Abstract
Background
Bispecific T-cell engagers (BTEs) are novel agents used to treat hematological malignancies. Early trials were underpowered to define cardiovascular adverse events (CVAE) and no large-scale studies systematically examined the CVAEs associated with BTEs.
Methods
Leveraging the US Food and Drug Administration’s Adverse Event Reporting System-(FAERS), we identified the relative frequency of CVAEs after initiation of five BTE products approved by the Food and Drug Administration between 2014 and 2023 for the treatment of hematological malignancies. Adjusted reporting ORs (aROR) were used to identify disproportionate reporting of CVAEs with BTEs compared with background rates in the database. Fatality rates and risk ratios (RRs) for each adverse event (AE) were calculated.
Results
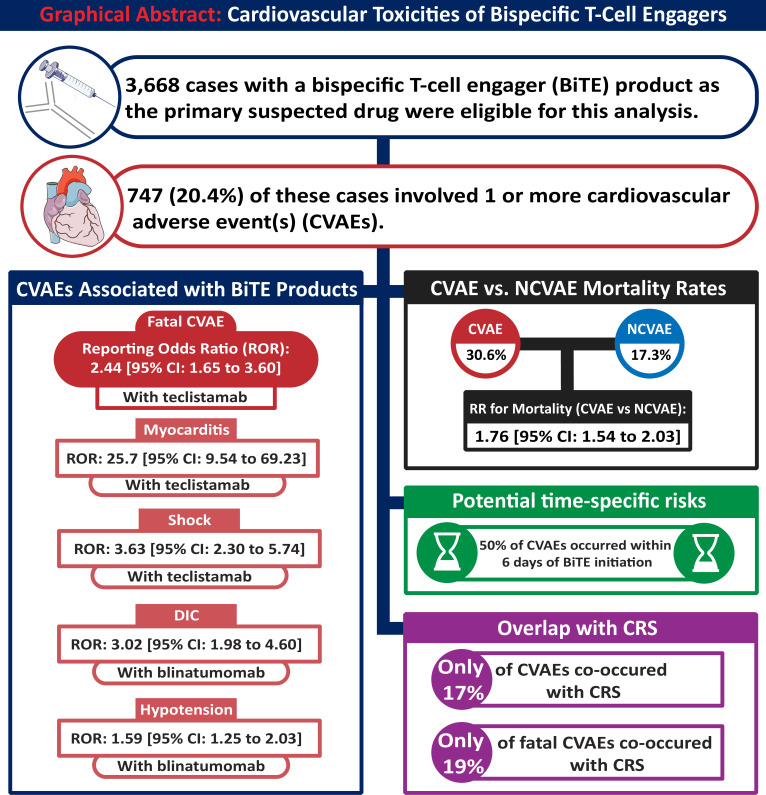
From 3668 BTE-related cases reported to FAERS, 747 (20.4%) involved CVAEs. BTEs as a class were associated with fatal CVAEs (aROR 1.29 (95% CI 1.12 to 1.50)), an association mainly driven by teclistamab (aROR 2.44 (95% CI 1.65 to 3.60)). Teclistamab was also associated with a disproportionate risk of myocarditis (aROR 25.70 (95% CI 9.54 to 69.23)) and shock (aROR 3.63 (95% CI 2.30 to 5.74)), whereas blinatumomab was associated with a disproportionate risk of disseminated intravascular coagulation (aROR 3.02 (95% CI 1.98 to 4.60)) and hypotension (aROR 1.59 (95% CI 1.25 to 2.03)). CVAEs were more fatal compared with non-CVAEs (31.1% vs 17.4%; RR 1.76 (95% CI 1.54 to 2.03)). Most CVAEs (83.3%) did not overlap with cytokine release syndrome.
Conclusion
In the first postmarketing surveillance study of BTEs, CVAEs were involved in approximately one in five AE reports and carried a significant mortality risk.
Keywords: Antibodies, Bispecific; Cytotoxicity, Immunologic
WHAT IS ALREADY KNOWN ON THIS TOPIC.
Bispecific T-cell engager (BTE) therapy is an emerging treatment option for hematological malignancies; however, the potential cardiovascular adverse event (CVAE) risks remain largely unknown.
WHAT THIS STUDY ADDS
Nearly one in five reported events with BTE therapies involved a CVAE. The likelihood of myocarditis, hypotension, and fatal CVAEs was disproportionately increased with BTE treatment. Most events did not occur in the context of CRS. In addition, patients who developed CVAEs saw a higher risk of death than patients who did not.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
Given the expanding indications of BTE therapy, increased vigilance, and research into the mechanisms and optimal preventative strategies for CVAEs are needed.
Introduction
Bispecific T-cell engager (BTE) therapies are a novel class of targeted immunotherapies with efficacy against hematologic malignancies.1–3 They enable endogenous T-cells to recognize and eliminate malignant cells with tumor-associated antigens (TAAs). BTEs possess two binding domains, one constantly binds to CD3 on the T-cell receptor, while the other is a modifiable domain designed to bind specific TAAs.4 Two approved BTEs are widely available for clinical use. Blinatumomab targets the CD19 domain on B-cells and has revolutionized the treatment of advanced acute lymphoblastic leukemias.1–3 The second, teclistamab, targets B-cell maturation antigen expressed on myeloma cells and is approved for use in relapsed/refractory multiple myeloma.5 6 These immunotherapeutic agents are associated with high oncological disease response and increased survival.1–3 5 6 More recently, three other BTEs, namely mosunetuzumab, glofitamab, and epcoritamab, have also been approved for the treatment of non-Hodgkin’s lymphoma.
