, communication skills
Introduction
Effective communication between physicians and patients is a core clinical skill to achieve meaningful, trust-based relationships that enable accurate decision making, improved outcomes, and satisfaction. 1 Since 1995, medical school accreditation has required instruction for communication skills as one of the core competencies for medical education.2,3 Currently, the Georgetown University School of Medicine (GUSoM) offers required courses on physician-patient communication to help students develop a foundation for their interviewing skills and learn the importance of this interpersonal relationship. 4 Studies have shown that communication skills can be enhanced and learned through specific training early in medical school. 5 Additionally, studies have shown that physicians often overestimate their communication skills. 6 Art can help enhance the communication skills of a doctor by creating further insight into their emotions, the experience of life and the human experience, and by improving the ability of students to reflect on how they process the world and think. 7 Effective physician communication skills lead to improved and lasting health outcomes for patients.8,9 According to the Joint Commission, 80% of medical errors are due to miscommunication between providers. 10
For the past 20 years, multiple medical institutions have studied the effects of visual art instruction on improving empathy, observation, perception of bias, and reflective capabilities.11–13 In December 2020, the Association of American Medical Colleges (AAMC) acknowledged the importance of integrating the arts and humanities into medical education and asserted that physicians must learn emotional intelligence and critical thinking skills to provide for patients. 14 The visual arts are one such avenue that can improve communication because they encourage students develop an ability to think more speculatively, notice negative findings, and understand the complexity of the human experience.13,15 Even 3h of visual art training at the beginning of clerkships can improve the ability of medical students to interpret, think, and use analogies. 16
The OUAM course is taught annually to a combined class of first-year medical students from Columbia University Vagelos College of Physicians and Surgeons and Weill Cornell Medical College. The average enrollment of 12 students per year (6 students per school) was deemed appropriate for museum-based teaching. 17
At the University of Cincinnati, second-year medical students underwent an art education course and were followed through rotations. They noticed observational skill improvement during their clerkships and a lack of education on interpretive skills in other parts of their curriculum. 13 At Johns Hopkins University, third-year and fourth-year medical students participated in sessions held at The Baltimore Museum of Art. They completed postsession surveys and focus groups which were qualitatively analyzed and showed that students were challenged to critically think about their communication styles. 18 At the University of Texas Health Science Center San Antonio, medical and nursing students attended an Arts Rounds program and were evaluated based on the Communication Skills Attitudes Scale where researchers found that after the program the students’ positive views toward professional communication skills were increased. 19 Recently, at Baylor College of Medicine, first-year medical students were led in activities at a local museum and then assessed using a validated questionnaire on changes in empathy. 20 However, neither of these studies included comparison to a control group.
Although there is a multitude of promising studies assessing visual arts education, a review by Mukunda et al mentions that research conducted up until this point has mainly revolved around subjective and qualitative data. There is a need for evidence-based methods and proof of long-term improvements with validated measures to explicitly assess the impact of art education on communication skills. 21 A study was conducted in 2019 by authors Madeleine Ward and Julia Langley to address the needs mentioned by Mukunda et al particularly regarding the effects of art education on communication skills. Preliminary data from that study conducted on 22 participants showed that there may be value in teaching communication skills in an arts-based, nontraditional classroom. However, the data analysis did not provide results with sufficient clarity. Therefore, a paper was never published and the decision was made to repeat the study. This article is the result of recreating the first study, analyzing new data, and further exploring and validating their hypothesis by quantitatively evaluating the effects of visual arts instruction on medical students’ perception of their own communication skills.
Methods
Design
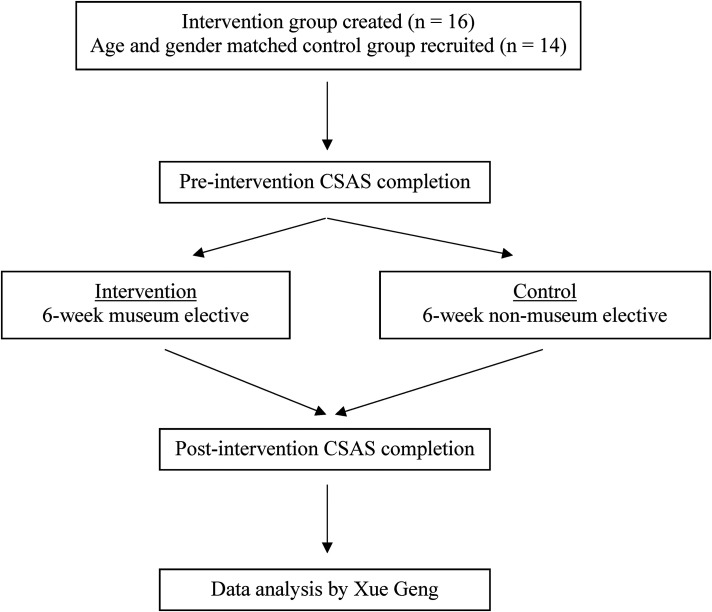
This study was a nonrandomized, controlled, quantitative design with pre-evaluation and post-evaluation of a visual arts learning intervention. The design was based upon the 2019 study conducted, by Madeleine Ward and Julia Langley with variations including an increase in participants from n = 22 to n = 30 and new data analysis leading to concrete, publishable results. See Figure 1 for visualization.
