Abstract
Objectives
This study aimed to identify factors influencing orthopaedic trauma patients’ experiences and satisfaction with emergency department (ED) care and follow-up through Virtual Fracture Care (VFC) review workflow.
Design
This study employed an explorative, descriptive, qualitative design using individual, semistructured interviews.
Setting
An urban level 2 trauma centre and teaching hospital in Amsterdam, the Netherlands.
Participants
Eligible patients were Dutch-speaking or English-speaking orthopaedic trauma patients, aged 18 years or above, who visited the hospital’s ED between June and September 2022, and were treated through VFC review workflow. Exclusion criteria were: reason for follow-up other than injury, eye/motor/verbal score <15 at ED admission, follow-up treatment in another hospital, treatment initiated in another hospital, acute hospital admission (<24 hours). Twenty-three patients were invited for participation, of whom 15 participated and were interviewed.
Results
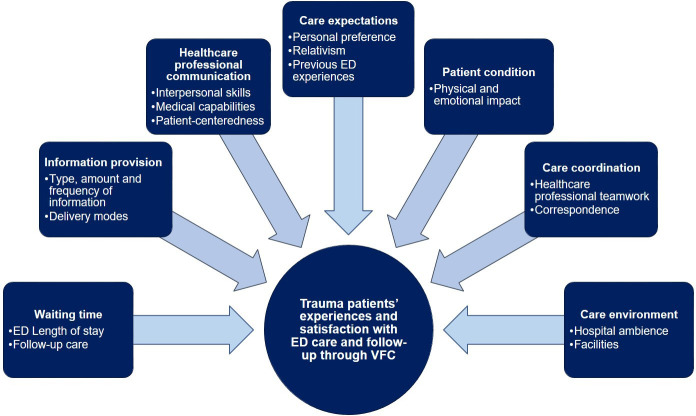
Several influential factors contributed to seven generic themes: (1) waiting times, (2) information provision, (3) healthcare professional communication, (4) care expectations, (5) care coordination, (6) care environment and (7) patient condition. Overall, participants were satisfied with received care. Interpersonal skills of healthcare professionals, and timing and content of provided information were specifically valued. Additionally, patients stated that their needs in the ED differed from those after ED discharge, and appreciated the way the VFC review workflow addressed this. Points of improvement included more active involvement of patients in the care process and prevention of inconsistent instructions by different healthcare professionals.
Conclusions
Patient experiences with ED care and VFC review follow-up are influenced by factors categorised into seven themes. The VFC review workflow effectively addresses these factors, leading to positive feedback. Recommendations for healthcare professionals include anticipating evolving post-ED information needs, engaging patients early to provide clarity about the care process, involving them in treatment decisions and expanding information provision across the entire care pathway.
Keywords: ACCIDENT & EMERGENCY MEDICINE, Orthopaedic & trauma surgery, Trauma management
STRENGTHS AND LIMITATIONS OF THIS STUDY.
Heterogeneous sample in terms of gender, age, type of injury and treatment strategy with continuance of data collection until the point of data saturation.
Interviews were conducted by two independent researchers not involved in the development of the Virtual Fracture Care (VFC) review workflow or daily clinical care, which was emphasised to the participants to encourage them to speak frankly, with the semistructured nature of the interviews enabling uncovering of further potential off-topic information.
Involvement of different types of healthcare professionals in the development of the topic list enhanced the variety of addressed perspectives in the interviews.
Since this study was conducted among patients who received care according to specific workflow (ie, the VFC review workflow), the results may not be transferable to settings with other types of workflow.
The explorative, descriptive, qualitative study design did not allow examination of the relative importance of influential factors.
Introduction
In the Netherlands, orthopaedic trauma patients accounted for one-third of emergency department (ED) visits in 2022 (661 000/1 800 000), and this number has increased over the years.1 This increase poses significant challenges to the already strained ED healthcare services in providing timely and high-quality care to orthopaedic trauma patients.2 3 Patient satisfaction and experiences are critical indicators of the quality of care delivered by EDs, emphasising the need to evaluate the impact of this increasing burden on these outcomes for this population.4 5
To maintain high-quality orthopaedic trauma care, innovative workflow has been introduced in the Netherlands, including the Virtual Fracture Care (VFC) review workflow.6 With VFC review, ED healthcare professionals electronically refer patients to a multidisciplinary VFC meeting on the next workday for review and treatment planning by the attending (orthopaedic) trauma surgeon. Immediately following the VFC review meeting, patients are contacted by phone to inform them of their definitive diagnosis, treatment and complete follow-up plan. This workflow aims to streamline orthopaedic trauma care by transferring part of the diagnostic phase from the ED visit to an organised, supervised setting on the next workday and by directly scheduling follow-up appointments with appropriate healthcare professionals. Previous studies have demonstrated positive results regarding patient satisfaction with ED care and follow-up through similar VFC workflow, but an exploration of patients’ experiences is lacking.7 8
A qualitative analysis of these experiences would complement quantitative studies and inform interventions to enhance patient experiences and satisfaction by providing a deeper understanding of the perceived quality of care and patients’ needs and expectations.9 Therefore, the aim of this study was to identify factors influencing orthopaedic trauma patients’ experiences and satisfaction with ED care and follow-up through the VFC review workflow.
