Abstract
A 81-year-old male patient presented macroscopic hematuria. Flexible cystoscopy didn't give any diagnosis and urinary citology was negative. Total body CT showed a bladder inguinal hernia with diffuse thickening of the bladder wall, while abdomen bladder was regular.
Diagnosis was difficult because flexible cystoscope could not reach the lesion, preventing diagnosis and bladder resection. We decided to reduce inguinal hernia surgically and perform a partial cystectomy removing the suspect neoplastic part of the bladder. Histologic examination showed muscle invasive squamous cell carcinoma with negative margins. After two years follow up, patient was free from bladder cancer, without any significative LUTS.
Keywords: Muscle invasive bladder cancer, Tumor in vescical hernia, Partial cystectomy
1. Introduction
Radical cystectomy is the gold standard for muscle invasive bladder cancer.1
Conversely, when considering partial cystectomy for primary malignancies, the primary indication is for solitary, primary, muscle-invasive, or high-grade bladder cancer that does not involve specific regions of the bladder such as the bladder trigone, vesical neck, or posterior urethra and that can be resected with adequate surgical margins (1–2 cm).2In this way, a well described indication for partial cystectomy is the removal of an adenocarcinoma or urachal carcinoma that develops in the dome of the bladder.
Following conservative surgery, continuous surveillance, including imaging, cystoscopy, and cytology, is crucial because the local recurrence rate is high (37–78%).3
Patients who undergo partial cystectomy for bladder cancer should undergo cystoscopy and urinary cytologic examination every 3 months for at least 2 years. Regular CT scans of the pelvis and abdomen are recommended in the first several years of follow-up.
With proper patient selection, long-term, bladder-sparing survival rates with partial cystectomy range from 35 to 70%.3
In our report we present a rare case of bladder hernia at the inguino-scrotal level with a neoplasm inside without involvement of the remaining abdominal bladder, making diagnosis challenging with traditional methods due to the neoplasm location.
2. Case presentation
A 81-year-old male patient was admitted to urologic department for macroscopic hematuria.
Patient was on anticoagulant therapy, experiencing episodes of urinary retention caused by blood cots.
Flexible cystoscopy and urinary cytology yielded negative results. An enhanced CT-scan revealed an inguino-scrotal vesical hernia with diffuse wall thickening. The remaining abdominal bladder appeared regular (Fig. 1, Fig. 2).
Fig. 1.
Focus on bladder hernia obtained through CT scan in sagittal projection.
Fig. 2.
Bladder hernia obtained through CT scan in sagittal projection.
Diagnosis was not possible because the angle created by vesical hernia did not allow flexible cystoscopy and obviously rigid resector entrance.
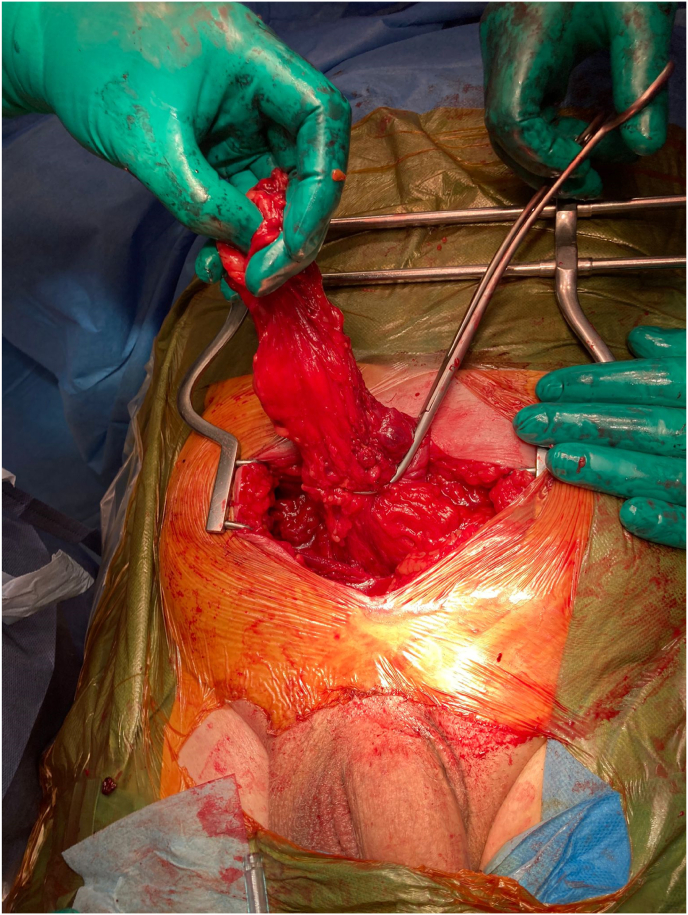
Subsequently, after the patient was explained with adequate counseling both the risk of a probable neoplasm within the bladder hernia and the probable need to carry out a partial cystectomy, we performed a surgical reduction of vesical hernia. During operation, vesical tumoral herniated tissue seemed far from bladder trigone, allowing us to clamp this tissue and remove vesical hernia without opening bladder. Care was taken to leave 2 cm or more of sane tissue (Fig. 3, Fig. 4).
