Abstract
Oral health is important to general health, yet is often overlooked. During pregnancy, women may be more prone to periodontal (gum) disease and cavities, and research has shown an association between these conditions and adverse pregnancy outcomes. Additionally, a mother’s oral health status is a strong predictor of her children’s oral health status. Primary care providers often have an opportunity to influence their patients’ attitudes and behaviors regarding the importance of oral health during pregnancy. Through a cooperative agreement with the Centers for Disease Control and Prevention, the American Academy of Pediatrics worked to create Protect Tiny Teeth, an oral health communications resource that aims to facilitate conversations between pregnant women and their health care providers, as well as educate women and families about the importance of oral health.
Keywords: oral health, pregnancy, periodontal disease, dental caries, communication, resource
Introduction
YOU LOSE A TOOTH with every baby, right? This is a common misperception, but women may be more prone to certain oral conditions during pregnancy.1 Oral health is integral to general health, and one cannot be healthy without good oral health. Traditionally, oral health has not been considered an important aspect of prenatal care; however, poor oral health during pregnancy can lead to poor outcomes for the mother and baby.
Many pregnant women are unaware that dental care during pregnancy is safe and important, and may not be counseled by maternity care providers to visit a dentist. Clinical studies have shown that preventive dental care during pregnancy is safe and effective, and periodontal treatment, if needed, is safe as well.2 Even though 84% of obstetricians associate poor dental hygiene with preterm delivery, only 29% performed an oral exam during a prenatal visit.3 Data from the 2015 Pregnancy Risk Assessment Monitoring System (PRAMS) survey showed that 56% of women had their teeth cleaned before pregnancy, yet only 48% had their teeth cleaned during pregnancy.4 Additionally, when oral complications occurred during pregnancy, only half of women sought care.5
One Tooth for Every Baby
The old wives’ tale that you lose a tooth for every baby is unsupported by science, yet a 2005 study showed that one in five women believe this statement.6 While calcium is lost from maternal bones to support fetal development, minerals, such as calcium, are not taken from teeth during pregnancy and lactation.7 The effects of pregnancy on oral health are limited mainly to the soft tissues in the oral cavity.7 Few studies have reviewed the effects of number of children (parity) and tooth loss. While some studies have shown an association between greater parity and increased tooth loss,8 others have shown no association.9
Health Impact on Pregnant Women
There are two main oral conditions that occur in pregnant women: gingivitis, a mild form of periodontal (gum) disease, and dental caries (also known as tooth decay or cavities). Nearly 60%–75% of pregnant women have gingivitis, an early stage of periodontal disease that occurs when the gums become red and swollen due to inflammation.10 While there are no comparable data on gingivitis prevalence for nonpregnant women, data from 2009 to 2012 show that 46% of adults had some form of periodontal disease.11 Pregnant women may also be at risk for dental caries due to changes in behaviors and eating habits.12
Gingivitis/Periodontal Disease
In 2004, a report in the Journal of Periodontology13 studied the effects of pregnancy on the oral health status of nearly 1000 women. This study showed that 13% of pregnant women had moderate/severe periodontal disease present at enrollment to the study, with an increased prevalence among pregnant women who are smokers, African American, and of low socioeconomic status.13 Women with moderate/severe periodontal disease were 27% more likely to experience a progression of periodontal disease during pregnancy compared with women with no or mild disease at enrollment to the study.13
Periodontal disease is an inflammatory disease that affects the hard and soft structures that support the teeth.14 A higher level of pregnancy hormones, namely progesterone and estrogen, are thought to result in gingiva (gums) becoming more easily infected and inflamed, thus leading to a decline in periodontal health status.15 If left untreated, gingivitis may lead to periodontitis, the most severe form of periodontal disease, an inflammatory response in which pockets of destructive bacteria form in the gums and surrounding bones.16 However, the effect this heightened hormone production in pregnant women has on the immune modulation has not been thoroughly investigated.
