Abstract
Purpose
AirSeal is a valve-less trocar insufflation system which is widely used in robotic urologic surgeries. More evidence is needed concerning the application and cost of AirSeal in retroperitoneal robot-assisted laparoscopic partial nephrectomy.
Methods
We conducted a randomized controlled trial enrolling 62 patients who underwent retroperitoneal robot-assisted laparoscopic partial nephrectomy from February 2022 to February 2023 in the Peking Union Medical College Hospital. Patients were randomly assigned into AirSeal insufflation (AIS) group and conventional insufflation (CIS) group. The primary outcome was the rate of subcutaneous emphysema (SCE).
Results
The SCE rate in the AIS group (12.9%) was significantly lower than that in the CIS group (35.5%) (P = 0.038). Lower maximum end-tidal carbon dioxide (CO2) (41 vs 45 mmHg, P = 0.011), PaCO2 at the end of the operation (40 vs 45 mmHg, P < 0.001), maximum tidal volume (512 vs 570 ml, P = 0.003), frequency of lens cleaning (3 vs 5, P < 0.001), pain score at 8 h (3 vs 4, P = 0.025), 12 h (2 vs 3, P = 0.029) postoperatively and at time of discharge (1 vs 2, P = 0.002) were observed in the AIS group, despite a higher hospitalization cost (68,197 vs 64658RMB, P < 0.001). Logistic regression analysis identified insufflation approach was the only influencing factor for the occurrence of SCE events.
Conclusion
AirSeal insufflation system exhibited similar efficacy and improved safety for retroperitoneal robot-assisted laparoscopic partial nephrectomy than conventional insufflation system, despite an affordable increase of hospitalization costs.
Keywords: AirSeal, Insufflation system, Robotic surgery, Partial nephrectomy, Renal cell carcinoma
Introduction
The incidence of renal cell carcinoma (RCC) is increasing, with approximately 400,000 new cases per year worldwide [1]. Partial nephrectomy is recommended for RCC whenever surgically applicable according to the latest European Association of Urology guideline [2]. Robot-assisted laparoscopic partial nephrectomy has been the standard approach to partial nephrectomy [3, 4] and shown an advantage over laparoscopic and open partial nephrectomy [5, 6].
For robot-assisted laparoscopic partial nephrectomy, a stable pneumocavity is critical. Conventional insufflation system utilized a one-way valve trocar to place instruments into the pneumocavity while maintaining insufflation [7]. However, a significant loss of insufflation may occur when passing instruments through the trocar or sucking smoke. Meanwhile, continuous insufflation may result in pressure spikes since the conventional insufflation system is closed [8]. Unstable pneumoperitoneum can cause the collapse of pneumocavity and moisture accumulation at the camera lens, thus disrupting the exposure of surgical field, prolonging operation time and increasing the risk of accidental injury. Furtherly, prolonged operation time can lead to excess absorption of carbon dioxide (CO2) which contributes to insufflation-related complications including subcutaneous emphysema (SCE) and shoulder pain [9, 10].
AirSeal is a three-lumen trocar insufflation system which creates a valve-less pressure curtain by continuous pressure flow [11]. The system can respond to the slight change of intra-abdominal pressure and create stable insufflation. Previous studies have shown that the system can improve visualization of the surgical field, enable continuous smoke sucking and reduce CO2 absorption and consumption [12, 13]. In the field of urologic surgery, AirSeal system has exhibited superiority over conventional insufflation system in robot-assisted laparoscopic nephrectomy [8, 14–16], prostatectomy [17, 18] and cystectomy [19].
Previous studies have fully investigated the efficacy and safety of AirSeal insufflation system in robot-assisted laparoscopic partial nephrectomy. However, special attention should be paid on retroperitoneal robot-assisted laparoscopic partial nephrectomy since the retroperitoneal cavity is more confined compared to transperitoneal cavity. Besides, there has been no evidence on the cost of AirSeal system in robotic urologic surgery.