Fig. 3.
Bladder hernia isolation procedure.
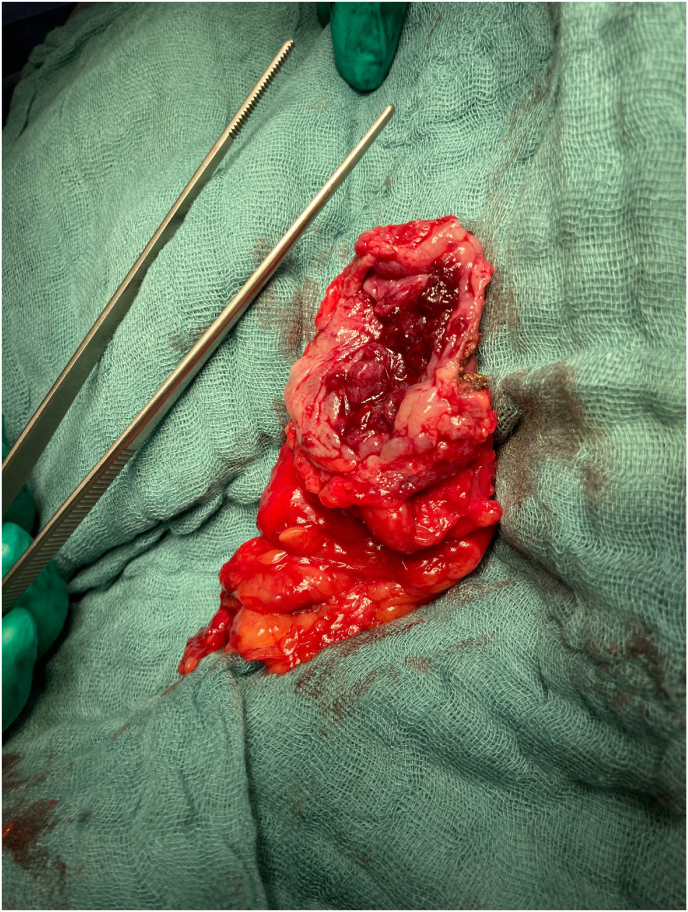
Fig. 4.
Removed bladder hernia.
After partial cystectomy, bladder wall was closed.
Histologic examination showed squamous muscle invasive bladder carcinoma with wide negative surgical margins. No adjuvant therapy was administered.
Patient underwent a close oncological follow up with urinary cytology, cystoscopies every 3 months and CT scan every 6 months. After two years he remains free of oncologic recurrences and does not exhibit significant LUTS (Low urinary tract symptoms).
3. Discussion and conclusions
An inguinal hernia involving the bladder is an uncommon condition, representing less than 4% of all inguinal hernias. Even rarer is the coexistence of a bladder neoplasm within the herniated bladder portion.4 In cases of herniated bladder neoplasms, there is a lack of studies comparing different surgical treatments, partly due to the low number and heterogeneity of enrolled subjects and the low level of evidence in available studies. This is partly attributed to the fact that only around 1% of bladder cancers are intra-diverticular, and instances where the tumor is located in a herniated bladder are even rarer.
In cases where obtaining an histological analysis is feasible, a transurethral resection of bladder (TURB) becomes a viable option. Conversely, the impossibility, as in our case due to anatomical reasons, of obtaining a histological analysis poses a significant challenge requiring alternative solutions.