Periodontitis may be associated with poor pregnancy outcomes, including preterm birth and low birth weight.17 However, the exact mechanism by which periodontitis is associated with adverse pregnancy outcomes is not yet understood.
Dental Caries
The cause of dental caries, also known as tooth decay or cavities, is multifactorial.18 With a daily ingestion of carbohydrates, bacteria that can metabolize these carbohydrates produce an acid. Prolonged exposure of the enamel to this acid can cause tiny breaks in the tooth surface and, if untreated, can lead to a cavity.
Untreated dental caries affect approximately one in four women of childbearing age.19 There is no credible evidence that supports a greater risk of dental caries during or after pregnancy. However, there is evidence that risk factors for cavities could occur or increase during pregnancy or postpartum, including:
consumption of a greater quantity of sugary foods and/or at a greater frequency,16
neglect of oral hygiene due to being busy or stressed,16
not visiting a dental health care provider for professional routine plaque removal (teeth cleaning),6
postponement of getting a decayed tooth filled. Many pregnant women delay dental care until after pregnancy. Postponement of getting a dental filling may lead to a progression of decay, but this is not due to pregnancy or postpartum,16
erosion of tooth enamel may occur during pregnancy due to vomiting. Nausea and vomiting during pregnancy are very common, and the presence of stomach acid in vomit may lead to tooth enamel loss at the surface of the tooth. Hyperemesis gravidarum (severe vomiting) is rare and only occurs in up to 2% of pregnancies.20
A mother’s oral health status is a strong predictor of her children’s oral health status. Women who have a high level of cavity-causing bacteria during pregnancy and after delivery could transmit this bacteria from their mouth to the mouth of their baby,21 also known as vertical transmission of cavities. Early colonization of this bacteria—amplified by the exposure to frequent acid-producing sugars, such as through frequent snacking or taking a bottle to bed—can lead to early childhood caries and the need for extensive dental care at a young age. Children of mothers with high levels of untreated caries or tooth loss are more than three times more likely to have caries.22 Additionally, children with poor oral health status are nearly three times more likely to miss school as a result of dental pain.23
Access and Barriers to Oral Health Care
The lack of dental insurance coverage in the United States is one of the primary factors contributing to unmet dental needs in adults.24 Medicaid, the main source of public funding for health care services, covers over 45% of births, making it the largest financer of births in the United States.25 Federal minimum requirements state that Medicaid covers dental services for low-income children, but states decide whether to provide dental benefits for adults. Additionally, while state Medicaid programs must cover pregnancy-related services, dental coverage is not explicitly included, and federal law allows states to choose whether they cover dental benefits for pregnant women.26
Less than one-third of states provide emergency-only dental services for adults through Medicaid, and less than half provide extensive dental care (Fig. 1). As an example, before 2015, Medicaid coverage in Virginia did not provide dental benefits to pregnant women. According to Virginia PRAMS data from 2011, less than a quarter of pregnant Medicaid recipients reported seeing a dentist.27 These data were used to support the development of a statewide oral health improvement plan in 2014, funding dental coverage for all pregnant women on Medicaid. Since this policy change, more than 14,000 now-eligible pregnant women have received dental services in Virginia.27 To reach lower-income populations with a high unmet need for dental care, state Medicaid plans may want to consider adopting comprehensive dental services, especially for pregnant women.
FIG. 1.
