Abstract
Background:
In our prior study, the authors determined that pulling on the superficial adipose layer is more effective in lifting the skin than pulling on the superficial musculoaponeurotic system (SMAS). Applying this concept of using the superficial adipose layer to transmit the lifting force to the skin, this study examined improvements in patients who underwent lateral midface lifting using our minimally invasive multilayer lifting technique and measured the duration of those improvements.
Methods:
Along the hairline in front of the sideburns, a W-shaped zigzag incision of 3 to 8 mm in width and 3 to 4 cm in length was made. On the temporal scalp, 3 to 4 cm away from the first incision, a second incision was made more lateral/posterior to the first incision, and an elliptical excision of 3 to 5 mm in width and 3 to 4 cm in length was made. From the medial cut margin of the anterior first incision, the superficial temporal fascia/SMAS (the deep layer), and the superficial adipose layer (the superficial layer) were purchased with 3-0 polyester sutures, tunneled under the soft tissue, and fixed to the deep temporal fascia of the second posterior temporal incision. Prior to the excised temporal scalp closure, the dermis in the medial cut margin of the second incision was pulled to the rear as much as possible and fixed to the deep temporal fascia.
Results:
The effects of surgery were monitored for 6 to 42 months after surgery. The nasolabial folds were improved. Skin elasticity also showed significant improvements, which lasted throughout the follow-up period (up to 42 mo).
Conclusions:
Unlike traditional wide dissection SMAS facelift, our method requires minimal incisions and does not require skin undermining. Therefore, the operating time is shorter, and postoperative swelling is minimized. In our technique, the superficial adipose layer, the superficial temporal fascia/SMAS, and the dermis were pulled individually to lift all layers of the lateral midface soft tissues. This results in a significant and long-lasting lateral midface rejuvenation.
Key Words: CaSS, cutaneous layer, facial rejuvenation, minimally invasive facelift, SMAS, midface lift
In modern society, aging individuals increasingly engage in social activities and take a greater interest in health and appearance. The desire to look younger than one’s age is also becoming stronger. Most clinicians agree that various surgical facelifts are effective in restoring a younger-looking face. However, the fact that most facelift surgery is an extensive procedure requiring a long recovery time interferes with patients’ social and work activities. This places some limitations on selecting surgery as the first choice of treatment modality.
Many surgical methods involve pulling the superficial musculoaponeurotic system (SMAS) while the skin is detached as a dual plane. To improve skin elasticity, excess skin is pulled separately and removed to tighten the skin. Unfortunately, facelift methods using this concept can often lead to inadequate surgical outcomes for the midface, despite the wide extent of surgery. The deep-plane facelift technique also has difficulty correcting the midface, as medial deep dissection increases the chance of nerve injury.
The authors previously confirmed, by testing skin tension, that when the SMAS was lifted without subcutaneous detachment and then the superficial adipose layer was subsequently lifted (thus 2-layer pull in combination without detachment), there was an improvement in sagging skin.1 Based on this result, a new surgical method that involves making a skin incision near the sideburn and lifting sagging facial skin without subcutaneous detachment was developed, implemented, and observed over the course of long-term follow-up. Observations of progress from at least 6 and up to 42 months after surgery demonstrated improvements in the lateral midface, thereby yielding a rejuvenating effect in a similar manner to other more extensive facelift procedures.
METHODS
The authors operated on 93 patients from March 2017 to August 2022 (70 months) using the cutaneous layer and SMAS suspension (CaSS) lift procedure. To ensure consistency in the surgical outcomes, the study consisted of the patients of the first author. The participants in the study had facial sagging but did not require neck lifting. Participants who required and underwent neck lifting were excluded from the study. The procedures were performed under local anesthesia or local anesthesia plus IV sedation.
