Abstract
Background:
Racially and ethnically minoritized (REM) women experience social and structural factors that may affect their response to mental health treatment and menopausal symptoms during the menopause transition (MT). This scoping review on mental health during the MT for REM women in the United States was conducted to characterize factors associated with mental health challenges.
Materials and Methods:
Five databases were searched. Articles were included if focused on MT in REM women in the United States and its territories with specific mental illnesses and published in English from 2005 to 2021. Titles and abstracts and full text were screened. Screening and data collection were completed in duplicate by two reviewers in Covidence.
Results:
Sixty-five articles were included and indicate that REM women experience a disproportionate burden of depressive symptoms during the MT. Less evidence is reported about anxiety, Post-Traumatic Stress Disorder, psychosis, schizophrenia, and other mental illnesses. The risk factors associated with mental illness during MT are social, structural, and biological. Treatment response to therapeutic interventions is often underpowered to explain REM differences.
Conclusion:
Depression during the MT is associated with negative outcomes that may impact REM women differentially. Incorporating theoretical frameworks (e.g., intersectionality, weathering) into mental health research will reduce the likelihood that scientists mislabel race as the cause of these inequities, when racism and intersecting systems of oppression are the root causes of differential expression of mental illness among REM women during the MT. There is a need for interdisciplinary research to advance the mental health of REM women.
Keywords: menopause transition, mental health, race, ethnicity, perimenopause, women
Introduction
Racial and ethnic inequities in health persist in the United States despite decades of research and programs. Structural racism is one upstream area that must be addressed to dismantle such inequities. Structural racism is defined as “the totality of ways in which societies foster racial discrimination through mutually reinforcing systems of housing, education, employment, earnings, benefits, credit, media, healthcare, and criminal justice.”1 There are other exposures such as socioeconomic status, experience of everyday discrimination, and life stress that Dr. David Williams depicts in his “house that racism built.”2 These structures create access barriers that then compound the disparities for racially and ethnically minoritized (REM) women who experience mental illness. REM women refers to those women historically marginalized by the majority (non-Hispanic White [NHW]) due to race, ethnicity, or both3 and includes Black/African American, Hispanic/Latina/ex, Native/Indigenous, and Asian and Pacific Islander.
The menopause transition (MT), “the period immediately before menopause (when the endocrinologic, biologic, and clinical features of approaching menopause commence) and the first year after menopause,”4 is an important journey in a woman's life. Over two million U.S. women enter menopause annually,5 including 460,000 REM women. Menopause symptoms impact at least 20% of all women, and a higher prevalence of psychiatric symptoms is reported among women going through a symptomatic MT.6 There is limited information on the cause of this higher prevalence of psychiatric symptoms in women in general and in REM women in particular. While studies show that mental health and menopause symptoms are inextricably linked and disproportionately impact REM women,7 the factors that contribute to this difference in prevalence of mental illness among REM women are understudied.
Therefore, this scoping review presents a synthesis of the findings from the literature on mental health research as it relates to REM women during the MT. The aim is to summarize the evidence from literature on mental health during the MT in REM women in the United States with a focus on vasomotor symptoms (VMS), quality of life, mental health outcomes, and clinical management and to identify research gaps for future research efforts.
Materials and Methods
Frameworks
Intersectionality and the weathering hypothesis were used to inform the research question, hone the eligibility criteria, and to identify research gaps for this scoping review.8,9
Protocol and registration
We followed the scoping review methods from the Joanna Briggs Institute.10 A protocol was written a priori following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) Checklist11 (Supplementary File S1), and the PRISMA-ScR was used for reporting of this review.
Eligibility criteria
For inclusion, articles needed to include study findings on REM women during the MT where the age range fell within ages 48 and 58 years. Studies that included a mix of NHW and REM women were included. All studies must have been conducted in the United States, including its territories and published in English from 2005 to 2021. Studies were required to examine at least one of the following mental illnesses or risk factors: mood disorders, psychosis, generalized anxiety disorder, schizophrenia, substance use and co-occurring mental illnesses, obsessive compulsive disorder, bipolar disorder, disruptive mood dysregulation disorder, borderline personality disorder, family violence, intimate partner violence, and post-traumatic stress disorder (PTSD).
Articles were excluded if (1) REM women were not included in the study; (2) the article focused exclusively on women before or after the MT; (3) the research participants did not reside in the United States, including its territories; (4) the article was not in English; or (5) the article type was any type of review article, commentary, letter, conference abstract, errata, or corrigenda.
Information sources and search strategy
The search strategy was developed by the biomedical librarian (A.A.L.) in consultation with two members of the review team (T.L.J. and L.M.R.). The search strategy was validated through the retrieval of a preidentified set of relevant studies and peer reviewed by another librarian. The biomedical librarian searched five databases: CINAHL Plus (Ebscohost, 1981–current), EMBASE (Elsevier, 1947–current), PsycNet (American Psychological Association, 1806–current), PubMed (U.S. National Library of Medicine, 1946–current), and Web of Science: Core Collection (Clarivate Analytics, 1900–current). The searches were limited to results published in English from 2005 to 2021. In addition, a search strategy was used to limit studies conducted in the United States or its territories as that was the study location of interest. Finally, we used search strategies (see Supplementary File S2) to remove animal studies and specific article types (e.g., conference abstracts, letters, editorials, reviews) that were detailed in our exclusion criteria from search results.
A combination of keywords and controlled vocabulary search terms (i.e., CINAHL Subject Headings, EMTREE, Medical Subject Headings [MeSH], Thesaurus of Psychological Index Terms) were used for each concept of interest: menopause, REM women menopause, and mental health conditions. The searches were conducted in February 2022. See Supplementary File S2 for comprehensive details on the search strategy.
For all included articles, the bibliographies were reviewed to identify other potentially relevant articles not identified in the original search. In addition, review team members who are experts in the field of health disparities research, women's health, psychiatry, and clinical psychology identified additional relevant published research articles for potential inclusion. All articles identified through these supplemental methods were further screened using the eligibility criteria.
All results from the database searches were exported into EndNote 20 (Clarivate Analytics) and duplicates identified. The unique records retrieved were then exported into Covidence (Veritas Health Innovations), which was used for study screening and data collection.
Selection of sources of evidence
Before commencing screening, 6 reviewers conducted a pilot of the screening process at both levels using a random sample of 20 records selected by the biomedical librarian. After completing the screening pilot, the team discussed conflicts and clarified the eligibility criteria (see Supplementary File S1 for the protocol).
A two-step screening process was used. First, two reviewers independently screened the titles and abstracts using the eligibility criteria. Next, the full text of all articles included after title and abstract screening was independently screened using the same criteria. The six reviewers were divided into three pairs to screen the full text of articles to ensure that they met the eligibility criteria. A different third reviewer adjudicated discrepancies by reviewing the article and discussing the discrepancy with the two reviewers to arrive at a consensus for the article to be included or excluded.
Data collection and data items
Covidence was used for data collection. A pilot of the data collection step was completed by L.M.R. and T.L.J. and revisions made to the data collection form in Covidence before commencing to further clarify the items to collect. Two reviewers (L.M.R., T.L.J.) collected data from each included article. One reviewer (T.L.J.) reconciled all discrepancies in Covidence from data collection.
The data collected included citation information, race and ethnicity, total sample by race and ethnic group and overall, study setting, state/city of study, study design, intervention tested, stage of MT, menopausal symptoms reported, mental health and other health conditions studied, study instruments used, if a secondary data set was used and from where, study outcomes, study outcomes by racial and ethnic group, limitations of study, funding source, and possible conflicts of interest. Excel (Microsoft) was used for data cleaning and analysis. Key characteristics were extracted from the data and are found in Table 1. Data are descriptively summarized in the Results and qualitatively synthesized in the Discussion section.
Table 1.
