Abstract
BACKGROUND
Brachioradial pruritus (BRP) is a rare form of chronic dysesthesia characterized by persistent itching, burning, or tingling commonly involving the dorsolateral upper extremities. Although the exact pathophysiology remains unclear, the condition may be a manifestation of atypical cervical radiculopathy.
OBSERVATIONS
The authors describe two patients with BRP, a 44-year-old female and a 51-year-old male, both of whom benefited from surgical intervention for atypical cervical radiculopathy, while also highlighting their presentation, diagnostic testing, treatment, and outcomes.
LESSONS
The cases demonstrate the potential relationship between cervical spondylosis and BRP while examining the role of surgical intervention as a treatment option.
KEYWORDS: brachioradial pruritus, atypical cervical radiculopathy, surgery, artificial disc replacement
ABBREVIATIONS: ACDF = anterior cervical discectomy and fusion, BRP = brachioradial pruritus, MRI = magnetic resonance imaging, UV = ultraviolet
Brachioradial pruritus (BRP) is a rare form of chronic dysesthesia characterized by persistent itching, burning, or tingling commonly involving the dorsolateral upper extremities. The condition, initially described as a solar pruritus in 1968 by Waisman,1 was thought to be associated with prolonged sunlight exposure. Other studies have reported extended ultraviolet (UV) light and tropical climate exposure as potential etiologies.2,3 Although the exact pathophysiology remains unclear, past reports have posited that patients with BRP might also have underlying spine pathology. In 1983, Heyl4 proposed that although UV light exposure may contribute to BRP, peripheral nervous system pathology was the primary cause. Several studies have since suggested that cervical spine pathology may play a role in the etiology of BRP.5–9
Cervical radiculopathy classically presents with neck pain, arm pain radiating in a myotomal pattern, and paresthesia radiating in a dermatomal pattern.10 However, several studies have suggested a possible correlation between cervical spondylosis and other atypical symptoms.11–14 One study described a subset of patients with C6–7 spondylosis who primarily presented with unilateral subscapular and chest pain alleviated only after cervical discectomy and fusion despite prior attempts to treat the patient for cardiac causes of chest pain.14 A recent meta-analysis reviewed 27 studies in which patients presented with a myriad of atypical complaints, including cervicogenic headache, tinnitus, and nausea.11 These studies demonstrate that cervical spondylosis may be implicated in symptoms other than those classically described.
There is a paucity of data reporting BRP as an atypical presentation of cervical radiculopathy. In 1997, Fisher5 asserted a relationship between BRP and cervical nerve root impingement, arguing that dermatological photosensitivity disorders do not involve such focal areas as outlined in typical BRP presentations. One retrospective study found that among 22 patients with BRP, 11 had undergone cervical spine radiography displaying abnormalities including spondylosis, foraminal narrowing, and bones spurs, predominantly between C3 and C7.6 Binder et al.7 performed a case study in which magnetic resonance imaging (MRI) in a patient with BRP showed a right-sided mediolateral disc herniation causing mild compression of the spinal cord and severe compression of the right C6 nerve root.
Several authors have described surgical intervention as a successful treatment modality for some patients with BRP.7,15,16 However, there has been little research on the overall efficacy of surgical intervention for patients with BRP.
The objective of this case report was to describe 2 patients with BRP who benefited from surgical treatment while also highlighting their presentation, diagnostic testing, treatment, and outcomes. Furthermore, we aimed to emphasize that cervical spine pathology should be considered in the differential diagnosis in patients presenting with BRP.
Illustrative Cases
Case 1
A 44-year-old female presented with an 8-month history of severe, progressively worsening pruritus in the bilateral forearms. She had already seen primary care, dermatology, and neurology clinicians and an orthopedic hand and wrist specialist without relief. Symptoms were initially episodic and infrequent and then became nearly constant both during the day and at night. Seven months later, she developed burning pain in the right scapula. Her symptoms were not affected by neck position or movement. She was treated with topical steroids, topical antifungals, oral antihistamines, oral steroids, massage, and acupuncture, with little to no improvement. The patient noted that because of the severity of her itching, she had developed excoriations and ecchymosis. Her symptoms were only alleviated with frequent application of ice directly to the forearm.
