Abstract
Background
Manipulation and mobilisation are commonly used to treat neck pain. This is an update of a Cochrane review first published in 2003, and previously updated in 2010.
Objectives
To assess the effects of manipulation or mobilisation alone compared wiith those of an inactive control or another active treatment on pain, function, disability, patient satisfaction, quality of life and global perceived effect in adults experiencing neck pain with or without radicular symptoms and cervicogenic headache (CGH) at immediate‐ to long‐term follow‐up. When appropriate, to assess the influence of treatment characteristics (i.e. technique, dosage), methodological quality, symptom duration and subtypes of neck disorder on treatment outcomes.
Search methods
Review authors searched the following computerised databases to November 2014 to identify additional studies: the Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE, EMBASE and the Cumulative Index to Nursing and Allied Health Literature (CINAHL). We also searched ClinicalTrials.gov, checked references, searched citations and contacted study authors to find relevant studies. We updated this search in June 2015, but these results have not yet been incorporated.
Selection criteria
Randomised controlled trials (RCTs) undertaken to assess whether manipulation or mobilisation improves clinical outcomes for adults with acute/subacute/chronic neck pain.
Data collection and analysis
Two review authors independently selected studies, abstracted data, assessed risk of bias and applied Grades of Recommendation, Assessment, Development and Evaluation (GRADE) methods (very low, low, moderate, high quality). We calculated pooled risk ratios (RRs) and standardised mean differences (SMDs).
Main results
We included 51 trials (2920 participants, 18 trials of manipulation/mobilisation versus control; 34 trials of manipulation/mobilisation versus another treatment, 1 trial had two comparisons).
Cervical manipulation versus inactive control:For subacute and chronic neck pain, a single manipulation (three trials, no meta‐analysis, 154 participants, ranged from very low to low quality) relieved pain at immediate‐ but not short‐term follow‐up.
Cervical manipulation versus another active treatment:For acute and chronic neck pain, multiple sessions of cervical manipulation (two trials, 446 participants, ranged from moderate to high quality) produced similar changes in pain, function, quality of life (QoL), global perceived effect (GPE) and patient satisfaction when compared with multiple sessions of cervical mobilisation at immediate‐, short‐ and intermediate‐term follow‐up. For acute and subacute neck pain, multiple sessions of cervical manipulation were more effective than certain medications in improving pain and function at immediate‐ (one trial, 182 participants, moderate quality) and long‐term follow‐up (one trial, 181 participants, moderate quality). These findings are consistent for function at intermediate‐term follow‐up (one trial, 182 participants, moderate quality). For chronic CGH, multiple sessions of cervical manipulation (two trials, 125 participants, low quality) may be more effective than massage in improving pain and function at short/intermediate‐term follow‐up. Multiple sessions of cervical manipulation (one trial, 65 participants, very low quality) may be favoured over transcutaneous electrical nerve stimulation (TENS) for pain reduction at short‐term follow‐up. For acute neck pain, multiple sessions of cervical manipulation (one trial, 20 participants, very low quality) may be more effective than thoracic manipulation in improving pain and function at short/intermediate‐term follow‐up.
Thoracic manipulation versus inactive control: Three trials (150 participants) using a single session were assessed at immediate‐, short‐ and intermediate‐term follow‐up. At short‐term follow‐up, manipulation improved pain in participants with acute and subacute neck pain (five trials, 346 participants, moderate quality, pooled SMD ‐1.26, 95% confidence interval (CI) ‐1.86 to ‐0.66) and improved function (four trials, 258 participants, moderate quality, pooled SMD ‐1.40, 95% CI ‐2.24 to ‐0.55) in participants with acute and chronic neck pain. A funnel plot of these data suggests publication bias. These findings were consistent at intermediate follow‐up for pain/function/quality of life (one trial, 111 participants, low quality).
Thoracic manipulation versus another active treatment: No studies provided sufficient data for statistical analyses. A single session of thoracic manipulation (one trial, 100 participants, moderate quality) was comparable with thoracic mobilisation for pain relief at immediate‐term follow‐up for chronic neck pain.
Mobilisation versus inactive control: Mobilisation as a stand‐alone intervention (two trials, 57 participants, ranged from very low to low quality) may not reduce pain more than an inactive control.
Mobilisation versus another active treatment:For acute and subacute neck pain, anterior‐posterior mobilisation (one trial, 95 participants, very low quality) may favour pain reduction over rotatory or transverse mobilisations at immediate‐term follow‐up. For chronic CGH with temporomandibular joint (TMJ) dysfunction, multiple sessions of TMJ manual therapy (one trial, 38 participants, very low quality) may be more effective than cervical mobilisation in improving pain/function at immediate‐ and intermediate‐term follow‐up. For subacute and chronic neck pain, cervical mobilisation alone (four trials, 165 participants, ranged from low to very low quality) may not be different from ultrasound, TENS, acupuncture and massage in improving pain, function, QoL and participant satisfaction at immediate‐ and intermediate‐term follow‐up. Additionally, combining laser with manipulation may be superior to using manipulation or laser alone (one trial, 56 participants, very low quality).
Authors' conclusions
Although support can be found for use of thoracic manipulation versus control for neck pain, function and QoL, results for cervical manipulation and mobilisation versus control are few and diverse. Publication bias cannot be ruled out. Research designed to protect against various biases is needed.
Findings suggest that manipulation and mobilisation present similar results for every outcome at immediate/short/intermediate‐term follow‐up. Multiple cervical manipulation sessions may provide better pain relief and functional improvement than certain medications at immediate/intermediate/long‐term follow‐up. Since the risk of rare but serious adverse events for manipulation exists, further high‐quality research focusing on mobilisation and comparing mobilisation or manipulation versus other treatment options is needed to guide clinicians in their optimal treatment choices.
Keywords: Humans; Acute Pain; Acute Pain/rehabilitation; Chronic Pain; Chronic Pain/rehabilitation; Manipulation, Orthopedic; Manipulation, Orthopedic/adverse effects; Manipulation, Orthopedic/methods; Massage; Neck; Neck Pain; Neck Pain/rehabilitation; Quality of Life; Randomized Controlled Trials as Topic; Recovery of Function; Thorax; Transcutaneous Electric Nerve Stimulation
Plain language summary
Manipulation and mobilisation for neck disorders
Review question
This update assessed the effect of manipulation or mobilisation alone compared with a control or another treatment on pain, function, disability, patient satisfaction, quality of life and global perceived effect in adults experiencing neck pain with or without arm symptoms and headache at immediate‐ to long‐term follow‐up.
Background
Neck pain can cause varying levels of disability for the affected individual and is a common musculoskeletal complaint. Neck pain can be accompanied by pain radiating down the arms (radiculopathy) or by headache (cervicogenic headache). Manipulation (adjustments to the spine) and mobilisation (movement imposed on joints and muscles) can be used alone or in combination with other physiotherapies to treat neck pain.
Study characteristics
This updated review includes 51 trials: 18 trials contrasted manipulation or mobilisation against no treatment or pretend treatment; 34 trials compared manipulation or mobilisation against another treatment (electrotherapy, exercise, medication) and various techniques or dosages. [Note one trial included two comparison groups].
Key results
Although other reviews focusing on adverse events suggest that mobilisation is safe and manipulation may result in rare but serious side effects such as stroke, disc herniation or serious neurological deficits, our review noted temporary and benign side effects with both approaches; more than half of the included trials did not report on adverse effects.
• Manipulation or mobilisation versus inactive treatment: For subacute/chronic neck pain, a single manipulation produced temporary pain relief. However, conflicting evidence was found at short‐term follow‐up for pain reduction with multiple sessions. At short‐term and intermediate‐term follow‐up, multiple sessions of thoracic manipulation were favoured for pain reduction among participants with acute/subacute neck pain, and for functional improvement among those with acute to chronic neck pain. No additional pain relief was reported when thoracic mobilisation was used.
• Manipulation or mobilisation versus another active treatment: Cervical manipulation produced changes in pain, function, quality of life, global perceived effect and patient satisfaction that were comparable with those attained with cervical mobilisation up to intermediate‐term follow‐up for patients with neck pain of any duration. Cervical manipulation for acute/subacute neck pain was more effective than varied combinations of analgesics, muscle relaxants and non‐steroidal anti‐inflammatory drugs for improving pain and function at up to long‐term follow‐up. For chronic cervicogenic headache, cervical manipulation provided greater benefit than light massage in improving pain and function at short‐term and intermediate‐term follow‐up. For chronic CGH, cervical manipulation may be superior to transcutaneous electrical nerve stimulation (TENS) in improving pain at short‐term follow‐up. For acute neck pain, cervical manipulation may be more effective than thoracic manipulation in improving pain and function up to intermediate‐term follow‐up. Finally, for subacute and chronic neck pain, cervical mobilisation appeared similar to pulsed ultrasound, TENS, acupuncture and massage in improving pain, function, quality of life and patient satisfaction up to intermediate‐term follow‐up. However, combining laser with manipulation may be superior to using manipulation or laser alone.
Quality of the evidence
No high‐quality evidence was found, so uncertainty about the effectiveness of mobilisation or manipulation for neck pain remains. Future research is likely to have an important impact on the effect estimate. Authors of this review encountered many challenges, for example, the number of participants in most trials was small, 80% (41/51) of the included studies were of low or very low quality and evidence on the optimum dosage requirement was limited.