However, BTEs also associated with potentially substantial adverse events (AEs). In oncological trials, the most frequently reported AEs of BTEs are cytokine release syndrome (CRS), hematological toxicities, and neurotoxicity.1 2 5 7–12 This profile of AEs is based on efficacy-focused clinical trials, wherein the statistical power to detect other AEs was unavailable. With other T-cell modulatory therapies (eg, chimeric T-cell antigen therapies (CAR-T)), safety analyses revealed signals of serious cardiovascular AEs (CVAEs) not observed in initial clinical trials.13–16 These events are now recognized as limitations to post-treatment survival.17
With BTEs, only limited and conflicting data are available. In an evaluation of 63 ALL patients in Italy, <2% developed reported high-grade CVAEs.18 In a subsequent study of 50 patients in South Korea, nearly 15% developed reported CVAEs.19 Yet, whether CVAEs are consistently reported with BTE therapies or carry prognostic implications for survival remains unknown.
To that end, we sought to better define CVAEs (if any) associated with BTE treatment and their implications with respect to survival.
Methods
Data source
Leveraging the US Food and Drug Administration’s Adverse Event Reporting System (FAERS) publicly available database, we investigated the frequency and association of CVAE reporting with BTE, the prognostic implications of CVAEs in patients receiving BTEs, as well as to what extent these events overlap with CRS.20 The dataset is partitioned into four quarters annually. For this analysis, we used data from the last quarter of 2014 (the first approval of a BTE product, blinatunomab) to the third-quarter of 2023 (the latest available date). Thus, our analysis included AE reports from October 2014 to September 2023.
The five BTE products under consideration were blinatumomab, teclistamab, mosunetuzumab, glofitamab, and epcoritamab. These five BTE products are currently the only BTE products approved by the Food and Drug Administration (FDA) specifically for the treatment of hematological malignancies. Additional details are shown in online supplemental methods.
jitc-2023-008518supp001.pdf (165.5KB, pdf)
Outcomes
CVAEs of interest included bleeding, hypotension or shock, thromboembolic disease (including overall thromboembolic events, arterial and venous thromboembolic events, and disseminated intravascular coagulation (DIC)), coronary disease, myocardial infarction, heart failure, conduction abnormalities (including tachyarrhythmia, bradycardia, QT-prolongation, and premature contractions), myocarditis, pericardial disease (including both pericardial effusion and pericarditis), vasculitis, and sudden death. AEs corresponding to each case are coded using the Medical Dictionary for Regulatory Activities (MedDRA).21 Specific terms used to code CVAEs are provided in online supplemental table 1.
Statistical analysis
We assessed the association between different CVAEs and BTE using multivariable logistic regression models with CVAEs as the dependent variable to yield adjusted reporting ORs (aROR). Independent variables included the variable of interest (BTE use) and factors that could potentially confound the relationship due to their association with the use of BTE and CVAEs. These included age, sex, disease status, anthracycline use, an interaction between age and each of disease status and sex, and an interaction between disease status and sex. We modeled age using restricted cubic splines to allow for potential non-linearity between age and CVAEs. In accordance with previous disproportionately analyses, we only calculated aRORs for events which occurred at least three times with BTE products. Further details are provided in online supplemental methods.
We also assessed the time to onset of CVAEs (vs non-CVAEs) and the time to onset of specific CVAEs. This was done using graphical displays of the empirical cumulative distribution function of each AE. Statistical significance was assessed using the Wilcoxon two-sample test.
The fatality of CVAEs is reported in two ways. First, we reported the percentage of patients who died after the BTE-related CVAE. Second, we used logistic regression models with death as the dependent variable. The independent variables included the CVAE of interest, age, and sex. We then applied average marginal effects to obtain adjusted mortality rates and risk ratios (RRs) corresponding to each AE.22
Rates of overlap between CRS and each AE are reported. We also reported the concomitant presence or effect of cardiovascular comorbidities in patients experiencing fatal CVAEs. The presence of cardiovascular comorbidities was inferred through the use of medications with a recorded cardiovascular indication.
All analyses were performed using R, V.4.2.0 (The R Foundation for Statistical Computing, Vienna, Austria).23 Data loading and cleaning were performed using the “data.table” package.24 The “marginaleffects” package was used to obtain adjusted mortality rates and RRs from logistic regression models.25 The “ggplot2” package was used to produce graphical figures.26 Statistical significance is denoted by a 95% CI that excludes the null value or p<0.05. The code related to this work can be obtained by contacting the first author (asu.ahmed.sayed@gmail.com).
Results
Characteristics of BTE-related cases reported in the FAERS database
From October 2014 to September 2023, a total of 1,437,817 FAERS cases were included in this analysis. Of these, 3668 cases of BTE-related AEs were reported. Among BTE-related AEs, 2712 (73.9%) and 409 (11.2 %) listed blinatumomab and teclistamab, respectively, as the primary suspected drug. Mosunetuzumab (272 reports; 7.4%), glofitamab (189 reports; 5.2%), and epcoritamab (86 reports; 2.3%) accounted for a smaller proportion of events. The indication for BTE therapy was leukemia/lymphoma in 88.7% of cases, MM in 11.2% of cases, and both in 0.1% of cases.
The median age of patients was 52.0 years (IQR: 41.0 years), and 44.4% of BTE recipients were female. Most reports came from the USA (43.2%), Japan (10.4%), or France (6.2%), with the rest of reports (40.2%) coming from 52 different countries. 95.6% of the reports were made by health professionals, 4% by consumers, and 0.3% did not state the reporting source.
