Introduction
Acute diverticulitis (AD) is one of the most common clinical conditions encountered in the emergency setting1. Possible complications include abscess, perforation, fistulas, obstruction, and bleeding. Fistulas are often the consequence of repeated acute episodes, with localized perforation into adjacent viscera2. Multiple AD episodes can also increase the risk of stricture formation. The risk of developing an AD in a patient with diverticulosis is estimated at 4% throughout a patient’s lifetime3.
Management of this condition has recently changed, with guidelines published by the World Society of Emergency Surgery (WSES) and the European Society of Coloproctology (ESCP)4,5. However, the levels of evidence are inconsistent and recommendations may vary according to the health systems and the resources available. There can be a lag of years from publication to implementation6.
Considering these variations and the latest published management recommendations, the aim of the present study was to establish a consensus among colorectal surgeons on the diagnosis and management of AD based on Swiss national practice.
Methods
All Swiss hospitals that performed, according to the national statistics (2015–2017), at least 50 colorectal resections annually, over a 3-year interval, were contacted (52 hospitals). Each centre could include up to three board-certified surgeons at a consultant level, regularly performing colorectal resection for benign and malignant indications. No minimal individual surgeon volume was required. A three-round Delphi consensus was conducted, which is detailed in the Supplementary Methods. Consensus was defined as greater than or equal to 70% agreement, either obtained within one single answer or with multiple answers pointing in the same direction (either positive or negative), for questions on a Likert scale (1–2 versus 4–5).
Results
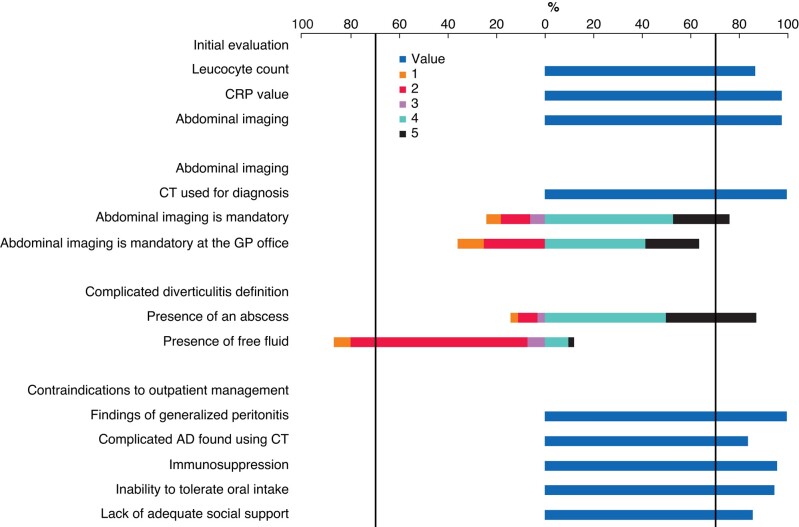
Initial evaluation, abdominal imaging, complicated diverticulitis definition, and outpatient management (Fig. 1)
Fig. 1.
Initial evaluation, abdominal imaging, complicated diverticulitis definition and contraindications to outpatient management
Likert scale: 1, strongly disagree; 2, partially agree; 3, neutral; 4, agree; and 5, strongly agree. CRP, C-reactive protein; GP, general practitioner; AD, acute diverticulitis.
Abdominal CT reached consensus as the recommended imaging modality (100%) for diagnosis of AD. Complicated diverticulitis was defined as the presence of an abscess (88%), fistula (84%), pericolic (86%) or distant (83%) free air, and rectal contrast extravasation (95%). Stenosis (62%) and free fluid in the pelvis (40%) or in the upper abdomen (48%) were not deemed to be complicated diverticulitis.
Fever (58%), findings of localized peritonitis (47%), antibiotic requirement (14%), and leucocytes greater than 20×109/l (49%) were not considered as contraindications for outpatient management if taken individually. Additional results are available in the Supplementary material.