Key Characteristics of Included Articles
| Author (year) | Study setting | Stage of menopause reported | Sample size | Racial and ethnic groups included | Study design | Mental illness or symptoms reported | Menopause symptoms reported | Were race and ethnicity included in analysis? |
|---|---|---|---|---|---|---|---|---|
| Freeman et al. (2005)39 | Pennsylvania | Stage of Reproductive Aging Workshop criteria (STRAW) | N = 436 | African American, White | Cohort study—Penn Ovarian Aging Study (POAS) | Anxiety, Depressive symptoms | Hot flashes | Yes |
| Schnatz et al. (2005)12 | Connecticut | Perimenopausal, Early postmenopausal | N = 80 | Hispanic, Non-Hispanic (White, African American, Asian, Other) | Cross-sectional study | Depressive symptoms | Hot flashes, Night sweats, Sexual dysfunction, Vaginal dryness, Sleep quality, Insomnia | No |
| Suau et al. (2005)27 | Puerto Rico | Menopausal, Premenopausal | N = 64 | Hispanic (Puerto Rican, Dominican, Cuban, South American, Central American) | Cross-sectional study | Depressive symptoms | Not reported | Not applicable |
| Xu et al. (2005)28 | Michigan | Perimenopausal, Early Postmenopausal, Premenopausal | N = 342 | White, African American, Other, Not Reported | Cross-sectional study | Anxiety, Depressive symptoms, Irritability | Hot flashes, Night sweats, Sexual dysfunction, Vaginal dryness | Yes |
| Freeman et al. (2006)13 | Pennsylvania | STRAW criteria | N = 231 | African American, White | Cohort study—POAS | Depression, Depressive symptoms | Hot flashes, Sleep quality, Insomnia | No |
| Kravitz et al. (2006)40 | California, Illinois, Massachusetts, Michigan, New Jersey, Pennsylvania | Perimenopausal, Premenopausal | N = 1,538 | African American, Caucasian, Japanese, Chinese | Cohort study—Study of Women Across the Nation (SWAN) | Depressive symptoms | Hot flashes, Night sweats | Yes |
| Sajatovic et al. (2006)29 | USA, Not Specified | Perimenopausal, Early Postmenopausal | N = 91 | African American, White, Other | Cross-sectional study | Bipolar disorder, Depression, Schizophrenia | Vasomotor, Psychosocial, Physical, Sexual | Yes |
| Wang (2006)30 | Florida | Perimenopausal, Early Postmenopausal, Premenopausal | N = 333 | Hispanic, White non-Hispanic | Cross-sectional study | Anxiety, Depressive symptoms, Irritability | Hot flashes, Night sweats, Sexual dysfunction, Vaginal dryness, Sleep quality, Insomnia | Yes |
| Bromberger et al. (2007)41 | California, Illinois, Massachusetts, Michigan, New Jersey, Pennsylvania | Perimenopausal, Early Postmenopausal, Premenopausal | N = 3,302 | African American, Chinese, Hispanic, Japanese, White | Cohort study—SWAN | Depressive symptoms | Hot flashes, Night sweats | Yes |
| Freeman et al. (2007)42 | Pennsylvania | STRAW criteria | N = 404 | African American, White | Cohort study—POAS | Depressive symptoms | Hot flashes, Sexual dysfunction, Vaginal dryness, Sleep quality, Insomnia | Yes |
| Gallicchio et al. (2007)31 | Maryland | Perimenopausal, Premenopausal | N = 634 | Black, White, Other | Cross-sectional study | Depressive symptoms | Hot flashes, Sexual dysfunction, Vaginal dryness, Sleep quality, Insomnia | Yes |
| Haren et al. (2007)24 | Missouri | Perimenopausal or Premenopausal, Postmenopausal | N = 244 | Black or African American | Cross-sectional study | Depressive symptoms | Not reported | Not applicable |
| Matthews et al. (2007)43 | California, Illinois, Massachusetts, Michigan, New Jersey, Pennsylvania | Perimenopausal, Early Postmenopausal, Premenopausal, surgical menopause, indeterminant | N = 3239 | African American, Chinese, Hispanic, Japanese, White |
Cohort study—SWAN | Depressive symptoms | Not reported | Yes |
| Torigoe and Brown (2007)26 | Hawaii | Perimenopausal, Early Postmenopausal, Premenopausal | N = 74 | Other: multiethnic | Cross-sectional—Hilo Women's Health Study | Other: mood; perceived stress | Hot flashes | Not applicable |
| Woods et al. (2007)14 | Washington | Menopause Transition, Middle and Late perimenopausal, Postmenopausal | N = 41 | African American Asian/Pacific Islander, White, Other: Hispanic, mixed | Cohort study—Seattle Midlife Women's Health Study (SMWHS) | Depressive symptoms | Hot flashes, Sexual dysfunction, Vaginal dryness, Sleep quality, Insomnia | No |
| Goldbacher (2007)44 | Pennsylvania | Perimenopausal, Early Postmenopausal, Postmenopausal included hysterectomy, oophorectomy | N = 421 | Black, White | Cohort study—SWAN | Anxiety, Depression | Not Reported | Yes |
| Nelson et al. (2008)45 | Pennsylvania | Menopause transition, Early Postmenopausal, Premenopausal | N = 436 | African American, Non-Hispanic White | Cohort study—Women living in Philadelphia | Anxiety, Depressive symptoms | Hot flashes, Night sweats, Sexual dysfunction, Vaginal dryness, Sleep quality, Insomnia | Yes |
| Pien et al. (2008)46 | Pennsylvania | Menopause Transition, Early Postmenopausal, Premenopausal | N = 436 | African American, White | Cohort study—POAS | Anxiety, Depressive symptoms | Hot flashes, Sleep quality, Insomnia | Yes |
| Thurston et al. (2008)47 | Pennsylvania | Perimenopausal, Early Postmenopausal, Premenopausal, indeterminant | N = 332 | African American, White | Cohort study—SWAN | Depressive symptoms, Other: Childhood trauma | Hot flashes, Night sweats | Yes |
| Thurston et al. (2008)48 | California, Illinois, Massachusetts, Michigan, New Jersey, Pennsylvania | Perimenopausal, Early Postmenopausal, Premenopausal, indeterminant | N = 1042 | African American, White, Chinese, Japanese | Cohort study—SWAN | Anxiety, Depressive symptoms, Irritability | Hot flashes, Night sweats, Sleep quality, Insomnia | Yes |
| Woods et al. (2008)15 | Washington | Menopause Transition, Early Postmenopausal, Premenopausal | N = 302 | African American Asian/Pacific Islander, White, Other: Hispanic, mixed | Cohort study—SMWHS | Depressive symptoms | Hot flashes | No |
| Avis et al. (2009)49 | United States not specified | Perimenopausal, Early Postmenopausal, Surgical menopause at follow-up were not included in analysis | N = 2943 | Caucasian, African American, Hispanic, Chinese, Japanese | Cohort study—SWAN | Depressive symptoms, Other: Stress | Hot flashes, Night sweats, Sexual dysfunction, Vaginal dryness, Sleep quality, Insomnia, Other: Leaking urine | Yes |
| Bromberger et al. (2009)50 | Pennsylvania | Perimenopausal, Premenopausal | N = 266 | African American, White | Cohort study—SWAN | Anxiety, Depression | Hot flashes, Night sweats | Yes |
| Woods et al. (2009)16 | Washington | Menopause Transition, Early Postmenopausal, Late reproductive, menopausal transition stages—early and late | N = 418 | African American, Asian/Pacific Islander, White, Other: Hispanic, mixed | Cohort study—SMWHS | Depressive symptoms | Hot flashes | No |
| Bromberger et al. (2010)51 | California, Illinois, Massachusetts, Michigan, New Jersey, Pennsylvania | Perimenopausal, Early Postmenopausal, Premenopausal | N = 3296 | African American, White, Chinese, Japanese, Hispanic | Cohort study—SWAN | Depressive symptoms | Hot flashes, Night sweats | Yes |
| Green et al. (2010)52 | New Jersey | Premenopausal, Perimenopausal, and Postmenopausal | N = 419 | Hispanic, White | Cohort study—SWAN | Anxiety, Depressive symptoms | Sleep quality, Insomnia | Yes |
| Greendale et al. (2010)53 | California, Illinois, Massachusetts, Michigan, New Jersey, Pennsylvania | Perimenopausal, Early Postmenopausal, Premenopausal | N = 1903 | African American, Caucasian, Chinese, Hispanic, Japanese | Cohort study—SWAN | Anxiety, Depressive symptoms, Irritability | Hot flashes, Night sweats, Sleep quality, Insomnia | Yes |