Therefore, to shed further light upon the application of AirSeal in robot-assisted laparoscopic partial nephrectomy, we conducted a single-center, randomized controlled trial comparing the efficacy, safety and cost of AirSeal versus conventional insufflation system in robot-assisted laparoscopic partial nephrectomy via retroperitoneal approach.
Materials and methods
The study was centrally approved by the Ethics Committee in accordance with the Declaration of Helsinki. The Approval Number was I-22PJ903.
Patients
We prospectively enrolled patients who underwent retroperitoneal robot-assisted laparoscopic partial nephrectomy from February 2022 to February 2023 in the Peking Union Medical College Hospital. The inclusion criteria were as follows: (1) patients were aged between 18 and 80 years; (2) patients were diagnosed as a single renal lesion with a size within 6 cm; (3) patients were planned to undergo retroperitoneal robot-assisted laparoscopic partial nephrectomy; (4) patients were capable to give informed consent. Patients with active systemic or cutaneous infection, pre-existing immunodeficiency disorder and/or chronic use of systemic steroids, uncontrolled diabetes mellitus, ascites, body mass index (BMI) greater than 45 kg/m2 or less than 18 kg/m2, severe co-existing morbidities, significant anaemia with haemoglobin (Hb) less than 10 g/dl, renal insufficiency with creatine (CREA) greater than 2.5 mg/dl, and significant history of bleeding diathesis, coagulopathy or von Willebrand’s disease were excluded from enrolment. Females who were pregnant or planning to become pregnant within 3 months of surgery, or lactating were also excluded.
Randomization and masking
Patients were randomly assigned in a 1:1 ratio into AirSeal insufflation (AIS) group and conventional insufflation (CIS) group. Randomization was performed by an online random number generator (www.random.org) with clinical team and research staffs masked. Though the surgical procedure could not be masked due to different insufflator appearances, the pathological diagnosis, inpatient care, outpatient follow-up and statistical analysis were all masked.
Data collection and outcomes
Patients’ clinical characteristics including sex, age, BMI, history of smoking, hypertension and diabetes, Charlson comorbidity index (CCI), side and size of the tumour lesion, and RENAL score were collected.
The primary outcome was the rate of SCE assessed by the surgeon at the end of the operation. SCE was categorized as “clinically significant” (as determined by measurement at neck or head level), “subclinical” (only seen around port sites or to chest level), or not present [15]. Secondary outcomes included operation time (from the time when the pneumoperitoneum was established to the time when the pneumoperitoneum was finished), warm ischemia time, blood loss, maximum peak airway pressure, maximum end-tidal CO2, PaCO2 at the end of the operation, maximum tidal volume, the frequency of lens cleaning, perioperative Hb difference, perioperative CREA difference, pain score evaluated by visual analog scale and obtained at 4, 8, 12 h postoperatively and at time of discharge, postoperative hospital stay and hospitalization costs. Peak airway pressure, end-tidal CO2 and tidal volume were measured every 15 min during the surgery.
Operations
The da Vinci Xi surgical robot system was used for all patients. The standard pressure was set as 12 mmHg in the AIS group and 15 mmHg in the CIS group. A retroperitoneal 4-port partial nephrectomy was performed in both groups. The AirSeal system is composed of an Intelligent Flow System control unit, one valve-less access port and one contiguous trilumen filter tube set. In the AIS group, a 12-mm AirSeal trocar was placed as the assistant port instead of a regular trocar. All the operations were performed by the same team of surgeon and assistant with a 10-year experience. The patient positioning, port placement, robotic instrument use and detailed surgical procedures were the same as described in our previously published research [20].
Statistical analysis
The sample size calculation was based on the primary outcome of SCE. The one-sided type I error rate was set at 10% and type II error rate set at 20%, giving 80% power. Based upon the previous study [15], we hypothesized that the SCE rate was 38.5% in the CIS group and 15.2% in the AIS group. It was estimated that 62 patients were required. Following randomizing the sample size in a 1:1 ratio, 31 patients were needed in each group.
