Abstract
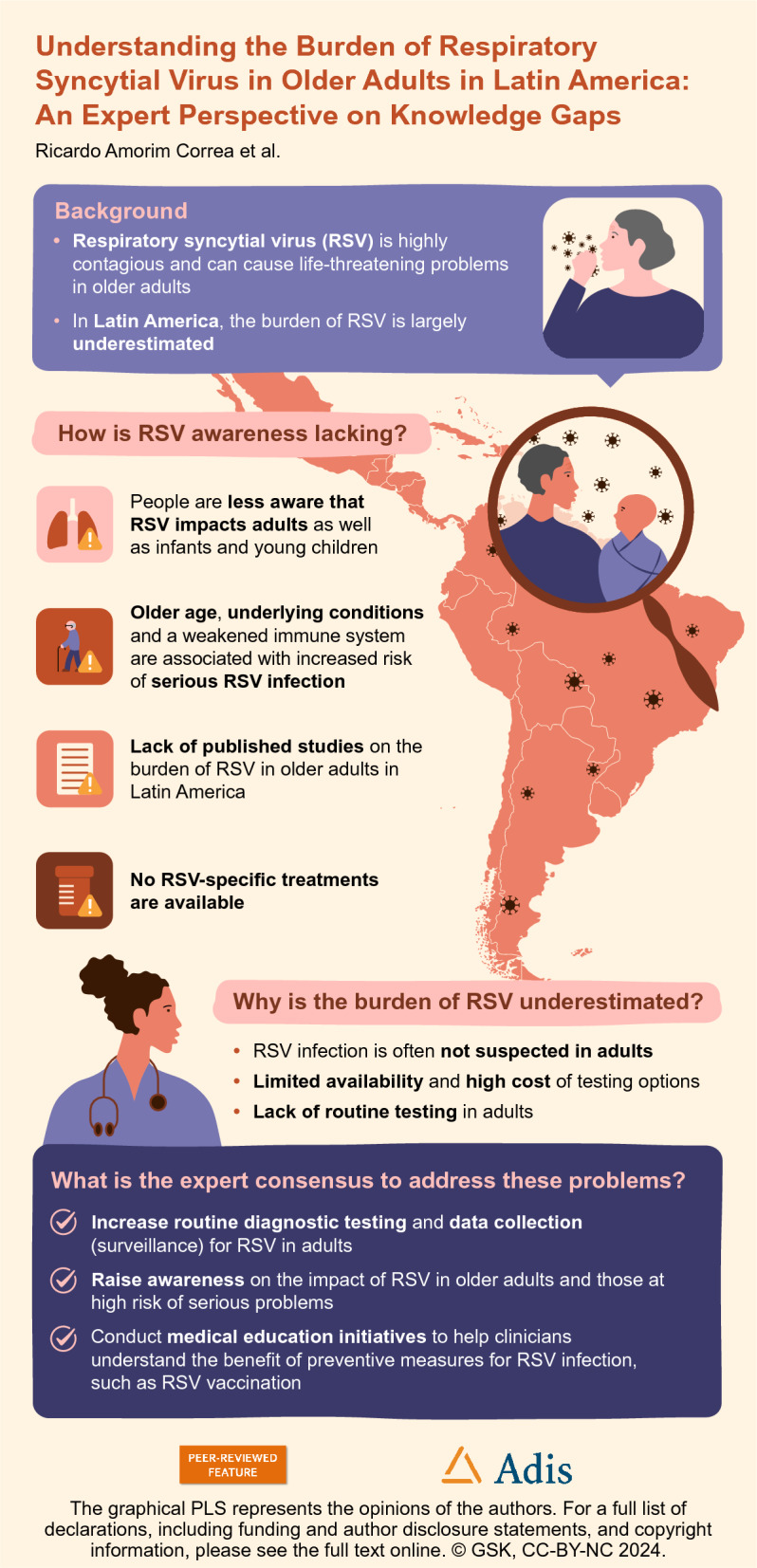
Respiratory syncytial virus (RSV) is a significant global health concern and major cause of hospitalization, particularly among infants and older adults. The clinical impact of RSV is well characterized in infants; however, in many countries, the burden and risk of RSV in older populations are overlooked. In Latin America, there are limited data on RSV epidemiology and disease management in older adults. Therefore, the impact of RSV in this region needs to be addressed. Here, current insights on RSV infections in older populations in Latin America, including those with underlying health conditions, are discussed. We also outline the key challenges limiting our understanding of the burden of RSV in Latin America in a worldwide context and propose an expert consensus to improve our understanding of the burden of RSV in the region. By so doing, we aim to ultimately improve disease management and outcomes of those at risk and to alleviate the impact on healthcare systems.
A graphical plain language summary is available with this article.
Graphical Plain Language Summary
Keywords: Respiratory syncytial virus, RSV, Latin America, Epidemiology, Consensus, Disease burden, Vaccination
Key Summary Points
| Respiratory syncytial virus (RSV) is a highly contagious virus that is a recognized global health concern; however, our understanding of the burden of RSV in Latin America is limited, particularly among older adults and those with underlying health conditions. |
| In light of this, we provide an overview of the available data on RSV in Latin America, highlight significant epidemiological challenges, and propose an expert consensus on the efforts needed to improve our understanding of RSV and alleviate its burden in the region. |
| Overall, we found a substantial lack of epidemiological data on RSV in Latin America and discuss its potential underestimated prevalence due to underdiagnosis and limited surveillance, as well as its considerable impact in older adults and those with comorbidities, on the basis of insights from other regions. |
| Considering these findings, we advocate for routine testing of RSV, medical education initiatives to inform clinicians on RSV in older adults, and the development of a surveillance taskforce to accurately monitor the burden of RSV in Latin America. |
Digital Features
This article is published with digital features, including a graphical plain language summary, to facilitate understanding of the article. To view digital features for this article, go to 10.6084/m9.figshare.24989493.
Introduction
Respiratory infections pose a significant global health challenge, particularly among older adults and those with underlying health conditions [1–5]. Respiratory syncytial virus (RSV) is a highly contagious viral pathogen that is a well-known health concern among infants and young children. The burden and risk of RSV in older adults, however, are often underestimated, despite being recognized by the World Health Organization (WHO) [6]. In 2023, the USA Food and Drug Administration (FDA) granted approval for the use of two RSV vaccines for the prevention of lower respiratory tract disease caused by RSV in adults aged ≥ 60 years, as recommended by the Advisory Committee on Immunization Practices (ACIP) [7]. In addition to older age, the ACIP also recently recognized the significant risk of severe RSV disease among individuals with underlying chronic health conditions, including cardiovascular and lung diseases [7]. These recommendations mark a significant public health milestone in preventing RSV infection, which can be life-threatening in older adults [8].
In Latin America, there are notable gaps in the data on the epidemiology and management of RSV, especially among older adults [9]. Respiratory infections, including RSV, have been shown to impose a substantial societal and economic burden in Latin America with respect to both public health and productivity [10, 11]. Here, we outline the key challenges in understanding the burden of RSV, with a focus on older adults and those with underlying health conditions. We outline an expert consensus that aims to help promote healthy aging and relieve the burden of RSV on healthcare systems across Latin America [12].
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Awareness of RSV and Its Impact in Latin America
RSV is an acute respiratory infection and is highly contagious in all age groups [13]. One of the greatest challenges faced in the management and prevention of RSV infections in Latin America is the lack of disease awareness among healthcare professionals (HCPs) on the impact of RSV in older adults (aged ≥ 60 years) [14]. A global survey conducted in 2021, including HCPs and researchers from Argentina and Brazil, reported that knowledge on RSV was low and that its public health impact in older populations was not fully recognized in their countries [14]. Furthermore, according to a systematic review of RSV in Latin America, HCPs in the region often do not consider RSV infection to be a primary cause of respiratory illness in adults aged > 65 years [15]. This is a cause for concern as the Pan American Health Organization (PAHO) and WHO have reported increasing RSV activity among pediatric populations in Latin American countries in 2023, compared with previous years [16].
