Abstract
Stroke is a significant public health problem, with non-valvular atrial fibrillation (NVAF) being one of its main causes. This cardiovascular arrhythmia predisposes to the production of intracardiac thrombi, mostly formed in the left atrial appendage (LAA). When there are contraindications to treatment with oral anticoagulants, another therapeutic option to reduce the possibility of thrombus formation in the LAA is the implantation of an occlusion device by cardiac catheterization. The effectiveness of LAA occlusion is dependent on accurate preprocedural device sizing and proper device positioning at the LAA ostium, to ensure sufficient device anchoring and avoid peri-device leaks. Additive manufacturing, commonly known as three-dimensional printing (3DP), of LAA models is beginning to emerge in the scientific literature to address these challenges through procedural simulation. This review aims at clarifying the impact of 3DP on preprocedural planning of LAA occlusion, specifically in the training of cardiac surgeons and in the assessment of the perfect adjustment between the LAA and the biomedical implant.
Keywords: stroke, left atrial appendage, occlusion device, additive manufacturing
Introduction
Stroke is a significant public health problem. According to data from the Portuguese Stroke Society, Portugal has the highest death rate in Western Europe, particularly among people under 65 years old. Non-valvular atrial fibrillation (NVAF), an atrial arrhythmia that predisposes to the formation of intracardiac thrombi, is one of the primary causes of strokes. Most thrombi in this context form in the left atrial appendage (LAA).
Oral anticoagulant (OAC) medications are highly effective at reducing the incidence of stroke; however, they also carry a risk of bleeding. In the most recent clinical trials, one-fifth of the patients had to stop OAC treatment due to adverse side effects. In patients with contraindications to the first-line treatment with OACs, minimally invasive implantation of an occlusion device in the LAA is one of the therapeutic options to lower the risk of thrombus formation.
To address the complication risk with improper device sizing/positioning, 3DP of LAA models have recently emerged in the literature. In this context, the purpose of the present review is to illustrate the impact of 3DP on the preprocedural planning of LAA occlusion. Nonetheless, it should be mentioned that, even though this procedure is already performed at several reference hospitals, there is a risk of complications, some of which may require emergent cardiac surgery. The effectiveness of the procedure could be diminished by challenges such as peri-implant leakage, device-related thrombosis (DRT), and device embolization.1
It should also be highlighted that medical error is one of the leading causes of mortality; therefore, providing health professionals with technology that enables them to be more accurate in the assessment/treatment of various diseases is a remarkable benefit to medicine.
Stroke, one of the most common cardiovascular diseases, is a sudden event that results from a blockage that limits blood flow to the brain.2,3 Literature reports that 90% of blood clots in non-valve atrial fibrillation (NVAF) develop at the level of the LAA.4 Increased thrombogenicity in the LAA can be attributed to its narrow entrance orifice. When this is combined with the structure of the LAA, there is a predisposition to blood stasis and thrombus formation.5
The substantial morbidity and mortality associated with NVAF make stroke prevention a priority for physicians, patients, their families, and society in general. For decades, warfarin, an OAC treatment, has been the leading option for preventing stroke in patients with NVAF. In recent years, the introduction of non-vitamin K antagonist oral anticoagulants (NOACs) and the evolution of minimally invasive mechanical options for left atrial appendage occlusion (LAAO) have introduced therapeutic alternatives for many patients who are ineligible for OAC therapy or who have failed optimal OAC treatment.
As a result of the aforementioned therapeutic limitations and the severity of NVAF-related systemic embolic events, there is a great deal of interest in developing novel therapeutic strategies, namely the concept of LAA exclusion as a method of reducing stroke and other embolic complications in patients with NVAF. Figure 1 schematically represents the available strategies for stroke prevention in patients with atrial fibrillation.
FIG. 1.
Available strategies for stroke prevention in patients with atrial fibrillation.
Among all the LAA exclusion methods, in this study only the percutaneous endocardial approach will be addressed.
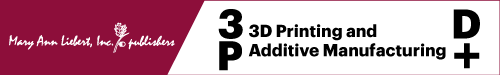
Numerous devices have been tested in the past decade and some of those are currently available for clinical use.6 At the moment, the most common percutaneous LAAO devices available are Watchman (Boston Scientific, Natick, MA), Watchman FLX (Boston Scientific), and Amplatzer Amulet (Abbott Laboratories, Chicago, IL), Figure 2 shows an example of Watchman, Watchman FLX, and Amplatzer Amullet devices.7,8
FIG. 2.
An example of (A) Watchman and (B) Watchman FLX (C) Amplatzer Amullet devices.9
The interaction between the LAAO device, the LAA's anatomical features, particularly the variety in the LAA ostium and body morphology, and the tissue properties of the underlying atrial tissue may likely determine the incidence of peri-device leakage (PDL).10 A mismatch in terms of geometry can result in an incomplete LAAO and a greater chance of residual PDL.
Even though it is reported in several studies that there is a potential for DRT to occur after the implantation of LAAO devices, there is still a lack of information regarding the incidence and ability to predict it. Current investigations have revealed that DRT occurs in 3% to 4% of patients following LAAO, associated with a significantly increased risk of ischemic events.11–13
Patient-Specific Procedural Planning
Personalized medicine is an innovative method of providing medical care in which patients' treatments are personalized to meet their individual requirements.14 It has been demonstrated that using a customized strategy leads to improved patient outcomes, with customized treatments often demonstrating more effective responses and higher safety margins than conventional, one-size-fits-all solutions. It is necessary to have a complete understanding of cardiac anatomy and physiology to perform structural heart procedures such as LAAO.
Due to the diverse LAA patient anatomy, it is highly recommendable to use the personalized medicine approach, in which each procedure is carefully tailored for each patient.15 Applying methods such as computational fluid dynamics (CFD) and 3DP has made it feasible to make significant advancements in customized medicine, notably in structural heart disease.16 The CFD can simulate the dynamic characteristics of cardiac pathophysiology, and 3DP can reduce the early operator learning curve for new technology adaption.17–20 A vision flowchart of a personalized approach for LAAO is displayed in Figure 3.
FIG. 3.
Design, production, validation, and implantation of a left atrial appendage occlusion device customized for each patient.1
The percutaneous LAA occlusion devices are minimally invasive endocardial devices that have shown non-inferior effectiveness in stroke prevention with a marked reduction in bleeding risk. A comprehensive pre-implantation assessment of the LAA anatomy is critical for procedural success and treatment outcomes in LAAO. For that, it is important to evaluate all imaging plans to obtain several parameters, including the diameter of the landing zone, depth, the orientation of the main anchoring lobe, and the number and origin of additional lobes, all useful to select LAAO device type and size.
The 3D acquisition technology enables virtual reality reconstruction of LAA geometry and simulation of virtual implantation of percutaneous devices.21 However, this method demonstrates low accuracy in predicting the interaction between the LAAO device and its surroundings during and after implantation.22
Imaging-based computational modeling
Numerous cardiac imaging techniques are currently used to assess the anatomy and size of the LAA, including 2D transesophageal echocardiography (TEE), 3D TEE, and computerized tomography (CT).
The TEE remains the gold standard for intraoperative preprocedural assessment, due to its high-definition features of the right and left atria, atrial septum, and LAA anatomy.23 The TEE has a high degree of sensitivity (92%) regarding thrombus detection. While 2D TEE offers higher-resolution images due to a higher frame rate, 3D TEE helps to overcome some of the drawbacks of 2D imaging, like insufficient imaging planes, to enable a more thorough evaluation of the LAA.