Continuous variables were presented as median and interquartile range (IQR). Categorical variables were presented as frequency and percentage. Difference test of the primary outcome was conducted using the chi-square test. The secondary outcomes were presented as median and IQR and compared using Mann–Whitney U test. Logistic regression analysis was used to determine factors influencing SCE. Statistical analyses were conducted using SPSS software (version 25, IBM). All tests were two-sided, and P < 0.05 indicated statistical significance.
Results
Patient characteristics
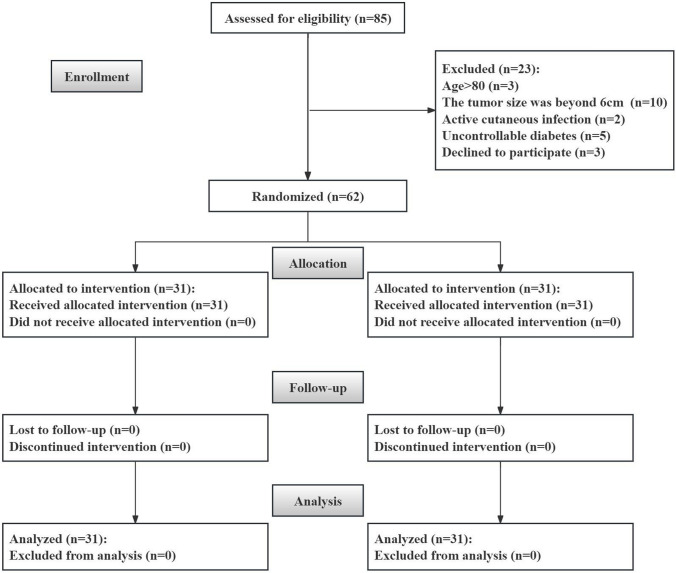
A total of 62 patients were eventually enrolled in the study, with 31 patients in each group. The flow chart of randomization was shown in Fig. 1. Baseline characteristics of the two groups were shown in Table 1. All characteristics were comparable between the two groups. The median age of the whole cohort was 53.0 years (IQR: 46.8–63.3 years). There were 37 men and 25 women. The median tumour size was 3.2 cm (IQR: 2.2–4.3 cm). The median RENAL score was 7 (IQR: 5.8–9). Pathologic analysis showed that all the renal lesions were RCC. All the operations were performed successfully without conversion to open surgery.
Fig. 1.
The flow chart of the study
Table 1.
Baseline characteristics of the CIS group and AIS group
| Characteristics | CIS (n = 31) | AIS (n = 31) |
|---|---|---|
| Sex (man/woman) | 17(54.8)/14(45.2) | 20(64.5)/11(35.5) |
| Age, years | 57(44, 63) | 53(48, 64) |
| BMI, kg/m2 | 24.3(22.6, 27.0) | 25.4(22.7, 27.7) |
| Smoking (yes/no) | 8(25.8)/23(74.2) | 10(32.3)/21(67.7) |
| Hypertension (yes/no) | 18(58.1)/13(41.9) | 14(45.2)/17(54.8) |
| Diabetes (yes/no) | 7(22.6)/24(77.4) | 5(16.1)/26(83.9) |
| CCI | 3(2, 5) | 3(2, 4) |
| Tumor side (left/right) | 16(51.6)/15(48.4) | 15(48.4)/16(51.6) |
| Tumor size, cm | 2.9(2.0, 3.8) | 3.5(2.5, 4.5) |
| RENAL score | 7(5, 9) | 7(6, 9) |
CIS conventional insufflation, AIS AirSeal insufflation, BMI body mass index, CCI Charlson comorbidity index
Outcomes
The incidence rate of SCE, including clinically significant SCE and subclinical SCE, was significantly lower in the AIS group than the CIS group (12.9% vs 35.5%, P = 0.038). Nearly all the SCE events were subclinical but in the CIS group, two patients developed clinically significant SCE extending to neck. They had local discomfort without dyspnoea, distress and chest pain and recovered within one week without surgical or medical intervention. The outcomes were summarized in Table 2. Patients in the AIS group had significantly lower maximum end-tidal CO2 (41 vs 45 mmHg, P = 0.011), PaCO2 at the end of the operation (40 vs 45 mmHg, P < 0.001), maximum tidal volume (512 vs 570 ml, P = 0.003), frequency of lens cleaning (3 vs 5, P < 0.001), pain score at 8 h (3 vs 4, P = 0.025), 12 h (2 vs 3, P = 0.029) postoperatively and at time of discharge (1 vs 2, P = 0.002). However, a higher hospitalization cost was observed in the AIS group (68,197 vs 64,658RMB, P < 0.001). Operation time, warm ischemia time, blood loss, maximum peak airway pressure, perioperative Hb difference, perioperative CREA difference, pain score at 4 h and postoperative hospital stay were comparable between the two groups.