Her medical history included adult attention-deficit/hyperactivity disorder. She did not have any other known medical conditions or allergies. She reported infrequent cigarette smoking, less than 14 cigarettes per month, and did not drink alcohol regularly.
On examination, she had normal cranial nerve function, normal and symmetric muscle bulk, and normal bilateral upper-extremity strength. No significant erythema, edema, or discoloration was present on the forearms.
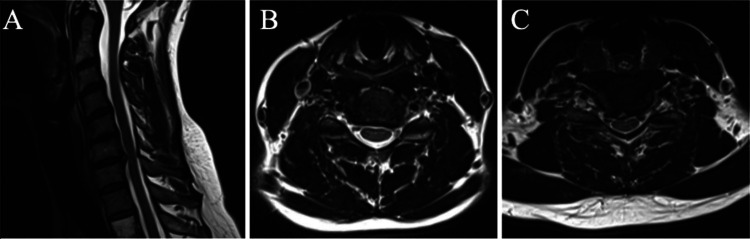
Cervical spine MRI demonstrated degenerative disc disease and spondylosis at C5–6 and C6–7 as well as a disc osteophyte complex, right paracentral disc extrusion, and mild bilateral foraminal stenosis at C6–7 (Fig. 1). Electromyography and nerve conduction study of the bilateral upper extremities showed normal findings with no electrodiagnostic evidence of cervical radiculopathy, brachial plexopathy, or focal mononeuropathy. Diagnostic cervical epidural steroid injection with fluoroscopic guidance was performed at the left C5–6 and right C6–7 levels, after which the patient reported decreased frequency and severity of the pruritus for 3 months. Given the return of symptoms despite medications and epidural steroid injection, the decision was made to perform an artificial disc replacement at C5–6 and C6–7.
FIG. 1.
Case 1. A: Sagittal MRI of the cervical spine showing degenerative disc disease and spondylosis at C3–4, C4–5, C5–6, and C6–7. B: Axial MRI at C5–6 revealing left foraminal stenosis. C: Axial MRI at C6–7 showing disc displacement, right paracentral disc extrusion, and mild bilateral foraminal stenosis.
Surgery was successful without complications (Fig. 2). At the 7-week follow-up, the patient endorsed significant resolution of symptoms, and, by 3 months, she had complete resolution of the pruritus, durable at 6 months as well.
FIG. 2.

Case 1. Lateral radiograph of the cervical spine at 6 months after surgery, showing artificial disc replacement at C5–6 and C6–7.
Case 2
A 51-year-old male presented with a 3-year history of severe pruritus from the midanterolateral upper arm to the middorsal forearm, left worse than right, with associated numbness radiating to the left thumb, index finger, and middle finger. The patient had originally had similar symptoms 7 years prior that resolved completely after anterior cervical discectomy and fusion (ACDF) at C6–7. His symptoms returned 2 years after the surgery and became progressively intractable. He tried topical medications, oral medications, physical therapy, massage, and chiropractic treatment.
He did not have any medical conditions or allergies. He was a former smoker and had quit 10 years prior and reported occasional alcohol use. He was an avid surfer, and his wife noticed that he and his friends were frequently scratching their forearms while standing on the beach.
The patient had a normal neurological examination with full strength in the upper extremities and intact sensation to light touch and pin prick. Cervical spine MRI revealed moderate left foraminal stenosis at C5–6 and C6–7 (Fig. 3). Electromyography and nerve conduction study showed chronic left C6 and C7 radiculopathy. Given the refractory symptoms, the patient underwent a left C6–7 laminoforaminotomy, performed without complications.
FIG. 3.
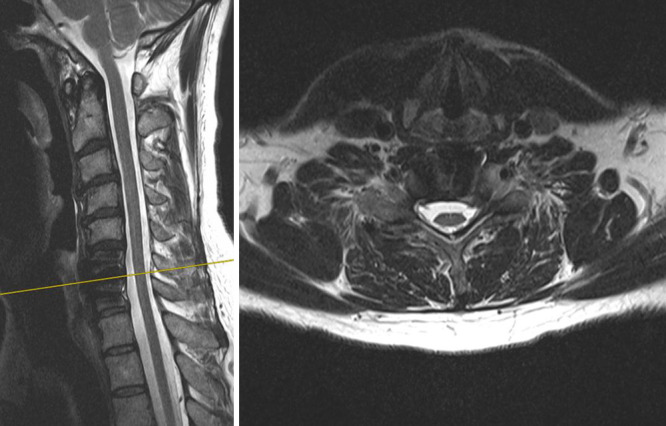
Case 2. Left: Sagittal MRI of the cervical spine revealing prior ACDF at C6–7. Right: Axial MRI at C6–7 showing moderate left foraminal stenosis.