Summary of findings
Summary of findings for the main comparison. Manipulation (cervical) compared with oral medicine for acute/subacute neck pain.
| Manipulation (cervical) compared with oral medicine for acute/subacute neck pain | ||||
|
Patient or population: patients with acute and subacute neck pain Settings: outpatient clinics, ambulatory care services Intervention: manipulation of cervical region ‐ multiple sessions Comparison: oral medicine ‐ varied combinations of non‐steroidal anti‐inflammatory drugs (NSAIDs), analgesics, opioid analgesics and muscle relaxants | ||||
| Outcomes | Relative effect (95% CI) | Number of participants (studies) | Quality of the evidence (GRADE) | Comments |
| PAIN | ||||
| Acute and subacute neck pain Intermediate‐term follow‐up |
SMD ‐0.21 (‐0.5 to 0.08) |
182 (1 trial; Bronfort 2012) | ⊕⊕⊕⊝ Moderatea |
No significant differences between groups |
| Acute and subacute neck pain Long‐term follow‐up |
SMD ‐0.32 (‐0.61 to ‐0.02) |
181 (1 trial; Bronfort 2012) | ⊕⊕⊕⊝ Moderatea |
Pain reduction favouring manipulation over medication |
| FUNCTION | ||||
| Acute and subacute neck pain Intermediate‐term follow‐up |
SMD ‐0.30 (‐0.59 to ‐0.00) |
182 (1 trial; Bronfort 2012) | ⊕⊕⊕⊝ Moderatea |
Functional improvement favouring manipulation over medication |
| Acute and subacute neck pain Long‐term follow‐up |
SMD ‐0.11 (‐0.40 to 0.18) |
181 (1 trial; Bronfort 2012) | ⊕⊕⊕⊝ Moderatea |
No significant difference between groups |
| PARTICIPANT SATISFACTION | ||||
| Acute and subacute neck pain Long‐term follow‐up |
Not estimable | 182 (1 trial; Bronfort 2012) | ⊕⊕⊕⊝ Moderatea |
Manipulation favoured over medication |
| QUALITY OF LIFE | ||||
| Acute and subacute neck pain Intermediate‐term follow‐up |
SMD 0.22 (‐0.07 to 0.51) |
181 (1 trial; Bronfort 2012) | ⊕⊕⊕⊝ Moderatea |
No significant differences between groups |
| Acute and subacute neck pain Long‐term follow‐up |
SMD: 0.19 (‐0.10 to 0.49) | 181 (1 trial; Bronfort 2012) | ⊕⊕⊕⊝ Moderatea |
No significant differences between groups |
| Moderate‐quality evidence suggests that multiple sessions of cervical manipulation are more effective than medication (analgesics and non‐steroidal anti‐inflammatory drugs (NSAIDs)) for improving pain at immediate‐term and long‐term follow‐up (1 trial; 181 participants); function at intermediate term and satisfaction over the long term. Quality of life was similar between groups (1 trial, 182 participants) at intermediate‐ and long‐term follow‐up. | ||||
| GRADE Working Group grades of evidence. High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||
aIndirectness: ‐1; a second independent trial is needed to clarify emerging data.
Summary of findings 2. Manipulation (thoracic) compared with inactive control for neck pain.
| Manipulation (thoracic) compared with inactive control for neck pain | ||||
|
Patient or population: patients with acute, subacute and chronic neck pain Settings: outpatient clinics, ambulatory care services Intervention: manipulation of thoracic region ‐ multiple sessions Comparison: inactive control | ||||
| Outcomes | Relative effect (95% CI) | Number of participants (studies) | Quality of the evidence (GRADE) | Comments |
| PAIN | ||||
| Acute and subacute neck pain Short‐term follow‐up |
SMD pooled ‐1.46 (‐2.20 to ‐0.71) |
242
(4 trials; Fernandez 2004 JWRD; Fernandez 2009; Gonzalez‐Iglesias 2009 JO; Masaracchio 2013) |
⊕⊕⊕⊝ Moderatea |
Favoured treatment; NNTB: 4 to 7; magnitude of effect: medium |
| Chronic neck pain Intermediate‐term follow‐up |
SMD ‐0.64 (‐1.04 to ‐0.25) |
111 (1 trial; Cheung Lau 2011) | ⊕⊕⊝⊝ Lowb,c |
Favoured treatment; NNTB 4; magnitude of effect: small |
| FUNCTION | ||||
| Acute and subacute neck pain Short‐term follow‐up |
SMD pooled ‐1.73 (‐2.68 to ‐0.78) |
258 (3 trials; Gonzalez‐Iglesias 2009 JO; Gonzalez‐Iglesias 2009 MT; Masaracchio 2013) | ⊕⊕⊕⊝ Moderatea |
Favoured treatment; NNTB 4 to 5; magnitude of effect: medium |
| Chronic neck pain Short‐term follow‐up |
SMD ‐0.50 (‐0.89 to ‐0.10) |
111 (1 trial; Cheung Lau 2011) | ⊕⊕⊝⊝ Lowb,c |
Favoured treatment; NNTB 5; magnitude of effect: small |
| Chronic neck pain Intermediate‐term follow‐up |
SMD ‐0.38 (‐0.77 to 0.01) |
111 (1 trial; Cheung Lau 2011) |
⊕⊕⊝⊝ Lowb,c |
Favoured treatment; NNTB 5; magnitude of effect: small |
| QUALITY OF LIFE (QoL) | ||||
| Chronic neck pain Short‐term follow‐up |
SMD ‐0.82 (‐1.23 to ‐0.42) |
111 (1 trial; Cheung Lau 2011) | ⊕⊕⊝⊝ Lowb,c |
Favoured treatment |
| Chronic neck pain Intermediate‐term follow‐up |
SMD ‐0.61 (‐1.01 to ‐0.22) |
111 (1 trial; Cheung Lau 2011) | ⊕⊕⊝⊝ Lowc |
Favoured treatment |
| Seven trials (428 participants) using multiple sessions of thoracic manipulation for acute to chronic neck pain were assessed at 3 time intervals. At short‐term follow‐up, moderate‐quality evidence favoured thoracic manipulation for pain reduction among participants with acute/subacute neck pain, and with acute to chronic neck pain, it improved function. These findings were consistent but small at intermediate follow‐up for pain, function and quality of life (low‐quality evidence). | ||||
| GRADE Working Group grades of evidence. High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||
bIndirectness: ‐1, immediate post‐treatment data have limited clinical relevance; single trials with only immediate‐ and short‐term follow‐up are downgraded (ceiling effect) because future research is likely to have an important impact on the direction of the reported effect, and a second independent trial is needed to clarify emerging short‐term data.
cImprecision: ‐1, small sample size.
aInconsistency: P value = 0.002; I² = 84%; sensitivity analysis: Statistical differences led us to explore heterogeneity by the following PICO factors: P: about the same; I: about the same; C: about the same; O: for pain, VAS, NPRS; for disability, NPQ, NDI; RoB: most often low RoB but when the trial of high RoB is removed, pooled SMD increases to ‐2.18 (‐2.71 to ‐1.65) for pain, but these data were derived from trials conducted in the same lab.
Summary of findings 3. Manipulation compared with mobilisation for neck pain.
| Manipulation compared with mobilisation for neck pain | ||||
|
Patient or population: patients with acute, subacute and chronic neck pain Settings: ambulatory care or outpatient clinic Intervention: manipulation of cervical region ‐ multiple sessions Comparison: mobilisation | ||||
| Outcomes | Relative effect (95% CI) | Number of participants (studies) | Quality of the evidence (GRADE) | Comments |
| PAIN | ||||
| Acute, subacute and chronic neck pain Intermediate‐term follow‐up |
MD pooled ‐0.07 (‐0.72 to 0.59) |
446 (2 trials; Hurwitz 2002, Leaver 2010) | ⊕⊕⊕⊝ Moderatea |
No significant differences between groups |
| FUNCTION AND DISABILITY | ||||
| Acute and subacute neck pain Short‐term follow‐up |
SMD: ‐0.06 (‐0.35 to 0.24) |
176 (1 trial; Leaver 2010) | ⊕⊕⊕⊝ Moderateb |
No significant differences between groups |
| Acute, subacute and chronic neck pain Intermediate‐term follow‐up |
SMD pooled: 0.10 (‐0.18 to 0.37) |
446 (2 trials; Hurwitz 2002; Leaver 2010) | ⊕⊕⊕⊕ High |
No significant differences between groups |
| PARTICIPANT SATISFACTION | ||||
| Subacute and chronic neck pain Short‐term follow‐up |
SMD: ‐0.02 (‐0.21 to 0.24) |
269 (1 trial; Hurwitz 2002) | ⊕⊕⊕⊝ Moderateb |
No significant differences between groups |
| GLOBAL PERCEIVED EFFECT | ||||
| Acute and subacute neck pain Intermediate‐term follow‐up |
SMD: ‐0.06 (‐0.35 to 0.24) | 177 (1 trial; Leaver 2010) | ⊕⊕⊕⊝ Moderateb |
No significant differences between groups |
| QUALITY OF LIFE | ||||
| Acute and subacute neck pain Short‐term follow‐up |
SMD: 0.08 (‐0.21 to 0.38) |
176 (1 trial; Leaver 2010) | ⊕⊕⊕⊝ Moderateb |
No significant differences between groups |
| Acute and subacute neck pain Intermediate‐term follow‐up |
SMD: ‐0.06 (‐0.35 to 0.24) |
177 (1 trial; Leaver 2010) | ⊕⊕⊕⊝ Moderateb |
No significant differences between groups |
| Moderate‐ to high‐quality evidence (2 trials, 446 participants) suggests that multiple sessions of cervical manipulation produced similar changes in pain, function, quality of life, global perceived effect and patient satisfaction when compared with multiple sessions of cervical mobilisation at immediate‐, short‐ and intermediate‐term follow‐up. | ||||
| GRADE Working Group grades of evidence. High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||
aInconsistency: ‐1.
bIndirectness: ‐1.