Table 2.
Outcomes of the CIS group and AIS group
| Outcomes | CIS (n = 31) | AIS (n = 31) | P value |
|---|---|---|---|
| Subcutaneous emphysema (yes/no) | 11(35.5%)/20(64.5%) | 4(12.9%)/27(87.1%) | 0.038* |
| Operation time, min | 100(90, 130) | 90(90, 128) | 0.704 |
| Warm ischemia time, min | 20(15, 25) | 19(15, 24) | 0.810 |
| Blood loss, ml | 50(20, 50) | 50(20, 50) | 0.341 |
| Maximum peak airway pressure, mmHg | 24(23, 28) | 23(20, 25) | 0.118 |
| Maximum end-tidal CO2, mmHg | 45(40, 47) | 41(36, 44) | 0.011* |
| PaCO2 at the end of the operation, mmHg | 45(41, 53) | 40(35, 41) | <0.001* |
| Maximum tidal volume, ml | 570(505, 644) | 512(478, 557) | 0.003* |
| Frequency of lens cleaning | 5(5, 5) | 3(3, 3) | <0.001* |
| Perioperative Hb difference, g/L | 17(10, 26) | 15(10, 23) | 0.647 |
| Perioperative CREA difference, μmol/L | 15(9, 23) | 14(5, 29) | 0.485 |
| Pain score at 4h | 5(3, 8) | 4(3, 6) | 0.144 |
| Pain score at 8h | 4(3, 7) | 3(3, 4) | 0.025* |
| Pain score at 12h | 3(2, 5) | 2(2, 4) | 0.029* |
| Pain score at time of discharge | 2(1, 3) | 1(1, 2) | 0.002* |
| Postoperative hospital stay, day | 5(4, 6) | 5(4, 6) | 0.959 |
| Hospitalization costs, RMB | 64658(62636, 69181) | 68197(66162, 70543) | <0.001* |
CIS conventional insufflation, AIS AirSeal insufflation, CO2 carbon dioxide, Hb hemoglobin, CREA creatine
*Statistically significant at α = 0.05
Factors influencing the occurrence of SCE
As shown in Table 3, univariable logistic regression analysis revealed that insufflation approach was the only influencing factor for the occurrence of SCE events (OR = 4.263; 95% CI 1.192–15.252; P = 0.026).
Table 3.
Logistic regression analysis for factors influencing SCE
| Characteristics | Univariable analysis | ||
|---|---|---|---|
| β | OR (95% CI) | P value | |
| Sex (man) | −0.191 | 0.827 (0.261, 2.615) | 0.746 |
| Age, years | −0.010 | 0.990 (0.945, 1.036) | 0.658 |
| BMI, kg/m2 | 0.183 | 1.201 (0.979, 1.474) | 0.080 |
| Smoking (no) | −0.531 | 0.588 (0.176, 1.967) | 0.389 |
| Hypertension (no) | 0.087 | 1.091 (0.350, 3.404) | 0.881 |
| Diabetes (no) | 1.551 | 4.714 (0.558, 39.853) | 0.155 |
| CCI | −0.123 | 0.885 (0.608, 1.287) | 0.522 |
| Tumor side (left) | −0.338 | 0.713 (0.227, 2.240) | 0.562 |
| Tumor size, cm | 0.122 | 1.130 (0.720, 1.775) | 0.595 |
| RENAL score | 0.096 | 1.101 (0.805, 1.507) | 0.548 |
| Insufflation approach (CIS) | 1.450 | 4.263 (1.192, 15.252) | 0.026* |
SCE subcutaneous emphysema, OR odds ratio, CI confidence interval, BMI body mass index, CCI Charlson comorbidity index, CIS conventional insufflation system
*Statistically significant at α = 0.05.