In addition, 3D TEE allows for improved separation and differentiation between nearby structures, as well as a more exhaustive study of the LAA, its complex morphology, and the surrounding structures.24–26 As a result of recent developments in percutaneous device therapy for LAA closure, 3D TEE has emerged as a crucial technique for guiding device delivery into the LAA.27
A computer tomography (CT) scan is a non-invasive medical imaging technique used to produce detailed images of sliced cross-sections of internal structures within the body.28,29 Multi-slice cardiac computed tomography, a variation of CT, is a useful examination for the procedural planning of either a percutaneous or surgical LAAO procedure. CT scan not only enables an accurate study of the LAA and the structures that surround it, but it also allows the selection of the most appropriate device for the procedure.
When it comes to determining whether or not thrombotic formations are present, cardiac CT has a high sensitivity of 96%.30 After the cardiac CT images have been collected, post-processing is conducted, which involves carrying out multi-planar reconstruction of axial data. The final benefit of using 3D reconstruction is that it allows for complete visualization of the appendage. In addition, the multi-planar reconstruction enables to accurately select the correct size of the device.31
Computational models based on virtual and physical 3D CT imaging have been employed to simulate device implementation into patient-specific cardiac anatomy, predict the ideal placement strategy, and estimate the optimal device dimensions to lower the risk of PDL.
Additive manufacturing
Three-dimensional printing has emerged as a new method for visualizing image models, and its application in the medical field is also growing.32 According to the American Society for Testing and Materials (ASTM) 52900:2021 standard, 3DP refers to a group of seven processes that employs digital design data to manufacture a component layer upon layer.33,34 It has acquired prominence in the media and captivated the public, as well as numerous researchers in several fields.
Due to recent interest, AM is continuously being adapted to a broader range of applications, including automotive, aerospace, engineering, medicine, biological systems, and food supply chains.35 The additive approach is an attractive concept that can produce complex structures using a wide variety of materials. Therefore, it is not surprising that there has been a substantial amount of recent interest and investment in AM technologies.
The decreasing cost of programmable controllers, lasers, inkjet printing, and computer-aided design (CAD) software has revolutionized the design process, enabling anybody to use, think with, and innovate with these technologies.36 Consumers and industries that rely on low-to-moderate fidelity prototypes during the early stages of product design have been the primary market drivers for such systems. Several startups are developing novel and inexpensive 3D printers for thermoplastics. The 3D printing technologies are simple and almost entirely computer controlled. Future research on non-layer-based technologies and tool path planning may help increase AM possibilities further.37,38
The AM processes use a layer-by-layer approach to build up physical parts and products from a 3D CAD model with the assistance of a computer-aided manufacturing (CAM) system. In the first phase, a 3D computer model is created using 3D CAD design, 3D scanning, or feasible technology. Subsequently occurs the slicing stage, where CAM computer software is used to acquire a model, slice it, and determine the printing path.
This phase includes, if needed, the addition of support to maintain stability and integrity during the printing process. It should be noted that 3DP equipment prints the model using the print path set by the computer numerical control algorithms. The post-processing, which comes last in AM, occurs after the print process is complete. It usually includes removing the support structures or performing other necessary operations to achieve the best net-shape results in relation to the initial 3D model.34,39 Figure 4 shows the 3DP workflow.
FIG. 4.
3DP process workflow. 3DP, three-dimensional printing.
A brief description of the seven processes in AM, according to ASTM 52900:2021, is given.40
Powder Bed Fusion (PBF). Powder materials are selectively consolidated using a thermal energy, in most cases a laser or electron beam. Selective laser sintering (SLS), electron beam melting (EBM), and selective laser melting (SLM) fall into this category of AM processes.41–43
Binder Jetting. Thin layers of powder ink are bonded together using liquid bonding agent (organic and inorganic material). The liquid bonding agent is selectively deposited to enable the selective fusion process.41–43
Material Jetting. Selective deposition of a photopolymer and initiator as build material (in the form of droplets) are deposited to form thin layers. These systems use machines with an inkjet head and include the popular polyjet machine.42,43
Sheet Lamination. Sheets of materials are stacked and laminated together to form an object. Laminated Object Manufacturing (LOM) and Ultrasound Additive Manufacturing (UAM) make up the prominent technologies in this AM category.41–43
Direct Energy Deposition (DED). A focused beam of thermal energy (e.g., in laser or plasma arc technologies) is used to fuse metal or metal-hybrid materials by controlled melting while being deposited. Some of the main technologies within this category are laser deposition (LD), laser engineered net shaping (LENS), and plasma arc melting.41–43
Vat Photopolymerization. A liquid photopolymer is placed inside a moveable vat, and selectively cured using an ultra-violet light-activated polymerization process. Digital light stereolithography (SLA) as well as processing (DLP) can be classed in this AM category.41–43
Material Extrusion. A filament form material heated and selectively extruded through a nozzle or orifice in tracks or beads combined in multi-layer models. Direct Ink Writing (DIW) and fused filament fabrication (FFF) fall into this category.41–43
As the primary benefits of AM, these techniques enable design freedom (for mass product customization), waste minimization (for lower costs), rapid prototyping and manufacturing (for faster market delivery), and a more efficient manufacturing and supply chain. Consequently, the growth of additive manufacturing has expanded prospects for enhanced design, production, and end-user applications.44
The use of additive manufacturing for LAAO procedure planning
As a result of the significant and variable angles between the landing zone and the ostium, the center of the disk may be positioned eccentrically, which could lead to incomplete closure. These conformational changes generated by complex interactions between lobes and landing zone ranges can only be evaluated via realistic preprocedural simulations based on 3D printing. Procedural safety may be improved by reducing the number of implantation attempts using this strategy. The clinical impact of 3D printing in the LAAO procedure is reported in the literature.8
The preprocedural planning of LAAO implantation is a critical step in ensuring the success of the procedure. One of the primary goals of preprocedural planning is to minimize the incidence of PDL 10. Several studies have been conducted in this area, and the results of these studies are presented in Table 1. Various phases of the preprocedural planning process must be addressed to minimize PDL.
Table 1.
