Abstract
Background
Bipolar disorder is identified as a cause of severe damage to the physical, psychological and social functioning of adolescents and young adults.
Aims
The aim of this study is to ascertain the trends in the burden of bipolar disorder among individuals aged 10–24 years at global, regional and national levels from 1990 to 2019.
Methods
The data analysed in this study were from the Global Burden of Diseases 2019. The numbers, rates per 100 000 population, average annual percentage changes (AAPCs) of incidence, prevalence and years lived with disability (YLDs) of bipolar disorder are reported at the global, regional and national levels among individuals aged 10–24 years. Global trends by age, sex and Social Development Index (SDI) were further analysed.
Results
Globally, the incidence of bipolar disorder among adolescents and young adults increased from 79.21 per 100 000 population (95% uncertainty interval (UI): 58.13 to 105.15) in 1990 to 84.97 per 100 000 population (95% UI: 61.73 to 113.46) in 2019, AAPC 0.24 (95% confidence interval (CI): 0.22 to 0.26). In the past three decades, there has been an increase in incidence, prevalence and YLDs in both males and females. The largest increase in incidence between 1990 and 2019 was observed in those aged 20–24 years old (from 51.76 per 100 000 population (95% UI: 26.81 to 87.20) in 1990 to 58.37 per 100 000 population (95% UI: 30.39 to 98.55) in 2019; AAPC 0.42 (95% CI: 0.38 to 0.47)). By the SDI quintile, the largest increase in incidence was observed in the middle SDI; however, the high SDI countries had the highest incidence. Regionally, the largest increase in incidence was observed in southern Latin America. At the national level, the most pronounced increase in the incidence was in Greenland.
Conclusions
The global increase in incidence among adolescents and young adults between 1990 and 2019 indicates that strategies to improve their mental health still need to be emphasised.
Keywords: Bipolar Disorder, Adolescent Health Services, Adolescent Psychiatry
WHAT IS ALREADY KNOWN ON THIS TOPIC.
Bipolar disorder has a high burden among adolescents and young adults. However, the burden and trends of bipolar disorder in this population are less reported.
WHAT THIS STUDY ADDS
The burden of disease for bipolar disorder from 1990 to 2019 is reported, and secondary analysis of the data using Joinpoint regression reports the average annual percentage change.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
Consider incorporating the psychological characteristics of adolescents and young adults when developing health policies and services. Encourage governments and policymakers to make a more rational allocation of health resources.
Introduction
Mental health concerns are prevalent throughout the world and are clearly on the rise.1 According to the Global Burden of Diseases, Injuries, and Risk Factors Study (GBD) 2019, mental disorders remain among the top 10 global burden-causing conditions.2 Bipolar disorder is one of the most injurious psychiatric diseases. It is a common, recurrent mental health problem that can range in severity and is challenging to diagnose. It typically affects people who are more likely to have other mental health disorders, drug use disorders and associated chronic conditions.3 Bipolar disorder affects approximately 2.4% of the global population and is associated with reduced functioning, cognitive impairment and decreased quality of life as a lifelong and recurrent disorder.4 It is one of the leading causes of disability in young people and increases mortality, especially death by suicide.5 According to data from epidemiologic research, a person with bipolar disorder has a lifetime risk of suicide attempt of 29.2% compared with 15.9% for a person with a unipolar condition.6
The first episode of bipolar disorder can occur at any age. However, the most common age of onset appears to be between 15 and 19 years.7 It has been demonstrated that the age of the first episode of bipolar disorder is a significant predictor of prognosis, with early onset—especially before puberty—being linked to greater comorbidity, poorer quality of life and the most severe functional impairment.8 Adolescence is a remarkably unique period, implying rapid physical growth and a major transformation of social roles. World Health Organization defines 10–19 years as adolescents. However, as society has evolved and adolescents’ physical development and major social role transitions have changed, it would be more beneficial to expand the definition of young people to include the age group of 10–24 years old to develop an appropriate service system.9 The 10–24-year-old group comprises a quarter of the world’s population, and mental disorders are pervasive among these young people.10 Adolescents with mental health problems are more prone to social isolation, discrimination, stigmatisation (which impacts their motivation to seek care), difficulty in education, risk-taking behaviours, poor physical health and human rights abuses.
Bipolar disorder imposes a serious disease burden on adolescents and young adults. Their burden extends to include high rates of substance abuse, hospitalisations, legal problems, academic and psychosocial dysfunction and suicide.11 In a Canadian community health survey, the incidence rate of psychiatric comorbidities is very high, and nearly half of the young people with bipolar disorder have anxiety, problematic drug use and suicidal behaviour.12 Adolescent suicide not only negatively impacts parents and families but also profoundly affects teachers and peers at school.13 According to self-reported health, youth with bipolar disorder had poorer quality of life compared with healthy youth, youth with chronic conditions, youth with behavioural disorders and youth with other non-behavioural/non-emotional disorders.14 Unfortunately, approximately only 56.1% of youth with bipolar disorder have received mental health services.12
There is a growing consensus that bipolar disorder in adolescents and young adults is a major public health problem. Despite an increased awareness of the problem, there is little published literature assessing the global burden of bipolar disorder in young populations. The aetiology of mood disorders has been extensively studied at the individual level, but their characterisation at the population level has not received much attention.15 Previous studies of global bipolar disorder have targeted all age groups, using age-standardised rates to examine the global burden.16 He et al described the prevalence and burden of bipolar disorder using 2017 Global Burden of Diseases data, assessing only 195 countries.17 Thus, based on the latest data from GBD 2019, we analysed the global, regional and national levels of bipolar disorder among adolescents and young adults and their trends from 1990 to 2019. This study aims to facilitate stakeholder access and interpretation of GBD 2019 estimates, thereby providing policy recommendations for the prevention of adolescent mental illnesses and the improvement of adolescent mental health, especially for bipolar disorder.
Methods
Study population and data collection
Data in this article were collected from the Global Health Data Exchange.18 It is a public database and contains incidence, prevalence, mortality, years lived with disability (YLDs), years of life lost (YLLs) and disability-adjusted life years (DALYs) data from 1990 to 2019 for 369 diseases and injuries for males and females in 23 age groups from 21 regions and 204 countries and territories.16 The GBD data were extracted from national censuses, disease registries, civil registration and vital statistics, health service use, and from reviewing the published literature on the incidence and prevalence of various diseases and other sources. To ensure consistency between the incidence, prevalence, remission, excess mortality and cause-specific mortality for most causes, GBD 2019 used the Bayesian meta-regression modelling tool DisMod-MR V.2.1.16 The GBD project provides a wealth of data on the burden of disease that can be effectively used to support health decision-making and policy at the local, regional, national and global levels.
