Abstract
Objective:
Given the rapidly changing food environment and proliferation of ultra-processed foods (UPF) in South Africa (SA), this study aimed to critically evaluate dietary quality and adequacy of low-income adults using the Nova classification system and WHO and World Cancer Research Fund dietary guidelines.
Design:
Secondary household data and 1-d 24-h recalls were analysed from two cross-sectional studies conducted in 2017–2018. Foods consumed were classified according to the Nova classification system. Compliance with WHO dietary guidelines and UPF consumption trends were evaluated.
Setting:
Three low-income areas (Langa, Khayalitsha and Mount Frere) in SA were included.
Participants:
In total, 2521 participants (18–50 years) were included in the study.
Results:
Participants had a mean energy intake of 7762 kJ/d. Most participants were within the acceptable WHO guideline range for saturated fat (80·4 %), total fat (68·1 %), Na (72·7 %) and free sugar (57·3 %). UPF comprised 39·4 % of diets among the average adult participant. Only 7·0 % of all participants met the WHO guideline for fruit and vegetables and 18·8 % met the guideline for fibre. Those within the highest quartile of share of energy from UPF consumed statistically higher amounts of dietary components to limit and were the highest energy consumers overall.
Conclusions:
Low-income adults living in SA are consuming insufficient protective dietary components, while UPF consumption is prevalent. Higher UPF consumers consume larger amounts of nutrients linked to increased chronic disease risk. Policy measures are urgently needed in SA to protect against the proliferation of harmful UPF and to promote and enable consumption of whole and less UPF.
Keywords: Ultra-processed, South Africa, Dietary quality, Low income, Nutrition policy
The manner in which food is produced, distributed and marketed has changed drastically in recent history. Although food security has improved (prior to the onset of the COVID-19 pandemic), economic development has displaced traditional dietary patterns and driven a shift in food preferences, resulting in the nutrition transition(1). This changing food environment, synonymous with a proliferation of packaged foods high in sugar, salt and saturated fat, otherwise known as ultra-processed foods (UPF), undermines dietary patterns based on minimally and unprocessed food and processed culinary ingredients(2). UPF refer to ‘formulations mostly of cheap industrial sources of dietary energy and nutrients plus additives, using a series of processes’(3). These are typically industrially processed foods, high in nutrients known to negatively affect health (Na, saturated and trans-fats and added sugars) and are energy dense(4). These high-energy, low nutritional quality foodstuffs are usually made from cheap ingredients and contain additives such as artificial colourants and flavourants, but are very palatable, require little preparation and are convenient for consumers(5). The entry of large transnational food corporations in the Global South over the last few decades has resulted in rapidly increasing consumption rates of UPF in low- and middle-income countries(6). Consumption habits and choices are continually shifting towards unhealthy UPF due to the price, taste, convenience, availability and marketing strategies employed by large corporations(2).
Although South Africa is classified as an upper-middle income country, it has one of the highest levels of income inequality in the world, with 55 % of the population living in poverty(7), and a continually rising unemployment rate, at 34 % in 2022(8). Given the country’s historical discriminatory past of apartheid, with black people segregated to reside in under-resourced townships with poor access to education and employment, those living in low-income townships remain particularly vulnerable to the effects of rising food prices. Like much of the rest of the Global South, the food environment within South Africa is rapidly changing, with multinational food companies accounting for the majority of the market share(9). Foods are increasingly being eaten away from home, with fast-food options increasing. The higher cost and limited availability of healthy foods make convenient healthy options unattainable for the majority of the population(7,10,11). Additionally, the built environment in townships makes it difficult for low-income shoppers to select healthy foods, with less availability and poorer quality options available in low socioeconomic neighbourhoods(12). As a result, cheap, energy-dense, ultra-processed and unhealthy food options are becoming the food of choice for many(10).
Numerous studies associate the increased consumption of UPF with obesity and diet-related non-communicable diseases (NCD) like hypertension, diabetes, dyslipidaemia and certain cancers(13–16). These diet-related NCD result in increased mortality levels, particularly in low- and middle-income countries, where the majority of these deaths occur(17). Studies in South Africa have shown that foods are selected because they are cheap, filling and tasty, but not necessarily nutritious(10,11). Consequently, NCD, such as diabetes and hypertension, are fast becoming the most burdensome diseases in the South African health system(18,19). One in five women in South Africa is severely obese. Sixty-eight percent of women are overweight or obese, as are 31 % of men. Hypertension, overweight and obesity prevalence have been increasing since 1998(20), and those living with obesity are more likely to suffer from disease multimorbidity(21). On a macronutrient level, obese individuals may appear to be food secure, but on a micronutrient level, food and nutritional insecurities are prevalent(22).
As UPF have been shown to be harmful to health, it is important to examine their intake when assessing dietary patterns and health of individuals and populations(23). The Nova classification system, as a tool to identify UPF, has been used to assess dietary intake in a growing number of countries(24–29). In 2015, the FAO included the Nova system in their guidelines on collecting food processing information from food surveys(30), and a recent WHO report has used the Nova classification system to describe the increase in UPF intake in Latin America over the past decade(31). Applying the Nova food classification system to food composition databases has been identified as a way to quantify the contribution of UPF to the food supply. This can assist in evaluating the quality of dietary intake in various population groups(25). To our knowledge, only one other study has assessed dietary intake in relation to level of processing in South Africa(32).
Therefore, the aims of this study are twofold. First, we seek to describe what share of the diet of low-income adults living in South Africa is comprised of UPF. Second, we seek to assess the adequacy of the diet of low-income adults in South Africa using WHO and World Cancer Research Fund dietary recommendations and evaluate potential associations with level of UPF consumption. Using international criteria to assess dietary intake creates the potential for comparison to other contexts, and analysing the intake of UPF in South Africa allows for better monitoring of the nutrition transition.
Methods
Secondary analysis of dietary data from two purposively selected datasets collected in three low-income areas in South Africa (Langa and Khayelitsha in Cape Town and Mount Frere in the Eastern Cape) was undertaken. These two studies used different sampling strategies, but the same methodology and data collection instruments.
Sampling procedures and data collection
Sampling procedures used in Khayelitsha and Mount Frere differed to those used in Langa, to meet their primary study objectives. The primary objective of the study conducted in Khayelitsha and Mount Frere was to assess the obesogenic food environment(33), whilst the primary objective of the study conducted in Langa was to evaluate dietary changes as a result of the introduction of the health promotion levy (sugary beverage tax)(34). Individuals were only included in the studies if they met the inclusion criteria, which included being between the ages of 18 and 50, residing in the study area, having knowledge about household food purchasing and consumption habits and providing informed consent to participate in the study.
In the study conducted in Khayelitsha and Mount Frere, 300 households were randomly sampled at each site in October and November 2017, with a 20 % oversampling margin to compensate for non-responders. A semi-purposive stratified sampling strategy was used to select research clusters. Four clusters per site were selected based on proximity to key features (transport hubs, supermarkets, main roads and living areas) as well as by housing type. Households in each quadrant were counted to determine an appropriate sampling interval for each cluster and a purposively selected starting point was chosen. In each household, one randomly selected individual was chosen as a respondent between the age of 18–50 years (respondents were stratified to ensure representation of gender). For the Langa sample, systematic door-to-door sampling was conducted in February and March 2018 throughout the entire area of Langa, with a target sample size of 2250 participants. One randomly selected consenting adult between the ages of 18–39 years old per household was included in the study.