| Kornstein et al. (2010)32 | 41 primary or psychiatric care settings across the United States | Premenopausal, Perimenopausal Early Postmenopausal | N = 2652 | Race: Black, White, Ethnicity: Hispanic, Not Hispanic | Cross-sectional study—secondary analysis of Sequenced Treatment Alternatives to Relieve Depression (STAR*D) | Depression, Depressive symptoms, Comorbidity: Anxiety, PTSD Obsessive Compulsive Disorder, social phobia, agoraphobia, somatoform, hypochondriasis, bulimia, and drug and alcohol abuse | Not reported | Yes |
| Matthews et al. (2010)54 | California, Illinois, Massachusetts, Michigan, New Jersey, Pennsylvania | Perimenopausal, Early Postmenopausal, Hysterectomy, status unknown | N = 1781 | African American, White, Chinese, Hispanic, Japanese | Cohort study—SWAN | Depressive symptoms | Sleep problems | Yes |
| Rebbeck et al. (2010)55 | Pennsylvania | Menopause Transition, Early Postmenopausal, Premenopausal | N = 436 | African American, White | Cohort study—POAS | Depressive symptoms | Hot flashes | Yes |
| Schnatz et al. (2010)56 | Connecticut | Perimenopausal, Postmenopausal | N = 102 | Hispanic, Non-Hispanic, Ethnicity not reported | Cohort study—Women's Life Center at Hartford Hospital | Anxiety, Depression | Sexual dysfunction, Vaginal dryness, Sleep quality, Insomnia | Yes |
| Seritan et al. (2010)33 | California | Perimenopausal, Early Postmenopausal, Premenopausal | N = 487 | African American, White, Asian, Hispanic | Cross-sectional study | Anxiety, Depressive symptoms | Hot flashes, Night sweats | Yes |
| Wheatley (2009)17 | Florida | Perimenopausal, Postmenopausal | N = 206 | African American | Cross-sectional study | Depressive symptoms | Hot flashes, Sexual dysfunction, Vaginal dryness, Sleep quality, Insomnia | No |
| Bromberger et al. (2011)57 | Pennsylvania | Perimenopausal, Menopause Transition, Early Postmenopausal Premenopausal | N = 221 | African American, Caucasian | Cohort study—SWAN | Depression, Depressive symptoms | Hot flashes, Night sweats | Yes |
| Kravitz et al. (2011)58 | California, Illinois, Michigan, Pennsylvania | Perimenopausal, Early Postmenopausal | N = 343 | African American, Caucasian, or White, Chinese | Cohort study—SWAN | Anxiety, Depressive symptoms | Hot flashes, Night sweats | Yes |
| Morrison et al. (2011)59 | Pennsylvania | STRAW criteria | N = 436 | African American, White | Cohort study—POAS | Depression, Depressive symptoms | Not reported | Yes |
| Woods et al. (2011)18 | Washington | Menopause Transition, Early Postmenopausal | N = 184 | African American, Asian/Pacific Islander, White, Other: Hispanic, mixed | Cohort study—SMWHS | Anxiety, Depressive symptoms | Hot flashes, sleep quality, Insomnia | No |
| Bromberger et al. (2012)60 | Illinois, New Jersey, Pennsylvania | Perimenopausal Premenopausal | N = 934 | African American, Hispanic, White, | Cohort study—SWAN | Depression, Other: Premenstrual symptoms (mood) | Not reported | Yes |
| Gibson et al. (2012)61 | California, Illinois, Massachusetts, Michigan, New Jersey, Pennsylvania | Perimenopausal Premenopausal, hysterectomy with ovarian conservation, reported hysterectomy with bilateral oophorectomy | N = 1970 | African American, Hispanic, Asian, White | Cohort study—SWAN | Anxiety, Depressive symptoms | Not reported | Yes |
| Brandon et al. (2013)19 | Texas, Pennsylvania | Perimenopausal, Early Postmenopausal Premenopausal, surgical menopause | N = 355 | White, Black, Hispanic, Other | Nonrandomized Clinical Trial | Depression, Depressive symptoms | Not reported | No |
| Bromberger et al. (2013)62 | California, Illinois, Massachusetts, Michigan, New Jersey, Pennsylvania | Perimenopausal, Early Postmenopausal, Premenopausal, postmenopausal, and hormone therapy | N = 2956 | African American, White, Chinese, Hispanic, Japanese | Cohort study—SWAN | Anxiety | Hot flashes, Night sweats | Yes |
| Greenblum et al. (2013)20 | Florida | Menopause Transition, Early Postmenopausal | N = 112 | White, Hispanic, African American, Asian | Cross-sectional study | Anxiety, Irritability | Hot flashes, night sweats, sexual dysfunction, Vaginal dryness, sleep quality, Insomnia | No |
| Kornstein et al. (2013)21 | 41 primary or psychiatric care settings across the United States | Premenopausal, Perimenopausal, Postmenopausal | N = 1883 | Race: Black, White, Ethnicity: Hispanic, Not Hispanic |
Clinical trial—secondary analysis of STAR*D | Depression, Depressive symptoms | Not reported | No |
| Appelhans et al. (2014)63 | California, Illinois, Massachusetts, Michigan, New Jersey, Pennsylvania | Perimenopausal, Early Postmenopausal, Premenopausal, undetermined, and surgical menopause | N = 3220 | African American, White, Chinese, Hispanic, Japanese |
Cohort study—SWAN | Depressive symptoms | Not reported | Yes |
| Colvin et al. (2014)64 | Pennsylvania | Perimenopausal, Premenopausal | N = 303 | African American, White | Cohort study—SWAN | Anxiety, Depression | Hot flashes, Night sweats | Yes |
| Kravitz et al. (2014)65 | Pennsylvania | Perimenopausal, Premenopausal | N = 425 | Black, White |
Cohort study—SWAN | Anxiety, Depression, Depressive symptoms | Hot flashes, Night sweats | Yes |
| Richard et al. (2014)34 | USA Not Specified | Perimenopausal | N = 193 | White, Black, Mexican American, Other | Cross-sectional study—National Health and Nutrition Survey | Depressive symptoms | Not reported | Yes |
| Avis et al. (2015)66 | California, Illinois, Massachusetts, Michigan, New Jersey, Pennsylvania | Perimenopausal, Early Postmenopausal, Premenopausal | N = 1,449 | African American, White, Chinese, Hispanic, Japanese | Cohort study—SWAN | Anxiety, Depressive symptoms, Other: Perceived stress | Hot flashes, Night sweats | Yes |
| Dugan et al. (2015)67 | California, Illinois, Massachusetts, Michigan, New Jersey, Pennsylvania | Perimenopausal, Early Postmenopausal | N = 2,891 | African American, White, Chinese, Hispanic, Japanese | Cohort study—SWAN | Depressive symptoms | Hot flashes, Night sweats | Yes |
| Im et al. (2015)35 | United States Not specified | Perimenopausal, Early Postmenopausal, Premenopausal | N = 542 | African American, White, Hispanic, Asian | Cross-sectional study—secondary analysis of a large internet survey study | Depressive symptoms | Not reported | Yes |
| Prairie et al. (2015)68 | California, Illinois, Massachusetts, Michigan, New Jersey, Pennsylvania | Perimenopausal, Early Postmenopausal, Premenopausal, surgical postmenopausal, undeterminable | N = 1716 | African American, White, Chinese, Japanese, Hispanic | Cohort study—SWAN | Depressive symptoms | Sexual dysfunction, Vaginal dryness, Sleep quality, Insomnia | Yes |
| Freeman et al. (2016)69 | Pennsylvania | Straw criteria | N = 436 | African American, Black, Caribbean, Continental African, White, Non-Hispanic | Cohort study—POAS | Anxiety, Depression, Irritability, Mood deterioration | Hot flashes, Night sweat, Sexual dysfunction, Vaginal dryness Sleep quality, Insomnia | Yes |
| Keshishian et al. (2016)22 | United States Not specified | Menopause symptoms diagnosis and/or hormone therapy claim, No menopause symptoms and/or a hormone therapy claim | N = 142,152 | Black, White, Hispanic, Asian, American Indian or Alaskan Native, Native Hawaiian or Other Pacific Islander, Other | Cross-sectional study—U.S. national database | Anxiety, Depression | Sleep quality, Insomnia | No |
| Colvin et al. (2017)70 | Pennsylvania | Perimenopausal, Early Postmenopausal, Premenopausal | N = 303 | African American, Black, Caribbean, Continental African, White, Non-Hispanic | Cohort study—SWAN | Depression | Hot flashes, Night sweats | Yes |
| Marsh et al. (2017)71 | California, Illinois, Massachusetts, Michigan, New Jersey, Pennsylvania | Perimenopausal, Menopause Transition, Early Postmenopausal | N = 1,306 | African American, White, Chinese, Hispanic, Japanese | Cohort study—SWAN | Depressive symptoms | Hot flashes, Night sweats | Yes |