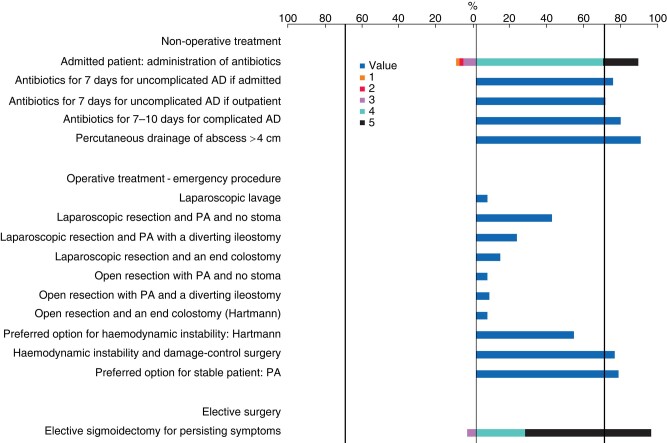
Non-operative/operative treatment and elective surgery (Fig. 2)
Fig. 2.
Non-operative/operative treatment and elective surgery
Likert scale: 1, strongly disagree; 2, partially agree; 3, neutral; 4, agree; and 5, strongly agree. AD, acute diverticulitis; PA, primary anastomosis.
Antibiotic treatment and percutaneous drainage are described in Fig. 2. In the case of drainage, no consensus was reached on the necessity to perform control abdominal imaging (51%).
No procedure reached consensus for surgical management in the emergency setting (Fig. 2). Primary anastomosis was the preferred option when the patient is stable (77%) (stapled end to end, 73%). From a technical point of view, no consensus was reached on the type of dissection (28% for total mesorectal excision versus 42% for close-to-bowel dissection). Insertion of a pelvic drain (90%) reached consensus for emergency procedures.
Elective surgical resection was recommended in patients with persistent symptoms (95%) or immunosuppression (89%). Age (14%) and number of episodes of recurrent AD (27%) were not considered criteria for elective surgery. Standard planned elective sigmoidectomy after a complicated case of AD (42%) or after a percutaneously drained abscess (65%) did not gain consensus. Laparoscopic resection was the favoured approach for elective sigmoidectomy (98%). Additional results are available in the Supplementary material.
Discussion
Swiss colorectal surgeons reached consensus on the management of AD with regard to diagnosis, outpatient management, and indication for elective surgery. Emergency surgical management did not reach consensus.
Many radiological classifications have described the different stages of diverticular disease; however, none is currently universally accepted7. This was also apparent in this study. The definitive treatment for each stage also depends on the clinical condition and patient co-morbidity. More recent classifications (Sallinen and WSES) that combine clinical, radiological, and physiological parameters were not considered in this study, limiting the generalization of the results in clinical practice8,9.
Non-operative management of AD has changed over the past few decades. Two randomized controlled studies (AVOD and DIABOLO trials) confirmed that this approach was not associated with a higher recurrence or rate of sigmoidectomy10,11. However, controversies and habits tend to persist, as highlighted in the present study, where a consensus was reached in favour of antibiotic treatment10–13. In ESCP guidelines, antibiotics are recommended for immunocompromised patients or sepsis5. Percutaneous drainage of a pericolic abscess is another unresolved question. A systematic review revealed comparable treatment failure rates for antibiotics (19.9%) and percutaneous drainage (20.8%)14. Based on these results, it was suggested that abscesses greater than 4 cm should be drained, confirming the results of the present study.
A systematic review demonstrated that outpatient management of AD was safe, but no criteria of failure were identified, which makes patient selection difficult15. The present study identified subjective contraindications for outpatient management, such as generalized peritonitis, immunosuppression, or complicated diverticulitis. These criteria were assessed individually, not in combination. Management decisions should be made based on the general and physiological condition of the patient.