All three study sites used the same questionnaires to collect dietary and general household information. The only exception was BMI derived from measured height and weight, which was only collected in Langa. The household socio-demographic questionnaire included previously validated socio-demographic questions, such as household characteristics, the household hunger scale(35) and the lived poverty index(36). A one-day standardised 24-h dietary recall was collected for each participant. Fieldworkers were extensively trained and fluent in languages spoken at the study sites. They used cellphones to digitally record socio-demographic data and paper-based questionnaires to complete the 24-h dietary recalls.
Participants from these primary studies were only included for secondary analysis if they had completed all the questionnaires and did not have any missing dietary intake data. In total, 2161 participants were included from Langa (85·3 % of respondents), 191 from Khayalitsha (61·2 % of respondents) and 169 from Mount Frere (51·2 % of respondents), for a total sample of 2521 adults.
Data coding and analysis
All 24-h dietary recalls were coded by trained data capturers with a tertiary-level nutrition qualification. The South Africa Medical Research Council (SAMRC) food quantities(37) and food composition tables(38) (FCT) were used for coding. An extensive assumptions manual was developed to ensure assumptions were made in a standardised manner when necessary.
Demographic characteristics of study participants included age, sex, area of residence, household income and educational status. BMI was used to assess nutritional status. Dietary intake of study participants was assessed using intake reported in the 1-d 24-h dietary recall, and intake was examined by using mean, median and sd. Food and beverages were classified as UPF according to the Nova food classification system, a system that groups foods, for the purpose of public health policy, into four categories based on the purpose, nature and extent of industrial processing(3,23). The four groups are (1) unprocessed or minimally processed foods, (2) processed culinary ingredients, (3) processed foods and (4) UPF(3,39). As the share of energy intake coming from UPF was the outcome of interest, we classified products into two groups, UPF (Nova group 4) or not (Nova groups 1–3). Two registered dietitians independently applied the Nova classification to the foods and beverages consumed by study participants. Discrepancies between classifications were resolved by consulting with a third dietitian and reaching consensus. Quartiles of UPF consumption were created, based on the share of energy intake that UPF accounted for. Participants were considered to be low UPF consumers if they were within the lowest quartile of UPF consumption and high UPF consumers if they were in the highest quartile.
We used the Healthy Diet Indicator 2020 (HDI-2020)(40) to assess components of diet quality. The HDI-2020 criteria is based on WHO(41,42) and other international dietary recommendations. There are six components for which dietary intake should be restricted, and five components that should be encouraged, following the criteria shown in Table 1. More detail on the HDI-2020 can be read elsewhere(40). When the data from the 24-h dietary recall alone were insufficient to assess whether or not the HDI-2020 criteria were met, the global diet quality questionnaire (DQ-Q) guidelines of the global diet quality score(43) were used to identify products to include in the HDI-2020 criteria. Unfortunately, for nutrient-specific evaluations, missing values in the SAMRC FCT resulted in underreporting of intake for some nutrients in the analyses. This was particularly pronounced for total and added sugar. Please see the limitations section and Appendix A and B for more details. Additionally, there are no free sugar values in the food composition table, so added sugar was used as a proxy. The probability of meeting international dietary recommendations was compared between the lowest and highest quartiles of UPF consumers. For WHO guidelines that use the share of energy as the criteria, the contribution to share of total energy was calculated by quartile of UPF. For components where the guidelines were in grams, rather than share of total energy, the contribution per 1000 kJ was calculated.
Table 1.
Global dietary recommendations assessed using the healthy diet indicator 2020 (HDI-2020)
| Dietary element Elements based on HDI-2020 |
Global recommendation | Reference source for guideline | Criteria for scoring (quantitative intake in one day) | Approach to coding and analysing data | ||
|---|---|---|---|---|---|---|
| Dietary components to limit | 1 | Total fat | <30 % total energy | World Health Organisation | <30 % total energy | Total fat identified and calculated from 24-h diet recall data |
| 2 | Saturated fat | <10 % total energy | World Health Organisation | <10 % total energy | Saturated fat identified and calculated from 24-h diet recall data | |
| 3 | Salt (dietary sodium) | <5 g/d (<2000 mg sodium/d) | World Health Organisation | <2000 mg sodium | Dietary sodium identified and calculated from 24-h diet recall data | |
| 4a | Free (added) sugars (24-h recall) | <10 % total energy | World Health Organisation | <10 % total energy | Added sugars identified and calculated from 24-h diet recall data | |
| 4b | Free sugars (DQ-Q) | <10 % total energy | World Health Organisation | <10 % total energy | Free sugars identified using DQ-Q criteria Amount consumed calculated from 24-h diet recall data |
|
| 5 | Processed meat | ‘Consume very little, if any, processed meat’ | World Cancer Research Fund | 0 g | Processed meat identified using DQ-Q criteria Amount consumed calculated from 24-h diet recall data |
|
| 6 | Unprocessed red meat | ≤350–500 g/week | World Cancer Research Fund | ≤71 g | Unprocessed red meat identified using DQ-Q criteria Amount consumed calculated from 24-h diet recall data |
|
| Dietary components to encourage | 7 | Fruits and vegetables | ≥400 g/d | World Health Organisation | ≥400 g | Fruits and vegetables identified using DQ-Q criteria Amount consumed calculated from 24-h diet recall data |
| 8 | Beans and other legumes | ‘A healthy diet contains…legumes’ | World Health Organisation | >0 g | Beans and legumes identified using DQ-Q criteria Amount consumed calculated from 24-h diet recall data |
|
| 9 | Nuts and seeds | ‘A healthy diet contains… nuts’ | World Health Organisation | >0 g | Nuts and seeds identified using DQ-Q criteria Amount consumed calculated from 24-h diet recall data |
|
| 10 | Whole grains | ‘A healthy diet contains…whole grains’ | World Health Organisation | >0 g | Whole grains identified using DQ-Q criteria Amount consumed calculated from 24-h diet recall data |
|
| 11 | Dietary fibre | >25 g/d | World Health Organisation | >25 g | Dietary fibre identified and calculated from 24-h diet recall data |
DQ-Q, diet quality questionnaire.
We used STATA version 15 (StataCorp) to review, clean and analyse the data. Nutrient content was verified by identifying outliers, checking the original 24-h recalls and correcting the information when appropriate. Participants who consumed more than 20 000 kJ/d or < 400 kJ/d were excluded. Descriptive dietary intake statistics were performed and scores calculated for the household hunger scale(35), lived poverty index(36). The dietary diversity score was calculated from the dietary intake reported the 24-h recall and was assessed by evaluating the minimum dietary diversity for women(44). The Mann–Whitney U test was used to compare differences in nutritional intake by gender. Due to the non-parametric nature of the data, quantile regression analysis was performed to assess differences in median nutrient intake by quartile of UPF consumption. Logistic regression analysis was performed to calculate the probability of low and high UPF consumers meeting WHO and other international dietary guidelines (using the HDI-2020 criteria). All models were adjusted for age, sex, household income and area of residence. For all analyses, a level of significance was assumed at P < 0·05.