Following surgery, the patient endorsed instant relief of his pruritus, which remained durable upon subsequent follow-up visits out to 8 months.
Patient Informed Consent
The necessary patient informed consent was obtained in this study.
Discussion
Observations
BRP is a rare neuropathic condition whose etiology remains a point of dispute. Previous studies have identified various potential causes of BRP, but there still is no consensus about the best form of management. Waisman1 introduced the notion that BRP may be associated with prolonged sunlight exposure and UV light radiation, and several studies2,17–19 have demonstrated pruritus improvement with protection from sunlight and topical capsaicin therapy. However, the recent literature has proposed an alternative origin of BRP, with evidence supporting cervical spine pathology as a potential cause.
Heyl4 initially suggested this idea, referencing 4 of 5 patients with BRP with cervical vertebral osteoarthritis. Barry and Rogers19 found similar results with 5 of 7 patients with BRP exhibiting evidence of cervical osteoarthritis. Several studies have outlined cases of neuropathic BRP associated with factors such as cervical disc herniation and stenosis.7,15,16,20 Morosanu and colleagues15 highlighted the case of a 63-year-old female with BRP in the C5–6 distribution whose MRI revealed a C5–6 disc protrusion. Marziniak and colleagues21 found that 80.5% of 41 patients with BRP had intervertebral foraminal stenosis or cervical disc protrusions with nerve compression on magnetic resonance tomography. The location of the nerve compression lesions significantly correlated with the dermatomal localization of the pruritus (Spearman correlation coefficient 0.893, p < 0.01).21
Cervical radiculopathy has been classically associated with neck pain, arm pain, and paresthesia, although recent studies have described other atypical symptoms thought to be related to cervical spondylosis. A recent meta-analysis of 27 studies demonstrated a correlation between cervical spondylosis and headache, tinnitus, and nausea, and the authors described possible pathophysiological mechanisms connecting cervical spondylosis and the sympathetic nervous system.11
The cases highlighted in our report suggest that BRP may be another atypical manifestation of cervical radiculopathy for which surgical intervention may be viable treatment. Both patients experienced BRP in the bilateral upper extremities, and, despite a variety of conservative treatment options, including oral medications, topical therapy, and massages, neither patient reported durable symptom relief. Both patients endorsed a complete resolution of symptoms within 3 months of surgery.
Several studies have reported similar outcomes after surgical intervention. Salzmann et al.16 described a 56-year-old male with a 6-year history of chronic pruritus in the bilateral upper extremities whose imaging had revealed multilevel cervical spondylosis with notable spinal stenosis and cord flattening at C2–4 and C4–5. Multilevel foraminal stenosis from C3 to C7 was also present. After undergoing multilevel ACDF from C3 to C7, the patient experienced complete and instantaneous symptom relief, durable to the last follow-up at 4 months. Morosanu and colleagues15 described a 63-year-old female with a C5–6 disc protrusion who had undergone ACDF and experienced a complete resolution of symptoms at the 3-month follow-up. Binder et al.7 reported a 64-year-old female with a history of BRP on the right dorsal forearm whose imaging studies had revealed intervertebral osteochondrosis, most prominent at the C5–6 level. MRI had also demonstrated right-sided mediolateral disc herniation with mild compression of the spinal cord and severe compression of the right C6 nerve root. After symptomatic treatment with gabapentin, the patient underwent ventral C5–6 discectomy and C6 nerve root decompression followed by C5–6 fusion, with complete relief of dysesthesias within 1 week after surgery.
Lessons
BRP remains an enigmatic condition with insufficient research to clearly elucidate its etiology, presentation, and treatment. However, the cases outlined in the present study, in addition to those described in similar reports, highlight the importance of further investigation of cervical pathology when patients present with atypical radicular symptoms such as BRP. Cases of BRP should not be immediately dismissed or neglected as nonneurological in order to minimize misdiagnosis resulting in a delay of necessary treatment. However, various diagnostic modalities, including cervical MRI, electromyography, spinal injections, and skin biopsies, can be used to garner information before proceeding with more invasive surgical interventions.