The present study reached a consensus on the necessity for emergency surgery in patients with sepsis. However, the levels of evidence are inconsistent in patients with perforation without haemodynamic instability5. WSES guidelines suggest a Hartmann procedure in patients with faecal peritonitis or sepsis4. Conversely, ESCP guidelines state that the choice of the procedure should be left to the surgeon, according to their experience, but resection is recommended5. The present study has not established a consensus on the most appropriate surgical technique. The experience and the logistics according to the hospital (ICU, theatres, and out-of-hours access) probably play an important role in decision-making. Damage-control surgery (DCS) is an option in unstable patients. A retrospective study of 203 consecutive patients treated with DCS by applying a decision algorithm for severe intra-abdominal sepsis confirmed that it was feasible and 65% of patients were stoma free at hospital discharge16. However, none of the guidelines recommends DCS over a Hartmann procedure4,5. Indications, timing, and techniques of the DCS approach need to be further assessed (for example primary anastomosis with a diverting loop ileostomy or Hartmann procedure).
The use of laparoscopic lavage for purulent peritonitis is controversial; however, due to the lack of proof supporting its inferiority, this technique may be used according to the ESCP guidelines5. The present study demonstrated no consensus for the role of laparoscopic lavage. The SCANDIV trial results suggested that the use of laparoscopic lavage versus primary resection did not reduce severe postoperative complications and led to a higher reoperation rate17,18.
The target surgeon group was chosen to include colorectal experts, aiming to provide a well-founded basis for the diagnosis and management of AD. This study addressed the question in a methodologically robust way. The Delphi technique is a widely used and validated method to transform opinion into group consensus among experts and specific questions or issues19. The aim of the study was not to generate new guidelines for AD, but to confirm/challenge them within a group of national experts, as published guidelines are not systematically accepted or applied in practice today.
Collaborators
Swiss Colorectal Working Group
Aamr Orban (Seespital, Horgen, Switzerland); Adrienne Imhof (Praxis Imhof, Schaffhausen, Switzerland); Alex Ochsner (Spitallimmattal, Schlieren, Switzerland); Alfred Kuhrmeier (Clinica Luganese Moncucco, Lugano, Switzerland); Andrea Donadini (Clinica Luganese Moncucco, Lugano, Switzerland); Andreas Keerl (Kantonsspital Baden, Baden, Switzerland); Andreas Kohler (Inselspital, Bern, Switzerland); Andreas Scheiwiller (Luzerner Kantonsspital, Luzern, Switzerland); Andreas Zerz (eSwiss Medical & Surgical Center, St Gallen, Switzerland); Anita Scheiwiller (Klinik Beau-Site, Bern, Switzerland); Annette Ringger (Solothurner Spitäler, Solothurn, Switzerland); Antje Lechleiter (Inselspital, Bern, Switzerland); Antonio Nocito (Kantonsspital Baden, Baden, Switzerland); Beat Muggli (Praxis Beat Muggli, Bern, Switzerland); Beat Schnüriger (Inselspital, Bern, Switzerland); Béatrice Kern (Clarunis, Basel, Switzerland); Bernhard Egger (HFR, Fribourg, Switzerland); Boumediene Mustapha Guendil (Hôpital du Valais, Sion, Switzerland); Carsten Thomas Viehl (Spitalzentrum Biel, Biel/Bienne, Switzerland); Cedric Vallet (Clinique de la Source, Lausanne, Switzerland); Christian Nebiker (Kantonsspital Aarau, Aarau, Switzerland); Christine Maurus (Hôpital du Valais, Sion, Switzerland); Claudio Soravia (Clinique générale Baulieu, Genève, Switzerland); Cornelia Frei (Spital Zollikerberg, Zollikerberg, Switzerland); Daniel Steinemann (Clarunis, Basel, Switzerland); David Petermann (EHC, Morges, Switzerland); Duri Gianom-Campell (Clinica Luganese Moncucco, Lugano, Switzerland); Emanuel Gmuer (GZO Spital Wetzikon, Wetzikon, Switzerland); Eric Grossen (Seespital, Horgen, Switzerland); Fabian Hauswirth (Spital Thurgau, Frauenfeld, Switzerland); Franc Hetzer (Viszeralchirurgie Bellaria, Zürich, Switzerland); François Pugin (HFR, Fribourg, Switzerland); Frank-Rainer Müller (Stadtspital, Zürich, Switzerland); Gaël Simoné (Clinique de Genolier, Genolier, Switzerland); Georg Linke (Spital Thun, Thun, Switzerland); Giacinto Basilicata (Spital Bülach, Bülach, Switzerland); Ida Füglistaler (Claraspital, Basel, Switzerland); Ivo Fischer (Spital Bülach, Bülach, Switzerland); Jan Schmidt (Praxis Swiss Surgery, Zürich, Switzerland); Jens Forberger (Spital Männedorf, Männedorf, Switzerland); Karoline Horisberger (USZ, Zurich, Switzerland); Luca Di Mare (EHC, Morges, Switzerland); Marc Daniel Worreth (RHNe, Neuchâtel, Switzerland); Marc-Olivier Guenin (Clarunis, Basel, Switzerland); Marc-Olivier Sauvain (RHNe, Neuchâtel, Switzerland); Mark Hartel (Kantonsspital Aarau, Aarau, Switzerland); Markus Gass (Luzerner Kantonsspital, Luzern, Switzerland); Markus Müller (Spital Thurgau, Frauenfeld, Switzerland); Michel Erne (eHnv, Yverdon-les-Bains, Switzerland); Nicolas Buchs (Hôpital de la Tour, Genève, Switzerland); Olivier Gié (Clinica Luganese Moncucco, Lugano, Switzerland); Olivier Pittet (Hôpital Riviera-Chablais, Rennaz, Switzerland); Othmar Schöb (Chirurgisches Zentrum, Zürich, Switzerland); Peter Sandera (Spitäler Schaffausen, Schaffhausen, Switzerland); Peter Studer (VISCERA Bauchmedizin, Bern, Switzerland); Raffaele Galli (Kantonsspital Baselland, Liestal, Switzerland); Rebecca Kraus (Kantonsspital Graubünder, Chur, Switzerland); Riadh Ksontini (Hôpital Riviera-Chablais, Rennaz, Switzerland); Robert Rosenberg (Kantonsspital Baselland, Liestal, Switzerland); Roland Chautems (RHNe, Neuchâtel, Switzerland); Sebastian Lamm (Kantonsspital Baselland, Liestal, Switzerland); Stefan Wildi (Stadtspital, Zürich, Switzerland); Stephan Sager (Seespital, Horgen, Switzerland); Stephan Vorburger (Spital Emmental, Burgdorf, Switzerland); Teresa Cereser (Kantonsspital Winterthur, Winterthur, Switzerland); Thomas Kinsbergen (SRO Klinik, Langenthal, Switzerland); Thomas Simon (Hôpital du Valais, Visp, Switzerland); Urs Zingg (Spital Limattal, Schlieren, Switzerland).
Supplementary Material
Acknowledgements
T.G. and D.M. contributed equally and share first authorship.
Contributor Information
Timothée Girardin, Department of Visceral Surgery, Lausanne University Hospital (CHUV), University of Lausanne (UNIL), Lausanne, Switzerland.
David Martin, Department of Visceral Surgery, Lausanne University Hospital (CHUV), University of Lausanne (UNIL), Lausanne, Switzerland.
Enrique Lázaro-Fontanet, Department of Visceral Surgery, Lausanne University Hospital (CHUV), University of Lausanne (UNIL), Lausanne, Switzerland.
Daniel Clerc, Department of Visceral Surgery, Lausanne University Hospital (CHUV), University of Lausanne (UNIL), Lausanne, Switzerland.
Martin Hübner, Department of Visceral Surgery, Lausanne University Hospital (CHUV), University of Lausanne (UNIL), Lausanne, Switzerland.
Lukas Brügger, Department of Visceral Surgery, Bern University Hospital (Inselspital), Bern, Switzerland.
Matthias Turina, Department of Visceral Surgery, Zurich University Hospital, Zurich, Switzerland.
Walter Brunner, Department of Visceral Surgery, St-Gallen Kantonsspital, St-Gallen, Switzerland.
Dimitri Christoforidis, Department of Visceral Surgery, Oespedale Regionale di Lugano, Lugano, Switzerland.
Frederic Ris, Department of Visceral Surgery, Hôpitaux Universitaires de Genève (HUG), Genève, Switzerland.