Among the 93 patients, 71 who were available for follow-up observations at least 6 months after surgery were evaluated using the midface esthetic scale. The average time of follow-up was 11.4 months, and the longest follow-up was 42 months. Patients’ age ranged from 26 to 65 years, and most were women (n=58). Two were in their 20s, 7 in their 30s, 19 in their 40s, 37 in their 50s, and 6 in their 60s. Of the 71 patients, 39 underwent CaSS lift and lower blepharoplasty using a suborbicularis oculi fat (SOOF) lift (Supplemental Table 1, Supplemental Digital Content 1, http://links.lww.com/SCS/F596; Table 2, Supplemental Digital Content 2, http://links.lww.com/SCS/F597).
Operative Method
Design
The operation was designed while the patient was in a sitting position. The face skin was pulled multiple times from the sideburns, placing pressure on the skin through the fingertips. An oblique angle at which the upper cheek, the lower cheek, and the nasolabial fold were to most improve was identified, and the direction of traction was marked.
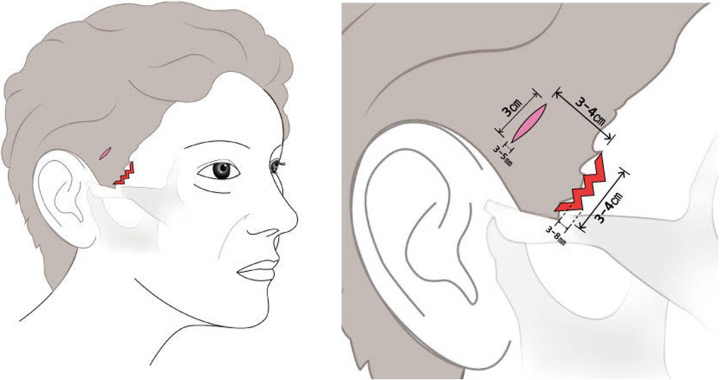
A W shape of 3 to 8 mm in width and 3 to 4 cm in length were marked along the anterior border of the sideburns in an oblique direction. If the sideburn was located relatively anteriorly, the location of the incision marking was moved inside the hairline (more laterally) in order to prevent facial nerve damage. A 3 to 4 cm long fusiform incision in an oblique direction was then designed in the temporal scalp, 3 to 4 cm from the first incision (Fig. 1).
FIGURE 1.
When designing the incision line, an oblique angle should be chosen such that the upper cheek and the lower cheek can most effectively be lifted.
Incision and Dissection
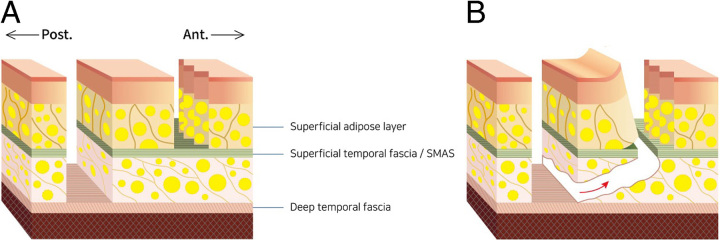
Using a number 15 blade, the first anterior skin and the superficial adipose layer were excised, taking care not to damage the hair follicles. In the second temporal scalp incision, the skin, the superficial adipose layer, and the superficial temporal fascia/SMAS were excised to expose the deep temporal fascia (Fig. 2A). From the temporal incision, undermining was performed along the space between the deep temporal fascia layer and the superficial temporal fascia layer to reach the initial sideburn incision, and the superficial temporal fascia layer/SMAS was then cut from underneath to create a tunnel and expose the underlying layer (Fig. 2B).
FIGURE 2.
Skin and the subcutaneous fat layer are excised in the anterior incision, while skin, the subcutaneous fat layer, and the superficial temporal fascia/superficial musculoaponeurotic system are excised in the posterior incision (A). In the posterior incision site, the deep temporal fascia is exposed, and a dissection toward the anterior incision is made with scissors. Upon reaching the anterior incision site from underneath (red arrow), the superficial temporal fascia / superficial musculoaponeurotic system layer is encountered and is cut from underneath to create a tunnel (B).