The lack of awareness of RSV in Latin America is in stark contrast to other infectious diseases, such as coronavirus disease 2019 (COVID-19) and influenza, for which HCPs’ and the public’s knowledge, attitudes, and practices have been well established since the latest pandemic. A survey of 251 HCPs residing in 19 Latin American countries during the COVID-19 pandemic reported that 77% had engaged in institutional training, resulting in enhanced knowledge of the disease [17]. Another survey of the general public in Latin America demonstrated that almost all respondents (99%) were aware of the common symptoms associated with COVID-19, as well as its mode of transmission (93%) and how to recognize nonspecific symptoms (93%) [18]. However, general awareness of RSV in Latin America may be increasing, following the publication of pivotal studies and RSV health initiatives in other countries, such as the approval of preventative vaccine options in the USA and Europe [7, 19–24].
A primary cause behind the lack of RSV awareness is the absence of comprehensive, published studies in Latin America. A systematic literature review, published in 2020, on RSV epidemiology in adults identified 18 relevant articles in Latin America, of which 5 (28%) carried a high risk of bias and 4 (22%) an intermediate risk for over- or underestimating RSV prevalence [9]. While these studies documented RSV as a cause of illness among adults in Latin America presenting with acute respiratory infections (ARIs), influenza-like illnesses (ILIs), or community-acquired pneumonia (CAP), there was clear variation in the prevalence data reported across studies, including within the same country [9]. These differences may be a consequence of biases, variable RSV seasons across the region, and short study lengths as well as a lack of routine testing and a common definition for RSV infections [9].
Cohort-based and surveillance studies of respiratory tract infections have been conducted in Latin America, which can provide invaluable insights into RSV, including the seasonality and incidence of RSV subtypes [25–31]. However, the impact of age and comorbid health conditions on RSV epidemiology remains a topic that needs addressing, as highlighted by various studies across Latin America [30, 32, 33]. The scarcity of RSV epidemiological data in older adults may be a consequence of several factors. Two contributing factors, among the others discussed throughout this consensus, include the heterogeneity of older populations and potential age bias in research. Compared with younger cohorts, older adults have highly variable health states, cognitive abilities, and socioeconomic backgrounds; therefore, designing studies that capture this diversity and produce generalizable results is a challenge. Additionally, age biases are important to consider in research, whereby studies in older adults may be neglected owing to notions of low importance or clinical impact. The presence of age-related stereotypes, leading to the generalization that all older adults are frail, cognitively impaired, or have a lack of interest, can also discourage participation from both researchers and older adults themselves. Despite these potential challenges, there is growing recognition of the importance of research on older adults [34], particularly as the aging population is increasing worldwide; hence, the health and well-being of older adults is of key interest.
The significance of generating new information focusing on adults from Latin American countries is paramount, as it will serve as a foundation for initiating discussions with patients, HCPs, and policymakers on the impact of RSV. The observed changes in RSV seasonality during and following the global COVID-19 pandemic further warrant the need for up-to-date, local data [16, 35, 36]. Accumulating comprehensive regional data on RSV infection in adult patients is vital to drive routine testing of RSV by HCPs and to prompt changes in healthcare policies and clinical practice guidelines.
While such data are not available, insights on RSV epidemiology can be taken from other geographical regions. Existing data from Asian, European, and North American countries have demonstrated the substantial burden of RSV in the adult population, especially in patients aged ≥ 60 years [34, 37, 38] and those with underlying health conditions [39–42]. This information should be leveraged to raise awareness on the potential burden of RSV, as similar epidemiology is expected in Latin America on the basis of the limited local data currently available.
Investing in medical educational activities, updating training programs for health specialists and general practitioners, and conducting scientific meetings and patient-focused awareness campaigns will be vital to disseminate key knowledge on RSV infection in Latin America and support informed decision-making by HCPs and patients on the need to be protected against RSV. Examples of online, patient-focused medical education on the risks of RSV include articles published by the American Heart Association and the Centers for Disease Control and Prevention [43, 44]. Efforts to raise both HCP and public awareness of the impact of RSV in the older population should be considered a health priority in Latin America.
Underdiagnosis of RSV
The lack of routine diagnostic testing for RSV in adults is a likely contributor to the scarcity of epidemiological data on RSV among adults in Latin America, compounding the limited awareness of the burden and the prevalence of RSV. The clinical presentation of RSV may vary in older adults compared with younger adults or children, as respiratory airways become larger with age [4]. Therefore, the symptoms of RSV infection could resemble those of other respiratory infections, further complicating initial diagnoses and burden estimations of RSV [9, 45]. While reverse transcription-polymerase chain reaction (RT-PCR) is the gold standard for RSV diagnosis, its widespread use in Latin America is hindered by its cost, limited availability, and need for specialized equipment and expertise [46, 47]. Over recent years, rapid antigen detection test (RADT) options have been made available for RSV; although RADTs have modest sensitivity compared with RT-PCR, they are easy and quick to perform, making them valuable diagnostic tools (particularly in children) where access to RT-PCR may be limited [47, 48]. Early use of RADTs is important, as prolonged symptoms are associated with false-negative test results [49]; however, the cost and necessity of RADTs should also be evaluated. RADT options may be beneficial for future surveillance research, particularly where RT-PCR is not feasible.
Low levels of RSV testing in older adults were documented in the USA prior to the introduction of the two RSV vaccines approved for use in older adults in 2023 [50, 51]. These low rates of diagnostic testing may be due to the perception of RSV as a pediatric disease and the lack of therapeutic options against RSV, which may be limiting diagnostic factors from the perspective of HCPs. However, considering the significant rates of RSV-associated hospitalization, increased utilization of diagnostic testing is key to increase awareness of the risks of RSV among communities and subsequently inform the allocation of resources and research. Research has also suggested that point-of-care testing (POCT) for RSV could improve patient outcomes. A study conducted across emergency departments in Denmark found that patients with a positive POCT result for influenza A/B or RSV were significantly less likely to be treated with antibiotics and had a significantly reduced hospitalization time [52].
It has been reported that low testing rates [50] and inconsistent diagnostic testing characteristics [42, 53] can contribute to an underestimation of RSV incidence and disease burden. A 2023 systematic review of RSV-associated ARIs also reported that the actual burden of RSV-associated hospitalizations could be 2.2 times greater than reported in existing studies, after adjusting for variations in RSV diagnostic characteristics [53].
The level of health coverage and medical care received by patients across demographics in Latin America should also be evaluated; for example, in the experience of the authors, in some healthcare centers, the etiological origin of pneumonia may not be investigated as a result of limited diagnostic capabilities. Medical insurance companies should also be informed on the importance of RSV diagnosis and management and should provide economic support to patients with RSV. In Brazil, influenza and other respiratory diseases are known to have a substantial clinical and economic impact, with higher hospitalization costs associated with older age groups [54]. It is imperative that routine and accurate diagnostic testing and surveillance systems are instituted for RSV and ARIs.