Discussion
To further illustrate the role of the application of AirSeal in robot-assisted laparoscopic partial nephrectomy, we prospectively enrolled 62 RCC patients who underwent retroperitoneal robot-assisted laparoscopic partial nephrectomy using conventional or AirSeal insufflation system. Results revealed that AirSeal insufflation system exhibited less SCE rate, end-tidal CO2, PaCO2, tidal volume, frequency of lens cleaning, and postoperative pain compared to conventional insufflation system, despite a higher hospitalization cost.
Retroperitoneal approach is widely used in robot-assisted laparoscopic partial nephrectomy [21]. Compared to transperitoneal approach, the space of retroperitoneal cavity is smaller and less distensible [22]. Therefore, a stable pneumoperitoneum is more essential for a better exposure of the surgical field and the smooth running of the operation. AirSeal insufflation system can ensure a stable pneumoperitoneum with sustaining smoke evacuation during surgery, providing a useful tool for robotic retroperitoneal partial nephrectomy. However, despite the less frequency of lens cleaning in the AIS group, our study found no significant differences in operation time, warm ischemia time and blood loss between the AIS and CIS groups. The rich experience of the surgical team and the relatively small size and common complexity of the tumour lesions may explain this.
Besides, given the lack of the peritoneum lining, the inflated air can spread within the retroperitoneal tissues and furtherly into loose subcutaneous layer. Therefore, retroperitoneal approach can cause a higher SCE rate than transperitoneal approach [15]. This disadvantage may be overcome to some extent since AirSeal can allow a lower pre-set pneumoperitoneum pressure and reduce the occurrence of pressure spikes. Our study reported a SCE rate of 12.9% in the AIS group, similar to 15.2% in the previous study [15], significantly lower than 35.5% in the CIS group. Moreover, insufflation approach was an independent influencing factor for the occurrence of SCE events.
In terms of CO2 pressure, unstable pneumoperitoneum can cause increased CO2 absorption and higher end-tidal CO2 and PaCO2 which are associated with reduced venous flow and respiratory compliance [23]. More tidal volume is needed to expel excess CO2. In addition, a higher CO2 pressure may contribute to overstretching of the diaphragmatic muscle fibres and postoperative shoulder pain [9]. Our study observed less end-tidal CO2, PaCO2, tidal volume and postoperative pain in the AIS group, indicating the advantage of AirSeal insufflation system in reducing CO2 absorption.
Until now, there have been three major studies investigating the efficacy and safety of AirSeal insufflation system for robot-assisted laparoscopic partial nephrectomy [14–16], including two randomized controlled trials and one prospective cohort study. Filippo Annino et al. firstly compared the AirSeal with a standard insufflator system and found that patients in the AirSeal group had shorter operative time and warm ischemia time [14]. A large prospective randomized clinical trial demonstrated that 12 mmHg AirSeal insufflation improved intraoperative cardiopulmonary parameters and safety profile compared to 15 mmHg AirSeal insufflation and conventional insufflation in robot-assisted laparoscopic partial nephrectomy [15]. Feng et al. also noted that 12 mmHg AirSeal insufflation was associated with reduced risk of SCE and shoulder pain in robot-assisted laparoscopic partial nephrectomy [16]. Besides, retroperitoneal surgical approach was a significant predictor for developing SCE, possibly due to ease of CO2 tracking without barriers as peritoneum in transperitoneal approach. In comparison with previous studies, we first adopted PaCO2 as a secondary outcome. PaCO2 is usually measured via extraction of arterial blood and can reflect a more precise level of intracorporal CO2 than end-tidal CO2 [24]. Besides, we firstly investigated the cost of AirSeal insufflation system. A difference of 3539RMB (about 5% of the total hospitalization costs) in hospitalization costs between AIS and CIS groups was observed, which was affordable for the majority of Chinese patients.