Results
Demographics and dietary intake of low-income adults
Of the 2521 study participants, 68·1 % were female. Whilst 40·0 % of participants with anthropometric measurements (n 2024) had a normal weight, obesity prevalence levels were much higher in women, with 43·7 % (n 587) of women, and 7·9 % of men (n 54), living with obesity. The majority (86·2 %) of participants had not completed secondary education, and more than half of the participants had a monthly household income of R3000 (226 USD based on 2018 exchange rates) or less. Dietary diversity was only achieved for 24·3 % of female participants. Despite this, 86·4 % of participants reported little to no household hunger, and 60·5 % reported a low lived poverty index (see Table 2 Panel A).
Table 2.
Share of total energy intake from ultra-processed foods (UPF) according to demographic characteristics†
| Panel A | Panel B | |||||
|---|---|---|---|---|---|---|
| Distribution | Mean share of total energy intake from UPF | P value* | ||||
| n | % | % | se | |||
| Sex | Male | 804 | 31·89 | 38·97 | 0·85 | 0·062 |
| Female | 1717 | 68·11 | 37·09 | 0·56 | ||
| Age | 18–29 | 1453 | 57·64 | 40·24 | 0·62 | <0·001* |
| 30–39 | 974 | 38·64 | 35·36 | 0·75 | ||
| 40–50 | 94 | 3·73 | 22·28 | 1·95 | ||
| Area | Khayelitsha | 191 | 7·58 | 29·81 | 1·57 | <0·001* |
| Langa | 2161 | 85·72 | 39·52 | 0·50 | ||
| Mount Frere | 169 | 6·70 | 23·13 | 1·68 | ||
| Household income (per month) | <R3001 | 1116 | 52·87 | 36·64 | 0·70 | 0·087 |
| R3001–R4000 | 312 | 14·78 | 36·72 | 1·31 | ||
| R4001–R5000 | 211 | 10·00 | 38·22 | 1·74 | ||
| R5001–R7500 | 207 | 9·81 | 38·86 | 1·58 | ||
| R7501–R10000 | 137 | 6·49 | 39·87 | 2·11 | ||
| >R10000 | 128 | 6·06 | 37·93 | 2·13 | ||
| Nutritional** status | Underweight | 108 | 5·34 | 40·90 | 2·24 | 0·933 |
| Normal weight | 809 | 39·97 | 39·85 | 0·83 | ||
| Overweight | 466 | 23·02 | 38·00 | 1·06 | ||
| Obese | 325 | 16·06 | 37·67 | 1·30 | ||
| Severely obese | 184 | 9·09 | 40·12 | 1·75 | ||
| Morbidly obese | 132 | 6·52 | 42·10 | 2·02 | ||
| Education level | No/min formal completed | 123 | 4·90 | 30·17 | 2·13 | 0·002* |
| Completed primary | 2042 | 81·32 | 37·82 | 0·52 | ||
| Completed secondary | 346 | 13·78 | 39·42 | 1·33 | ||
| Completed tertiary | 0 | 0·00 | – | |||
| Lived poverty | Low (<0·51) | 1491 | 60·51 | 37·89 | 0·62 | 0·023 |
| Low-med (0·51–1·0) | 598 | 24·27 | 39·26 | 0·92 | ||
| High-moderate (1·1–1·5) | 214 | 8·69 | 38·08 | 1·67 | ||
| High (>1·5) | 161 | 6·53 | 30·75 | 1·73 | ||
| Household hunger | Little/no hunger | 2169 | 86·41 | 37·83 | 0·51 | 0·469 |
| Moderate hunger | 324 | 12·91 | 36·55 | 1·34 | ||
| Severe hunger | 17 | 0·68 | 39·05 | 6·24 | ||
| Minimum dietary diversity for women (MDD-W)‡ | Achieved MDD-W | 417 | 24·33 | 37·35 | 0·91 | 0·784 |
| Did not achieve MDD-W | 1297 | 75·67 | 37·00 | 0·69 | ||
Regression analysis used to calculate P value. Level of significance assumed at P < 0.05.
Missing values are due to anthropometry measurements only being taken in Langa (sample age 18–39 years; 2024 measurements taken).
Minimum dietary diversity for women (MDD-W) includes only women, up to age of 49 years.
The mean energy intake was significantly higher amongst men than women (8551 kJ/d v. 7393 kJ/d; P < 0·001). This trend was also observed for most other nutrients. Men consumed significantly more total fat (59·7 g/d, P = 0·001) and saturated fat (16·8 g/d, P = 0·005) than women who consumed a mean 51·9 g/d and 14·9 g/d, respectively. The mean daily protein consumption was 10g higher in men than women (67·5 g v. 57·7 g, P < 0·001), whilst total sugar only differed by 2 g/d (64·3 g v. 62·5 g; P = 0·699). Interestingly, despite their energy intake being lower, women consumed significantly more added sugar than men (23·8 g/d v. 20·5 g/d; P < 0·001). They also consumed more whole grains and fruits and vegetables than men, although this was not statistically significant. The average fibre intake amongst participants was 17·4 g/d (see Table 3).
Table 3.
Dietary intake of males and females aged 18–50 years in Langa, Khayelitsha and Mount Frere
| Female | Male | Total | P value | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | s d | Median | IQR | Mean | sd | Median | IQR | Mean | sd | Median | IQR | ||
| Energy (kJ) | 7392·83 | 3123·21 | 6918·08 | 3894·77 | 8550·79 | 3549·63 | 8046·90 | 4332·76 | 7762·13 | 3308·87 | 7328·42 | 4074·97 | <0·001** |
| Energy from UPF (kJ) | 2873·91 | 2384·44 | 2415·70 | 2794·00 | 3464·03 | 2787·10 | 2984·65 | 3281·54 | 3062·11 | 2534·27 | 2595·88 | 3025·00 | <0·001* |
| Protein (g) | 57·65 | 29·69 | 52·43 | 35·52 | 67·47 | 34·05 | 62·12 | 40·67 | 60·78 | 31·48 | 55·27 | 36·35 | <0·001* |
| Total fat (g)‡ | 51·91 | 34·53 | 45·12 | 41·54 | 59·71 | 42·85 | 49·76 | 45·19 | 54·40 | 37·55 | 46·30 | 43·18 | 0·001* |
| Saturated fat (g) | 14·90 | 11·54 | 12·34 | 12·01 | 16·79 | 14·24 | 13·28 | 12·60 | 15·50 | 12·49 | 12·54 | 11·97 | 0·005* |
| MUFA (g) | 17·35 | 13·10 | 14·28 | 14·29 | 19·97 | 17·12 | 15·24 | 15·66 | 18·18 | 14·55 | 14·60 | 14·63 | 0·003* |
| PUFA (g) | 14·09 | 11·48 | 11·01 | 12·77 | 16·22 | 13·98 | 12·07 | 15·18 | 14·77 | 12·37 | 11·29 | 13·59 | 0·004* |
| Carbohydrate (g) | 246·96 | 107·65 | 233·11 | 131·74 | 276·35 | 117·43 | 265·30 | 149·31 | 256·33 | 111·68 | 243·99 | 140·09 | <0·001* |
| Total sugar (g)† | 62·47 | 46·03 | 53·40 | 58·23 | 64·34 | 49·97 | 56·56 | 63·15 | 64·07 | 47·32 | 54·40 | 58·23 | 0·699 |
| Added sugar (g)† | 23·81 | 31·33 | 16·63 | 35·59 | 20·52 | 31·31 | 4·61 | 31·52 | 22·76 | 31·36 | 14·63 | 34·28 | <0·001* |
| Dietary Na | 1534·28 | 1301·44 | 1252·68 | 1215·13 | 1825·11 | 1515·98 | 1558·64 | 1565·59 | 1627·03 | 1379·88 | 1318·66 | 1336·48 | <0·001* |
| Processed meat (g) | 20·57 | 57·04 | 0·00 | 0·00 | 24·91 | 74·47 | 0·00 | 0·00 | 21·95 | 63·15 | 0·00 | 0·00 | 0·905 |
| Unprocessed red meat (g) | 22·31 | 68·54 | 0·00 | 0·00 | 35·53 | 100·73 | 0·00 | 0·00 | 26·53 | 80·44 | 0·00 | 0·00 | 0·008* |
| Dietary fibre (g) | 16·82 | 10·48 | 14·79 | 11·27 | 18·62 | 11·35 | 16·66 | 12·74 | 17·40 | 10·80 | 15·30 | 11·78 | <0·001* |
| Fruits and vegetables (g) | 129·52 | 171·08 | 75·00 | 170·00 | 127·29 | 167·86 | 68·50 | 187·00 | 128·81 | 170·03 | 75·00 | 175·00 | 0·186 |
| Beans and other legumes (g) | 4·09 | 23·92 | 0·00 | 0·00 | 5·43 | 30·23 | 0·00 | 0·00 | 4·52 | 26·10 | 0·00 | 0·00 | 0·447 |
| Nuts and seeds (g) | 1·71 | 7·94 | 0·00 | 0·00 | 2·79 | 11·36 | 0·00 | 0·00 | 2·06 | 9·18 | 0·00 | 0·00 | 0·080 |
| Whole grains (g) | 29·47 | 99·37 | 0·00 | 0·00 | 23·67 | 88·09 | 0·00 | 0·00 | 27·62 | 95·94 | 0·00 | 0·00 | 0·133 |
Level of significance assumed at P < 0.05. Mann–Whitney U test used to analyse level of significant difference between males and females.