Surveillance and Reporting Challenges
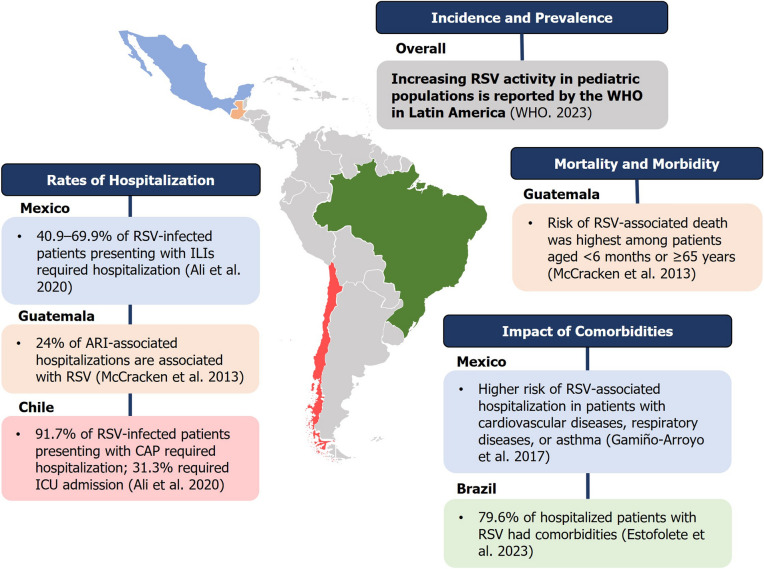
The scarcity and inconsistencies in data collection across healthcare settings pose significant challenges in obtaining comprehensive and accurate evidence on RSV epidemiology in Latin America [9], which are further amplified by the lack of awareness and diagnostic challenges experienced in the region. Substantial data gaps on RSV burden are evidenced throughout Latin America (Fig. 1). Sentinel surveillance of respiratory viruses in Brazil during 2000–2010 recognized the lack of such data but identified a substantial proportion of confirmed RSV infections, which circulated year-round [26]. The Global Epidemiology of RSV (GERi) network, comprising surveillance systems from 16 countries including Brazil, Chile, and Ecuador, has identified that, although the greatest burden of RSV is evident in those aged < 1 year old, there is a notable lack of RSV surveillance data in the older adult population [55].
Fig. 1.
Limited data available on RSV burden in Latin America. Data reported from Refs. [6, 9, 28, 30, 58]. ARI acute respiratory infection, CAP community-acquired pneumonia, ICU intensive care unit, ILI influenza-like illness, RSV respiratory syncytial virus, WHO World Health Organization
The lack of surveillance data in the older adult population may be influenced by a variety of factors that have been previously identified in Western countries; for example, upper respiratory tract sampling, in some cases, cannot detect infections in adults owing to the shorter duration of viral shedding than observed with infants [51]. In addition, the limited availability of RT-PCR for RSV detection and the lack of studies accounting for the seasonality of RSV infections in adult populations may also be factors contributing to the lack of surveillance data [9]. The absence of standardized case definitions for RSV in older adults further complicates surveillance, contributing to difficulties in appropriately stratifying reported cases. Hence, differences in how HCPs diagnose and report RSV cases can produce data that are challenging to compare and analyze across geographical regions [51]. Failure to stratify results by age can also lead to an underestimation of the burden of severe disease in older adults [51].
The PAHO/WHO recommends that Member States strengthen RSV surveillance and adopt measures for the prevention and control of severe outcomes [16]. To address these challenges effectively, we strongly advocate for the establishment of a collective taskforce responsible for ensuring consistent and reliable testing methods, data collection, analysis, and reporting (Table 1). By standardizing these practices, such a taskforce could help to establish uniformity in data collection, testing methodologies, and RSV case definitions for older adults and therefore facilitate necessary, comprehensive analyses. Surveillance should focus on all RSV cases, regardless of severity, to provide an accurate depiction of the local burden. Furthermore, data sharing between communities, healthcare institutions, governmental bodies, and research organizations must be encouraged. A collaborative approach between countries and scientific societies could ultimately contribute to a centralized repository of RSV data, simplifying access, analyses, and reporting at regional and national levels, which are critical to informing policy recommendations.
Table 1.
Key actions to raise awareness and improve understanding of the burden of RSV in Latin America
| Support the availability of accurate diagnostic testing for RSV |
| Increase the levels of routine diagnostic testing for RSV |
| Improve the awareness and knowledge of HCPs regarding the impact of RSV among older adults, particularly those with underlying health conditions, through medical education initiatives |
| Support the formation of a surveillance taskforce to monitor the widespread epidemiology of RSV across all ages |
| Raise awareness on vaccination in older adults as a preventative measure against RSV |
HCPs healthcare professionals, RSV respiratory syncytial virus
Underestimation of RSV Morbidity and Mortality
The morbidity and mortality of RSV are well recognized in infants [55]; however, it is crucial to evaluate its impact in older adults. In the UK, patients aged > 65 years are estimated to account for approximately 79% of RSV-related hospitalizations per average season [56]. A nationwide cost-of-illness study in Germany also indicated that the overall burden of RSV is greater among hospitalized adults versus hospitalized children, with higher risks of severe complications and more costly treatments reported in adults [57]. RSV infections have also been identified as a significant cause of hospitalization in adult populations in Latin America, with older patients at an increased risk for hospitalization versus younger adult patients [9, 30, 32, 58]. Among RSV-positive patients hospitalized with ARIs in Guatemala, the odds of severe outcomes, including intensive care unit (ICU) admission, mechanical ventilation, or death, were highest among those aged < 6 months or ≥ 65 years [58]. Another study in Mexico also reported a significant association between older age and/or the presence of underlying conditions with a higher risk of RSV-related hospitalization [30]. One study in Brazil also reported that ventilatory support was required for 26.1% of RSV-infected patients, as well as high rates of dyspnea (42.1%) and respiratory distress (31.6%) [28]. A summary of studies highlighting the burden of RSV among adults in Latin America is presented in Table 2.
Table 2.
Summary of key studies reporting on the burden of RSV in Latin America
| Country; Ref. | Study type (study period) | Patient population | Key findings | Gaps |
|---|---|---|---|---|
| Mexico, Brazil, Chile, Venezuela, Colombia, and Guatemala; Ali et al. [9] | Systematic literature review (2011–2017) | Patients aged ≥ 18 years | Eighteen articles from six Latin American countries were identified | RSV data in adult populations are lacking in Latin America |
| High or moderate risk of bias was reported for 9/18 articles | Further data among adults with RSV in Latin America are necessary to further understand the burden of RSV | |||
| Rates of RSV detection varied highly among adults with respiratory infections (0–77.9%), influenza-like illness (1.0–16.4%), and community-acquired pneumonia (1.3–13.5%) | ||||
| RSV-infected adults accounted for high proportions of patients hospitalized with ILI (40.9–69.9%) in Mexico and CAP (91.7%) in Guatemala | ||||
| Mexico; Gamiño-Arroyo et al. [30] | Prospective cohort (2010–2014) | Patients aged ≥ 1 month who presented with an ILI | A substantial number of RSV cases (n = 171) were identified among adults across six hospitals | The study was limited to ILI case definitions; therefore, not all patients with RTIs were eligible for inclusion |
| Older adults accounted for high proportions, and increasing age was associated with significantly higher risk, of RSV-associated hospitalization | ||||
| Mexico; Galindo-Fraga et al. [32] | Observational cohort (2010–2011) | Patients aged > 3 months who presented with an ILI | Hospitalization was required for a higher proportion of patients with RSV (56%) than for influenza (29%) and COVID-19 (32%) | Data were limited to patients with clinical manifestation of ILIs |
| Of the hospitalized patients aged ≥ 60 years, those with RSV infection had a mortality rate > 10% | ||||
| Mexico; Noyola et al. [80] | Prospective observational cohort (2010–2014) | Patients infected with one or two viruses | Patients with RSV required hospitalization more often than reported for coronavirus, rhinovirus, parainfluenza virus, adenovirus, and human metapneumovirus, as well as when compared with coinfections of RSV and parainfluenza or coronavirus | Limited insight on the overall severity of infection between viruses and the role of comorbidities |
| Brazil; Estofolete et al. [28] | Retrospective surveillance cohort (2021–2022) | Patients aged ≥ 15 years | Mean age of patients infected with RSV was significantly higher compared with influenza (59.2 versus 39.4 years) | Data on the clinical impact of RSV in the general adult population, not just those at risk, are needed |
| Comorbidities were present in 79.6% of patients with RSV, significantly higher than those with influenza (47.4%) | ||||
| Ventilatory support was required for 26.1% of RSV-infected patients, with symptoms of dyspnea and respiratory distress reported in 42.1% and 31.6% of RSV-infected patients, respectively | ||||
| Guatemala; McCracken et al. [58] | Prospective surveillance cohort (2007–2012) | Hospitalized patients with ARIs and RSV test results (no age restriction) | RSV infections were reported in 24% of 6287 hospitalizations and 12% of 2565 clinic visits for ARIs, with 6% and 5% of patients aged ≥ 50 years, respectively | Data were only collected from three regions of Guatemala, which may be limited by the article’s case definition in the outpatient setting |
| The highest incidence of RSV among adults was reported in patients aged ≥ 65 years (2.9 cases/10,000 persons per year) | ||||
| Chile; Luchsinger et al. [68] | Prospective cohort (2005–2007) | Patients aged ≥ 18 years with CAP | RSV was the most common viral pathogen identified among 356 adults with CAP | Data were collected from two hospitals in Santiago, Chile |
| RSV infections among patients with CAP were predominant during May, June, and July | The impact of RSV infection on the clinical outcome of CAP requires further investigation |
ARIs acute respiratory infections, CAP community-acquired pneumonia, ILI influenza-like illness, RSV respiratory syncytial virus, RTIs respiratory tract infections
Given the overall concern that RSV-associated morbidity and mortality may be largely underestimated in Latin America, data from other regions should be considered. In the USA, while RSV hospitalizations may occur at a lower rate than those associated with COVID-19 or influenza, several publications have indicated that RSV is associated with more severe clinical outcomes, particularly for patients aged ≥ 60 years [59–62]. Consistent with this, lower 1-year survival rates following hospital admission for RSV compared with influenza have been reported, which is thought to be driven by chronic inflammation associated with persistent, sometimes progressive, pulmonary disease observed in patients with RSV infection [59]. However, comparisons between ARIs such as RSV and COVID-19 should be taken with caution, given differences in the nature of these diseases as well as their impact and associated health risks.