Figure 1.
Experimental design.
Participants
The participants (n = 30) were all second-year medical students at GUSoM. The study was approved as exempt by the Georgetown University Internal Review Board and lasted for 6 weeks. Ethics approval was waived. The intervention group (IG) consisted of 16 second-year students who were attending the NGA elective course and agreed to participate in this study. The IG participants would have participated in the elective whether they had consented to study participation or not. The control group (CG) consisted of 14 second-year students who volunteered and were selected based on the following eligibility criteria: (1) any second-year medical student at GUSoM, (2) any second-year medical student who matches the age and gender of a participant in the elective, (3) any second-year medical student who has not majored in Art History in the past or have extensive art training, and (4) any second-year medical student who is not currently enrolled in the “Communicating Disease Through Art,” elective that Julia Langley is also teaching. Twenty-eight students volunteered to be part of the control group but only 14 were selected in order to age and gender-match them to one of the IG participants and maintain internal validity. All students provided written consent for this study and were offered a $10 Starbucks gift card in exchange for their participation.
Art-based intervention
Julia Langley, MA, MBA, Faculty Director, Georgetown Lombardi Arts and Humanities Program and Lorena Bradford, PhD, Manager of Accessible Programs, NGA, co-taught a 6-week museum-based elective course called “The National Gallery of Art and the Making of the Modern Physician (NGAMMP),” during August to September 2022. An initial introduction was held on GUSoM campus, then 4 meetings at the NGA to critically analyze works of art, ending with a final session at GUSoM. Each meeting focused on 1 of the 4 major communication themes: observation, perception, empathy, and bias (Table 1 and Appendix A). Pedagogical approaches included curriculum from Harvard Graduate School of Education Project Zero such as “See, Think, Wonder,” and activities by Amy E. Herman, author of “Visual Intelligence.”22,23 The exercises on empathy and bias were designed by museum educator Bradford and medical humanities scholar Langley.
Table 1.
Exercises at the NGA.
| EXERCISE | COMMUNICATION THEME | OBJECTIVE(S) |
|---|---|---|
| “See/Think/Wonder” | Observation | Understanding the difference between observation and interpretation |
| Describe and Draw | Perception | Understanding the difference between speaking and being understood |
| Art + History | Empathy | Understanding how context leads to comprehension and empathy |
| Listen then Look | Bias | Understanding how words can prejudice what we see |
List of visual art-based educational activities with associated themes and objectives. See Appendix A for full descriptions of exercises. Abbreviation: NGA, National Gallery of Art.
Outcome measures
Prior to the elective data was collected on the intervention participants regarding their age and gender in order to recruit matched CG participants. Both intervention and control participants completed a de-identified nonvalidated background questionnaire consisting of college minors, college art and art history courses, extracurricular experience in arts, previous professional experience, and previous museum visits (Table 2). Items were answered with either yes or no. This background questionnaire was to be used to later compare the intervention and control students’ experience and interest in art with their subsequent intervention results. We did not collect race or cultural background data on our participants. Prior to and following the 6-week elective course, participants completed the Communication Skills Attitude Scale (CSAS). The CSAS is a validated quantitative survey that was developed in 2002 by UK psychiatrist Charlotte Rees et al for measuring medical students’ attitudes toward learning communication skills (Appendix B). 24 The 26-item questionnaire is scored on a Likert Scale where 1 = strongly disagree, 2 = disagree, 3 = neutral, 4 = agree, and 5 = strongly agree. Data was collected using Qualtrics. We hypothesized that visual intelligence education would enhance medical students’ self-perception of their communication skills in the IG. We also hypothesized that intervention participants would have a self-assessed improved perception of the importance of communication skills compared to the control participants and that control participants would have no change in their perception of communication skills.
Table 2.
Background characteristics of control and intervention participants.
| OVERALL | INTERVENTION | CONTROL | ||
|---|---|---|---|---|
| n = 30 | n = 16 | n = 14 | ||
| Art minor in college (%) | Yes | 2 (7) | 1 (6) | 1 (7) |
| No | 28 (93) | 15 (94) | 13 (93) | |
| Art history classes in college (%) | Yes | 7 (23) | 7 (44) | 0 (0) |
| No | 23 (77) | 9 (56) | 14 (100) | |
| Art extracurriculars in college (%) | Yes | 22 (73) | 14 (88) | 8 (57) |
| No | 8 (27) | 2 (12) | 6 (43) | |
| Museum visit in the last year (%) | Yes | 21 (70) | 10 (63) | 11 (79) |
| No | 9 (30) | 6 (37) | 3 (21) | |
| Professional clinical experience prior to medical school (%) | Yes | 19 (63) | 9 (56) | 10 (71) |
| No | 11 (37) | 7 (44) | 4 (29) |
Percentage of participants of IG and CG who participated in art-related experience prior to medical school. Abbreviations: CG, control group; IG, intervention group.