| Gordon et al. (2018)76 | North Carolina | STRAW criteria | N = 172 | African American, White | Randomized Clinical Trial | Depressive symptoms | Hot flashes, Night sweats | Yes |
| Bromberger et al. (2019)72 | California, Illinois, Massachusetts, Michigan, New Jersey, Pennsylvania | Perimenopausal, Premenopausal | N = 3,300 | White, Black, Japanese, Chinese Hispanic | Cohort study—SWAN | Depressive symptoms | Hot flashes, Night sweats, Sleep quality, Insomnia | Yes |
| Gibson et al. (2019)73 | California | Perimenopausal, Menopause Transition, Postmenopausal, hormone therapy |
N = 2,016 | White, Black or African American, Latina or Hispanic | Cohort study—Reproductive Risks of Incontinence Study at Kaiser | Anxiety, Depressive symptoms, PTSD | Hot flashes, Night sweats, Sexual dysfunction, Vaginal dryness, Sleep quality, Insomnia | Yes |
| Dickins et al. (2020)23 | Massachusetts | Perimenopausal | N = 33 | Black or African American, White, American Indian, More than one race, Hispanic | Cross-sectional study—Secondary data analysis of a study of menopause and health symptoms in women with and without HIV | Anxiety, Depression | Sleep quality, Insomnia | No |
| Im et al. (2020)36 | USA Not Specified | Perimenopausal, Early Postmenopausal, Premenopausal | N = 1,054 | African American, White, Hispanic, Asian | Cross-sectional study—Secondary analysis of two larger internet survey studies | Depressive symptoms | Sleep quality, Insomnia | Yes |
| Jones et al. (2020)74 | California | Perimenopausal, Early Postmenopausal, Premenopausal | N = 264 | African American, Latina, White | Cohort study—Midlife Women's Health Study | Depressive symptoms | Hours of sleep (self-reported) | Yes |
| Still et al. (2020)25 | Midwest, USA | Perimenopausal, Menopausal | N = 184 | African American, Black, Caribbean, Continental African | Cross-sectional study—Secondary analysis of a large multisite study | Depression | Hot flashes, Sexual dysfunction, Vaginal dryness, Sleep quality, Insomnia | Not applicable |
| De Mello et al. (2021)37 | Arizona | Perimenopausal, Early Postmenopausal | N = 255 | African American, Asian, Hispanic, White, Other | Cross-sectional study | Anxiety, Depressive symptoms | Hot flashes, Sexual dysfunction, Vaginal dryness | Yes |
| de Wit et al. (2021)75 | Massachusetts | STRAW criteria | N = 50 | Black, White, Native American, Asian | 8-week Observational study | Depressive symptoms, Irritability | Vasomotor symptom frequency | Yes |
| Ji et al. (2021)38 | Texas | Menopausal | N = 384 | Black, White, Hispanic | Cross-sectional study—Secondary analysis of the Dallas Heart Study | Depressive symptoms | Hot flashes, Sexual dysfunction, Vaginal dryness | Yes |
Patient and public involvement
While neither patients nor the public were involved in this scoping review, the results may be of interest and most generalizable to persons who identify as REM women, their clinicians, researchers, and funders in that knowledge gaps are identified, and future areas of research highlighted in the Discussion section.
Results
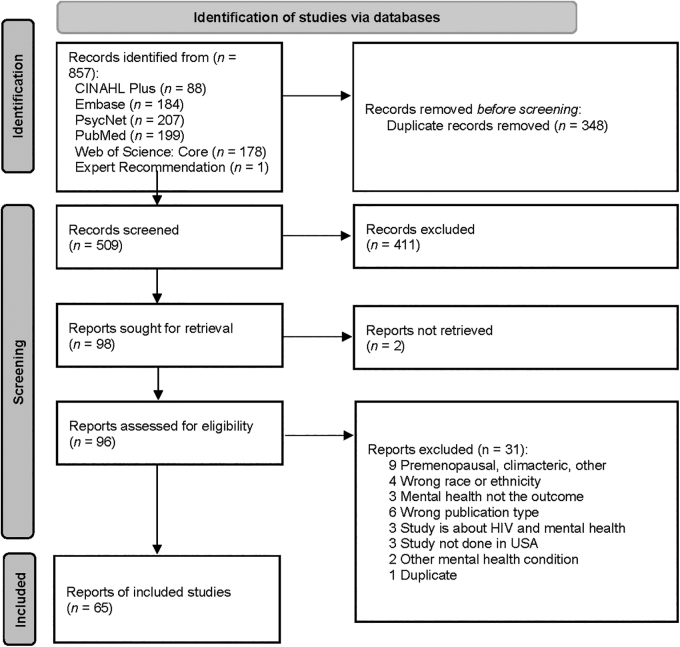
A total of 857 articles were retrieved from the 5 databases searched, including 1 article recommended by team members, of which 348 were duplicates and 509 were unique. Of the 509 screened at title and abstract level, 411 were excluded and 96 proceeded to full text review. After full text screening, 65 articles were included in the review and 31 were excluded (Fig. 1).
FIG. 1.
PRISMA Flow Diagram.
Study characteristics
Sixty-five studies were reported on mental illnesses during the MT among REM women. The key characteristics of race, ethnicity, sample size, mental health symptoms or illnesses, stage of MT, menopause symptoms, study design, and study settings are presented in Table 1.
Race and ethnicity
Twelve studies12–23 did not include race or ethnicity in the statistical analysis, and three studies included only Black, African American, Caribbean, or Continental African women,17,24,25 one included only “multiethnic” women from Hilo, Hawaii,26 and one included only Hispanic women.27
Study design
There were 20 cross-sectional,12,17,20,22–38 41 cohort,13–16,18,39–74 1 observational,75 and 3 clinical trial studies.19,21,76 Of the cohort studies, 26 were from the Study of Women Across the Nation (SWAN),40,41,43,44,47–54,57,58,60–68,70–72 7 from the Penn Ovarian Aging Study (POAS),13,39,46,55,59,69 4 from the Seattle Midlife Women's Health Study (SMWHS),14–16,18,74 1 from the Midlife Women's Health Study,74 1 from the Reproductive Risks of Incontinence Study at Kaiser,73 1 from data collected at Women's Life Center at Hartford Hospital,56 and 1 from data collected from women in Philadelphia.45
Study setting
Thirty-nine studies12–18,20,23,24,26–28,30,31,33,37–39,42–47,50,52,55–57,59,64,65,69,70,73–76 used a state or U.S. territory as the study setting. Eighteen studies19,25,40,41,47,51,53,54,58,60–63,66–68,71,72 used multiple states as the study setting, and eight studies21,22,29,32,34–36,49 used a nationwide study setting. The SWAN and POAS cohort study data recruited women from urban and suburban areas. Sample Size:The sample sizes ranged from 33 to 142,152, with the largest using data from a U.S. national database.
Stage of MT
Seven studies used the Stages of Reproductive Aging Workshop to determine the stage of MT,13,39,42,59,69,75,76 seven studies included surgical menopause, hysterectomy, or oophorectomy in the definition of the stage of MT,19,43,44,49,54,61,63 and the rest defined the menopausal stage by menstrual bleeding patterns, timing of last menstrual period, or midlife age range.
Mental illness or symptoms
The majority (63 of 65) of studies reported findings on depressive symptoms or major depression. This was followed by 26 studies on anxiety,18,20,22,23,28,30,32,33,37,39,44–46,48,50,52,53,56,58,60,61,64–66,69,73 and 7 assessing irritability.20,28,30,48,53,69,75 Three studies reported findings on serious mental illnesses such as PTSD, bipolar disorder, or schizophrenia.29,32,73
Menopausal symptoms
The majority of studies reported on menopause symptoms such as vasomotor or sleep problems (52 of 65) and how these related to mental health and quality of life. Of the three clinical trials, one was a double-blinded, placebo-controlled trial of estradiol and progesterone,76 one was a nonrandomized trial of cognitive therapy (CT),19 and one was a secondary analysis of Sequenced Treatment Alternatives to Relieve Depression (STAR*D)21 with only one76 of these studies, including race/ethnicity in the analysis.76
Discussion
Mental health outcomes during MT
The MT is a period of increased vulnerability to negative mental health outcomes, particularly depression. Studies that include REM women report prevalence rates of depressive symptoms ranging from 16.5% to 28%31,41,68,74 or major depression ranging from 11% to 15.8%.50,60 A 10-year study found a two- to four-fold increase in risk for a major depressive episode in women who were in the MT or postmenopausal compared to women who were premenopausal.57 Similar findings have been reported by other studies.13,25,41,42,51 In general, studies show that the risk is higher in the MT than in postmenopause,33 with some suggestion that late MT is the most vulnerable period.15,70 However, despite this consensus, some studies have found either no relationship between menopausal status and depressive symptoms or lower depressive symptoms in the MT compared to premenopause.31,59,61 These discrepancies were attributed to differences in subject samples (e.g., inclusion of only women without a history of mental health problems, and not taking psychotropic medication).