Published Studies Concerning Preprocedural Planning of Left Atrial Appendage Occlusion Implantation
| Year | Author | Publication type | Preprocedural imaging | Device | AM technique | Sample size | Material | Reference |
|---|---|---|---|---|---|---|---|---|
| 2015 | Otton et al. | Case report | Multidetector CT | Watchman | PolyJet | 1 | Tango (Rubber-like material) | 62 |
| 2016 | Liu et al. | Prospective observational study | 3D TEE | Watchman | Stereolithography | 8 | Gelatin (Rubber-like material) | 63 |
| 2016 | Wang et al. | Case series | CT | Watchman | — | 53 | — | 64 |
| 2017 | Goitein et al. | Case series | Multidetector CT | Amplatzer Amulet + Watchman |
— | 29 | TangoPlus FLX930 | 65 |
| 2017 | Hell et al. | Prospective observational study | CT | Watchman | — | 22 | 52 | |
| 2017 | Li et al. | Randomized controlled trial | Cardiac CT | Watchman | Stereolithography | 42 | — | 66 |
| 2017 | Obasare et al. | Case report; Prospective |
CT | Watchman | Stereolithography | 1 | Latex resin | 67 |
| 2017 | Song et al. | Prospective observational study | 3D TEE | LAmbre | Material Jetting | 18 | Hard material of photosensitive resins + Tango Plus, Shore hardness 26–28 A |
68 |
| 2018 | Ciobotaru et al. | Observational study; Two consecutive cohorts: retrospective case-control and prospective double arm |
Multidetector CT | Amplatzer Amulet + Amplatzer cardiac plug (ACP) |
Stereolithography | 76 | Flexible photopolymer resin | 69 |
| 2018 | Eng et al. | Randomized trial | Multidetector CT | Watchman | — | 24 | — | 46 |
| 2019 | Conti et al. | Case-control | Cardiac CT | Amplatzer cardiac plug (ACP) | Form 2 Desktop printer vat-photopolymerization |
20 | — | 50 |
| 2019 | Hachulla et al. | Prospective observational study |
Multidetector CT | Amplatzer Amulet | — | 15 | TangoPlus FLX 930 | 70 |
| 2019 | Fan et al. | Case report; Two consecutive cohorts: retrospective case-control and prospective double arm |
3D TEE | Watchman | — | 1 | Silicon | 71 |
| 2022 | Hong et al. | Prospective observation study | Computed tomography angiography (CTA) | — | Fused filament fabrication + Stereolithography |
10 | TPU 95A filament + Flexa693 (photopolymer resin) |
72 |
One of the critical phases is medical image processing techniques, which involve capturing high-quality images to create CAD models. Accurate and precise images are necessary to ensure the precision of the digital model to mimic the real LAA properly. When it comes to advanced imaging techniques used in cardiology, three of the most commonly used are 3D Transesophageal Echocardiography (3D TEE), Computed Tomography (CT), and Multidetector CT (MDCT).
While each technique has unique advantages and disadvantages, all three are valuable tools for diagnosing and treating heart conditions.45–49 Three-dimensional TEE uses high-frequency sound waves to create a detailed 3D image of the heart's structures. One of its advantages is its ability to provide clear images of the heart's internal structures, such as the mitral valve and left atrium.
However, one of its disadvantages is the need for an invasive procedure, as it requires the insertion of a small probe into the patient's esophagus.26,45,46 CT imaging, on the other hand, uses X-rays to produce high-resolution images of the heart's anatomy. Its advantages also include its ability to produce quick results and detect changes in the heart's structure and function over time.
However, its main disadvantage is radiation exposure, which may be harmful over time.50–53 The MDCT is a variation of CT that provides even higher-resolution images of the heart's structures, making it helpful in detecting even the slightest abnormalities. Its ability to produce quick results is also a significant advantage, especially in emergency cases. However, like CT, MDCT also exposes patients to radiation.54 Ultimately, the choice of imaging technique depends on the patient's condition and the type of information needed to make an accurate diagnosis and treatment plan.
Another important aspect of preprocedural planning is selecting appropriate technology and materials to produce the LAA physical model using the previous CAD model. The use of AM technologies has revolutionized the implantation of occlusion devices since it enables the production of highly accurate personalized LAA physical models to plan and simulate the procedural accurately. PolyJet, Stereolithography (SLA), and FFF are the most used.
Each technology uses a different approach to create physical objects from digital designs. PolyJet is a high-precision 3D printing technology that uses liquid polymeric resins to create parts layer-by-layer. PolyJet printers can produce highly detailed and accurate parts with smooth surface finish, but they tend to be more expensive and have higher operating costs than other printing technologies.55,56
The SLA uses a laser to promote the photopolymerization of liquid resins into solid parts. The SLA printers can not only produce detailed, high-precision parts with excellent surface finish, but they also tend to be more expensive than other printing technologies, and the resins used are very few, can be expensive, and potentially hazardous.57–59 The FFF is a technology that extrudes melted thermoplastic filaments to create parts.
The FFF equipment are relatively inexpensive and easy to use, making them popular for hobbyists and small businesses. However, FFF-printed parts may have a different precision or surface finish level than those produced with other printing technologies.34,60,61 However, there is no direct relation between the mentioned technologies and the medical procedure.
Suitable materials are crucial for pre-procedural planning since the selected material must mimic the LAA biological tissue. The high level of detail and accuracy of the technologies can help to create highly accurate models of the LAA, allowing physicians to understand the anatomy better and plan the procedure accordingly.
Similarly, the ability to print models with multiple materials and colors could be useful in representing different tissues or structures within the LAA. Table 1 summarizes the published studies that included 3D printing in their preprocedural planning of LAAO implantation.
Otton et al. reported an LAA closure procedure of a 74-year-old man guided by individualized 3D-printed cardiac reconstruction. Before the surgery, the authors performed a multidetector CT of the left atrium and atrial appendage. Then, to simulate atrial geometry and mechanical properties, the CT imaging data were segmented (Mimics; Materialise) and 3DP in a rubber-like material (Tango Plus Material, Stratasys Objet Connex 500 printer, and Stratasys).
The model was implanted with 21, 24, and 27 mm Watchman devices and reimaged using clinical CT. The anatomical deformation of each Watchman device was determined by analyzing the 3D-printed LAA models with the Watchman devices. The proper device size (24 mm) was identified and implanted uneventfully using the patient-specific 3D-printed model and procedural simulation.62
Liu et al. studied, in eight patients, the clinical feasibility of producing 3D printing models of LAA by employing real-time 3D TEE data for the preoperative reference of LAA occlusion. The LAA models from the patients who underwent LAAO using a Watchman device were printed and then used for preoperative reference and procedural simulation.
The authors observed that all the eight device sizes predicted using the 3D printed models were in accordance with those placed during the actual procedure, one more than the prediction by pre-procedural 2D TEE. The 3D-printed models also allow forecasting technical challenges and the existence of peri-implant leaking.63
Wang et al. studied how 3D CT-guided procedural planning affects the early-operator learning curve for the Watchman device implantation in 53 patients. Based on CT studies showing the recommended implantation and device characteristics, preprocedural case plans were generated. The selected patients underwent LAAO with the Watchman device. The CT data from each patient were segmented and then printed.
To evaluate the device's size and obtain an approximation of the landing zone for its implantation, a Watchman device was implanted ex vivo into the 3D-printed LAA. Using CT imaging, the authors reported that device selection was completely accurate. If only 2D TEE measurements had been employed, 62.3% of the cases would require larger devices. According to the measurements from the 3D TEE, 52.3% of the cases also would require larger devices.64
The viability of multidetector computed tomography (MDCT)-based models on predicting the appropriate size of the device for LAA occlusion procedures was evaluated by Goitein et al. In total, 29 patients were enrolled in this trial. Before implantation, patients who underwent LAA occlusion were subjected to MDCT, which was utilized to create and print 3D LAA models. Three cardiologists examined the 3D models and manually adjusted them to determine the device's proper size.
The actual equipment placed during the procedure was compared with these predictions. Amplatzer and Watchman devices were implanted in 12 and 17, respectively, patients. As expected by all three physicians, two interventions were abandoned due to occlusion failure. For Amplatzer devices, there was a strong correlation between the 3D models and the implanted device, with a concordance correlation coefficient of 0.778 (p = 0.001).
However, the agreement was poor for Watchman devices, with a concordance correlation coefficient of 0.315 (p = 0.203). The calculated average intra-class correlation for the Amplatzer and Watchman devices was 0.915 and 0.816, respectively, indicating high agreement among the physicians. The authors concluded that the Amplatzer device's LAA-printed 3D model was correct for predicting the size of the LAA occlusion device but that the Watchman device's model was not.65
Hell et al. investigated (in 22 patients) whether the use of 3D-printed LAA models based on preprocedural computed tomography (CT) allows optimal device sizing. LAA closure, with the Watchman device, was performed on 22 patients (73 ± 8 years, 55% male) with atrial fibrillation that required anticoagulation at significant risk of bleeding.