As RSV-infected patients may also have a higher risk of ICU admission than observed for influenza cases [60], communication on RSV in ICUs and emergency rooms is imperative, especially during seasonal outbreaks. Increasing awareness of RSV in such settings may promote better clinical management of cases, reducing the number of unnecessary antibiotic prescriptions and the use of antivirals against influenza, which is a common practice observed in Latin American ICUs [63]. Antibiotic use has been reported in up to 93% of patients with confirmed RSV at centers in the Netherlands and Israel [64].
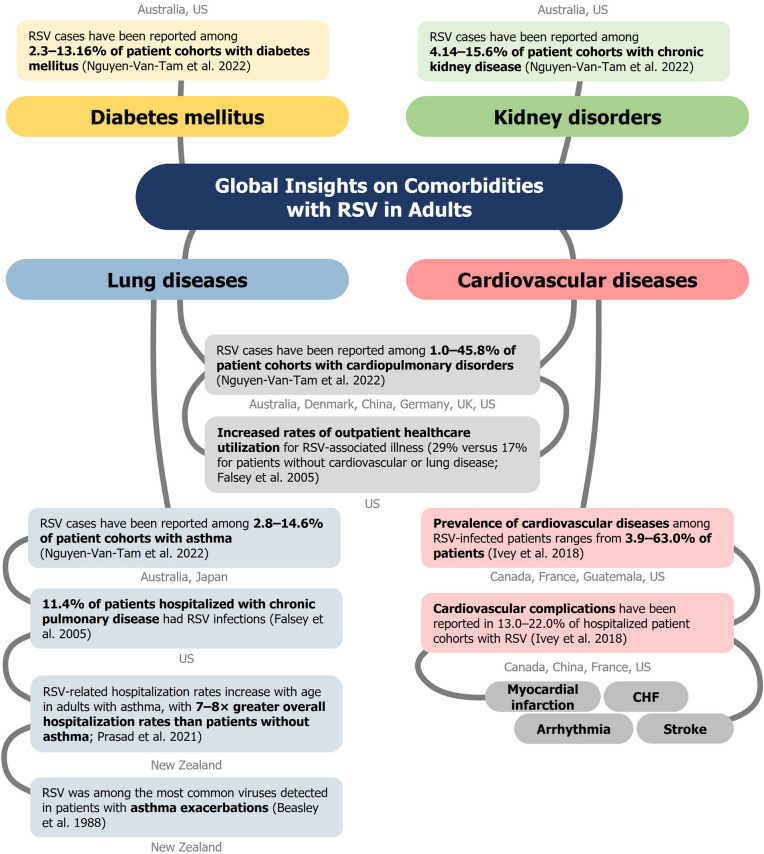
Comorbidity Complexity
RSV may be further underestimated as a cause of morbidity and mortality in “at-risk” older adults, such as those with respiratory comorbidities (e.g., asthma and chronic obstructive pulmonary disease [COPD]), compromised immune systems, or frailty [65, 66]. The Global Initiative for Chronic Obstructive Disease (GOLD) has recognized the impact of RSV in COPD, advocating the recommendation for RSV vaccination in patients aged ≥ 60 years in their 2024 report [67]. Pulmonary complications, including pneumonia, exacerbation of asthma and COPD, chronic bronchitis or emphysema, have been reported to occur at a greater frequency following RSV infection compared with influenza, even after adjustments for baseline comorbidities [59, 66]. Furthermore, a global systematic literature review and metaanalysis of RSV infection in older and at-risk adults identified that those with comorbidities are at substantial risk of severe outcomes within this population of individuals [34]. Global insights on the association of RSV infections with underlying conditions are shown in Fig. 2. In Latin America, we found one study in Chile of hospitalized adult patients with CAP, which reported that RSV was the most common viral pathogen identified [68].
Fig. 2.
Global insights on comorbidities in RSV-infected adults. Data reported from Refs. [34, 69, 72, 81, 82]. CHF congestive heart failure, RSV respiratory syncytial virus, US USA
RSV is also associated with cardiovascular diseases [69]. There is evidence that RSV may share some of the mechanisms by which other viral infections contribute to cardiovascular injury, whereby the inflammatory response may lead to disruption and rupture of arterial plaques and increased risk of acute coronary syndrome such as myocardial infarction [69–71]. However, truly understanding the risk factors for severe RSV in older adults is complex, owing to the diversity in health status, comorbidities, and living conditions within this age group [45]. Falsey et al. (2005) previously highlighted the significant health impact of RSV among older adults (aged ≥ 65 years) and high-risk adults (i.e., with chronic heart or lung disease), with 39% and 45% of patients unable to perform normal activities of daily living, respectively, along with high use of medical care services, similar to data reported on influenza [72].
A study in Mexico among adults aged ≥ 18 years reported that older patients, males, and those with any underlying conditions (e.g., cardiovascular diseases, chronic lung disease, or asthma) had a significantly higher risk of RSV-associated hospitalization [30], indicating the likelihood of a high prevalence of RSV-related comorbidities in Latin American patients; however, additional surveillance data are required to confirm this. These findings align with collective data reported in the USA, Canada, Europe, and Asia [37]. A recent population-based surveillance study in the USA reported that most RSV-hospitalized patients aged ≥ 60 years had underlying conditions (95.5%), namely COPD (33.7%) and congestive heart failure (CHF; 33.2%), all of which were associated with severe outcomes [66]. Another USA study found 3.5–13.4 times higher hospitalization rates for patients with COPD aged ≥ 65 years and 5.9–7.6 times higher rates for patients with CHF aged 60–79 years, compared with patients without these conditions [73]. Such data are important to consider, as the underdiagnosis of clinical conditions such as COPD can be as high as 89% in Latin American countries [74]. There is also an added concern of RSV outbreaks in hospital settings, where patients with underlying conditions could be at a significant risk of contracting RSV, with severe associated outcomes [75].