Anterior Purchase of Tissues
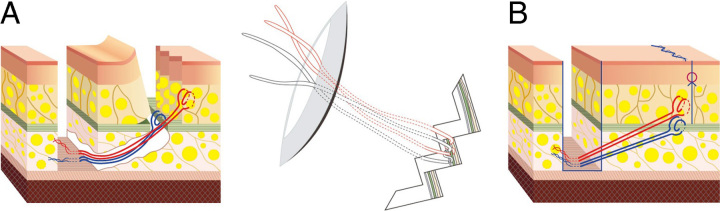
Through the anterior incision, a sling was made by purchasing the superficial temporal fascia/SMAS using 3-0 Ethibond (blue thread in Fig. 3A, Supplemental Digital Content Video 1, Supplemental Digital Content 3, http://links.lww.com/SCS/F598), and another sling was formed by purchasing the superficial adipose layer using 3-0 Ethibond (red thread in Fig. 3A, Supplemental Digital Content Video 2, Supplemental Digital Content 4, http://links.lww.com/SCS/F599), and both were pulled in a premarked oblique direction (Fig. 3B).
FIGURE 3.
(A) A suture purchasing the superficial temporal fascia/superficial musculoaponeurotic system and another suture purchasing the superficial adipose layer using 3-0 Ethibond are fixed to the deep temporal fascia through the tunnel. (B) After the sutures are tied, the distal skin, superficial adipose layer, and superficial temporal fascia/superficial musculoaponeurotic system are advanced proximally.
The slings purchasing the superficial temporal fascia/SMAS were pulled in 2 directions to lift the deeper layer of the upper cheek and the lower cheek. In addition, the slings purchasing the superficial adipose layer were also pulled in 2 directions to lift the superficial layers of the upper cheek and the lower cheek. Thus, there were 4 sutures exerting pulling forces (Supplemental Digital Content Video 3, Supplemental Digital Content 5, http://links.lww.com/SCS/F600).
Fixation
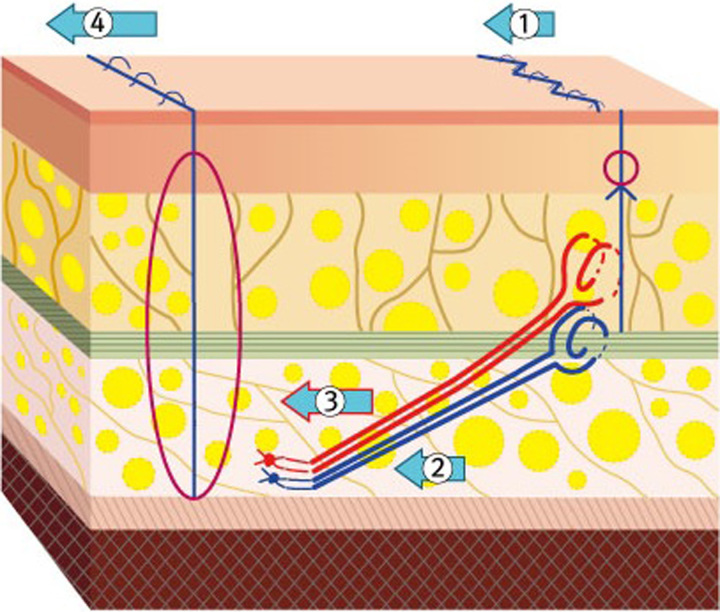
Before the slings were tied down to the deep temporal fascia, the skin incision around the sideburn was sutured. Slings were then passed cephalad through the recently created tunnel and pulled out to the lateral temporal scalp incision. Each sling was fixed to the deep temporal fascia while maintaining the initially planned vector pull. The lower cheek was pulled and fixated first, followed by the upper cheek. In terms of the sequence of layer fixation, the lower layer (superficial temporal fascia/SMAS) was fixed first, while the upper layer (superficial adipose layer) was fixed afterward (Fig. 4).
FIGURE 4.
After the sideburn incision is sutured first ①, sutures purchasing the superficial temporal fascia/superficial musculoaponeurotic system are fixed to the deep temporal fascia ② and then sutures purchasing the superficial adipose layer are fixed to the deep temporal fascia ③. Finally, the dermal edges of the temporal scalp incision are closed ④.