Methods
Study design and setting
This was an explorative, descriptive study using a generic qualitative design. This study was conducted in an urban level 2 trauma centre and teaching hospital in Amsterdam, the Netherlands. Approximately 85 000 patients visit the ED of this hospital annually. Patients were eligible for participation in this study if they were Dutch-speaking or English-speaking orthopaedic trauma patients, aged 18 years or above, who visited the hospital’s ED between June and September 2022, and who were treated through the VFC review workflow. Exclusion criteria were: reason for follow-up other than the injury (eg, social care reasons), eye/motor/verbal score <15 at ED admission, follow-up treatment in another hospital, treatment initiated at another hospital, direct hospital admission (<24 hours). One of the researchers (GW) contacted patients on the next workday after their ED visit to inform them about the study and provide them with an information letter and consent form. Patients were selected using a purposive maximum variation sampling method to ensure a heterogeneous sample in terms of gender, age, type of injury and treatment strategy. The sample size was determined by the principle of data saturation.10 This study was reported according to the Standards for Reporting Qualitative Research (online supplemental appendix A).11
bmjopen-2023-076040supp001.pdf (106.2KB, pdf)
The VFC workflow
At the study institution, orthopaedic trauma patients who require follow-up treatment (non-operative and scheduled operative treatment) are managed through the VFC review workflow.6 ED healthcare professionals provide patients with appropriate immobilisation measures and refer them to a VFC review meeting scheduled for the next workday via the electronic patient record. Upon referral to the VFC review meeting, patients receive information leaflets regarding the VFC workflow and their injury. During the VFC review meeting, a multidisciplinary team (consisting of a casting technician, surgical resident, orthopaedic trauma surgeon and administrative outpatient clinic assistant) reviews all referrals (approximately 30 patients per meeting) and assigns predefined digital trauma care protocols to each patient via dropdown menus within the electronic patient records. These protocols provide an extensive treatment plan for the entire follow-up treatment, including all follow-up appointments and radiographic imaging. The VFC team can further tailor these protocols to specifically fit each patient’s situation if necessary. After VFC review, patients are contacted by phone to provide information about their injury and treatment plan, and to reach consent on the definitive treatment. Patients then receive their follow-up treatment plan by mail or via their electronic patient record within 1 workday after their ED visit.
Data collection
Data were collected using individual, semistructured interviews. The interviews were conducted using the online video communication platform Microsoft Teams. Participants who were not able to use Teams were interviewed by telephone. Two experienced researchers (EM and IK) who were not part of the medical team conducted the interviews, using a topic list with several open-ended questions (online supplemental appendix B). The research team piloted the topic list to ensure its clarity and comprehensiveness, and subsequently modified it as necessary. Field notes were taken to document contextual information after each interview. Verbatim transcriptions of the audio recordings were obtained, using a professional transcription service.
bmjopen-2023-076040supp002.pdf (97.7KB, pdf)
Data analysis
The transcripts and fields notes were analysed by the same researchers who conducted the interviews. The six steps of inductive, thematic analysis as described by Braun and Clarke were followed, namely: (1) becoming familiar with the data, (2) generating initial codes, (3) searching for themes, (4) reviewing themes, (5) defining and naming themes, and (6) writing up the results.12 Researcher triangulation (between EM and IK) was used to increase the quality and credibility of the data analysis.13 The researchers independently analysed data, discussed discrepancies and reached consensus about the final themes and interpretations. Memos were written to help the researchers keep track of decisions made during data analysis. The data analysis was facilitated by NVivo V.12 (QSR International, 2020).
Patient and public involvement
Patients were not involved in the design, intervention, research question or outcome measures of the current study. Healthcare professionals were involved in the design of the topic lists for the semistructured interviews.