It is crucial to also recognize that long-term care facilities (LTCFs) may be highly susceptible to respiratory disease outbreaks, as their residents are often more frail and therefore highly vulnerable to infection and severe outcomes [76]. This was exemplified during the COVID-19 pandemic, where outbreaks of ILIs in LTCFs in São Paulo, Brazil, attributed to COVID-19, influenza, and other viruses, accounted for more than 70% of all deaths [76]. Concerning RSV, living in a LTCF has been shown to increase the likelihood of severe clinical outcomes, including ICU admission, mechanical ventilation, and/or death, by over fourfold compared with patients living independently or with assistance in the community [77]. Prehospitalization living situation has also been identified as an important correlate for functional decline of older adults aged ≥ 60 years from prehospitalization to 6 months postdischarge [78]. Although more data are needed in Latin America, we believe that frailty is potentially a more important predictor of severe outcomes than age alone, as chronic conditions and many comorbidities are associated with frailty [77]. In a multicenter, European observational cohort study of 1564 patients with COVID-19, frailty was determined to be a better predictor of disease outcomes than either age or presence of comorbidities [79]. Together, these findings underscore the critical need for RSV testing in LTCFs, where older, multimorbid, and frail individuals are at a heightened risk of severe RSV infection.
One challenge to consider regarding RSV-related comorbidities is their frequent association with age-related immunosenescence or immunosuppression (e.g., cancer or transplantation treatments), which can complicate RSV diagnosis. This is of particular importance given the increasing aging population. Age-related cognitive impairments or degenerative disorders, such as dementias, could further complicate diagnosis in older adults. Hence, assessing the degree of association between RSV and the worsening of comorbidities can be challenging. Considering the available epidemiological data presented, it is reasonable to assume that many older adults hospitalized with RSV in Latin America are likely to present with one or more comorbidities that could increase the risk of severe outcomes. Therefore, we advocate for routine diagnostic testing for viral infections in hospitals and via epidemiological surveillance units, especially in patients with severe respiratory conditions (Table 2). This change is necessary to ensure that the burden of RSV can be accurately recognized and addressed in the aging population.
Conclusions
The challenges related to RSV in older adults and individuals with underlying conditions in Latin America are multifaceted and complex. This expert consensus emphasizes that lack of awareness, underdiagnosis, and data scarcity pose significant challenges that must be addressed in the region. To overcome these challenges, it is imperative to prioritize routine diagnostic testing for RSV, advocate for comprehensive data collection and dissemination efforts, and emphasize the importance of understanding the significant impact of RSV among adult populations. Furthermore, we call for the establishment of local initiatives and a taskforce to address challenges associated with RSV surveillance in Latin America. The initiatives discussed here would be pivotal in addressing poor awareness, improving patient management, and reducing the burden of RSV in the region. Moreover, this consensus will help guide regional and national responses to RSV in older adults, highlighting preventive measures, increased diagnostic testing, and targeted interventions, and may also help increase the awareness of other viruses that can cause respiratory infections in susceptible populations. It is a shared responsibility among healthcare practitioners, public health bodies, and policymakers to improve RSV patient outcomes in Latin America and promote the prevention of RSV in older adults.
Acknowledgements
Medical writing/editorial assistance.
The authors acknowledge Bella Dragova-Maurin, GSK, Belgium for publication management. The authors also thank Costello Medical for editorial assistance and publication coordination, on behalf of GSK, and acknowledge Samuel Shields, Costello Medical, UK for medical writing and editorial assistance based on authors’ input and direction. The authors also acknowledge Hannah Avery, Nucleus Global, UK for supporting with the initial review of the literature and for providing editorial support.
Author Contributions
Substantial contributions to study conception and design: Ricardo Amorim Correa, Francisco Arancibia, Renato De Ávila Kfouri, Alberto Chebabo, Gabriel García, Luis Miguel Gutiérrez Robledo, Gustavo Lopardo, Julio Nemerovsky, Carlos M. Pérez, Adrian Rendon, Guillermo M. Ruiz-Palacios, Bhumika Aggarwal, Arnas Berzanskis, and Otavio Cintra; substantial contributions to analysis and interpretation of the data: Ricardo Amorim Correa, Francisco Arancibia, Renato De Ávila Kfouri, Alberto Chebabo, Gabriel García, Luis Miguel Gutiérrez Robledo, Gustavo Lopardo, Julio Nemerovsky, Carlos M. Pérez, Adrian Rendon, Guillermo M. Ruiz-Palacios, Bhumika Aggarwal, Arnas Berzanskis, and Otavio Cintra; drafting the article or revising it critically for important intellectual content: Ricardo Amorim Correa, Francisco Arancibia, Renato De Ávila Kfouri, Alberto Chebabo, Gabriel García, Luis Miguel Gutiérrez Robledo, Gustavo Lopardo, Julio Nemerovsky, Carlos M. Pérez, Adrian Rendon, Guillermo M. Ruiz-Palacios, Bhumika Aggarwal, Arnas Berzanskis, and Otavio Cintra; final approval of the version of the article to be published: Ricardo Amorim Correa, Francisco Arancibia, Renato De Ávila Kfouri, Alberto Chebabo, Gabriel García, Luis Miguel Gutiérrez Robledo, Gustavo Lopardo, Julio Nemerovsky, Carlos M. Pérez, Adrian Rendon, Guillermo M. Ruiz-Palacios, Bhumika Aggarwal, Arnas Berzanskis, and Otavio Cintra.
Funding
This manuscript was sponsored by GlaxoSmithKline Biologicals SA. Support for third-party writing assistance and the Rapid Service and open access fees for this article were also funded by GSK in accordance with Good Publication Practice (GPP 2022) guidelines (https://www.ismpp.org/gpp-2022).
Declarations
Conflict of Interest
Bhumika Aggarwal, Arnas Berzanskis, and Otavio Cintra: employees and stock owners of GSK. Francisco Arancibia: received payment of honoraria for lectures, presentations, speakers bureaus, manuscript writing, or educational events from OM-Pharma and Pfizer; participated on a Data Safety Monitoring Board or Advisory Board for OM-Pharma and GSK; and had a leadership of fiduciary role in other board, society, committee, or advocacy group, paid or unpaid, for ALAT (President). Alberto Chebabo: received grants or contracts from Pfizer; payment of honoraria for lectures, presentations, speakers bureaus, manuscript writing, or educational events from GSK, Pfizer, MSD, and Takeda; support for attending meetings and/or travel from Pfizer and Takeda; and participated on a Data Safety Monitoring Board or Advisory Board for GSK, Takeda, and Pfizer. Ricardo Amorim Correa: received grants or contracts from Janssen, MSD, and Bayer; consulting fees from Janssen, MSD, and Bayer; payment of honoraria for lectures, presentations, speakers bureaus, manuscript writing, or educational events from Janssen and Bayer; payment for expert testimony from Janssen, MSD, and Bayer; support for attending meetings and/or travel from AstraZeneca and Bayer; and had a leadership of fiduciary role in other board, society, committee, or advocacy group, paid or unpaid, for SBPT (President Elect). Gabriel García: received payment of honoraria for lectures, presentations, speakers bureaus, manuscript writing, or educational events from GSK, Boehringer Ingelheim, Novartis, Sanofi, and Chiesi. Luis Miguel Gutiérrez Robledo: received grants or contracts from GSK; consulting fees from GSK; payment of honoraria for lectures, presentations, speakers bureaus, manuscript writing, or educational events from GSK; support for attending meetings and/or travel from Sanofi; participated on an Advisory Board for GSK. Renato De Ávila Kfouri: received grants or contracts from Pfizer; consulting fees from Pfizer, GSK, Sanofi, MSD, Takeda, and Moderna; payment of honoraria for lectures, presentations, speakers bureaus, manuscript writing, or educational events from Pfizer, GSK, Takeda, Sanofi, AstraZeneca, and MSD; support for attending meetings and/or travel from Pfizer and Sanofi; participated on a Data Safety Monitoring Board or Advisory Board for Clover Vaccines; and had a leadership of fiduciary role in other board, society, committee, or advocacy group, paid or unpaid, for Sociedade Brasileira de Pediatria (Pres do Depto Immunization), Sociedade Brasileira De Imunizações (Vice President), and NITAG Brasil (member). Gustavo Lopardo: received grants or contracts from MSD; consulting fees from GSK and Pfizer; and support for attending meetings and/or travel from Pfizer. Julio Nemerovsky: received grants or contracts from GSK; payment of honoraria for lectures, presentations, speakers bureaus, manuscript writing, or educational events from GSK and Casasco; support for attending meetings and/or travel from Baliarda; and participated on a Data Safety Monitoring Board or Advisory Board for GSK. Carlos M. Pérez: received grants or contracts from Merck and Sinovac to institution; consulting fees from GSK/ViiV; payment of honoraria for lectures, presentations, speakers bureaus, manuscript writing, or educational events from GSK/ViiV, Pfizer, and Gador; support for attending meetings and/or travel from Pfizer and Gador; and participated on a Data Safety Monitoring Board or Advisory Board for GSK/ViiV. Adrian Rendon: received grants or contracts from Pfizer and Boehringer Ingelheim; payment of honoraria for lectures, presentations, speakers bureaus, manuscript writing, or educational events from GSK, AstraZeneca, Chiesi, and Sanofi; support for attending meetings and/or travel from GSK and AstraZeneca; and participated on a Data Safety Monitoring Board or Advisory Board for GSK. Guillermo M. Ruiz-Palacios: participated on a Data Safety Monitoring Board or Advisory Board for GSK.
