Abstract
Introduction:
Performing endoscopic retrograde cholangiopancreatography (ERCP) in duodenal switch (DS) patients is challenging given their surgically altered anatomy. There have been very few reported cases of trans enteric rendezvous ERCP to relieve biliary obstruction in DS patients. More specifically, there has not been any reported cases of this procedure being performed in loop DS, also known as SADI (single anastomosis duodeno-ileostomy) or SIPS (stomach intestinal pylorus sparing procedure).
Case Description:
This case reports describes a 50-year-old male with prior loop DS who presented with gallstone pancreatitis. He underwent a laparoscopic cholecystectomy with positive intraoperative cholangiogram requiring the need for trans enteric rendezvous ERCP.
Discussion:
Although never reported, trans enteric rendezvous ERCP is a feasible approach in relieving biliary obstruction in patients with loop DS anatomy.
Keywords: Bariatric surgery, Choledocholithiasis, Gallstone pancreatitis, Loop duodenal switch, Rendezvous technique, SADI, Single anastomosis duodeno-ileostomy, SIPS, Stomach intestinal pylorus sparing procedure, Trans enteric endoscopic retrograde cholangiopancreatography
INTRODUCTION
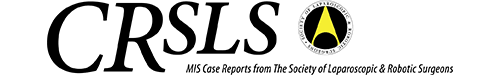
In current clinical practice, endoscopic retrograde cholangiopancreatography (ERCP) is considered the gold standard modality for relieving biliary obstruction. However, in patients with surgically altered anatomy, e.g., Whipple, Billroth II, Roux-en-Y hepaticojejunostomy, Roux-en-Y gastric bypass (RYGB), and duodenal switch (DS), the typical transoral approach of ERCP is not feasible. Few nonconventional approaches of ERCP have been documented in literature to tackle these complex patients. Endoscopic ultrasound (EUS)-directed ERCP is one nonconventional approach reported to be used patients with surgically altered anatomy.1 This is a two-staged approach that involves EUS guidance to create either a trans gastric (RYGB patients) or entero enteric fistula (non-RYGB patients) followed by interval ERCP for definitive biliary decompression. Laparoscopic-assisted trans gastric ERCP is another nonconventional approach reported to be used specifically in RYGB patients.2 A laparoscopic gastrotomy is created in the bypassed stomach ERCP is then carried out through a previously made laparoscopic port site and the gastrotomy is immediately closed after with sutures or staples. The most rarely documented nonconventional approach is the laparoscopic-assisted trans enteric rendezvous ERCP used for DS patients. This method has only been documented in classical DS, also known as biliopancreatic diversion, patients. Loop DS, also known as SADI (single anastomosis duodeno-ileostomy) or SIPS (stomach intestinal pylorus sparing procedure), is a newer technique that was first introduced in 2007.5 The purpose of this technique was to minimize the malabsorptive risks of classical DS by eliminating the alimentary limb and lengthening the common channel to 200–300 cm (Figure 1).
Figure 1.
Anatomy of classical DS (left) versus loop DS (right).
CASE PRESENTATION
A 50-year-old male with history of prior lap band surgery in 2004 with subsequent revision to loop DS in September 2022 presented with epigastric pain with radiation to the back for one day. Overall, he had lost 88 pounds since his loop DS surgery. The pain began after eating and was associated with bloating and nausea. Labs were significant for leukocytosis (white blood cell 13.3 K/μL) and elevated lipase (>5000 U/L). Aspartate transaminase (AST), alanine transaminase (ALT), alkaline phosphatase, and total bilirubin were within normal limits. Abdominal ultrasound revealed cholelithiasis with gallbladder wall thickening. Common bile duct (CBD) was measured to be 6 mm. Computed tomography (CT) abdomen and pelvis revealed peripancreatic fat stranding and inflammation with diffuse pancreatic parenchymal edema and swelling suggestive of acute pancreatitis.
