Abstract
Purpose
To evaluate the variations in hip muscles strength following arthroscopy and 6-month rehabilitation in patients treated for femoroacetabular impingement (FAI).
Methods
A retrospective analysis was carried out on a series of patients who were arthroscopically treated for FAI at La Tour Hospital between 2020 and 2022. Bilateral isometric strengths of 8 hip-related muscles (abductors, adductors, hamstrings, quadriceps, extensors, flexors, internal and external rotators) were assessed using a handheld dynamometer before surgery and postoperatively after 6 months of rehabilitation in terms of relative strength changes between time points.
Results
A total of 29 patients (aged 26.9 ± 7.1 years, 86% of women) were included. Except for the abductors, which remained of comparable strength than before surgery, a statistically significant (P < .05) increase in hip muscle strength on the operated side could be noted at 6 postoperative months for hamstrings (9% ± 17%, P = .041), quadriceps (11% ± 27%, P = .045), extensors (17% ± 32%, P = .006), flexors (17% ± 29%, P = .003), adductors (18% ± 23%, P < .001), and internal rotators (32% ± 36%, P < .001). The proportion of patients who reached a strength level above their preoperative status ranged from 62% (quadriceps) to 86% (adductors and flexors), depending on the muscle studied. The external rotators were the only muscles that remained significantly weakened at 6 months on both operated (–13% ± 26%, P = .002) and nonoperated (–17% ± 25%, P < .001) sides, with a decrease beyond 15% in almost half of the patients (45% and 48%, respectively).
Conclusions
Arthroscopic treatment followed by 6-month rehabilitation granted to most FAI patients a higher strength level for several hip muscles, except for abductors and external rotators, which remained comparable and weakened, respectively.
Level of Evidence
Level IV, therapeutic case series.
The major cause of femoroacetabular impingement (FAI) is biomechanical. Conservative care comprising physical therapy leads to beneficial effects and can be proposed as a first-line approach. Recent systematic reviews and meta-analyses, however, reported superior outcomes for surgical treatments in both the short and long term.1, 2, 3 Surgical treatments have gained in popularity to mechanically fix femoral and/or acetabular bony deformations.4 Arthroscopic surgery has evolved5 and is increasingly performed since it grants satisfactory patient-reported outcomes while being mini-invasive.6, 7, 8, 9, 10 Compared to open procedures, this surgical approach might also have the advantage of requiring a shorter rehabilitation period, thereby offering a fast return to daily activities in satisfying conditions.11,12
Several authors have emphasized the role of physical therapy following arthroscopy. Published rehabilitation protocols usually comprise several phases to progressively improve strength and endurance as well as hip mobility and stability.13,14 Recently, different authors reported that changes in hip muscles strength per se are of great importance in the rehabilitation success.15, 16, 17, 18, 19, 20, 21, 22
Still, current recommendations for FAI rehabilitation are based on expert opinions or protocols used for other surgical procedures23 but not on objective and impairments-based criteria. This could potentially lead to impairment of clinical reasoning and distort decision-making.24 This emphasizes the importance of strength measurement in evidence-based physical therapy, which can be performed using isokinetic or handheld dynamometry (HHD), with the latter having the advantage of being inexpensive, easy to use, and less time-consuming.
There are little published data on hip muscle strength evolution after rehabilitation of FAI arthroscopy. One recent study revealed a significant strength alteration at 3 postoperative months, notably for abductors.20 However, it should be noted that this study reported the strength changes halfway through the FAI rehabilitation program solely. Therefore, the purpose of the present study was to evaluate the variations in hip muscle strength following arthroscopy and 6-month rehabilitation in patients treated for FAI. We hypothesized that patient hip muscle strength would be improved beyond the pathologic status they presented before surgery.
Methods
The authors retrospectively evaluated a series of patients treated by arthroscopy for FAI at La Tour Hospital from March 2020 to December 2022. Patients were included in this study if they were (1) living in the Geneva area and (2) performed their entire rehabilitation program at La Tour Hospital. Patients were excluded if they had the following a priori defined criteria: pregnancy, previous lower extremity surgeries, arthritis, stroke, spinal cord lesion or injury, peripheral diabetes, or any other type of neurologic disease that could influence the nervous system or signs of osteoarthritis. All patients presented a cam, pincer morphology, or mix of both with or without labral lesions. All patients were operated on by the same senior surgeon (P.C.) at La Tour Hospital following the same arthroscopic technique detailed below. All patients had a center edge angle (CEA) above 25° without any clinical or radiologic findings of miscroinstability. All patients had preoperative x-rays, arthro–magnetic resonance imaging (arthro-MRI), and computed tomography (CT) scans. Anteversion was assessed using the Murphy’s method on preoperative CT scans.25 Since this study is exploratory and based on clinical data that are routinely collected at our institution to evaluate patients’ clinical improvement, an a priori approval from the local ethical committee was not required. However, all patients included in this study gave their written informed consent for the use of their data in research projects.
