Abstract
Objective
To estimate the excess relative and absolute risks of hospital admissions and emergency department visits for natural causes, cardiovascular disease, and respiratory disease associated with daily exposure to fine particulate matter (PM2.5) at concentrations below the new World Health Organization air quality guideline limit among adults with health insurance in the contiguous US.
Design
Case time series study.
Setting
US national administrative healthcare claims database.
Participants
50.1 million commercial and Medicare Advantage beneficiaries aged ≥18 years between 1 January 2010 and 31 December 2016.
Main outcome measures
Daily counts of hospital admissions and emergency department visits for natural causes, cardiovascular disease, and respiratory disease based on the primary diagnosis code.
Results
During the study period, 10.3 million hospital admissions and 24.1 million emergency department visits occurred for natural causes among 50.1 million adult enrollees across 2939 US counties. The daily PM2.5 levels were below the new WHO guideline limit of 15 μg/m3 for 92.6% of county days (7 360 725 out of 7 949 713). On days when daily PM2.5 levels were below the new WHO air quality guideline limit of 15 μg/m3, an increase of 10 μg/m3 in PM2.5 during the current and previous day was associated with higher risk of hospital admissions for natural causes, with an excess relative risk of 0.91% (95% confidence interval 0.55% to 1.26%), or 1.87 (95% confidence interval 1.14 to 2.59) excess hospital admissions per million enrollees per day. The increased risk of hospital admissions for natural causes was observed exclusively among adults aged ≥65 years and was not evident in younger adults. PM2.5 levels were also statistically significantly associated with relative risk of hospital admissions for cardiovascular and respiratory diseases. For emergency department visits, a 10 μg/m3 increase in PM2.5 during the current and previous day was associated with respiratory disease, with an excess relative risk of 1.34% (0.73% to 1.94%), or 0.93 (0.52 to 1.35) excess emergency department visits per million enrollees per day. This association was not found for natural causes or cardiovascular disease. The higher risk of emergency department visits for respiratory disease was strongest among middle aged and young adults.
Conclusions
Among US adults with health insurance, exposure to ambient PM2.5 at concentrations below the new WHO air quality guideline limit is statistically significantly associated with higher rates of hospital admissions for natural causes, cardiovascular disease, and respiratory disease, and with emergency department visits for respiratory diseases. These findings constitute an important contribution to the debate about the revision of air quality limits, guidelines, and standards.
Introduction
A large number of epidemiological studies have consistently reported that exposure to ambient fine particulate matter (PM2.5) is associated with increased risk of morbidity and mortality.1 2 3 4 5 6 According to the Global Burden of Disease study,7 exposure to PM2.5 accounts for an estimated 7.6% of total global mortality and 4.2% of global disability adjusted life years. In light of this extensive body of evidence, the World Health Organization recently introduced an ambitious new air quality guideline limit in 2021, recommending that the 24 hour average PM2.5 levels should not exceed 15 μg/m3 on more than 3-4 days each year.8 In the US, the current national ambient air quality standards for the 24 hour average PM2.5 (calculated as 98th centile concentrations averaged over a three year period) were set at 35 μg/m3 in 2012, and a revision of these standards is currently being considered.9
Although the literature on the adverse health effects of short term exposure to PM2.5 is vast,1 2 3 4 5 6 several key knowledge gaps remain. Specifically, owing to the accessibility of national vital statistics data and Medicare data, most large scale studies in the US have focused on the health effects of PM2.5 among adults aged ≥65 years,1 5 with relatively few studies including young or middle aged adults; most studies have focused on mortality and hospital admissions as the outcomes,1 2 3 5 6 10 with relatively less information available on the impact of PM2.5 on emergency department visits (ie, where individuals are treated in the emergency department room but not admitted to hospital for inpatient care)11; and no study has specifically examined whether the observed associations persist at daily PM2.5 levels below the 2021 WHO air quality guideline limit.
To tackle these knowledge gaps, we estimated the association between short term exposure to PM2.5 at concentrations below the 2021 WHO air quality guideline limit and the risks of hospital admissions and emergency department visits for natural causes, cardiovascular disease, and respiratory disease among adults with health insurance in the contiguous US from 2010 to 2016 using the healthcare utilization deidentified claims data from the Optum Laboratories Data Warehouse (OLDW). We also examined whether the observed associations of PM2.5 level and morbidity differed across strata defined by age, sex, insurance type, and geographic region.
Methods
Study population
This study used deidentified medical claims data between 1 January 2010 and 31 December 2016 from OLDW.12 This database includes facility and physician claims and enrollment records for enrollees with either commercial or Medicare Advantage health insurance. The database contains longitudinal health information on more than 200 million enrollees, representing a diversity of ages and geographic regions across the US.
Medical claims in OLDW are classified using ICD-9 and ICD-10 (international classification of diseases, ninth revision and 10th revision, respectively) codes, revenue codes, current procedure terminology codes, and place of service codes (see supplementary table S1). We used claims to identify clinical encounters classified as either hospital admissions or emergency department visits. For each patient encounter, we extracted information on age, sex, county of residence, date of service, insurance type, and principal diagnoses. Analyses were limited to adults aged ≥18 years who had hospital admissions or emergency department visits for natural causes (ICD-9: 0-799 or ICD-10: A0-R99), cardiovascular disease (ICD-9: 390-459 or ICD-10: I00-I99), or respiratory disease (ICD-9: 460-519 or ICD-10: J00-J99).
For each health outcome, we aggregated medical claims into daily counts of hospital admissions or emergency department visits by age (18-29, 30-39, 40-49, 50-64, 65-74, or ≥75 years), sex (male v female), insurance type (commercial insurance v Medicare Advantage), and geographic regions of the country, as defined by the US Global Change Research Program’s Fourth National Climate Assessment (NCA4) for each county (see supplementary figure S1).