Summary of findings 4. Manipulation compared with exercise for neck pain.
| Manipulation compared with exercise for neck pain | ||||
|
Patient or population: patients with acute and subacute neck pain Settings: ambulatory care or outpatient clinic setting Intervention: manipulation of cervical region Comparison: exercise | ||||
| Outcomes | Relative effect (95% CI) | Number of participants (studies) | Quality of the evidence (GRADE) | Comments |
| PAIN | ||||
| Acute and subacute neck pain Intermediate‐term follow‐up |
SMD: ‐0.16 (‐0.45 to 0.13) |
182 (1 trial; Bronfort 2012) | ⊕⊕⊕⊝ Moderatea |
No significant differences between groups |
| Acute and subacute neck pain Long‐term follow‐up |
SMD: 0.06 (‐0.23 to 0.35) |
182 (1 trial; Bronfort 2012) | ⊕⊕⊕⊝ Moderatea |
No significant differences between groups |
| FUNCTION | ||||
| Acute and subacute neck pain Intermediate‐term follow‐up |
SMD: ‐0.01 (‐0.30 to 0.28) |
182 (1 trial; Bronfort 2012) | ⊕⊕⊕⊝ Moderatea |
No significant differences between groups |
| Acute and subacute neck pain Long‐term follow‐up |
SMD: ‐0.02 (‐0.31 to 0.27) |
182 (1 trial; Bronfort 2012) | ⊕⊕⊕⊝ Moderatea |
No significant differences between groups |
| PARTICIPANT SATISFACTION | ||||
| Acute and subacute neck pain Long‐term follow‐up |
Not estimable | 182 (1 trial; Bronfort 2012) | ⊕⊕⊕⊝ Moderatea |
Improvement in participant satisfaction for manipulation over exercise |
| GLOBAL PERCEIVED EFFECT | ||||
| Acute and subacute neck pain Immediate post‐treatment follow‐up |
Not estimable | 182 (1 trial; Bronfort 2012) |
⊕⊕⊕⊝ Moderatea |
No significant differences between groups |
| QUALITY OF LIFE | ||||
| Acute and subacute neck pain Intermediate‐term follow‐up |
SMD: ‐0.05 (‐0.35 to 0.24) | 182 (1 trial; Bronfort 2012) | ⊕⊕⊕⊝ Moderatea |
No significant differences between groups |
| Acute and subacute neck pain Long‐term follow‐up |
SMD: 0.0 (‐0.29 to 0.29) | 182 (1 trial; Bronfort 2012) | ⊕⊕⊕⊝ Moderatea |
No significant differences between groups |
| Moderate‐quality evidence suggests no differences in pain, function, global perceived effect and quality of life when multiple sessions of cervical manipulation are compared with exercise at immediate‐, intermediate‐ and long‐term follow‐up. Moderate‐quality evidence indicates that use of cervical manipulation led to greater participant satisfaction when compared with an exercise programme at long‐term follow‐up. | ||||
| GRADE Working Group grades of evidence. High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||
aIndirectness: ‐1.
Summary of findings 5. High dose of manipulation compared with low dose of manipulation for chronic neck pain.
| High dose of manipulation compared with low dose of manipulation for chronic neck pain | ||||
|
Patient or population: patients with chronic neck pain with cervicogenic headache (CGH) Settings: ambulatory care or outpatient clinic setting Intervention: manipulation of cervical region Comparison: high dose vs low dose | ||||
| Outcomes | Relative effect (95% CI) | Number of participants (studies) | Quality of the evidence (GRADE) | Comments |
| PAIN | ||||
| Chronic neck pain and CGH Intermediate‐term follow‐up |
SMD pooled: ‐0.40 (‐0.96 to 0.16) |
50 (2 trials; Haas 2004; Haas 2010) | ⊕⊕⊕⊝ Moderatea |
Two trials showed no significant differences between groups |
| FUNCTION | ||||
| Chronic neck pain and CGH Intermediate‐term follow‐up |
SMD pooled: ‐0.61 (‐1.38 to 0.17) |
50 (2 trials; Haas 2004; Haas 2010) | ⊕⊕⊕⊝ Moderatea |
Two trials showed no significant differences between groups |
| Moderate‐quality evidence shows that high‐dose (12 to 18 sessions) contrasted against low‐dose (3 to 8 sessions) cervical manipulation produced similar changes in pain and function at intermediate‐term follow‐up for individuals with chronic neck pain with cervicogenic headache. | ||||
| GRADE Working Group grades of evidence. High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||
aImprecision: ‐1.
Background
Description of the condition
Neck disorders are common, disabling to various degrees and costly (Hogg‐Johnson 2008). Most people can expect to have some degree of neck pain within their lifetime. Neck pain with or without symptoms that radiate to the arms or head may involve a variety of pathologies in one or several neurovascular, soft tissue and musculoskeletal structures such as nerves, ganglia, nerve roots, uncovertebral joints, intervertebral joints, discs, bones, periosteum, muscle and ligaments. We included in this review neck pain with cervicogenic headache ‐ a pain that emanates from the neck and suboccipital region and radiates to the forehead, orbital region, temples, vertex or ears and is aggravated by specific neck movements or sustained neck postures.
When examining new episodes of neck pain, we looked at the general population, the workforce and motor vehicle accident (MVA) victims. Every year, an episode of neck pain occurs in 15% to 20% of the general population, in 15% to 60% of the workforce and in 10% to 14% of those involved in traffic collisions (Guzman 2008). Prevalence of neck pain varies from 12% to 72% in the general population and from 27% to 48% among workers (Haldeman 2008). The annual prevalence of activity limitations related to neck pain has been reported as 11% in the UK and 14% in Canada (Côté, 2008). Societal and personal burden from persisting symptoms of postwhiplash injury has been described in up to 50% of those attending an emergency department (Kongsted 2007). Long‐term consequences for individuals and their spouses as detailed by Jennum 2013 include reduced quality of life, mood, ability to cope, social participation, employment rates and job income.
Direct costs attributable to visits to healthcare providers, sick leave and related loss of productive capacity (Borghouts 1998; Côté 2008; Linton 1998; Skargren 1998) are substantive. Mean inflation‐adjusted annual expenditures on medical care for people with back and neck conditions increased from $487 to $950 USD from 1999 to 2008 (Davis 2012). Work‐related claims for neck injury submitted to a Canadian Workers Compensation Board accounted for 5% of all lost time at work (Côté 2008). Indirect costs related to disease‐related work disability or premature mortality were significantly higher in people with neck injury and their spouses when compared with matched controls in a Danish study (Jennum 2013).
Description of the intervention
Manipulation and mobilisation are commonly used treatments for neck pain and may be performed by physical therapists, chiropractors, traditional bone setters, osteopaths, medical doctors and massage therapists. Manipulation consists of a localised force of high velocity and low amplitude directed at specific spinal segments (Basmajian 1993; Grieve 1988). Mobilisations use low‐grade/velocity, small‐ or large‐amplitude passive movement techniques or neuromuscular techniques within the patient's range of motion and within the patient's control (Basmajian 1993; Butler 2000; Grieve 1988). Neuromuscular mobilisation techniques employ the muscular efforts of individuals against a specific force applied by the clinician to more effectively mobilise a joint(s) and related tissues.
Description of the comparison
The methods most commonly compared in trials are inactive controls [placebo (e.g. sham/mock mobilisation or other sham treatment such as sham transcutaneous electrical nerve stimulation (TENS); adjunct treatment (e.g. mobilisation plus a treatment such as ultrasound versus same treatment); and wait list/no treatment)] and other active treatments [one intervention versus another intervention (e.g. manipulation versus exercise); one treatment technique versus another (e.g. rotatory break versus lateral break manipulation); and one dose of treatment versus another dose (e.g. three weeks at nine sessions of manipulation versus four weeks at 12 sessions)].
How the intervention might work
Spinal manipulation or mobilisation appear to have three main proposed underpinning physiological mechanisms. The underlying mechanisms are complex, multifactorial and poorly understood; unravelling these mechanisms continues to have important implications for rehabilitation. First, neurophysiological effects, including analgesic, motor and sympathetic nervous system effects, have been demonstrated (Bialosky 2009; Karason 2003; Perry 2008; Vincenzino 1996); second, mechanical effects, including transient/short‐term to permanent change in length of connective tissue and biomechanical dysfunction, have been revealed (Bialosky 2009; Calloca 2006; Fritz 2011; Martinez‐Segura 2006; Souvlis 2004); and finally, expectations or psychological factors associated with 'manual touch' may produce a placebo effect. The mechanical force of spinal manipulation triggers a chain of neurophysiological reactions that are thought to be the reason for the outcomes seen with spinal manipulation (Bialosky 2009). Proposed neurophysiological effects include pain reduction through inhibition of nociceptors, dorsal horn and descending pathways of the spinal cord (Bialosky 2009; Haavik 2012; Pickar 2002). A manipulation force can stimulate peripheral afferents, altering central mediated/supraspinal input and enhancing motoneuron excitability (Bialosky 2009; Schmid 2008). Increased muscle recruitment after manipulation has impacted spinal stiffness and muscle activity (Fritz 2011). It is difficult to assess to what degree 'hands‐on effects', attention, assessment techniques, other forms of feedback and interaction and communication between the manual therapist and the patient are 'unique' traits of those who provide manual therapy. We acknowledge that these effects may play some role in manual treatment methods.
Why it is important to do this review
Since our 2010 publication (Gross 2010), numerous systematic reviews on similar topics have been published (Boyles 2011; Chaibi 2012; Cross 2011; Furlan 2012; Huisman 2013; Lin 2012; Millan 2012; Posadzki 2011; Racicki 2013; Rodine 2012; Shaw 2010; Thoomes 2013; Vincent 2013; Walser 2009). High‐quality conclusions pertaining to effectiveness or superiority of manipulation or mobilisation over other treatment modalities have NOT been reported. Most evidence pertaining to subacute or chronic neck pain is of moderate to very low quality (Cross 2011; Furlan 2012; Gross 2010), and almost no evidence is available on manipulation or mobilisation as a single stand‐alone therapy for both acute neck disorders (Shaw 2010) or radiculopathy (Boyles 2011; Rodine 2012; Thoomes 2013). An update of this Cochrane systematic review is justified to strengthen our confidence in the evidence.
Objectives
To assess effects of manipulation or mobilisation alone compared wiith those of an inactive control or another active treatment on pain, function, disability, patient satisfaction, quality of life and global perceived effect in adults experiencing neck pain with or without radicular symptoms and cervicogenic headache at immediate‐ to long‐term follow‐up. When appropriate, to assess the influence of treatment characteristics (i.e. technique, dosage), methodological quality, symptom duration and subtypes of neck disorder on treatment outcomes.
Methods
Criteria for considering studies for this review
Types of studies
We included published and unpublished randomised controlled trials (RCTs) or quasi‐RCTs (QRCTs)in full‐text or abstract form. A QRCT uses methods of allocation that are subject to bias in assignment, such as odd‐even numbers, days of the week or patient record or social security number. We applied no restrictions to the methodological quality of RCTs.