Pre- and Postoperative Hip Muscle Strength Assessment
The isometric muscle strengths of both hips (maximal voluntary contraction, MVC) were evaluated before surgery as well as at 3 and 6 postoperative months, using HHD (Hoggan MicroFET2; Scientific L.L.C.) with a sampling frequency of 100 Hz.26 The measures concerned 8 hip-related muscle groups: (1) abductors, (2) adductors, (3) flexors, (4) extensors, (5) external/lateral rotators, (6) internal/medial rotators, (7) quadriceps, and (8) hamstrings. All evaluations were performed by a senior physical therapist (G.S.) following a strict methodology (Appendix Fig. 1, available at www.arthroscopyjournal.org).20 Patients were evaluated after a 6-minute warmup on a stationary bike in different testing positions, as described by Thorborg et al.27 in 2013. According to the recommendations by Thorborg et al.,27 the patients stabilized themselves by holding the examination table while a fixation belt was used to obtain a better test-retest reliability. After explaining procedures, 3 isometric maximum voluntary contractions of 6 seconds, separated by 30 seconds of rest, were performed on each muscle group under verbal encouragement. The highest value of the 3 repetitions was recorded. If the last measurement was the highest, another measurement was conducted until no further force increase was measured. Peak forces were measured in Newtons and then normalized by the arm lever (in meters) and by the body weight (kilogram), in order to be displayed in Nm/kg units.
Surgical Technique
Patients were placed in a supine position on a traction table. Both lower limbs were placed in minimal traction (1.5 cm of joint space) with a perineal post system (Arthrex) for a variable amount of time, and a standard disinfection/draping was performed. The procedure was performed using the anterolateral (AL), anterior-anterolateral (AAL), and medial-anterior (MAP) portals. For the central compartment, the status of the cartilage, labrum, and round ligament was checked. In case of an unstable labral lesion, debridement and/or reinsertion using anchors were performed. The presence of possible synovitis was also checked and, if positive, led to a synovectomy with capsular preservation. The shape and size of the anterior inferior iliac spine (AIIS) were correlated to the preoperative CT examination, and if needed, reduction of the AIIS was performed. Once these procedures were completed, the traction was released and an L-shaped capsulotomy keeping intact the medial limb of the iliofemoral ligament was performed. The hip was tested in flexion and internal rotation for any signs of impingement between the acetabular rim and the femoral neck. A head-neck recontouring was performed as necessary while respecting the retinacular vessels. The vertical capsulotomy was repaired with absorbable sutures, and a clinical and radiologic checkup was finally performed followed by a classical closure with Prolene sutures.
Postoperative Patient Rehabilitation
The supervised rehabilitation protocol started on the intervention day a few hours after surgery in accordance with the 2019 International Society for Hip Arthroscopy (ISHA) convention (Appendix Table 1, available at www.arthroscopyjournal.org).
First Stage—Immediate Postoperative
During hospitalization, patients walked using crutches with 15 kg partial weight bearing on the operated limb. Three or 4 days after surgery, the patients went home and were asked to keep using a continuous motion device.
Second Stage—Early Impairment
The second stage started 10 days following surgery when the scar healing allowed the patients to go into water. Nine hydrotherapy group sessions were then performed in a pool to mobilize the tissues and facilitate the kinematics of the hip while paying attention to the patients’ constraints and mobilization limitations. A land-based physical therapy session was added between the fourth and fifth hydrotherapy sessions to explain exercises to be performed independently at home. A booklet was then distributed at the end of the session to help patients reproduce correctly the aforementioned exercises.
Third Stage—Late Impairment
Full weight bearing was then progressively allowed in a third stage but adapted to patient pain. Specific attention was therefore paid to the gait pattern and hip muscle voluntary contractions. This third stage also comprised biweekly individual sessions of 30 minutes to closely follow the evolution of patients’ symptoms. A first functional test was performed to assess hip muscle strength at the end of this stage (around 3 postoperative months).
Fourth Stage—Functional Restoration
A progressive load was then applied during the fourth and last stage to increase hip muscle strength, endurance, function, dynamic balance, and gait pattern. Progressive and adapted physical activities were recommended, and manual therapy techniques were used to improve hip range of motion and reduce pain.13,28, 29, 30, 31 Rehabilitation was finally completed with a phase of muscle strengthening based on heavy-load exercises and return to full function of the hip. An additional stage of return to sports activity until return to presymptomatic performance (RTP) if necessary was also carried out, which generally lasted 1 to 3 months according to patient characteristics and targets. A second functional test was performed to assess hip muscle strength at the end of this last stage (around 6 postoperative months).
Sample Size Calculations and Statistical Analyses
Beck et al.32 recently published that preoperative hip extension strength was an important predictor of achieving a postoperative patient acceptable symptom state. Furthermore, the extensor peak force for operated hips was reported to be 2.97 ± 0.83 Nm/kg in FAI patients,33 and a difference of 15% in muscle strength appears to be clinically relevant since it has been used in a sample size calculation for a comparable study.34 Based on the aforementioned findings, 29 FAI patients would be required to significantly detect a 15% difference in extensor MVC on operated hips with a statistical power of 0.80 and a significant α level of 0.05.