For nutrient-specific evaluations, missing values in the South African food composition table resulted in an underestimate of values, which was particularly pronounced for total and added sugar (see Appendix Tables A and B for details).
Trans-fats excluded from all analysis due to insufficient data in the South African food composition table.
Ultra-processed product intake
The percentage of total energy intake from UPF was similar amongst men and women (39·0 % and 37·1 %, respectively, P = 0·062). UPF intake accounted for a significantly larger share of dietary intake amongst younger consumers, contributing 40·2 % of daily energy intake amongst 18–29-year-olds, and 22·3 % of intake amongst 40–50-year-olds (P < 0·001). Household income was not associated with the proportion of UPF consumed (P = 0·087), as those with the lowest household income (<R3001/d) consumed a similar proportion of UPF to the highest income households (>R10 000/d), at 36·7 % and 37·9 % of total daily intake, respectively. Those without any formal education consumed significantly lower amounts of UPF (30·2 %) than those who had completed primary (37·8 %) and secondary (39·4 %) education (P = 0·002) (see Table 2 Panel B).
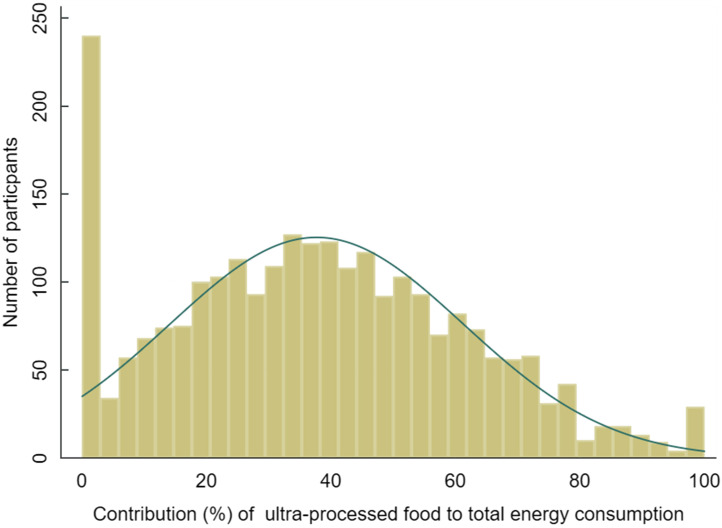
Figure 1 shows the distribution of the share of UPF to total energy intake amongst study participants. Very few participants (7·6 %, n 192) reported that they did not consume any UPF in the previous day. There were clear gradients with respect to nutrient intake, when analysed by quartile of share of energy from UPF. The highest quartile of UPF consumers consumed a median 10264 kJ/d of total energy (60·3 % of which was accounted for by UPF intake), whilst the lowest quartile consumed a median 5605 kJ/d (of which 7·8 % was attributed to UPF). The same significant trend by quartile for median intake was observed for total fat, saturated fat, total sugar and Na, with the highest UPF consumers consuming the largest quantities of these nutrients of concern linked with NCD and obesity. Added sugar intake also increased by UPF quartile, but the difference between quartiles was NS. Interestingly, median total fibre and fruit and vegetable intake also increased by quartile of UPF consumers, although the increase was NS for fruits and vegetables. In both of these groups, despite the increase in absolute terms, the opposite trend, which was significant, was observed for g/1000kJ, with the contribution decreasing with each ascending quartile (whilst Na had the opposite trend) (Table 4).
Fig. 1.
Distribution of the share of UPF to total energy intake. UPF, ultra-processed foods.
Table 4.
Dietary intake by quartile of share of energy from ultra-processed foods (UPF) for adults aged 18–50 years in Langa, Khayalitsha and Mount Frere
| UPF | P value | Share of total energy | P value | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N † | Q1 | Q2 | Q3 | Q4 | Q1 UPF | Q2 UPF | Q3 UPF | Q4 UPF | ||||||||||||
| Median | se | Median | se | Median | se | Median | se | % | se | % | se | % | se | % | se | |||||
| Dietary components to limit | Total energy (kJ/d) | 2111 | 5605·07 | 144·28 | 6485·22 | 127·44 | 7604·26 | 137·92 | 10264·25 | 155·25 | <0·001* | – | – | – | – | – | ||||
| Energy from UPF (kJ/d) | 2111 | 529·87 | 40·53 | 1931·93 | 26·70 | 3281·72 | 38·36 | 5803·44 | 105·89 | <0·001* | 7·75 | 0·67 | 30·58 | 0·69 | 44·47 | 0·77 | 60·29 | 0·88 | <0·001* | |
| Total fat (g/d) | 2111 | 28·24 | 1·06 | 38·06 | 0·98 | 50·23 | 0·96 | 79·64 | 2·09 | <0·001* | 20·44 | 0·46 | 23·07 | 0·56 | 25·53 | 0·39 | 29·44 | 0·58 | <0·001* | |
| Saturated fat (g/d) | 2111 | 7·57 | 0·35 | 10·59 | 0·31 | 13·67 | 0·37 | 21·74 | 0·65 | <0·001* | 5·27 | 0·15 | 6·03 | 0·14 | 6·84 | 0·16 | 8·28 | 0·22 | <0·001* | |
| Total sugar‡ (g/d) | 2111 | 31·24 | 1·57 | 48·16 | 1·78 | 63·63 | 1·88 | 85·94 | 2·73 | <0·001* | 9·15 | 0·42 | 13·18 | 0·50 | 14·66 | 0·40 | 14·53 | 0·42 | <0·001* | |
| Added sugar‡ (g/d) | 2111 | 6·48 | 0·95 | 12·82 | 1·62 | 12·88 | 1·71 | 21·34 | 1·80 | 0·331 | 1·93 | 0·28 | 3·23 | 0·39 | 2·90 | 0·39 | 3·36 | 0·35 | 0·016* | |
| Contribution (mg or g) per 1000kJ energy | ||||||||||||||||||||
| Dietary Na (mg/d) | 2111 | 466·87 | 28·61 | 1073·50 | 21·27 | 1584·16 | 34·82 | 2624·83 | 57·66 | <0·001* | 83·38 | 5·71 | 172·32 | 3·27 | 215·07 | 4·69 | 262·35 | 5·89 | <0·001* | |
| Dietary components to encourage | Dietary Fibre (g/d) | 2111 | 12·00 | 0·43 | 14·45 | 0·46 | 15·74 | 0·30 | 19·50 | 0·42 | <0·001* | 2·26 | 0·06 | 2·20 | 0·05 | 2·11 | 0·04 | 1·89 | 0·04 | <0·001* |
| Fruits and Vegetables (g/d) | 2111 | 70·85 | 5·77 | 75·85 | 6·73 | 72·85 | 5·96 | 70·85 | 5·20 | 0·098 | 13·47 | 1·21 | 12·29 | 1·22 | 9·74 | 0·76 | 7·13 | 0·51 | 0·004* | |
Adjusted for age, sex, household income and area of residence. Level of significance assumed at P < 0.05.