Results
In total, 23 patients were invited for participation. Fifteen patients chose to participate and eight patients chose to refrain from participation or did not respond to the invitation. Characteristics of the participants (n=15) are shown in table 1. The median length of the interviews was 27 min and ranged from 16 to 33 min. Three interviews were conducted by telephone. Data saturation was achieved after 15 interviews.
Table 1.
Baseline characteristics of study participants (n=15)
| Sex, n (%) | |
| Male | 7 (47) |
| Female | 8 (53) |
| Age, median (range) | 42 (23–66) |
| Type of injury, n (%) | |
| Acromioclavicular joint dislocation | 1 (7) |
| Mid-shaft clavicle fracture | 1 (7) |
| Glenohumeral joint dislocation+humerus fracture | 1 (7) |
| Humerus fracture | 2 (13) |
| Metatarsal shaft fracture | 2 (13) |
| Distal phalanx fracture | 1 (7) |
| Distal radius fracture | 3 (20) |
| Radial head fracture | 1 (7) |
| Talus fracture | 1 (7) |
| Triquetrum fracture | 2 (13) |
| Treatment strategy, n (%) | |
| Non-operative | 10 (67) |
| Operative | 5 (33) |
A variety of factors influencing orthopaedic trauma patients’ experiences and satisfaction with ED care and follow-up through VFC review were identified and subsequently categorised into seven generic themes, namely: (1) waiting times, (2) information provision, (3) healthcare professional communication, (4) care expectations, (5) patient condition, (6) care coordination and (7) care environment (figure 1). Relevant quotes were selected to illustrate the results (table 2).
Figure 1.
An overview of the identified themes with the relevant influential factors. ED, emergency department; VFC, Virtual Fracture Care.
Table 2.
Quotes per identified theme
| Theme | # | Participant | Quote |
| Waiting times | |||
| ED length of stay | #1 | Participant 5, M, 35 years | ‘I was positively surprised that everything went as quickly as it did. I imagined this long queue at the emergency department with ambulances rushing in with patients who were worse off than me. However, nothing could be further from the truth. I was in and out of the emergency department within 2 hours.’ |
| #2 | Participant 15, F, 26 years | ‘At one point, my partner asked me: What are we actually waiting for? That might be something that could be improved. Since it was my first time there, I had no idea how long such a visit would take.’ | |
| #3 | Participant 7, M, 39 years | ‘Well, the fact that the pain was much less, that certainly made a lot of difference. When you are continuously in pain, it makes something like this feel like a lot longer.’ | |
| Follow-up care | #4 | Participant 14, F, 32 years | ‘It is very important to have information in a timely manner. For example, if I needed surgery or not. I was glad that I did not have to leave the house for this information. I was not that mobile.’ |
| Information provision | |||
| Type, amount and frequency | #5 | Participant 14, F, 32 years | ‘For example, my wrist is still swollen. Is that because of the oedema or is it because of something else? Can I maybe do more than just keeping my wrist elevated? Is it useful to put some ice on it? Maybe some tips for a better recovery would have been nice.’ |
| #6 | Participant 1, M, 51 years | ‘I can imagine that if you are there alone (ED), things will pass you by. Because you have so many other things going through your mind. What about work? And things at home? A thousand and one things are going through your mind. So it was very nice that you also got an information leaflet with you. And yes, the phone call with the doctor the next morning. Of course, afterwards (after the ED visit), I had a little more time to write down one or two other questions that I could ask the doctor during the phone call the next day.’ | |
| Delivery mode | #7 | Participant 10, M, 30 years | ‘It is always very nice if you can read back some information afterwards.’ |
| Healthcare professional communication | |||
| Interpersonal skills | #8 | Participant 14, F, 32 years | ‘You couldn't really tell that they were busy. They were just focused on me and engaged with me at that time. So I thought that was really nice.’ |
| Medical capabilities | #9 | Participant 2, F, 59 years | ‘At that time, you are in a lot of pain. If someone then tells you what needs to be done and how, and that it is going to be incredibly painful, but that the pain will be over afterwards…At that point…well…you leave yourself in their hands, because you think: this person knows what she is doing.’ |
| Patient-centredness | #10 | Participant 4, F, 58 years | ‘Also with the second X-ray, they said: oh, the fracture is clearly visible. But unfortunately, I did not see it for myself. That was a shame, I would have liked to see it. That is something that they could pay more attention to.’ |
| Care expectations | |||
| Personal preference | #11 | Participant 9, F, 56 years | ‘Just giving you a glass of water after you just threw up. Well, I think you really shouldn’t have to ask for that.’ |
| Relativism | #12 | Participant 10, M, 30 years | ‘And I do not feel like it was that bad. I also felt like it was going to be okay the whole time (during ED visit).’ |
| Previous ED experiences | #13 | Participant 6, F, 44 years | ‘I had something entirely else some time ago, at the start of this year. When I compare that situation to this one, I’m like wow, I got so much attention now! That would have been nice the last time. So I experienced a lot of luxury this time.’ |