Descriptive statistics were used to summarize the data. Continuous variables were reported as mean ± standard deviation and 95% confidence intervals (CIs) while categorical data were reported as proportions. The normality of continuous variable distributions was assessed by the Shapiro-Wilk test. Muscle strength comparisons between different time points as well as between operated and nonoperated hips were also conducted using Wilcoxon signed rank tests or paired Student t tests. The effect size of the rehabilitation was calculated using Hedges’s g for the different studied outcomes and interpreted as follows: negligible (Hedges’s g < 0.2), small (0.2 ≤ Hedges’s g < 0.5), medium (0.5 ≤ Hedges’s g < 0.8), and large (0.8 ≤ Hedges’s g < 1.2).35 Relative strength changes between time points were interpreted using a threshold of 15%, which seems to be clinically relevant.34 The strength improvement at 6 months compared to the preoperative status was also interpreted using the additional difference in strength that exists between a healthy and nonoperated FAI hip (not available for the quadriceps and hamstrings): extensors (1%), abductors (11%), internal rotators (14%), external rotators (18%), flexors (26%), and adductors (28%).36 The correlation between hip muscle strength change on the operated and nonoperated sides was analyzed for the muscles weakened after surgery using Pearson coefficient, reported with 95% CI and interpreted as negligible (r = 0.00 to 0.09), weak (r = 0.10 to 0.39), moderate (r = 0.40 to 0.69), strong (r = 0.70 to 0.89), or very strong (r = 0.90 to 1.00).37 The analyses were performed using R (version 3.6.2; R Foundation for Statistical Computing), and P values <.05 were considered significant.
Results
Seventy-five cases were operated during the period of interest, with 29 finally included and rigorously evaluated before and after surgery at the Motion Analysis Laboratory of the physical therapy department. Included patients were aged 26.9 ± 7.1 years at index surgery and comprised 25 women (86%) and 4 men (14%). None of the patients were excluded.
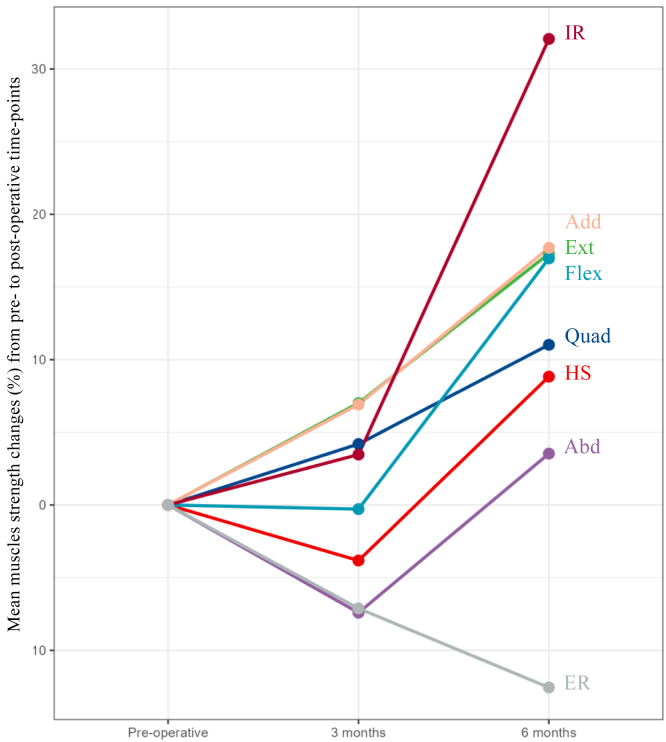
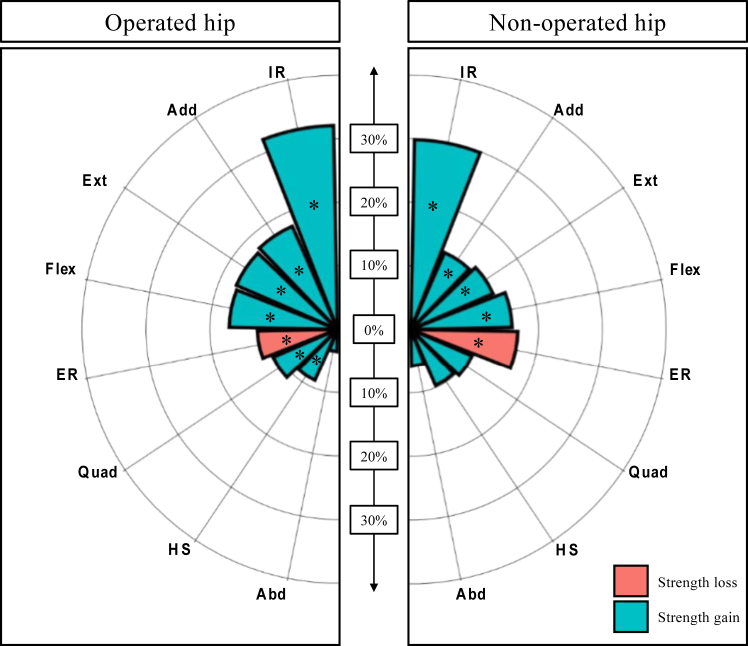
Several hip muscles, mainly abductors and external rotators, remained weakened 3 months after surgery (Table 1, Fig 1). However, most muscles on the operated side were statistically stronger after 6 postoperative months compared to the preoperative pathologic status: hamstrings (9% ± 17%, Hedges’s g = 0.275), quadriceps (11% ± 27%, Hedges’s g = 0.369), extensors (17% ± 32%, Hedges’s g = 0.472), flexors (17% ± 29%, Hedges’s g = 0.586), adductors (18% ± 23%, Hedges’s g = 0.621), and internal rotators (32% ± 36%, Hedges’s g = 0.896) (Fig 2). It is worth mentioning that abductors exhibited a comparable strength (4% ± 26%, Hedges’s g = 0.002) and that external rotators remained significantly weakened (–13% ± 26%, Hedges’s g = –0.745) despite the complete rehabilitation protocol.
Table 1.