Ethical Approval
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
References
- 1.Du Y, Yan R, Wu X, et al. Global burden and trends of respiratory syncytial virus infection across different age groups from 1990 to 2019: a systematic analysis of the Global Burden of Disease 2019 Study. Int J Infect Dis. 2023;135:70–76. doi: 10.1016/j.ijid.2023.08.008. [DOI] [PubMed] [Google Scholar]
- 2.Ejaz H, Alsrhani A, Zafar A, et al. COVID-19 and comorbidities: Deleterious impact on infected patients. J Infect Public Health. 2020;13(12):1833–1839. doi: 10.1016/j.jiph.2020.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gupta A, Marzook H, Ahmad F. Comorbidities and clinical complications associated with SARS-CoV-2 infection: an overview. Clin Exp Med. 2023;23(2):313–331. doi: 10.1007/s10238-022-00821-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Häder A, Köse-Vogel N, Schulz L, et al. Respiratory infections in the aging lung: implications for diagnosis, therapy, and prevention. Aging Dis. 2023;14(4):1091–104. 10.14336/ad.2023.0329. [DOI] [PMC free article] [PubMed]
- 5.Márquez-Salinas A, Fermín-Martínez CA, Antonio-Villa NE, et al. Adaptive metabolic and inflammatory responses identified using accelerated aging metrics are linked to adverse outcomes in severe SARS-CoV-2 infection. J Gerontol A Biol Sci Med Sci. 2021;76(8):e117–e126. doi: 10.1093/gerona/glab078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.WHO. Respiratory Syncytial Virus (RSV) disease. https://www.who.int/teams/health-product-policy-and-standards/standards-and-specifications/vaccine-standardization/respiratory-syncytial-virus-disease [Accessed November 2023].
- 7.Melgar M, Britton A, Roper LE, et al. Use of respiratory syncytial virus vaccines in older adults: recommendations of the advisory committee on immunization practices — United States, 2023. MMWR Morb Mortal Wkly Rep. 2023;72(29):793–801. doi: 10.15585/mmwr.mm7229a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Thompson WW, Shay DK, Weintraub E, et al. Mortality associated with influenza and respiratory syncytial virus in the United States. JAMA. 2003;289(2):179–186. doi: 10.1001/jama.289.2.179. [DOI] [PubMed] [Google Scholar]
- 9.Ali A, Lopardo G, Scarpellini B, Stein RT, Ribeiro D. Systematic review on respiratory syncytial virus epidemiology in adults and the elderly in Latin America. Int J Infect Dis. 2020;90:170–180. doi: 10.1016/j.ijid.2019.10.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Buendía JA, Patino DG, Sinisterra D. Cost of illness of RSV infection in a middle-income tropical country. Turk J Pediatr. 2021;63(4):673–82. 10.24953/turkjped.2021.04.015. [DOI] [PubMed]
- 11.Mosegui GBG, Antoñanzas F, de Mello Vianna CM. Cost of lost productivity from acute respiratory infections in South America. Rev Panam Salud Publica. 2023;47:e65. 10.26633/rpsp.2023.65. [DOI] [PMC free article] [PubMed]
- 12.Doherty TM, Del Giudice G, Maggi S. Adult vaccination as part of a healthy lifestyle: moving from medical intervention to health promotion. Ann Med. 2019;51(2):128–140. doi: 10.1080/07853890.2019.1588470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hall CB. Respiratory syncytial virus: its transmission in the hospital environment. Yale J Biol Med. 1982;55(3–4):219–223. [PMC free article] [PubMed] [Google Scholar]
- 14.Carbonell-Estrany X, Simões EAF, Bont LJ, et al. Identifying the research, advocacy, policy and implementation needs for the prevention and management of respiratory syncytial virus lower respiratory tract infection in low- and middle-income countries. Front Pediatr. 2022;10:1033125. doi: 10.3389/fped.2022.1033125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bardach A, Rey-Ares L, Cafferata ML, et al. Systematic review and meta-analysis of respiratory syncytial virus infection epidemiology in Latin America. Rev Med Virol. 2014;24(2):76–89. doi: 10.1002/rmv.1775. [DOI] [PubMed] [Google Scholar]
- 16.Pan American Health Organization, World Health Organization. Epidemiological Alert: Influenza, respiratory syncytial virus and SARS-CoV-2. 6 June 2023. https://www.paho.org/en/documents/epidemiological-alert-influenza-respiratory-syncytial-virus-and-sars-cov-2-6-june-2023.
- 17.Sousa MLA, Shimizu IS, Patino CM, et al. COVID-19 knowledge, attitudes, and practices among health care workers in Latin America. J Bras Pneumol. 2022;48(5):e20220018. 10.36416/1806-3756/e20220018. [DOI] [PMC free article] [PubMed]
- 18.Mejia CR, Aveiro-Robalo TR, Garlisi Torales LD, et al. Basic COVID-19 knowledge according to education level and country of residence: Analysis of twelve countries in Latin America. Front Med. 2022;9. 10.3389/fmed.2022.978795. [DOI] [PMC free article] [PubMed]
- 19.Jain S, Self WH, Wunderink RG, et al. Community-acquired pneumonia requiring hospitalization among U.S. Adults. N Engl J Med. 2015;373(5):415–27. 10.1056/NEJMoa1500245. [DOI] [PMC free article] [PubMed]
- 20.Nuwer R. Better awareness of RSV in older adults is needed to fight a growing burden. Nature. 2023;621:S58–S59. doi: 10.1038/d41586-023-02958-y. [DOI] [PubMed] [Google Scholar]
- 21.European Medicines Agency. Abrysvo. https://www.ema.europa.eu/en/medicines/human/EPAR/abrysvo. Accessed December 2023.
- 22.European Medicines Agency. Arexvy. https://www.ema.europa.eu/en/medicines/human/EPAR/arexvy. Accessed December 2023.