Michel Adamina, Department of Visceral Surgery, Winterthur Kantonsspital, Winterthur, Switzerland.
Marco von Strauss, Department of Visceral Surgery, St Claraspital und Universitätsspital Basel, Basel, Switzerland.
Dieter Hahnloser, Department of Visceral Surgery, Lausanne University Hospital (CHUV), University of Lausanne (UNIL), Lausanne, Switzerland.
Swiss Colorectal Working Group:
Aamr Orban, Adrienne Imhof, Alex Ochsner, Alfred Kuhrmeier, Andrea Donadini, Andreas Keerl, Andreas Kohler, Andreas Scheiwiller, Andreas Zerz, Anita Scheiwiller, Annette Ringger, Antje Lechleiter, Antonio Nocito, Beat Muggli, Beat Schnüriger, Béatrice Kern, Bernhard Egger, Boumediene Mustapha Guendil, Carsten Thomas Viehl, Cedric Vallet, Christian Nebiker, Christine Maurus, Claudio Soravia, Cornelia Frei, Daniel Steinemann, David Petermann, Duri Gianom-Campell, Emanuel Gmuer, Eric Grossen, Fabian Hauswirth, Franc Hetzer, François Pugin, Frank-Rainer Müller, Gaël Simoné, Georg Linke, Giacinto Basilicata, Ida Füglistaler, Ivo Fischer, Jan Schmidt, Jens Forberger, Karoline Horisberger, Luca Di Mare, Marc Daniel Worreth, Marc-Olivier Guenin, Marc-Olivier Sauvain, Mark Hartel, Markus Gass, Markus Müller, Michel Erne, Nicolas Buchs, Olivier Gié, Olivier Pittet, Othmar Schöb, Peter Sandera, Peter Studer, Raffaele Galli, Rebecca Kraus, Riadh Ksontini, Robert Rosenberg, Roland Chautems, Sebastian Lamm, Stefan Wildi, Stephan Sager, Stephan Vorburger, Teresa Cereser, Thomas Kinsbergen, Thomas Simon, and Urs Zingg
Funding
The authors have no funding to declare.
Disclosure
The online voting system was made available by Johnson&Johnson, Switzerland. The authors declare no other conflict of interest.
Supplementary material
Supplementary material is available at BJS Open online.
Data availability
Data are available on request.
References
- 1. Wilkins T, Embry K, George R. Diagnosis and management of acute diverticulitis. Am Fam Physician 2013;87:612–620 [PubMed] [Google Scholar]
- 2. Bahadursingh AM, Virgo KS, Kaminski DL, Longo WE. Spectrum of disease and outcome of complicated diverticular disease. Am J Surg 2003;186:696–701 [DOI] [PubMed] [Google Scholar]
- 3. Shahedi K, Fuller G, Bolus R, Cohen E, Vu M, Shah Ret al. Long-term risk of acute diverticulitis among patients with incidental diverticulosis found during colonoscopy. Clin Gastroenterol Hepatol 2013;11:1609–1613 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Sartelli M, Weber DG, Kluger Y, Ansaloni L, Coccolini F, Abu-Zidan Fet al. 2020 update of the WSES guidelines for the management of acute colonic diverticulitis in the emergency setting. World J Emerg Surg 2020;15:32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Schultz JK, Azhar N, Binda GA, Barbara G, Biondo S, Boermeester MAet al. European Society of Coloproctology: guidelines for the management of diverticular disease of the colon. Colorectal Dis 2020;22:5–28 [DOI] [PubMed] [Google Scholar]