Frequency and associations of CVAEs reported with BTE
From a total of 3668 cases with a reported BTE-related AE, 747 (20.4%) involved a CVAE (Graphical Abstract). Figure 2 shows the most frequently reported CVAEs. These were bleeding (211 events), thromboembolic events (196 events), hypotension (96 events), shock (97 events), and heart failure (52 events). Additional CVAEs included atrial fibrillation/flutter (23 events), pericardial effusions (13 events), myocardial infarction (16 events), ventricular tachyarrhythmia (9 events), myocarditis (8 events), pericarditis (4 events), and sudden death (2 event) (table 1).
Figure 1.
Graphical abstract. Cardiovascular toxicities of bispecific T-cell engagers. CRS, cytokine release syndrome; DIC, disseminated intravascular coagulation; NCVAE, non-CVAE.
Figure 2.
Frequency of cardiovascular adverse events reported with bispecific T-cell engagers. Because each case may involve more than one adverse event, these numbers are not mutually exclusive.
Table 1.
Association between adverse cardiovascular events and the use of bispecific T-cell engagers
| Outcome | Bispecific T-cell engagers | Blinatumomab | Teclistamab | ||||||||||||
| Reporting OR (95% CI)* | N | Proportion of events resulting in death† | Proportion of events co-occurring with CRS (%) | Proportion of events co-occurring with CV comorbidities (%) | Reporting OR (95% CI)* | N | Proportion of events resulting in death† | Proportion of events co-occurring with CRS (%) | Proportion of events co-occurring with CV comorbidities (%) | Reporting OR (95% CI)* | N | Proportion of events resulting in death† | Proportion of events co-occurring with CRS (%) | Proportion of events co-occurring with CV comorbidities (%) | |
| CVAE | 0.76 (0.70 to 0.83) |
747 | 30.1 | 16.7 | 3.7 | 0.75 (0.68 to 0.83) | 571 | 29.5 | 15.1 | 1.8 | 0.60 (0.46 to 0.79) | 65 | 44.4 | 18.5 | 7.7 |
| Fatal CVAE | 1.29 (1.12 to 1.50) |
214 | 100 | 18.7 | 3.3 | 1.06 (0.89 to 1.25) | 159 | 100 | 16.4 | 1.3 | 2.44 (1.65 to 3.60) | 28 | 100 | 25 | 3.6 |
| Heart failure | 0.77 (0.58 to 1.02) | 52 | 44.2 | 17.3 | 7.7 | 0.79 (0.57 to 1.08) | 41 | 48.8 | 19.5 | 4.9 | 0.59 (0.22 to 1.59) | 4 | 25 | 25 | 0 |
| Myocarditis | 2.38 (1.10 to 5.14) | 8 | 50 | 25 | 0 | N/A | 2 | 100 | 0 | 0 | 25.70 (9.54 to 69.23) | 5 | 40 | 40 | 0 |
| Thromboembolic disease | 0.80 (0.69 to 0.93) | 196 | 29.9 | 16.8 | 2.6 | 1.00 (0.85 to 1.18) | 168 | 31.3 | 17.3 | 1.2 | 0.23 (0.11 to 0.50) | 7 | 28.6 | 0 | 0 |
| Disseminated intravascular coagulation | 3.22 (2.16 to 4.79) | 33 | 42.4 | 39.4 | 3 | 3.02 (1.98 to 4.60) | 31 | 45.2 | 38.7 | 0 | N/A | 1 | 0 | 0 | 0 |
| Bleeding | 1.13 (0.98 to 1.31) | 211 | 40.9 | 18 | 2.8 | 1.09 (0.93 to 1.28) | 181 | 42 | 15.5 | 0.6 | 0.85 (0.46 to 1.55) | 11 | 60 | 27.3 | 9.1 |
| Shock | 0.88 (0.71 to 1.08) | 97 | 57.7 | 19.6 | 5.2 | 0.56 (0.43 to 0.73) | 61 | 50.8 | 23 | 3.3 | 3.63 (2.30 to 5.74) | 20 | 70 | 15 | 5 |
| Hypotension | 1.53 (1.23 to 1.91) | 96 | 18.2 | 21.9 | 2.1 | 1.59 (1.25 to 2.03) | 83 | 17.3 | 16.9 | 0 | N/A | 1 | 0 | 0 | 0 |
| Coronary disease | 0.53 (0.35 to 0.83) | 21 | 19 | 14.3 | 9.5 | 0.39 (0.22 to 0.69) | 12 | 25 | 8.3 | 8.3 | 0.60 (0.19 to 1.88) | 3 | 33.3 | 0 | 33.3 |
| Myocardial infarction | 0.55 (0.33 to 0.90) | 16 | 18.8 | 6.2 | 12.5 | 0.37 (0.18 to 0.74) | 8 | 25 | 0 | 12.5 | 0.74 (0.24 to 2.31) | 3 | 33.3 | 0 | 33.3 |
| Tachyarrhythmia | 1.04 (0.77 to 1.41) | 45 | 20 | 26.7 | 15.6 | 0.83 (0.55 to 1.25) | 25 | 20 | 20 | 8 | 0.85 (0.35 to 2.06) | 5 | 40 | 20 | 60 |