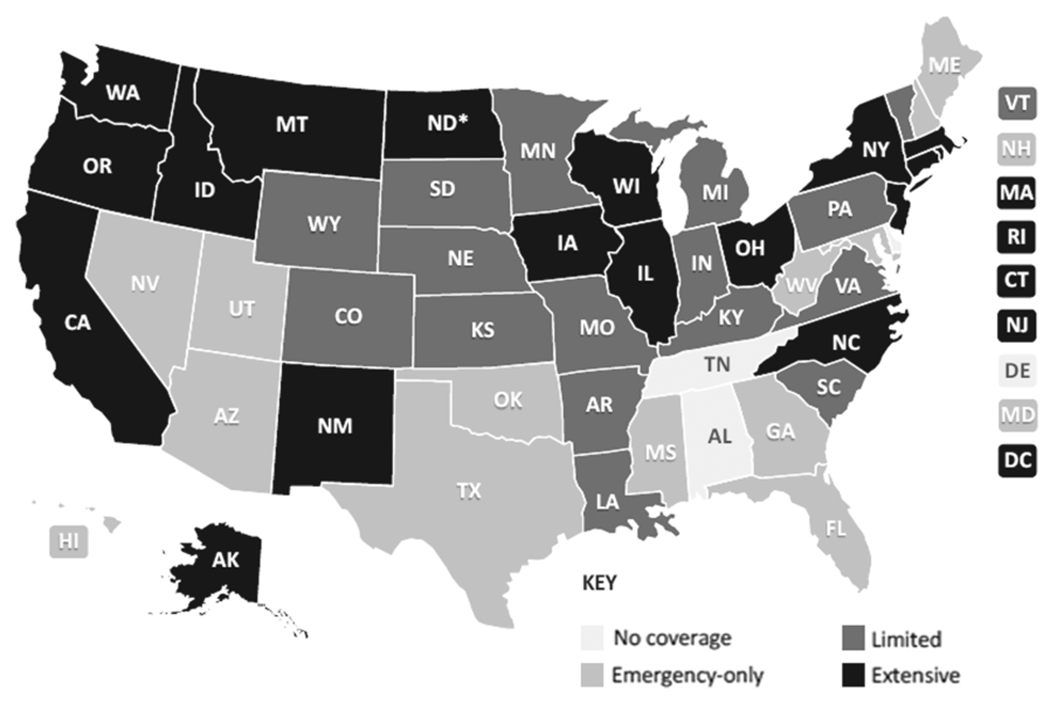
State Medicaid coverage of adult dental benefits, July 2018. There are no minimum requirements for adult dental coverage. Source: Center for Health Care Strategies, Inc. Retrieved from www.chcs.org/media/Adult-Oral-Health-Fact-Sheet_072718.pdf
An additional barrier to care is identifying providers who accept public insurance. As of 2015, only 38% of dentists reported that they accepted Medicaid or the Children’s Health Insurance Program.28
Dentist Perceptions of Care During Pregnancy
Even when women do seek care, some are turned away by dentists until after pregnancy. A national survey in 2009 showed that 77% of obstetricians and gynecologists reported that their patients were declined dental treatment by an oral health care provider because they were pregnant.29 Studies show that although dentists understand the importance of oral health care during pregnancy, they are sometimes reluctant to treat pregnant women due to fears of harming the fetus, fear of litigation, or patients’ safety concerns.4,30
Additionally, a meta-analysis reviewing dentists’ attitudes, behaviors, and knowledge about care during pregnancy found a wide variation in the knowledge of appropriateness of procedures.31 Factors such as uncertainty in the safety of X-rays, nitrous oxide administration, long-acting anesthetic injections, and over-the-counter pain medications may prevent dentists from providing comprehensive care to pregnant women.31
Recognizing this issue in the oral health community, the Children’s Dental Health Project recently released an issue brief to prioritize pregnant women and their oral health. This brief can be found online and is free to the public at www.cdhp.org/resources/339-issue-brief-oral-health-during-pregnancy. The resource has a series of briefs, infographics, and reports meant to spark renewed momentum for change and collaboration among all oral health stakeholders.
Protect Tiny Teeth: A Communications Toolkit for Primary Care Providers
Communication tools for health care providers to educate pregnant women and their families about the importance of oral health are limited. Through a cooperative agreement with the Centers for Disease Control and Prevention (CDC), the American Academy of Pediatrics (AAP) worked to create Protect Tiny Teeth (www.aap.org/tinyteeth), an oral health communications resource that aims to spark and support dialogue between a pregnant woman and her health care provider.