- 6. Faes S, Hübner M, Demartines N, Hahnloser D, Martin D; Swiss Snapshot Diverticulitis Group . Elective surgery for diverticulitis in Swiss hospitals. Front Surg 2021;8:717228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Klarenbeek BR, de Korte N, van der Peet DL, Cuesta MA. Review of current classifications for diverticular disease and a translation into clinical practice. Int J Colorectal Dis 2012;27:207–214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Sallinen VJ, Leppäniemi AK, Mentula PJ. Staging of acute diverticulitis based on clinical, radiologic, and physiologic parameters. J Trauma Acute Care Surg 2015;78:543–551 [DOI] [PubMed] [Google Scholar]
- 9. Sartelli M, Moore FA, Ansaloni L, Di Saverio S, Coccolini F, Griffiths EAet al. A proposal for a CT driven classification of left colon acute diverticulitis. World J Emerg Surg 2015;10:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Chabok A, Påhlman L, Hjern F, Haapaniemi S, Smedh K; AVOD Study Group . Randomized clinical trial of antibiotics in acute uncomplicated diverticulitis. Br J Surg 2012;99:532–539 [DOI] [PubMed] [Google Scholar]
- 11. van Dijk ST, Daniels L, Ünlü Ç, de Korte N, van Dieren S, Stockmann HBet al. Long-term effects of omitting antibiotics in uncomplicated acute diverticulitis. Am J Gastroenterol 2018;113:1045–1052 [DOI] [PubMed] [Google Scholar]
- 12. Isacson D, Smedh K, Nikberg M, Chabok A. Long-term follow-up of the AVOD randomized trial of antibiotic avoidance in uncomplicated diverticulitis. Br J Surg 2019;106:1542–1548 [DOI] [PubMed] [Google Scholar]
- 13. Daniels L, Ünlü Ç, de Korte N, van Dieren S, Stockmann HB, Vrouenraets BCet al. Randomized clinical trial of observational versus antibiotic treatment for a first episode of CT-proven uncomplicated acute diverticulitis. Br J Surg 2017;104:52–61 [DOI] [PubMed] [Google Scholar]
- 14. Gregersen R, Mortensen LQ, Burcharth J, Pommergaard HC, Rosenberg J. Treatment of patients with acute colonic diverticulitis complicated by abscess formation: a systematic review. Int J Surg Lond Engl 2016;35:201–208 [DOI] [PubMed] [Google Scholar]
- 15. Cirocchi R, Randolph JJ, Binda GA, Gioia S, Henry BM, Tomaszewski KAet al. Is the outpatient management of acute diverticulitis safe and effective? A systematic review and meta-analysis. Tech Coloproctol 2019;23:87–100 [DOI] [PubMed] [Google Scholar]
- 16. Faes S, Hübner M, Girardin T, Demartines N, Hahnloser D. Rate of stoma formation following damage-control surgery for severe intra-abdominal sepsis: a single-centre consecutive case series. BJS Open 2021;5:zrab106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Schultz JK, Wallon C, Blecic L, Forsmo HM, Folkesson J, Buchwald Pet al. One-year results of the SCANDIV randomized clinical trial of laparoscopic lavage versus primary resection for acute perforated diverticulitis. Br J Surg 2017;104:1382–1392 [DOI] [PubMed] [Google Scholar]
- 18. Schultz JK, Yaqub S, Wallon C, Blecic L, Forsmo HM, Folkesson Jet al. Laparoscopic lavage vs primary resection for acute perforated diverticulitis: the SCANDIV randomized clinical trial. JAMA 2015;314:1364–1375 [DOI] [PubMed] [Google Scholar]
- 19. Jones J, Hunter D. Consensus methods for medical and health services research. BMJ 1995;311:376–380 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data are available on request.