| Atrial fibrillation or flutter | 0.88 (0.58 to 1.34) | 23 | 21.7 | 34.8 | 21.7 | 0.64 (0.33 to 1.24) | 9 | 11.1 | 22.2 | 11.1 | 0.82 (0.30 to 2.19) | 4 | 50 | 25 | 50 |
| Ventricular tachyarrhythmia | 1.06 (0.53 to 2.11) | 9 | 22.2 | 11.1 | 11.1 | 0.87 (0.40 to 1.90) | 7 | 28.6 | 14.3 | 14.3 | N/A | 0 | N/A | N/A | N/A |
| Ventricular tachycardia | 1.28 (0.54 to 3.03) | 6 | 0 | 0 | 0 | 0.82 (0.29 to 2.31) | 4 | 0 | 0 | 0 | N/A | 0 | N/A | N/A | N/A |
| Ventricular fibrillation | 1.46 (0.44 to 4.88) | 3 | 66.7 | 33.3 | 33.3 | 1.81 (0.52 to 6.28) | 3 | 66.7 | 33.3 | 33.3 | N/A | 0 | N/A | N/A | N/A |
| Ventricular extrasystole | N/A | 2 | 0 | 0 | 0 | N/A | 2 | 0 | 0 | 0 | N/A | 0 | N/A | N/A | N/A |
| QT Prolongation | 0.65 (0.32 to 1.34) | 8 | 12.5 | 37.5 | 0 | 0.51 (0.24 to 1.10) | 7 | 14.3 | 42.9 | 0 | N/A | 1 | 0 | 0 | 0 |
| Sudden death | N/A | 2 | 100 | 50 | 0 | N/A | 0 | N/A | N/A | N/A | N/A | 1 | 100 | 0 | 0 |
| Pericarditis | 0.57 (0.21 to 1.58) | 4 | 25 | 0 | 0 | 0.40 (0.12 to 1.28) | 3 | 33.3 | 0 | 0 | N/A | 0 | N/A | N/A | N/A |
| Pericardial effusion | 1.06 (0.60 to 1.88) | 13 | 30.8 | 15.4 | 0 | 0.94 (0.52 to 1.71) | 12 | 25 | 16.7 | 0 | N/A | 1 | 100 | 0 | 0 |
| Valvular disease | N/A | 1 | 100 | 0 | 0 | N/A | 1 | 100 | 0 | 0 | N/A | 0 | N/A | N/A | N/A |
| Bradycardia | 0.69 (0.39 to 1.22) | 13 | 23.1 | 30.8 | 7.7 | 0.55 (0.29 to 1.04) | 10 | 20 | 40 | 10 | N/A | 3 | 33.3 | 0 | 0 |
*Reporting ORs were only calculated for events which were reported with a given drug at least three times.
†These proportions are based on the subset of events which had outcome data available.
CRS, cytokine release syndrome; CVAE, cardiovascular adverse events; N/A, not available.
Of these, in multivariable logistic regression models, BTEs as a class were associated with myocarditis ROR 2.38 (95% CI 1.10 to 5.14), hypotension (ROR 1.53 (95% CI 1.23 to 1.91)) and DIC (ROR 3.22 (95% CI 2.16 to 4.79)). Blinatumomab was the primary driver of these associations for both of DIC (ROR 3.02 (95% CI 1.98 to 4.60)) and hypotension (ROR 1.59 (95% CI 1.25 to 2.03)). In contrast, teclistamab was associated with myocarditis (ROR 25.70 (95% CI 9.54 to 69.23)) and shock (ROR 3.63 (95% CI 2.30 to 5.74)) (table 1). No significant associations with CVAE were observed with the other three BTE products (glofitamab, mosunetuzumab, and epcoritamab).
BTEs were not associated with overall CVAE (ROR 0.76 (95% CI 0.70 to 0.83)) but were significantly associated with fatal CVAE (ROR 1.29 (95% CI 1.12 to 1.50)). There was no statistically significant interaction with age or sex (p for interaction between BTE and age/sex: 0.10 and 0.21, respectively). Individually, the association with fatal CVAEs was most apparent with teclistamab (ROR 2.44 (95% CI 1.65 to 3.60)). Of the 214 fatal BTE-associated fatal CVAEs, 207 (96.7%) occurred in patients without a recorded cardiovascular comorbidity. The proportion of fatal CVAEs was comparable in patients with or without recorded cardiovascular comorbidities (6.2% vs 5.9%, respectively).
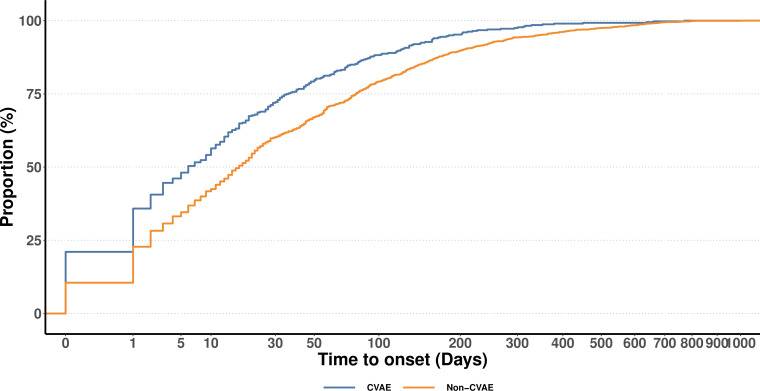
Time to onset of BTE-related AEs
Figure 3 shows the time to onset of CVAEs in comparison with non-CVAEs. In general, CVAEs tended to occur sooner following BTE therapy compared with non-CVAEs (median time to onset: 6 days vs 17 days; p<0.001). Online supplemental figure 1 shows the time to onset of specific CVAEs. DIC and hypotension events occurred at a median time of 1 day following BTE initiation, which was slightly earlier compared with other CVAEs (p≤0.001 and 0.001 for DIC and hypotension, respectively).