Statistical analysis
Xue Geng, biostatistician, aided the team in completing the analysis. Since the responses of each questionnaire item were scored on a Likert Scale with more than 4 categories, we viewed the responses as continuous variables. The data normality was checked using the Shapiro-Wilk test. Data characteristics were summarized by using frequencies and percentages for categorical variables and mean with standard deviation (SD) or median with interquartile range (IQR) for continuous variables based on data normality.
In order to test the difference in the response of each questionnaire item and in the overall score between the IGs and CGs before and after the intervention, the 2-sided t-test or 2-sided Wilcoxon rank-sum test was used based on data normality. Either the 2-sided paired t-test or 2-sided Wilcoxon-signed rank test was used to test the difference in the responses of each questionnaire item and the overall score between pre-intervention and postintervention within each group.
All tests are at a significance level of 0.05. All analyses were performed using the statistical software RStudio (Version 2022.07.2).
Results
We collected data from 16 second-year medical students at GUSoM who were participating in the NGAMMP elective. These medical students were age and gender-matched to 14 recruited control participants.
After statistical analysis, we found that when comparing the presurvey results of the CG to the presurvey results of the IG, there was no statistically significant difference. Then, we compared postsurvey data between the CG and IG and found the statistically significant differences presented in Table 3. The intervention participants had a more positive response in their perception of the importance of communication skills development, their perception of communication skills learning on teamwork and patient relations, and the perception that communication ability is a lifelong skill.
Table 3.
Statistically significant CSAS questions comparing postsurveys between control and intervention participants.
| QUESTION | CONTROL | INTERVENTION | P-value | |
|---|---|---|---|---|
| Q4 median [IQR] | Developing my communication skills is just as important as developing my knowledge of medicine | 4.00 [4.00–5.00] | 5.00 [5.00–5.00] | .022 |
| Q9 median [IQR] | Learning communication skills has helped or will help facilitate my team-working skills | 4.50 [4.00–5.00] | 5.00 [5.00–5.00] | .027 |
| Q10 median [IQR] | Learning communication skills has improved my ability to communicate with patients | 5.00 [4.00–5.00] | 5.00 [5.00–5.00] | .049 |
| Q19 median [IQR] | I do not need good communication skills to be a doctor | 1.00 [1.00–2.00] | 1.00 [1.00–1.00] | .049 |
| Q21 median [IQR] | I think it is useful to learn communication skills during my medical degree | 5.00 [4.00–5.00] | 5.00 [5.00–5.00] | .004 |
| Q25 median [IQR] | Learning communication skills is important because my ability to communicate is a lifelong skill | 5.00 [4.00–5.00] | 5.00 [5.00–5.00] | .049 |
P-value significant if < .05. Abbreviations: CSAS, Communication Skills Attitude Scale; IQR, interquartile range.
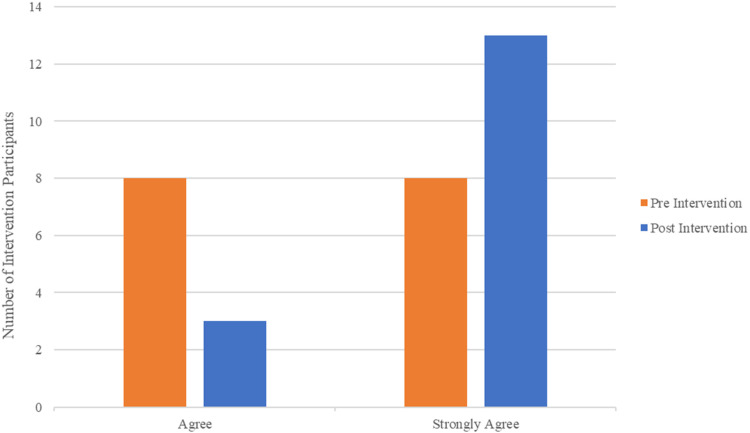
Next, when comparing the presurvey and postsurvey responses among the intervention participants, we found that there were statistically significant results for the questions presented in Table 4. There were remarkable changes before and after the elective for questions related to the importance of communication skills learning, learning communication skills as being fun, helping to respect colleagues and patients, and the skills as being useful. The IG also more strongly disagreed that communication skills learning should be more scientific, that it is difficult to take learning communication skills seriously, and that it is hard to admit having problems with communication skills. One of the most important questions on the survey is question 4. The number of intervention participants who selected “strongly agree” rather than “agree” is visibly increased as depicted in Figure 2.