410 participants excluded from all analysis due to missing data on household income.
For nutrient-specific evaluations, missing values in the South African food composition table resulted in an underestimate of values, which was particularly pronounced for total and added sugar (see Appendix Tables A and B for details).
Quantile regression analysis performed due to non-parametric data to assess differences in intake by quartile of UPF consumption. Quartiles of UPF consumption were created based on the share of absolute energy intake that UPF accounted for. Participants were considered to be low UPF consumers if they were within the lowest quartile of UPF consumption, and high UPF consumers if they were in the highest quartile of UPF consumption.
Analysis of processed meats, unprocessed red meat, beans and other legumes, nuts and seeds and whole grains excluded from analysis due to low number of participants consuming these dietary components and small cell counts not permitted for quantile regression.
Adequacy of the diet based on international recommendations
In Table 5, Panel A shows that overall, very few participants met international recommendations for dietary components that are beneficial to health. Only 7·0 % of participants met the WHO recommended intake of 400 g of fruit and vegetables per day in the previous day. The mean intake amongst the 1963 participants who did not meet the guideline was 93·0 g/d. Similarly, low numbers of participants met the protective recommendations for frequent consumption of beans and other legumes, nuts and seeds and whole grains (with 4·6 %, 7·3 % and 15·6 % meeting each respective guideline). Slightly more (18·8 %) participants met the recommended intake of 25 g or more of fibre per day, although the mean intake amongst those who did not meet it remained low, at 13·9 g/d
Table 5.
Using the healthy diet indicator 2020 to assess the probability of low and high ultra-processed foods (UPF) consumers meeting WHO and other international dietary guidelines
| Panel A | Panel B | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Dietary element | Criteria for scoring (quantitative intake in one day) | n† | Meets guideline | Does not meet guideline | P-value* | ||||||||||||
| n | % | Mean | s e | n | % | Mean | se | Predicted probability of meeting guideline if low UPF consumer‡ | Predicted probability of meeting guideline if high UPF consumer‡ | ||||||||
| % | se | % | se | ||||||||||||||
| Dietary components to limit | 1 | Total fat | <30 % total energy | 2111 | 1437 | 68·07 | 39·44 | 0·59 | 674 | 31·93 | 85·49 | 1·63 | 78·59 | 1·80 | 52·40 | 2·22 | <0·001* |
| 2 | Saturated fat | <10 % total energy | 2111 | 1698 | 80·44 | 11·63 | 0·17 | 413 | 19·56 | 31·06 | 0·82 | 88·89 | 1·38 | 66·34 | 2·11 | <0·001* | |
| 3 | Dietary Na | <2000 mg sodium | 2111 | 1535 | 72·71 | 1001·80 | 14·24 | 576 | 27·29 | 3290·02 | 66·29 | 97·88 | 0·61 | 25·00 | 1·94 | <0·001* | |
| 4a | Free (added) sugars (24-h recall) | <10 % total energy | 2111 | 1732 | 82·05 | 12·86 | 0·40 | 379 | 17·95 | 67·00 | 2·05 | 79·77 | 1·73 | 83·71 | 1·67 | 0·109 | |
| 4b | Free sugars (DQ-Q) | <10 % total energy | 2111 | 1209 | 57·27 | 22·09 | 0·83 | 902 | 42·73 | 23·24 | 1·13 | 79·76 | 1·80 | 40·35 | 2·13 | <0·001* | |
| 5 | Processed meat | 0 g | 2111 | 1680 | 79·58 | 0·00 | 0·00 | 431 | 20·42 | 103·63 | 5·01 | 94·21 | 0·98 | 60·86 | 2·19 | <0·001* | |
| 6 | Unprocessed red meat | ≤71 g | 2111 | 1834 | 86·88 | 1·96 | 0·26 | 277 | 13·12 | 189·25 | 8·09 | 87·72 | 1·46 | 84·66 | 1·56 | 0·156 | |
| Dietary components to encourage | 7 | Fruits and vegetables | ≥400 g | 2111 | 148 | 7·01 | 589·65 | 18·84 | 1963 | 92·99 | 93·86 | 2·26 | 7·49 | 1·19 | 6·82 | 1·07 | 0·678 |
| 8 | Beans and other legumes | >0 g | 2111 | 98 | 4·64 | 99·62 | 7·96 | 2013 | 95·36 | 0·00 | 0·00 | 7·34 | 1·16 | 2·95 | 0·73 | 0·002* | |
| 9 | Nuts and seeds | >0 g | 2111 | 153 | 7·25 | 29·27 | 1·65 | 1958 | 92·75 | 0·00 | 0·00 | 1·46 | 0·52 | 12·26 | 1·48 | <0·001* | |
| 10 | Whole grains | >0 g | 2111 | 329 | 15·59 | 167·25 | 9·58 | 1782 | 84·41 | 0·00 | 0·00 | 10·15 | 1·31 | 17·32 | 1·70 | 0·001* | |
| 11 | Dietary fibre | >25 g | 2111 | 396 | 18·76 | 34·72 | 0·54 | 1715 | 81·24 | 13·91 | 0·14 | 15·06 | 1·56 | 26·56 | 1·96 | <0·001* | |
UPF,ultra-processed foods.
Logistic regression analysis performed to calculate the probability of meeting dietary guidelines by quartile of UPF intake. Adjusted for age, sex, household income and area of residence. Level of significance assumed at P < 0.05.
410 participants excluded from all analysis due to missing data on household income. For nutrient-specific evaluations, missing values in the South African food composition table resulted in an underestimate of compliance with guidelines. This was particularly pronounced for total and added sugar (see Appendix A and B for more details).
Low UPF consumers are those with the lowest quartile of UPF consumption, and high UPF consumers are those with the highest quartile of UPF consumption.