After completing all the sling fixations, the medial cut end of the temporal scalp was pulled posteriorly and fixated at the deep temporal fascia (Supplemental Digital Content Video 4, Supplemental Digital Content 6, http://links.lww.com/SCS/F601). This maneuver reduces the tension on the sideburn and minimizes the potential for poor wound healing around the sideburn.
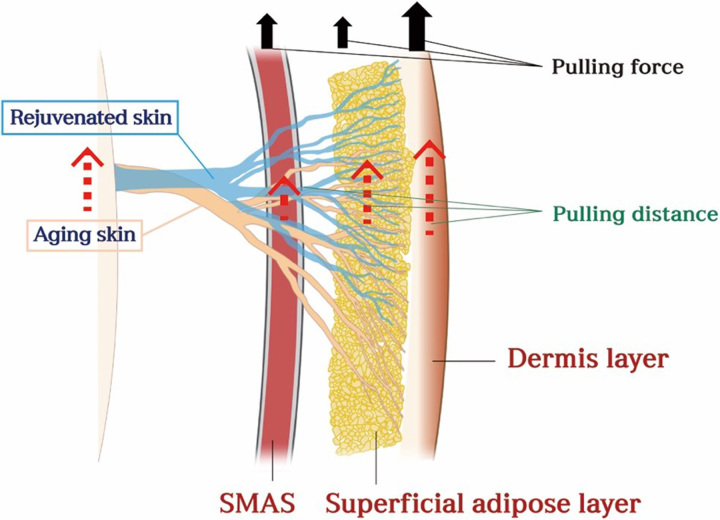
The Mechanism of How Aged Skin Transforms Into Rejuvenated Skin
The pulling forces of the SMAS, superficial adipose layer, and dermis have to be adjusted in the following manner. The pulling force applied to the dermis should be the greatest. The pulling force applied to the superficial adipose layer should be the least. And the pulling force applied on the SMAS should be intermediate (Fig. 5). The least amount of force is needed to the superficial adipose layer, as it has the fewest elastic fibers and resistant connective tissues. More force is needed on the skin as skin tissue laxity is greater than the underlying adipose and SMAS layers.
FIGURE 5.
The mechanism of how aging skin transforms into rejuvenated skin. When pulling these layers [superficial musculoaponeurotic system (SMAS), superficial adipose layer, and the dermis], the principle of force applied to these layers is the following: forces should be applied where the amount of tissue moved is greatest at the skin (largest red arrow), followed by the superficial adipose layer (medium size red arrow), and the least amount of tissue movement is at the SMAS (smallest red arrow). In order to achieve these types of movements, more force should be applied to the dermis (largest black arrow), followed by the SMAS (medium size black arrow), and the least amount of force should be applied to the superficial adipose layer (smallest black arrow).
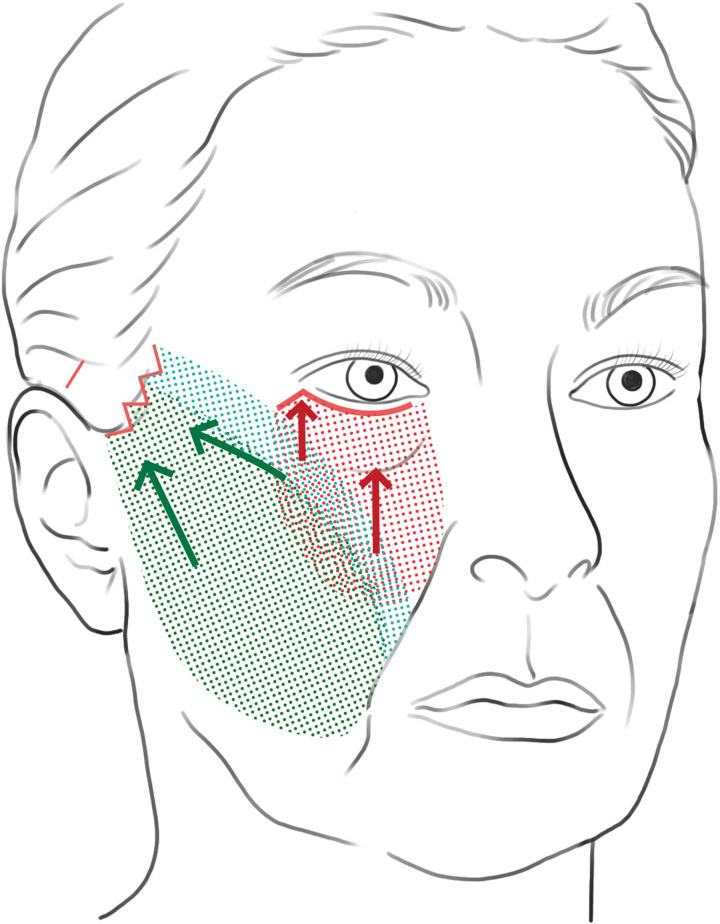
Combination With Lower Blepharoplasty Including SOOF Lift
The CaSS lift significantly improve the lateral midface region (Fig. 6). However, its ability to improve medial midface aging is minimal. Since the concavity of the cheek and deficiency of volume that comes with age are not improved by the CaSS lift, lower blepharoplasty via fat transposition and the SOOF lift can maximize the rejuvenating effect. Therefore, a synergistic effect can be achieved by performing the CaSS lift in combination with lower blepharoplasty (fat transposition and SOOF lift) to obtain maximum results. In cases where the lateral midface sagging is significant or there is asymmetrically more sagging on one side, then the side with significant sagging can be corrected by increasing the pulling force / tension during CaSS lift.