The TEE and third-generation dual-source CT were used before the procedure to determine the size of the LAA. To simulate the process of device implantation, 3DP models' anatomy of the LAA was generated using the patient's CT scans. A CT scan of the 3D model with the implanted device was used to evaluate any device compression. Every patient experienced successful implantation.
According to TEE, the mean diameter of the LAA ostium was 22.4 mm, and according to CT, it was 25.3 mm (p = 0.014). In 21 out of 22 patients (or 95%), the device size predicted based on simulations of implantation in the 3D model was identical to the device size ultimately implanted. The TEE would have resulted in an undersized device in 10 out of 22 patients (45%).
The device compression obtained in the 3D CT model had a very close correlation with the compression that was determined on implantation (16.3% vs. 18.5%, r = 0.622, p = 0.003). Figure 5 displays the percentage success of device size prediction by TEE, CT, and 3D model with implanted device and agreement with the final implanted device size.52
FIG. 5.
Device size prediction by TEE, CT, and 3D model with implanted device and agreement with final implanted device size.52 TEE, transesophageal echocardiography.
The authors concluded that patient-specific CT-based 3DP models might assist in device selection and predicting device compression in interventional LAA closure.52
In the Li et al. study, 42 patients with atrial fibrillation (average age: 69.3 ± 7.8 years) were randomly assigned to two groups equally (3DP and control). The authors assessed the feasibility and effectiveness of the 3DP technology for LAA. The measurements of the LAA orifice size between the groups were taken using transesophageal echocardiography (TOE), LAA angiography, and cardiac computed tomography angiography.
The procedure times, radiographic exposure, contrast agent volumes, residual shunt, and costs were compared between the two groups. The LAA occlusion procedure performed on each patient using the Watchman device was successful. In the control group, occlusion devices were chosen following intraoperative TOE and LAA angiography measurements. In both patient groups, the occlusion was successful. The diameter of the occlusion devices utilized by the 3DP group and the control group was 27.6 ± 2.4 mm (21–33 mm) and 26.3 ± 3.4 mm (21–33 mm), respectively.
The TOE revealed that the compression ratios of the occlusion devices were 19.7% ± 0.8% and 19.3% ± 1.0%, respectively (p < 0.05). After occlusion, TOE revealed that three patients in the control group exhibited minor residual shunting (two patients with a 2-mm residual shunt and one with a 4-mm residual shunt). There was no residual shunt noticed in the 3DP group. For the 3DP and control groups, the procedure times, contrast agent volumes, and costs were 96.4 ± 12.5 versus 101.2 ± 13.6 min, 22.6 ± 3.0 versus 26.9 ± 6.2 mL, and 12,676.1 versus 12,088.6 dollars, respectively.
Radiographic exposure was considerably reduced in the 3DP group compared with the control group (561.4 ± 25.3 vs. 651.6 ± 32.1 mGy, p < 0.05). Neither group had no procedural problems (postoperative complications, DRT, or ischemic events). It is possible to guide LAA occlusion with 3DP technology. This method is useful for clinical use since it ensures the effectiveness of occlusion, improving clinical efficiency.66
Obasare et al. evaluated 24 patients (71 ± 11 years old, 42% female) who underwent Watchman device implantation. All had complete two-dimensional TEE. In addition, 14 patients underwent cardiac computed tomography (CCT) with 3DP to create a latex model of the LAA for pre-procedure planning. The authors reported that the device implantation was unsuccessful in two cases (one with and one without the 3D model).
The 3D model correlated perfectly with implanted device size (R2 = 1; p < 0.001), whereas TEE-predicted size showed an inferior correlation (R2 = 0.34; 95% CI: 0.23–0.98, p = 0.03). The LAA's patient-specific models enhance the precision of closure device sizing. Utilizing the printed model facilitated the rapid and straightforward identification of the optimal landing zone for the device.67
Song et al. studied 18 patients to evaluate the possibility of 3DP LAA models using data from 3D TEE, as well as the possible benefits of these models in treating LAA occlusions. In this study, there were a total of 18 patients who had transcatheter LAA occlusion, as well as pre-procedure 3D TEE and cardiac computed tomography. A 3D printer was used to manufacture two types of 3D models of the LAA, namely the complex chamber model and the flexible wall model.
In this case, the authors used the 3D chamber model to evaluate the LAA's morphological classification and lobe identification, and the 3D wall model was used to estimate the LAA's dimensions. In cases with complex LAA morphology, a simulation operative rehearsal was also carried out on the 3D models to comprehend the interactions between the device and the model.
In each patient, the three-dimensional TEE volumetric data of the LAA were successfully reprocessed and produced as three-dimensional LAA chamber models and three-dimensional LAA wall models. The level of concordance between the morphological classifications of the LAA based on 3D models and cardiac computed tomography was found to be 0.92 (p < 0.01).
The LAA ostium dimensions and depth measured using the 3D models did not significantly differ from those measured on the 3D TEE (p > 0.05). In the 3D models of the two challenging cases, a simulated occlusion was accomplished successfully and compared with the real-world procedure. This result may be interesting for the individualized planning of transcatheter LAA occlusion, because the echocardiographic 3DP approach is both practicable and accurate in reflecting the spatial anatomy of the LAA.68
The objective of the study performed by Ciobotaru et al. was to evaluate the predictive effectiveness of simulation based on 3D-printed models before LAAO for PDL and the impact on procedural outcomes in comparison to traditional imaging. Using flexible photopolymer resin, 76 patients who were submitted for LAAO with a double disk device underwent the development of a 3D-printed LA model. A retrospective implant simulation was carried out in Group 1 (55 patients), evaluating the value of 3D-printed models in predicting device sizing and risk of peri-device leaks. Without knowing the size of the implanted device, a simulation was conducted on the 3D-printed model after the LAAO procedure.
In Group 2 (21 patients), the authors studied the clinical value of a 3D-printed model simulation in addition to multimodality imaging regarding LAAO efficacy, fluoroscopy time, and the number of prostheses used per patient. However, due to contrast agent contraindications, two patients were excluded. Results indicated that, in Group 1, the incidence of PDL was 27% (15 patients), and there were 14 (25%) patients with an off-axis device location.
When using 3D simulation prospectively (group 2), the incidence of leaks was reduced compared with conventional imaging alone (5% vs. 27%, respectively). The LAAO double disk device size is optimized by patient-specific, versatile, and adaptable LA models manufactured on a 3D printer. The authors reported that this could potentially lower the duration of the treatment and the number of implants used per patient. Moreover, fluoroscopy time (19 min vs. 13.5 min, respectively) and total fluoroscopy dose (7291 vs. 1978 mGy·cm2, respectively) were also reduced.69
Eng et al. analyzed 24 patients who underwent LAAO procedure using either TEE or 3D-CT. The authors reported 100% and 92% procedure success for the 3D-CT and 2D-TEE cohorts, respectively. Using 3D-CT and 2D-TEE imaging techniques, the accuracy for the first device selection was 92% and 27% (p = 0.01), respectively. Case planning utilizing 3D-CT was considerably more effective in terms of device utilization (CT 1.33 ± 0.7 vs. 2D-TEE 2.5 ± 1.2 p = 0.01), guide catheters (CT 1 vs. 2D-TEE 1.7 ± 0.8 p = 0.01), and procedure time (3D-CT 55 ± 17 min vs. 2D-TEE 73 ± 24 min p < 0.05).