A rapid review of available research on the topic of caries prevention in children, as well as a series of key informant interviews, informed where there are gaps in the messages being communicated to the public about children’s oral health. For example, the information available on the topic of children’s oral health was extensive, but information on pregnant women was lacking. Recognizing that pregnancy is the stage when women are seeking information and are more receptive to lifestyle changes, draft creative concepts were developed and tested to specifically target pregnant women and those with very young children.
Using these concepts, focus groups were conducted in Alexandria, Virginia, and Orlando, Florida, with participants who were low-income mothers or expectant mothers who reported that they did not see a dentist during pregnancy or had not taken their child to the dentist and let their baby, at least sometimes, sleep with a bottle. Participants were segmented into three groups: pregnant women; first-time mothers with babies less than a year old; mothers with children between 1 and 3 years of age.
Creative concepts were inserted into a real parent or pregnancy magazine, alongside real advertisements, that participants were asked to skim through in the waiting room ahead of the focus group. This aimed to evaluate these concepts when performed in a simulated “real life” situation. Findings from these focus groups are summarized in Table 1.
Table 1.
Focus Group Findings
| 1. Mix up resonating creative. Similar approaches can be adopted from the creative elements that performed best. |
| 2. Be wary of tone. New moms are bombarded with criticism and unsolicited advice, which (understandably) makes them very sensitive to tone. Messages should avoid over-commanding statements. |
| 3. Frame a familiar issue in a new way. Viewing cavity prevention through the lens of bacteria prevention or the care of baby teeth can help moms understand and engage in an issue. |
| 4. You’re doing it “for two.” Pregnant women are very used to the phrase “for two” in the context of behaviors while pregnant. Drawing the connection between pregnancy, oral health care, and well-being of the baby using this phrase (like “brushing for two”) was well received with participants. |
| 5. Give the “why.” Moms are continually sifting through a barrage of often conflicting safety advice. Giving a rationale such as “pregnant women are at higher risk” can make the advice more believable. |
| 6. Provide an online resource for more information. Most moms said they needed to do more research before accepting the advice. Provide an online resource with trusted sources (such as AAP or CDC). |
AAP, American Academy of Pediatrics; CDC, Centers for Disease Control and Prevention.
From these concepts, the Protect Tiny Teeth toolkit was developed. It includes a mix of attention-grabbing materials for the woman to spark awareness that oral health should be part of routine care for them and for their infants. The toolkit also includes resources for medical providers and community liaisons with infographics and brief videos with tips for how to reach the target audience. These materials are designed to support assessing women’s and young children’s needs, talking points for a conversation about oral health, and resources to leave with the patient (Fig. 2).
FIG. 2.

Protect Tiny Teeth toolkit.
The Protect Tiny Teeth toolkit is available for free access on aap.org/tinyteeth with materials in English and Spanish and some materials available in multiple languages. A companion, consumer-facing website is also available at Healthychildren.org/tinyteeth. The first round of materials developed included two infographics (one for pregnant women and one for mothers of new babies), two short videos (one for pregnant women and one for mothers of new babies), two waiting-room posters (one focused on pregnancy and the other on early childhood oral health), and one provider brochure (Fig. 2). Promotion of the entire toolkit began in February 2019 in celebration of the National Children’s Dental Health Month.
Implementation Tips
More research and resources may help when seeking to improve women’s and health care providers’ attitudes and behaviors about the importance of oral health during pregnancy. Health care providers for women of reproductive age, including primary care and maternity care providers, may consider paying more careful attention to oral health. In some states, low-income pregnant women have access to some dental benefits through Medicaid, and maternity care providers may be able to provide linkages to assist pregnant women to needed dental care. Health care providers and dental professionals may provide education and counseling to assure their patients that dental care during pregnancy is safe and necessary.