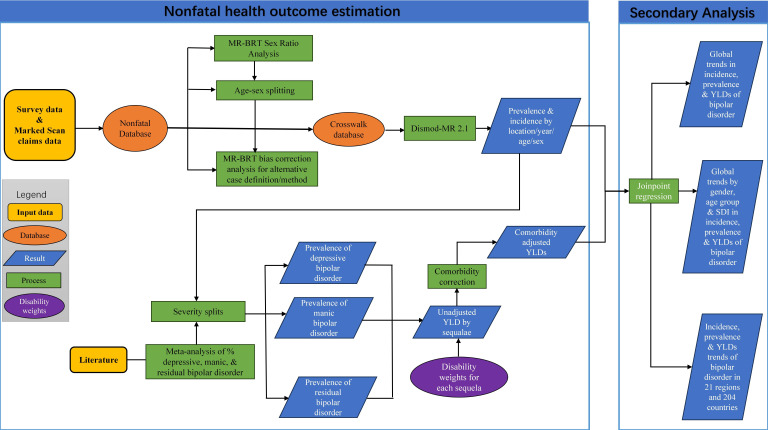
The mental disorders included in the GBD 2019 were depressive disorders, anxiety disorders, bipolar disorder, schizophrenia, autism spectrum disorders, conduct disorder, attention-deficit hyperactivity disorder, eating disorders, idiopathic developmental, intellectual disability and a residual category of other mental disorders.2 Bipolar disorder is a mood disorder that incorporates disability from manic, hypomanic or major depressive episodes.19 Included in the GBD disease modelling were cases meeting diagnostic criteria for bipolar disorder according to the Diagnostic and Statistical Manual of Mental Disorders-Fourth Edition, Text Revision (DSM-IV-TR) or the equivalent diagnosis in the International Classification of Diseases (ICD).16 These are identified by the following codes: DSM-IV-TR: 296.0–296.7, 296.89, 301.13; ICD-10: F30.0–F30.9, F31.0–F31.6, F31.8–F31.9, F34.0. The exclusions were bipolar disorder due to a general medical condition or substance-induced cases. A diagnosis of bipolar disorder involves the experience of one or more manic, hypomanic and/or major depressive episodes. According to DSM-IV-TR, a manic episode involves the experience of elevated, expansive or irritable mood lasting for at least 1 week. The specific process can be viewed in figure 1 and retrieved in another article.16
Figure 1.
Study flowchart. The diagram depicts the inclusion and exclusion criteria, the Bayesian meta-regression modelling process for bipolar disorder data in the Global Burden of Diseases database and the secondary analysis process. MR-BRT, Meta-Regression-Bayesian Regularised Trimmed; SDI, Social Development Index; YLDs, years lived with disability.
The data on incidence, prevalence and YLDs were collected from both sexes in 4 age groups (10–14 years, 15–19 years, 20–24 years and 10–24 years) and by the 21 regional groupings of countries that are geographically close and epidemiologically similar. YLDs are expressed as the number of years lived with any short-term or long-term health loss, weighted by the severity of the disability weights. In the GBD database, YLLs are not estimated for mental disorders that are not recognised as causes of death. YLDs approximate DALYs,2 so YLDs are used directly to indicate the burden of disease rather than DALYs. All rates were reported per 100 000 population. The 95% uncertainty intervals (UIs) were defined by the 25th and 75th values of the ordered 1000 estimates based on the GBD’s algorithm.
The Social Demographic Index (SDI) is a metric provided by GBD 2019 for each country. SDI is a composite index of developmental status strongly correlated with health outcomes. It is the geometric mean of the total fertility rate under age 25, the average education of those who are 15 years and older and the lagged distributed income per capita index. SDI serves as a composite index that classifies countries into five classes: low, low middle, middle, high middle and high. The index takes on a range of values from 0 to 1, with 0 indicating that the location would have the lowest theoretical level of health-related development and 1 indicating that the location would have the highest theoretical level.20
This study follows the Guidelines for Accurate and Transparent Health Estimates Reporting Guidelines for cross-sectional studies.
Statistical analysis
This research mainly adopts the Joinpoint regression model to analyse the temporal trend of global, regional and national bipolar disorder in adolescents and young adults from 1990 to 2019.
Traditional regression methods typically assess the overall disease trend across the entire study period, lacking the ability to reveal localised variations. Joinpoint regression, conversely, is centred on segmenting the regression based on disease temporal distribution characteristics. By segmenting the study period at various inflection points and optimising trend analysis within each segment, this approach allows for a detailed assessment of disease change across different time intervals within the entire study duration. It yields more nuanced insights into trend changes, so we opted for the Joinpoint regression model.
Because our analysis concerns the incidence, prevalence and YLD rate of bipolar disorder, we opted for the log-linear model. In addition, we adopted the default modelling method of Joinpoint—the grid search method, and the Monte Carlo permutation test was used for model optimisation. For a comprehensive understanding of the regression equation and further methodological details, please refer to the cited source.21 22
The data from 1990 to 2019 were divided by every decade in the analysis. In the text, we report the average annual percentage change (AAPC) from 1990 to 1999, 2000 to 2009, 2010 to 2019 and 1990 to 2019, as well as the years with the most significant changes in trend. Global trends are then stratified by age group, gender and SDI. Finally, regional and national trends are presented in the text.
The AAPC of the trends was obtained by Joinpoint regression. This model constructs a piecewise regression and performs trend fitting and optimisation on the data points in each segment based on the temporal properties of the disease distribution. By joining a number of different line segments on a logarithmic scale, the Joinpoint regression analysis is used to pinpoint the years with the most notable trends in the measures mentioned above. The simplest model (ie, 0 joinpoints) is a straight line. Each joinpoint is checked using the Monte Carlo permutation approach as additional joinpoints are added. The final model of the Joinpoint programme was chosen based on the authors’ expert knowledge and the Weighted Bayesian Information Criterion approaches.
The AAPC is a summary measure of the trend over a prespecified fixed interval and is calculated as a weighted average of annual percentage change (APC). It is a summary assessment of the trend over a predetermined fixed time. The different yearly percentage change data from the regression analysis were geometrically weighted to get the APC. The AAPC value represents the percent change that happens annually (increase, reduction or no change). For instance, if the AAPC value is 0, it indicates that there has not been any change to the annual growth rate. The rate pattern is displayed by the AAPC value and its 95% confidence interval (CI).