Figure 3.
Time to onset of adverse events (CVAEs vs NCVAEs) associated with bispecific T-cell engagers. Each line represents the cumulative proportion of adverse events that occurred by a given time point. A cubic root transformation was applied to the x-axis to aid in visualization. CVAE, cytokine release syndromes; NCVAE, non-CVAEs.
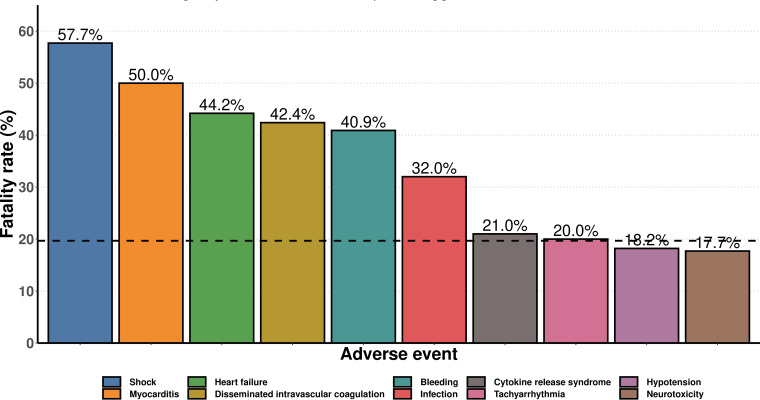
Mortality rates associated with BTE-related CVAEs
CVAEs were associated with a significantly higher risk of mortality compared with non-CVAEs (30.1% vs 16.8%; p<0.001) (figures 4 and 5). The CVAEs with the highest mortality rates were myocarditis (50%), shock (57.7%), heart failure (44.2%), DIC (42.4%), and bleeding (40.9%). Conversely, mortality rates associated with CRS (21%), neurotoxicity (17.7%), and infections (32.0%) were lower.
Figure 4.
Fatality rates of adverse events reported with bispecific T-cell engagers. The black dashed line denotes the average fatality rate of adverse events reported with bispecific T-cell engagers.
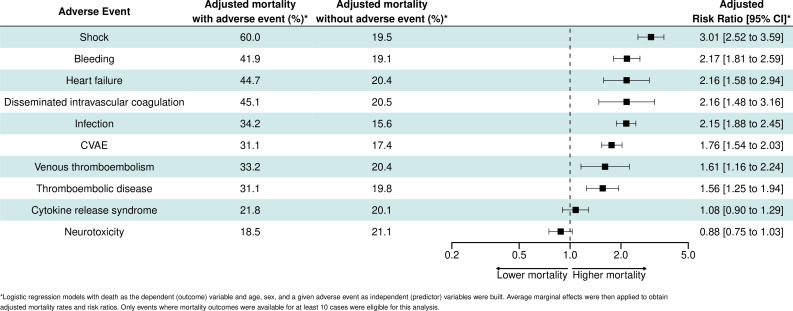
Figure 5.
Mortality risk ratios of adverse events reported with bispecific T-cell engagers. These values were obtained using logistic regression models with death as the dependent (outcome) variable and age, sex, and a given adverse event as independent (predictor) variables. Average marginal effects were then applied to obtain adjusted mortality rates and risk ratios. CVAE, cardiovascular adverse event.
Figure 4 shows the corresponding RR (adjusted for age and sex) for mortality with each AE in multivariable regression models adjusted for age and sex. CVAEs as a whole were associated with significantly higher mortality rates compared with non-CVAEs (RR 1.76 (95% CI 1.54 to 2.03)). Specific CVAEs associated with statistically significant increases in mortality included shock (RR 3.01 (95% CI 2.52 to 3.59)), HF (RR 2.16 (95% CI 1.58 to 2.94)), bleeding (RR 2.17 (95% CI 1.81 to 2.59)), DIC (RR 2.16 (95% CI 1.48 to 3.16)), thromboembolic disease (RR 1.56 (95% CI 1.25 to 1.94)), and venous thromboembolic disease (RR 1.61 (95% CI 1.16 to 2.24)).
Among non-CVAEs, infections (RR 2.15 (95% CI 1.88 to 2.45)) were associated with statistically significant increases in mortality but CRS (RR 1.08 (95% CI 0.90 to 1.29)) and neurotoxicity (RR 0.88 (95% CI 0.75 to 1.03)) were not.
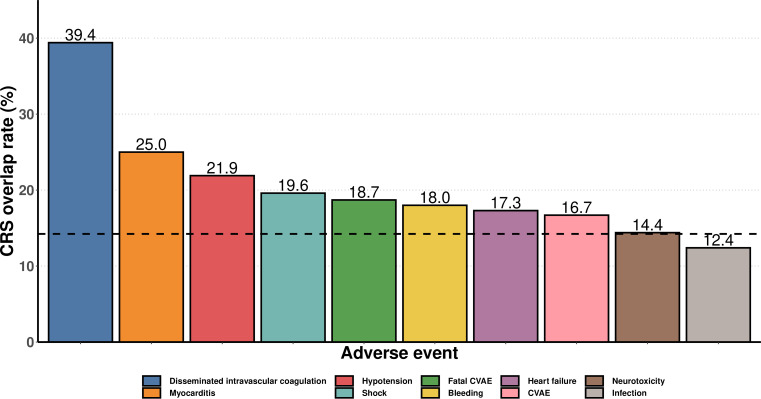
Overlap rates between BTE-related CVAEs and CRS
The 3 CVAEs which most frequently co-occurred with CRS were DIC (13 of 33 events; 39.4%), myocarditis (2 of 8 events; 25%), and heart failure (9 of 52 events; 25%). Overall, the rates of overlap between CVAEs and CRS were low (16.7%), as were the rates of overlap between fatal CVAEs and CRS (18.7%). Additionally, most cases of neurotoxicity and infection did not occur in the context of CRS (figure 6).