There are exceptions,12,38,74 but prevalence rates tend to be higher in Black and Hispanic women during MT.30,41,51 For example, in the SWAN study the prevalence rate for an episode of major depression over 10 years of follow-up was 33.8% for Black women compared to 29.9% for NHW women,57 and another SWAN report showed that Black women are 71% more likely to have an onset of depression over 7 years of follow-up.50 Higher rates of depression in Black compared to NHW women have been reported in other cohorts as well.34 Despite these relevantly consistent findings, there is evidence that Black women are less likely than NHW women to have a trajectory of increasing depressive symptoms over time, although the effect did not remain significant after controlling for education, financial strain, smoking, and bodily pain.72 Studies generally show higher rates of depression in Hispanic compared to NHW women.52,71,77 A longitudinal study reported that Hispanic women were more likely than NHW women to have a trajectory of increasing depressive symptoms over time.72 There is evidence of variability within Hispanic women. One study reported higher depressive symptoms in Puerto Rican women than in Dominican, Cuban, and South American women.52
Depression is associated with several negative outcomes. In addition to more severe menopausal symptoms such as hot flash bother48 and decreased sexual desire,14 negative physical outcomes include metabolic syndrome44 and greater waist circumference,44 particularly when depression is experienced in combination with nonemployment.63 Depression is associated with sleep disruption,14 higher levels of stress,16 and risk for other mental health symptoms, such as drug and alcohol misuse and anxiety.44 There is also evidence of depression-related cognitive dysfunction such as difficulty concentrating14 and slower cognitive processing speed.53 Some of the negative correlates appear to disproportionately impact Black and Hispanic women. For example, one study reported that Black and Hispanic women were more likely than NHW women to report functional disability,49 and another study found that sleep disruption was more strongly related to depression in Hispanic women.72 However, another study that examined depressive symptoms and sleep related symptoms among REM women in the MT found that total number of depressive and sleep related symptoms were highest among Asian women followed by Hispanic and Black women. Asian women were more likely to experience depression than other REM women but were frequently underreported, underdiagnosed, and undertreated for depressive and sleep related symptoms during midlife.36
Symptoms of anxiety may also increase during the MT,62 but the evidence for REM differences is mixed. Higher anxiety has been reported in Hispanic and Black women compared to NHW women.62 However, one study showed increasing anxiety in NHW but not Black women,28 while another found the opposite.61 Within Hispanic women, Dominican women report more trait anxiety than South American and Cuban women. Risk factors for anxiety include more severe menopausal symptoms,33,39,62 sexual dysfunction,56 financial strain and other stressors,23,62 previous anxiety,62 lower education,62 and poor health.62 Anxiety symptoms are associated with reduced quality of life,20 increases in blood pressure,26 reduced memory and slower processing speed,53 and a higher risk for depression.65
There is less research on other mental illnesses during the MT. Potential reasons for the gap in research include but are not limited to the possibility that women with other mental illnesses may be lost to follow-up, the lack of targeted sampling of women with other mental illnesses, or exclusion criteria that prohibited women with serious mental illness from participating in clinical trials. A few studies suggest that lifetime history of interpersonal violence and sexual assault, childhood abuse or neglect, and current PTSD are associated with menopause symptoms.47,73 Women with serious mental illness (schizophrenia or schizoaffective disorder, bipolar disorder, and major depression) report feeling depressed, anxious, tired or worn out, and lacking in energy, and report experiencing poor memory.29
VMS impact on mental health and quality of life
Although most women experience some degree of VMS during the MT, Black women report the longest duration (median 10.1 years) of VMS compared to NHW, Chinese, Japanese, and Hispanic women.66 Risk factors for longer duration of VMS include younger age, lower educational level, greater perceived stress, and symptom sensitivity.66 Self-reported depressive and anxiety symptoms were associated with bothersomeness of VMS.33 Findings from the SWAN Mental Health study found a history of childhood abuse, and neglect was associated with increased VMS. When comparisons of NHW and Black women with a past history of child abuse and neglect and VMS were conducted, the findings were not statistically significant but did suggest a stronger association in Black women.47 When researchers controlled for frequency of VMS, Black women were more bothered by VMS than NHW and Japanese women but the reason for REM differences is understudied.48
Quality of life during the MT includes a complex array of factors. A study of midlife women found that sleep disturbances, fatigue, and anxiety most significantly affected quality of life.20 Lower health related quality of life, reduced role functioning, more negative appraisal of aging, and perceived poorer health were higher in women with depression.16,49,66 African American and Hispanic women reported more bodily pain and reduced social functioning that NHW.49
Clinical management of mental health during MT
Treatments that specifically target mood disorders, anxiety, and psychosis associated with the MT have not been developed. However, several investigators have found that standard treatments for depression and anxiety are effective for some women in the MT. Expert consensus guidelines recommend selective serotonin reuptake inhibitors (SSRIs), serotonin and norepinephrine reuptake inhibitors (SNRIs), and psychotherapy as first-line treatments.78 While estrogen-based therapies have not been FDA approved for depression, there is evidence to suggest that estrogen has similar antidepressant effects to SSRIs and SNRIs for women during the MT but not postmenopause.79,80 Estrogen therapies78 have been shown to be most effective for treatment of depression as a monotherapy or augmentation to antidepressant treatment for women during the MT.
Despite the reported higher prevalence of depression in Black and Hispanic women, few studies specifically address feasibility, accessibility, and efficacy of frontline treatments for MT associated mood disorders among REM women. No studies addressed treatment of symptoms specifically due to psychosis, anxiety, or PTSD, known risk factors that are highly prevalent for REM women. Among the two studies19,21 of frontline treatments for depression during MT, treatment rates were not detailed by race or ethnicity. The impact of secondary or other specific interventions (i.e., taking hormonal therapy, exercising more than the recommended physical activity guidelines) on the outcome of depressive symptoms was explored in two studies32,67 but only included small samples of REM groups with the intervention (31% and 16.8%, respectively). One study, a randomized double-blinded, placebo trial of estradiol and progesterone, included similar sample sizes of REM (85%) to White (81%) women in the treatment intervention group.76 All, but one study,35 which assessed views on exercise and associated depressive symptoms, fell short of comparing REM and NHW women. In addition, receptiveness and accessibility to treatment were understudied.
Data from the STAR*D study were analyzed to understand if depression in women differs by stage of menopause or hormone therapy. The results from this analysis showed that women taking hormone therapy were significantly less likely to be Hispanic, Black, or of another race and were more likely to be NHW, more educated, married, and privately insured. Women taking hormone therapy were more likely to have a recurrent course of depression along with increased medical comorbidities. This analysis showed that women taking hormone therapy reported better physical functioning, fewer melancholic features, and less sympathetic arousal compared with women not taking hormone therapy.32
Exercise has been shown to be part of a combination of effective treatments for mood disorders during the MT. A study of REM women (Hispanic [23.4%], Asian [22.7%], Black [24.9%], and NHW [29.0%]) found that depressive symptoms negatively correlated with active living and exercise physical activities and positively correlated with occupational physical activities. Race was not associated with the magnitude of exercise related improvement in mood.35 Analysis of SWAN data found that physical activity was associated with lower risk of high depressive symptoms (i.e., CES-D score of 16 or higher) across 10 years. Japanese and Hispanic women reported higher depressive symptoms compared to NHW women. Whether exercise effectively reduces high depressive symptoms for Japanese or Hispanic women was not discussed.67
Among psychotherapies, CT has the most evidence for effective treatment of mood during the MT. A study of the effectiveness of CT in women who were not taking or had discontinued psychotropic medication indicated that greater than one-half (55%) of the women, despite stage of menopause, had a reduction in symptoms. In addition, the rate of early and late response, as well as noncompletion and completion of CT, was assessed but didn't compare differences in these categories for women of varying racial backgrounds.19
Research gaps (translational, intervention, and services research)
This scoping review identified several research gaps on mental illness during the MT in REM women. Approximately 25% of the studies did not consider REM group in the statistical analysis. Another gap was the lack of large enough sample sizes to explain REM differences in studies that investigated treatment responses to therapeutic interventions for mental health symptoms. This highlights the necessity of sample sizes sufficiently powered to analyze data by REM group for future studies.