Environmental data
To estimate daily concentrations of 24 hour average PM2.5 at 1 km × 1 km grid cells in the contiguous US, we used a previously developed spatiotemporal ensemble model.13 The model incorporates three machine learning algorithms: neural network, random forest, and gradient boosting. These algorithms relied on multiple predictor variables, including satellite data at 1 km × 1 km resolution, meteorological conditions, such as ambient temperature, land use variables, such as elevation and road density, and predictions from chemical transport models.13 The predictions of daily PM2.5 level from each algorithm were then combined with a geographically weighted generalized additive model.13 14 Additionally, we obtained monitoring data for PM2.5 from 2156 surveillance sites operated by the US Environmental Protection Agency. To account for spatial and temporal autocorrelation, we calculated lagged PM2.5 levels from monitoring sites and incorporated these as supplementary inputs into the ensemble models, along with the aforementioned mentioned predictor variables.13 14 The final ensemble model showed good performance when predicted values were compared with monitored data, achieving a 10-fold cross validation R2 of 0.86.13 14
We also derived meteorological variables, including daily outdoor ambient air temperature and relative humidity, from the Parameter-elevation Relationships on Independent Slopes model (PRISM) dataset, which is a publicly available gridded climate dataset.15 16 The dataset we used provides daily estimates of several meteorological variables at a horizontal grid spacing of about 4 km across the contiguous US.15 16
Daily PM2.5 concentrations and meteorological variables were calculated at the county level by extracting the grid values at the population centroids for each census tract (based on the 2000 US Census) within a given county. We then calculated the population weighted average values based on the proportion of the county’s population residing in each census tract.15 17 The concentration of PM2.5 and meteorological variables were assigned to each county and the exposure data linked with time series data of hospital admissions and emergency department visits in each respective county.
Statistical analysis
To estimate the association between short term exposure to PM2.5 and risks of hospital admissions and emergency department visits for natural causes, cardiovascular disease, and respiratory disease, we used a case time series design—a novel approach suitable for analyzing small area data.18 19 This design incorporates the self-matched structure in case only models into a traditional time series form, providing a flexible and computationally efficient tool for complex longitudinal data.18 19 In the case time series design, observations defined as cases are collected longitudinally over a period of time at equally spaced time intervals, forming a set of case level time series data.18 The time series of cases can be either individual level outcomes or aggregated measurements over small geographic areas.18 19 In our study, we aggregated medical claims into county specific daily time series of hospital admission and emergency department visit counts and linked these case time series with county level PM2.5 concentrations and meteorological conditions. We chose a case time series design because of its suitability to accommodate the longitudinal time series structure of health outcomes at small area level, strict control for time invariant confounding, and flexibility to adjust time varying confounding in the modeling framework.18 19
We used a conditional quasi-Poisson log-link regression model stratified by year, month, day of week, and county of residence, therefore adjusting for the differential baseline morbidity risk and trends across the different spatiotemporal strata. Meanwhile, we controlled the residual temporal variations with time varying covariates, such as ambient temperature and relative humidity. Consistent with previous studies,1 2 6 our primary analyses considered the moving average of the current and previous day (lag 0-1) PM2.5 as the exposure of interest and assumed a linear exposure-response association between exposure to PM2.5 and risk of morbidity. In the models, we adjusted for the two day moving average of daily mean ambient temperature using a natural cubic spline function with three degrees of freedom, and the two day moving average of daily mean relative humidity using a natural cubic spline function with three degrees of freedom.1 To account for spatial heterogeneity of ambient temperature, we interacted the temperature splines with NCA4 regions. We additionally adjusted for federal holiday (dummy variable). Low level PM2.5 was defined as daily PM2.5 concentrations below the 2021 WHO air quality guideline limit of 15 μg/m3. To estimate the association between short term exposure to low level PM2.5 and risk of morbidity, we restricted our analyses to days with daily PM2.5 concentrations <15 μg/m3. To examine the lag structure of the association, we also fitted the models with separate terms for PM2.5 on the same day of admission (lag 0) and 1 day previously (lag 1).
We presented results as both the excess relative risk and the excess absolute risk of hospital admissions or emergency department visits associated with a 10 µg/m3 increase in PM2.5 concentrations.1 4 20 Excess relative risk was defined as (relative risk−1)×100%, and excess absolute risk was calculated as α×(relative risk−1)/relative risk, where α is the incidence rate of cause specific hospital admissions or emergency department visits (see supplementary eAppendix).
Several sensitivity analyses were performed to examine the robustness of our findings. First, to examine the exposure-response association between exposure to PM2.5 and risk of morbidity, we used a natural cubic spline with three degrees of freedom for lag 0-1 PM2.5. Second, to assess whether our findings were robust to the choice of temperature metric, we replaced the daily mean ambient temperature in the models with daily maximum ambient temperature or daily minimum ambient temperature. Third, to account for spatial heterogeneity in relative humidity, we additionally included an interaction term between relative humidity splines and NCA4 regions in the models. Fourth, to examine the association between exposure to PM2.5 and morbidity across the range of PM2.5 levels, we repeated the main analysis without restricting our analyses to days with daily PM2.5 concentrations <15 μg/m3.
To evaluate potential differences in susceptibility, we examined whether the association between exposure to PM2.5 and risk of morbidity differed across subgroups of the population defined by age, sex, insurance type, and geographic region. We fit separate models for each stratum and conducted Wald tests to evaluate the heterogeneity across these strata.21
All statistical analyses were conducted in R software (version 4.0.2). We used the “gnm” (version 1.1.1) package22 to fit the conditional Poisson regression models and the “dlnm” (version 2.4.2) package23 to model the non-linear exposure-response functions.