One major adverse event, a stroke, occurred in the 2D-TEE group. Figure 6 shows an ex vivo fit-testing of all delivery catheters and devices using a 3D-printed model of the patient's heart.46
FIG. 6.

Bench test catheter simulation in 3D-printed patient-specific left atrial appendage.46
Conti et al. studied six patients with LAA leaks (cases) and 14 patients without LAA leaks (controls) after LAAO. The authors aimed at examining the effectiveness of LAA 3DP obtained from CT in estimating the size of LAAO devices, compared with routine measurement using LAA leakage as the endpoint. A patient-specific LAA 3D printed model was developed using CT pre-operative imaging for each group.
The recommended dimensions of the 3D-printed prototype were compared with those of the implanted device. Fifty-five percent of the devices were smaller than the 3D-printed model; the two sizing approaches agreed in 35% of the patients, and in 10% of the patients, the 3D printed model overestimated the size. The incidence of LAA leakage was significantly higher in patients with undersized devices implanted using the conventional technique (p = 0.019). The authors concluded that 3DP of the LAA may add value to the current process for LAAO device sizing, with the potential to reduce LAA leakage.50
Hachulla et al. studied 15 patients to explore the utility of customized 3D-printed models of the LAA to guide device size selection (Amulet device). The Vitrea® software that uses semiautomatic algorithms was utilized to segment the LAA. The LAA model was printed with a 1.5 mm thick shell to have a flexible but resistant material allowing deformation of the device without breaking the model, using Tango Plus FLX 930 flexible material.
Different sizes of Amulet cardiac plugs were implanted into the 3D-printed model. The authors concluded that the device size predicted by 3D-TEE and CT was the same as the size of the implanted device in 8 out of 15 (53%) and 10 out of 15 (67%) cases, respectively. The device size that the personalized 3D-printed models predicted was accurate in every patient, allowing excellent contact with the LAA wall.
These results were accomplished without any instances of device instability or excessive compression. Personalized 3D-printed models-CT performed with the implanted device demonstrated device deformation as well as the location of the disk to the pulmonary veins. With this information, the authors could identify the optimal device size for each one of the 15 patients.70
Fan et al. established the relationship between model-based device selection and procedure and determined whether preprocedural model testing results in superior outcomes. In 72 patients who experienced imaging-guided LAAO, 3D models of the LAA were retrospectively constructed using 3D TEE data sets. These models were used in the study (retrospective cohort). The in vitro model testing was done to find the ideal device, and then that device was compared with the used device.
Analyses were performed on the associations between model-match and model-mismatch device sizes and the outcomes. In addition to imaging, device selection in another 32 patients was prospectively guided by 3D models (prospective cohort). By contrasting the two cohorts, the authors could evaluate the effect that model-based sizing had on the results.
Patients in the retrospective cohort with model-mismatch sizing experienced longer procedure times, higher cumulative incidence rates of ischemic stroke and cardiovascular or unexplained death, more implantation failures, more devices used per procedure, more procedural complications, more peri-device leak, more device thrombus, and longer procedure times after LAA occlusion.
Compared with the retrospective imaging-guided cohort, prospective model-guided patients had a greater implantation success rate and shorter procedural times without issues. Clinical device compression and protrusion were substantially correlated to model testing. Non-windsock morphology and extensive LAA trabeculations predicted size mismatch.
The authors concluded that device size selection according to the 3D-printed model-based sizing is related to enhanced safety and efficacy in patients undergoing LAA occlusion. Better results might be obtained from preprocedural device sizing using 3D models and imaging guidance.71
To determine the occlusion device size before intervention, Hong et al. evaluated 10 patients. The authors printed LAAO phantoms that were patient-personalized according to computed tomography angiography (CTA) images. First, the CTA-observed heart anatomy was segmented, and then the left atrium and its associated components were modeled using the LAAO approach.
Phantoms were created using both FFF and stereolithography (SLA) techniques with thermoplastic polyurethane (TPU) and flexible resin materials, respectively. Figure 7 shows the LAAO phantom fabricated using both techniques.72
FIG. 7.
LAAO 3D CAD model and respective phantom fabricated by two techniques: (A) 3D CAD model, (B) model printed by FFF and (C) model printed by SLA.72 CAD, computer-aided design; FFF, fused filament fabrication; LAAO, left atrial appendage occlusion; SLA, stereolithography.
The phantoms were then evaluated by comparing their physical and structural properties. The 3DP phantoms were utilized directly to confirm the LAA's shape and estimate the LAAO device's size. The hardness of the FFF processed TPU was ∼80–85 shore A, whereas that of the SLA flexible resin was ∼50–85 shore A. The STL model and 3DP-printed phantoms presented a dimensional mismatch between 0.45 and 0.37 mm (Bland–Altman, limits of agreement from 1.8 to 1.6 mm).
During the practice trial, the estimates of device sizes for each of the 10 patients were identical to those provided during the performed procedures.72 The authors reported some issues in accurately mimicking the texture of the actual human body with the currently available 3DP materials. Therefore, using silicone or similar materials for the 3DP technologies is suggested.
In their research, Gharaie et al. introduced an economical approach using 3D printing to create highly elastic structures from a two-part silicone resin. The study demonstrated that the 3D-printed object could stretch up to 38% more than its molded counterpart before breaking, with an elongation capacity of 1859%. The authors also highlighted the potential of their methodology to produce intricate structures with internal cavities, such as a human heart.73
In addition, the authors recommended that the selected or developed material be transparent to observe the position of the device during the simulation. This suggestion, although entirely understandable, raises the problem of using amorphous polymers (transparent) that have higher dependence of the mechanical properties with the environmental conditions (temperature and humidity) than semi-crystalline ones. In conclusion, simulation with a 3D-printed left atrium phantom might be utilized to correctly estimate the size of the LAAO insertion device before the procedure.
Limitations
Despite the improvements in LAAO preprocedural planning, several challenges remain. As the heart is a dynamic organ that continuously cycles between systole and diastole, the choice of material utilized in 3DP may be crucial. When simulating heart tissue using 3D-printed models, it would be ideal if the material's elasticity, density, and asperity closely resembled those of the heart's tissue.
However, the printed product may become distorted due to temperature fluctuations that cause the material to contract. Identifying patients who might benefit most from 3DP simulation is an additional concern. Although technological and equipment advancements in 3DP have made it easier to develop models of individual hearts, the 3DP and simulation procedure is associated with a higher cost and longer time requirement.
Consequently, 3DP in the LAAO process should be limited to situations with expected sizing or procedural difficulties. Those with LAA thrombi, eccentric ostium, exceptionally large or small LAA, multilobes or proximal bifurcation, and additional structural complications may present size challenges. In addition, the position of the septal puncture is an essential step in the surgery, and 3D-printed models that contain the right atrium may enable preprocedural planning. To better describe cases with size discrepancies between 2D imaging and implanted devices and their anatomical properties, additional research is required.52
Conclusions
The anatomy of the LAA is highly complex and varies considerably from patient to patient. Despite breakthroughs in the field of LAAO device design, there is still a substantial fraction of patients with an anatomy-device mismatch. A mismatch between the anatomy and the device can lead to partial LAAO peri device leakage and DRT, all of which are associated with an increased risk of thromboembolic complications.