Health care services delivery, prevention intervention, intersectional research, mixed methods, and implementation science approaches are also absent from this body of research. Gender identity and sexual orientation were also not considered in this research. Incorporating research that includes gender identity and sexual orientation data will strengthen mental health research during the MT. Most studies did not consistently report the use of hormone therapy by study participants and its effect on mental health outcomes. Improved reporting on use of hormone therapy among REM women will advance this area of research. Most studies did not include American Indian, Alaskan Native, Native Hawaiian, and Pacific Islander women. Finally, the current literature does not address structural racism and as such scientists often mislabeled race as the cause of inequities when racism and intersecting systems of oppression are the root causes. Each of these topics deserves prospective research.
Limitations
Although the highest rates of suicide for women occur during ages 45–64 years,81 coinciding with the MT, no articles on suicidal ideation were included in this scoping review. Although mental illness can contribute to a heightened risk for suicidal thoughts and behavior, suicide is often a response to a stressful life event that can include social, cultural, and economic factors as well. Future research is needed to examine suicidal behavior during MT with a focus on REM women.
Conclusions
To our knowledge, this is the first scoping review on mental health during the MT among REM women living in the United States. These findings reflect that mental illness among REM women is understudied. Nonetheless, there is an opportunity to improve mental health research by putting REM women at the center of research through an integration of societal, economic, cultural, and biological factors and the use of research methods that advance a better understanding of mental illness among REM women. This transformative research requires multidisciplinary science that advances multilevel interventions grounded in local, state, and national policy efforts to improve mental health outcomes for REM women.
Supplementary Material
Acknowledgment
The authors thank Brittney Haynes, National Institutes of Mental Health, for her assistance with screening during this scoping review and Yolanda L. Jones, National Institutes of Health Library, and Brian Barnett, National Institute of Mental Health, for editing assistance.
Authors' Contributions
T.L.J.: Conceptualization, Methodology, Investigation; Data Curation; Project Administration; Writing—Original draft preparation; Writing—Reviewing and Editing.
L.M.R.: Methodology, Investigation; Data Curation; Writing—Original draft preparation; Writing—Reviewing and Editing.
M.S.A.: Abstract Screening; Investigation; Writing—Original draft preparation.
C.T.C.: Investigation; Writing—Original draft preparation; Writing—Reviewing and Editing.
V.M.D.: Investigation; Writing—Original draft preparation.
A.A.L.: Data Curation; Methodology; Writing—Original draft preparation; Writing—Reviewing and Editing; Project Administration (supporting).
M.S.: Investigation; Writing—Original draft preparation; Writing—Reviewing and Editing.
Author Disclosure Statement
V.M.D. is owner of CerebroFit Integrated Brain Health. C.T.C. provides consultation services for Seven Starling and SixSense.
No other competing financial interests exist.
Funding Information
For T.L.J. and L.M.R., this work was funded as part of the National Institute of Mental Health's Extramural Research Program. For A.A.L., this work was done as part of the NIH Library, Office of Research Services, support of the NIH Intramural Research Program. For V.M.D., this work is supported by the National Institute on Aging (Grant No. U19AG073172, U19AG065169, R21AG077307), the National Science Foundation (Grant No. 2112455), and the Alzheimer's Association (Grant No. AARG-NTF-21-852145).
Supplementary Material
References
- 1. Bailey ZD, Krieger N, Agénor M, et al. Structural racism and health inequities in the USA: Evidence and interventions. Lancet 2017;389(10077):1453–1463; doi: 10.1016/s0140-6736(17)30569-x [DOI] [PubMed] [Google Scholar]
- 2. Williams DR, Lawrence JA, Davis BA, et al. Understanding how discrimination can affect health. Health Serv Res 2019;54 Suppl 2(Suppl 2):1374–1388; doi: 10.1111/1475-6773.13222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Letang SK, Lin SS, Parmelee PA, et al. Ethnoracial disparities in cognition are associated with multiple socioeconomic status-stress pathways. Cogn Res Princ Implic 2021;6(1):64; doi: 10.1186/s41235-021-00329-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Sherman S. Defining the menopause transition. Am J Med 2005;118(12B):3S–7S; doi: 10.1016/j.amjmed.2005.11.002 [DOI] [PubMed] [Google Scholar]
- 5. OlaOlorun FM, Shen W. Menopause. In: Oxford Research Encyclopedia of Global Public Health. Oxford University Press: 2020. Available from: https://oxfordre.com/publichealth/view/10.1093/acrefore/9780190632366.001.0001/acrefore-9780190632366-e-176 [Last accessed: July 31, 2023].
- 6. Hu LY, Shen CC, Hung JH, et al. Risk of psychiatric disorders following symptomatic menopausal transition: A nationwide population-based retrospective cohort study. Medicine (Baltimore) 2016;95(6):e2800; doi: 10.1097/md.0000000000002800 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Harlow SD, Burnett-Bowie SM, Greendale GA, et al. Disparities in reproductive aging and midlife health between Black and White women: The Study of Women's Health Across the Nation (SWAN). Womens Midlife Health 2022;8(1):3; doi: 10.1186/s40695-022-00073-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Bowleg L. The problem with the phrase women and minorities: Intersectionality—an important theoretical framework for public health. Am J Public Health 2012;102(7):1267–1273; doi: 10.2105/AJPH.2012.300750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Forde AT, Crookes DM, Suglia SF, et al. The weathering hypothesis as an explanation for racial disparities in health: A systematic review. Ann Epidemiol 2019;33:1–18.e3; doi: 10.1016/j.annepidem.2019.02.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Peters M, Godfrey C, McInerney P, et al. Chapter 11: Scoping Reviews. In: JBI Manual for Evidence Synthesis (Aromataris E, Munn Z, eds.) JBI: Adelaide, Australia; 2020. Available from: https://synthesismanual.jbi.global/ [Last accessed: July 31, 2023].
- 11. Tricco AC, Lillie E, Zarin W, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and explanation. Ann Intern Med 2018;169(7):467–473; doi: 10.7326/m18-0850 [DOI] [PubMed] [Google Scholar]
- 12. Schnatz PF, Banever AE, Greene JF, et al. Pilot study of menopause symptoms in a clinic population. Menopause 2005;12(5):623–629; doi: 10.1097/01.GME.0000156347.54144.AC [DOI] [PubMed] [Google Scholar]
- 13. Freeman EW, Sammel MD, Lin H, et al. Associations of hormones and menopausal status with depressed mood in women with no history of depression. Arch Gen Psychiatry 2006;63(4):375–382; doi: 10.1001/archpsyc.63.4.375 [DOI] [PubMed] [Google Scholar]
- 14. Woods NF, Smith-Dijulio K, Percival DB, et al. Symptoms during the menopausal transition and early postmenopause and their relation to endocrine levels over time: Observations from the Seattle Midlife Women's Health Study. J Womens Health (Larchmt) 2007;16(5):667–677; doi: 10.1089/jwh.2006.0138 [DOI] [PubMed] [Google Scholar]
- 15. Woods NF, Smith-DiJulio K, Percival DB, et al. Depressed mood during the menopausal transition and early postmenopause: Observations from the Seattle Midlife Women's Health Study. Menopause 2008;15(2):223–232; doi: 10.1097/gme.0b013e3181450fc2 [DOI] [PubMed] [Google Scholar]
- 16. Woods NF, Mitchell ES, Percival DB, et al. Is the menopausal transition stressful? Observations of perceived stress from the Seattle Midlife Women's Health Study. Menopause 2009;16(1):90–97; doi: 10.1097/gme.0b013e31817ed261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Wheatley MA. Personal characteristics, chronic stress, and depressive symptoms in midlife African-American women. Case Western Reserve University; Columbus, OH, USA; 2009. Available from: https://rave.ohiolink.edu/etdc/view?acc_num=case1239929001 [Last accessed: July 31, 2023].