Patient and public involvement
As the study used deidentified medical claims data, no patients or members of the public were involved in implementing the study design.
Results
Descriptive statistics
Of the 3144 counties in the contiguous US, we excluded those with no recorded hospital admissions or emergency department visits during the study period, resulting in a total of 2935 to 2939 counties included in the analysis, depending on the specific outcome (see supplementary table S2). Between 1 January 2010 and 31 December 2016, a total of 10.3 million hospital admissions and 24.1 million emergency department visits for natural causes were recorded among 50.1 million adults aged ≥18 years with commercial or Medicare Advantage health insurance (see supplementary table S3). The incidence rates of hospital admissions and emergency department visits for natural causes were 207.9 and 485.7 per million enrollees per day during the study period, respectively (see supplementary table S4).
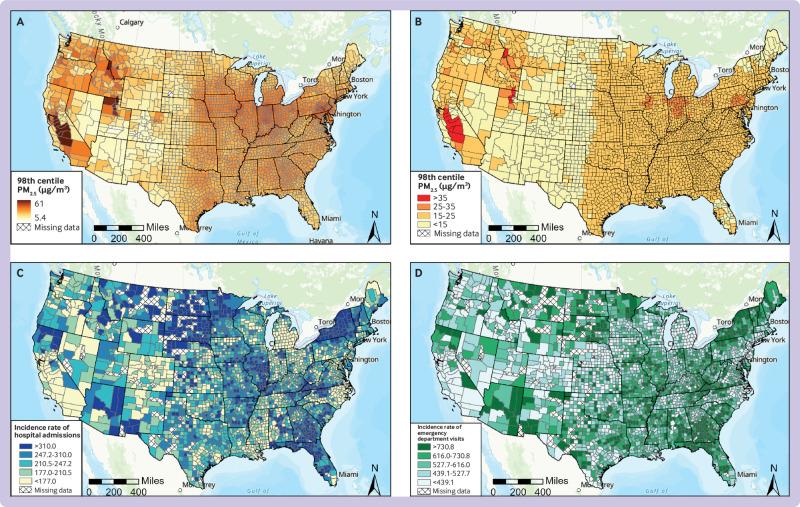
Of these healthcare encounters, more than 50% of hospital admissions and 28% of emergency department visits were for cardiovascular and respiratory diseases, and the distribution varied considerably across different age groups (fig 1 and fig 2). For example, among adults aged <30 years, only 11.3% of all hospital admissions were attributed to cardiovascular or respiratory diseases, but this percentage increased to 92.7% among those aged ≥75 years. In terms of absolute numbers, the incidence rates for hospital admissions and emergency department visits increased with age and tended to be higher in women compared with men, except for cardiovascular disease (see supplementary table S4).
Fig 1.
Number of hospital admissions for cardiovascular, respiratory, and other diseases categorized by age and sex among adults with commercial or Medicare Advantage health insurance in the contiguous US, 2010-16. The width of age groupings is not uniform. The higher number of hospital admissions observed among adults aged 50-64 years partly results from the expansion of age ranges
Fig 2.
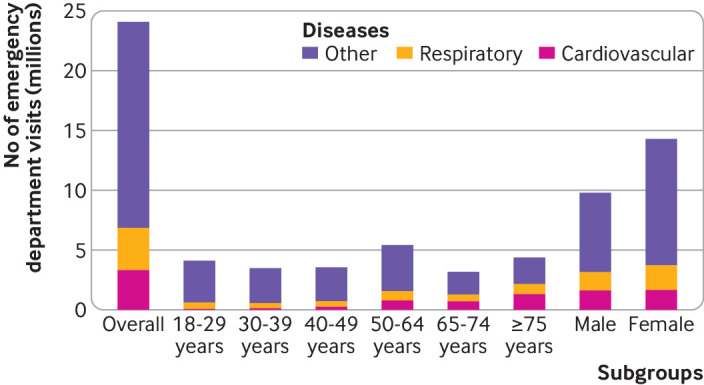
Number of emergency department visits for cardiovascular, respiratory, and other diseases categorized by age and sex among adults with commercial or Medicare Advantage health insurance in the contiguous US, 2010-16. The width of age groupings is not uniform. The higher number of hospital admissions and emergency department visits observed among adults aged 50-64 years partly results from the expansion of age ranges
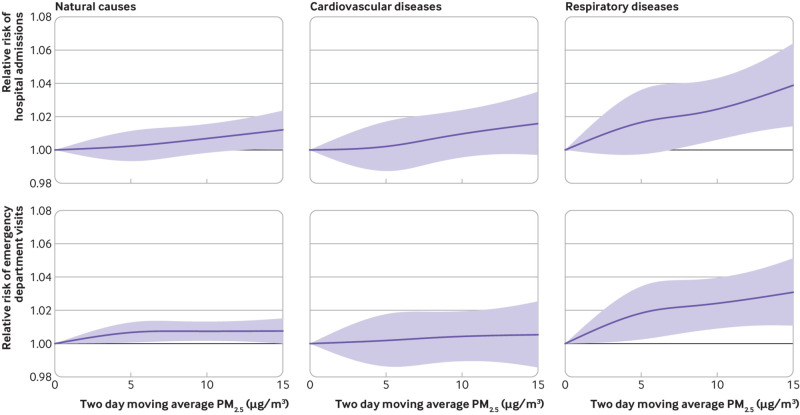
Incidence rates of hospital admissions and emergency department visits also varied across geographic regions. The highest incidence rates for hospital admissions related to natural causes were observed in the northern Great Plains and the northeast, whereas the highest incidence rates for emergency department visits for natural causes were documented in the southeast and midwest (fig 3). Supplementary tables S3 and S4 show the total number and incidence rates of hospital admissions and emergency department visits for natural causes and for cardiovascular and respiratory diseases across different geographic areas, respectively.