Table 4.
Statistically significant CSAS questions comparing within-group presurvey and postsurvey of intervention and control participants.
| QUESTION | PRE | POST | P-value | |
|---|---|---|---|---|
| Intervention participants | ||||
| Q4 median [IQR] | Developing my communication skills is just as important as developing my knowledge of medicine | 4.50 [4.00–5.00] | 5.00 [5.00–5.00] | .037 |
| Q5 median [IQR] | Learning communication skills has helped or will help me respect patients | 5.00 [4.00–5.00] | 5.00 [5.00–5.00] | .037 |
| Q12 median [IQR] | Learning communication skills is fun | 4.00 [3.00–4.00] | 4.00 [4.00–4.25] | .006 |
| Q14 median [IQR] | Learning communication skills has helped or will help me respect my colleagues | 4.00 [4.00–5.00] | 5.00 [5.00–5.00] | .003 |
| Q17 median [IQR] | Communication skills teaching would have a better image if it sounded more like a science subject | 2.00 [1.75–2.25] | 2.00 [1.00–2.00] | .020 |
| Q20 median [IQR] | I find it hard to admit to having some problems with my communication skills | 2.50 [2.00–3.00] | 2.00 [1.75–2.00] | .006 |
| Q21 median [IQR] | I think it is useful to learn communication skills during my medical degree | 5.00 [4.00–5.00] | 5.00 [5.00–5.00] | .048 |
| Q24 median [IQR] | I find it difficult to take communication skills learning seriously | 2.00 [1.75–2.00] | 1.50 [1.00–2.00] | .048 |
| Control Participants | ||||
| Q3 median [IQR] | Nobody is going to fail their medical degree for having poor communication skills | 2.00 [2.00–3.75] | 3.00 [2.00–4.00] | .006 |
| Q11 median [IQR] | Communication skills teaching states the obvious and then complicates it | 2.00 [1.25–2.75] | 2.00 [2.00–3.00] | .037 |
| Q17 median [IQR] | Communication skills teaching would have a better image if it sounded more like a science subject | 2.00 [2.00–3.00] | 2.00 [2.00–3.00] | .037 |
| Q18 median [IQR] | When applying for medicine, I thought it was a good idea to learn communication skills | 4.00 [3.25–5.00] | 4.00 [2.25–4.00] | .011 |
| Q19 median [IQR] | I do not need good communication skills to be a doctor | 1.00 [1.00–1.00] | 1.00 [1.00–2.00] | .048 |
| Q20 median [IQR] | I find it hard to admit to having problems with my communication skills | 3.00 [2.00–4.00] | 2.00 [2.00–4.00] | .037 |
P-value significant if < .05. Abbreviations: CSAS, Communication Skills Attitude Scale; IQR, interquartile range.
Figure 2.
Number of intervention participants who selected “agree” and “strongly agree” pre-NGAMMP and post-NGAMMP elective for question 4 on the CSAS: “Developing my communication skills is just as important as developing my knowledge of medicine.”
Abbreviations: CSAS, Communication Skills Attitude Scale; NGAMMP, National Gallery of Art and the Making of the Modern Physician
The control participants also had significant changes when comparing their presurvey and postsurvey responses. Even though they did not participate in the NGAMMP elective, there were significant positive changes for the question related to thinking it was a good idea to learn communication skills when applying for medical school. They also had numerous significant changes for questions with which they disagreed. They disagreed more with statements about communication skills teaching needing to be more scientific, not needing good communication skills to be a doctor, and finding it hard to admit problems with communication skills.
Discussion
The CSAS is a quantitative metric by which to measure the impact of visual arts education on communication skills. Previous studies have primarily focused on the benefits of art in medical education by focusing on improvement in observation skills, and measuring them through qualitative appraisal. 25 Quantitative data regarding the impact of the arts on communication skills, specifically among medical students, is lacking. In 2019, Julia Langley and then fourth-year medical student, Madeleine Ward, used the CSAS on 12 intervention and 10 control participants. Ward's unpublished study used different metrics and statistical analysis so the results are not directly comparable with our results. This study repeated their methods with different statistical analyses to demonstrate that museum-based learning of communication is beneficial to medical students. In this study, 16 second-year medical students at GUSoM participated in a comfortable, low-stakes, level playing field environment off campus without added competitive pressure. At the NGA, unlike traditional lecture-based medical school courses, experiential learning challenged the students and focused their attention on the difficulty and essential importance of good communication skills.