Pre- and Postoperative Hip Muscle Strength (Nm/kg)
| Characteristic | Mean | 95% CI | P Value | Hedges’s g |
|---|---|---|---|---|
| Quadriceps | ||||
| Preoperative | 2.70 | 2.48 to 2.92 | ||
| 3 months | 2.74 | 2.55 to 2.92 | .665 | 0.070 |
| Change (%) | 4 | –5 to 13 | ||
| 6 months | 2.91 | 2.69 to 3.12 | .045 | 0.369 |
| Change (%) | 11 | 1 to 21 | ||
| Hamstrings | ||||
| Preoperative | 1.48 | 1.34 to 1.63 | ||
| 3 months | 1.39 | 1.27 to 1.51 | .088 | –0.263 |
| Change (%) | –4 | –11 to 3 | ||
| 6 months | 1.58 | 1.45 to 1.72 | .041 | 0.275 |
| Change (%) | 9 | 3 to 15 | ||
| Extensors | ||||
| Preoperative | 2.10 | 1.89 to 2.32 | ||
| 3 months | 2.18 | 1.93 to 2.44 | .416 | 0.132 |
| Change (%) | 7 | –5 to 19 | ||
| 6 months | 2.39 | 2.15 to 2.63 | .006 | 0.472 |
| Change (%) | 17 | 5 to 30 | ||
| Flexors | ||||
| Preoperative | 1.83 | 1.68 to 1.99 | ||
| 3 months | 1.79 | 1.64 to 1.94 | .511 | –0.109 |
| Change (%) | 0 | –9 to 8 | ||
| 6 months | 2.09 | 1.91 to 2.26 | .003 | 0.586 |
| Change (%) | 17 | 6 to 28 | ||
| Abductors | ||||
| Preoperative | 1.92 | 1.77 to 2.08 | ||
| 3 months | 1.74 | 1.60 to 1.88 | .009 | –0.465 |
| Change (%) | –7 | –15 to 0 | ||
| 6 months | 1.92 | 1.80 to 2.05 | .992 | 0.002 |
| Change (%) | 4 | –6 to 13 | ||
| Adductors | ||||
| Preoperative | 1.74 | 1.59 to 1.90 | ||
| 3 months | 1.84 | 1.68 to 1.99 | .047 | 0.228 |
| Change (%) | 7 | 0 to 14 | ||
| 6 months | 2.02 | 1.84 to 2.20 | <0.001 | 0.621 |
| Change (%) | 18 | 9 to 26 | ||
| Internal rotators | ||||
| Preoperative | 1.10 | 0.98 to 1.21 | ||
| 3 months | 1.11 | 1.00 to 1.23 | .738 | 0.055 |
| Change (%) | 3 | –6 to 12 | ||
| 6 months | 1.40 | 1.26 to 1.53 | <0.001 | 0.896 |
| Change (%) | 32 | 18 to 46 | ||
| External rotators | ||||
| Preoperative | 1.15 | 1.00 to 1.30 | ||
| 3 months | 1.03 | 0.89 to 1.18 | .040 | –0.303 |
| Change (%) | –7 | –16 to 2 | ||
| 6 months | 0.92 | 0.86 to 0.99 | .002 | –0.745 |
| Change (%) | –13 | –23 to –2 |
CI, confidence interval.
Bold P-values indicate statistically significant differences.
Fig 1.
Line plot illustrating the muscle strength changes (%) from preoperative to postoperative time points.
Fig 2.
Pre- to postoperative changes (at 6 months) in muscle strength (%) on the operated and nonoperated hips. ∗Indicates a statistically significant variation. (Abd, abductors; Add, adductors; ER, external rotators; Ext, extensor; Fl, flexors; HS, hamstrings; IR, internal rotators; Quad, quadriceps.)
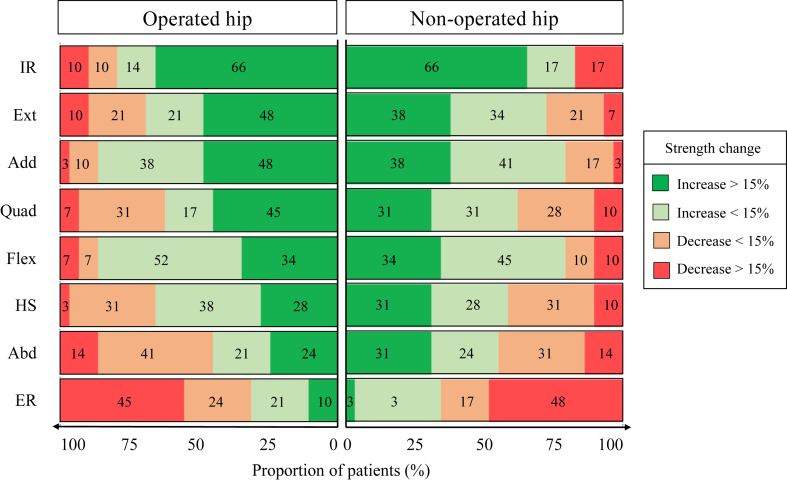
Among the muscles that were significantly strengthened at 6 months, a considerable proportion of patients reached a strength level that was above their pathologic preoperative status for the quadriceps (62%), hamstrings (66%), extensors (69%), internal rotators (80%), and adductors and flexors (86%) (Fig 3).
Fig 3.
Patient distribution according to the relevance of their muscle strength change 6 months following arthroscopy on the operated and nonoperated hip. Dark green and red indicate clinically relevant variations. (Abd, abductors; Add, adductors; ER, external rotators; Ext, extensor; Fl, flexors; HS, hamstrings; IR, internal rotators; Quad, quadriceps.)