FIGURE 6.
Illustration of the area where cutaneous layer and superficial musculoaponeurotic system suspension lift improve the lateral midface sagging (green color) and the area where lower blepharoplasty improves the medial midface (red color). If both techniques are applied, then both of these areas are improved, and improvement in the overall midface can be achieved by the synergistic effect of the 2 procedures.
RESULTS
Of the 71 patients that were followed for more than 6 months, 32 received only a CaSS lift, while 39 received a CaSS lift together with lower blepharoplasty. Thus, the majority of the patients had a combination of a CaSS lift and a lower blepharoplasty.
In the patients who received only a CaSS lift, minimal postsurgical swelling was observed from the profile view, while no swelling was noticeable from the frontal view. Thus, the recovery after surgery was rapid, and the incision scars improved to the point of not being visible 1 to 2 months after surgery. Postoperative complications such as hematoma or skin necrosis did not occur.
The follow-up period after surgery ranged from 6 to 42 months, with an average of 11.4 months. Lower blepharoplasty using a SOOF lift played a major role in improving the upper nasolabial fold and the medial midface, while the CaSS lift played a major role in improving the lower nasolabial fold and the lateral midface. The sagging lower face did not completely improve with only a CaSS lift. Therefore, patients with aging neck resulted in a less satisfactory outcome (Figs. 7–9).
FIGURE 7.
A 53-year-old patient taken preoperatively (left) and 20 months after an endoscopic forehead lift, upper and lower blepharoplasty, and cutaneous layer and superficial musculoaponeurotic system suspension lift (right).
FIGURE 9.
A 52-year-old female taken preoperatively (left) and 8 months after simultaneously performing lower blepharoplasty and cutaneous layer and superficial musculoaponeurotic system suspension lift (right).
FIGURE 8.
A 65-year-old female taken preoperatively (left) and 42 months after simultaneously performing an endoscopic forehead lift, lower blepharoplasty, and cutaneous layer and superficial musculoaponeurotic system suspension lift (right).
DISCUSSION
As people age, skin elasticity weakens and the tissue that supports the skin loosens. These factors and the force of gravity lead to overall soft tissue sagging. These changes are especially prominent in the forehead, periorbita, midface, nasolabial folds, and jowls. And these physical changes make people look older.