Our current study has several strengths. Unlike previous studies evaluating AirSeal insufflation system for robot-assisted laparoscopic partial nephrectomy, we focused on patients undergoing retroperitoneal approach. Besides, as mentioned above, we first adopted PaCO2 and hospitalization costs as secondary outcomes, providing more insights for the role of AirSeal insufflation system. However, there are several limitations in our study as well. First, the sample size of our study was relatively small. Large randomized controlled trials are needed to provide more solid evidence on this issue. Second, our result for hospitalization costs is only suitable for Chinese patients. For patients from other regions, the cost of AirSeal should be re-evaluated. Third, the median tumour size was only 3.2 cm and the median RENAL score was only 7, reflecting a relatively medium difficulty of partial nephrectomy in our study. Besides, the surgical team had a 10-year surgical experience. Whether AirSeal insufflation system is efficacious and safe for more challenging RCC and less experienced surgical teams is to be determined.
In summary, our randomized controlled trial comparing AirSeal against conventional insufflation system demonstrated similar efficacy and improved safety of AirSeal insufflation system for retroperitoneal robot-assisted laparoscopic partial nephrectomy, despite an affordable increase of hospitalization costs.
Acknowledgements
This study was supported by grants from the National High Level Hospital Clinical Research Funding (No. 2022-PUMCH-A-150).
Author’s contribution
Wei MC: Project development, Data collection, Manuscript writing. Yang WJ: Data collection, Data analysis. Zhou JM: Project development, Manuscript writing. Ye ZX: Data collection, Data management. Ji ZG: Project development, Manuscript editing. Xu WF: Project development, Data management, Manuscript editing. Dong J: Project development, Data management, Manuscript editing.
Funding
This study was supported by grants from the National High Level Hospital Clinical Research Funding (No. 2022-PUMCH-A-150).
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethics approval
The study was centrally approved by the ethics committee in accordance with the Declaration of Helsinki. The approval number was I-22PJ903.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Bray F, Ferlay J, Soerjomataram I et al (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68:394–424 [DOI] [PubMed] [Google Scholar]
- 2.Ljungberg B, Albiges L, Abu-Ghanem Y et al (2022) European association of urology guidelines on renal cell carcinoma: the 2022 update. Eur Urol 82:399–410 [DOI] [PubMed] [Google Scholar]
- 3.Antonelli A, Cindolo L, Sandri M et al (2022) Is off-clamp robot-assisted partial nephrectomy beneficial for renal function? Data from the CLOCK trial. BJU Int 129:217–224 [DOI] [PubMed] [Google Scholar]
- 4.Antonelli A, Cindolo L, Sandri M et al (2020) Safety of on- vs off-clamp robotic partial nephrectomy: per-protocol analysis from the data of the CLOCK randomized trial. World J Urol 38:1101–1108 [DOI] [PubMed] [Google Scholar]
- 5.Hoeh B, Wenzel M, Eckart O et al (2023) Comparison of peri- and intraoperative outcomes of open vs robotic-assisted partial nephrectomy for renal cell carcinoma: a propensity-matched analysis. World J Surg Oncol 21:189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Calpin GG, Ryan FR, McHugh FT et al (2023) Comparing the outcomes of open, laparoscopic and robot-assisted partial nephrectomy: a network meta-analysis. BJU Int. 10.1111/bju.16093 [DOI] [PubMed] [Google Scholar]
- 7.Hausner K (1998) Kurt Semm and an automatic insufflator. JSLS 2:395 [PMC free article] [PubMed] [Google Scholar]
- 8.Bucur P, Hofmann M, Menhadji A et al (2016) Comparison of pneumoperitoneum stability between a valveless trocar system and conventional insufflation: a prospective randomized trial. Urology 94:274–280 [DOI] [PubMed] [Google Scholar]