There were no statistically significant differences in the presurvey results of the NGAMMP intervention participants and the control participants, solidifying that the students in both groups were starting at a similar perception of communication skills and their importance. Contrary to control participants, students in the elective found developing these skills to be more important overall and recognized the necessity of good communication when working in a team and with patients. They also increasingly agreed with the statement that communication ability growth is a lifelong skill. Going to the museum and participating in the activities served as an opportunity to experience communication in a different way than they had experienced before or during their medical training. They challenged their communication skills within a nonmedical environment using art historical language as a stand-in for unfamiliar language patterns, particularly medical jargon. They practiced listening, discussed how bias can affect what we see, and learned that the first glance is not always accurate. They had to achieve this all in a short period of time, a very common occurrence for medical providers. They went further than solely practicing their observation skills, and practiced perspective-taking and empathy as well. Studies show empathy declines during medical school, with students becoming more detached and cynical as training continues.26,27 Clinician disengagement negatively impacts physician–patient relationships, leading to patient dissatisfaction with clinical practice. Hojat et al write that empathy is “positively associated with ratings of clinical competence in core clinical clerkships.” 26 Communication is also impaired by cultural barriers. 10 Improving one's empathy with exercises such as the “Art + History” exercise, an exercise focused on cultural context, can improve one's ability to understand and overcome these barriers.
Beyond the differences between the control and intervention participants in the postsurveys, the intervention participants experienced changes within their group from when they began the elective until after it was completed.
Students agreed more strongly with the statement that communication skills learning is fun, and this directly ties in with one of the goals of Julia Langley's program, to show students that leaving campus to learn in a low-stakes environment, and looking at as well as talking about art can be exciting, fun, and valuable to their chosen profession. The students also more strongly disagreed with the statement that having problems with their communication skills was difficult to admit. This indicates that participation in the elective increased their self-awareness. It offered them both a more comfortable environment in which to share their lack of confidence and made them realize that their skills were not as strong as they previously assumed. This realization may be a motivating factor for students to think differently about the importance of practicing communication. The students also changed their perception of how communication skills development can impact their respect for others. They more strongly agreed with the statements regarding respect for patients and respect for colleagues.
The control participants, interestingly, also had statistically significant differences between their presurvey and postsurvey results. Some of these significant differences were more strongly agreeing or disagreeing with statements that indicate a lack of improvement in their perception of the importance of communication skills. There was a statistically significant increase in the median for the question regarding failing their medical degree because of poor communication skills. They more strongly agreed with this statement after the intervention period for the other students. They also less strongly disagreed with the statement “I do not need good communication skills to be a doctor.” This could be due to the fact these students were not experiencing the benefits of learning about communication skills and their importance, allowing their opinions to solidify without the intervention of communication lessons exposure. These negative changes could additionally be due to a misunderstanding of the questionnaire's questions since it can be difficult to agree or disagree with negatively framed questions. There were also positive changes of more strongly disagreeing for questions 17 and 20, which inquired about whether or not communication skills teaching would be better if it was more scientific, and students finding it hard to admit having problems with communication skills. While they did not participate in the elective, one possible explanation for these positive changes is the self-selective nature of the students who elected to be part of the CG. A significant portion of them, 57%, had participated in art-related extracurricular activities in college and 79% had visited a museum in the past year.
Creating humanistic physicians, with the ability to observe closely and communicate broadly, is the goal of programs like the NGAMMP. While work has been done to show the positive effect visual arts training programs have on observation skills, few studies have linked visual arts training to medical students’ ability to communicate. This study, based on students’ self-assessment of communication, is the first of a series on communication abilities. The next study will focus on how learning communication skills in a museum benefits clinician–patient relations.
Limitations
This study's limitations include the small sample size and the lack of an equal number of intervention and control participants. No power analysis was performed for this study. There may also be selection bias given that a large number of intervention participants had an interest in visual arts before participating in the elective. The results were also collected at only one point, so they may not be sustained over time. These results are also self-reported, and cannot be generalized to say that the students’ communication skills necessarily improved after the visual arts training. Additional studies with data provided by third-party assessments of clinical encounters with patients (either real or standardized) will provide concrete information regarding the relationship between communication skills improvement and visual arts education.
Conclusion
Communication skills are vital to medical education and practice. They improve relationships with colleagues and patients and ensure that a physician is a successful team member. Communication skills are 1 of the 6 general competencies defined and adopted by the Accreditation Council for Graduate Medical Education and the American Board of Medical Specialties for medical training. In general, medical students are not taught communication skills in a low-stakes, noncompetitive environment. Museum-based experiences can provide this type of learning. Our data suggest that art interventions of the kind described in this article can increase self-awareness and self-perceptions on the importance of communication in the medical field. Quantitative data such as that presented in this article is essential to evaluate the effectiveness of art-based interventions for medical school curriculum development. The use of the CSAS is an effective way to assess growth in the area of communication. The students who participated in this study elected to do so likely because of their positive prior experiences with the arts. Greater sample sizes, randomization, and third-party assessments by standardized patients will strengthen future research on this topic. However, based on our data, the course had a positive impact on second-year medical students at GUSoM. Four times as many students “strongly agreed” with the statement, “Developing my communication skills is just as important as developing my knowledge of medicine,” after the intervention. Therefore, we can imagine the positive impact visual arts training could have on all medical students. Communication is a core clinical skill to become an effective, empathetic, and trustworthy physician.