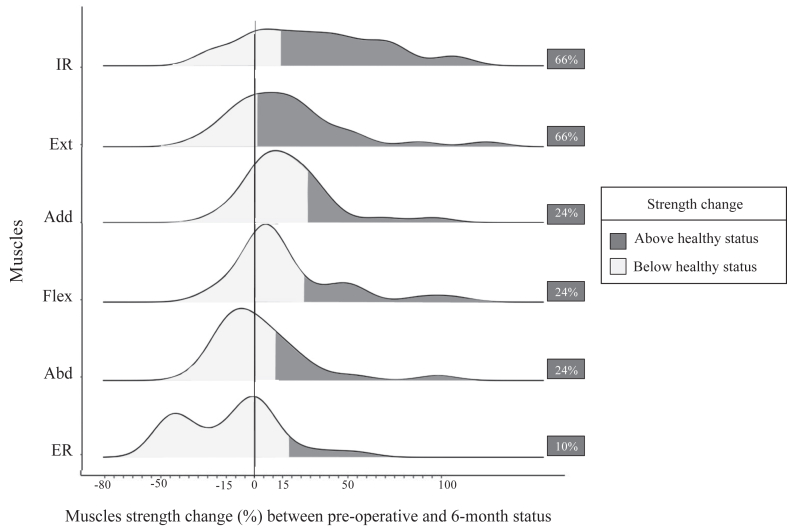
According to Casartelli et al.36 thresholds, a healthy strength level was obtained by 24% of the patients for the abductors, adductors, and flexors and 66% for the extensors and internal rotators (Fig 4). It is noteworthy, however, that almost half of the patients (45%) experienced a decrease in external rotator strength by more than 15% compared to initial pathologic status, with only 10% of the patients having a final strength equivalent or greater to a healthy status.
Fig 4.
Ridge line plot illustrating patients’ distribution and muscle strength changes according to healthy levels. (Abd, abductors; Add, adductors; ER, external rotators; Ext, extensor; Fl, flexors; HS, hamstrings; IR, internal rotators; Quad, quadriceps.)
On the nonoperated side, strengths exhibited at 6 postoperative months were greater than before surgery for the extensors (14% ± 24%, Hedges’s g = 0.523), flexors (16% ± 28%, Hedges’s g = 0.539), adductors (13% ± 20%, Hedges’s g = 0.523), and internal rotators (30% ± 37%, Hedges’s g = 0.669). Small and negligible effects could be observed for the quadriceps (10% ± 28%, Hedges’s g = 0.265), hamstrings (10% ± 26%, Hedges’s g = 0.218), and abductors (6% ± 23%, Hedges’s g = 0.115) (Fig 2, Appendix Table 2, available at www.arthroscopyjournal.org). Similarly to the operated side, the nonoperated external rotators exhibited a significant decrease at 6 months compared to the preoperative strength level (–17% ± 25%, Hedges’s g = –0.900). This strength decrease was beyond 15% for 48% of the cases and strongly correlated to that of the operated side (r = 0.86; 95% CI, 0.72-0.93; P < .001).
Finally, none of the included patients experienced a complication during surgery or within the 6 following months.
Discussion
The principal finding of this study was that arthroscopy combined with a 6-month rehabilitation has strengthened 6 of 8 periarticular hip muscle groups, restored preoperative abductor strength, but failed to recover preoperative external rotator strength. Thus, the initial hypothesis is almost confirmed since 7 of 8 muscle groups at least regained their preoperative strength levels. Specifically, most of the patients experienced a significant strength improvement at 6 months on quadriceps, hamstrings, extensors, flexors, adductors, and internal rotators compared to their preoperative status. However, specific attention should be paid to external rotators, which continuously decreased in strength throughout the rehabilitation period and not only on the operated side.
The proportion of patients who improved their strength at 6 postoperative months beyond their preoperative status ranged from 62% for the quadriceps to 86% for the flexors (Fig 3). The consistency of the bilateral findings might indicate that strength improvements are directly related to the physical therapy program rather than surgery, although the absence of a control group in this study prevents us from confirming it. Even though these findings seem very satisfactory, the lack of data on hip muscle strength changes after FAI arthroscopy in the scientific literature prevents us from drawing any conclusions. Beyond that, it remains difficult to evaluate whether such improvements are clinically relevant since reaching a strength level exhibited at a pathologic status is surely insufficient.38,39 Owing to the work published by Casartelli et al.,36 it seems that FAI patients, before being operated on, present at this time point a global strength deficit of 16% on average for most hip muscles compared to healthy matched participants. This threshold, even though being unspecific to each muscle, approximates well the 15% we chose as a clinically relevant change for hip muscle strength. According to healthy strength levels,36 almost 25% of our patients reached a healthy strength status on flexors, adductors, and abductors as well as 66% on extensors and internal rotators (Fig 4). Further studies are therefore needed to optimize current strengthening protocols after FAI arthroscopy to make our patients stronger and closer to healthy levels. Individualized and/or longer physical therapy after FAI could be recommended for some patients to bring them back to healthy levels or to higher expectations if needed.