Figure 6.
Rates of overlap between cytokine release syndrome (CRS) and other adverse events reported with bispecific T-cell engagers. CVAE, cardiovascular adverse events.
Discussion
To our knowledge, this is the first postmarketing pharmacovigilance analysis to define the cardiovascular toxicity associated with BTEs. Our analysis demonstrates several key findings. First, BTE-associated CVAE reporting was not uncommon. Among 3668 BTE-related reports submitted to FAERS, approximately 1 in 5 (20.4%) involved CVAEs as defined by MedDRA. Second, BTEs were associated with disproportionately higher rates of reporting myocarditis, hypotension, shock, and DIC. Third, BTEs were associated with disproportionately higher reporting rates of fatal CVAEs. Most (96.7%) of these fatal CVAEs occurred in individuals without recorded cardiovascular comorbidities. Fourth, reports involving CVAEs were more likely to be fatal compared with other AEs. Fifth, CVAEs were not necessarily a consequence of CRS, as approximately 85% of CVAE reports did not involve concurrent CRS. Given the expected rise in BTE use and the relative absence of data on cardiovascular safety, these observations may bear significant ramifications.
The observation of substantial cardiovascular risks with BTEs adds to a growing body of evidence linking T-cell modulatory therapies with prognostic CVAEs.17 27 In an analysis of patients treated with CAR-T therapy, CVAE development was the second-leading cause of death following therapy initiation.17 Combined with our analysis, these observations suggest CVAEs following anticancer T-cell therapy are poorly tolerated and lead to reduced survival after treatment. Similar to other T-cell therapies, BTEs are commonly linked to neurotoxicity and CRS,1 2 5 7–12 a finding corroborated by our analysis. However, our analysis shows that, compared with CVAEs, they are associated with lower mortality. The elevated risk of death following CVAEs was especially evident for myocarditis, heart failure, bleeding, and DIC, which exhiBTEd mortality rates two to three times higher than other AEs.
The etiology of CVAEs with novel T-cell-based therapies is not well understood. Although studies have suggested the possible role of proinflammatory cytokines in promoting immune cell infiltration of the myocardium and the hypercoagulable state induced by CRS, these studies were mainly based on CAR-T-associated CRS.28 29 Whether similar mechanisms drive BTE-related CVAEs is not known. In a previous postmarketing study of CAR-T therapy, nearly two-thirds of CVAEs overlapped with CRS.16 In the current BTE-focused examination, only 15% of CVAEs overlapped with CRS. Moreover, the safety signals observed in this analysis, namely myocarditis and DIC, were not observed in a previous FAERS pharmacovigilance analysis focused on CAR-T therapy.16 In sum, the different rates of CVAE-CRS overlap, as well as differences in the types of associated CVAEs, suggests the pathophysiology of CVAEs associated with the two types of T-cell modulatory therapies may be (at least partially) distinct. However, it is also important to note that the two products have different indications, as such, direct comparisons between different pharmacovigilance analyses are difficult.
We observed that not all BTE products may be associated with the same profile of toxicities, and CVAEs in particular may be differentially associated with certain types of BTEs. In this analysis, the risk of myocarditis and fatal CVAEs was especially elevated with teclistamab, safety signals not seen for other BTE products. Nevertheless, at this time, similar risks cannot be ruled out with other (new) BTE products, particularly mosunetuzumab, glofitamab, and epcoritamab, for which there were relatively few reports available to date. Whether different binding domains carry different implications with respect to the risk of CVAEs should be investigated in mechanistic and clinical studies. Supporting the possibility that CVAEs may not be uniform across different BTE products is the finding that, in the seminal trials forming the basis for FDA approval, rates of other AEs such as CRS varied widely. For example, whereas more than 70% of patients in the teclistamab arm of the MajesTEC-1 trial reported CRS,2 only 14.2% in the blinatumomab of the TOWER trial reported CRS.5
Limitations
Several limitations of this analysis warrant mention. First, because FAERS includes only BTE users who experienced BTE-associated AEs rather than all BTE users, we could not determine the risk of incident CVAEs. Second, the decision to report CVAEs was at the discretion of treating clinicians. Third, users of FAERS may only be incentivized to submit reports of serious AEs. Therefore, the fatality rates of AEs submitted to FAERS may be higher than average. Fourth, because BTEs have been approved relatively recently, there is a need for more (larger) pharmacovigilance analyses as more data accumulates. This is especially so for newer BTE products approved in recent months, for which relatively little data were available. Fifth, we could not ascertain the diagnostic criteria for the reported AEs. This is particularly important for diagnoses such as myocarditis, where in depth would have been helpful in verifying the nature of the event. Likewise, data for events such as hypotension and shock would have benefited from more granular data regarding their cause (eg, distributive, cardiogenic). Sixth, because the presence of comorbidities was inferred through the use of medications with a recorded cardiovascular indication, it is possible that the proportion of cardiovascular comorbidities was underestimated and that the proportion of fatal CVAEs occurring in patients with cardiovascular comorbidities is higher than observed in the current analysis. Finally, it is important to note that, as with all observational studies, causality cannot necessarily be inferred from our analyses. Confirmation of the causal nature of these signals will require further corroboration by independent sources of data as well as possibly mechanistic insight into BTE-related toxicity.