Types of participants
Participants were adults (≥ 18 years) with the following.
Neck pain without radicular findings, including neck pain without specific cause, whiplash‐associated disorder (WAD) category I and II (Guzman 2008; Spitzer 1987; Spitzer 1995), myofascial pain syndrome and neck pain associated with degenerative changes (Schumacher 1993).
Cervicogenic headache (Olesen 1988; Olesen 1997; Sjaastad 1990).
Neck disorders with radicular findings (Schumacher 1993), including degenerative joint or disc disease with spinal stenosis, spondylolisthesis or discogenic radiculopathy; WAD category III (Spitzer 1987; Spitzer 1995).
We defined symptom duration as acute (< 30 days), subacute (30 days to 90 days) or chronic (> 90 days).
We excluded studies if they investigated neck disorders with the following specific causes.
Definite or possible long tract signs (e.g. myelopathies).
Neck pain caused by other pathological entities (Schumacher 1993).
Headache not of cervical origin but associated with the neck.
Co‐existing headache when neck pain was not dominant, or when the headache was not provoked by neck movements or sustained neck postures.
'Mixed' headache, which includes more than one headache classification.
Types of interventions
We included studies using manipulation or mobilisation techniques. Although typically applied to the cervical region, they could be applied to other body regions; the guiding principle was to include a mobilisation or manipulation intervention provided with the intention to treat neck pain. Manipulation involves a localised force of high velocity and low amplitude directed at specific spinal segments. Mobilisations use low‐grade/velocity, small‐ or large‐amplitude passive movement techniques or neuromuscular techniques within the patient's range of motion and within the patient's control. In the included studies, investigators might use these techniques alone or in conjunction with other treatment agents, for example, mobilisation plus ultrasound versus ultrasound. All studies consisted of comparison with an inactive control or with another active treatment as follows.
Inactive control
Placebo, for example, sham/mock mobilisation or other sham treatment (e.g. sham TENS).
Adjunct treatment, for example, mobilisation plus a treatment (e.g. ultrasound) versus the same treatment (e.g. ultrasound).
Wait list or no treatment.
Active treatment for comparison
Manipulation or mobilisation versus another intervention (e.g. manipulation versus exercise).
One technique of manipulation or mobilisation versus another (e.g. rotatory break versus lateral break manipulation).
One dose of manipulation or mobilisation versus another dose (e.g. 3 weeks at 9 sessions manipulation versus 4 weeks at 12 sessions).
Types of outcome measures
Primary outcomes
Primary outcomes of interest included the following.
Pain relief.
Disability including, but not limited to, self report disability measures such as the Neck Disability Index (NDI), activities of daily living, return to work, sick leave and function.
Secondary outcomes
Secondary outcomes included the following.
Global perceived effect.
Patient satisfaction.
Quality of life.
We set no restrictions on the types of tools used to measure these outcomes, as no universally accepted tools are available, although we found that investigators in several studies did use validated tools. Function and disability could be measured using self report measures or observer‐based physical performance tests (Beattie 2001; Finch 2002). Measures of physical performance require testing the individual's ability to execute a simple activity in a standardised environment using a standardised test and scoring procedure; these measures are concerned with testing a co‐ordinated set of functions needed for purposeful activity (i.e. reaching, walking, driving). Although moderate correlation between self report scales and physical performance tests can be found in the low back literature, it remains unclear whether one is superior to the other (Lee 2001), and in the neck literature, this relationship remains unclear. We excluded tests used during a standard physical examination, such as inspection, range of motion, strength, palpation, provocation, muscular stability, neurological tests and cervical proprioception. We extracted data on adverse effects and costs of treatment. The duration of follow‐up was defined as follows.
Immediately post treatment (within one day).
Short‐term follow‐up (closest to four weeks; one day to four weeks).
Intermediate‐term follow‐up (closest to six months; longer than four weeks to six months).
Long‐term follow‐up (closest to 12 months; longer than six months to 12 months).
Search methods for identification of studies
A research librarian searched bibliographic databases, without language restrictions, for medical, chiropractic and allied health literature. All databases were originally searched from their inception. Subject headings (MeSH) and key words included anatomical terms, disorder or syndrome terms, treatment terms and methodological terms consistent with those advised by the Cochrane Back Review Group.
Electronic searches
We searched the following databases from their start to the dates provided:
Cochrane Central Register of Controlled Trials (CENTRAL) (Ovid, November 2014; includes the Back Review Group Trials Register).
MEDLINE (Ovid, 1950 to November 2014 week 4).
EMBASE (Ovid, 1980 to November 2014).
Cumulative Index to Nursing and Allied Health Literature (CINAHL) (EBSCO, 1982 to November 2014).
ClinicalTrials.gov (November 2014).
Manual Alternative and Natural Therapy Index System (MANTIS, Ovid, 1980 to May 2014).
Index to Chiropractic Literature (ICL) (January 2014).
See Appendix 1 for the search strategies used for CENTRAL, MEDLINE, EMBASE, CINAHL, MANTIS and ICL.
We performed a search update in June 2015. Those results have been added to ‘Studies awaiting classification’ and will be incorporated into the review at the next update.
Searching other resources
We also screened references, personally communicated with identified content experts and checked our own personal files to identify potential references up to November 2014.
Data collection and analysis
Selection of studies
At least two review authors with expertise in medicine, physiotherapy, chiropractic, massage therapy, statistics or clinical epidemiology independently conducted selection at two stages ‐ citation identification (citation posting plus abstract) followed by study selection (full text) ‐ using pre‐piloted forms. The assembled group did not author any of the primary trials. We assessed agreement on study selection using the quadratic weighted Kappa statistic (Kw) and Cicchetti weights (Cicchetti 1976). We consulted a third review author in cases of persisting disagreement.
Data extraction and management
Two review authors independently extracted data on pre‐piloted forms, as per all Cervical Overview Group reviews. We resolved disagreements through consensus. We consulted a neutral third party if consensus was not reached. We contacted study authors to ask for missing information and to clarify data. We used descriptive statistics to provide a summarised description of groups, interventions, outcomes, adverse effects of treatment and costs of care. We extracted data on design (RCT, number analysed/number randomly assigned, intention‐to‐treat analysis, power analysis), participants (disorder subtype, duration of disorder), interventions (treatment characteristics in treatment and comparison groups, dosage/treatment parameters, co‐interventions, treatment schedules, durations of follow‐up) and outcomes (baseline means, end of study means, absolute benefits, reported results, point estimates with 95% confidence intervals (CIs), side effects, costs of care and adverse events). We noted these factors in the Characteristics of included studies table. All results reported were based on the sample size analysed using the 'intention‐to‐treat' principle, in other words, the sample entering the study.
Assessment of risk of bias in included studies
At least two review authors independently assessed risk of bias (Appendix 2; Furlan 2009; Higgins 2011) using pre‐piloted forms. We resolved disagreements through consensus (Graham 2012). The Cervical Overview Group used a calibrated team of assessors, and at least two assessors independently assessed the following characteristics for risk of bias (maximum criteria = 12; low risk of bias = six or more criteria were met versus high risk of bias = five or fewer criteria were met): randomisation; concealment of treatment allocation; blinding of participant, provider and outcome assessor; incomplete data: withdrawal/dropout rate and intention‐to‐treat analysis; selective outcome reporting; and other: similar baseline values, similar co‐interventions, acceptable compliance and similar timing of assessment. We did not exclude studies from further analyses on the basis of results of risk of bias assessments.
Measures of treatment effect
For continuous data, we calculated standardised mean differences with 95% confidence intervals (SMDs; 95% CIs). Standard mean difference was selected over mean difference (MD) because different types of exercises were assessed, and most interventions used different outcome measures and different scales. Mean difference was used for trials reporting the same outcome measure. The Cochrane Back Review Group guidelines (Furlan 2009) were foundational to key estimations of minimum clinically important differences for pain and function/disability. We assumed that the minimum clinically important difference was 10 on a 100‐point pain intensity scale (Cleland 2008; Farrar 2001; Felson 1995; Goldsmith 1993). Similarly, we judged a minimum clinically important difference of 5/50 units, or 10%, to be relevant for the NDI (Stratford 1999); a recent systematic review (MacDermid 2009) reported that the minimal detectable change varied from 5/50 for non‐complicated neck pain to 10/50 for cervical radiculopathy. The clinically important difference varied from 5/50 to 19/50 and was noted to be inconsistent across studies (Cleland 2008; MacDermid 2009). For other outcomes (i.e. global perceived effect and quality of life scales) for which clear guidelines on the size of clinically important effect sizes were lacking, we applied a system commonly used by Cohen 1988: small (0.20), medium (0.50) or large (0.80).
For continuous outcomes reported as medians, we calculated effect sizes (Kendal 1963, page 237).
For dichotomous outcomes, we calculated risk ratios (RRs). A risk ratio less than one represented beneficial treatment. When neither continuous nor dichotomous data were available, we extracted findings and statistical significance as reported by the author(s) of the original study and noted them in the Characteristics of included studies table.
We calculated the number needed to treat for an additional beneficial outcome (NNTB: the number of patients a clinician needs to treat to achieve clinically important improvement in one patient) and treatment advantages (%: clinically important differences or changes in percentage) for primary findings, to give the reader a sense of the magnitude of the treatment effect (Gross 2002a; see Table 6 and Table 7 for operational definition, calculations and results).
1. Calculations for number needed to treat and treatment advantage.
| Term | Definiton |
| Per cent treatment advantage (%) | Calculation of the clinically important difference or change in a per cent scale was estimated as follows. Karlberg 1996 data are used in this example.
The assumption made was that a positive mean/median value is improvement and a negative value is deterioration.