All statistical analyses were performed using R software (V.4.2.2) and the Joinpoint Regression Program (V.4.6.0.0). The data processed in this paper used the tidyverse package and easyGBDR package.
Results
Global trends
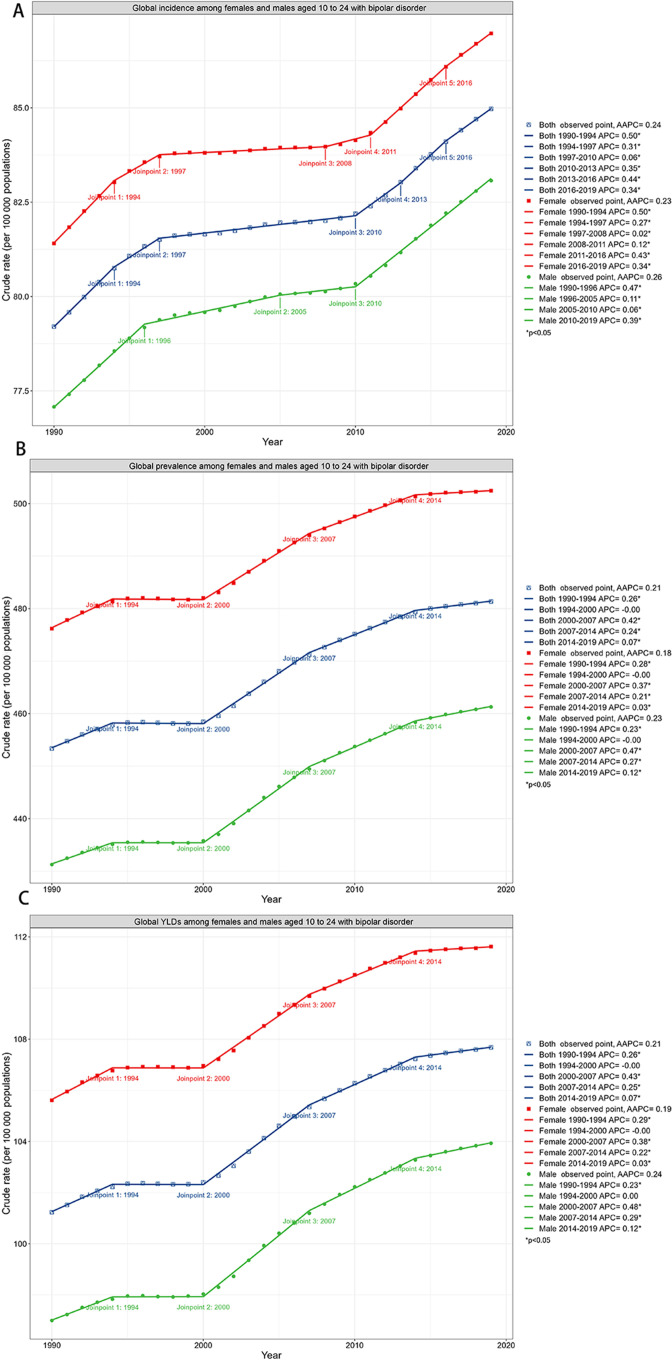
Globally, the incidence of bipolar disorders among adolescents and young adults increased slowly between 1990 and 2019 (AAPC 0.24 (95% CI: 0.22 to 0.26)). Meanwhile, it is also evident from the graph that the AAPC was rising over these three decades (table 1). Specific years in which incidence rates climbed significantly were 1994, 2010, 2013 and 2016. After being divided by decade, the incidence increased faster between 1990 and 1999 (AAPC 0.34 (95% CI: 0.30 to 0.37)), increased slower between 2000 and 2009 (AAPC 0.06 (95% CI: 0.05 to 0.06)) and continued to increase, but at a quicker rate, between 2010 and 2019 (AAPC 0.38 (95% CI: 0.33 to 0.43)). Overall, the incidence increased from 79.21 per 100 000 (95% UI: 58.13 to 105.15) in 1990 to 84.97 per 100 000 (95% UI: 61.73 to 113.46) in 2019. It is worth noting that not only was the incidence increasing, but the prevalence and YLDs were also rising. The prevalence and YLDs increased at a significant rate starting in 2000 (table 1 and figure 2).
Table 1.
Global average AAPC in incidence, prevalence and YLDs of bipolar disorders
| Sex | Years | Incidence | Prevalence | YLDs | |||
| AAPC (95% CI) | P value | AAPC (95% CI) | P value | AAPC (95% CI) | P value | ||
| All | 1990–1999 | 0.34 (0.30 to 0.37) | <0.001 | 0.11 (0.10 to 0.13) | <0.001 | 0.12 (0.10 to 0.13) | <0.001 |
| 2000–2009 | 0.06 (0.05 to 0.06) | <0.001 | 0.38 (0.37 to 0.39) | <0.001 | 0.39 (0.38 to 0.40) | <0.001 | |
| 2010–2019 | 0.38 (0.33 to 0.43) | <0.001 | 0.15 (0.14 to 0.16) | <0.001 | 0.15 (0.14 to 0.17) | <0.001 | |
| 1990–2019 | 0.24 (0.22 to 0.26) | <0.001 | 0.21 (0.20 to 0.21) | <0.001 | 0.21 (0.20 to 0.22) | <0.001 | |
| Female | 1990–1999 | 0.32 (0.30 to 0.34) | <0.001 | 0.13 (0.11 to 0.14) | <0.001 | 0.13 (0.11 to 0.15) | <0.001 |
| 2000–2009 | 0.03 (0.03 to 0.04) | <0.001 | 0.34 (0.33 to 0.34) | <0.001 | 0.34 (0.33 to 0.36) | <0.001 | |
| 2010–2019 | 0.37 (0.35 to 0.38) | <0.001 | 0.11 (0.10 to 0.12) | <0.001 | 0.11 (0.10 to 0.13) | <0.001 | |
| 1990–2019 | 0.23 (0.22 to 0.24) | <0.001 | 0.18 (0.18 to 0.19) | <0.001 | 0.19 (0.18 to 0.20) | <0.001 | |
| Male | 1990–1999 | 0.35 (0.33 to 0.36) | <0.001 | 0.10 (0.09 to 0.12) | <0.001 | 0.10 (0.08 to 0.13) | <0.001 |
| 2000–2009 | 0.08 (0.06 to 0.10) | <0.001 | 0.43 (0.41 to 0.44) | <0.001 | 0.44 (0.42 to 0.46) | <0.001 | |
| 2010–2019 | 0.39 (0.38 to 0.40) | <0.001 | 0.19 (0.17 to 0.20) | <0.001 | 0.19 (0.17 to 0.21) | <0.001 | |
| 1990–2019 | 0.26 (0.25 to 0.27) | <0.001 | 0.23 (0.22 to 0.24) | <0.001 | 0.24 (0.23 to 0.25) | <0.001 | |
AAPC, average annual percentage change; CI, confidence interval; YLDs, years lived with disability.