Acknowledgments
We thank Lorena Bradford for her contribution to the teaching of the National Gallery of Art course to our participating medical students.
Appendix A
NGA exercises extended description
The first in-museum class for the NGAMMP revolves around a thinking routine developed by Project Zero at the Harvard University Graduate School of Education called “See Think, Wonder.” The purpose of this routine is to teach students the difference between observation and interpretation, as well as the fact that slow looking leads to improved visual comprehension. In our iteration of this routine, students are asked to describe what they see in John Singleton Copley's (1778) “Watson and the Shark.” They are given a few minutes to study the painting, and then asked, “What do you see?” The goal of this question is for students to mention a person, place, or thing in the painting, without interpreting its meaning. Students often skip this step, and jump directly into reasoning for the existence of a person, place, or thing, instead. In developing an understanding of the difference between observation and interpretation, participants begin to break out all the individual components in front of them. In doing so, they realize that they may or may not see things in the same way and/or see the same things as their counterparts. Often, students hold differing impressions of the painting from that of their peers which, through discussion and engagement, are addressed. The timeline for this exercise is 45 min to an hour. The concept of slow looking is carried forward through several of the subsequent activities. Understanding that there may be multiple viewpoints for a single image or idea is essential for medical students to understand, as they must be able to communicate to patients, providers, and caregivers their view of a situation and the evidence for how they arrived at it.
The second activity in the galleries, known as “Describe and Draw,” builds on the first. In this exercise, students are faced with the difficulties of providing clear, concise communication to a partner who can neither see what they are describing nor ask them questions about it. It is designed to give participants a new perspective on communication by making it artificially difficult and one-sided. For the exercise to work, students are paired into groups of 2. One person is deemed “the Describer” and the other is “the Listener.” The Listener is given a clipboard with a sheet of white paper and a pencil. The Describer leads the Listener into a gallery of paintings unfamiliar to both of them. Then the Describer seats the Listener in front of a selected painting, with their back to it. For 3 timed minutes, the Describer narrates their painting to the Listener, who attempts to draw what is heard, but not seen. With the exception of the Describer talking, there can be no communication between the parties. Normal conversational cues are absent. The 2 can neither look at each other nor discuss what is being described or drawn. At the end of 3 min, the students view the painting together. Then the students switch roles and repeat the exercise. Afterwards, the group joins together for a conversation about the experience. The goal of Describe and Draw is for participants to learn that effective communication is especially difficult when it involves unfamiliar information, speaking without visual or verbal connection, and listening for replicable information without the ability to ask the speaker to slow down, clarify or repeat what has been said. They learn the value of developing a communication plan (eg, mentioning whether the painting is a portrait or landscape, seascape or city scene, etc) in order to orient the Listener to what is being discussed. In this exercise, the drawing is only about process, not product. The end result is inconsequential. Communication skills and the difficulty of sharing complex information is at the heart of this exercise.
The third in-museum activity centers on empathy, and how it is impeded by ambiguity. In order to show the importance of understanding patient stories and their context, the students center their attention on “The Artist and His Mother,” by Arshile Gorky. This work of art from 1942 features the artist as a young boy, standing next to his seated mother. Each figure looks out toward the viewer. It is difficult to gauge the relationship between the 2 due to their stiff postures, old-fashioned clothing, emotionless countenances, and the lack of setting behind them. Once the participants have described what they see in the painting, they are asked to surmise about the relationship between the figures and why the painting looks the way it does (eg, visible brushstrokes on one side, a smooth painted surface on the other, warm skin tones for the boy's face, pale gray tones for the mother). Then, they are presented with the tragic history behind the work of art. The painting is based upon a photograph of the 2 taken when Gorky was a child, before his mother died during the Armenian genocide, and he escaped to New York with his sister. A replica of the photograph upon which the painting is based is shown to the students, and they are asked whether or not knowing the story behind the painting influences how they feel about the characters within it. This exercise in close looking, followed by the unspooling of the tragic story, leading to an understanding that hearing people's stories is essential to the development of empathy. The exercise is designed to help students comprehend how a patient's story goes far beyond what is presented in a chart, and may assist in the understanding of their overall condition.