| Patient condition | |||
| Physical and emotional impact | #14 | Participant 9, F, 56 years | ‘Well, I mean…it’s obviously a huge event for me, you know. And for them…well, a broken shoulder is probably not that exciting for them. But to me, it meant a lot.’ |
| Care coordination | |||
| Healthcare professional teamwork | #15 | Participant 3, M, 26 years | ‘When I arrived, I was told to walk all the way to the end of the hallway after the first conversation. And it was not until after the radiographs were made, that I heard I shouldn’t walk anymore. So, I had to limp all the way back.’ |
| #16 | Participant 5, M, 36 years | ‘What I noticed was that everyone in the hospital has their own specific tasks, which is really great. However, for me, a broader view is required at a certain point, like what is specifically going on and what does this actually mean? So, kind of like…who is in charge?’ | |
| Correspondence | #17 | Participant 4, F, 58 years | ‘Well, I think I've received about 10 or 11 emails from the [hospital], and new information in my patient portal: appointment scheduled, appointment canceled. Just a lot of emails. It could be better because now you can't see the wood for the trees.’ |
| Care environment | |||
| Hospital ambience | #18 | Participant 6, F, 44 years | ‘I think that if you are surrounded by screaming people with all sorts of open wounds… that it would be hard to relax. And, that this would also influence the conversations that you have afterwards. So, I think the waiting area should help you feel as comfortable as possible.’ |
| Facilities | #19 | Participant 7, M, 39 years | ‘I found it very cold in that room. But that might also have been because I had just sustained that injury, and at some point, I did get a blanket, so that was well arranged, which was nice.’ |
ED, emergency department.
Waiting times
ED length of stay
Most participants indicated that they were positively surprised about the length of stay at the ED. Their waiting time was shorter than expected and they were able to leave the hospital in a timely manner. Participants whose waiting time was longer than expected were less satisfied. The participants mainly attributed waiting times to the volume of activity at the time of their ED visit (ie, on a weekday or at the weekend and at daytime or night-time) (Q#1). Some participants would have preferred more information about the underlying reason for waiting and how long they were expected to wait, since being uninformed makes waiting feel longer (Q#2). Furthermore, the participants preferred interaction with healthcare professionals when waiting by themselves. This provided distraction and prevented them from worrying. Participants who were accompanied by a family member or friend valued their companionship for this same distraction. The participants’ perceived waiting time was also influenced by their physical comfort. The presence of pain was particularly mentioned as a factor that contributes to the feeling of time moving slowly (Q#3).
Follow-up care
The participants preferred short time intervals between their ED visit and follow-up care. Clarity about follow-up care (eg, operative vs non-operative treatment, follow-up appointments, immobilisation method) was important to them, since they wanted to know what to expect as soon as possible. All participants valued the VFC phone call in this regard. Some participants requiring surgery also indicated that they were glad about not having to wait long for their surgery to take place (Q#4).
Information provision
Type, amount and frequency of information
In general, the participants were satisfied with the type and amount of information that was provided to them both during their ED visit and the next workday during the VFC phone call. They indicated that the information on various topics was relevant, sufficient and timely. Some participants mentioned that they missed individually tailored information, particularly regarding their recovery process (Q#5). The participants also valued the opportunity to ask questions the next day during the VFC phone call, since new questions often arose some time after leaving the ED (Q#6).
Delivery mode
The participants valued the provision of information leaflets. This allowed them to go through the information at their own pace and convenience. Some participants stressed the importance to read back information that was provided to them during their ED visit, since it is hard to remember everything at once (Q#7). In general, the delivery mode (face-to-face or by telephone) made no difference to the participants. Saving time was mentioned as an advantage of a telephone consultation. Moreover, the participants’ mobility was often limited by their injury, making a telephone consultation a much more practical alternative to a face-to-face consultation.
Healthcare professional communication
Interpersonal skills
In general, the participants were satisfied with the interpersonal skills of healthcare professionals. They described them as being very friendly, honest and empathic. Most participants indicated that healthcare providers took the time to listen to them. They were given plenty of opportunity to ask questions and their questions were adequately answered. The participants valued the efforts of healthcare professionals to understand their specific needs (Q#8). Some participants mentioned that specifically humour used by healthcare professionals could help to reframe tense situations.