Figure 2.
Joinpoint regression analysis of global bipolar disorder incidence, prevalence and years lived with disability (YLDs) of all, female and male adolescents and young adults ages 10–24 from 1990 to 2019. *p<0.05; AAPC, average annual percentage change; APC, annual percentage change; YLDs, years lived with disability.
Global trends by sex
There were global increases in bipolar disorder incidence from 1990 to 2019 in both females and males, with an AAPC of 0.23 in females (95% CI: 0.22 to 0.24; from 81.41 per 100 000 population (95% UI: 59.86 to 107.91) in 1990 to 86.97 per 100 000 population (95% UI: 63.04 to 116.17) in 2019). The AAPC for males was 0.26 (95% CI: 0.25 to 0.27; from 77.08 per 100 000 population (95% UI: 56.63 to 101.71) in 1990 to 83.07 per 100 000 population (95% UI: 60.55 to 110.88) in 2019). Among 1 582 095 global incident bipolar disorder cases in 2019, 790 028 (49.9%) occurred in females. Both males and females have had increases in the prevalence and YLDs in the past three decades, and there is little difference in trends between the sexes (figure 2; see online supplemental table S1).
gpsych-2023-101255supp001.pdf (647.1KB, pdf)
Global trends by age group
In 2019, those aged 15–19 years accounted for 669 188 (42.3%) of 1 582 095 incident cases among adolescents. Whether in 1990 or 2019, it is important to note that the number of incidences peaked at ages 15–19 years, followed by ages 10–14 years.
Globally, the largest growth in incidence between 1990 and 2019 was observed in those aged 20–24 years old (from 51.76 per 100 000 population (95% UI: 26.81 to 87.20) in 1990 to 58.37 per 100 000 population (95% UI: 30.39 to 98.55) in 2019; AAPC 0.42 (95% CI: 0.38 to 0.47)). Individuals aged 10–14 and 15–19 years also had an increase in incidence in the same period (from 84.04 per 100 000 population (95% UI 55.88 to 120.85) to 87.60 per 100 000 population (95% UI: 57.12 to 127.23); AAPC 0.14 (95% CI: 0.12 to 0.16) and 100.24 per 100 000 population (95% UI: 71.28 to 133.75) to 108.01 per 100 000 population (95% UI: 76.05 to 144.96); AAPC 0.26 (95% CI: 0.23 to 0.29)). The biggest growth in YLDs between 1990 and 2019 was observed in those aged 20–24 years (from 149.54 per 100 000 population (95% UI: 82.60 to 238.34) to 160.39 per 100 000 population (95% UI: 88.67 to 259.87); AAPC 0.25 (95% CI: 0.22 to 0.29)) (table 2). From 1990 to 2019, YLDs in all three age subgroups increased.
Table 2.
Global AAPC in incidence, prevalence and YLDs of bipolar disorders for age group
| Measure | Age group | 1990 | 2019 | AAPC (95% CI) |
||
| Case (95% UI) | Rate (per 100 000 population) | Case (95% UI) | Rate (per 100 000 population) | |||
| Incidence | 10–14 years | 451 052 (299 908 to 648 607) |
84.04 (55.88 to 120.85) | 562 576 (366 786 to 817 066) |
87.60 (57.12 to 127.23) | 0.14 (0.12 to 0.16) |
| 15–19 years | 520 826 (370 382 to 694 989) |
100.24 (71.28 to 133.75) | 669 188 (471 156 to 898 091) |
108.01 (76.05 to 144.96) | 0.26 (0.23 to 0.29) | |
| 20–24 years | 255 004 (132 066 to 429 590) |
51.76 (26.81 to 87.20) | 350 330 (182 388 to 591 447) |
58.37 (30.39 to 98.55) | 0.42 (0.38 to 0.47) | |
| 10–24 years | 1 226 881 (900 359 to 1 628 735) |
79.21 (58.13 to 105.15) | 1 582 095 (1 149 314 to 2 112 550) |
84.97 (61.73 to 113.46) | 0.24 (0.22 to 0.26) | |
| Prevalence | 10–14 years | 839 246 (556 043 to 1 197 801) |
156.37 (103.61 to 223.18) | 1 041 235 (682 882 to 1 504 146) |
162.14 (106.34 to 234.22) | 0.12 (0.10 to 0.14) |
| 15–19 years | 2 865 528 (2 001 573 to 3 915 037) |
551.48 (385.21 to 753.47) | 3 597 746 (2 491 755 to 4 951 051) |
580.71 (402.19 to 799.15) | 0.18 (0.15 to 0.21) | |
| 20–24 years | 3 317 656 (2 410 097 to 4 357 385) |
673.40 (489.19 to 884.43) | 4 323 451 (3 110 479 to 5 737 334) |
720.40 (518.29 to 955.99) | 0.24 (0.21 to 0.28) | |
| 10–24 years | 7 022 430 (5 097 382 to 9 329 749) |
453.36 (329.08 to 602.32) | 8 962 431 (6 442 959 to12 010 590) |
481.37 (346.05 to 645.08) | 0.21 (0.20 to 0.21) | |
| YLDs | 10–14 years | 189 777 (95 636 to 315 204) |
35.36 (17.82 to 58.73) | 235 697 (118 102 to 396 052) |
36.70 (18.39 to 61.67) | 0.13 (0.10 to 0.15) |
| 15–19 years | 641 554 (335 889 to 1 038 508) |
123.47 (64.64 to 199.87) | 806 688 (420 974 to 1 310 681) |
130.21 (67.95 to 211.56) | 0.19 (0.16 to 0.22) | |
| 20–24 years | 736 761 (406 970 to 1 174 262) |
149.54 (82.60 to 238.34) | 962 550 (532 149 to 1 559 610) |
160.39 (88.67 to 259.87) | 0.25 (0.22 to 0.29) | |
| 10–24 years | 1 568 093 (864 253 to 2 483 445) |
101.23 (55.80 to 160.33) | 2 004 935 (1 085 274 to 3 224 662) |
107.68 (58.29 to 173.19) | 0.21 (0.20 to 0.22) | |
AAPC, global average annual percentage change; CI, confidence interval; UI, uncertainty interval; YLDs, years lived with disability.