- 18. Woods NF, Mitchell ES. Symptom interference with work and relationships during the menopausal transition and early postmenopause: Observations from the Seattle Midlife Women's Health Study. Menopause 2011;18(6):654–661; doi: 10.1097/gme.0b013e318205bd76 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Brandon AR, Minhajuddin A, Thase ME, et al. Impact of reproductive status and age on response of depressed women to cognitive therapy. J Womens Health (Larchmt) 2013;22(1):58–66; doi: 10.1089/jwh.2011.3427 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Greenblum CA, Rowe MA, Neff DF, et al. Midlife women: Symptoms associated with menopausal transition and early postmenopause and quality of life. Menopause 2013;20(1):22–27; doi: 10.1097/gme.0b013e31825a2a91 [DOI] [PubMed] [Google Scholar]
- 21. Kornstein S, Toups M, Rush A, et al. Do menopause status and use of hormone therapy affect antidepressant treatment response? Findings from the Sequenced Treatment Alternatives to Relieve Depression (STAR*D) study. J Womens Health (Larchmt) 2013;22(2):121–131; doi: 10.1089/jwh.2012.3479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Keshishian A, Wang Y, Xie L, et al. The economic impact of symptomatic menopause among low-socioeconomic women in the United States. Expert Rev Pharmacoecon Outcomes Res 2016;16(2):305–313; doi: 10.1586/14737167.2015.1073589 [DOI] [PubMed] [Google Scholar]
- 23. Dickins KA, Looby SE. Behavioral and psychological health inequities in income disparate perimenopausal women: A brief report. Menopause 2020;28(1):86–92; doi: 10.1097/gme.0000000000001650 [DOI] [PubMed] [Google Scholar]
- 24. Haren MT, Malmstrom TK, Banks WA, et al. Lower serum DHEAS levels are associated with a higher degree of physical disability and depressive symptoms in middle-aged to older African American women. Maturitas 2007;57(4):347–360; doi: 10.1016/j.maturitas.2007.03.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Still CH, Tahir S, Yarandi HN, et al. Association of psychosocial symptoms, blood pressure, and menopausal status in African-American women. West J Nurs Res 2020;42(10):784–794; doi: 10.1177/0193945919898477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Torigoe S, Brown D. Blood pressure, vasomotor symptoms, and emotional stress in multiethnic menopausal women. Ethn Dis 2007;17(4 SUPPL. 5):S543–S544. [Google Scholar]
- 27. Suau GM, Normandia R, Rodriguez R, et al. Depressive symptoms and risk factors among perimenopausal women. P R Health Sci J 2005;24(3):207–210. [PubMed] [Google Scholar]
- 28. Xu JP, Bartoecs M, Neale AV, et al. Natural history of menopause symptoms in primary care patients: A MetroNet study. J Am Board Fam Med 2005;18(5):374–382; doi: 10.3122/jabfm.18.5.374 [DOI] [PubMed] [Google Scholar]
- 29. Sajatovic M, Friedman SH, Schuermeyer IN, et al. Menopause knowledge and subjective experience among peri- and postmenopausal women with bipolar disorder, schizophrenia and major depression. J Nerv Ment Dis 2006;194(3):173–178; doi: 10.1097/01.nmd.0000202479.00623.86 [DOI] [PubMed] [Google Scholar]
- 30. Wang X. The development of the scale women's health appraisal to address middle-aged women's menopausal symptoms. University of Miami; Coral Gables, FL; 2006. Available from: https://scholarship.miami.edu/esploro/outputs/doctoral/The-development-of-the-scale-Womens/991031447673202976 [Last accessed: July 31, 2023].
- 31. Gallicchio L, Schilling C, Miller SR, et al. Correlates of depressive symptoms among women undergoing the menopausal transition. J Psychosom Res 2007;63(3):263–268; doi: 10.1016/j.jpsychores.2007.02.003 [DOI] [PubMed] [Google Scholar]
- 32. Kornstein SG, Young EA, Harvey AT, et al. The influence of menopause status and postmenopausal use of hormone therapy on presentation of major depression in women. Menopause 2010;17(4):828–839; doi: 10.1097/gme.0b013e3181d770a8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Seritan AL, Iosif AM, Park JH, et al. Self-reported anxiety, depressive, and vasomotor symptoms: a study of perimenopausal women presenting to a specialized midlife assessment center. Menopause 2010;17(2):410–415; doi: 10.1097/gme.0b013e3181bf5a62 [DOI] [PubMed] [Google Scholar]
- 34. Richard A, Rohrmann S, Mohler-Kuo M, et al. Urinary phytoestrogens and depression in perimenopausal US women: NHANES 2005–2008. J Affect Disord 2014;156:200–205; doi: 10.1016/j.jad.2013.12.029 [DOI] [PubMed] [Google Scholar]
- 35. Im EO, Ham OK, Chee E, et al. Physical activity and depressive symptoms in four ethnic groups of midlife women. West J Nurs Res 2015;37(6):746–766; doi: 10.1177/0193945914537123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Im EO, Yang YL, Liu J, et al. The association of depressive symptoms to sleep-related symptoms during menopausal transition: Racial/ethnic differences. Menopause 2020;27(11):1315–1321; doi: 10.1097/gme.0000000000001611 [DOI] [PubMed] [Google Scholar]
- 37. De Mello A, Chavez A, Mukarram M, et al. Menopausal symptoms in the Southwest United States: A cross-sectional survey of women from areas with different socioeconomic resources. Maturitas 2021;154:7–12; doi: 10.1016/j.maturitas.2021.08.110 [DOI] [PubMed] [Google Scholar]
- 38. Ji X, Singleterry S, Kulikova A, et al. Association of menopause symptoms with depressive symptom severity in a diverse community-based sample. Maturitas 2021;143(0):78–80; doi: 10.1016/j.maturitas.2020.09.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Freeman EW, Sammel MD, Lin H, et al. The role of anxiety and hormonal changes in menopausal hot flashes. Menopause 2005;12(3):258–266; doi: 10.1097/01.gme.0000142440.49698.b7 [DOI] [PubMed] [Google Scholar]
- 40. Kravitz HM, Janssen I, Lotrich FE, et al. Sex steroid hormone gene polymorphisms and depressive symptoms in women at midlife. Am J Med 2006;119(9 Suppl 1):S87–S93; doi: 10.1016/j.amjmed.2006.07.010 [DOI] [PubMed] [Google Scholar]
- 41. Bromberger JT, Matthews KA, Schott LL, et al. Depressive symptoms during the menopausal transition: The Study of Women's Health Across the Nation (SWAN). J Affect Disord 2007;103(1–3):267–272; doi: 10.1016/j.jad.2007.01.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Freeman EW, Sammel MD, Lin H, et al. Symptoms associated with menopausal transition and reproductive hormones in midlife women. Obstet Gynecol 2007;110(2 I):230–240; doi: 10.1097/01.AOG.0000270153.59102.40 [DOI] [PubMed] [Google Scholar]
- 43. Matthews KA, Schott LL, Bromberger J, et al. Associations between depressive symptoms and inflammatory/hemostatic markers in women during the menopausal transition. Psychosom Med 2007;69(2):124–130; doi: 10.1097/01.psy.0000256574.30389.1b [DOI] [PubMed] [Google Scholar]
- 44. Goldbacher EM. Depression and the metabolic syndrome in middle-aged women: A longitudinal investigation. University of Pittsburgh; Pittsburgh; 2007. Available from: https://d-scholarship.pitt.edu/8996/[Last accessed: July 31, 2023].