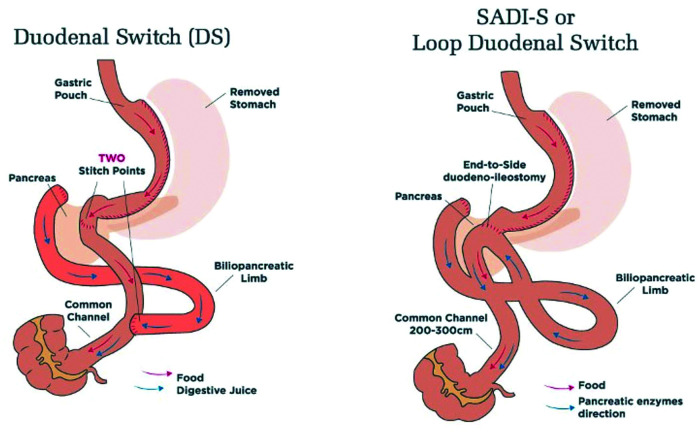
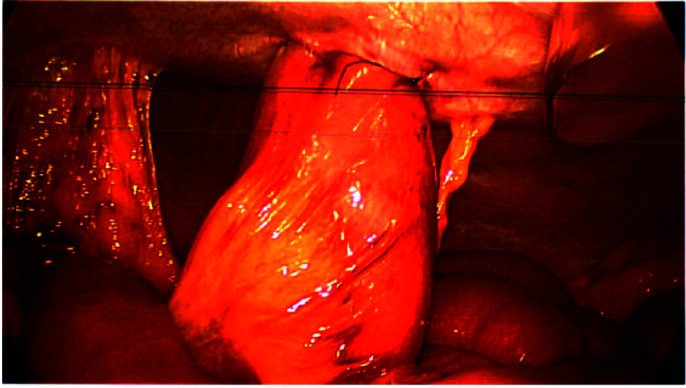
After improvement of pancreatitis symptoms and lipase, he was taken to the operating room for laparoscopic cholecystectomy and intraoperative cholangiogram (IOC). Laparoscopic cholecystectomy proceeded in standard fashion and IOC revealed a filling defect in the distal CBD. Saline flushing and glucagon injection were not successful. Due to unavailability of a choledochoscope, gastroenterology (GI) was consulted at this time for intraoperative ERCP. Multiple attempts to pass a guidewire through the cystic duct into the duodenum to assist with ERCP guidance but was unsuccessful. An enterotomy with a 2-0 PDS purse string suture was made approximately 30 cm distal to the ligament of Treitz (LT). Using the purse string suture, the bowel loop was brought up to the abdominal wall and a 15 mm port was advanced into the jejunum (Figure 2). The purse string suture was tied around the port for security. GI was able to advance the side viewing endoscope retrograde through the jejunum to the second portion of the duodenum. The papilla was identified and noted to be inverted. Multiple attempts at biliary cannulation were attempted but unsuccessful. The ERCP was aborted and the enterotomy was closed with running 3-0 V loc suture. Interventional radiology (IR) placed a percutaneous transhepatic cholangiography (PTC)-assisted 8.5 French Cook internal/external biliary drain across the CBD occlusion and into the duodenum. This drain was then used the following day for repeat trans enteric ERCP. A fresh enterotomy was made 20 cm distal to the LT. GI proceeded with trans enteric ERCP where the papilla was identified and the biliary drain was seen emanating from the ampulla. A 0.035 450 cm Jagwire was advanced through the PTC catheter into the duodenum. The wire was grasped with a snare and removed through the endoscope. A biliary sphincterotome was loaded over the wire and advanced into the biliary duct (Figure 3). The CBD was successfully cleared with multiple balloon sweeps. The IR placed biliary drain was then removed and enterotomy was closed via previously described technique. Patient did well postoperatively and was discharged after two days.
Figure 2.
Bowel loop brought up to abdominal wall with purse string suture.
Figure 3.
Port placement.
DISCUSSION
There are not many documented cases of trans enteric rendezvous ERCP. Furthermore, there are no documented cases of this procedure being performed in loop DS patients with PTC assistance. The most challenging part of this procedure is accessing the papilla from a retrograde approach, which we demonstrate is nearly impossible to do without wire guidance, especially if its inverted or has any abnormal orientation. One factor to consider in the future would be the preoperative placement of PTC guidewires in classical and loop DS patients presenting with suspected choledocholithiasis. This did not apply to our patient because he had normal AST/ALT, total bilirubin, and CBD size. Another factor to consider in the future is the location of the enterotomy in relation to the LT. Our case report details enterotomy sites at both 20 and 30 cm distal to the LT. Previous case reports used 40 cm. This is just something to keep in mind as more trans enteric rendezvous ERCPs are performed, and outcomes can be better assessed.