Medical capabilities
All participants indicated that they felt like they were in good hands. Healthcare professionals clearly explained their actions, which strengthened the participants’ confidence in their medical capabilities (Q#9).
Patient-centredness
Most participants preferred healthcare professionals to involve them in the different stages of the care process. However, they had different preferences for the exact level of involvement. While some participants preferred as much involvement as possible, others explicitly stated that they did not want to know or see everything. Sharing medical images was particularly mentioned as something that facilitates involvement and could help someone to better understand their injury (Q#10). Some participants stressed the importance of the use of plain language (ie, the avoidance of medical jargon) to increase their understanding of what exactly was said.
Care expectations
Personal preference
All participants expected to receive the best possible care. However, personal preference determined what exactly was important to someone. While some participants focused on the treatment of their injury, the focus of others was on other care aspects such as its personal touch. In general, participants’ care expectations were met. Unmet care expectations led to dissatisfaction (Q#11).
Relativism
Care expectations were also shaped by relativism (Q#12). In general, the participants recognised that healthcare professionals were busy and therefore accepted that they did not have much time for them except from carrying out their routines. Some participants were also aware of the ED’s triage process, accepting that patients who were worse off than themselves were given priority.
Previous ED experiences
Some participants had built up care expectations based on previous ED experiences, which determined how they evaluated their present experience (Q#13). Those with no previous experiences had no material for comparison and indicated that they did not know what to expect.
Patient condition
Physical and emotional impact
Most participants arrived at the ED in pain. They preferred healthcare professionals to anticipate on their pain by actively offering them analgesics instead of having to ask for it themselves. The emotional impact of their ED visit varied from person to person. In general, the participants felt vulnerable not knowing what they were up to. Some participants mentioned that they were stressed and anxious. They valued the ability of healthcare professionals to acknowledge and address their vulnerabilities (Q#14).
Care coordination
Healthcare professionals’ teamwork
In general, the participants experienced effective and efficient teamwork among healthcare professionals. Inconsistencies between the instructions of different healthcare professionals led to dissatisfaction (Q#15). Some participants indicated that they experienced fragmentation of care during their ED visit, with different healthcare professionals (eg, ED nurses, radiologists) working in their own silos. They missed someone who was primarily responsible for their case (Q#16).
Correspondence
Some participants mentioned that the hospital sent a large volume of appointment notification emails, causing them to lose the overview (Q#17). Moreover, the purpose of these appointments was not always clear. They would have preferred more information about this before leaving the hospital. One participant recounted receiving an email about an appointment with a surgeon within a few days, lacking any additional context. As a result, the participant assumed that she needed surgery. This caused this participant to worry, only to learn during that phone call that surgery was, in fact, not required.
Care environment
Hospital ambience
In general, the participants were satisfied with the hospital ambience. Some participants stressed the importance of a patient-friendly care environment with visual and auditory privacy (Q#18).
Facilities
The participants valued facilities such as the availability of hospital beds and blankets to keep them comfortable (Q#19). One participant was dissatisfied with the hospital’s high parking costs.
Discussion
This study identified factors influencing orthopaedic trauma patients’ experiences with ED care and follow-up through VFC. A variety of influential factors were identified and categorised into seven themes, namely: (1) waiting time, (2) information provision, (3) healthcare professional communication, (4) care expectations, (5) patient condition, (6) care coordination and (7) care environment. It is important to note that no influential factor is solely responsible for shaping the patient perspective. Our results show that patients were generally satisfied with the received care. The VFC review workflow addresses the majority of the identified influential factors, contributing to the positive feedback from participants.
Waiting time influences patient experiences, with less time spent waiting, resulting in more positive perception of care. Additionally, our results indicate the way patients perceive their waiting time is of greater influence on their satisfaction than the absolute amount of time spent waiting. These results are in accordance with current literature.9 14–17 Healthcare professionals can potentially reduce perceived waiting time in the ED by actively providing clarity about ED processes, expectations and addressing their concerns, and by timely providing analgesics.5 17–19 Furthermore, patients preferred clarity about their diagnosis and follow-up treatment plan as soon as possible. The VFC review workflow accommodates this by providing patients with a complete and supervised treatment plan on the first workday after their ED visit. This was perceived as timely and was highly valued by our patients.