A paradigm shift in LAAO procedures is necessary, considering these concerns. Recent developments in computer modeling have led to improvements in preprocedural planning using currently available devices. These improvements have assisted implant and interventional imaging physician teams in selecting the ideal device size and target implantation location.
Several research groups are currently progressing toward preprocedural planning concerning the LAA models that are custom-built based on patient data. These developments are made possible by developing fabrication procedures that utilize 3DP, therefore taking profit of one of the biggest advantages of additive manufacturing technologies: personalization.
In the future, LAAO procedures will be able to improve patient outcomes as a result of the increased adoption of data-driven approaches. These approaches use CT procedural planning and advanced additive manufacturing techniques to provide more patient-centric solutions. Therefore, training cardiological interventional doctors and chirurgical planning chirurgical are areas that will, undoubtedly, benefit from the advantages that can only be offered by 3DP in a near future.
Acknowledgment
This research is sponsored by national funds through FCT -Fundação para a Ciência e a Tecnologia, under the projects UIDB/00285/2020 and LA/P/0112/2020.
Authors' Contribution
S.V.: formal analysis (equal); methodology (equal); writing—original draft (lead); writing—review & editing (supporting); M.O.-S.: conceptualization (equal); formal analysis (equal); methodology (equal); writing—original draft (equal); writing—review & editing (supporting); L.G.: conceptualization (equal); supervision (equal); writing—review & editing (equal); A.M.A.: conceptualization (equal); supervision (lead); writing—review & editing (equal); A.P.: conceptualization (equal); supervision (lead); writing—review & editing (lead).
Author Disclosure Statement
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this article.
Funding Information
S.V. grant, UIDP/00285/2020, from FCT -Fundação para a Ciência e a Tecnologia.
References
- 1. Mendez K, Kennedy DG, Wang DD, et al. Left atrial appendage occlusion: Current stroke prevention strategies and a shift toward data-driven, patient-specific approaches. J Soc Cardiovasc Angiography Interv 2022;1(5):100405; doi: 10.1016/j.jscai.2022.100405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Yang Q, Cogswell ME, Flanders WD, et al. Trends in cardiovascular health metrics and associations with all-cause and CVD mortality among US adults. JAMA 2012;307(12):1273–1283; doi: 10.1001/jama.2012.339 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Bauer UE, Briss PA, Goodman RA, et al. Prevention of chronic disease in the 21st century: Elimination of the leading preventable causes of premature death and disability in the USA. Lancet 2014;384(9937):45–52; doi: 10.1016/S0140-6736(14)60648-6 [DOI] [PubMed] [Google Scholar]
- 4. Crystal E. Role of oral anticoagulation in management of atrial fibrillation. Heart 2004;90(7):813–817; doi: 10.1136/hrt.2003.021642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Al-Saady NM, Obel OA, Camm AJ. Left atrial appendage: Structure, function, and role in thromboembolism. Heart 1999;82(5):547–554; doi: 10.1136/hrt.82.5.547 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Safavi-Naeini P, Rasekh A. Closure of left atrial appendage to prevent stroke: Devices and status. Tex Heart Inst J 2018;45(3):172–174; doi: 10.14503/THIJ-18-6693 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Mazzone P, Laricchia A, D'Angelo G, et al. Role of different antithrombotic regimens after percutaneous left atrial appendage occlusion: A large single center experience. J Clin Med 2021;10(9):1959; doi: 10.3390/jcm10091959 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. DeCampos D, Teixeira R, Saleiro C, et al. 3D printing for left atrial appendage closure: A meta-analysis and systematic review. Int J Cardiol 2022;356:38–43; doi: 10.1016/j.ijcard.2022.03.042 [DOI] [PubMed] [Google Scholar]
- 9. Asmarats L, Rodés-Cabau J. The spectrum of devices for percutaneous left atrial appendage occlusion. Cardiac Interv Today 2018;12(3):34–39. Available from: https://citoday.com/articles/2018-may-june/the-spectrum-of-devices-for-percutaneous-left-atrial-appendage-occlusion [Last accessed: October 30, 2022].
- 10. Albaghdadi M, Kadlec A, Adler A, et al. Peri-device leaks after percutaneous left atrial appendage closure: Clinical significance and unmet diagnostic needs. Struct Heart 2020;4(6):475–481; doi: 10.1080/24748706.2020.1817642 [DOI] [Google Scholar]
- 11. Fauchier L, Cinaud A, Brigadeau F, et al. Device-related thrombosis after percutaneous left atrial appendage occlusion for atrial fibrillation. J Am Coll Cardiol 2018;71(14):1528–1536; doi: 10.1016/j.jacc.2018.01.076 [DOI] [PubMed] [Google Scholar]
- 12. Dukkipati SR, Kar S, Holmes DR, et al. Device-related thrombus after left atrial appendage closure: Incidence, predictors, and outcomes. Circulation 2018;138(9):874–885; doi: 10.1161/CIRCULATIONAHA.118.035090 [DOI] [PubMed] [Google Scholar]
- 13. Alkhouli M, Busu T, Shah K, et al. Incidence and clinical impact of device-related thrombus following percutaneous left atrial appendage occlusion: A meta-analysis. JACC Clin Electrophysiol 2018;4(12):1629–1637; doi: 10.1016/j.jacep.2018.09.007 [DOI] [PubMed] [Google Scholar]
- 14. Vogenberg FR, Isaacson Barash CI, Pursel M. Personalized medicine: Part 1: Evolution and development into theranostics. Pharm Ther 2010;35(10):560–576. [PMC free article] [PubMed] [Google Scholar]
- 15. Oliveira-Santos M de, Oliveira-Santos E, Gonçalves L, et al. Cardiovascular three-dimensional printing in non-congenital percutaneous interventions. Heart Lung Circ 2019;28(10):1525–1534; doi: 10.1016/j.hlc.2019.04.020 [DOI] [PubMed] [Google Scholar]
- 16. Wang DD, Qian Z, Vukicevic M, et al. 3D printing, computational modeling, and artificial intelligence for structural heart disease. JACC Cardiovasc Imaging 2021;14(1):41–60; doi: 10.1016/j.jcmg.2019.12.022 [DOI] [PubMed] [Google Scholar]