References
- 1. Wilkins T, Embry K, George R. Diagnosis and management of acute diverticulitis. Am Fam Physician 2013;87:612–620 [PubMed] [Google Scholar]
- 2. Bahadursingh AM, Virgo KS, Kaminski DL, Longo WE. Spectrum of disease and outcome of complicated diverticular disease. Am J Surg 2003;186:696–701 [DOI] [PubMed] [Google Scholar]
- 3. Shahedi K, Fuller G, Bolus R, Cohen E, Vu M, Shah Ret al. Long-term risk of acute diverticulitis among patients with incidental diverticulosis found during colonoscopy. Clin Gastroenterol Hepatol 2013;11:1609–1613 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Sartelli M, Weber DG, Kluger Y, Ansaloni L, Coccolini F, Abu-Zidan Fet al. 2020 update of the WSES guidelines for the management of acute colonic diverticulitis in the emergency setting. World J Emerg Surg 2020;15:32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Schultz JK, Azhar N, Binda GA, Barbara G, Biondo S, Boermeester MAet al. European Society of Coloproctology: guidelines for the management of diverticular disease of the colon. Colorectal Dis 2020;22:5–28 [DOI] [PubMed] [Google Scholar]
- 6. Faes S, Hübner M, Demartines N, Hahnloser D, Martin D; Swiss Snapshot Diverticulitis Group . Elective surgery for diverticulitis in Swiss hospitals. Front Surg 2021;8:717228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Klarenbeek BR, de Korte N, van der Peet DL, Cuesta MA. Review of current classifications for diverticular disease and a translation into clinical practice. Int J Colorectal Dis 2012;27:207–214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Sallinen VJ, Leppäniemi AK, Mentula PJ. Staging of acute diverticulitis based on clinical, radiologic, and physiologic parameters. J Trauma Acute Care Surg 2015;78:543–551 [DOI] [PubMed] [Google Scholar]
- 9. Sartelli M, Moore FA, Ansaloni L, Di Saverio S, Coccolini F, Griffiths EAet al. A proposal for a CT driven classification of left colon acute diverticulitis. World J Emerg Surg 2015;10:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Chabok A, Påhlman L, Hjern F, Haapaniemi S, Smedh K; AVOD Study Group . Randomized clinical trial of antibiotics in acute uncomplicated diverticulitis. Br J Surg 2012;99:532–539 [DOI] [PubMed] [Google Scholar]
- 11. van Dijk ST, Daniels L, Ünlü Ç, de Korte N, van Dieren S, Stockmann HBet al. Long-term effects of omitting antibiotics in uncomplicated acute diverticulitis. Am J Gastroenterol 2018;113:1045–1052 [DOI] [PubMed] [Google Scholar]
- 12. Isacson D, Smedh K, Nikberg M, Chabok A. Long-term follow-up of the AVOD randomized trial of antibiotic avoidance in uncomplicated diverticulitis. Br J Surg 2019;106:1542–1548 [DOI] [PubMed] [Google Scholar]
- 13. Daniels L, Ünlü Ç, de Korte N, van Dieren S, Stockmann HB, Vrouenraets BCet al. Randomized clinical trial of observational versus antibiotic treatment for a first episode of CT-proven uncomplicated acute diverticulitis. Br J Surg 2017;104:52–61 [DOI] [PubMed] [Google Scholar]
- 14. Gregersen R, Mortensen LQ, Burcharth J, Pommergaard HC, Rosenberg J. Treatment of patients with acute colonic diverticulitis complicated by abscess formation: a systematic review. Int J Surg Lond Engl 2016;35:201–208 [DOI] [PubMed] [Google Scholar]
- 15. Cirocchi R, Randolph JJ, Binda GA, Gioia S, Henry BM, Tomaszewski KAet al. Is the outpatient management of acute diverticulitis safe and effective? A systematic review and meta-analysis. Tech Coloproctol 2019;23:87–100 [DOI] [PubMed] [Google Scholar]
- 16. Faes S, Hübner M, Girardin T, Demartines N, Hahnloser D. Rate of stoma formation following damage-control surgery for severe intra-abdominal sepsis: a single-centre consecutive case series. BJS Open 2021;5:zrab106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Schultz JK, Wallon C, Blecic L, Forsmo HM, Folkesson J, Buchwald Pet al. One-year results of the SCANDIV randomized clinical trial of laparoscopic lavage versus primary resection for acute perforated diverticulitis. Br J Surg 2017;104:1382–1392 [DOI] [PubMed] [Google Scholar]
- 18. Schultz JK, Yaqub S, Wallon C, Blecic L, Forsmo HM, Folkesson Jet al. Laparoscopic lavage vs primary resection for acute perforated diverticulitis: the SCANDIV randomized clinical trial. JAMA 2015;314:1364–1375 [DOI] [PubMed] [Google Scholar]
- 19. Jones J, Hunter D. Consensus methods for medical and health services research. BMJ 1995;311:376–380 [DOI] [PMC free article] [PubMed] [Google Scholar]