- 9.Nyerges A (1994) Pain mechanisms in laparoscopic surgery. Semin Laparosc Surg 1:215–218 [DOI] [PubMed] [Google Scholar]
- 10.Zhao LC, Han JS, Loeb S et al (2008) Thoracic complications of urologic laparoscopy: correlation between radiographic findings and clinical manifestations. J Endourol 22:607–614 [DOI] [PubMed] [Google Scholar]
- 11.Nepple KG, Kallogjeri D, Bhayani SB (2013) Benchtop evaluation of pressure barrier insufflator and standard insufflator systems. Surg Endosc 27:333–338 [DOI] [PubMed] [Google Scholar]
- 12.Herati AS, Andonian S, Rais-Bahrami S et al (2011) Use of the valveless trocar system reduces carbon dioxide absorption during laparoscopy when compared with standard trocars. Urology 77:1126–1132 [DOI] [PubMed] [Google Scholar]
- 13.Luketina RR, Knauer M, Köhler G et al (2014) Comparison of a standard CO2 pressure pneumoperitoneum insufflator versus AirSeal: study protocol of a randomized controlled trial. Trials 15:239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Annino F, Topazio L, Autieri D et al (2017) Robotic partial nephrectomy performed with Airseal versus a standard CO(2) pressure pneumoperitoneum insufflator: a prospective comparative study. Surg Endosc 31:1583–1590 [DOI] [PubMed] [Google Scholar]
- 15.Desroches B, Porter J, Bhayani S et al (2021) Comparison of the safety and efficacy of valveless and standard insufflation during robotic partial nephrectomy: a prospective, randomized, multi-institutional trial. Urology 153:185–191 [DOI] [PubMed] [Google Scholar]
- 16.Feng TS, Heulitt G, Islam A et al (2021) Comparison of valve-less and standard insufflation on pneumoperitoneum-related complications in robotic partial nephrectomy: a prospective randomized trial. J Robot Surg 15:381–388 [DOI] [PubMed] [Google Scholar]
- 17.George AK, Wimhofer R, Viola KV et al (2015) Utilization of a novel valveless trocar system during robotic-assisted laparoscopic prostatectomy. World J Urol 33:1695–1699 [DOI] [PubMed] [Google Scholar]
- 18.La Falce S, Novara G, Gandaglia G et al (2017) Low pressure robot-assisted radical prostatectomy with the airseal system at OLV Hospital: results from a prospective study. Clin Genitourin Cancer 15:e1029–e1037 [DOI] [PubMed] [Google Scholar]
- 19.Covotta M, Claroni C, Torregiani G et al (2017) A prospective, randomized, clinical trial on the effects of a valveless trocar on respiratory mechanics during robotic radical cystectomy: a pilot study. Anesth Analg 124:1794–1801 [DOI] [PubMed] [Google Scholar]
- 20.Li X, Xu W, Fan S et al (2023) Robot-assisted partial nephrectomy with the newly developed kangduo surgical robot versus the da vinci si surgical system: a double-center prospective randomized controlled noninferiority trial. Eur Urol Focus 9:133–140 [DOI] [PubMed] [Google Scholar]
- 21.Carbonara U, Simone G, Minervini A et al (2021) Outcomes of robot-assisted partial nephrectomy for completely endophytic renal tumors: a multicenter analysis. Eur J Surg Oncol 47:1179–1186 [DOI] [PubMed] [Google Scholar]
- 22.Ng CS, Gill IS, Ramani AP et al (2005) Transperitoneal versus retroperitoneal laparoscopic partial nephrectomy: patient selection and perioperative outcomes. J Urol 174:846–849 [DOI] [PubMed] [Google Scholar]
- 23.Mertens zur Borg IR, Lim A, Verbrugge SJ, et al (2004) Effect of intraabdominal pressure elevation and positioning on hemodynamic responses during carbon dioxide pneumoperitoneum for laparoscopic donor nephrectomy: a prospective controlled clinical study. Surg Endosc 18:919–923 [DOI] [PubMed] [Google Scholar]
- 24.Kalmar AF, Foubert L, Hendrickx JF et al (2010) Influence of steep Trendelenburg position and CO(2) pneumoperitoneum on cardiovascular, cerebrovascular, and respiratory homeostasis during robotic prostatectomy. Br J Anaesth 104:433–439 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.