Another important finding of this study was the continuous strength decrease in external rotators following 6 months of rehabilitation. Almost half of the included patients exhibited a decrease in external rotator strength by more than 15%. Furthermore, this phenomenon was also observable on the nonoperated side (48%) with a strong correlation between the two, underlining that this strength decrease was bilateral. Our FAI rehabilitation protocol comprises, however, different bilateral exercises that are known to be effective at increasing the activation of external rotators (gluteus maximus, medius, and minus) such as step-up movement and its variants (crossover and lateral), as well as monster walk band at knee or pelvic drop.40 Furthermore, the authors do not think such findings could be related to traction during surgery since the latter was minimal with only 1.5 cm of joint space.
The real mechanism behind the loss of external rotator strength might be more complex. Persistent strength deficits following surgery have already been observed in different pathologies despite the use of recommended heavy reinforcement exercises. Modulations of the central nervous system are described and may implicate cortical or spinal pathways while affecting both involved and uninvolved limbs.41 This could explain the strength deficits obtained for external rotators on the contralateral limb. Furthermore, we know that inhibitory and/or facilitatory mechanisms acting at different levels of the central nervous system may affect both agonist and antagonist muscle groups around the joint.42 This element may provide an explanation of the improvements of internal rotator strength concomitant with impairments of external rotators observed in our study.
Limitations
This exploratory study has several limitations. First, our sample size might not be high enough to statistically detect light muscle strength changes. Second, this study was only focused on objective assessments of strength and did not comprise radiologic parameters or patient-reported outcome measures. Moreover, isometric assessment of muscle strength is not a perfect encapsulation of patient strength or function, although handheld dynamometers remain easy to use and affordable.24 Third, approximately 40% of the operated cases could be included in this study. However, the included cases did not differ from the others in terms of age (26.9 [95% CI, 24.3-29.5] vs 27.4 [95% CI, 25.2-29.6], P = .944) and sex (women, 86% vs 70%, P = .568). Fourth, our study cohort mainly comprised women (86%) and might not be comparable to FAI patients followed in other institutions. Even though the strength changes of hip muscles did not statistically differ between men and women, our results might not be generalizable. Fifth, this study did not comprise a control group and a standardized preoperative physical therapy. Additionally, the authors did not use Bonferroni correction in their analyses since this exploratory study could be hindered by such conservative statistical methods.43 Furthermore, the principal analysis was based on the evaluation of strength changes between the preoperative and 6-month follow-up status. Thus, their statistical significance should not be affected by the fact that additional information on intermediate strength changes at 3 postoperative months were reported.
Conclusions
Arthroscopic treatment followed by 6-month rehabilitation granted to most FAI patients a higher strength level for several hip muscles, except for abductors and external rotators, which remained comparable and weakened, respectively.
Disclosure
The authors report no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Footnotes
G.S. and H.B. contributed equally to this work. F.F. and P.C. contributed equally to this work.
Supplementary Data
References
- 1.Anzillotti G., Iacomella A., Grancagnolo M., et al. Conservative vs. surgical management for femoro-acetabular impingement: A systematic review of clinical evidence. J Clin Med. 2022;11:58522. doi: 10.3390/jcm11195852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gatz M., Driessen A., Eschweiler J., Tingart M., Migliorini F. Arthroscopic surgery versus physiotherapy for femoroacetabular impingement: A meta-analysis study. Eur J Orthop Surg Traumatol. 2020;30:1151–1162. doi: 10.1007/s00590-020-02675-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhu Y., Su P., Xu T., Zhang L., Fu W. Conservative therapy versus arthroscopic surgery of femoroacetabular impingement syndrome (FAI): A systematic review and meta-analysis. J Orthop Surg Res. 2022;17:296. doi: 10.1186/s13018-022-03187-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ferreira G.E., O'Keeffe M., Maher C.G., et al. The effectiveness of hip arthroscopic surgery for the treatment of femoroacetabular impingement syndrome: A systematic review and meta-analysis. J Sci Med Sport. 2021;24:21–29. doi: 10.1016/j.jsams.2020.06.013. [DOI] [PubMed] [Google Scholar]
- 5.Byrd J.W.T. Editorial commentary: Hip arthroscopy—a microcosm in the evolution of arthroscopy in sports medicine. Arthroscopy. 2020;36:773–775. doi: 10.1016/j.arthro.2020.01.005. [DOI] [PubMed] [Google Scholar]