At least 50 % of participants met the recommendations for all nutrients to limit. Sixty-eight percent of participants met the recommendation of consuming < 30 % of their total energy intake from fat, 80·4 % consumed < 10 % of their total energy intake from saturated fat per day and 72·7 % consumed < 2000 mg Na per day. No processed meat was consumed by 79·6 % of participants on the previous day, and 86·9 % of participants did not consume excessive amounts of red meat. Although free and added sugar intakes were difficult to assess (see the methods and limitation section for more details), depending on whether intake was assessed using the free sugar criteria from the DQ-Q or the 24-h recall data for added sugar, between 57·3 % and 82·1 % met the recommendation of < 10 % of total energy, respectively (Table 5 Panel A).
Alignment of international dietary recommendations and the Nova system in assessing dietary inadequacy
In Table 5, Panel B shows the predicted probabilities of meeting international guidelines by level of UPF consumption (high v. low). For dietary recommendations that consider the share of total energy (total fat, saturated fat and free sugar), high UPF consumers were significantly less likely to meet the recommendation than low UPF consumers. The only exception was free sugar intake when using added sugar from the 24-h recall, which did not have a significant difference. High UPF consumers were also significantly more likely to have excessive Na and processed meat intake and insufficient bean and legume consumption. However, high UPF consumers were significantly more likely to meet the recommendations for nuts and seeds, wholegrain and fibre intake. No significant differences were observed between high and low UPF consumers for fruit and vegetable intake or unprocessed red meat consumption.
Discussion
Despite the participants being low-income adults living in South Africa, most participants reported either low or low-medium levels of lived poverty, and only 13·6 % reported moderate to severe hunger. These findings are somewhat aligned with findings from studies conducted amongst low-income South Africans(45,46), although since undertaking this study (data collected in 2017 and 2018), levels of lived poverty and food insecurity have worsened in South Africa(45,46). Only 24·3 % of women met the criteria for minimum dietary diversity, indicating that although they might not report high levels of hunger, the diet is not nutritionally diverse, and is lacking in micronutrients. This is supported in that, for all components identified in the HDI-2020 to be protective for health, less than 20 % of participants consumed adequate amounts. The number of participants who met the fibre recommendation (18·8 %) was similar to the number of participants who met the wholegrain recommendation (15·6 %), which also contributes towards fibre intake. These protective foods are often costly, resulting in cheaper, more filling and unhealthier alternatives being selected instead(10).
While most participants met the recommendations for total fat, saturated fat and Na intake, examining nutrient intake based on energy consumed from UPF reveals that disparities exist in the healthfulness of participants diets. Those who consumed the most UPF also consumed the most energy and dietary components that are recommended to be restricted, except for red meat where no significant difference was observed in the two groups. Numerous studies have linked high UPF consumption to poor health outcomes(47). While we did not look at specific health outcomes, we found a clear positive gradient of association between share of energy from UPF and nutrients of concern and an inverse association between share of energy from UPF and dietary components to encourage. Consequently, the probability of meeting international dietary guidance is higher among those who are in the lowest UPF consumption quantile compared with those who are on the highest quantile of UPF consumption. Given the findings of this study, and others around the world that have found high and increasing intake of UPF(15), the WHO should consider introducing a recommendation regarding the maximum recommended share that UPF should contribute to total energy (similar to the guidelines it has developed for saturated fat or free sugar).
The high level of UPF consumption reported amongst low-income South Africans in our study supports literature that indicates that the nutrition transition is advanced in South Africa(48), which typically goes hand in hand with the proliferation of UPF, and increasing levels of obesity and nutrition-related NCD(15). This study highlights the need for the South African Government to implement better strategies to protect South Africans against the proliferation of UPF, and more importantly to protect low-income South Africans who are most vulnerable to the economic shocks of poor health outcomes from undue influence towards UPF consumption. Recent studies in South Africa have found that 76 % of packaged foods sold in South African supermarkets are UPF(49), and that more shelf space in stores is allocated to unhealthy products than healthy products(50) leaving little room for consumers to make healthy food choices. There is a need to ensure that healthy and nutritious foods are readily available, affordable and desirable to consumers, including low-income people, and that unhealthy UPF are less predominantly the food of choice.
A policy that the South African National Department of Health is currently considering and could contribute to an improved food environment is mandatory front-of-package warning labels(51). These labels inform consumers about products containing excessive amounts of nutrients of concern and can in turn be used to inform further regulations, such as marketing restrictions (e.g. barring two-for-the-price-of-one specials, promotions to win prizes, advertisements to children, etc.), restricting these products in schools or at point-of-sale in supermarkets where consumers are more likely to make rash decisions. Such policies have already been or are soon to be implemented in Chile, Mexico, Peru, Israel, Singapore and the United Kingdom. Additionally, measures similar to the Health Promotion Levy (a tax on sugary beverages which has been found to be effective in South Africa)(34,52) could be considered for products that carry a front-of-package warning label. Revenue raised could be used to subsidise the price of healthier food choices. In the same way that unhealthy UPF should be restricted, the consumption of healthy fresh foods should be encouraged.
Limitations and assumptions
This study has a number of limitations that need to be kept in mind when interpreting the data. First, only two of the nine provinces of South Africa were included, which limits the generalisability of findings. Data from two different studies were included. Although similar methodologies, standardised training and the same questionnaires were used for both studies, sampling strategies differed between the studies, some of the fieldworkers differed and study participants were not exactly the same. The sample size also differed significantly by area. To try and account for this, regression analysis results were adjusted for area of residence, age, sex and household income.
Second, seasonality has been found to influence dietary intake(53). Although three seasons were included during data collection (summer and autumn in Langa and spring in Khayalitsha and Mount Frere), it is possible that results may have differed had all four seasons been included.
Third, when collecting dietary data, one needs to take self-reported bias as well as social desirability bias into account. Dietary assessment was based on a single-day 24-h recall due to the available secondary data and did not capture intra-person day-to-day variation in intake. The distribution of intake would have been better accounted for with two or more 24-h recalls per participant or the inclusion of a quantified FFQ for a subset of the sample; however, the large sample size of this study allows for sufficiently accurate means with a single-day recall(53). Despite the one day of recall data likely resulting in a wider distribution of intake due to more measurement error, the rank ordering of quartiles is still appropriate, assuming measurement error is random. The observations in the top 25th percentile would very likely be the same, even with multiple days of recall.
Fourth, there were missing values in the SAMRC FCT, particularly for total and added sugar. Thus when the SAMRC FCT was applied to the intake data, we found that 19·4 % and 30·6 % of food items reported consumed were missing total and added sugar values, respectively. More than 50 % of these missing values were UPF products, and missingness was greater among UPF products than among all products. There were no missing values for energy, and five or less percent of missing values for total fat, saturated fat, Na and fibre, and thus the degree of underestimation of intake is higher for total and added sugar. Food groups where more than 40 % of consumed products were UPF included soups, sauces and seasonings; beverages; sugars, syrups and sweets and other products. These food groups tended to have higher numbers of missing values originating from UPF products than products that were not UPF (although this varied by nutrient and food group). As such, the findings presented in this paper regarding the share of nutrients of concern to discourage are likely conservative in terms of the association between the percentage of UPF consumed and nutrient outcomes (see Appendix A and B for more details). Additionally, the SAMRC FCT does not have brand level nutritional information (nor was this captured in the 24-h recalls). The nutritional composition of packaged UPF can differ significantly from one brand to another. However, the SAMRC FCT is the only South African specific FCT available, and thus remains the most appropriate FCT to use currently.