During the fourth visit to the National Gallery of Art, participants are presented with a clipboard and worksheet as they settle in front of a large painting. They are told to read the artists’ words before examining the artwork in front of them. In this case, the painting is James Whistler's (1862) Symphony in White, No.1: (The White Girl). Whistler famously said of the artwork, “My painting simply represents a girl in white standing in front of a white curtain.” The students are asked to find evidence in the painting for Whistler's words and write it down. In doing so, they realize that there is a dissonance between what has been said, and what can be seen. As the artist, Whistler is the authority on the work of art. The painting, however, shows much more than what Whistler claims. For example, the claim that “My painting simply represents a girl in white standing in front of a white curtain,” ignores the section of the painting showing a bloody bearskin rug upon which the girl stands, flowers fallen from her hand, and many more details. As the students work to reconcile the difference between what the artist has said and what they see in the painting, they grasp the problem of seeing and hearing 2 different stories. They learn to grapple with uncertainty and the problem of hearing a statement from a hierarchical figure whose words can influence the way in which someone or something is seen, understood and managed.
Appendix B
Communication Skills Attitude Scale questions
| Question | Statement |
|---|---|
| 1 | In order to be a good doctor, I must have good communication skills. |
| 2 | I cannot see the point in learning communication skills. |
| 3 | Nobody is going to fail their medical degree for having poor communication skills. |
| 4 | Developing my communication skills is just as important as developing my knowledge of medicine. |
| 5 | Learning communication skills has helped or will help me respect patients. |
| 6 | I do not have time to learn communication skills. |
| 7 | Learning communication skills is interesting. |
| 8 | I cannot be bothered to turn up to sessions on communication skills. |
| 9 | Learning communication skills has helped or will help facilitate my team-working skills. |
| 10 | Learning communication skills has improved my ability to communicate with patients. |
| 11 | Communication skills teaching states the obvious and then complicates it. |
| 12 | Learning communication skills is fun. |
| 13 | Learning communication skills is too easy. |
| 14 | Learning communication skills has helped or will help me respect my colleagues. |
| 15 | I find it difficult to trust information about communication skills given to me by nonclinical lectures. |
| 16 | Learning communication skills has helped or will help me recognize patients’ rights regarding confidentiality and informed consent. |
| 17 | Communication skills teaching would have a better image if it sounded more like a science subject. |
| 18 | When applying for medicine, I thought it was a really good idea to learn communication skills. |
| 19 | I do not need good communication skills to be a doctor. |
| 20 | I find it hard to admit to having some problems with my communication skills. |
| 21 | I think it is useful to learn communication skills on my medical degree. |
| 22 | My ability to pass exams will get me through medical school rather than my ability to communicate. |
| 23 | Learning communication skills is applicable to learning medicine. |
| 24 | I find it difficult to take communication skills learning seriously. |
| 25 | Learning communication skills is important because my ability to communicate is a lifelong skill. |
| 26 | Communication skills learning should be left to psychology students, not medical students. |
Footnotes
Author contributions: CJ was the main investigator for the 2022 study and wrote the majority of this manuscript. MW was the primary investigator for the 2019 version of the study and wrote the foundation of this manuscript. XG was the primary statistician for the results presented in this manuscript. AB was a researcher for the 2019 version of the study. JL was a teacher for the 2019 and 2022 National Gallery of Art courses and helped to write this manuscript.
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was performed without the aid of grant funding and was conducted with students participating in a course scheduled at Georgetown University School of Medicine taught by Julia Langley and Lorena Bradford.
ORCID iD: Xue Geng https://orcid.org/0000-0003-4100-9899
References
- 1.Ha JF, Longnecker N. Doctor-patient communication: a review. Ochsner J. 2010;10(1):38-43. [PMC free article] [PubMed] [Google Scholar]
- 2.Makoul GMSJAMA. Communication skills education in medical school and beyond. JAMA. 2003;289(1):93. doi: 10.1001/jama.289.1.93 [DOI] [PubMed] [Google Scholar]
- 3.Edgar L, McLean S, Hogan SO, Hamstra S, Holmboe ES. The milestones guidebook. Accreditation Council for Graduate Medical Education (ACGME). 2020; 1-40. [Google Scholar]
- 4.Physician-patient communication. Georgetown University School of Medicine. August 8, 2019. Accessed July 14, 2019. https://som.georgetown.edu/medicaleducation/curriculum/firstyearmodules/modules/ppc.