Global trends by SDI
Incidence AAPC shows an upward trend in all five different levels of SDI regions during the 30 years. The largest increase in incidence by SDI was observed in the middle SDI (from 69.27 per 100 000 population (95% UI: 50.76 to 91.94) in 1990 to 77.84 per 100 000 population (95% UI: 56.43 to 104.26) in 2019, AAPC 0.41 (95%CI: 0.38 to 0.43)). The minimum increase in incidence by SDI was observed in the low SDI region. Except for the low SDI region, all other SDI regions showed a higher incidence AAPC growth rate in males compared to females. Notably, in 2019, the high SDI countries had the highest incidence (120.29 per 100 000 population (95% UI: 96.13 to 148.64)), with only this region having a higher incidence rate in males than females.
Meanwhile, middle SDI countries still had the largest increase in YLDs (from 87.48 per 100 000 population (95% UI: 47.53 to 138.04) in 1990 to 100.59 per 100 000 population (95% UI: 54.92 to 162.14) in 2019; AAPC 0.48 (95% CI: 0.46 to 0.50)) (see online supplemental tables S1, S2 and S3).
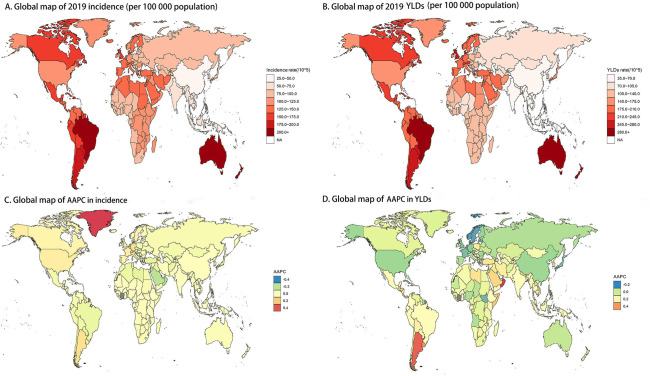
Regional trends
At the regional level, the largest increases in incidence between 1990 and 2019 were observed in Southern Latin America (from 166.56 per 100 000 population (95% UI: 112.80 to 236.23) in 1990 to 174.97 per 100 000 population (95% UI: 117.35 to 247.19) in 2019; AAPC 0.17 (95% CI: 0.15 to 0.18)), Western Europe (from 127.59 per 100 000 population (95% UI: 93.11 to 170.13) to 132.14 per 100 000 population (95% UI: 97.64 to 174.29); AAPC 0.12 (95% CI: 0.11 to 0.14)) and high-income North America (from 121.04 per 100 000 population (95% UI: 104.71 to 137.38) to 124.30 per 100 000 population (95% UI: 107.78 to 141.01); AAPC 0.09 (95% CI: 0.07 to 0.12); table 2). Between 1990 and 2019, Southern Latin America had the largest increase in YLDs both due to bipolar disorder (from 221.26 per 100 000 population (95% UI: 113.53 to 383.06) to 249.76 per 100 000 population (95% UI: 131.65 to 417.52) and AAPC 0.42 (95% CI: 0.38 to 0.46). Notably, in 2019, Australasia was the region with the highest incidence and YLDs of bipolar disorder (219.97 per 100 000 population (95% UI: 163.06 to 280.24); 315.08 per 100 000 population (95% UI: 180.38 to 501.78) and East Asia was the region with the lowest incidence and YLDs of bipolar disorder (27.14 per 100 000 population (95% UI: 19.89 to 35.60); 38.33 per 100 000 population (95% UI: 21.33 to 60.67); see online supplemental tables S1,S2 ans S3).
National trends
At the national level, the most pronounced increase in the incidence of bipolar disorder between 1990 and 2019 was in Greenland (from 107.40 per 100 000 population (95% UI: 73.13 to 150.84) to 121.88 (95% UI: 81.17 to 173.95); AAPC 0.44 (95% CI: 0.38 to 0.50)) and the most pronounced decrease in the incidence was in Qatar (from 127.42 per 100 000 population (95% UI: 83.69 to 182.71) to 113.65 (95% UI: 73.49 to 165.74); AAPC −0.40 (95% CI: −0.44 to −0.37)). Notably, the country with the highest incidence in 2019 was New Zealand (291.86 per 100 000 population (95% UI: 219.40 to 373.85) and the region with the lowest incidence in 2019 was Taiwan (province of China) (26.18 per 100 000 population (95% UI: 16.88 to 38.40); figure 3; online supplemental tables S4,S5 and S6).
Figure 3.
Global map of 2019 incidence of bipolar disorder (A) and years lived with disability (YLDs) (B) and average annual percentage change (AAPC) in the incidence of bipolar disorder (C) and YLDs (D) from 1990 to 2019. NA, not available.
Discussion
Main findings
Previous investigations have shown that there are various conditions associated with mental disorders. The distribution of the risk burden among adolescents and young adults across areas requires more study. Compared with the previous GBD study, which looked at the prevalence of mental illness across all age groups, we provide a more extensive and in-depth analysis of bipolar disorder among adolescents and young adults aged 10–24 years. To our knowledge, this is the first study to describe the prevalence and rate of change of bipolar disorder among adolescents and young adults aged 10–24 years in 204 countries at global, regional and national levels from 1990 to 2019.
The incidence of bipolar disorder in adolescents and young adults has increased every year since 1990. In 2019, those aged 15–19 years accounted for 669 188 (42.3%) of 1 582 095 cases among adolescents. Among adolescents and young adults, the group aged 15–19 takes up the largest proportion of bipolar disorder cases and presents the highest incidence. Globally, however, the greatest increase in incidence and YLDs was seen in the 20–24 age group (AAPC 0.42 (95% CI: 0.38 to 0.47)). This may be linked to global population growth.23 Especially from 2010 to 2019, the growth rate of incidence is greater than that of the previous two decades (AAPC 0.38 (95% CI: 0.33 to 0.43)).