Fifth, assumptions needed to be made when classifying products according to the Nova food classification categories. As the secondary dietary data used for this study were not detailed, certain assumptions such as whether products were home-made or shop bought needed to be made. Although steps were put in place to limit classification errors, it is possible that some products were incorrectly classified. Little to no analysis of UPF using 24-h recall data has been conducted in South Africa previously, so despite the limitations with the dietary data, this study provides a baseline assessment of UPF consumption amongst low-income people living in South Africa.
Conclusion
The nutrition transition is advanced, and UPF consumption is prevalent amongst low-income consumers in South Africa. UPF contribute disproportionately to energy intake, especially amongst those with the highest UPF consumption, and these high UPF consumers consume larger amounts of nutrients associated with increased NCD risk. Compared with low UPF consumers, high UPF consumers have higher overall energy consumption, higher Na, sugar and fat intake and are less likely to meet WHO recommendations for nutrients to limit. Most low-income adults living in South African assessed in this study consumed insufficient protective dietary components such as fibre, legumes, fruits and vegetables and had insufficient dietary diversity. Policy measures are urgently needed in South Africa to protect against the proliferation of harmful UPF and to promote and enable the consumption of whole and less processed foods. These measures could include a mandatory front-of-package warning label, marketing restrictions, restrictions on the types of foods available in schools. Additionally, a tax on unhealthy products could be used to promote the consumption of healthier food options by using revenue raised to subsidise the cost of healthy food options. There is an urgent need to realign the food system in South Africa and make healthy options achievable for all.
Supporting information
Frank et al. supplementary material
Acknowledgements
We wish to thank all the fieldworkers involved in data collection in Langa, Khayalitsha and Mount Frere, who did an outstanding job of collecting data, as well as the team involved in the broader ROFE project. Joelaine Chetty and Ria Laubscher from the South African Medical Research Council are thanked for their assistance with understanding and analysing the South African food composition data. We also wish to thank Jessica Ostrowski and Karen Ritter from the University of North Carolina; Jessica for assisting with Nova classification coding and Karen for providing support with dietary data analysis. The School of Public Health at the University of the Western Cape is thanked for their administrative support of the project.
Financial support
The International Development Research Centre (IDRC), Canada, funded this work and a student scholarship, grant number [108425–001]. Additional funding was received by Bloomberg Philanthropies and US NIH grant number CPC P2C HD050924.
Conflict of interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of the data; in writing the manuscript, or in the decision to publish the results.
Authorship
T.F., S.W.N. and E.C.S conceptualised and planned the methodology for the manuscript; T.F. took care of data curation, formal analysis, investigation and original draft preparation, while review and editing was performed by T.F., S.W.N, C.M.L., A.M.T. and E.C.S.; funding acquisition and resources were handled by S.W.N. and E.C.S; and E.C.S supervised the project.
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/S1368980023002811
Ethics of human subject participation
This study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving research study participants were approved by the Human and Social Sciences Research Ethics committee HS19/6/3 of the University of the Western Cape, SA. Written informed consent was obtained from all subjects.
References
- 1. Imamura F, Micha R, Khatibzadeh S et al. (2015) Dietary quality among men and women in 187 countries in 1990 and 2010: a systematic assessment. Lancet Glob Heal 3, e132–e142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Moodie R, Stuckler D, Monteiro C et al. (2013) Profits and pandemics: prevention of harmful effects of tobacco, alcohol, and ultra-processed food and drink industries. Lancet 381, 670–679. [DOI] [PubMed] [Google Scholar]
- 3. Monteiro CA, Cannon G, Moubarac JC et al. (2017) The UN decade of nutrition, the NOVA food classification and the trouble with ultra-processing. Public Health Nutr 21, 5–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Poti JM, Braga B & Qin B (2017) Ultra-processed food intake and obesity: what really matters for health—processing or nutrient content? Curr Obes Rep 6, 420–431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Monteiro CA, Moubarac JC, Cannon G et al. (2013) Ultra-processed products are becoming dominant in the global food system. Obes Rev 14, 21–28. [DOI] [PubMed] [Google Scholar]
- 6. Stuckler D, McKee M, Ebrahim S et al. (2012) Manufacturing epidemics: the role of global producers in increased consumption of unhealthy commodities including processed foods, alcohol, and tobacco. PLoS Med 9, e1001235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. World Bank (2023) Poverty and Equity Brief. Africa Eastern & Southen. South Africa. https://www.worldbank.org/en/topic/poverty/publication/poverty-and-equity-briefs (accessed October 2023).
- 8. Statistics South Africa (2022) Quarterly labour force survey. Quarter 4. Pretoria: Statistics South Africa. https://www.statssa.gov.za/publications/P0211/P02114thQuarter2022.pdf (accessed October 2023).
- 9. Igumbor EU, Sanders D, Puoane TR et al. (2012) “Big food,” the consumer food environment, health, and the policy response in South Africa. PLoS Med 9, e1001253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Temple NJ & Steyn NP (2011) The cost of a healthy diet: a South African perspective. Nutr 27, 505–508. [DOI] [PubMed] [Google Scholar]
- 11. Statistics South Africa (2015) Technical Report: Methodological report on rebasing of national poverty lines and development on pilot provincial poverty lines. Pretoria: Statistics South Africa. http://beta2.statssa.gov.za/publications/Report-03-10-11/Report-03-10-11.pdf (accessed October 2023).
- 12. Odunitan-Wayas F, Okop K, Dover R et al. (2018) Food purchasing characteristics and perceptions of neighborhood food environment of South Africans living in low-, middle- and high-socioeconomic neighborhoods. Sustainability 10, 4801. [Google Scholar]
- 13. Hall KD, Ayuketah A, Brychta R et al. (2019) Ultra-processed diets cause excess calorie intake and weight gain: an inpatient randomized controlled trial of ad libitum food intake. Cell Metab 30, 67–77.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Monteiro CA, Moubarac JC, Levy RB et al. (2018) Household availability of ultra-processed foods and obesity in nineteen European countries. Public Health Nutr 21, 18–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Baker P, Machado P, Santos T et al. (2020) Ultra-processed foods and the nutrition transition: global, regional and national trends, food systems transformations and political economy drivers. Obes Rev 21, 1–22. [DOI] [PubMed] [Google Scholar]
- 16. Chen X, Zhang Z, Yang H et al. (2020) Consumption of ultra-processed foods and health outcomes: a systematic review of epidemiological studies. Nutr J 19, 86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. World Health Organisation (2010) Global status report on noncommunicable diseases. Geneva: WHO. https://digitallibrary.un.org/record/706319?ln=en (accessed October 2023).
- 18. Wicks M, Wright H & Wentzel-Viljoen E (2017) Restricting the marketing of foods and non-alcoholic beverages to children in South Africa: are all nutrient profiling models the same? Br J Nutr 116, 2150–2159. [DOI] [PubMed] [Google Scholar]
- 19. Roomaney RA, van Wyk B, Turawa EB et al. (2021) Multimorbidity in South Africa: a systematic review of prevalence studies. BMJ Open 11, e048676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Statistics South Africa (2017) Key Indicator Report: South African Demographic and Health Survey (SADHS). Pretoria: Statistics South Africa. https://www.statssa.gov.za/publications/Report%2003-00-09/Report%2003-00-092016.pdf (accessed October 2023).