Fig 3.
Maps of the 98th centile distribution of PM2.5 (fine particulate matter) concentrations and incidence rates per million enrollees per day of hospital admissions and emergency department visits for natural causes across US counties, 2010-16: (A) 98th centile distributions of PM2.5 concentrations; (B) 98th centile distributions of PM2.5 concentrations categorized by World Health Organization and national ambient air quality standards; (C) incidence rate per million enrollees per day of hospital admissions for natural causes in US counties; (D) incidence rate per million enrollees per day of emergency department visits for any cause in US counties. Crosshatching represents counties with missing air pollution data—the total number of hospital admissions or emergency department visits in these counties fell below the small cell suppression limit of 11
During the study period, only 0.1% of county days (8344 out of 7 949 713) recorded daily PM2.5 concentrations that exceeded the current national ambient air quality standards of 35 μg/m3; these counties were primarily located in central California, northwestern Utah, southwestern Montana, and east Idaho. Daily PM2.5 levels were below the new WHO air quality guideline limit of 15 μg/m3 in 92.6% of county days (7 360 725 out of 7 949 713) (see supplementary figure S2). Restricting our sample of events to days below this level resulted in the exclusion of 9.4% of hospital admissions and 9.1% of emergency department visits.
Regression results
Exposure to PM2.5 at concentrations below the new WHO air quality guideline limit was associated with an increased risk of hospital admissions for natural causes, cardiovascular disease, and respiratory disease. Specifically, each 10 μg/m3 increase in lag 0-1 PM2.5 was associated with a 0.91% (95% confidence interval 0.55% to 1.26%) higher relative risk of hospital admissions for natural causes, 1.39% (0.81% to 1.98%) higher relative risk of hospital admissions for cardiovascular disease, and 1.90% (1.15% to 2.66%) higher relative risk of hospital admissions for respiratory disease (fig 4, also see supplementary table S5). The corresponding excess absolute risk was 1.87 (95% confidence interval 1.14 to 2.59), 1.04 (0.61 to 1.48), and 0.85 (0.52 to 1.18) per million enrollees per day for hospital admissions related to natural causes, cardiovascular disease, and respiratory disease, respectively (fig 4, also see supplementary table S6).
Fig 4.
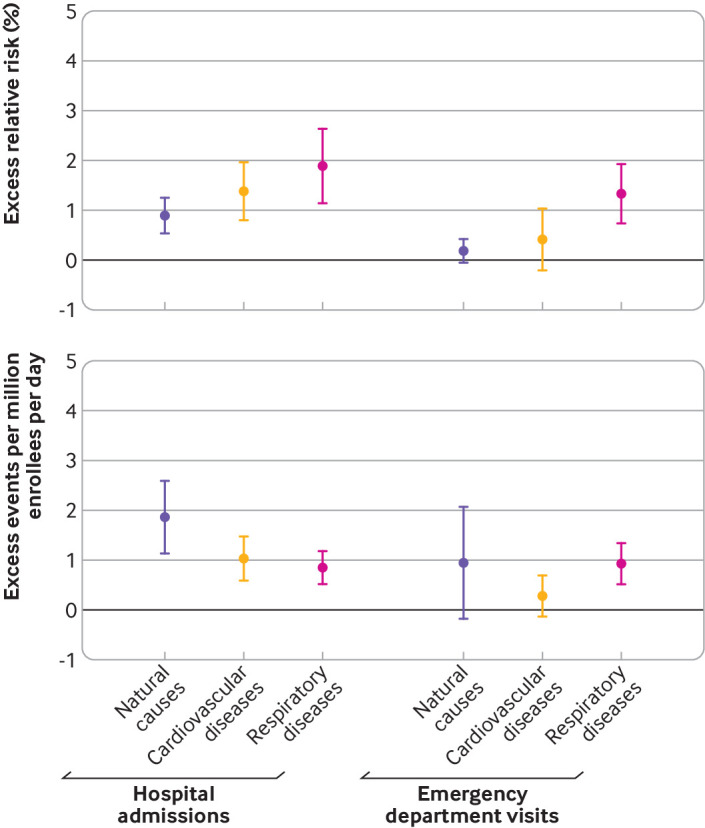
Excess relative risk (percentage) and excess events of hospital admissions and emergency department visits for natural causes, cardiovascular disease, and respiratory disease associated with each 10 μg/m3 increase in fine particulate matter (PM2.5) during the current and previous day
The association between exposure to PM2.5 and risk of hospital admissions was most pronounced at lag 0, but with little evidence of continued higher risk at lag 1, except for respiratory diseases. For example, a 10 μg/m3 increase in PM2.5 was associated with a 0.86% (95% confidence interval 0.52% to 1.19%) higher relative risk at lag 0 and a 0.04% (−0.31% to 0.38%) higher relative risk at lag 1 for hospital admissions related to natural causes. The corresponding excess relative risk for respiratory disease was 0.86% (95% confidence interval 0.16% to 1.57%) at lag 0 and 1.03% (0.31% to 1.76%) at lag 1 (see supplementary table S7).
For emergency department visits, a 10 μg/m3 increase in lag 0-1 PM2.5 was associated with a 1.34% (95% confidence interval 0.73% to 1.94%) excess relative risk of emergency department visits for respiratory disease (fig 4, also see supplementary table S5), corresponding to 0.93 (95% confidence interval 0.52 to 1.35) additional emergency department visits per million enrollees per day (fig 4, also see supplementary table S6). The estimated association between exposure to PM2.5 and emergency department visits for natural causes or for cardiovascular disease was weaker and not statistically significant.