Patient experiences are also influenced by the type of information they receive and how this is communicated by healthcare professionals.20–22 Patients highly valued healthcare professionals who make an effort to understand and address their personal situation and actively involve them in the decision-making process (eg, showing and explaining medical images).5 19 23 24 Additionally, it is not the mode of delivery that affected patient satisfaction regarding communication with healthcare professionals, but rather that their questions and needs were addressed sufficiently.4 5 21 24 These findings are also supported by several studies stating that remote care is a satisfactory alternative to face-to-face care.25–27 Interpersonal interaction, patient involvement in the treatment process and communication are therefore key determinants of patient satisfaction both in the ED and with the remote care through VFC review.
It is important to note that information needs in the ED may differ from those at home, after patients have had time to reflect and become aware of their situation. Furthermore, an ED visit can be stressful and patients’ capacity to process and retain information may be impaired.28 29 The VFC workflow addresses these challenges, as patients receive only the necessary information in the ED and are provided with (digital) leaflets containing information on the VFC review workflow, immobilisation material (brace or cast) and general information about their injury. After a 1-workday interval, they are informed of their definitive diagnosis and further treatment. This process allows patients the opportunity to review relevant information, address remaining or newly arisen concerns, needs or questions, and receive further treatment information in a less stressful setting.30 This was specifically valued by the study participants. The VFC review workflow also enhances the information provision by enabling healthcare professionals to timely inform patients of their entire follow-up treatment from start to finish, rather than just the next step in treatment. This may help patients timely shape realistic expectations for the complete treatment process, potentially increasing satisfaction and enabling self-care.
Although the VFC review workflow responds to several of the identified influential factors, others remain that are not addressed or altered by its implementation (eg, interpersonal skills, patient-centred communication, medical capabilities of healthcare professionals, hospital ambience and facilities, physical and emotional impact of injuries). The patient’s perspective is shaped by the sum of all influential factors, rather than a selected few, and every patient attributes a different measure of relevance to each different factor.9 14 17 19 Therefore, patient experiences can only be optimised if healthcare professionals keep investing in all identified factors. Based on our results, potential for further improvement of ED care and the VFC review workflow lies in more individually tailored communication and information, and adequate coordination between different types of caregivers, such as the administrative outpatient clinic assistant and the healthcare professionals who perform the VFC phone call. It is important to consider the effects of new workflow on all of these factors and try to find the optimal balance between them.
This study had several strengths. First, several qualitative research techniques were used to assure the rigour of this study. We selected a heterogeneous sample in terms of gender, age, type of injury and treatment strategy, and sampling and data collection continued until the point of data saturation. The interviews were conducted by two independent researchers, which was emphasised to the participants to encourage them to speak frankly. Second, the semistructured nature of the interviews enabled uncovering further potential off-topic information. Finally, involvement of different types of healthcare professionals in the development of the topic list enhanced the variety of addressed perspectives in the topics. The analysis was independently conducted by two researchers (ie, researcher triangulation) and relevant quotes were selected to illustrate results, contributing to the analysis’ transparency.
However, several limitations also applied to this study. First, since this study was conducted among patients who received care according to specific workflow (ie, the VFC review workflow), the results may not be transferable to settings with other types of workflow. Second, we only addressed the perspective of patients. Addressing the perspective of both patients and healthcare professionals could help substantiate feasible points of improvement and highlight potential discrepancies between these two stakeholder groups. Finally, although this study identified a variety of factors influencing patient experiences, the explorative, qualitative study design did not allow us to examine the relative importance of these factors and was not designed to compare the VFC review workflow with other types of workflow. Future research using a quantitative study design for this purpose could provide valuable data in this regard.
Conclusion
Patient experiences with ED care and follow-up through the VFC review workflow are shaped by several factors that can be categorised into seven generic themes. The VFC review workflow effectively addresses the majority of the identified influential factors, contributing to the positive feedback from participants. To improve patient experiences when restructuring similar trauma care workflow, recommendations include (1) anticipating the evolving information needs post-ED visit, (2) actively engaging patients early in the ED process to clarify care processes and shape expectations, (3) actively involving patients in treatment steps and the decision-making process (such as showing and explaining medical images), and (4) expanding the scope of information provision and treatment scheduling across the entire pathway.
Supplementary Material
Acknowledgments
On behalf of all contributing authors, we would like to thank the ED staff and casting technicians for their contribution to the implementation of the VFC review protocol and their efforts in sustaining high-quality trauma care. We would also like to thank GD Duijzings for her role as project lead in the VFC project. We also wish to thank Dr JCA Trappenburg (JT), associate professor at the Julius Center from the University Medical Center of Utrecht, and Dr K Romijnders and Dr W de Lange (EM) from The Healthcare Innovation Center, (THINC) for the assistance in the development of the surveys, collecting and analysing of the qualitative data.