- 21. Roomaney RA, van Wyk B, Cois A et al. (2022) One in five South Africans are multimorbid: an analysis of the 2016 demographic and health survey. PLoS One 17, e0269081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Mchiza Z, Steyn N, Hill J et al. (2015) A review of dietary surveys in the adult South African population from 2000 to 2015. Nutrients 7, 8227–8250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Moubarac JC, Parra DC, Cannon G et al. (2014) Food classification systems based on food processing: significance and implications for policies and actions: a systematic literature review and assessment. Curr Obes Rep. 3, 256–272. [DOI] [PubMed] [Google Scholar]
- 24. Monteiro CA, da Costa Louzada ML, Steele E et al. (2018) Ultra-processed food consumption and chronic non-communicable diseases-related dietary nutrient profile in the UK (2008–2014). Nutrients 10, 587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. O’Halloran SA, Lacy KE, Grimes CA et al. (2017) A novel processed food classification system applied to Australian food composition databases. J Hum Nutr Diet 30, 534–541. [DOI] [PubMed] [Google Scholar]
- 26. Juul F & Hemmingsson E (2015) Trends in consumption of ultra-processed foods and obesity in Sweden between 1960 and 2010. Public Health Nutr 18, 3096–3107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Solberg SL, Terragni L & Granheim SI (2016) Ultra-processed food purchases in Norway: a quantitative study on a representative sample of food retailers. Public Health Nutr 19, 1990–2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Moubarac JC, Martins APB, Claro RM et al. (2013) Consumption of ultra-processed foods and likely impact on human health. Evidence from Canada. Public Health Nutr 16, 2240–2248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. da Costa Louzada ML, Baraldi LG, Steele EM et al. (2015) Consumption of ultra-processed foods and obesity in Brazilian adolescents and adults. Prev. Med. 81, 9–15. [DOI] [PubMed] [Google Scholar]
- 30. Food and Agriculture Organization (2015) Guidelines on the collection of information on food processing through food consumption surveys. Rome: FAO. https://www.fao.org/documents/card/es/c/a7e19774-1170-4891-b4ae-b7477514ab4e/ (accessed October 2023).
- 31. Pan American Health Organization (2015) Ultra-processed food and drink products in Latin America: Trends, impact on obesity, policy implications. Washington, DC: PAHO. https://iris.paho.org/bitstream/handle/10665.2/7699/9789275118641_eng.pdf (accessed Oct 2023).
- 32. Jacobs I, Taljaard-Krugell C, Wicks M et al. (2022) Degree of food processing and breast cancer risk in black urban women from Soweto, South African: the SABC study. Br J Nutr 128, 2278–2289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Kroll F, Swart EC, Annan RA et al. (2019) Mapping obesogenic food environments in South Africa and Ghana: correlations and contradictions. Sustainability 11, 3924. [Google Scholar]
- 34. Essman M, Taillie LS, Frank T et al. (2021) Taxed and untaxed beverage intake by South African young adults after a national sugar-sweetened beverage tax: a before-and-after study. PLOS Med 18, e1003574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Ballard T, Coates J, Swindale A et al. (2011) Household Hunger Scale : Indicator Definition, Measurement Guide. Washington, DC: FANTA, FHI 360. https://www.fantaproject.org/sites/default/files/resources/HHS-Indicator-Guide-Aug2011.pdf (accessed October 2023).
- 36. Mattes R, Dulani B & Gyimah-Boadi E (2016) Africa’s growth dividend? Lived poverty drops across much of the continent. Policy Paper no. 29. Cape Town: Afrobarometer. https://afrobarometer.org/sites/default/files/publications/Policy%20papers/ab_r6_policypaperno29_lived_poverty_declines_in_africa_eng.pdf (accessed October 2023).
- 37. Langenhoven M, Conradie P, Wolmarans P et al. (1991) Medical Research Council Food Quantities Manual, 2nd ed. Cape Town: South African Medical Research Council. [Google Scholar]
- 38. Medical Research Council (2017) Food Composition Tables for South Africa, 5th ed. Cape Town: Medical Research Council. [Google Scholar]
- 39. Monteiro CA, Cannon G, Levy R et al. (2016) NOVA. The star shines bright. World Nutr 7, 28–38. [Google Scholar]
- 40. Herforth AW, Wiesmann D, Martínez-Steele E et al. (2020) Introducing a suite of low-burden diet quality indicators that reflect healthy diet patterns at population level. Curr Dev Nutr 4, 1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. World Health Organization (2012) Guideline: Sodium intake for adults and children. Geneva: WHO. https://www.who.int/publications/i/item/9789241504836 (accessed October 2023). [PubMed]
- 42. World Health Organization (2015) Guideline: Sugars intake for adults and children. Geneva: WHO. https://www.who.int/publications/i/item/9789241549028 (accessed October 2023). [PubMed]
- 43. Bromage S, Batis C, Bhupathiraju SN et al. (2021) Development and validation of a novel food-based global diet quality score (GDQS). J Nutr 151, 75S–92S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Food and Agriculture Organization (2021) Minimum dietary diversity for women. Rome: FAO. https://www.fao.org/nutrition/assessment/tools/minimum-dietary-diversity-women/en/ (accessed October 2023).
- 45. Mattes R (2020) Lived poverty on the rise: Decade of living-standard gains ends in Africa. Cape Town: Afrobarometer. https://www.afrobarometer.org/sites/default/files/publications/Policy%20papers/ab_r7_pap13_lived_poverty_on_the_rise_in_africa_1.pdf (accessed October 2023).
- 46. Statistics South Africa (2019) Measuring food security in South Africa: Applying the food insecurity experience scale. Report 03-00–19. Pretoria: Statistics South Africa. http://www.statssa.gov.za/publications/Report-03-00-19/Report-03-00-192020.pdf (accessed October 2023).
- 47. Popkin BM, Barquera S, Corvalan C et al. (2021) Towards unified and impactful policies to reduce ultra-processed food consumption and promote healthier eating. Lancet Diabetes Endocrinol. 9, 462–470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Haggblade S, Duodu KG, Kabasa JD et al. (2016) Emerging early actions to bend the curve in Sub-Saharan Africa’s nutrition transition. Food Nutr Bull 37, 219–241. [DOI] [PubMed] [Google Scholar]
- 49. Frank T, Thow AM, Ng SW et al. (2021) A fit-for-purpose nutrient profiling model to underpin food and nutrition policies in South Africa. Nutrients 13, 1–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Odunitan-Wayas FA, Okop KJ, Dover RVH et al. (2021) Food purchasing behaviour of shoppers from different South African socio-economic communities: results from grocery receipts, intercept surveys and in-supermarkets audits. Public Health Nutr. 24, 665–676. [DOI] [PubMed] [Google Scholar]
- 51. Bopape M, Taillie LS, Frank T et al. (2021) South African consumers’ perceptions of front-of-package warning labels on unhealthy foods and drinks. PLoS One 16, e0257626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Hofman KJ, Stacey N, Swart EC et al. (2021) South Africa’s health promotion levy: excise tax findings and equity potential. Obes Rev 22, 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Willett W (2012) Nutritional Epidemiology, 3rd ed. Oxford: University Press. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Frank et al. supplementary material