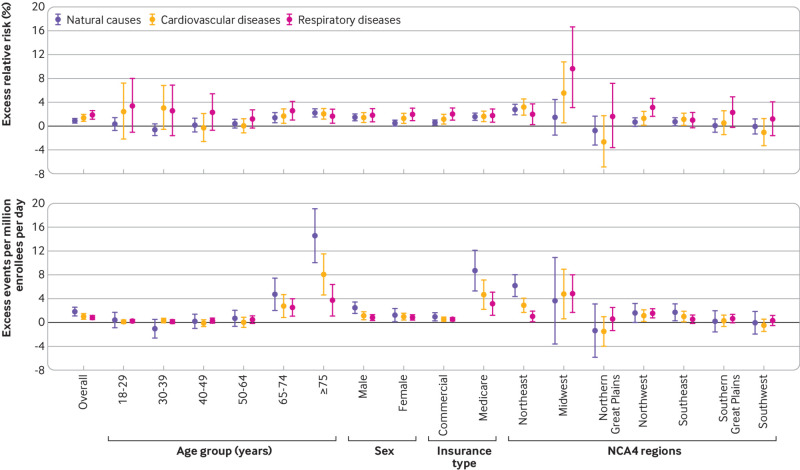
We performed a series of sensitivity analyses to evaluate the robustness of our findings. In analyses that allowed for a flexible exposure-response relation for the association between exposure to PM2.5 and morbidity, we found a monotonic association between exposure to PM2.5 and the relative risk of hospital admissions for natural causes, cardiovascular disease, and respiratory disease, with no indication of a threshold at lower concentrations (fig 5). We found a monotonic association between exposure to PM2.5 and relative risk of emergency department visits for respiratory disease, with the association appearing more pronounced at lower PM2.5 levels (fig 5). When we adjusted for daily maximum ambient temperature or daily minimum ambient temperature instead of daily mean temperature, the results remain consistent with our main findings, except for the association between PM2.5 level and emergency department visits for natural causes and cardiovascular disease, which became statistically significant when we adjusted for daily minimum temperature (see supplementary table S8). Our results were not materially different when we additionally included an interaction term between relative humidity splines and NCA4 regions in the models (see supplementary table S9). Additionally, when we expanded our analysis beyond days with daily PM2.5 concentrations <15 μg/m3, we generally found an attenuation in the association for PM2.5 compared with low level exposure to PM2.5, suggesting that PM2.5 concentrations are even more strongly associated with adverse outcomes <15 μg/m3 versus >15 μg/m3 (see supplementary table S10).
Fig 5.
Exposure-response curve for association between two day moving average of PM2.5 (fine particulate matter) concentrations and hospital admissions and emergency department visits for natural causes, cardiovascular disease, and respiratory disease. The reference point on the curve is the counterfactual concentration at 0 μg/m3 of the two day moving average PM2.5 during the study period
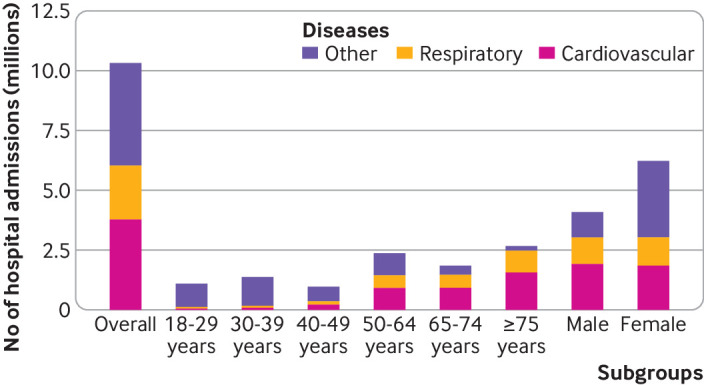
We found that the association between exposure to PM2.5 and hospital admissions for natural causes was statistically significant only among adults aged ≥65 years (fig 6). For example, a 10 μg/m3 increase in PM2.5 was associated with an excess relative risk of 0.36% (95% confidence interval −0.72% to 1.45%) among adults aged 18-29 years compared with 1.43% (0.60% to 2.26%) and 2.21% (1.52% to 2.91%) among those aged 65-74 years and ≥75 years, respectively. The corresponding excess absolute risks were 0.41 (95% confidence interval −0.84 to 1.67), 4.76 (2.04 to 7.48), and 14.57 (10.09 to 19.06) per million enrollee per day for adults aged 18-29 years, 65-74 years, and ≥75 years, respectively. The association between exposure to PM2.5 and hospital admissions for natural causes was more pronounced among men, those residing in the northeast US, and those with Medicare Advantage health insurance.
Fig 6.
Excess relative risk (percentage) and excess events of hospital admissions for natural causes, cardiovascular disease, and respiratory disease associated with each 10 μg/m3 increase in PM2.5 (fine particulate matter) during the current and previous day, stratified by age, sex, insurance type, and NCA4 (US Global Change Research Program’s Fourth National Climate Assessment) regions
For emergency department visits, we found a statistically significant association between exposure to PM2.5 and respiratory disease (see supplementary figure S3). This association was most pronounced in young and middle aged adults and in the southern Great Plains. For example, we found that adults aged 40-49 years had the highest excess relative risk of 2.57% (95% confidence interval 0.87% to 4.30%) compared with the older population among whom the association was attenuated and not statistically significant. A 10 μg/m3 increase in PM2.5 was associated with an excess relative risk of 5.64% (3.77% to 7.54%) in the southern Great Plains versus 1.07% (−0.43% to 2.59%) in the US northeast.