The first documented case of laparoscopic-assisted trans enteric rendezvous ERCP was published in Italy in 2007.3 This was a case of choledocholithiasis in a patient with classical DS anatomy. This approach involved making a laparoscopic enterotomy 40 cm distal to the LT, bringing the jejunum to the abdominal wall using the purse-string technique, and passing the duodenoscope through the jejunum in retrograde fashion. A guidewire was placed through the cystic duct via a tiny laparoscopic incision and advanced through the papilla under direct vision. This guidewire was then used by GI to cannulate the CBD. Following successful clearance of the CBD, cholecystectomy was performed and the enterotomy was closed with staples. The patient’s postoperative course was uneventful. The second and third documented cases were published as a combined case series in Brazil in 2017.4 These cases were also for choledocholithiasis in patients with classical DS anatomy and they used the same technique as mentioned previously. In contrast to the previous case reports, we present the first case report of a successful laparoscopic-assisted trans enteric rendezvous ERCP in a patient with loop DS anatomy.
In conclusion, performing a laparoscopic-assisted trans enteric ERCP is a feasible approach in relieving biliary obstruction in patients with loop DS anatomy. It allows for avoidance of more invasive procedures such as CBD exploration. Furthermore, using a PTC or transcystic guidewire is an appropriate adjunct for successfully cannulating the CBD during these procedures. However, the caveat is that it requires performance at institutions with skilled laparoscopic surgeons and endoscopists who can maneuver through the unique anatomy.
Footnotes
Disclosure of conflicts of interest and sources of financial support: There are no conflicts of interest or sources of financial support to disclose.
Contributor Information
Sarah Lee, Department of Surgery, Sutter Roseville Medical Center, Roseville, California, USA. (Dr Lee).
Subhash R. Patil, Department of Bariatric Surgery, Sutter Roseville Medical Center, Roseville, California, USA. (Drs Patil and Ganga).
Shilpa Lingala, Department of Gastroenterology, Sutter Roseville Medical Center, Roseville, California, USA. (Dr Lingala).
Benjamin G. Coombs, Department of Interventional Radiology, Sutter Roseville Medical Center, Roseville, California, USA. (Dr Coombs).
Rama R. Ganga, Department of Bariatric Surgery, Sutter Roseville Medical Center, Roseville, California, USA. (Drs Patil and Ganga).
References:
- 1.Ichkhanian Y, Yang J, James TW, et al. EUS-directed transenteric ERCP in non-Roux-en-Y gastric bypass surgical anatomy patients (with video). Gastrointest Endosc. 2020;91(5):1188–1194.e2. [DOI] [PubMed] [Google Scholar]
- 2.De Oliveira VL, De Moura DTH, Do Monte JE, et al. Laparoscopic-assisted endoscopic retrograde cholangiopancreatography (ERCP) versus endoscopic ultrasound-directed transgastric ERCP in patients with Roux-en-Y gastric bypass: a systematic review and meta-analysis. Cureus. 2022;14(10):e30196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mutignani M, Marchese M, Tringali A, et al. Laparoscopy-assisted ERCP after biliopancreatic diversion. Obes Surg. 2007;17(2):251–254. [DOI] [PubMed] [Google Scholar]
- 4.Marchesini JCD, Noda RW, Haida VM, et al. Transenteric ERCP for treatment of choledocholithiasis after duodenal switch. Surg Laparosc Endosc Percutan Tech. 2017;27(3):e28–e30. [DOI] [PubMed] [Google Scholar]
- 5.Sánchez-Pernaute A, Rubio Herrera MA, Pérez-Aguirre E, et al. Proximal duodenal-ileal end-to-side bypass with sleeve gastrectomy: proposed technique. Obes Surg. 2007;17(12):1614–1618. [DOI] [PubMed] [Google Scholar]