The prevalence rate of neuropathic BRP remains unclear; however, it is possible that patients with similar symptoms dismiss the condition as dermatological and seek inappropriate treatment options. As mentioned in the presentation for case 2, the patient’s wife noticed that he and his friends were frequently scratching their forearms while standing on the beach after surfing, shedding anecdotal insight into the prevalence of this condition. In this population of surfing hobbyists, individuals are frequently supine on the surfboard and extending the neck for prolonged periods of time. Studies have suggested that this behavior is associated with neuroforaminal narrowing and worsening clinical presentation of classic cervical radiculopathy.22,23 The concurrence of pruritic symptoms while engaging in an activity that requires frequent, repetitive extension of the neck suggests that cervical spine dynamics and pathology may contribute to BRP.
Given the small sample size coupled with a paucity of literature describing similar cases, our observations are unlikely to be generalizable to all patients experiencing BRP. Furthermore, although our cases suggest that BRP may be a form of atypical cervical radiculopathy, the etiology may be multifactorial in nature. Our clinical experience does not elucidate the condition’s relationship with prolonged sunlight and UV radiation exposure. Further larger-scale prospective studies on whether cervical spine MRI, electromyography, and injection results can consistently help to predict surgical outcomes are warranted. Documented cases of patients with BRP who have undergone surgery without significant relief would also be beneficial.
Although BRP continues to be a relatively uncommon and enigmatic condition, recent studies have suggested that its etiology may be attributed to pathology in the cervical spine. Research has demonstrated that surgical intervention can help patients achieve symptomatic relief. Our cases highlight the benefits of two different types of surgical interventions for patients with BRP whose symptoms remained refractory to conservative measures. Clinicians should consider cervical stenosis as a potential contributor to this rare but identifiable condition.
Author Contributions
Conception and design: Khalifeh, Musmar, Ozgur. Acquisition of data: Le. Analysis and interpretation of data: Ozgur. Drafting the article: Khalifeh, Musmar. Critically revising the article: Khalifeh, Musmar, Maroon, Kanter. Reviewed submitted version of manuscript: all authors. Approved the final version of the manuscript on behalf of all authors: Khalifeh. Administrative/technical/material support: Le, Musmar. Study supervision: Musmar.
References
- 1. Waisman M. Solar pruritus of the elbows (brachioradial summer pruritus) Arch Dermatol. 1968;98(5):481–485. [PubMed] [Google Scholar]
- 2. Wallengren J. Brachioradial pruritus: a recurrent solar dermopathy. J Am Acad Dermatol. 1998;39(5 Pt 1):803–806. doi: 10.1016/s0190-9622(98)70058-1. [DOI] [PubMed] [Google Scholar]
- 3. Walcyk PJ, Elpern DJ. Brachioradial pruritus: a tropical dermopathy. Br J Dermatol. 1986;115(2):177–180. doi: 10.1111/j.1365-2133.1986.tb05714.x. [DOI] [PubMed] [Google Scholar]
- 4. Heyl T. Brachioradial pruritus. Arch Dermatol. 1983;119(2):115–116. [PubMed] [Google Scholar]
- 5. Fisher DA. Brachioradial pruritus wanted: a sure cause (and cure) for brachioradial pruritus. Int J Dermatol. 1997;36(11):817–818. doi: 10.1046/j.1365-4362.1997.00354.x. [DOI] [PubMed] [Google Scholar]
- 6. Goodkin R, Wingard E, Bernhard JD. Brachioradial pruritus: cervical spine disease and neurogenic/neuropathic [corrected] pruritus. J Am Acad Dermatol. 2003;48(4):521–524. doi: 10.1067/mjd.2003.203. [DOI] [PubMed] [Google Scholar]