Conclusion
In this pharmacovigilance study, CVAEs were observed in nearly 20% of BTE-related AE reports and carried a significant risk of death. BTEs were associated with higher levels of fatal CVAEs. BTEs were also associated with myocarditis, bleeding, DIC, and hypotension. The vast majority of CVAEs did not occur in the presence of CRS, suggesting the need for clinical vigilance is warranted even in its absence. Given the expanding indications of BTE therapy, research into the mechanisms and optimal management strategies for CVAEs is needed.
Footnotes
Twitter: @ahmed_sayed_98, @DrSFeldman, @NEpperla
NE and DA contributed equally.
Contributors: Conceptualization: DA and NE. Data curation: AShaaban. Formal analysis: ASayed. Funding acquisition: DA and NE. Methodology: ASayed, DA and NE. Visualization: AShaaban, DA, NE, MM and SMG. Roles/Writing–original draft: AShaaban, MM, DA and NE. Writing–review and editing: SMG, MF, SKhan, ASayed, AH, OK-K, PR, SKrishan, SS, SF, SM, EHY and AM. ASayed acts as guarantor and accepts full responsibility for the work and/or conduct of the study, had access to the data, and controlled the decision to publish.
Funding: This work was supported in part by an NIH P50-CA140158 grant. Dr. Addison is supported by NIH grants K23-HL155890, R01HL168045, and R01HL170038, and an American Heart Association‐Robert Wood Johnson Foundation (Harold Amos) grant.
Competing interests: No, there are no competing interests.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available in a public, open access repository. The the code related to this project to GitHub (https://github.com/ahmedsayedcardio/Cardiovascular-Toxicity-of-Bispecific-T-cell-engagers). In combination with the publicly available nature of FAERS (https://fis.fda.gov/extensions/FPD-QDE-FAERS/FPD-QDE-FAERS.html), this can be used to rerun and independently verify and replicate our analyses. The coding dictionary of the adverse events (defined by MedDRA) is available on request for interested researchers (https://www.meddra.org/)
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study was exempted from the institutional review board’s approval because it used anonymized data in a public database.
References
- 1. Goekbuget N, Dombret H, Bonifacio M, et al. BLAST: A Confirmatory, single-arm, phase 2 study of Blinatumomab, a Bispecific T-cell Engager (bite®) antibody construct, in patients with minimal residual disease B-precursor acute Lymphoblastic leukemia (ALL). Blood 2014;124. 10.1182/blood.V124.21.379.379 [DOI] [Google Scholar]
- 2. Kantarjian H, Stein A, Gökbuget N, et al. Blinatumomab versus chemotherapy for advanced acute Lymphoblastic leukemia. N Engl J Med 2017;376:836–47. 10.1056/NEJMoa1609783 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Drugs@FDA [database on the Internet]. U.S. Food and Drug Administration . Drug approval package Blincyto (blinatumomab) injection, Available: http://www.accessdata.fda.gov/drugsatfda_docs/nda/2014/125557Orig1s000TOC.cfm
- 4. Goebeler M-E, Bargou RC. T cell-engaging therapies — bites and beyond. Nat Rev Clin Oncol 2020;17:418–34. 10.1038/s41571-020-0347-5 [DOI] [PubMed] [Google Scholar]
- 5. Moreau P, Garfall AL, van de Donk NWCJ, et al. Teclistamab in Relapsed or refractory multiple myeloma. N Engl J Med 2022;387:495–505. 10.1056/NEJMoa2203478 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. FDA APPROVES Teclistamab-Cqyv for Relapsed or refractory multiple myeloma. n.d. Available: URL: https://www.fda.gov/drugs/resources-information-approved-drugs/fda-approves-teclistamab-cqyv-relapsed-or-refractory-multiple-myeloma
- 7. Topp MS, Gökbuget N, Zugmaier G, et al. Phase II trial of the anti-Cd19 Bispecific T cell–Engager Blinatumomab shows hematologic and molecular remissions in patients with Relapsed or refractory B-precursor acute Lymphoblastic leukemia. J Clin Oncol 2014;32:4134–40. 10.1200/JCO.2014.56.3247 [DOI] [PubMed] [Google Scholar]
- 8. Topp MS, Gökbuget N, Stein AS, et al. Safety and activity of Blinatumomab for adult patients with Relapsed or refractory B-precursor acute Lymphoblastic leukaemia: a Multicentre, single-arm, phase 2 study. Lancet Oncol 2015;16:57–66. 10.1016/S1470-2045(14)71170-2 [DOI] [PubMed] [Google Scholar]
- 9. Derache A-F, Rialland F, Michel G, et al. Safety and efficacy of Blinatumomab used in children with B-precursor acute Lymphoblastic leukemia (ALL) treated in French hematological centers. Blood 2016;128. 10.1182/blood.V128.22.5190.5190 [DOI] [Google Scholar]
- 10. von Stackelberg A, Locatelli F, Zugmaier G, et al. Phase I/phase II study of Blinatumomab in pediatric patients with Relapsed/refractory acute Lymphoblastic leukemia. JCO 2016;34:4381–9. 10.1200/JCO.2016.67.3301 [DOI] [PubMed] [Google Scholar]
