Abstract
Purpose
To present the clinical and histological characteristics of a basal cell carcinoma, which appears to emanate from the lacrimal punctum.
Observations
An 81-year-old caucasian female presented with an irritating lesion arising from the left upper punctum for approximately four months. Examination demonstrated a pedunculated pinkish lesion emerging from the left upper punctum. The patient elected to pursue the removal of the lesion. An excisional biopsy was performed by placing a curette within the upper eyelid punctum, and the lesion was scooped out. Pathology showed invasive nodular basal cell carcinoma. Following the diagnosis, a wedge resection of the left upper punctal region was performed, which showed no residual carcinoma.
Conclusion and importance
This case describes a unique instance of a basal cell carcinoma clinically appearing to arise solely from the upper eyelid punctum. A level of suspicion should be maintained when excising benign-appearing eyelid lesions, and a histopathological analysis is warranted.
Keywords: Basal cell carcinoma, BCC, Punctum, Mimicking lesion
1. Introduction
Basal cell carcinoma (BCC) is the most common skin cancer. More than 75% of BCC occurs in the head and neck region, whereas approximately 20% appears in the periocular region. Invasion to the orbit is rare, with a reported incidence of about 2%. BCC typically develops in patients over 60 years of age.1 Most BCCs develop on the lower lid, medial canthus, and rarely on the upper eyelid or lateral canthus.2,3 Canalicular or punctal BCC is rare with only a few reported in the literature. Of those reported, none were isolated to the punctal region. Herein, we report a rare case of BCC appearing to be emanating from punctum.
2. Case report
An 81-year-old Caucasian female presented with a gradually growing mass on her left upper eyelid that caused eye irritation for the past four months. The mass had not bled or ulcerated. The patient denied any prior eyelid or punctal injury, infection, lesion, or mass. Past medical history included essential hypertension, hypothyroidism, gout, and malignant neoplasm of the breast. The patient denied a history of skin cancer, excessive sun exposure, smoking, or use of immunosuppressants. On examination, a pedunculated pinkish lesion, appearing to emanate from the left upper punctum was noted (Fig. 1). The rest of the eye exam was normal.
Fig. 1.
Preoperative appearance of BCC emerging from the left upper punctum.
Due to the clinical appearance of the lesion, an excisional biopsy of the lesion was planned. The lesion underwent an incisional biopsy, which was done by scraping the lesion out from the punctal opening using a 2 mm curette. Hemostasis was maintained without need for cautery. Histologic examination revealed an invasive nodular BCC (Fig. 2). Though, no definitive canalicular or punctal structures were identified, the biopsy was limited and may not have been representative of the structural involvement suspected clinically: due to embedding and processing. After obtaining the pathology, a wedge resection of the left upper eyelid, encompassing the punctum, was performed. The repeat excision showed no residual carcinoma. One year later the patient had no clinical evidence of recurrence.
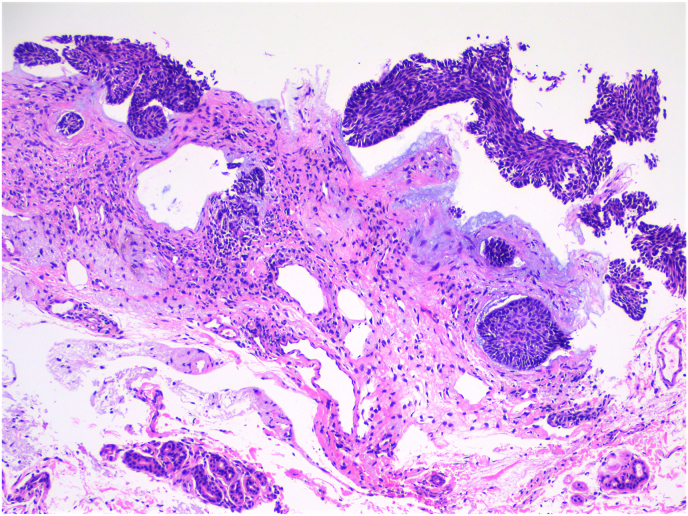
Fig. 2.
Histologic examination demonstrates an invasive basal cell carcinoma of the nodular type with peripheral palisading and artifactual clefting.
3. Discussion
Basal cell carcinoma is a neoplasm that rarely involves the lacrimal system. Lacrimal sac invasion is rare, and canalicular involvement is even more uncommon.4, 5, 6, 7, 8, 9, 10, 11 A case of BCC originating in the lacrimal sac was depicted by Katircioglu et al.,6 while Altan-Yaycioglu et al. described a lacrimal sac BCC with focal squamous differentiation.11
Fosko et al. reported a case of BCC involving the lacrimal canaliculus and punctum. Still, the site origin of origin was debated, and involvement might have been secondary to local tumor invasion.10
Our case has no definite histopathological proof of BCC originating from the canalicular system. Histologically, the canaliculus near the lacrimal punctum is lined with non-keratinized and non-mucin-producing stratified squamous epithelium. It is clearly discriminated from the anteriorly situated keratinized epithelium of the palpebral epidermis.12 In our specific case, the histological background strongly corroborates the likelihood of the eyelid serving as the point of origin. This is evidenced by the presence of keratinizing squamous epithelium with a granular layer, adnexal structures, and the presence of solar elastosis, all of which align with the traditional UV light exposure pathway. Garrett et al. presented a case of BCC with a canalicular origin and speculated that theoretically, the carcinoma could originate from the canalicular basement membrane of the stratified squamous epithelium.8 Therefore, we can postulate that the BCC in our case originated adjacent to that transition junction, either from the palpebral epidermis or canalicular basement membrane. While exceedingly uncommon, basal cell carcinoma can indeed originate from the conjunctiva, and this possibility should be considered within the differential diagnosis. Nevertheless, the presence of background squamous mucosa with keratinization and a granular layer suggests an affiliation with eyelid skin rather than the conjunctiva. Furthermore, the absence of goblet cells provides no support for a conjunctival origin.13 Mohs micrographic surgery of primary periorbital BCC has been reported to have a 5-year cure rate of 97–99%.14,15 In previous cases of BCCs with lacrimal drainage system involvement, carcinomas were excised using Mohs micrographic surgery.4,5,8,10
4. Conclusions
In summary, we report a case of BCC which clinically appeared to emanate from the upper punctum. This clinical presentation, specifically isolated in the punctal region, is an infrequent and unusual occurrence. Providers should have a high level of suspicion and low threshold to obtain a biopsy for atypical benign appearing lesions.