- 45. Nelson DB, Sammel MD, Freeman EW, et al. Effect of physical activity on menopausal symptoms among urban women. Med Sci Sports Exerc 2008;40(1):50–58; doi: 10.1249/mss.0b013e318159d1e4 [DOI] [PubMed] [Google Scholar]
- 46. Pien GW, Sammel MD, Freeman EW, et al. Predictors of sleep quality in women in the menopausal transition. Sleep 2008;31(7):991–999. [PMC free article] [PubMed] [Google Scholar]
- 47. Thurston RC, Bromberger J, Chang Y, et al. Childhood abuse or neglect is associated with increased vasomotor symptom reporting among midlife women. Menopause 2008;15(1):16–22. [PMC free article] [PubMed] [Google Scholar]
- 48. Thurston RC, Bromberger JT, Joffe H, et al. Beyond frequency: Who is most bothered by vasomotor symptoms? Menopause 2008;15(5):841–847; doi: 10.1097/gme.0b013e318168f09b [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Avis NE, Colvin A, Bromberger JT, et al. Change in health-related quality of life over the menopausal transition in a multiethnic cohort of middle-aged women: Study of Women's Health Across the Nation. Menopause 2009;16(5):860–869; doi: 10.1097/gme.0b013e3181a3cdaf [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Bromberger JT, Kravitz HM, Matthews K, et al. Predictors of first lifetime episodes of major depression in midlife women. Psychol Med 2009;39(1):55–64; doi: 10.1017/s0033291708003218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Bromberger JT, Schott LL, Kravitz HM, et al. Longitudinal change in reproductive hormones and depressive symptoms across the menopausal transition: Results from the Study of Women's Health Across the Nation (SWAN). Arch Gen Psychiatry 2010;67(6):598–607; doi: 10.1001/archgenpsychiatry.2010.55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Green R, Santoro NF, McGinn AP, et al. The relationship between psychosocial status, acculturation and country of origin in mid-life Hispanic women: Data from the Study of Women's Health Across the Nation (SWAN). Climacteric 2010;13(6):534–543; doi: 10.3109/13697131003592713 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Greendale GA, Wight RG, Huang MH, et al. Menopause-associated symptoms and cognitive performance: Results from the Study of Women's Health Across the Nation. Am J Epidemiol 2010;171(11):1214–1224; doi: 10.1093/aje/kwq067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Matthews KA, Schott LL, Bromberger JT, et al. Are there bi-directional associations between depressive symptoms and C-reactive protein in mid-life women? Brain Behav Immun 2010;24(1):96–101; doi: 10.1016/j.bbi.2009.08.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Rebbeck TR, Su HI, Sammel MD, et al. Effect of hormone metabolism genotypes on steroid hormone levels and menopausal symptoms in a prospective population-based cohort of women experiencing the menopausal transition. Menopause 2010;17(5):1026–1034; doi: 10.1097/gme.0b013e3181db61a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Schnatz PF, Whitehurst SK, O'Sullivan DM. Sexual dysfunction, depression, and anxiety among patients of an inner-city menopause clinic. J Womens Health (Larchmt) 2010;19(10):1843–1849; doi: 10.1089/jwh.2009.1800 [DOI] [PubMed] [Google Scholar]
- 57. Bromberger JT, Kravitz HM, Chang YF, et al. Major depression during and after the menopausal transition: Study of Women's Health Across the Nation (SWAN). Psychol Med 2011;41(9):1879–1888; doi: 10.1017/s003329171100016x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Kravitz HM, Avery E, Sowers M, et al. Relationships between menopausal and mood symptoms and EEG sleep measures in a multi-ethnic sample of middle-aged women: The SWAN sleep study. Sleep 2011;34(9):1221–1232; doi: 10.5665/sleep.1244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Morrison MF, Freeman EW, Lin H, et al. Higher DHEA-S (dehydroepiandrosterone sulfate) levels are associated with depressive symptoms during the menopausal transition: Results from the PENN Ovarian Aging Study. Arch Womens Ment Health 2011;14(5):375–382; doi: 10.1007/s00737-011-0231-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Bromberger JT, Schott LL, Matthews KA, et al. Association of past and recent major depression and menstrual characteristics in midlife: Study of Women's Health Across the Nation. Menopause 2012;19(9):959–966; doi: 10.1097/gme.0b013e318248f2d5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Gibson CJ, Joffe H, Bromberger JT, et al. Mood symptoms after natural menopause and hysterectomy with and without bilateral oophorectomy among women in midlife. Obstet Gynecol 2012;119(5):935–941; doi: 10.1097/AOG.0b013e31824f9c14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Bromberger JT, Kravitz HM, Chang Y, et al. Does risk for anxiety increase during the menopausal transition? Study of Women's Health Across the Nation. Menopause 2013;20(5):488–495; doi: 10.1097/gme.0b013e3182730599 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Appelhans BM, Segawa E, Janssen I, et al. Employment status, depressive symptoms, and waist circumference change in midlife women: The Study of Women's Health Across the Nation (SWAN). Ann Epidemiol 2014;24(3):187–192; doi: 10.1016/j.annepidem.2013.12.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Colvin A, Richardson GA, Cyranowski JM, et al. Does family history of depression predict major depression in midlife women? Study of Women's Health Across the Nation Mental Health Study (SWAN MHS). Arch Womens Ment Health 2014;17(4):269–278; doi: 10.1007/s00737-014-0433-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Kravitz HM, Schott LL, Joffe H, et al. Do anxiety symptoms predict major depressive disorder in midlife women? The study of Women's Health Across the Nation (SWAN) Mental Health Study (MHS). Psychol Med 2014;44(12):2593–2602; doi: 10.1017/s0033291714000075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Avis NE, Crawford SL, Greendale G, et al. Duration of menopausal vasomotor symptoms over the menopause transition. JAMA Intern Med 2015;175(4):531–539; doi: 10.1001/jamainternmed.2014.8063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Dugan SA, Bromberger JT, Segawa E, et al. Association between physical activity and depressive symptoms: Midlife women in SWAN. Med Sci Sports Exerc 2015;47(2):335–342; doi: 10.1249/mss.0000000000000407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Prairie BA, Wisniewski SR, Luther J, et al. Symptoms of depressed mood, disturbed sleep, and sexual problems in midlife women: Cross-sectional data from the Study of Women's Health Across the Nation. J Womens Health (Larchmt) 2015;24(2):119–126; doi: 10.1089/jwh.2014.4798 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Freeman EW, Sammel MD. Methods in a longitudinal cohort study of late reproductive age women: The Penn Ovarian Aging Study (POAS). Womens Midlife Health 2016;2:1; doi: 10.1186/s40695-016-0014-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Colvin A, Richardson GA, Cyranowski JM, et al. The role of family history of depression and the menopausal transition in the development of major depression in midlife women: Study of Women's Health Across the Nation Mental Health Study (SWAN MHS). Depress Anxiety 2017;34(9):826–835; doi: 10.1002/da.22651 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Marsh WK, Bromberger JT, Crawford SL, et al. Lifelong estradiol exposure and risk of depressive symptoms during the transition to menopause and postmenopause. Menopause 2017;24(12):1351–1359; doi: 10.1097/gme.0000000000000929 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Bromberger JT, Schott LL, Avis NE, et al. Psychosocial and health-related risk factors for depressive symptom trajectories among midlife women over 15years: Study of Women's Health Across the Nation (SWAN). Psychol Med 2019;49(2):250–259; doi: 10.1017/s0033291718000703 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Gibson CJ, Huang AJ, McCaw B, et al. Associations of intimate partner violence, sexual assault, and posttraumatic stress disorder with menopause symptoms among midlife and older women. JAMA Intern Med 2019;179(1):80–87; doi: 10.1001/jamainternmed.2018.5233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Jones HJ, Minarik PA, Gilliss CL, et al. Depressive symptoms associated with physical health problems in midlife women: A longitudinal study. J Affect Disord 2020;263(0):301–309; doi: 10.1016/j.jad.2019.11.166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. de Wit AE, Giltay EJ, de Boer MK, et al. Predictors of irritability symptoms in mildly depressed perimenopausal women. Psychoneuroendocrinology 2021;126(105128; doi: 10.1016/j.psyneuen.2021.105128 [DOI] [PubMed] [Google Scholar]
- 76. Gordon JL, Rubinow DR, Eisenlohr-Moul TA, et al. Efficacy of transdermal estradiol and micronized progesterone in the prevention of depressive symptoms in the menopause transition: A randomized clinical trial. JAMA Psychiat 2018;75(2):149–157; doi: 10.1001/jamapsychiatry.2017.3998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Cortés YI, Marginean V, Berry D. Physiologic and psychosocial changes of the menopause transition in US Latinas: A narrative review. Climacteric 2021;24(3):214–228; doi: 10.1080/13697137.2020.1834529 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Maki PM, Kornstein SG, Joffe H, et al. Guidelines for the evaluation and treatment of perimenopausal depression: Summary and recommendations. Menopause 2018;25(10):1069–1085; doi: 10.1097/gme.0000000000001174 [DOI] [PubMed] [Google Scholar]
- 79. Schmidt PJ, Nieman L, Danaceau MA, et al. Estrogen replacement in perimenopause-related depression: A preliminary report. Am J Obstet Gynecol 2000;183(2):414–420; doi: 10.1067/mob.2000.106004 [DOI] [PubMed] [Google Scholar]
- 80. Soares CN, Almeida OP, Joffe H, et al. Efficacy of estradiol for the treatment of depressive disorders in perimenopausal women: A double-blind, randomized, placebo-controlled trial. Arch Gen Psychiat 2001;58(6):529–534; doi: 10.1001/archpsyc.58.6.529 [DOI] [PubMed] [Google Scholar]
- 81. Garnett MF, Curtin SC, Stone DM. Suicide mortality in the United States, 2000–2020. NCHS Data Brief 2022;433(0):1–8; doi: 10.15620/cdc:114217 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.