The materials created for the Protect Tiny Teeth toolkit aim to raise awareness of this issue and make conversations between patients and providers easier. Those who interact with pregnant women and their families may consider using and sharing the free resources available in this toolkit.
Conclusion
The CDC and the AAP hope that Protect Tiny Teeth, the new oral health toolkit, will raise awareness of the importance of children’s oral health from the start—during pregnancy. Protect Tiny Teeth provides tools and resources for medical and dental providers who care for pregnant women. These materials help raise awareness about the importance of oral health as part of routine prenatal care, and support clinicians in talking with pregnant women about their oral health and the future oral health of their baby.
Disclaimer
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Footnotes
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Barak S, Oettinger-Barak O, Oettingern M, Machtei E, Peled M, Ohel G. Common oral manifestations during pregnancy: A review. Obstet Gynecol Surv 2003;58:624–628. [DOI] [PubMed] [Google Scholar]
- 2.Michalowicz BS, DiAngelis AJ, Novak MJ, et al. Examining the safety of dental treatment in pregnant women. J Am Dent Assoc 2008;139:685–695. [DOI] [PubMed] [Google Scholar]
- 3.Strafford KE, Shellhaas C, Hade EM. Provider and patient perceptions about dental care during pregnancy. J Matern Fetal Neonatal Med 2008;21:63–71. [DOI] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention. Selected 2012 through 2015 Maternal and Child Health (MCH) Indicators. PRAMS. Available at: www.cdc.gov/prams/pramstat/pdfs/mch-indicators/PRAMS-All-Sites-2012-2015-508.pdf Accessed November 30, 2018. [Google Scholar]
- 5.Gaffield ML, Colley Gilbert BJ, Malvitz DM, Romaguera R. Oral health during pregnancy: An analysis of information collected by the pregnancy risk assessment monitoring system. J Am Dent Assoc 2001;132:1009–1016. [DOI] [PubMed] [Google Scholar]
- 6.Al Habashneh R, Guthmiller JM, Levy S, et al. Factors related to utilization of dental services during pregnancy. J Clin Periodontol 2005;32:815–821. [DOI] [PubMed] [Google Scholar]
- 7.Russell SL, Mayberry LJ. Pregnancy and oral health: A review and recommendations to reduce gaps in practice and research. J Matern Child Nurs 2008;33:32. [DOI] [PubMed] [Google Scholar]
- 8.Christensen K, Gaist D, Jeune B, Vaupel JW. A tooth per child? Lancet 1998;352:204. [DOI] [PubMed] [Google Scholar]
- 9.Scheutz F, Baelum V, Matee MI, Mwangosi I. Motherhood and dental disease. Community Dent Health 2002;19:67–72. [PubMed] [Google Scholar]
- 10.American Dental Association Council on Access, Prevention, and Interprofessional Relations. Women’s oral health issues [white paper] 2006. Available at: http://ebusiness.ada.org/productcatalog/product.aspx?ID=2313 Accessed December 4, 2018.