- 17. Wang Q, Primiano C, McKay R, et al. CT image-based engineering analysis of transcatheter aortic valve replacement. JACC Cardiovasc Imaging 2014;7(5):526–528; doi: 10.1016/j.jcmg.2014.03.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Mao W, Caballero A, McKay R, et al. Fully-coupled fluid-structure interaction simulation of the aortic and mitral valves in a realistic 3D left ventricle model. PLoS One 2017;12(9):e0184729; doi: 10.1371/journal.pone.0184729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Qian Z, Wang K, Liu S, et al. Quantitative prediction of paravalvular leak in transcatheter aortic valve replacement based on tissue-mimicking 3D printing. JACC Cardiovasc Imaging 2017;10(7):719–731; doi: 10.1016/j.jcmg.2017.04.005 [DOI] [PubMed] [Google Scholar]
- 20. Vukicevic M, Vekilov DP, Grande-Allen JK, et al. Patient-specific 3D valve modeling for structural intervention. Struct Heart 2017;1(5–6):236–248; doi: 10.1080/24748706.2017.1377363 [DOI] [Google Scholar]
- 21. Vivoli G, Gasparotti E, Rezzaghi M, et al. Simultaneous functional and morphological assessment of left atrial appendage by 3D virtual models. J Healthc Eng 2019;2019:1–8; doi: 10.1155/2019/7095845 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Viles-Gonzalez JF, Kar S, Douglas P, et al. The clinical impact of incomplete left atrial appendage closure with the watchman device in patients with atrial fibrillation. J Am Coll Cardiol 2012;59(10):923–929; doi: 10.1016/j.jacc.2011.11.028 [DOI] [PubMed] [Google Scholar]
- 23. Collado FMS, Lama von Buchwald CM, Anderson CK, et al. Left atrial appendage occlusion for stroke prevention in nonvalvular atrial fibrillation. J Am Heart Assoc 2021;10(21):e022274; doi: 10.1161/JAHA.121.022274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Karakus G, Kodali V, Inamdar V, et al. Comparative assessment of left atrial appendage by transesophageal and combined two- and three-dimensional transthoracic echocardiography. Echocardiography 2008;25(8):918–924; doi: 10.1111/j.1540-8175.2008.00758.x [DOI] [PubMed] [Google Scholar]
- 25. Nakajima H, Seo Y, Ishizu T, et al. Analysis of the left atrial appendage by three-dimensional transesophageal echocardiography. Am J Cardiol 2010;106(6):885–892; doi: 10.1016/j.amjcard.2010.05.014 [DOI] [PubMed] [Google Scholar]
- 26. Marek D, Vindis D, Kocianova E. Real time 3-dimensional transesophageal echocardiography is more specific than 2-dimensional TEE in the assessment of left atrial appendage thrombosis. Biomed Papers 2013;157(1):22–26; doi: 10.5507/bp.2012.012 [DOI] [PubMed] [Google Scholar]
- 27. Beigel R, Wunderlich NC, Ho SY, et al. The left atrial appendage: Anatomy, function, and noninvasive evaluation. JACC Cardiovasc Imaging 2014;7(12):1251–1265; doi: 10.1016/j.jcmg.2014.08.009 [DOI] [PubMed] [Google Scholar]
- 28. Noroozi R, Tatar F, Zolfagharian A, et al. Additively manufactured multi-morphology bone-like porous scaffolds: Experiments and micro-computed tomography-based finite element modeling approaches. Int J Bioprint 2022;8(3):40–53; doi: 10.18063/ijb.v8i3.556 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Zolfagharian A, Gregory TM, Bodaghi M, et al. Patient-specific 3D-printed splint for mallet finger injury. Int J Bioprint 2020;6(2):1–13; doi: 10.18063/ijb.v6i2.259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Hong SJ, Kim JY, Kim JB, et al. Multidetector computed tomography may be an adequate screening test to reduce periprocedural stroke in atrial fibrillation ablation: A multicenter propensity-matched analysis. Heart Rhythm 2014;11(5):763–770; doi: 10.1016/j.hrthm.2014.01.026 [DOI] [PubMed] [Google Scholar]
- 31. Gilhofer TS, Saw J. Periprocedural imaging for left atrial appendage closure. Card Electrophysiol Clin 2020;12(1):55–65; doi: 10.1016/j.ccep.2019.11.007 [DOI] [PubMed] [Google Scholar]
- 32. Bartel T, Rivard A, Jimenez A, et al. Medical three-dimensional printing opens up new opportunities in cardiology and cardiac surgery. Eur Heart J 2018;39(15):1246–1254; doi: 10.1093/eurheartj/ehx016 [DOI] [PubMed] [Google Scholar]
- 33. Wu H, Fahy WP, Kim S, et al. Recent developments in polymers/polymer nanocomposites for additive manufacturing. Prog Mater Sci 2020;111:100638; doi: 10.1016/j.pmatsci.2020.100638 [DOI] [Google Scholar]
- 34. Cano-Vicent A, Tambuwala MM, Hassan SkS, et al. Fused deposition modelling: Current status, methodology, applications and future prospects. Addit Manuf 2021;47:102378; doi: 10.1016/j.addma.2021.102378 [DOI] [Google Scholar]
- 35. Jiang R, Kleer R, Piller FT. Predicting the future of additive manufacturing: A Delphi study on economic and societal implications of 3D printing for 2030. Technol Forecast Soc Change 2017;117:84–97; doi: 10.1016/j.techfore.2017.01.006 [DOI] [Google Scholar]
- 36. Guo N, Leu MC. Additive manufacturing: Technology, applications and research needs. Front Mech Eng 2013;8(3):215–243; doi: 10.1007/s11465-013-0248-8 [DOI] [Google Scholar]
- 37. Chen Y, Zhou C, Lao J. A layerless additive manufacturing process based on CNC accumulation. Rapid Prototyp J 2011;17(3):218–227; doi: 10.1108/13552541111124806 [DOI] [Google Scholar]
- 38. Pan Y, Zhou C, Chen Y, et al. Multitool and multi-axis computer numerically controlled accumulation for fabricating conformal features on curved surfaces. J Manuf Sci Eng 2014;136(3):031007; doi: 10.1115/1.4026898 [DOI] [Google Scholar]
- 39. Rajan K, Samykano M, Kadirgama K, et al. Fused deposition modeling: Process, materials, parameters, properties, and applications. Int J Adv Manuf Technol 2022;120(3–4):1531–1570; doi: 10.1007/s00170-022-08860-7 [DOI] [Google Scholar]
- 40. International Standard Organization, CH, ISO/ASTM 52900:2021 Additive manufacturing—General principles—Fundamentals and vocabulary. Available from: https://www.iso.org/obp/ui/#iso:std:iso-astm:52900:ed-2:v1:en, 2021 [Last accessed: November 13, 2022].