Discussion
Using data encompassing more than 10 million hospital admissions and 24 million emergency department visits across the contiguous US from 2010 to 2016, we found that short term exposure to PM2.5, even at concentrations below the new WHO air quality guideline limit of 15 μg/m3, was statistically significantly associated with a higher risk of hospital admissions for natural causes, cardiovascular disease, and respiratory disease, as well as emergency department visits for respiratory disease.
Comparison with other studies
Studies of the potential health effects of PM2.5 at low levels (by today’s standards) provide valuable insights and critically inform national health policies. However, relatively few such studies have been conducted.1 24 25 For example, in a pooled analysis of multiple European cohorts, one study evaluated the association between long term exposure to PM2.5 and mortality, with a focus on the health effects of such exposure below the current standards and guidelines of the European Union (25 μg/m3) and US (12 μg/m3) and previous guidelines from WHO (10 μg/m3).24 Another study used mortality data from the US Medicare fee-for-service population to estimate the association between short term exposure to PM2.5 below the current daily national ambient air quality standard (35 μg/m3) and mortality in the US.1 In a recent study, researchers found that the adverse health effects of PM2.5 on all cause mortality persisted at lower levels of PM2.5 below the previous WHO air quality guideline limit of 25 μg/m3.3 26 Our study investigated whether the risk of morbidity occurs at levels of PM2.5 below the newly revised WHO air quality guideline limit of 15 μg/m3 , using data on both hospital admissions and emergency department visits among younger and older adults in the US.
The new WHO air quality guideline calls for a limit on 24 hour mean PM2.5 concentrations to 15 μg/m3, a reduction from the previous limit of 25 μg/m3 set in 2005, in response to compelling evidence of substantial health effects of PM2.5 even at concentrations below the earlier limit. Our study identified a consistent monotonic exposure-response association between exposure to PM2.5 at levels below the new WHO air quality guideline limit and hospital admissions for natural causes, cardiovascular disease, and respiratory disease, and emergency department visits for respiratory diseases. Notably, when examining emergency department visits, we noted that the association between PM2.5 level and respiratory disease appears to be more pronounced at lower PM2.5 levels. These findings provided evidence that PM2.5 continues to pose adverse health risks even when concentrations are below the newly revised WHO air quality guidelines, which corroborates the conclusion that probably no safe level of exposure to PM2.5 exists—that is, the level below which no adverse health effects are observed.1 24 25 26
Our findings that PM2.5 level was associated with hospital admissions among adults ≥aged 65 years but not among adults aged <65 years were consistent with previous studies.10 27 For example, a nationwide study in Italy, examining the link between air pollution and hospital admissions for respiratory disease, found that PM2.5 level was associated with higher risk of hospital admissions among adults aged ≥75 years but not among adults aged <75 years.10
We found statistically significant associations between exposure to PM2.5 and increased risk of emergency department visits for respiratory disease exclusively among adults aged <50 years. These findings indicate that previous studies that focused on older populations may not have fully captured the adverse health effects of PM2.5 on respiratory related emergency department visits. Relying on such studies could potentially lead to an underestimation of the health effects of PM2.5, particularly among younger age groups. Our findings were consistent with a US nationwide study among 40 million respiratory related emergency department visits collected through the Centers for Disease Control and Prevention’s national environmental public health tracking network.11 This study found a strong association between PM2.5 level and emergency department visits for respiratory disease among children and young people aged 0-18 years, a moderate association among adults aged 19-64 years, and no significant association among older adults aged ≥65 years.11
We found that most of the adverse health effects of PM2.5 were more pronounced among adults with Medicare Advantage health insurance than among adults with commercial health insurance. Enrollees in the Medicare Advantage programme are largely adults aged >65 years. Thus, the health effect of PM2.5 among Medicare enrollees is similar to that among people aged ≥65 years. For example, no association was found between short term exposure to PM2.5 and emergency department visits for respiratory disease among both Medicare enrollees and older adults. We observed geographic differences in the health effects of PM2.5, with beneficiaries residing at higher latitudes tending to show higher risk of hospital admissions and emergency department visits for cardiovascular disease associated with exposure to PM2.5. We speculate that geographic locations may modify the association between exposure to PM2.5 and morbidity, possibly through factors such as differences in local temperature,28 29 and particle composition contributing to varying levels of oxidative potential.30
Limitations and strengths of this study
Our study has several limitations. First, we used county level PM2.5 level as a proxy for personal exposure to PM2.5, which could potentially lead to misclassification of exposure. Additionally, the absence of information on patients’ time-activity patterns might introduce additional misclassification of exposure. Nevertheless, we expect that any potential misclassification would likely be non-differential and would tend to bias our results toward the null hypothesis of no association.31 Second, our study population was limited to US adults with health insurance, which may limit the generalizability of our findings to individuals without medical insurance, children and adolescents, and individuals living outside the contiguous US. Third, our analysis was conducted using data available up to 2016. Future studies with more recent data on exposure to air pollution and morbidity are warranted to provide further evaluation of the evidence on the association between exposure to PM2.5 and morbidity, particularly at daily PM2.5 levels below the 2021 WHO air quality guideline limit.
Our study has three main strengths. First, our study population included more than 10 million hospital admissions and 24 million emergency department visits among beneficiaries with commercial and Medicare Advantage insurance. The enrollees span a broad spectrum of age groups older than 18 years, and they are distributed across different climate regions in the contiguous US. Second, we not only assessed the excess relative risk of morbidity for natural causes, cardiovascular disease, and respiratory disease but also quantified the absolute risk associated with short term exposure to PM2.5. Therefore, our study provides a comprehensive evaluation of the health effects of daily PM2.5 at levels below the new WHO air quality guideline limit of 15 µg/m3. Third, we included both hospital admissions and emergency department visits as our primary health outcomes, allowing us to compare the health impacts of PM2.5 levels on different morbidity metrics.