- 7. Binder A, Fölster-Holst R, Sahan G, et al. A case of neuropathic brachioradial pruritus caused by cervical disc herniation. Nat Clin Pract Neurol. 2008;4(6):338–342. doi: 10.1038/ncpneuro0807. [DOI] [PubMed] [Google Scholar]
- 8. Tait CP, Grigg E, Quirk CJ. Brachioradial pruritus and cervical spine manipulation. Australas J Dermatol. 1998;39(3):168–170. doi: 10.1111/j.1440-0960.1998.tb01274.x. [DOI] [PubMed] [Google Scholar]
- 9. Cohen AD, Masalha R, Medvedovsky E, Vardy DA. Brachioradial pruritus: a symptom of neuropathy. J Am Acad Dermatol. 2003;48(6):825–828. doi: 10.1067/mjd.2003.494. [DOI] [PubMed] [Google Scholar]
- 10. Carette S, Fehlings MG. Cervical radiculopathy. N Engl J Med. 2005;353(4):392–399. doi: 10.1056/NEJMcp043887. [DOI] [PubMed] [Google Scholar]
- 11. Garg K, Aggarwal A. Effect of cervical decompression on atypical symptoms cervical spondylosis—a narrative review and meta-analysis. World Neurosurg. 2022;157:207–217.e1. doi: 10.1016/j.wneu.2021.09.110. [DOI] [PubMed] [Google Scholar]
- 12. Li J, Jiang DJ, Wang XW, Yuan W, Liang L, Wang ZC. Mid-term outcomes of anterior cervical fusion for cervical spondylosis with sympathetic symptoms. Clin Spine Surg. 2016;29(6):255–260. doi: 10.1097/BSD.0b013e31827b4cec. [DOI] [PubMed] [Google Scholar]
- 13. Sun YQ, Zheng S, Yu J, Yan K, Tian W. Effect of total disc replacement on atypical symptoms associated with cervical spondylosis. Eur Spine J. 2013;22(7):1553–1557. doi: 10.1007/s00586-013-2785-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Ozgur BM, Marshall LF. Atypical presentation of C-7 radiculopathy. J Neurosurg. 2003;99(2) suppl:169–171. doi: 10.3171/spi.2003.99.2.0169. [DOI] [PubMed] [Google Scholar]
- 15. Morosanu CO, Etim G, Alalade AF. Brachioradial pruritus secondary to cervical disc protrusion – a case report. J Surg Case Rep. 2022;2022(8):rjac277. doi: 10.1093/jscr/rjac277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Salzmann SN, Okano I, Shue J, Hughes AP. Disabling pruritus in a patient with cervical stenosis. J Am Acad Orthop Surg Glob Res Rev. 2020;4(3):e19.00178. doi: 10.5435/JAAOSGlobal-D-19-00178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Wallengren J, Sundler F. Brachioradial pruritus is associated with a reduction in cutaneous innervation that normalizes during the symptom-free remissions. J Am Acad Dermatol. 2005;52(1):142–145. doi: 10.1016/j.jaad.2004.09.030. [DOI] [PubMed] [Google Scholar]
- 18. Knight TE, Hayashi T. Solar (brachioradial) pruritus—response to capsaicin cream. Int J Dermatol. 1994;33(3):206–209. doi: 10.1111/j.1365-4362.1994.tb04955.x. [DOI] [PubMed] [Google Scholar]
- 19. Barry R, Rogers S. Brachioradial pruritus—an enigmatic entity. Clin Exp Dermatol. 2004;29(6):637–638. doi: 10.1111/j.1365-2230.2004.01642.x. [DOI] [PubMed] [Google Scholar]
- 20. Grabnar M, Tiwari M, Vallabh J. Brachioradial pruritus due to cervical spine pathology. JMIR Dermatol. 2022;5(3):e39863. doi: 10.2196/39863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Marziniak M, Phan NQ, Raap U, et al. Brachioradial pruritus as a result of cervical spine pathology: the results of a magnetic resonance tomography study. J Am Acad Dermatol. 2011;65(4):756–762. doi: 10.1016/j.jaad.2010.07.036. [DOI] [PubMed] [Google Scholar]
- 22. Mao H, Driscoll SJ, Li JS, Li G, Wood KB, Cha TD. Dimensional changes of the neuroforamina in subaxial cervical spine during in vivo dynamic flexion-extension. Spine J. 2016;16(4):540–546. doi: 10.1016/j.spinee.2015.11.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Farmer JC, Wisneski RJ. Cervical spine nerve root compression. An analysis of neuroforaminal pressures with varying head and arm positions. Spine (Phila Pa 1976) 1994;19(16):1850–1855. doi: 10.1097/00007632-199408150-00010. [DOI] [PubMed] [Google Scholar]