- 6.Griffin D.R., Dickenson E.J., O'Donnell J., et al. The Warwick Agreement on femoroacetabular impingement syndrome (FAI syndrome): An international consensus statement. Br J Sports Med. 2016;50:1169–1176. doi: 10.1136/bjsports-2016-096743. [DOI] [PubMed] [Google Scholar]
- 7.Maempel J.F., Ting J.Z., Gaston P. Assessing the outcome of hip arthroscopy for labral tears in femoroacetabular impingement using the minimum dataset of the British Non-arthroplasty Hip Register: A single-surgeon experience. Arthroscopy. 2018;34:2131–2139. doi: 10.1016/j.arthro.2018.02.038. [DOI] [PubMed] [Google Scholar]
- 8.Gillinov S.M., Kim D.N., Moran J., et al. Low rates of 5-year secondary surgery and postoperative complications after primary hip arthroscopy in more than 30,000 patients. Arthroscopy. 2023;39:1639–1648. doi: 10.1016/j.arthro.2023.01.100. [DOI] [PubMed] [Google Scholar]
- 9.Jan K., Fenn T.W., Kaplan D.J., Nho S.J. Patients maintain clinically significant outcomes at 5-year follow-up after hip arthroscopy for femoroacetabular impingement syndrome: A systematic review. Arthroscopy. 2023;39:1869–1881.e1861. doi: 10.1016/j.arthro.2023.04.021. [DOI] [PubMed] [Google Scholar]
- 10.Dwyer T., Whelan D., Shah P.S., Ajrawat P., Hoit G., Chahal J. Operative versus nonoperative treatment of femoroacetabular impingement syndrome: A meta-analysis of short-term outcomes. Arthroscopy. 2020;36:263–273. doi: 10.1016/j.arthro.2019.07.025. [DOI] [PubMed] [Google Scholar]
- 11.Hassan M.M., Farooqi A.S., Feroe A.G., et al. Open and arthroscopic management of femoroacetabular impingement: A review of current concepts. J Hip Preserv Surg. 2022;9:265–275. doi: 10.1093/jhps/hnac043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Minkara A.A., Westermann R.W., Rosneck J., Lynch T.S. Systematic review and meta-analysis of outcomes after hip arthroscopy in femoroacetabular impingement. Am J Sports Med. 2019;47:488–500. doi: 10.1177/0363546517749475. [DOI] [PubMed] [Google Scholar]
- 13.Heerey J., Risberg M.A., Magnus J., et al. Impairment-based rehabilitation following hip arthroscopy: Postoperative protocol for the HIP ARThroscopy international randomized controlled trial. J Orthop Sports Phys Ther. 2018;48:336–342. doi: 10.2519/jospt.2018.8002. [DOI] [PubMed] [Google Scholar]
- 14.Lynch T.S., Minkara A., Aoki S., et al. Best practice guidelines for hip arthroscopy in femoroacetabular impingement: Results of a Delphi process. J Am Acad Orthop Surg. 2020;28:81–89. doi: 10.5435/JAAOS-D-18-00041. [DOI] [PubMed] [Google Scholar]
- 15.Di Benedetto P., Vidi D., Buttironi M.M., Mancuso F., Ricciarelli M., Causero A. Outcomes in arthroscopic surgery and proposal rehabilitative treatment in femoral acetabular impingement syndrome. Acta Biomed. 2022;92 doi: 10.23750/abm.v92iS3.12710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Freke M.D., Kemp J., Svege I., Risberg M.A., Semciw A., Crossley K.M. Physical impairments in symptomatic femoroacetabular impingement: A systematic review of the evidence. Br J Sports Med. 2016;50:1180. doi: 10.1136/bjsports-2016-096152. [DOI] [PubMed] [Google Scholar]
- 17.Ishoi L., Thorborg K., Kemp J.L., Reiman M.P., Holmich P. Maximal hip muscle strength and rate of torque development 6-30 months after hip arthroscopy for femoroacetabular impingement syndrome: A cross-sectional study. J Sci Med Sport. 2021;24:1110–1115. doi: 10.1016/j.jsams.2021.05.006. [DOI] [PubMed] [Google Scholar]
- 18.Mayne E., Memarzadeh A., Raut P., Arora A., Khanduja V. Measuring hip muscle strength in patients with femoroacetabular impingement and other hip pathologies: A systematic review. Bone Joint Res. 2017;6:66–72. doi: 10.1302/2046-3758.61.BJR-2016-0081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Saavedra M., Moraga R., Diaz P., Camacho D., Mardones R. Comparative analysis of kinesiotherapy rehabilitation after hip arthroscopy, quantified by Harris and Vail hip scores: A retrospective study. Muscles Ligaments Tendons J. 2016;6:420–426. doi: 10.11138/mltj/2016.6.3.420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Servant G., Fourchet F., Pernoud A., Bothorel H., Christofilopoulos P. Evolution of hip muscles strength in femoroacetabular impingement patients treated by arthroscopy or surgical hip dislocation: A Retrospective exploratory study. Biology (Basel) 2022;11:1765. doi: 10.3390/biology11121765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Reiman M.P., Peters S., Sylvain J., Hagymasi S., Ayeni O.R. Prevalence and consistency in surgical outcome reporting for femoroacetabular impingement syndrome: A scoping review. Arthroscopy. 2018;34:1319–1328.e1319. doi: 10.1016/j.arthro.2017.11.037. [DOI] [PubMed] [Google Scholar]
- 22.Yang F., Mamtimin M., Duan Y.P., et al. Volume of gluteus maximus and minimus increases after hip arthroscopy for femoroacetabular impingement syndrome. Arthroscopy. 2021;37:862–870. doi: 10.1016/j.arthro.2020.10.049. [DOI] [PubMed] [Google Scholar]
- 23.Tranovich M.J., Salzler M.J., Enseki K.R., Wright V.J. A review of femoroacetabular impingement and hip arthroscopy in the athlete. Phys Sportsmed. 2014;42:75–87. doi: 10.3810/psm.2014.02.2050. [DOI] [PubMed] [Google Scholar]
- 24.Servant G., Barrue-Belou S., Gojanovic B., Fourchet F. Avoiding cognitive bias: example of quantified assessment of muscle strength. Rev Med Suisse. 2023;19:1370–1373. doi: 10.53738/REVMED.2023.19.835.1370. [DOI] [PubMed] [Google Scholar]