Treatment/Control
Mean/Median; Mean/Median; Mean/Median; Mean/Median
Baseline (SD); Final (SD); Baseline (SD); Final (SD)
54 (23); 31 (10); 56 (1); 55 (20)
% improvement (treatment) equals the difference between the change in the treatment group (23) divided by the treatment baseline (54), which equals 42.6%. % improvement (control) equals the difference between the change in the control group (1) divided by the control baseline (56), which equals 1.8%. Treatment advantage = 42.6% ‐ 1.8% = 40.8% |
| Number needed to treat (NNTB) | For this example, Karlberg 1996 outcomes measured at short‐term follow‐up are used to derive the data. Number needed to treat is the number of patients a clinician needs to treat to achieve a clinically important improvement in 1. If we assume the minimal clinically important difference to be 10% of the baseline mean in the control group, and the control group mean at baseline is 56, then 10% of 56 is 5.6 The effect is baseline ‐ final value; therefore:
Converting these to standard normal values means that:
NNTB = 1 divided by the difference in areas under the normal curve (experimental group ‐ control group):
|
2. NNTB and treatment advantage.
| Author/Comparison | NNTB | Advantage, % |
| PAIN | ||
| Haas 2004: pain | 12 (clinically important pain reduction) at ST | 23 |
| Haas 2010: pain | 4 (clinically important pain reduction) at IT | 29 |
| Cleland 2005 outcome: pain | 5 (clinically important pain reduction) | 29 |
| Cheung Lau 2011: pain | 4 (clinically important pain reduction) | |
| Fernandez 2004a outcome: pain | Unable to calculate because baseline data not reported (study author was unable to provide these data) | |
| Gonzalez‐Iglesias 2009 outcome: pain | 7 (clinically important pain reduction) | 47 |
| Martinez‐Segura 2006, outcome: pain | 2 (clinically important pain reduction) | 54 |
| Massaracchio 2013: pain | 4 (clinically important pain reduction) | |
| von Piekartz 2011: pain | 2 (clinically important pain reduction) at IT | |
| FUNCTION | ||
| Cheung Lau 2011: function | 5 (clinically important functional improvement) at IT | |
| Gonzalez‐Iglesias 2009 outcome: function | 5 (clinically important functional improvement) | 41 |
| Haas 2010: function | 5 (clinically important functional improvement) at ST and IT | ST: 41 IT: 39 |
| Massaracchio 2013: function | 4 (clinically important functional improvement) | |
Dealing with missing data
We contacted the primary authors to request missing outcomes. To facilitate analysis, we used data imputation rules when necessary (Appendix 3).
Assessment of heterogeneity
Before calculating a pooled effect measure using RevMan 2014, we assessed the reasonableness of pooling on clinical grounds (Verbeek 2012). Possible sources of heterogeneity considered were symptom duration (acute versus chronic); subtype of neck pain (e.g. WAD); intervention type (e.g. mobilisation versus manipulation); characteristics of treatment (e.g. dosage, technique); and outcomes (pain relief, measures of function and disability, participant satisfaction, quality of life). We tested statistical heterogeneity between studies by using a random‐effects model. In the absence of heterogeneity (P value > 0.1 and I² > 40%), we combined data across studies as pooled SMDs, MDs or RRs using methods available in RevMan 2014.
Assessment of reporting biases
We used a funnel plot to detect reporting bias.
Data synthesis
We combined data across studies as pooled SMDs, MDs or RRs using methods available in RevMan 2014 after we assessed heterogeneity. We assessed the quality of the body of evidence using the Grading of Recommendations, Assessment, Development and Evaluation (GRADE) approach of The Cochrane Collaboration (Guyatt 2010; Higgins 2011; Appendix 4). Domains that may decrease the quality of the evidence include study design, limitations ‐ risk of bias, consistency of results, directness (generalisability), precision (sufficient data) and reporting biases. We defined high‐quality evidence as reported by RCTs with low risk of bias that provided consistent, direct and precise results for the outcome. We reduced the quality of the evidence by one level for each domain not met..
High quality: Further research is very unlikely to change our confidence in the estimate of effect. Consistent findings among 75% of RCTs with low risk of bias are generalisable to the population in question. Sufficient data, with narrow confidence intervals, are available. No reporting biases are known or suspected. (All domains are met.)
Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. (One domain is not met.)
Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. (Two domains are not met.)
Very low quality: We are very uncertain about the estimate. (Three domains are not met.)
No evidence: We identified no RCTs that measured the outcome.
We considered various factors to place the results into a larger clinical context: temporality, plausibility, strength of association, dose response, adverse events and costs.
Subgroup analysis and investigation of heterogeneity
Although we planned to perform subgroup analyses to assess the influence of three factors: risk of bias (concealment of allocation, blinding of outcome assessor), duration (acute, subacute, chronic) and subtypes of the disorder (non‐specific, WAD, work‐related, degenerative change‐related, radicular findings, cervicogenic headache), we found that this was not possible. We denoted subgroups to descriptively explore the effects of treatment dosage for manipulation alone or mobilisation alone, as meta‐regression was not possible. We consistently denoted trial risk of bias, quality of the evidence and duration of the disorder.
Sensitivity analysis
We did not perform sensitivity analyses on other factors (i.e. characteristics of the intervention examined, the intervention compared and the outcome (time point); arising analysis factors) nor meta‐regression because data in any one category of mobilisation or manipulation were insufficient. However, we did present data according to body region of manipulation or mobilisation.
Results
Description of studies
This update included 26 new trials for manipulation or mobilisation versus inactive control or another active treatment (Aquino 2009; Bronfort 2012; Cheung Lau 2011; Escortell‐Mayor 2011;Fernandez 2009; Gemmell 2010;Gonzalez‐Iglesias 2009 JO; Gonzalez‐Iglesias 2009 MT; Haas 2010;Leaver 2010;Madson 2010;Martel 2011; Martinez‐Segura 2006a; Masaracchio 2013; Puentedura 2011;Ragonese 2009; Saavedra‐Hernandez 2012CR; Saavedra‐Hernández 2012JO;Saayman 2011; Schomacher 2009;Shin 2006;Sillevis 2010; Sterling 2010; von Piekartz 2011; Youssef 2013; Yurkiw 1996).
Results of the search
Figure 1 describes the flow of studies from our previous updates (1822 citation postings) and from this update (1011 + 1004 + 280 citation postings). From 168 references representing 126 RCTs, we selected 51 RCTs (2910/3294 participants analysed/randomly assigned), and four are pending from our most recent update. Manipulation/Mobilisation versus control represented 18 publications for manipulation or mobilisation performed as a single‐modal application; manipulation/mobilisation versus another treatment represented 34 publications for manipulation or mobilisation performed as a single‐modal application and one publication that compared manipulation/mobilisation versus an inactive control and another active treatment (Saayman 2011); data on multi‐modal approaches that included manual therapy were obtained from this report and were presented separately (D'Sylva 2010; Miller 2010).
1.
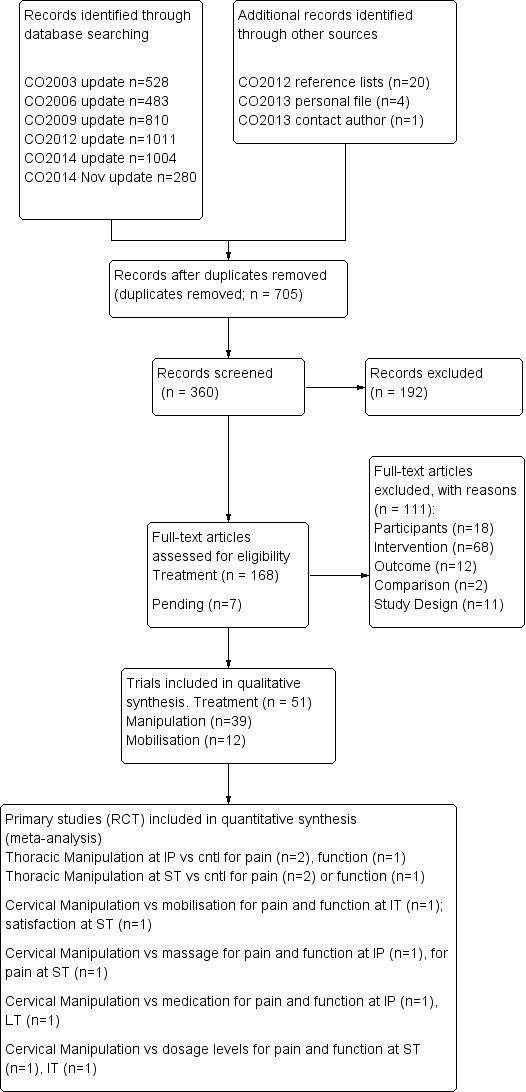
PRISMA diagram for manipulation and mobilisation.
See the reference list for multiple publications per study; the primary trials are depicted here. See Characteristics of included studies for further details on treatment characteristics, co‐interventions, baseline values, absolute benefits, reported results, SMDs, RRs, side effects and costs of care. Agreement between pairs of independent review authors from diverse professional backgrounds for manual therapy was Kw 0.84 (standard error (SE) 0.08).
Included studies
See Characteristics of included studies.
For comparison with various inactive control trials, the following disorder categories emerged.
18 studies included individuals with neck pain without radicular findings: acute (Fernandez 2009; Gonzalez‐Iglesias 2009 JO; Gonzalez‐Iglesias 2009 MT); chronic (Bitterli 1977; Cheung Lau 2011; Cleland 2005; Lin 2013; Martel 2011; Saavedra‐Hernandez 2012CR); mixed (Fernandez 2004 JWRD; Howe 1983; Martinez‐Segura 2006a; Masaracchio 2013; Saayman 2011; Sloop 1982; Sterling 2010); and symptom duration not reported (Krauss 2008; Parkin‐Smith 1998).
13 studies investigated neck pain: acute (Fernandez 2009; Gonzalez‐Iglesias 2009 JO; Gonzalez‐Iglesias 2009 MT); chronic (Cheung Lau 2011; Cleland 2005; Lin 2013; Martel 2011; Saavedra‐Hernandez 2012CR); mixed (Martinez‐Segura 2006a; Masaracchio 2013; Saayman 2011); and symptom duration not reported (Krauss 2008; Parkin‐Smith 1998).
Two investigated whiplash‐associated disorders: mixed (Fernandez 2004 JWRD; Sterling 2010).
Two investigated degenerative changes: chronic (Bitterli 1977); and mixed (Sloop 1982).