- 23.Papi A, Ison MG, Langley JM, et al. Respiratory syncytial virus prefusion F protein vaccine in older adults. N Engl J Med. 2023;388(7):595–608. doi: 10.1056/NEJMoa2209604. [DOI] [PubMed] [Google Scholar]
- 24.Walsh EE, Pérez Marc G, Zareba AM, et al. Efficacy and safety of a bivalent RSV prefusion F vaccine in older adults. N Engl J Med. 2023;388(16):1465–1477. doi: 10.1056/NEJMoa2213836. [DOI] [PubMed] [Google Scholar]
- 25.Baumeister E, Duque J, Varela T, et al. Timing of respiratory syncytial virus and influenza epidemic activity in five regions of Argentina, 2007–2016. Influenza Other Respir Viruses. 2019;13(1):10–17. doi: 10.1111/irv.12596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.de Mello Freitas FT. Sentinel surveillance of influenza and other respiratory viruses, Brazil, 2000–2010. Braz J Infect Dis. 2013;17(1):62–68. doi: 10.1016/j.bjid.2012.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Echavarría M, Marcone DN, Querci M, et al. Clinical impact of rapid molecular detection of respiratory pathogens in patients with acute respiratory infection. J Clin Virol. 2018;108:90–95. doi: 10.1016/j.jcv.2018.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Estofolete CF, Banho CA, Verro AT, et al. Clinical characterization of respiratory syncytial virus infection in adults: a neglected disease? Viruses. 2023;15(9):1848, https://www.mdpi.com/1999-4915/15/9/1848. [DOI] [PMC free article] [PubMed]
- 29.Fernandes-Matano L, Monroy-Muñoz IE, Angeles-Martínez J, et al. Prevalence of non-influenza respiratory viruses in acute respiratory infection cases in Mexico. PLoS One. 2017;12(5):e0176298. doi: 10.1371/journal.pone.0176298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gamiño-Arroyo AE, Moreno-Espinosa S, Llamosas-Gallardo B, et al. Epidemiology and clinical characteristics of respiratory syncytial virus infections among children and adults in Mexico. Influenza Other Respir Viruses. 2017;11(1):48–56. doi: 10.1111/irv.12414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Riquelme R, Rioseco ML, Agüero Y, et al. Infección por virus respiratorios en adultos hospitalizados en un Servicio de Medicina Interna. Revista médica de Chile. 2014;142:696–701, http://www.scielo.cl/scielo.php?script=sci_arttext&pid=S0034-98872014000600002&nrm=iso. [DOI] [PubMed]
- 32.Galindo-Fraga A, Ortiz-Hernández AA, Ramírez-Venegas A, et al. Clinical characteristics and outcomes of influenza and other influenza-like illnesses in Mexico City. Int J Infect Dis. 2013;17(7):e510–e517. doi: 10.1016/j.ijid.2013.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ramírez-Soto MC, Ortega-Cáceres G, Garay-Uribe J. Characteristics of respiratory syncytial virus versus influenza infection in hospitalized patients of Peru: a retrospective observational study. Trop Med Infect Dis. 2022 doi: 10.3390/tropicalmed7100317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Nguyen-Van-Tam JS, O’Leary M, Martin ET, et al. Burden of respiratory syncytial virus infection in older and high-risk adults: a systematic review and meta-analysis of the evidence from developed countries. Eur Respir Rev. 2022 doi: 10.1183/16000617.0105-2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mosscrop LG, Williams TC, Tregoning JS. Respiratory syncytial virus after the SARS-CoV-2 pandemic - what next? Nat Rev Immunol. 2022;22(10):589–590. doi: 10.1038/s41577-022-00764-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pan American Health Organization, World Health Organization. Epidemiological Alert: Anticipation of the onset of respiratory virus season. 22 September 2023. https://www.paho.org/en/documents/epidemiological-alert-anticipation-onset-respiratory-virus-season-22-september-2023.
- 37.Savic M, Penders Y, Shi T, Branche A, Pirçon J-Y. Respiratory syncytial virus disease burden in adults aged 60 years and older in high-income countries: a systematic literature review and meta-analysis. Influenza Other Respir Viruses. 2023;17(1):e13031. doi: 10.1111/irv.13031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Htar MTT, Yerramalla M, Moïsi J, Swerdlow D. The burden of respiratory syncytial virus in adults: a systematic review and meta-analysis. Epidemiol Infect. 2020 doi: 10.1017/S0950268820000400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Shi T, Vennard S, Jasiewicz F, Brogden R, Nair H, Investigators R. Disease burden estimates of respiratory syncytial virus related acute respiratory infections in adults with comorbidity: a systematic review and meta-analysis. J Infect Dis. 2021;226(Supplement 1):S17–S21. doi: 10.1093/infdis/jiab040. [DOI] [PubMed] [Google Scholar]
- 40.Belongia EA, King JP, Kieke BA, et al. Clinical features, severity, and incidence of RSV illness during 12 consecutive seasons in a community cohort of adults ≥60 years old. Open Forum Infect Dis. 2018 doi: 10.1093/ofid/ofy316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chatzis O, Darbre S, Pasquier J, et al. Burden of severe RSV disease among immunocompromised children and adults: a 10 year retrospective study. BMC Infect Dis. 2018;18(1):111. doi: 10.1186/s12879-018-3002-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.McLaughlin JM, Khan F, Begier E, Swerdlow DL, Jodar L, Falsey AR. Rates of medically attended RSV among US adults: a systematic review and meta-analysis. Open Forum Infect Dis. 2022 doi: 10.1093/ofid/ofac300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.American Heart Association. RSV and Heart Health. https://www.heart.org/en/health-topics/rsv [Accessed November 2023].
- 44.CDC. Respiratory Syncytial Virus Infection (RSV). https://www.cdc.gov/rsv/index.html [Accessed November 2023].
- 45.Falsey AR, Walsh EE. Respiratory syncytial virus infection in elderly adults. Drugs Aging. 2005;22(7):577–587. doi: 10.2165/00002512-200522070-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Zuurbier RP, Korsten K, Verheij TJM, et al. Performance assessment of a rapid molecular respiratory syncytial virus point-of-care test: a prospective community study in older adults. J Infect Dis. 2022;226(Suppl 1):S63–S70. doi: 10.1093/infdis/jiab600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Chartrand C, Tremblay N, Renaud C, Papenburg J. Diagnostic accuracy of rapid antigen detection tests for respiratory syncytial virus infection: systematic review and meta-analysis. J Clin Microbiol. 2015;53(12):3738–3749. doi: 10.1128/jcm.01816-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Larsson E, Johansson S, Frøbert O, Nordenskjöld A, Athlin S. Evaluation of the IMMUVIEw RSV test for rapid detection of respiratory syncytial virus in adult patients with influenza-like symptoms. Microbiol Spectr. 2021;9(3):e0093721. doi: 10.1128/Spectrum.00937-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Pfeil J, Tabatabai J, Sander A, Ries M, Grulich-Henn J, Schnitzler P. Screening for respiratory syncytial virus and isolation strategies in children hospitalized with acute respiratory tract infection. Medicine (Baltimore) 2014;93(25):e144. doi: 10.1097/md.0000000000000144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Rozenbaum MH, Judy J, Tran D, Yacisin K, Kurosky SK, Begier E. Low levels of RSV testing among adults hospitalized for lower respiratory tract infection in the United States. Infect Dis Ther. 2023;12(2):677–685. doi: 10.1007/s40121-023-00758-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Rozenbaum MH, Begier E, Kurosky SK, et al. Incidence of respiratory syncytial virus infection in older adults: limitations of current data. Infect Dis Ther. 2023;12(6):1487–1504. doi: 10.1007/s40121-023-00802-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Schneider UV, Holm MKA, Bang D, et al. Point-of-care tests for influenza A and B viruses and RSV in emergency departments - indications, impact on patient management and possible gains by syndromic respiratory testing, Capital Region, Denmark, 2018. Euro Surveill. 2020;25(44):1900430. doi: 10.2807/1560-7917.Es.2020.25.44.1900430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Li Y, Kulkarni D, Begier E, et al. Adjusting for case under-ascertainment in estimating RSV hospitalisation burden of older adults in high-income countries: a systematic review and modelling study. Infect Dis Ther. 2023;12(4):1137–1149. doi: 10.1007/s40121-023-00792-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Reis Neto JPD, Juliana Martinho; Araujo, Rafael Rodrigo; Barbosa, Aline; Chagas, Kelem; Teich, Vanessa; Boiron, Luis. Perfil de hospitalizações potencialmente relacionadas à influenza: dados de uma autogestão do Sistema de Saúde Suplementar do Brasil. J Bras Econ Saúde. 2020;12(3):255–63.