- 11. Gökbuget N, Dombret H, Bonifacio M, et al. Blinatumomab for minimal residual disease in adults with B-cell precursor acute Lymphoblastic leukemia. Blood 2018;131:1522–31. 10.1182/blood-2017-08-798322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Locatelli F, Zugmaier G, Rizzari C, et al. Effect of Blinatumomab vs chemotherapy on event-free survival among children with high-risk first-relapse B-cell acute Lymphoblastic leukemia: a randomized clinical trial. JAMA 2021;325:843–54. 10.1001/jama.2021.0987 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Alvi RM, Frigault MJ, Fradley MG, et al. Cardiovascular events among adults treated with Chimeric antigen receptor T-cells (CAR-T). J Am Coll Cardiol 2019;74:3099–108. 10.1016/j.jacc.2019.10.038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Guha A, Addison D, Jain P, et al. Cardiovascular events associated with Chimeric antigen receptor T cell therapy: cross-sectional FDA adverse events reporting system analysis. Biol Blood Marrow Transplant 2020;26:2211–6. 10.1016/j.bbmt.2020.08.036 [DOI] [PubMed] [Google Scholar]
- 15. Ganatra S, Redd R, Hayek SS, et al. Chimeric antigen receptor T-cell therapy–associated cardiomyopathy in patients with refractory or Relapsed non-Hodgkin lymphoma. Circulation 2020;142:1687–90. 10.1161/CIRCULATIONAHA.120.048100 [DOI] [PubMed] [Google Scholar]
- 16. Goldman A, Maor E, Bomze D, et al. Adverse cardiovascular and pulmonary events associated with Chimeric antigen receptor T-cell therapy. J Am Coll Cardiol 2021;78:1800–13. 10.1016/j.jacc.2021.08.044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Mahmood SS, Riedell PA, Feldman S, et al. Biomarkers and cardiovascular outcomes in Chimeric antigen receptor T-cell therapy recipients. Eur Heart J 2023;44:2029–42. 10.1093/eurheartj/ehad117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Foà R, Bassan R, Vitale A, et al. Dasatinib-Blinatumomab for pH-positive acute Lymphoblastic leukemia in adults. N Engl J Med 2020;383:1613–23. 10.1056/NEJMoa2016272 [DOI] [PubMed] [Google Scholar]
- 19. Jung S-H, Lee S, Yang D-H, et al. Efficacy and safety of Blinatumomab treatment in adult Korean patients with Relapsed/refractory acute Lymphoblastic leukemia on behalf of the Korean society of hematology ALL working party. Ann Hematol 2019;98:151–8. 10.1007/s00277-018-3495-2 [DOI] [PubMed] [Google Scholar]
- 20. Food and Drug Administration . FDA Aes reporting system (FAERS) public dashboard. n.d. Available: https://www.fda.gov/drugs/questions-and-answers-fdas-adverse-event-reporting-system-faers/fda-adverse-event-reporting-system-faers-latest-quarterly-data-files
- 21. Mozzicato P. Meddra. Pharm Med 2009;23:65–75. 10.1007/BF03256752 [DOI] [Google Scholar]
- 22. Norton EC, Dowd BE, Maciejewski ML. Marginal effects-Quantifying the effect of changes in risk factors in logistic regression models. JAMA 2019;321:1304–5. 10.1001/jama.2019.1954 [DOI] [PubMed] [Google Scholar]
- 23. R Core Team . R: A language and environment for statistical computing. In: R Foundation for Statistical Computing. Vienna, Austria, 2022. Available: https://www.R-project.org [Google Scholar]
- 24. Dowle M, Srinivasan A. Data.table: Extension of 'data.frame'. R package version 1.14.2, 2021. Available: https://CRAN.R-project.org/package=data.table [Google Scholar]
- 25. Arel-Bundock V. marginaleffects: Predictions, Comparisons, Slopes, Marginal Means, and Hypothesis Tests. R package version 0.13.0, Available: https://CRAN.R-project.org/package=marginaleffects [Google Scholar]
- 26. Wickham H. Ggplot2. In: ggplot2: Elegant Graphics for Data Analysis. Cham: Springer-Verlag New York, 2016. 10.1007/978-3-319-24277-4 [DOI] [Google Scholar]
- 27. Chen L-R, Li Y-J, Zhang Z, et al. Cardiovascular effects associated with Chimeric antigen receptor T cell therapy in cancer patients: A meta-analysis. Front Oncol 2022;12. 10.3389/fonc.2022.924208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Baik AH, Oluwole OO, Johnson DB, et al. Mechanisms of cardiovascular toxicities associated with Immunotherapies. Circ Res 2021;128:1780–801. 10.1161/CIRCRESAHA.120.315894 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Yamasaki-Morita M, Arai Y, Ishihara T, et al. Relative Hypercoagulation induced by suppressed Fibrinolysis after Tisagenlecleucel infusion in malignant lymphoma. Blood Adv 2022;6:4216–23. 10.1182/bloodadvances.2022007454 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
jitc-2023-008518supp001.pdf (165.5KB, pdf)
Data Availability Statement
Data are available in a public, open access repository. The the code related to this project to GitHub (https://github.com/ahmedsayedcardio/Cardiovascular-Toxicity-of-Bispecific-T-cell-engagers). In combination with the publicly available nature of FAERS (https://fis.fda.gov/extensions/FPD-QDE-FAERS/FPD-QDE-FAERS.html), this can be used to rerun and independently verify and replicate our analyses. The coding dictionary of the adverse events (defined by MedDRA) is available on request for interested researchers (https://www.meddra.org/)