Midface aging starts to show in the periorbital region and as the aging progresses, tear-trough deformity, an Indian groove, deep nasolabial fold, and drooping of the jowl appear on the face. The bone structures that make up the midface are the zygomatic bone and the maxillary bone. The midface can be categorized into the lateral midface and the medial midface. Medial midface aging can be improved with lower blepharoplasty that utilizes the SOOF lift method. However, there are many aspects that need to be considered when it comes to improving lateral midface aging.
Facelift surgery is both effective and has a long-lasting result in improving facial sagging. Therefore, it has long been recognized as a standard method to improve aging appearance. However, some patients may hesitate to select facelift surgery because the typical surgery involves extensive undermining of tissue and an extensive recovery time. In addition, the potential for complications such as nerve injury and hematoma further deters patients from surgery. Meanwhile, nonsurgical methods have been developed, such as Botox injections,2,3 filler injections,4,5 and radiofrequency therapy,6,7 as well as various forms of thread lifts.8,9 A tendency has emerged to choose nonsurgical methods before surgical methods because of the following: lower cost, faster recovery, fewer scars, and minimal disruption of daily life. However, it is difficult to obtain a satisfactory result with these nonsurgical methods because they lead to only mild improvements in facial sagging and have short-lasting effects.
The standard facelift method10-18 using SMAS plication is to detach the skin from the SMAS layer, pull the loosened SMAS up, and remove the excess skin to maintain adequate skin tension in order to restore skin elasticity. However, in the process of detaching the skin, the vertically oriented fibrous network within the superficial adipose layer that connects the skin and the SMAS is severed. For this reason, even if the SMAS layer is pulled tight, unless the skin is pulled even tighter, the skin tension will not be maintained for the expected duration, and sagging will recur. Thus, in order to improve the elasticity of the skin, the skin is pulled tight, which creates tension at the incision site, which can lead to postoperative scarring.
The composite flap method,19,20 which does not separate the skin and SMAS, results in a more natural outcome and better incision scars than the method that detaches the skin and SMAS, since it maintains the fibrous network between the skin and SMAS. However, this method requires extensive deep-plane undermining and therefore increases the potential for facial nerve injury.
Improving the nasolabial fold and the midface is challenging through the dual-plane SMAS facelift technique because the SMAS and the skin are pulled in separate vectors. The SMAS is elevated typically along the direction of the zygomatic major muscle (oblique direction) while the skin is pulled in a more horizontal direction.21 Therefore, the synergistic effect of the combined lifting vector is lost, and less force is transmitted to the distal region of the face (the nasolabial fold and the midface). In order to resolve this problem, the SMAS was detached from the zygomatic arch, and the dissection extended medially and then pulled toward the anterior zygoma to improve the nasolabial fold.22,23 These maneuvers require significant medial facial dissection, which increases postoperative swelling and nerve injury.
In our CaSS lift technique, the lifting effect of the lateral midface is better than that of the medial midface. This is because the vector of the pull transmits toward the lateral midface but less toward the medial midface. Another limitation of our technique is that the force is not transmitted to the most distal region of the lower face. Therefore, if the patient desires correction of these aging effects in the lower face, then traditional SMAS or deep-plane facelift procedures are required.
The superficial adipose layer is present with a considerable thickness anterior to or below the sideburn. Unlike the other subcutaneous fat layer regions, the superficial adipose layer around the sideburn is composed of numerous septa arranged in an array.24,25 The superficial adipose layer is closely connected to the SMAS/the superficial temporal fascia, and the dermis. In order for the SMAS pull to transmit the force to the skin, the force would have to be transferred to the superficial adipose layer first and then to the skin. However, the superficial adipose layer pull will directly transmit the force to the skin without any intermediate layer. For this reason, the force of pull transmitted to the sagging skin is greater if the superficial adipose layer is pulled than simply pulling on the SMAS. According to our prior study, the pulling effect of the superficial adipose layer on the skin is quite significant. Thus, the superficial adipose layer can lift the overlying skin by using only 50% of the pulling force required on the SMAS layer to get the same lifting of the skin.1 However, the superficial adipose layer tissue is more fragile than the SMAS tissue. Therefore, if the superficial adipose layer is pulled with too much force, then a cheese-wiring effect can occur. In order to circumvent this issue of cheese-wiring, the force used to retract the superficial adipose layer should only be slightly more than half of the force used to pull the SMAS. In addition, when the posterior incision is sutured, cheese-wiring of the superficial adipose layer can be minimized by pulling the dermis of the temporal scalp posteriorly and fixating on the deep temporal fascia. This will help offload some of the tension on the anterior superficial adipose layer.