- 41. Ligon SC, Liska R, Stampfl J, et al. Polymers for 3D printing and customized additive manufacturing. Chem Rev 2017;117(15):10212–10290; doi: 10.1021/acs.chemrev.7b00074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Palmero EM, Casaleiz D, de Vicente J, et al. Composites based on metallic particles and tuned filling factor for 3D-printing by fused deposition modeling. Compos Part A Appl Sci Manuf 2019;124:105497; doi: 10.1016/j.compositesa.2019.105497 [DOI] [Google Scholar]
- 43. Li VCF, Kuang X, Hamel CM, et al. Cellulose nanocrystals support material for 3D printing complexly shaped structures via multi-materials-multi-methods printing. Addit Manuf 2019;28:14–22; doi: 10.1016/j.addma.2019.04.013 [DOI] [Google Scholar]
- 44. Dizon JRC, Espera AH, Chen Q, et al. Mechanical characterization of 3D-printed polymers. Addit Manuf 2018;20:44–67; doi: 10.1016/j.addma.2017.12.002 [DOI] [Google Scholar]
- 45. Jia D, Zhou Q, Song HN, et al. The value of the left atrial appendage orifice perimeter of 3D model based on 3D TEE data in the choice of device size of LAmbreTM occluder. Int J Cardiovasc Imaging 2019;35(10):1841–1851; doi: 10.1007/s10554-019-01627-4 [DOI] [PubMed] [Google Scholar]
- 46. Eng MH, Wang DD, Greenbaum AB, et al. Prospective, randomized comparison of 3-dimensional computed tomography guidance versus TEE data for left atrial appendage occlusion (PRO3DLAAO). Cathet Cardiovasc Interv 2018;92(2):401–407; doi: 10.1002/ccd.27514 [DOI] [PubMed] [Google Scholar]
- 47. Asami M. Computed tomography measurement for left atrial appendage closure. Cardiovasc Interv Ther 2022;37(3):440–449; doi: 10.1007/s12928-022-00852-4 [DOI] [PubMed] [Google Scholar]
- 48. Saint Croix G, Imran Zaidi S, Loescher VS, et al. Computed tomography-derived three-dimensional printed models versus two-dimensional transesophageal echocardiography for left atrial appendage occlusion device planning: A systematic review and meta-analysis. J Atr Fibrillation 2020;13(4):2433; doi: 10.4022/jafib.2433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Chen T, Liu G, Mu Y, et al. Application of cardiac computed tomographic imaging and fluoroscopy fusion for guiding left atrial appendage occlusion. Int J Cardiol 2021;331:289–295; doi: 10.1016/j.ijcard.2021.01.035 [DOI] [PubMed] [Google Scholar]
- 50. Conti M, Marconi S, Muscogiuri G, et al. Left atrial appendage closure guided by 3D computed tomography printing technology: A case control study. J Cardiovasc Comput Tomogr 2019;13(6):336–339; doi: 10.1016/j.jcct.2018.10.024 [DOI] [PubMed] [Google Scholar]
- 51. Korsholm K, Jensen JM, Nørgaard BL, et al. Peridevice leak following amplatzer left atrial appendage occlusion: Cardiac computed tomography classification and clinical outcomes. JACC Cardiovasc Interv 2021;14(1):83–93; doi: 10.1016/j.jcin.2020.10.034 [DOI] [PubMed] [Google Scholar]
- 52. Hell MM, Achenbach S, Yoo IS, et al. 3D printing for sizing left atrial appendage closure device: Head-to-head comparison with computed tomography and transoesophageal echocardiography. EuroIntervention 2017;13(10):1234–1241; doi: 10.4244/EIJ-D-17-00359 [DOI] [PubMed] [Google Scholar]
- 53. Beutler DS, Gerkin RD, Loli AI. The morphology of left atrial appendage lobes: A novel characteristic naming scheme derived through three-dimensional cardiac computed tomography. World J Cardiovasc Surg 2014;04(03):17–24; doi: 10.4236/wjcs.2014.43004 [DOI] [Google Scholar]
- 54. Burrill J, Dabbagh Z, Gollub F, et al. Multidetector computed tomographic angiography of the cardiovascular system. Postgrad Med J 2007;83(985):698–704; doi: 10.1136/pgmj.2007.061804 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Gaynor AT, Meisel NA, Williams CB, et al. Multiple-material topology optimization of compliant mechanisms created via polyjet three-dimensional printing. J Manuf Sci Eng Trans ASME 2014;136(6):1–11; doi: 10.1115/1.4028439 [DOI] [Google Scholar]
- 56. Gülcan O, Günaydın K, Tamer A. The state of the art of material jetting—a critical review. Polymers (Basel) 2021;13(16):2829; doi: 10.3390/polym13162829 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Robinson SS, Aubin CA, Wallin TJ, et al. Stereolithography for personalized left atrial appendage occluders. Adv Mater Technol 2018;3(12):1800233; doi: 10.1002/admt.201800233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Melchels FPW, Feijen J, Grijpma DW. A review on stereolithography and its applications in biomedical engineering. Biomaterials 2010;31(24):6121–6130; doi: 10.1016/j.biomaterials.2010.04.050 [DOI] [PubMed] [Google Scholar]
- 59. Pagac M, Hajnys J, Ma QP, et al. A review of vat photopolymerization technology: Materials, applications, challenges, and future trends of 3d printing. Polymers (Basel) 2021;13(4):1–20; doi: 10.3390/polym13040598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Fico D, Rizzo D, Casciaro R, et al. A review of polymer-based materials for fused filament fabrication (FFF): Focus on sustainability and recycled materials. Polymers (Basel) 2022;14(3):465; doi: 10.3390/polym14030465 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Vyavahare S, Teraiya S, Panghal D, et al. Fused deposition modelling: A review. Rapid Prototyp J 2020;26(1):176–201; doi: 10.1108/RPJ-04-2019-0106 [DOI] [Google Scholar]
- 62. Otton JM, Spina R, Sulas R, et al. Left atrial appendage closure guided by personalized 3D-printed cardiac reconstruction. JACC Cardiovasc Interv 2015;8(7):1004–1006; doi: 10.1016/j.jcin.2015.03.015 [DOI] [PubMed] [Google Scholar]
- 63. Liu P, Liu R, Zhang Y, et al. The Value of 3D printing models of left atrial appendage using real-time 3D transesophageal echocardiographic data in left atrial appendage occlusion: Applications toward an Era of Truly personalized medicine. Cardiology 2016;135(4):255–261; doi: 10.1159/000447444 [DOI] [PubMed] [Google Scholar]
- 64. Wang DD, Eng M, Kupsky D, et al. Application of 3-dimensional computed tomographic image guidance to WATCHMAN implantation and impact on early operator learning curve. JACC Cardiovasc Interv 2016;9(22):2329–2340; doi: 10.1016/j.jcin.2016.07.038 [DOI] [PubMed] [Google Scholar]
- 65. Goitein O, Fink N, Guetta V, et al. Printed MDCT 3D models for prediction of left atrial appendage (LAA) occluder device size: A feasibility study. EuroIntervention 2017;13(9):e1076–e1079; doi: 10.4244/EIJ-D-16-00921 [DOI] [PubMed] [Google Scholar]
- 66. Li H, Qingyao, Bingshen, et al. Application of 3D printing technology to left atrial appendage occlusion. Int J Cardiol 2017;231:258–263; doi: 10.1016/j.ijcard.2017.01.031 [DOI] [PubMed] [Google Scholar]
- 67. Obasare E, Mainigi SK, Morris DL, et al. CT based 3D printing is superior to transesophageal echocardiography for pre-procedure planning in left atrial appendage device closure. Int J Cardiovasc Imaging 2018;34(5):821–831; doi: 10.1007/s10554-017-1289-6 [DOI] [PubMed] [Google Scholar]
- 68. Song H, Zhou Q, Zhang L, et al. Evaluating the morphology of the left atrial appendage by a transesophageal echocardiographic 3-dimensional printed model. Medicine (United States) 2017;96(38):e7865; doi: 10.1097/MD.0000000000007865 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Ciobotaru V, Combes N, Martin CA, et al. Left atrial appendage occlusion simulation based on three-dimensional printing: New insights into outcome and technique. EuroIntervention 2018;14(2):176–184; doi: 10.4244/EIJ-D-17-00970 [DOI] [PubMed] [Google Scholar]
- 70. Hachulla AL, Noble S, Guglielmi G, et al. 3D-printed heart model to guide LAA closure: Useful in clinical practice? Eur Radiol 2019;29(1):251–258; doi: 10.1007/s00330-018-5569-x [DOI] [PubMed] [Google Scholar]
- 71. Fan Y, Yang F, Cheung GS-H, et al. Device sizing guided by echocardiography-based three-dimensional printing is associated with superior outcome after percutaneous left atrial appendage occlusion. J Am Soc Echocardiogr 2019;32(6):708–719; doi: 10.1016/j.echo.2019.02.003 [DOI] [PubMed] [Google Scholar]
- 72. Hong D, Moon S, Cho Y, et al. Rehearsal simulation to determine the size of device for left atrial appendage occlusion using patient-specific 3D-printed phantoms. Sci Rep 2022;12(1):7746; doi: 10.1038/s41598-022-11967-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Gharaie S, Zolfagharian A, Moghadam AAA, et al. Direct 3D printing of a two-part silicone resin to fabricate highly stretchable structures. Prog Addit Manuf 2023; doi: 10.1007/s40964-023-00421-y [DOI] [Google Scholar]