- 55.Staadegaard L, Caini S, Wangchuk S, et al. The Global Epidemiology of RSV in Community and Hospitalized Care: Findings From 15 Countries. Open Forum Infect Dis. 2021;8(7):ofab159. 10.1093/ofid/ofab159. [DOI] [PMC free article] [PubMed]
- 56.Fleming DM, Taylor RJ, Lustig RL, et al. Modelling estimates of the burden of Respiratory Syncytial virus infection in adults and the elderly in the United Kingdom. BMC Infect Dis. 2015;15:443. doi: 10.1186/s12879-015-1218-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Niekler P, Goettler D, Liese JG, Streng A. Hospitalizations due to respiratory syncytial virus (RSV) infections in Germany: a nationwide clinical and direct cost data analysis (2010–2019) Infection. 2023 doi: 10.1007/s15010-023-02122-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.McCracken JP, Prill MM, Arvelo W, et al. Respiratory syncytial virus infection in Guatemala, 2007–2012. J Infect Dis. 2013;208(Suppl 3):S197–206. doi: 10.1093/infdis/jit517. [DOI] [PubMed] [Google Scholar]
- 59.Ackerson B, Tseng HF, Sy LS, et al. Severe morbidity and mortality associated with respiratory syncytial virus versus influenza infection in hospitalized older adults. Clin Infect Dis. 2018;69(2):197–203. doi: 10.1093/cid/ciy991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ambrosch A, Luber D, Klawonn F, Kabesch M. Focusing on severe infections with the respiratory syncytial virus (RSV) in adults: Risk factors, symptomatology and clinical course compared to influenza A / B and the original SARS-CoV-2 strain. J Clin Virol. 2023;161:105399. doi: 10.1016/j.jcv.2023.105399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Begley KM, Monto AS, Lamerato LE, et al. Prevalence and clinical outcomes of respiratory syncytial virus vs influenza in adults hospitalized with acute respiratory illness from a prospective multicenter study. Clin Infect Dis. 2023;76(11):1980–1988. doi: 10.1093/cid/ciad031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Surie D, Yuengling KA, DeCuir J, et al. Disease severity of respiratory syncytial virus compared with COVID-19 and influenza among hospitalized adults Aged ≥60 Years — IVY Network, 20 U.S. States, February 2022–May 2023. 2023;72(40):1083–8. [DOI] [PMC free article] [PubMed]
- 63.Levy Hara G, Rojas-Cortés R, Molina León HF, et al. Point prevalence survey of antibiotic use in hospitals in Latin American countries. J Antimicrob Chemother. 2021;77(3):807–815. doi: 10.1093/jac/dkab459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.van Houten CB, Cohen A, Engelhard D, et al. Antibiotic misuse in respiratory tract infections in children and adults-a prospective, multicentre study (TAILORED Treatment) Eur J Clin Microbiol Infect Dis. 2019;38(3):505–514. doi: 10.1007/s10096-018-03454-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Lees C, Godin J, McElhaney JE, et al. Frailty hinders recovery from influenza and acute respiratory illness in older adults. J Infect Dis. 2020;222(3):428–437. doi: 10.1093/infdis/jiaa092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Havers FP, Whitaker M, Melgar M, et al. Characteristics and outcomes among adults aged ≥60 Years hospitalized with laboratory-confirmed respiratory syncytial virus - RSV-NET, 12 States, July 2022-June 2023. MMWR Morb Mortal Wkly Rep. 2023;72(40):1075–82. 10.15585/mmwr.mm7240a1. [DOI] [PMC free article] [PubMed]
- 67.Global intiative for chronic obstructive lung disease. Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease (2024 Report). https://goldcopd.org/2024-gold-report/ [Accessed November 2023].
- 68.Luchsinger V, Ruiz M, Zunino E, et al. Community-acquired pneumonia in Chile: the clinical relevance in the detection of viruses and atypical bacteria. Thorax. 2013;68(11):1000–1006. doi: 10.1136/thoraxjnl-2013-203551. [DOI] [PubMed] [Google Scholar]
- 69.Ivey KS, Edwards KM, Talbot HK. Respiratory syncytial virus and associations with cardiovascular disease in adults. J Am Coll Cardiol. 2018;71(14):1574–1583. doi: 10.1016/j.jacc.2018.02.013. [DOI] [PubMed] [Google Scholar]
- 70.Franczuk P, Tkaczyszyn M, Kulak M, Domenico E, Ponikowski P, Jankowska EA. Cardiovascular complications of viral respiratory infections and COVID-19. Biomedicines. 2022 doi: 10.3390/biomedicines11010071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Corrales-Medina VF, Madjid M, Musher DM. Role of acute infection in triggering acute coronary syndromes. Lancet Infect Dis. 2010;10(2):83–92. doi: 10.1016/S1473-3099(09)70331-7. [DOI] [PubMed] [Google Scholar]
- 72.Falsey AR, Hennessey PA, Formica MA, Cox C, Walsh EE. Respiratory syncytial virus infection in elderly and high-risk adults. N Engl J Med. 2005;352(17):1749–1759. doi: 10.1056/NEJMoa043951. [DOI] [PubMed] [Google Scholar]
- 73.Branche AR, Saiman L, Walsh EE, et al. Incidence of respiratory syncytial virus infection among hospitalized adults, 2017–2020. Clin Infect Dis. 2022;74(6):1004–1011. doi: 10.1093/cid/ciab595. [DOI] [PubMed] [Google Scholar]
- 74.Perez-Padilla R, Menezes AMB. Chronic obstructive pulmonary disease in Latin America. Ann Glob Health. 2019 doi: 10.5334/aogh.2418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.French CE, McKenzie BC, Coope C, et al. Risk of nosocomial respiratory syncytial virus infection and effectiveness of control measures to prevent transmission events: a systematic review. Influenza Other Respir Viruses. 2016;10(4):268–290. doi: 10.1111/irv.12379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Lucas PCdC, Duarte YAdO, Masuda ET, et al. Epidemiological characteristics of influenza-like illness outbreaks in long-term care facilities of the state of São Paulo, Brazil. Geriat Gerontol Aging. 2021;15:1–10.
- 77.Goldman CR, Sieling WD, Alba LR, et al. Severe clinical outcomes among adults hospitalized with respiratory syncytial virus infections, New York City, 2017–2019. Public Health Rep. 2022;137(5):929–935. doi: 10.1177/00333549211041545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Branche AR, Saiman L, Walsh EE, et al. Change in functional status associated with respiratory syncytial virus infection in hospitalized older adults. Influenza Other Respir Viruses. 2022;16(6):1151–1160. doi: 10.1111/irv.13043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Hewitt J, Carter B, Vilches-Moraga A, et al. The effect of frailty on survival in patients with COVID-19 (COPE): a multicentre, European, observational cohort study. Lancet Public Health. 2020;5(8):e444–e451. doi: 10.1016/s2468-2667(20)30146-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Noyola DE, Hunsberger S, Valdés Salgado R, et al. Comparison of rates of hospitalization between single and dual virus detection in a Mexican cohort of children and adults with influenza-like illness. Open Forum Infect Dis. 2019 doi: 10.1093/ofid/ofz424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Beasley R, Coleman ED, Hermon Y, Holst PE, O’Donnell TV, Tobias M. Viral respiratory tract infection and exacerbations of asthma in adult patients. Thorax. 1988;43(9):679–683. doi: 10.1136/thx.43.9.679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Prasad N, Walker TA, Waite B, et al. Respiratory syncytial virus-associated hospitalizations among adults with chronic medical conditions. Clin Infect Dis. 2020;73(1):e158–e163. doi: 10.1093/cid/ciaa730. [DOI] [PubMed] [Google Scholar]