- 11.Eke PI, Dye BA, Wei L, et al. Update on prevalence of periodontitis in adults in the United States: NHANES 2009 to 2012. J Periodontol 2015;86:611–622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Romero BC, Chiquito CS, Elejalde LE, Bernadoni CB. Relationship between periodontal disease in pregnant women and the nutritional condition of their newborns. J Periodontol 2002;73:1177–1183. [DOI] [PubMed] [Google Scholar]
- 13.Lieff S, Boggess KA, Murtha AP, et al. The oral conditions and pregnancy study: Periodontal status of a cohort of pregnant women. J Periodontol 2004;75:116–126. [DOI] [PubMed] [Google Scholar]
- 14.American Academy of Periodontology. Periodontal disease fact sheet. Available at: http://perio.org/newsroom/periodontal-disease-fact-sheet Accessed December 4, 2018. [Google Scholar]
- 15.Wu M, Chen S, Jiang S. Relationship between gingival inflammation and pregnancy. Mediators Inflamm 2015;2015:623427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Silk H, Douglass A, Douglass J, Silk L. Oral health during pregnancy. Am Fam Physician 2008;77:1139–1144. [PubMed] [Google Scholar]
- 17.Corbella S, Taschieri S, Del Fabbro M, Francetti L, Weinstein R, Ferrazzi E. Adverse pregnancy outcomes and periodontitis: A systematic review and meta-analysis exploring potential association. Quintessence Int 2016;47:193–204. [DOI] [PubMed] [Google Scholar]
- 18.Featherstone JDB. Prevention and reversal of dental caries: Role of low level fluoride. Community Dent Oral Epidemiol 1999;27:31–40. [DOI] [PubMed] [Google Scholar]
- 19.Azofeifa A, Yeung LF, Alverson CJ, Beltrán-Aguilar E. Dental caries and periodontal disease among U.S. pregnant women and nonpregnant women of reproductive age, National Health and Nutrition Examination Survey, 1999–2004. J Public Health Dent 2016;76:320–329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ismail SK, Kenney L. Review of hyperemesis gravidarum. Best Pract Res Clin Gastroenterol 2007;21:755–769. [DOI] [PubMed] [Google Scholar]
- 21.Lindquist B, Emilson CG. Colonization of Streptococcus mutans and Streptococcus sobrinus genotypes and caries development in children to mothers harboring both species. Caries Res 2004;38:95–103. [DOI] [PubMed] [Google Scholar]
- 22.Dye BA, Vargas CM, Lee JJ, Magder L, Tinanoff N. Assessing the relationship between children’s oral health status and that of their mothers. J Am Dent Assoc 2011;142:173–183. [DOI] [PubMed] [Google Scholar]
- 23.Jackson SL, Vann WF, Kotch JB, Pahel BT, Lee JY. Impact of poor oral health on children’s school attendance and performance. Am J Public Health 2011;101:1900–1906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wall TP, Vujicic M, Nasseh K. Recent trends in the utilization of dental care in the United States. Dent Educ 2012;76:1020–1027. [PubMed] [Google Scholar]
- 25.Markus AR, Andres E, West KD, Garro N, Pellegrini C. Medicaid Covered Births, 2008 Through 2010, in the Context of the Implementation of Health Reform. Womens Health Issues 2013;23:e273–e280. [DOI] [PubMed] [Google Scholar]
- 26.National Health Law Program. Dental coverage for low-income pregnant women. Issue brief 2012. Available at: https://healthlaw.org/resource/dental-coverage-for-low-income-pregnant-women Accessed December 4, 2018. [Google Scholar]
- 27.Smith K, Robinson M. Pregnancy Risk Assessment Monitoring System (PRAMS) [Presentation]. 2017. Available at: www.vdh.virginia.gov/content/uploads/sites/65/2017/06/PRAMS-101.pdf Accessed December 4, 2018. [Google Scholar]
- 28.ADA Health Policy Institute. Dentist participation in Medicaid or CHIP. Available at: www.ada.org/en/science-research/health-policy-institute/dental-statistics/dental-benefits-and-medicaid Accessed December 4, 2018. [Google Scholar]
- 29.Morgan MA, Crall J, Goldenberg RL, Schulkin J. Oral health during pregnancy. J Matern Fetal Neonatal Med 2009;22:733–739. [DOI] [PubMed] [Google Scholar]
- 30.Da Costa EP, Lee JY, Rozier RG, Zeldin L. Dental care for pregnant women: An assessment of North Carolina general dentists. J Am Dent Assoc 2010;141:986–994. [DOI] [PubMed] [Google Scholar]
- 31.George A, Shamim S, Johnson M, et al. How do dental and prenatal care practitioners perceive dental care during pregnancy? Current evidence and implications. Birth 2012;39:238–247. [DOI] [PubMed] [Google Scholar]