Conclusions and policy implications
Short term exposures to PM2.5 below the new WHO air quality guideline limit of 15 µg/m3 are associated with higher risks of hospital admission for natural causes, cardiovascular disease, and respiratory disease as well as for emergency department visits for respiratory disease among adults with health insurance in the contiguous US. Our study contributes to the evidence that ambient air pollution is associated with morbidity even at PM2.5 levels below the current WHO air quality guideline limit. Our study provides an initial assessment of the newly revised WHO guidelines for PM2.5 and provides valuable reference for future national air pollution standards.
What is already known on this topic
Short term exposure to fine particulate matter (PM2.5) has been associated with increased risk of morbidity and mortality
Previous studies have primarily focused on older adults or used data on hospital admissions
Evidence for the association between short term exposure to PM2.5 and morbidity at levels below the new World Health Organization air quality guideline limit remains unclear
What this study adds
In this nationwide study in the US, exposure to ambient PM2.5 at levels below the new WHO air quality guideline limit of 15 µg/m3 was statistically significantly associated with hospital admissions for natural causes, cardiovascular disease, and respiratory disease, and emergency department visits for respiratory disease
These findings provide evidence of health harms associated with short term exposure to PM2.5 even at levels below the new WHO air quality guideline limit
Web extra Extra material supplied by authors
Supplementary information: eAppendix, tables S1-S10, and figures S1-S3
Contributors: SS and GAW contributed equally to this paper. YS, SS, and GAW designed the study. YS, CWM, SS, and GAW developed the analysis plan. YS performed statistical analysis and took responsibility for the accuracy of the data analysis. YS and GAW drafted the manuscript. CWM, KRS, YW, JS, FD, and AN-S contributed to the interpretation of the results and revision of the final manuscript. YS is the guarantor. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Funding: This study was supported by the National Institutes of Health (R01-ES029950). JS was supported by the National Institute of Environmental Health Sciences (R01ES032418-01). The funders had no role in considering the study design or in the collection, analysis, interpretation of data, writing of the report, or decision to submit the article for publication.
Competing interests: All authors have completed the ICMJE uniform disclosure form at www.icmje.org/coi_disclosure.pdf and declare: all authors had financial support from the National Institutes of Health and the National Institute of Environmental Health Sciences for the submitted work; GAW previously served as a consultant for Google (Mountain View, CA) and currently serves as a consultant for the Health Effects Institute (Boston, MA); no other relationships or activities that could appear to have influenced the submitted work.
The lead author (YS) affirms that the manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned and registered have been explained.
Dissemination to participants and related patient and public communities: There are no plans to disseminate the results of the research directly to study participants. We plan to disseminate the results of the research to the general public through media outreach, including press releases by the media departments of the authors’ research institutes and plain language messaging in social media.
Provenance and peer review: Not commissioned; externally peer reviewed.
Publisher’s note: Published maps are provided without any warranty of any kind, either express or implied. BMJ remains neutral with regard to jurisdictional claims in published maps.
Ethics statements
Ethical approval
This study involved analysis of pre-existing, deidentified data and was exempted from institutional review board approval.
Data availability statement
No additional data available.
References
- 1. Di Q, Dai L, Wang Y, et al. Association of Short-term Exposure to Air Pollution With Mortality in Older Adults. JAMA 2017;318:2446-56. 10.1001/jama.2017.17923 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Liu C, Chen R, Sera F, et al. Ambient Particulate Air Pollution and Daily Mortality in 652 Cities. N Engl J Med 2019;381:705-15. 10.1056/NEJMoa1817364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Wang K, Hao Y, Au W, Christiani DC, Xia ZL. A Systematic Review and Meta-Analysis on Short-Term Particulate Matter Exposure and Chronic Obstructive Pulmonary Disease Hospitalizations in China. J Occup Environ Med 2019;61:e112-24. 10.1097/JOM.0000000000001539 [DOI] [PubMed] [Google Scholar]
- 4. Wei Y, Wang Y, Di Q, et al. Short term exposure to fine particulate matter and hospital admission risks and costs in the Medicare population: time stratified, case crossover study. BMJ 2019;367:l6258. 10.1136/bmj.l6258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Chen C, Warrington JA, Dominici F, et al. Temporal variation in association between short-term exposure to fine particulate matter and hospitalisations in older adults in the USA: a long-term time-series analysis of the US Medicare dataset. Lancet Planet Health 2021;5:e534-41. 10.1016/S2542-5196(21)00168-6 [DOI] [PubMed] [Google Scholar]
- 6. Dominici F, Peng RD, Bell ML, et al. Fine particulate air pollution and hospital admission for cardiovascular and respiratory diseases. JAMA 2006;295:1127-34. 10.1001/jama.295.10.1127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Cohen AJ, Brauer M, Burnett R, et al. Estimates and 25-year trends of the global burden of disease attributable to ambient air pollution: an analysis of data from the Global Burden of Diseases Study 2015. Lancet 2017;389:1907-18. 10.1016/S0140-6736(17)30505-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.World Health Organization. WHO global air quality guidelines: Particulate matter (PM2.5 and PM10), ozone, nitrogen dioxide, sulfur dioxide and carbon monoxide. World Health Organization, 2021 [cited 2023 Nov 29]. https://iris.who.int/bitstream/handle/10665/345329/9789240034228-eng.pdf?sequence=1 [PubMed]
- 9.United States Environmental Protection Agency (EPA). NAAQS Table. EPA, 2012 [cited 2023 Oct 31]; https://www.epa.gov/criteria-air-pollutants/naaqs-table
- 10. Renzi M, Scortichini M, Forastiere F, et al. BEEP collaborative Group . A nationwide study of air pollution from particulate matter and daily hospitalizations for respiratory diseases in Italy. Sci Total Environ 2022;807:151034. 10.1016/j.scitotenv.2021.151034 [DOI] [PubMed] [Google Scholar]
- 11. Strosnider HM, Chang HH, Darrow LA, Liu Y, Vaidyanathan A, Strickland MJ. Age-Specific Associations of Ozone and Fine Particulate Matter with Respiratory Emergency Department Visits in the United States. Am J Respir Crit Care Med 2019;199:882-90. 10.1164/rccm.201806-1147OC [DOI] [PubMed] [Google Scholar]
- 12.Optum Labs. Optum Labs and Optum Labs Data Warehouse (OLDW) Descriptions and Citation. Eden Prairie, MN: March 2023. PDF. Reproduced with permission from Optum Labs.