Two investigated cervicogenic headache: chronic (Bitterli 1977); and mixed (Howe 1983).
One investigated neck disorders with radicular signs and symptoms: mixed (Howe 1983).
For comparison with active treatment trials, the following disorder categories emerged.
34 studies included a comparison group (see Figure 2) (Aquino 2009; Bronfort 2012; Cassidy 1992; Chen 2007; Coppieters 2003; David 1998; Egwu 2008; Escortell‐Mayor 2011; Gemmell 2010; Giles 1999; Haas 2004; Haas 2010; Hurwitz 2002; Kanlayanaphotporn 2009; Kanlayanaphotporn 2010a; Leaver 2010; Lee 2013; Madson 2010; Muller 2005; Nilsson 1997; Puentedura 2011; Ragonese 2009; Saavedra‐Hernández 2012JO; Saayman 2011; Savolainen 2004; Schomacher 2009; Shin 2006; Sillevis 2010; Strunk 2008; van Schalkwyk 2000; von Piekartz 2011; Wood 2001; Youssef 2013; Yurkiw 1996).
21 investigated neck pain without radicular findings: subacute (Gemmell 2010; Wood 2001; Yurkiw 1996); chronic (Aquino 2009; Escortell‐Mayor 2011; Kanlayanaphotporn 2009; Kanlayanaphotporn 2010a; Madson 2010;Muller 2005; Saavedra‐Hernández 2012JO; Sillevis 2010); mixed (Bronfort 2012; Cassidy 1992; Coppieters 2003; David 1998; Egwu 2008; Leaver 2010;Saayman 2011; Strunk 2008); and symptom duration not reported (Savolainen 2004; van Schalkwyk 2000).
One investigated neck pain with headache: chronic (Nilsson 1997).
Two investigated neck pain with or without radicular symptoms: acute (Puentedura 2011); and symptom duration not reported (Fernandez 2004 JWRD).
2.
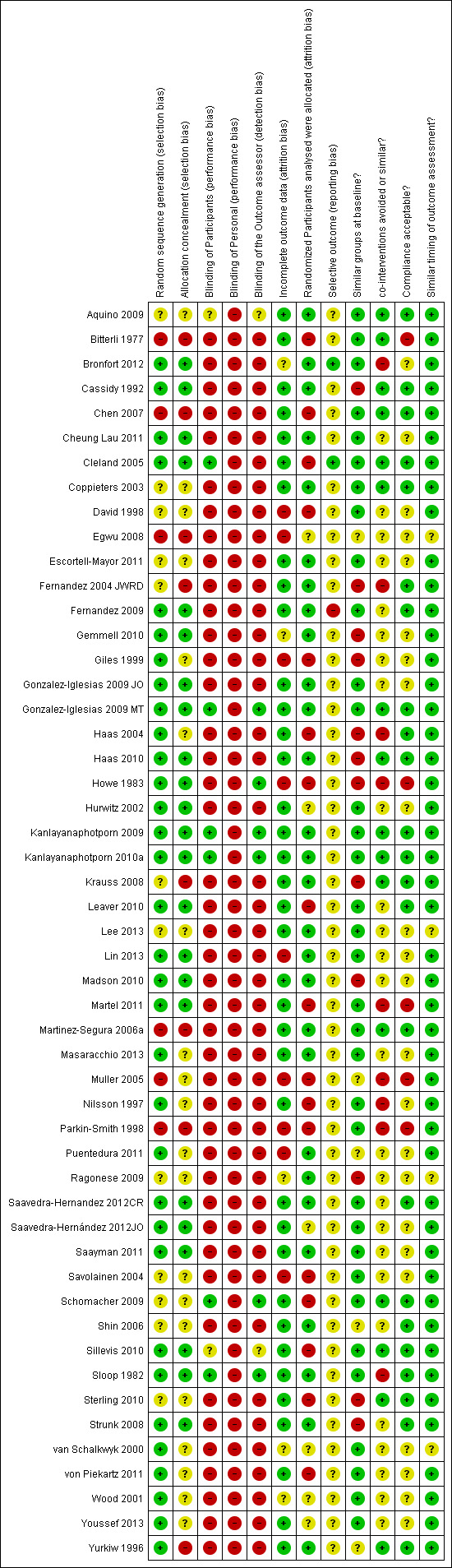
Methodological quality summary: review authors' judgements about each methodological quality item for each included study.
One investigated neck pain with radicular signs and symptoms: duration not reported (Ragonese 2009).
One investigated neck pain with degenerative changes: chronic (Giles 1999).
One investigated a specific neck disorder (herniated disc): chronic (Shin 2006).
Three investigated cervicogenic headache: chronic (Haas 2004; Haas 2010; Youssef 2013)
One investigated cervicogenic headache with degenerative changes: chronic (Chen 2007)..
One investigated cervicogenic headache with or without radicular symptoms: mixed (Hurwitz 2002).
One investigated cervicogenic headache with temporomandibular joint (TMJ) dysfunction (von Piekartz 2011).
Ongoing studies
We recognised in this review a total of 13 ongoing studies from 1995 through 2015. With nine of 13 protocols/pilot studies published in 2010 or before, we could not rule out publication bias. See Characteristics of ongoing studies.
Studies awaiting classification
For Moretti 2004 and Cleland 2007, we are awaiting additional data; therefore classification is pending (see Characteristics of studies awaiting classification). For Leonelli 2013, we are awaiting a translation. We retrieved four studies in our most recent (June 2015) update, and they are pending data extraction (Casanova‐Mendez 2014; El Soleny 2014; Izquierdo‐Perez 2014; Karas 2014).
Excluded studies
We excluded 107 RCTs using the PICO (population, intervention, comparison and outcome) format. We excluded 18 trials on the basis of population (i.e. spasmodic torticollis, unable to split data from combined neck and low back trials, normal cervical spine); 68 for interventions (i.e. manual therapy in both treatment and control groups); 10 for design (i.e. mechanistic or multi‐modal trial design); and 11 for outcomes (i.e. range of motion data only).. See Characteristics of excluded studies.
Risk of bias in included studies
Risk of bias of included manipulation/mobilisation versus inactive controls
A total of 18 studies included a control (see Figure 2) (Bitterli 1977; Cheung Lau 2011; Cleland 2005; Fernandez 2004 JWRD; Fernandez 2009; Gonzalez‐Iglesias 2009 JO; Gonzalez‐Iglesias 2009 MT; Howe 1983; Krauss 2008; Lin 2013; Martel 2011; Martinez‐Segura 2006a; Masaracchio 2013; Parkin‐Smith 1998; Saavedra‐Hernandez 2012CR; Saayman 2011; Sloop 1982; Sterling 2010).
Researchers failed to describe or use appropriate concealment of allocation (39%, 7/18).
Study lacked effective blinding procedures (outcome assessor 83%, 15/18; participant 100%, 18/18; personnel/care provider 100%, 18/18). We acknowledge that it is difficult to blind participants and impossible to blind care providers when manual treatments are provided.
Selective outcome reporting bias was seen in 5% (1/18). The Cervical Overview Group has found that very few investigators register their studies with the research database.
Co‐intervention was avoided in a small number of studies (28%, 5/18), and compliance was monitored in 44% (8/18).
Risk of bias of included manipulation/mobilisation versus active comparisons
A total of 34 studies included a comparison group (see Figure 2) (Aquino 2009; Bronfort 2012; Cassidy 1992; Chen 2007; Coppieters 2003; David 1998; Egwu 2008; Escortell‐Mayor 2011; Gemmell 2010; Giles 1999; Haas 2004; Haas 2010; Hurwitz 2002; Kanlayanaphotporn 2009; Kanlayanaphotporn 2010a; Leaver 2010; Lee 2013; Madson 2010; Muller 2005; Nilsson 1997; Puentedura 2011; Ragonese 2009; Saavedra‐Hernández 2012JO; Saayman 2011; Savolainen 2004; Schomacher 2009; Shin 2006; Sillevis 2010; Strunk 2008; van Schalkwyk 2000; von Piekartz 2011; Wood 2001; Youssef 2013; Yurkiw 1996). Thirteen studies (13/34, 38%) had low risk of bias and 21 (21/34, 62%) had high risk of bias.
Researchers failed to adequately describe or use an appropriate randomisation technique in 13 studies (38%, 13/34).
Study authors failed to adequately describe or use appropriate concealment of allocation in 22 studies (65%, 22/34).
Effective blinding procedures were lacking in 31 studies regarding the participant (91%, 31/34), in 34 studies regarding the care provider (100%, 34/34) and in 31 studies regarding the outcome assessor (91%, 31/34). We acknowledge that it is difficult to blind the participant and impossible to blind the care provider when manual treatments are provided.
Investigators described acceptable dropout rates in 23 studies (68%, 23/34).
All randomly assigned participants were reported/analysed in the group to which they were allocated by randomisation in 18 studies (53%, 18/34).
Information regarding reporting bias was lacking in 33 studies (97%, 33/34).
Groups were similar at baseline regarding the most important prognostic indicators in 20 studies (59%, 20/34).
Co‐intervention was avoided or similar between participants in 10 studies (29%, 10/34).
Researchers monitored acceptable compliance in 14 studies (41%, 14/34).
Timing of the outcome assessment was similar in all groups in 30 studies (88%, 30/34).
Other potential sources of bias
Funnel plot analysis suggests the presence of publication bias (Figure 3).
3.
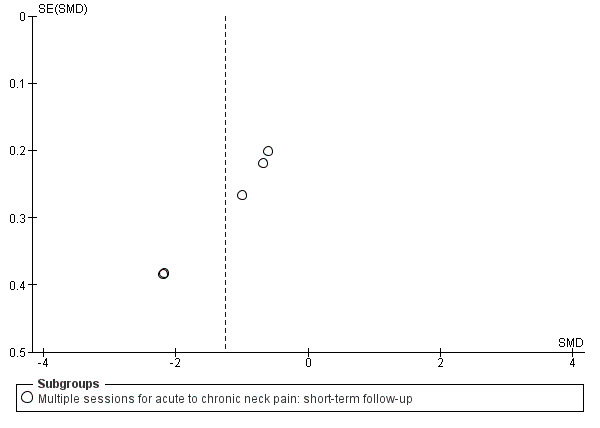
Funnel plot of comparison: manipulation vs control, outcome: FUNNEL PLOT for PAIN: thoracic manipulation vs same treatment in both arms.