Our technique does not separate the skin from the underlying tissues. Therefore, the duration of the surgery is short, and the recovery is rapid. The sideburn incision is short, and it can easily be covered with hair during the healing process. Thus, the patient can resume normal activity without the stigma of surgery. Postoperatively, we did notice a slight dimple at the incision site in a few patients, which resolved within 3 months without any need for surgical intervention. This technique is applicable for patients who have lateral midface aging without lower face (jowls, jawline contour, and neck) aging. If there is medial midface aging, then the patient will require lower blepharoplasty with a SOOF lift. In addition, this technique can be added to the traditional lower facelift to improve the lateral midface, as the lateral midface is difficult to improve with many traditional facelift procedures.
Our technique will work well and benefit patients with very thin skin or patients with compromised blood supply to the skin, such as patients who underwent multiple facelifts in the past. Thin skin and soft tissue weigh less. Thus, the effect of the pull on thin-skinned patients would be greater than that of Asian patients in our study, whose skin was thicker and heavier. For patients who had multiple facelift surgeries, our noninvasive technique would not disturb the remaining blood vessels and therefore, would be ideal for these patients.
CONCLUSION
From a limited sideburn incision, the SMAS, the superficial adipose layer, and the dermis are sequentially pulled to give a lifting effect on the lateral midface. The vertical fibrous septa connecting the SMAS, the superficial adipose layer, and the dermis are not disrupted in our technique. Therefore, the combined pulling forces applied to these tissues deliver a composite tissue elevation. These tissues are fixed to the temporalis muscle fascia at the posterior hairline incision site. Therefore, there is minimal tension on the sideburn hairline incision site. Our limited-incision/minimally invasive technique is applicable to patients who desire improvement of the nasolabial fold and the lateral midface with a fast recovery time.
Supplementary Material
Footnotes
The patients provided written informed consent for the publication and the use of their images.
The authors report no conflicts of interest.
Supplemental Digital Content is available for this article. Direct URL citations are provided in the HTML and PDF versions of this article on the journal’s website, www.jcraniofacialsurgery.com.
Contributor Information
Jin Suk Byun, Email: jinsuk.byun55@gmail.com.
Kenneth K. Kim, Email: kennethkimmd@gmail.com.
REFERENCES
- 1. Byun JS, Hwang K, Lee SY, et al. Forces required to pull the superficial fascia in facelifts. Plast Surg 2018;26:40–45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Wanitphakdeedecha R, Yan C, Apinuntham C. Intradermal micro-dosing of abobotulinumtoxin a for face-lifting: how long does it last? Dermatol Ther 2020;10:779–789 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Gassia V, Beylot C, Béchaux S, et al. Botulinum toxin injection techniques in the lower third and middle of the face, the neck and the décolleté: the “Nefertiti lift”. Ann Dermatol Venereol 2009;136:111–118 [DOI] [PubMed] [Google Scholar]
- 4. Youn CS, Hong JY, Park KY, et al. A review of hydrolifting: a new modality for skin rejuvenation. J Cosmet Laser Ther 2018;20:28–33 [DOI] [PubMed] [Google Scholar]