- 13. Di Q, Amini H, Shi L, et al. An ensemble-based model of PM2.5 concentration across the contiguous United States with high spatiotemporal resolution. Environ Int 2019;130:104909. 10.1016/j.envint.2019.104909 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Di Q, Kloog I, Koutrakis P, Lyapustin A, Wang Y, Schwartz J. Assessing PM2.5 Exposures with High Spatiotemporal Resolution across the Continental United States. Environ Sci Technol 2016;50:4712-21. 10.1021/acs.est.5b06121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Spangler KR, Weinberger KR, Wellenius GA. Suitability of gridded climate datasets for use in environmental epidemiology. J Expo Sci Environ Epidemiol 2019;29:777-89. 10.1038/s41370-018-0105-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Daly C, Halbleib M, Smith JI, et al. Physiographically sensitive mapping of climatological temperature and precipitation across the conterminous United States. Int J Climatol 2008;28:2031-64 10.1002/joc.1688. [DOI] [Google Scholar]
- 17. Sun S, Spangler KR, Weinberger KR, Yanosky JD, Braun JM, Wellenius GA. Ambient Temperature and Markers of Fetal Growth: A Retrospective Observational Study of 29 Million U.S. Singleton Births. Environ Health Perspect 2019;127:67005. 10.1289/EHP4648 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Gasparrini A. The Case Time Series Design. Epidemiology 2021;32:829-37. 10.1097/EDE.0000000000001410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Gasparrini A. A tutorial on the case time series design for small-area analysis. BMC Med Res Methodol 2022;22:129. 10.1186/s12874-022-01612-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Sun S, Weinberger KR, Nori-Sarma A, et al. Ambient heat and risks of emergency department visits among adults in the United States: time stratified case crossover study. BMJ 2021;375:e065653. 10.1136/bmj-2021-065653 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rothman KJ, Greenland S, Lash TL. Modern epidemiology. 3rd ed. Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins; 2008. Chapter 15, Introduction to Stratified Analysis – Test Homogeneity; p279. [Google Scholar]
- 22.Turner H, Firth D. Generalized nonlinear models in R: An overview of the gnm package. 2007.
- 23. Gasparrini A. Distributed lag linear and non-linear models in R: the package dlnm. J Stat Softw 2011;43:1-20. 10.18637/jss.v043.i08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Brunekreef B, Strak M, Chen J, et al. Mortality and Morbidity Effects of Long-Term Exposure to Low-Level PM2.5, BC, NO2, and O3: An Analysis of European Cohorts in the ELAPSE Project. Res Rep Health Eff Inst 2021;2021:1-127. [PMC free article] [PubMed] [Google Scholar]
- 25. Shi L, Zanobetti A, Kloog I, et al. Low-Concentration PM2.5 and Mortality: Estimating Acute and Chronic Effects in a Population-Based Study. Environ Health Perspect 2016;124:46-52. 10.1289/ehp.1409111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Liu RA, Wei Y, Qiu X, Kosheleva A, Schwartz JD. Short term exposure to air pollution and mortality in the US: a double negative control analysis. Environ Health 2022;21:81. 10.1186/s12940-022-00886-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Tian Y, Liu H, Zhao Z, et al. Association between ambient air pollution and daily hospital admissions for ischemic stroke: A nationwide time-series analysis. PLoS Med 2018;15:e1002668. 10.1371/journal.pmed.1002668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Sun S, Cao P, Chan KP, Tsang H, Wong CM, Thach TQ. Temperature as a modifier of the effects of fine particulate matter on acute mortality in Hong Kong. Environ Pollut 2015;205:357-64. 10.1016/j.envpol.2015.06.007 [DOI] [PubMed] [Google Scholar]
- 29. Bergmann S, Li B, Pilot E, Chen R, Wang B, Yang J. Effect modification of the short-term effects of air pollution on morbidity by season: A systematic review and meta-analysis. Sci Total Environ 2020;716:136985. 10.1016/j.scitotenv.2020.136985 [DOI] [PubMed] [Google Scholar]
- 30. Vinson A, Sidwell A, Black O, Roper C. Seasonal variation in the chemical composition and oxidative potential of PM2.5 . Atmosphere. 2020;11:1086 10.3390/atmos11101086. [DOI] [Google Scholar]
- 31. Kioumourtzoglou MA, Spiegelman D, Szpiro AA, et al. Exposure measurement error in PM2.5 health effects studies: a pooled analysis of eight personal exposure validation studies. Environ Health 2014;13:2. 10.1186/1476-069X-13-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary information: eAppendix, tables S1-S10, and figures S1-S3
Data Availability Statement
No additional data available.