Prevalence, incidence and YLDs of bipolar disorder did not differ significantly between males and females over the past 30 years. However, the overall prevalence, incidence and YLDs in females were slightly higher than those in males. In the past, many studies have discussed whether there is a gender difference in the prevalence and incidence of bipolar disorder. One ‘received wisdom’ is that there is no significant gender difference in bipolar disorder. Most studies also found almost equal sex ratios for 12 months and lifetime prevalence of bipolar disorder.24 However, studies have found that females are more likely to have rapid cycling, more mixed states, greater severity of acute episodes and a more severe course of illness than males.25 In addition, although the prevalence is comparable, females are more likely to receive specialist services for bipolar disorder,26 which may contribute to the higher prevalence of bipolar disorder in females because it is more likely to be diagnosed.
The incidence and burden of bipolar disorder among adolescents and young adults varies considerably by region and country according to the SDI. At the regional level, Australasia was the region with the highest incidence and YLDs of bipolar disorder (219.97 per 100 000 population (95% UI: 163.06 to 280.24) and 315.08 per 100 000 population (95% UI: 180.38 to 501.78), respectively), while East Asia was the region with the lowest incidence and YLDs (27.14 per 100 000 population (95% UI: 19.89 to 35.60) and 38.33 per 100 000 population (95% UI: 21.33 to 60.67), respectively) and the largest increase in incidence between 1990 and 2019 was observed in Southern Latin America (AAPC 0.17 (95% CI: 0.15 to 0.18)). This may be because Australasia provides the most complete data on the prevalence of common mental disorders.27
Bipolar disorder is the third leading cause of the burden of mental disorders among adolescents and young adults aged 15–24 years, and the burden has continued to grow since 1990 with no evidence of a reduction.2 Without intervention, this burden is likely to keep increasing. Specifically, inadequate global mental capital and unmet treatment needs among many adolescents with bipolar disorder may worsen this burden.28 The current low global median spending on mental health (US$2.50 per person annually, less than 2% of total health spending) may be a major reason for the large gap between young people’s mental health needs and the availability of preventive interventions.28 Some northern European countries have seen decreasing disease burden over the past 30 years, but the burden remains high in most countries across Europe. Although there are more financial investments and evidence-based interventions in high-income Europe than in other regions, services still fall far short of adolescents’ vast needs.29 Southern Latin America, experiencing the fastest growth in YLD over the past three decades and comprising more low-income and middle-income countries, has even less mental health capital to cope with the growing burden.28 30 Resources for preventing adolescent bipolar disorder and promoting mental health are unequally distributed around the world, and access to mental health services is severely inadequate for adolescents, especially in low-income and middle-income countries. Therefore, greater investments and initiatives to stem the rising burden are urgently needed.
The trend of increasing incidence of AAPC was observed in all five differing levels of SDI areas during the three decades. Middle SDI countries had the largest increase in incidence among adolescents and young adults (AAPC 0.41 (95% CI: 0.38 to 0.43)). Although growing at a slower rate, the high SDI and low SDI countries had a considerable number of original morbidity cases, far exceeding the other countries. Middle SDI countries did not have high incidence rates, but over three decades of development, the highest growth rates were observed in these countries, most likely due to economic and social changes. Thus, mental illness is now the most critical health problem facing the young in both developing and developed countries.31
In many global mental health studies, an intriguing observation emerges: high-income countries tend to exhibit higher prevalence rates of mental disorders (similar to the results of this study), although this seems perverse.32 33 A high proportion of individuals residing in less developed or low-income countries are at risk of mental disorders due to extreme stress caused by poverty, violence and disasters. Conversely, in developed countries, most individuals are shielded from these adversities. Why do high-income or developed countries exhibit a higher prevalence of mental disorders? One explanation is based on the ‘hedonic treadmill’ theory, in which people’s expectations rise in parallel with their wealth, which can lead to stagnation of happiness and even depression.32 34Simultaneously, some scholars combine this theory and infer that societal context moderates the pathogenic effect of stressors.33 35 For example, the same traumatic event, such as a car accident, may cause less psychological trauma to individuals after it occurs in a war-torn country than in a developed country.
Furthermore, social inequality may play a prominent role in the high prevalence in developed countries. This contribution may be particularly pronounced among those who are least likely to experience the socioeconomic advantages enjoyed by their wealthier compatriots in developed countries.32 This subgroup could be more susceptible to psychological trauma, especially based on the ‘hedonism treadmill’ theory, where the gap between the expectations and the actual wealth may be even more pronounced among these marginalised groups in developed countries.
As the results demonstrate, the burden of bipolar disorder disease has been increasing among adolescents and young adults. Adolescents with bipolar disorder suffer long-term effects such as an increase in unpleasant life events and a resulting decline in quality of life.36 In the psychological aspect, these age groups with bipolar disorder typically have poorer self-esteem, more hopelessness, more traumatic life events and more trouble controlling their emotions in situations that can make them angry.37
With the transformation of the job market, the use of high technology means that education is very significant. Several adolescents and young people have interrupted their education or work as a result of their diseases. A family and society invest a great deal of time and money in the development of an adolescent. If an adolescent has bipolar disorder during adolescence, there is not only a loss of upfront investment but also a loss of potential for future realisation, resulting in a loss of productivity. Despite the obvious and significant economic costs of mental illness, sufficient funding for this field has been woefully underfunded globally, particularly in non‐WEIRD (western, educated, industrialized, rich and democratic) countries.10 This situation results from several causes, including the prevalence of infectious diseases, widespread poverty, a lack of political stability and will, and inadequate infrastructure.10
The enormous burden of mental health disorders has reminded many leaders and researchers that despite the actions that have been taken, measures may be inefficient in terms of outcomes.38 First, adolescence is a very unique time, which dictates that alleviating their disease burden must consider some of the adolescents’ individual conditions. Psychopharmacotherapy, in conjunction with psychosocial therapies, is advised for treating bipolar disorder in adolescents.39 Second, adolescents may choose not to seek health services because of stigma and embarrassment, poor mental health knowledge and a preference for self-reliance.40 Destigmatisation is, therefore, also an important means of improving mental health. In addition, it is also vital to raise the health awareness of caregivers because their perceptions of mental illness stigmatisation can also affect mental health service utilisation and health expenditures.41
Last but not least, mental health services in the regions need to undergo transformational reforms to better meet the needs of young people.31 At the same time, interventions should focus not only on students within the education system but also on those outside the education system. However, the insufficient number of psychiatric professionals may also be a significant factor leading to the current unmet need for services for adolescents and young adults with bipolar disorder.42 This, therefore, requires that we design different services and interventions for bipolar disorder that consider different regional contexts and the different needs of adolescents and young adults, as well as scaling up mental health funding.