Traditionally, radical cystectomy has been considered the “gold standard” for managing localized muscle-invasive bladder cancer (MIBC), with curative intent radiotherapy reserved for those with inoperable tumors or multiple co-morbidities precluding surgery.1 On the other hand, partial cystectomy is proposed in specific situations, such as solitary, primary, muscle-invasive, or high-grade bladder cancer that does not involve critical regions of the bladder. This includes the bladder trigone, vesical neck, or posterior urethra, and can be resected with adequate surgical margins (1–2 cm). Additionally, partial cystectomy is considered for the removal of an adenocarcinoma or urachal carcinoma developing in the dome of the bladder.2 Although no randomized controlled trials comparing partial cystectomy (PC) to radical cystectomy (RC) exist, retrospective studies and case series suggest that, in appropriately selected patients, PC may be an acceptable alternative with similar oncological outcomes.2
In our case, conventional cystoscopy failed to diagnose the bladder neoplasm inside the herniated bladder due to anatomical constraints. Instead, a CT scan with contrast injection was employed to visualize the neoplasm. The inability to access the lesion for histological analysis and the absence of a histological examination ruled out the possibility of proceeding with a radical cystectomy.
Consequently, the choice of a partial cystectomy in our case was motivated by the need for an histological examination and the CT scans failure to reveal involvement in critical bladder regions. We conducted a flexible cystoscopy and urinary cytology to confirm the CT results, exclude the involvement of the explorable bladder, and rule out the concomitant presence of carcinoma in situ (CIS). Considering the age of the patient, extension of the neoplasm into the bladder hernia and the risk of possible perforations of the hernia wall with an endoscopic procedure, we opted for partial cystectomy. The partial cystectomy, performed after reducing the bladder hernia, ensured margins free of neoplasia of at least 2 cm. The histological examination revealed squamous muscle-invasive bladder carcinoma with wide negative surgical margins. Considering the negative resection margins, we opted for close follow-up rather than radical cystectomy. In another case report, Na Yin et al. highlight that, despite the diagnosis of squamous cell carcinoma (SCC) of the bladder, a 65-year-old female patient remained free of disease recurrence and metastasis 10 years after partial cystectomy (PC).5
Following partial cystectomy, our patient did not undergo adjuvant therapy but participated in a close follow-up program involving urinary cytology, cystoscopies every three months, and CT scans every six months. Presently, after two years of follow-up, the patient remains free of oncological recurrences and without significant low urinary tract symptoms (LUTS).
Statement of ethics
Published research complies with the guidelines for human studies and is conducted ethically in accordance with the World Medical Association Declaration of Helsinki. The patient has given his written informed consent to publish his case (including publication of images).
Informed consent
Written consent and permission to publish the case report was obtained by the patient.
Funding sources
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for- profit sectors.
CRediT authorship contribution statement
Roberto Falabella: Data curation, Conceptualization. Sabrina La Falce: Writing – review & editing. Franco Camillo Ponti: Writing – review & editing. Giuseppe Di Fino: Writing – original draft, Data curation. Vincenzo Francesco Caputo: Writing – original draft, Data curation. Saveriano Lioi: Methodology, Conceptualization.
Declaration of competing interest
All authors have no conflicts of interest to declare.
Footnotes
A rare case of muscle invasive bladder cancer in a vescical inguinal hernia
References
- 1.Myths about Bladder Preservation in Muscle-Invasive Bladder Cancer. Thiraviyam Elumalai, Nuradh Joseph, Ananya Choudhury. PMID: 36517194 DOI:10.1016/j.semradonc.2022.10.007. [DOI] [PubMed]
- 2.Partial cystectomy for muscle-invasive bladder cancer: a review of the literature. Taylor C. Peak and Ashok Hemal. Transl Androl Urol. 2020;9(6):2938–2945. doi: 10.21037/tau.2020.03.04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Does Partial Cystectomy Compromise Oncologic Outcomes for Patients with Bladder Cancer Compared to Radical Cystectomy? A matched case-control analysis. John J Knoedler 1 , Stephen A Boorjian, Simon P Kim, Christopher J Weight, Prabin Thapa, Robert F Tarrell, John C Cheville, Igor Frank PMID: 22901583 DOI: 10.1016/j.juro.2012.06.029.. [DOI] [PubMed]
- 4.Diagnosis and Treatment of Inguinal Hernia of the Bladder: A Systematic Review of the Past 10 Years 5 Benjamin Branchu, Yohann Renard, Stephane Larre, and Priscilla Leon PMCID: PMC6134980 PMID: 30487042. [DOI] [PMC free article] [PubMed]
- 5.Cystectomy for Bladder Squamous Cell Carcinoma with a 10-year Follow-Up: A Case Report. Na Yin, Wei Zhao, Tao He, Tingchao Li, Xu Lei, Hao He, Zongmin Long, and Yan Wang. PMCID: PMC10446963 PMID: 37621677.. [DOI] [PMC free article] [PubMed]