- 5.Hausberg MC, Hergert A, Kröger C, Bullinger M, Rose M, Andreas S. Enhancing medical students’ communication skills: development and evaluation of an undergraduate training program. BMC Med Educ. 2012;(12):16. doi: 10.1186/1472-6920-12-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tongue JR, Epps HR, Forese LL. Communication skills for patient-centered care: research-based, easily learned techniques for medical interviews that benefit orthopaedic surgeons and their patients. J Bone Joint Surg Am. 2005;87(3):652-658. [Google Scholar]
- 7.Perry M, Maffulli N, Willson S, Morrissey D. The effectiveness of arts-based interventions in medical education: a literature review. Med Educ. 2011;45(2):141-148. doi: 10.1111/j.1365-2923.2010.03848.x [DOI] [PubMed] [Google Scholar]
- 8.Tavakoly Sany SB, Behzhad F, Ferns G, Peyman N. Communication skills training for physicians improves health literacy and medical outcomes among patients with hypertension: a randomized controlled trial. BMC Health Serv Res. 2020;20(1):60. doi: 10.1186/s12913-020-4901-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stewart MA. Effective physician-patient communication and health outcomes: a review. CMAJ. 1995;152(9):1423-1433. [PMC free article] [PubMed] [Google Scholar]
- 10.Joint Commission International. Communicating clearly and effectively to patients: how to overcome common communication challenges in health care [White paper]. Joint Commission Resources, Inc; 2018. [Google Scholar]
- 11.Bardes CL, Gillers D, Herman AE. Learning to look: developing clinical observational skills at an art museum. Med Educ. 2001;35(12):1157-1161. doi: 10.1046/j.1365-2923.2001.01088.x [DOI] [PubMed] [Google Scholar]
- 12.Dolev JC, Friedlaender LK, Braverman IM. Use of fine art to enhance visual diagnostic skills. JAMA. 2001;286(9):1020-1021. doi: 10.1001/jama.286.9.1020 [DOI] [PubMed] [Google Scholar]
- 13.Elder NC, Tobias B, Lucero-Criswell A, Goldenhar L. The art of observation: impact of a family medicine and art museum partnership on student education. Fam Med. 2006;38(6):393-398. [PubMed] [Google Scholar]
- 14.Howley L, Gaufberg E, King B. The fundamental role of the arts and humanities in medical education. AAMC. 2020:1-54. [Google Scholar]
- 15.Naghshineh S, Hafler JP, Miller AR, et al. Formal art observation training improves medical students’ visual diagnostic skills. J Gen Intern Med. 2008;23 (7):991-997. doi: 10.1007/s11606-008-0667-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jasani SK, Saks NS. Utilizing visual art to enhance the clinical observation skills of medical students. Med Teach. 2013;35(7):e1327-e1331. doi: 10.3109/0142159X.2013.770131 [DOI] [PubMed] [Google Scholar]
- 17.Gowda D, Dubroff R, Willieme A, Swan-Sein A, Capello C. Art as sanctuary: a four-year mixed-methods evaluation of a visual art course addressing uncertainty through reflection. Acad Med. 2018;Nov 93:S8-S13. doi: 10.1097/ACM.0000000000002379 [DOI] [PubMed] [Google Scholar]
- 18.Kagan HJ, Kelly-Hedrick M, Benskin E, Wolffe S, Suchanek M, Chisolm MS. Understanding the role of the art museum in teaching clinical-level medical students. Med Educ Online. 2022;27(1):2010513. doi: 10.1080/10872981.2021.2010513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Klugman CM, Peel J, Beckmann-Mendez D. Art rounds: teaching interprofessional students visual thinking strategies at one school. Acad Med. 2011;86(10):1266-1271. doi: 10.1097/ACM.0b013e31822c1427 [DOI] [PubMed] [Google Scholar]
- 20.Rezaei S, Childress A, Kaul B, Rosales KM, Newell A, Rose S. Using visual arts education and reflective practice to increase empathy and perspective taking in medical students. MedEdPORTAL. 2023;19:11346. doi: 10.15766/mep_2374-8265.11346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mukunda N, Moghbeli N, Rizzo A, Niepold S, Bassett B, DeLisser HM. Visual art instruction in medical education: a narrative review. Med Educ Online. 2019;24(1):1558657. doi: 10.1080/10872981.2018.1558657 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. The See / Think / Wonder thinking routine was developed by Project Zero, a research center at the Harvard Graduate School of Education.
- 23.Herman A. Visual intelligence: sharpen your perception, change your life. 1st ed. Mariner Books; 2017. [Google Scholar]
- 24.Rees C, Sheard C, Davies S. The development of a scale to measure medical students’ attitudes towards communication skills learning: the Communication Skills Attitude Scale (CSAS). Med Educ. 2002;36(2):141-147. doi: 10.1046/j.1365-2923.2002.01072.x [DOI] [PubMed] [Google Scholar]
- 25.Ike JD, Howell J. Quantitative metrics and psychometric scales in the visual art and medical education literature: a narrative review. Med Educ Online. 2022;27(1):2010299. doi: 10.1080/10872981.2021.2010299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hojat M, Mangione S, Nasca TJ, et al. An empirical study of decline in empathy in medical school. Med Educ. 2004;38(9):934-941. doi: 10.1111/j.1365-2929.2004.01911.x [DOI] [PubMed] [Google Scholar]
- 27.Shin HS, Park H, Lee YM. The relationship between medical students’ empathy and burnout levels by gender and study years. Patient Educ Couns. 2022;105(2):432-439. doi: 10.1016/j.pec.2021.05.036 [DOI] [PubMed] [Google Scholar]