Limitations
Despite considerable efforts to provide a comprehensive analysis, limitations still exist in the study. First of all, this article fails to confirm that the prevalence of bipolar disorder is different among ethnic groups. Diverse ethnic populations cannot be accessed through GBD studies, so ethnicity information should be collected and analysed in future studies. Second, deaths attributable to bipolar disorder were not reported in GBD 2019, and thus, YLLs were not found. Finally, this study addresses analysis at the national and regional levels and cannot extrapolate conclusions from the microlevel (communities, individuals) to avoid ecological fallacies.
Implications
The findings of this study indicate a rise in the prevalence of bipolar disorder in adolescents and young adults globally between 1990 and 2019, with marked regional differences. There is an urgent need to expand funding for mental health, destigmatise mental disorders, design interventions and provide specialist services for bipolar disorder tailored to different regions and adolescents and young adults.
Acknowledgments
Thanks to Yuancun Li and Xiao Ming for sharing the Global Burden of Disease (GBD) database analysis procedure, making exploring the GBD database easier.
Biographies
Yunxi Zhong obtained her bachelor's degree from Shanxi Medical University in China. Currently, she is pursuing her master's degree at the Health Management and Policy Research Center, School of Public Health, Shandong University, China. Her master’s study is under the supervision of Professor Long Sun. Her main research interests include public mental health and health services research.

Yifan Chen obtained his bachelor's degree in public affairs administration from Chongqing Medical University in China in 2022. Yifan is currently studying in a master’s program at the Health Management and Policy Research Center, School of Public Health, Shandong University, Jinan, China. His master’s study is under the supervision of Professor Long Sun. His main research interests include the global burden of disease of mental health and mental health services and policies to promote population mental health.
Footnotes
YZ and YC contributed equally.
Contributors: YZ: conceptualisation, formal analysis, methodology, software, supervision, visualisation, writing the original draft, review and editing. YC: conceptualisation, formal analysis, methodology, software, writing the original draft, review and editing. XS: supervision, review and editing. MW: supervision, review and editing. QL: supervision, review and editing. ZS: supervision, review and editing. LS: conceptualisation, funding acquisition, project administration, supervision, review and editing. LS is responsible for the overall content as the guarantor, accepts full responsibility for the work and/or the conduct of the study, has access to the data, and controlls the decision to publish. YZ and YC are the co-first authors.
Funding: This work was supported by the National Natural Science Foundation of China (grant number 71974114).
Map disclaimer: The inclusion of any map (including the depiction of any boundaries therein), or of any geographic or locational reference, does not imply the expression of any opinion whatsoever on the part of BMJ concerning the legal status of any country, territory, jurisdiction or area or of its authorities. Any such expression remains solely that of the relevant source and is not endorsed by BMJ. Maps are provided without any warranty of any kind, either express or implied.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available in a public, open access repository. Data in this article were collected from the Global Health Data Exchange (https://vizhub.healthdata.org/gbd-results/).
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
Not applicable.
References
- 1. Shah SM, Sun T, Xu W, et al. The mental health of China and Pakistan, mental health laws and COVID-19 mental health policies: a comparative review. Gen Psychiatr 2022;35:e100885. 10.1136/gpsych-2022-100885 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. GBD 2019 Mental Disorders Collaborators . Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990-2019: a systematic analysis for the global burden of disease study 2019. Lancet Psychiatry 2022;9:137–50. 10.1016/S2215-0366(21)00395-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Marzani G, Price Neff A. Bipolar disorders: evaluation and treatment. Am Fam Physician 2021;103:227–39. [PubMed] [Google Scholar]
- 4. Bonnín CDM, Reinares M, Martínez-Arán A, et al. Improving functioning, quality of life, and well-being in patients with bipolar disorder. Int J Neuropsychopharmacol 2019;22:467–77. 10.1093/ijnp/pyz018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Grande I, Berk M, Birmaher B, et al. Bipolar disorder. The Lancet 2016;387:1561–72. 10.1016/S0140-6736(15)00241-X [DOI] [PubMed] [Google Scholar]
- 6. Chen Y-W, Dilsaver SC. Lifetime rates of suicide attempts among subjects with bipolar and unipolar disorders relative to subjects with other axis I disorders. Biological Psychiatry 1996;39:896–9. 10.1016/0006-3223(95)00295-2 [DOI] [PubMed] [Google Scholar]
- 7. Sajatovic M. Bipolar disorder: disease burden. Am J Manag Care 2005;11:S80–4. [PubMed] [Google Scholar]
- 8. Moor S, Crowe M, Luty S, et al. Effects of comorbidity and early age of onset in young people with bipolar disorder on self harming behaviour and suicide attempts. Journal of Affective Disorders 2012;136:1212–5. 10.1016/j.jad.2011.10.018 [DOI] [PubMed] [Google Scholar]
- 9. Sawyer SM, Azzopardi PS, Wickremarathne D, et al. The age of adolescence. Lancet Child Adolesc Health 2018;2:223–8. 10.1016/S2352-4642(18)30022-1 [DOI] [PubMed] [Google Scholar]
- 10. McGorry PD, Mei C, Chanen A, et al. Designing and scaling up integrated youth mental health care. World Psychiatry 2022;21:61–76. 10.1002/wps.20938 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Crowley MJ, McCrory DC, Chatterjee R, et al. Prioritization of research addressing antipsychotics for adolescents and young adults with bipolar disorder. Ann Intern Med 2014;160:492–8. 10.7326/M13-2549 [DOI] [PubMed] [Google Scholar]
- 12. Kozloff N, Cheung AH, Schaffer A, et al. Bipolar disorder among adolescents and young adults: results from an epidemiological sample. Journal of Affective Disorders 2010;125:350–4. 10.1016/j.jad.2010.02.120 [DOI] [PubMed] [Google Scholar]
- 13. Cai C, Yin C, Tong Y, et al. Development of the Life Gatekeeper suicide prevention training programme in China: a Delphi study. Gen Psychiatr 2023;36:e101133. 10.1136/gpsych-2023-101133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. McGinty KR, Janos J, Seay J, et al. Comparing self-reported quality of life in youth with bipolar versus other disorders. Bipolar Disorders 2023;25:648–60. 10.1111/bdi.13320 [DOI] [PubMed] [Google Scholar]
- 15. Shahbazi F, Shahbazi M, Poorolajal J. Association between socioeconomic inequality and the global prevalence of anxiety and depressive disorders: an ecological study. Gen Psychiatr 2022;35:e100735. 10.1136/gpsych-2021-100735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Diseases GBD, Injuries C . Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the global burden of disease study 2019. Lancet 2020;396:1204–22. 10.1016/S0140-6736(20)30925-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. He H, Hu C, Ren Z, et al. Trends in the incidence and DALYs of bipolar disorder at global, regional, and national levels: results from the global burden of Disease Study 2017. J Psychiatr Res 2020;125:96–105. 10.1016/j.jpsychires.2020.03.015 [DOI] [PubMed] [Google Scholar]
- 18. Global Burden of Disease Collaborative Network . Global burden of disease study 2019 (GBD 2019) results. Seattle, United States: Institute for Health Metrics and Evaluation (IHME), 2020. [Google Scholar]
- 19. Bipolar disorder. 2020. Available: https://www.thelancet.com/pb-assets/Lancet/gbd/summaries/diseases/bipolar-disorder.pdf [Accessed 2 May 2023].