Patient Consent
Consent to publish the case report was not obtained. This report does not contain any personal information that could result in patient identification.
There is no funding or grant support for this case report.
Authorship
All authors attest that they meet the current ICMJE criteria for Authorship. Internal Review Board (IRB) approval was deemed not necessary by the IRB as the research is not generalizable.
CRediT authorship contribution statement
Tom Kornhauser: Writing – review & editing, Writing – original draft, Visualization, Validation, Methodology, Formal analysis, Data curation, Conceptualization. James S. Nix: Writing – review & editing, Writing – original draft, Visualization, Validation, Supervision, Methodology, Investigation, Formal analysis, Data curation. John D. Pemberton: Writing – review & editing, Writing – original draft, Validation, Supervision, Project administration, Methodology, Investigation, Formal analysis, Data curation, Conceptualization.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Furdova A., Kapitanova K., Kollarova A., Sekac J. Periocular basal cell carcinoma-clinical perspectives. Oncol Rev. 2020;14(1) doi: 10.4081/oncol.2020.420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shi Y., Jia R., Fan X. Ocular basal cell carcinoma: a brief literature review of clinical diagnosis and treatment. OncoTargets Ther. 2017;10:2483. doi: 10.2147/OTT.S130371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Malhotra R., Huilgol S.C., Huynh N.T., Selva D. The Australian Mohs database, part I: periocular basal cell carcinoma experience over 7 years. Ophthalmology. 2004;111(4):624–630. doi: 10.1016/j.ophtha.2003.12.003. [DOI] [PubMed] [Google Scholar]
- 4.Rush J.L., Nijhawan R.I. Basal cell carcinoma invasion of the lacrimal system. JAAD Case Rep. 2020;6(4):276. doi: 10.1016/j.jdcr.2020.01.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hatano Y., Terashi H., Kurata S., et al. Invasion of the lacrimal system by basal cell carcinoma. Dermatol Surg. 1999;25(10):823–826. doi: 10.1046/j.1524-4725.1999.99013.x. [DOI] [PubMed] [Google Scholar]
- 6.Katircioglu Y.A., Yildiz E.H., Kocaoglu F.A., Ozer E., Ornek F., Duman S. Basal cell carcinoma in lacrimal sac. Orbit. 2007;26(4):303–307. doi: 10.1080/01676830600987441. [DOI] [PubMed] [Google Scholar]
- 7.Heindl L.M., Jünemann A.G.M., Kruse F.E., Holbach L.M. Tumors of the lacrimal drainage system. Orbit. 2010;29(5):298–306. doi: 10.3109/01676830.2010.492887. [DOI] [PubMed] [Google Scholar]
- 8.Garrett A.B., Dufresne R.G., Ratz J.L., Berlin A.J. Basal cell carcinoma originating in the lacrimal canaliculus. Ophthalmic Surg Lasers Imaging Retina. 1993;24(3):197–199. [PubMed] [Google Scholar]
- 9.Salasche S.J., Shore J.W., Olbricht S.M. Periocular tumors. Dermatol Clin. 1992;10(4):669–685. [PubMed] [Google Scholar]
- 10.Fosko S.W., Gibney M.D., Holds J.B. Basal cell carcinoma involving the lacrimal canaliculus: a documented mechanism of tumor spread. Dermatol Surg. 1997;23(3):203–206. doi: 10.1111/j.1524-4725.1997.tb00023.x. [DOI] [PubMed] [Google Scholar]
- 11.Altan-Yaycioglu R., Bolat F., Akova Y.A. Basosquamous carcinoma of the lacrimal sac: a case report. Orbit. 2007;26(4):267–269. doi: 10.1080/01676830600987565. [DOI] [PubMed] [Google Scholar]
- 12.Kominami R., Yasutaka S., Taniguchi Y., Shinohara H. Anatomy and histology of the lacrimal fluid drainage system. Okajimas Folia Anat Jpn. 2000;77(5):155–160. doi: 10.2535/ofaj1936.77.5_155. [DOI] [PubMed] [Google Scholar]
- 13.Low K.L., Lai Y.P., Alias R., Hamzah J.C. Primary basal cell carcinoma of the conjunctiva. Cureus. 2022;14(11) doi: 10.7759/cureus.31516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mohs F.E. Micrographic surgery for the microscopically controlled excision of eyelid cancers. Arch Ophthalmol. 1986;104(6):901–909. doi: 10.1001/archopht.1986.01050180135046. [DOI] [PubMed] [Google Scholar]
- 15.Moul D.K., Chern P.L., Shumaker P.R., Zelac D.E., Greenway H.T. Mohs micrographic surgery for eyelid and periorbital skin cancer. Int Ophthalmol Clin. 2009;49(4):111–127. doi: 10.1097/IIO.0b013e3181b80482. [DOI] [PubMed] [Google Scholar]