- 25.Murphy S.B., Simon S.R., Kijewski P.K., Wilkinson R.H., Griscom N.T. Femoral anteversion. J Bone Joint Surg Am. 1987;69:1169–1176. [PubMed] [Google Scholar]
- 26.Mentiplay B.F., Perraton L.G., Bower K.J., et al. Assessment of lower limb muscle strength and power using hand-held and fixed dynamometry: A reliability and validity study. PLoS One. 2015;10 doi: 10.1371/journal.pone.0140822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Thorborg K., Bandholm T., Holmich P. Hip- and knee-strength assessments using a hand-held dynamometer with external belt-fixation are inter-tester reliable. Knee Surg Sports Traumatol Arthrosc. 2013;21:550–555. doi: 10.1007/s00167-012-2115-2. [DOI] [PubMed] [Google Scholar]
- 28.Kemp J.L., Johnston R.T.R., Coburn S.L., et al. Physiotherapist-led treatment for femoroacetabular impingement syndrome (the PhysioFIRST study): A protocol for a participant and assessor-blinded randomised controlled trial. BMJ Open. 2021;11 doi: 10.1136/bmjopen-2020-041742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kemp J.L., Risberg M.A., Mosler A., et al. Physiotherapist-led treatment for young to middle-aged active adults with hip-related pain: Consensus recommendations from the International Hip-related Pain Research Network, Zurich 2018. Br J Sports Med. 2020;54:504–511. doi: 10.1136/bjsports-2019-101458. [DOI] [PubMed] [Google Scholar]
- 30.Takla A., O'Donnell J., Voight M., et al. The 2019 International Society of Hip Preservation (ISHA) physiotherapy agreement on assessment and treatment of femoroacetabular impingement syndrome (FAIS): An international consensus statement. J Hip Preserv Surg. 2020;7:631–642. doi: 10.1093/jhps/hnaa043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wahoff M., Dischiavi S., Hodge J., Pharez J.D. Rehabilitation after labral repair and femoroacetabular decompression: Criteria-based progression through the return to sport phase. Int J Sports Phys Ther. 2014;9:813–826. [PMC free article] [PubMed] [Google Scholar]
- 32.Beck E.C., Nwachukwu B.U., Krivicich L.M., et al. Preoperative hip extension strength is an independent predictor of achieving clinically significant outcomes after hip arthroscopy for femoroacetabular impingement syndrome. Sports Health. 2020;12:361–372. doi: 10.1177/1941738120910134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ishoi L., Thorborg K., Kraemer O., Holmich P. Return to sport and performance after hip arthroscopy for femoroacetabular impingement in 18- to 30-year-old athletes: A cross-sectional cohort study of 189 athletes. Am J Sports Med. 2018;46:2578–2587. doi: 10.1177/0363546518789070. [DOI] [PubMed] [Google Scholar]
- 34.Hallberg S., Sansone M., Augustsson J. Full recovery of hip muscle strength is not achieved at return to sports in patients with femoroacetabular impingement surgery. Knee Surg Sports Traumatol Arthrosc. 2020;28:1276–1282. doi: 10.1007/s00167-018-5337-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cohen J. Statistical Power Analysis for the Behavioral Sciences. Routledge Academic; New York, NY: 1988. [Google Scholar]
- 36.Casartelli N.C., Maffiuletti N.A., Item-Glatthorn J.F., et al. Hip muscle weakness in patients with symptomatic femoroacetabular impingement. Osteoarthritis Cartilage. 2011;19:816–821. doi: 10.1016/j.joca.2011.04.001. [DOI] [PubMed] [Google Scholar]
- 37.Schober P., Boer C., Schwarte L.A. Correlation coefficients: Appropriate use and interpretation. Anesth Analg. 2018;126:1763–1768. doi: 10.1213/ANE.0000000000002864. [DOI] [PubMed] [Google Scholar]
- 38.Nepple J.J., Goljan P., Briggs K.K., Garvey S.E., Ryan M., Philippon M.J. Hip strength deficits in patients with symptomatic femoroacetabular impingement and labral tears. Arthroscopy. 2015;31:2106–2111. doi: 10.1016/j.arthro.2015.04.095. [DOI] [PubMed] [Google Scholar]
- 39.Casartelli N.C., Sutter R., Leunig M. Editorial commentary: Do patients with femoroacetabular impingement syndrome already show hip muscle atrophy? Arthroscopy. 2019;35:1454–1456. doi: 10.1016/j.arthro.2019.02.025. [DOI] [PubMed] [Google Scholar]
- 40.Macadam P., Cronin J., Contreras B. An examination of the gluteal muscle activity associated with dynamic hip abduction and hip external rotation exercise: A systematic review. Int J Sports Phys Ther. 2015;10:573–591. [PMC free article] [PubMed] [Google Scholar]
- 41.Rush J.L., Glaviano N.R., Norte G.E. Assessment of quadriceps corticomotor and spinal-reflexive excitability in individuals with a history of anterior cruciate ligament reconstruction: A systematic review and meta-analysis. Sports Med. 2021;51:961–990. doi: 10.1007/s40279-020-01403-8. [DOI] [PubMed] [Google Scholar]
- 42.Palmieri-Smith R.M., Kreinbrink J., Ashton-Miller J.A., Wojtys E.M. Quadriceps inhibition induced by an experimental knee joint effusion affects knee joint mechanics during a single-legged drop landing. Am J Sports Med. 2007;35:1269–1275. doi: 10.1177/0363546506296417. [DOI] [PubMed] [Google Scholar]
- 43.Bender R., Lange S. Multiple test procedures other than Bonferroni's deserve wider use. BMJ. 1999;318:600–601. doi: 10.1136/bmj.318.7183.600a. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.