- 20. Institute for Health Metrics and Evaluation . Global burden of disease study 2019 (GBD 2019) socio-demographic index (SDI) 1950–2019. 2019. Available: https://ghdx.healthdata.org/record/ihme-data/gbd-2019-socio-demographic-index-sdi-1950-2019 [Accessed 2 May 2023].
- 21. Kim HJ, Fay MP, Feuer EJ, et al. Permutation tests for Joinpoint regression with applications to cancer rates. Stat Med 2000;19:335–51. [DOI] [PubMed] [Google Scholar]
- 22. Clegg LX, Hankey BF, Tiwari R, et al. Estimating average annual per cent change in trend analysis. Stat Med 2009;28:3670–82. 10.1002/sim.3733 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Nations U. Shifting demographics. 2018. Available: https://www.un.org/en/un75/shifting-demographics [Accessed 2 May 2023].
- 24. Diflorio A, Jones I. Is sex important? Gender differences in bipolar disorder. International Review of Psychiatry 2010;22:437–52. 10.3109/09540261.2010.514601 [DOI] [PubMed] [Google Scholar]
- 25. Martínez-Ortega JM, Jurado D, Gutiérrez-Rojas L, et al. Stability of sex differences by diagnosis in psychiatric hospitalizations. Psychiatry Research 2012;198:161–3. 10.1016/j.psychres.2011.11.023 [DOI] [PubMed] [Google Scholar]
- 26. Cunningham R, Crowe M, Stanley J, et al. Gender and mental health service use in bipolar disorder: national cohort study. BJPsych Open 2020;6:e138. 10.1192/bjo.2020.117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Baxter AJ, Patton G, Scott KM, et al. Global epidemiology of mental disorders: what are we missing PLoS One 2013;8:e65514. 10.1371/journal.pone.0065514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Fusar‐Poli P, Correll CU, Arango C, et al. Preventive psychiatry: a blueprint for improving the mental health of young people. World Psychiatry 2021;20:200–21. 10.1002/wps.20869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Neufeld SAS. The burden of young people’s mental health conditions in Europe: no cause for complacency. Lancet Reg Health Eur 2022;16:100364. 10.1016/j.lanepe.2022.100364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Fonseca L, Sena BF, Crossley N, et al. Diversity matters: opportunities in the study of the genetics of psychotic disorders in low- and middle-income countries in Latin America. Braz J Psychiatry 2021;43:631–7. 10.1590/1516-4446-2020-1240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. McGorry PD, Goldstone SD, Parker AG, et al. Cultures for mental health care of young people: an Australian blueprint for reform. Lancet Psychiatry 2014;1:559–68. 10.1016/S2215-0366(14)00082-0 [DOI] [PubMed] [Google Scholar]
- 32. Heim E, Wegmann I, Maercker A. Cultural values and the prevalence of mental disorders in 25 countries: a secondary data analysis. Social Science & Medicine 2017;189:96–104. 10.1016/j.socscimed.2017.07.024 [DOI] [PubMed] [Google Scholar]
- 33. McNally RJ. Resolving the vulnerability paradox in the cross-national prevalence of posttraumatic stress disorder. Journal of Anxiety Disorders 2018;54:33–5. 10.1016/j.janxdis.2018.01.005 [DOI] [PubMed] [Google Scholar]
- 34. Diener E, Lucas RE, Scollon CN. Beyond the hedonic treadmill: revising the adaptation theory of well-being. Am Psychol 2006;61:305–14. 10.1037/0003-066X.61.4.305 [DOI] [PubMed] [Google Scholar]
- 35. Knight J, Gunatilaka R. Income, aspirations and the Hedonic Treadmill in a poor society. Journal of Economic Behavior & Organization 2012;82:67–81. 10.1016/j.jebo.2011.12.005 [DOI] [Google Scholar]
- 36. Hauser M, Galling B, Correll CU. Suicidal ideation and suicide attempts in children and adolescents with bipolar disorder: a systematic review of prevalence and incidence rates, correlates, and targeted interventions. Bipolar Disorders 2013;15:507–23. 10.1111/bdi.12094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Rucklidge JJ. Psychosocial functioning of adolescents with and without paediatric bipolar disorder. Journal of Affective Disorders 2006;91:181–8. 10.1016/j.jad.2006.01.001 [DOI] [PubMed] [Google Scholar]
- 38. Christensen H, Reynolds CF, Cuijpers P. Protecting youth mental health, protecting our future. World Psychiatry 2017;16:327–8. 10.1002/wps.20437 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Cichoń L, Janas-Kozik M, Siwiec A, et al. Clinical picture and treatment of bipolar affective disorder in children and adolescents. Psychiatr Pol 2020;54:35–50. 10.12740/PP/OnlineFirst/92740 [DOI] [PubMed] [Google Scholar]
- 40. Gulliver A, Griffiths KM, Christensen H. Perceived barriers and facilitators to mental health help-seeking in young people: a systematic review. BMC Psychiatry 2010;10:113. 10.1186/1471-244X-10-113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Ziebold C, Silva-Ribeiro W, King D, et al. Utilisation and costs of mental health-related service use among adolescents. PLoS One 2022;17:e0273628. 10.1371/journal.pone.0273628 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Findling RL, Stepanova E. The workforce shortage of child and adolescent psychiatrists: is it time for a different approach Journal of the American Academy of Child & Adolescent Psychiatry 2018;57:300–1. 10.1016/j.jaac.2018.02.008 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
gpsych-2023-101255supp001.pdf (647.1KB, pdf)
Data Availability Statement
Data are available in a public, open access repository. Data in this article were collected from the Global Health Data Exchange (https://vizhub.healthdata.org/gbd-results/).