Footnotes
Correction notice: This article has been corrected since it was first published. Author names have been updated.
Contributors: GW, JS and RvV conceived the idea for this study. Together with EM and BT, the study design was set up, the study protocol was written and conduct of the study was planned. Approval for the study was requested by GW. Data were then collected and analysed by GW, EM and JS. Substantial contributions to detailed interpretation of the data were consequently made by BT, RvV and CG. The first draft of the manuscript was written by GW, JS and EM. CG, BT and RvV critically revised this manuscript, and revisions were performed by GW and EM. All authors approved the final version of the manuscript for publication and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. GW acts as guarantor for this study.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available upon reasonable request. Study data will be saved on a secure drive of the UMC Utrecht and will be available upon reasonable request.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
The study was not subject to the Dutch Medical Research involving Human Subjects Act. Therefore, a waiver for ethical approval was provided by the Medical Research Ethics Committee: NedMec in Utrecht, the Netherlands (document number 22/034). The participants provided written informed consent prior to the interviews. Data were handled according to the Dutch Implementation Act of the General Data Protection Regulation (GDPR).
References
- 1. VeiligheidNL . Cijferrapportage Letsels 2021. Veiligheid NL: kerncijfers LIS; 2022. [Google Scholar]
- 2. King DM, Vakkalanka JP, Junker C, et al. Emergency department overcrowding LOWERS patient satisfaction scores. Acad Emerg Med 2021;28:363–6. 10.1111/acem.14046 [DOI] [PubMed] [Google Scholar]
- 3. Tekwani KL, Kerem Y, Mistry CD, et al. Emergency department crowding is associated with reduced satisfaction scores in patients discharged from the emergency department. West J Emerg Med 2013;14:11–5. 10.5811/westjem.2011.11.11456 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. de Steenwinkel M, Haagsma JA, van Berkel ECM, et al. Patient satisfaction, needs, and preferences concerning information dispensation at the emergency department: a cross-sectional observational study. Int J Emerg Med 2022;15:5. 10.1186/s12245-022-00407-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Sonis JD, Aaronson EL, Lee RY, et al. Emergency department patient experience: a systematic review of the literature. J Patient Exp 2018;5:101–6. 10.1177/2374373517731359 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Geerdink TH, Salentijn DA, de Vries KA, et al. Optimizing orthopedic trauma care delivery during the COVID-19 pandemic. A closed-loop audit of implementing a virtual fracture clinic and fast-track pathway in a Dutch level 2 trauma center. Trauma Surg Acute Care Open 2021;6:e000691. 10.1136/tsaco-2021-000691 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Davey MS, Coveney E, Rowan F, et al. Virtual fracture clinics in orthopaedic surgery - a systematic review of current evidence. Injury 2020;51:2757–62. 10.1016/j.injury.2020.11.001 [DOI] [PubMed] [Google Scholar]
- 8. Little M, Huntley D, Morris J, et al. The virtual fracture clinic improves quality of care for patients with hand and wrist injuries: an assessment of 3709 patients. J Hand Surg Eur Vol 2020;45:748–53. 10.1177/1753193420930610 [DOI] [PubMed] [Google Scholar]
- 9. Taylor C, Benger JR. Patient satisfaction in emergency medicine. Emerg Med J 2004;21:528–32. 10.1136/emj.2002.003723 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Saunders B, Sim J, Kingstone T, et al. Saturation in qualitative research: exploring its conceptualization and operationalization. Qual Quant 2018;52:1893–907. 10.1007/s11135-017-0574-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. O’Brien BC, Harris IB, Beckman TJ, et al. Standards for reporting qualitative research: a synthesis of recommendations. Acad Med 2014;89:1245–51. 10.1097/ACM.0000000000000388 [DOI] [PubMed] [Google Scholar]
- 12. Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77–101. 10.1191/1478088706qp063oa [DOI] [Google Scholar]
- 13. Patton MQ. Enhancing the quality and credibility of qualitative analysis. Health Serv Res 1999;34(5 Pt 2):1189–208. [PMC free article] [PubMed] [Google Scholar]