- 5. Xi W, Han S, Feng S, et al. The injection for the lower eyelid retraction: a mechanical analysis of the lifting effect of the hyaluronic acid. Aesth Plast Surg 2019;43:1310–1317 [DOI] [PubMed] [Google Scholar]
- 6. Sunghee K, Moonjong K. Trends of noninvasive radiofrequency and minimally invasive treatment for the management of facial aging. J Cosmet Dermatol Sci Appl 2019;9:30–40 [Google Scholar]
- 7. Dendle Julia BA, Wu Douglas C, Fabi Sabrina G, et al. A retrospective evaluation of subsurface monopolar radiofrequency for lifting of the face, neck, and jawline. Dermatol Surg 2016;42:1261–1265 [DOI] [PubMed] [Google Scholar]
- 8. Gülbitti Haydar Aslan, Colebunders Britt, Pirayesh Ali, et al. Thread-lift sutures: still in the lift? A systematic review of the literature. Plast Reconstr Surg 2018;141:341e–347e [DOI] [PubMed] [Google Scholar]
- 9. Karimi K, Reivitis A. Lifting the lower face with an absorbable polydioxanone (PDO) thread. J Drugs Dermatol 2017;16:932–934 [PubMed] [Google Scholar]
- 10. Massiha H. Short-scar face lift with extended SMAS platysma dissection and lifting and limited skin undermining. Plast Reconstr Surg 2003;112:663–669 [DOI] [PubMed] [Google Scholar]
- 11. Tonnard P, Verpaele A, Monstrey S, et al. Minimal access cranial suspension lift: a modified S-lift. Plast Reconstr Surg 2002;109:2074–2086 [DOI] [PubMed] [Google Scholar]
- 12. Warren R, Aston S, Mendelson B. Face lift. Plast Reconstr Surg 2011;128:747e–764ee [DOI] [PubMed] [Google Scholar]
- 13. Gosain A, Yousif J, Madiedo G, et al. Surgical anatomy of the SMAS a reinvestigation. Plast Reconstr Surg 1993;92:1254–1263 [PubMed] [Google Scholar]
- 14. Barton F. The SMAS and the nasolabial fold. Plast Reconstr Surg 1992;89:1054–1057 [PubMed] [Google Scholar]
- 15. Har-Shai Y, Bodner S, Egozy-Golan D, et al. Mechanical properties and microstructure of the superficial musculoaponeurotic system. Plast Reconstr Surg 1996;98:59–70 [DOI] [PubMed] [Google Scholar]
- 16. Kim BJ, Choi JH, Lee YH. Development of facial rejuvenation procedures: thirty years of clinical experiences with face lifts. Arch Plat Surg 2015;42:521–531 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Baker TJ, Stuzin JM. Personal technique of face lifting. Plast Reconstr Surg 1997;100:502–508 [DOI] [PubMed] [Google Scholar]
- 18. Skoog T. Plastic Surgery. Philadelphia, PA: Saunders; 1974. [Google Scholar]
- 19. Hamra ST. Composite rhytidectomy. Plast Reconstr Surg 1992;90:1–13 [DOI] [PubMed] [Google Scholar]
- 20. Hamra ST. The zygorbicular dissection in composite rhytidectomy: An ideal midface plane. Plast Reconstr Surg 1998;102:1646–1657 [DOI] [PubMed] [Google Scholar]
- 21. Mendelson B. Surgery of the superficial musculoaponeurotic system: principles of realease, vectors, and fixation. Plast Reconstr Surg 2001;107:1545–1552 [PubMed] [Google Scholar]
- 22. Barton FE, Jr, Hunt J. The high-superficial aponeurotic system technique in facial rejuvenation: an update. Plast Reconstr Surg 2003;112:1910–1917 [DOI] [PubMed] [Google Scholar]
- 23. Stuzin JM, Baker TJ, Gordon HL, et al. Extended SMAS dissection as an approach to midface rejuvenation. Clin Plast Surg 1995;22:295–311 [PubMed] [Google Scholar]
- 24. Macchi V, Tiengo C, Porzionato A, et al. Histotopographic study of the fibroadipose connective cheek system. Cells Tissues Organs 2010;191:47–56 [DOI] [PubMed] [Google Scholar]
- 25. Nakajima H, Imanishi N, Kishi K, et al. Anatomical study of subcutaneous adipofascial tissue: a concept of the protective adipofascial system (PAFS) and lubricant adipofascial system (LAFS). Scand J Plast Reconstr Surg Hand Surg 2004;38:261–266 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.