Effects of interventions
See: Table 1; Table 2; Table 3; Table 4; Table 5
As data were limited, we were unable to carry out subgroup analyses or meta‐regression for symptom duration, subtype of neck disorder or methodological quality, although we did consistently note them in the text. High‐quality evidence provides greatest certainty about the effectiveness of treatment.
Manipulation alone of cervical region
In all, 24 trials met the inclusion criteria for this section. Twelve of them had low risk of bias (Bronfort 2012; Cassidy 1992; Haas 2004; Haas 2010; Hurwitz 2002; Leaver 2010; Saayman 2011; Sillevis 2010; Sloop 1982; Strunk 2008;Wood 2001; Yurkiw 1996), and 12 had high risk of bias (Bitterli 1977; Chen 2007; Gemmell 2010; Giles 1999; Howe 1983; Martinez‐Segura 2006a; Muller 2005; Nilsson 1997; Puentedura 2011; Saavedra‐Hernández 2012JO; Savolainen 2004; van Schalkwyk 2000). We reported the following observations: (1) results from a single session, which may not depict clinical practice but nevertheless were assessed in clinical trials; and (2) findings of trials using multiple treatment sessions, dose responses and comparison trials.
Manipulation alone of cervical region versus inactive control
Pain
Single session
Three very small RCTs, one at high risk of bias and two at low risk, assessed the effect of a single session of manipulation (see Figure 2): One mock treatment indicated that a single session of manipulation resulted in immediate pain relief (very low quality, number needed to treat for an additional beneficial outcome (NNTB) 2, 71 participants; Martinez‐Segura 2006a) for neck disorders of mixed duration; two trials showed that a single session of manipulation as adjunct treatment to certain medications offered no short‐term benefit for pain relief in chronic neck disorders with radicular findings or headache (very low quality, 29 participants; Howe 1983), nor in subacute and chronic neck disorders with associated cervical spondylosis (low quality, 39 participants; Sloop 1982).
Multiple sessions
Two very small RCTs, one at high and one at low risk of bias, assessed the effects of multiple sessions of manipulation versus a control and provided conflicting evidence. Two trials (low quality, 60 participants; Bitterli 1977; Saayman 2011) that assessed people with subacute and chronic neck pain yielded conflicting results. These results could not be combined because they consisted of different types of data. Six sessions of manipulation over three weeks when added to laser showed pain reduction at short‐term follow‐up (low quality, 40 participants; Saayman 2011). Four sessions over three weeks when compared with an inactive control revealed no evidence of benefit for pain reduction at short‐term follow‐up (low quality, 20 participants; Bitterli 1977).
Manipulation alone of cervical region versus oral medication
Three trials compared cervical manipulation versus use of oral medication.
Non‐steroidal anti‐inflammatory drugs (NSAIDs), acetaminophen, opioids and muscle relaxants (moderate quality, 181 participants with acute and subacute neck pain; Bronfort 2012).
Tenoxicam with ranitidine (very low quality, 35 participants with chronic neck pain; Giles 1999).
Celaconxin, rofecoxib or paracetamol (very low quality, 42 participants with chronic neck pain; Muller 2005).
See Table 1 for main results representing evidence of moderate quality.
Pain
For acute/subacute neck pain, manipulation was more effective than use of certain oral medications [non‐steroidal anti‐inflammatory drugs (NSAIDs), acetaminophen, opioids and muscle relaxants] at immediate post treatment (moderate quality, 182 participants, SMD ‐0.34, 95% CI ‐0.64 to ‐0.05; Bronfort 2012) and at long‐term follow‐up (moderate quality, 181 participants, SMD ‐0.32, 95% CI ‐0.61 to ‐0.02; Bronfort 2012) (see Figure 4). Cervical manipulation was found to be no more effective than certain medications at intermediate‐term follow‐up (moderate quality, 216 participants, SMD ‐0.21, 95% CI ‐0.5 to 0.08; Bronfort 2012).
4.
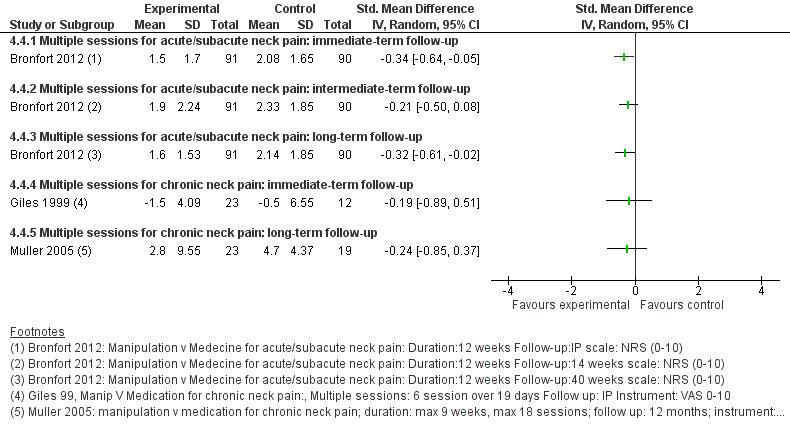
Forest plot of comparison: manipulation vs another treatment, outcome: PAIN: cervical manipulation vs medicine.
For chronic neck pain, manipulation was no different from use of certain medications (see above, per author) at immediate post treatment (very low quality, 35 participants; Giles 1999) and at long‐term follow‐up (very low quality, 42 participants; Muller 2005).
Function and disability
For acute/subacute neck pain, manipulation showed a slight advantage over oral medication (see above) immediate post treatment and at intermediate‐term follow‐up (SMD ‐0.30, 95% CI ‐0.59 to ‐0.00) but not over the long term (SMD ‐0.11, 95% CI ‐0.40 to 0.18, moderate quality, 182 participants; Bronfort 2012).
For chronic neck pain, investigators reported no differences between manipulation and oral medication (see above) at immediate post treatment (very low quality, 30 participants; Giles 1999) and over the long term (very low quality, 42 participants; Muller 2005).
Global perceived effect
Bronfort 2012 (moderate quality, 182 participants) suggested that 12 weeks of manipulation was superior to use of oral medication (see above) for global perceived effect at long‐term follow‐up of participants with acute/subacute neck pain.
Patient satisfication
Bronfort 2012 (moderate quality, 182 participants) suggested that 12 weeks of manipulation was superior to use of oral medication (see above) for satisfaction at long‐term follow‐up among participants with acute/subacute neck pain.
Quality of life
Bronfort 2012 (moderate quality, 182 participants) found no significant results for oral medication (see above) at immediate‐, intermediate‐ and long‐term follow‐up.
Manipulation alone of cervical region versus mobilisation and other manual techniques
Pain
Single session
Two trials assessed the effects of a single session of cervical manipulation versus varied comparisons.
A single session of manipulation (low quality, 100 participants; Cassidy 1992) was comparable with a neuromuscular mobilisation approach using muscle energy technique for immediate pain relief in neck disorders of mixed duration.
A single session of manipulation (low quality, 28 participants; Yurkiw 1996) showed no significant differences in pain relief when compared with a single session of activator instrument.
None of the above trials showed differences between groups for pain relief at immediate term among individuals with subacute or chronic neck disorders.
Multiple sessions
Ten trials assessed the effects of four to 20 sessions of manipulation conducted over two to 12 weeks against:
mobilisations (36 participants, Gemmell 2010; 269 participants, Hurwitz 2002; 177 participants, Leaver 2010);
massage ‐ soft tissue treatments (32 participants, Haas 2010; 53 participants, Nilsson 1997);
manipulation of the thoracic spine alone (20 participants, Puentedura 2011);
combined therapeutic approach including muscle energy provided to the thoracic spine and sacroiliac joint (six participants, Strunk 2008);
manipulation of varied dosages (15 participants, Haas 2004; 32 participants, Haas 2010);
manipulation of varied techniques (30 participants, van Schalkwyk 2000);
mobilisation plus heat; mobilisation plus electronic muscle stimulation (EMS); mobilisation plus heat and EMS (269 participants, Hurwitz 2002); and
activator instrument (36 participants, Gemmell 2010; 30 participants, Wood 2001).
Manipulation was no more effective than mobilisation in improving pain at short‐term (SMD ‐0.05, 95% CI ‐0.34 to 0.25; Leaver 2010) and intermediate‐term follow‐up (moderate quality, 446 participants, MD pooled ‐0.07, 95% CI ‐0.72 to 0.59; Hurwitz 2002; Leaver 2010) (see Figure 5; Table 3). One trial (of very low quality) assessed the effects of six sessions of manipulation conducted over three weeks compared with six sessions of mobilisation (Gemmell 2010). Despite lack of data, none of these studies showed significant differences between groups for pain relief at immediate‐, short‐, intermediate‐ and long‐term (Gemmell 2010) follow‐up for those with subacute and chronic neck pain. Both Haas 2010 and Nilsson 1997 have concluded that manual therapy was more effective than "light manual therapy" (massage) at short term (low quality, 85 participants, SMD pooled ‐0.5, 95% CI ‐0.93 to ‐0.70) follow‐up. These findings are supported by Haas 2010 at intermediate‐term (low quality, 72 participants, SMD ‐0.79, 95% CI ‐1.47 to ‐0.11) follow‐up. A clinician would have to treat five people (NNTB 5) to achieve this intermediate‐term result in one person.
5.
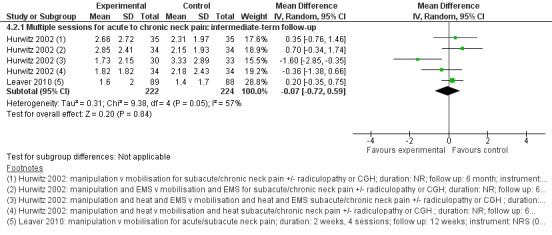
Forest plot of comparison: manipulation vs another treatment, outcome: PAIN: cervical manipulation vs mobilisation at intermediate‐term follow‐up.