- 14. Abass G, Asery A, Al Badr A, et al. Patient satisfaction with the emergency department services at an academic teaching hospital. J Family Med Prim Care 2021;10:1718–25. 10.4103/jfmpc.jfmpc_8_20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Boudreaux ED, O’Hea EL. Patient satisfaction in the emergency department: a review of the literature and implications for practice. J Emerg Med 2004;26:13–26. 10.1016/j.jemermed.2003.04.003 [DOI] [PubMed] [Google Scholar]
- 16. Muntlin A, Gunningberg L, Carlsson M. Patients' perceptions of quality of care at an emergency department and identification of areas for quality improvement. J Clin Nurs 2006;15:1045–56. 10.1111/j.1365-2702.2006.01368.x [DOI] [PubMed] [Google Scholar]
- 17. Sonis JD, White BA. Optimizing patient experience in the emergency department. Emerg Med Clin North Am 2020;38:705–13. 10.1016/j.emc.2020.04.008 [DOI] [PubMed] [Google Scholar]
- 18. Downey LVA, Zun LS. Pain management in the emergency Department and its relationship to patient satisfaction. J Emerg Trauma Shock 2010;3:326–30. 10.4103/0974-2700.70749 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Flynn SB, Gordee A, Kuchibhatla M, et al. Moving toward patient-centered care in the emergency department: patient-reported expectations, definitions of success, and importance of improvement in pain-related outcomes. Acad Emerg Med 2021;28:1286–98. 10.1111/acem.14328 [DOI] [PubMed] [Google Scholar]
- 20. Blackburn J, Ousey K, Goodwin E. Information and communication in the emergency department. Int Emerg Nurs 2019;42:30–5. 10.1016/j.ienj.2018.07.002 [DOI] [PubMed] [Google Scholar]
- 21. Downey LVA, Zun LS. The correlation between patient comprehension of their reason for hospital admission and overall patient satisfaction in the emergency department. J Natl Med Assoc 2010;102:637–43. 10.1016/s0027-9684(15)30641-6 [DOI] [PubMed] [Google Scholar]
- 22. Haug M, Dahm M, Gewald H, et al. Just talk to me - a qualitative study of patient satisfaction in emergency departments. Stud Health Technol Inform 2022;290:385–9. 10.3233/SHTI220102 [DOI] [PubMed] [Google Scholar]
- 23. Blank FSJ, Tobin J, Jaouen M, et al. A comparison of patient and nurse expectations regarding nursing care in the emergency department. J Emerg Nurs 2014;40:317–22. 10.1016/j.jen.2013.02.010 [DOI] [PubMed] [Google Scholar]
- 24. Olthuis G, Prins C, Smits M-J, et al. Matters of concern: a qualitative study of emergency care from the perspective of patients. Ann Emerg Med 2014;63:311–9. 10.1016/j.annemergmed.2013.08.018 [DOI] [PubMed] [Google Scholar]
- 25. Rauer T, Scherer J, Stäubli P, et al. Satisfaction with telemedicine in patients with orthopedic trauma during the COVID-19 lockdown: interview study. JMIR Form Res 2022;6:e35718. 10.2196/35718 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Rizzi AM, Polachek WS, Dulas M, et al. “The new 'normal': rapid adoption of telemedicine in orthopaedics during the COVID-19 pandemic”. Injury 2020;51:2816–21. 10.1016/j.injury.2020.09.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Ekeland AG, Bowes A, Flottorp S. Effectiveness of telemedicine: a systematic review of reviews. Int J Med Inform 2010;79:736–71. 10.1016/j.ijmedinf.2010.08.006 [DOI] [PubMed] [Google Scholar]
- 28. Engel KG, Heisler M, Smith DM, et al. Patient comprehension of emergency department care and instructions: are patients aware of when they do not understand. Ann Emerg Med 2009;53:454–61. 10.1016/j.annemergmed.2008.05.016 [DOI] [PubMed] [Google Scholar]
- 29. Rowe A, Knox M. The impact of the healthcare environment on patient experience in the emergency department: a systematic review to understand the implications for patient-centered design. HERD 2023;16:310–29. 10.1177/19375867221137097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Shuen JA, Wilson MP, Kreshak A, et al. Telephoned, texted, or typed out: a randomized trial of physician-patient communication after emergency department discharge. J Emerg Med 2018;55:573–81. 10.1016/j.jemermed.2018.07.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2023-076040supp001.pdf (106.2KB, pdf)
bmjopen-2023-076040supp002.pdf (97.7KB, pdf)
Data Availability Statement
Data are available upon reasonable request. Study data will be saved on a secure drive of the UMC Utrecht and will be available upon reasonable request.