Puentedura 2011 (very low quality, 20 participants) demonstrated that cervical manipulation was more effective than thoracic manipulation at short‐ (SMD ‐2.43, 95% CI ‐3.64 to ‐1.21, NNTB 12) and intermediate‐term (SMD ‐2.70, 95% CI ‐3.98 to ‐1.42, NNTB 6) follow‐up. Cervical manipulation contrasted against a combined therapeutic approach of thoracic and sacroiliac manipulation (one trial, six participants; Strunk 2008) yielded similar findings for subacute/chronic neck pain at immediate post treatment. Haas 2004 and Haas 2010 reported no significant results regarding the utilisation of 12 sessions of manipulation versus three sessions at short‐ (low quality, 47 participants, SMD pooled ‐0.66, 95% CI ‐1.81 to 0.49) and intermediate‐term (moderate quality, 50 participants, SMD pooled ‐0.40, 95% CI ‐0.96 to 0.16) follow‐up for chronic neck pain with CGH (see Table 5). Three trials compared one manipulation technique versus another and found no difference in immediate‐ and short‐term pain relief when a rotary break manipulation was compared with a lateral break manipulation for 10 sessions over four weeks in participants with neck disorder of undefined duration (very low quality; van Schalkwyk 2000); and when manual manipulation was compared with instrumental manipulation (activator) for subacute neck disorder after eight sessions over four weeks (very low quality; Wood 2001) and after six sessions over three weeks (very low quality; Gemmell 2010).
Function and disability
Manipulation was no more effective than mobilisation at short‐ (SMD ‐0.06, 95% CI: ‐0.35 to 0.24; Leaver 2010) and intermediate‐term follow‐up (high quality, 446 participants; Hurwitz 2002; Leaver 2010; SMD pooled 0.10, 95% CI ‐0.18 to 0.37). One additional trial (very low quality, 31 participants; Gemmell 2010) assessed the effects of six sessions of manipulation conducted over three weeks compared with six sessions of mobilisation. Despite lack of data, none of these studies showed significant differences between groups in functional improvement at immediate‐, short‐, intermediate‐ and long‐term follow‐up for those with subacute and chronic neck pain. Haas 2010 (low quality, 36 participants) concluded that manipulation was more effective than "light manual therapy" ‐ massage to improve function at short‐ (low quality, 36 participants; SMD ‐0.87, 95% CI ‐1.60 to ‐0.14) and intermediate‐term (SMD ‐0.72, 95% CI ‐1.39 to ‐0.04) follow‐up. A clinician would have to treat five people (NNTB 5) to achieve this medium advantage (29% treatment advantage) for one person at both time points.
Puentedura 2011 (very low quality, 20 participants) concluded that cervical manipulation was more effective than thoracic manipulation at short‐ (SMD ‐1.01, 95% CI ‐1.96 to ‐0.07; NNTB 5) and intermediate‐term (SMD ‐1.22, 95% CI ‐2.19 to ‐0.24; NNTB 4) follow‐up. Haas 2004 suggested that 12 sessions of manipulation was superior to three sessions for immediate functional improvement in individuals with chronic cervicogenic headache (SMD ‐1.15, 95% CI‐2.27 to ‐0.03). Haas 2004 and Haas 2010 reported no significant results regarding the utilisation of 12 to 16 sessions of manipulation compared with three to eight sessions at short‐ (low quality, 47 participants, SMD pooled ‐0.75, 95% CI ‐1.71 to 0.22) and intermediate‐term (moderate quality, 50 participants, SMD pooled ‐0.61, 95% CI ‐1.38 to 0.17) follow‐up (Table 5). One trial assessed the effects of six sessions of manipulation conducted over three weeks compared with six sessions of application of the activator instrument (very low quality, 27 participants; Gemmell 2010); no significant differences between groups were noted in functional improvement at immediate‐, short‐, intermediate‐ and long‐term follow‐up for those with subacute and chronic neck pain.
Global perceived effect
One trial assessed the effects of four sessions of manipulation conducted over two weeks compared with four sessions of mobilisation (moderate quality, 177 participants; Leaver 2010) in individuals with subacute to chronic neck pain. Results showed no differences between groups at immediate‐ (SMD ‐0.18, 95% CI ‐0.47 to 0.12) and intermediate‐term (SMD ‐0.06, 95% CI ‐0.35 to 0.24) follow‐up for global perceived effect. Gemmell 2010 (very low quality, 36 participants) compared the effectiveness of manipulation, mobilisation and the activator instrument. This study showed no significant differences between treatment groups at immediate‐, short‐, intermediate‐ and long‐term follow‐up in global perceived effect for those with subacute neck pain.
Patient satisfication
One trial (moderate quality, 269 participants; Hurwitz 2002) assessed the effect of 12 sessions of manipulation conducted over six weeks compared with mobilisation (SMD ‐0.02, 95% CI ‐0.21 to 0.24). Findings showed no differences in short‐term participant satisfaction among those with subacute and chronic neck pain.
Quality of life
One trial (moderate quality, 176 participants; Leaver 2010) showed no significant differences in quality of life between manipulation and mobilisation at immediate‐, short‐ (SMD 0.08, 95% CI ‐0.21 to 0.38), intermediate‐ (SMD ‐0.06, 95% CI ‐0.35 to 0.24) and long‐term follow‐up for participants with subacute and chronic neck pain. Gemmell 2010 (very low quality, 28 participants) compared the effects of six sessions of manipulation versus application of the activator instrument conducted over three weeks. This trial showed no differences in quality of life between groups at immediate‐, short‐, intermediate‐ and long‐term follow‐up for those with subacute neck pain.
Manipulation alone of cervical region versus exercise or other physical medicine modalities
Pain
Single session
One trial assessed the effects of a single session of cervical manipulation compared with a single use of kinesio‐tape (very low quality, 76 participants; Saavedra‐Hernández 2012JO) and showed no significant differences in pain relief at immediate‐term follow‐up for individuals with subacute or chronic neck disorders.
Multiple sessions
Five trials assessed the effects of manipulation conducted over two to 12 weeks against:
exercise (moderate quality, 182 participants; Bronfort 2012);
low‐level laser therapy (low quality, 40 participants; Saayman 2011);
TENS (very low quality, 70 participants; Chen 2007);
acupuncture (very low quality, 43 participants; Muller 2005); and
low‐voltage electrical acupuncture (very low quality, 38 participants; Giles 1999).
Cervical manipulation was found to be no more effective than exercise (moderate quality, 216 participants; Bronfort 2012) at immediate‐ (SMD ‐0.13, 95% CI ‐0.43 to 0.16), intermediate‐ (SMD ‐0.16, 95% CI ‐0.45 to 0.13) and long‐term (SMD 0.06, 95% CI ‐0.23 to 0.35) follow‐up. See Table 4. One trial (low quality, 40 participants; Saayman 2011) assessed the effects of six sessions of manipulation conducted over three weeks compared with six sessions of low‐level laser therapy at short‐term follow‐up for those with subacute and chronic neck pain; results favoured manipulation plus low‐level laser therapy and showed no differences between manipulation and low‐level laser therapy alone. Chen 2007 (very low quality, 70 participants) demonstrated that manipulation was more effective than TENS for individuals with chronic CGH at short‐term (SMD ‐1.92, 95% CI ‐2.49 to ‐1.35) follow‐up. Manipulation was found to be no different from low‐voltage electrical acupuncture (very low quality, 38 participants; Giles 1999) immediately post treatment or from acupuncture (very low quality, one trial, 43 participants; Muller 2005) in terms of pain relief at long‐term follow‐up.
Function and disability
Single session
One trial (very low quality, 76 participants; Saavedra‐Hernández 2012JO) demonstrated that use of kinesio‐tape for seven days was more effective than performance of two manipulation techniques to improve function immediately after treatment (SMD 0.46, 95% CI 0.01 to 0.92). This difference did not reach the clinically important difference.
Multiple sessions
Manipulation was no more effective than exercise (moderate quality, 182 participants; Bronfort 2012) at immediate‐ (SMD ‐0.21, 95% CI ‐0.50 to 0.08), intermediate‐ (SMD ‐0.01, 95% CI ‐0.30 to 0.28) and long‐term (SMD ‐0.02, 95% CI ‐0.31 to 0.27) follow‐up. Other studies reported no significant differences between groups at any follow‐up time point as follows. No difference in function was noted between low‐voltage electrical acupuncture (very low quality, 38 participants; Giles 1999) immediately post treatment and acupuncture (very low quality, 43 participants; Muller 2005) at long‐term follow‐up. One trial (very low quality, 76 participants; Saayman 2011) assessed the effects of six sessions of manipulation conducted over three weeks versus six sessions of low‐level laser therapy at short‐term follow‐up and showed a significant difference favouring the combination of cervical manipulation plus low‐level laser therapy.
Global perceived effect
Despite the lack of data for statistical analysis, one trial (moderate quality, 182 participants; Bronfort 2012) showed no differences for this outcome between 12 weeks of manipulation and application of a home exercise programme at long‐term follow‐up.
Participant satisfication
Bronfort 2012 (moderate quality, 182 participants) suggested that 12 weeks of cervical manipulation was superior to application of a home exercise programme for participant satisfaction at long‐term follow‐up in participants with acute or subacute neck pain.
Quality of life
One trial (moderate quality, 182 participants; Bronfort 2012) showed no differences (SMD 0.0, 95% CI ‐0.29 to 0.29) between cervical manipulation and a home exercise programme at intermediate‐ and long‐term follow‐up.
Manipulation alone of thoracic region
Twelve trials looked at manipulation alone in the thoracic region.
Manipulation alone of thoracic region versus inactive control
Ten trials (six low risk of bias, four high risk of bias) assessed manipulation alone versus an inactive control in the thoracic region. See Table 2.
Pain
Single session
Three RCTs ‐ two with low and one with high risk of bias ‐ assessed the effects of a single session of manipulation. They were clinically heterogeneous owing to disorder type and comparison (see Figure 2). One trial found that manipulation decreased pain when compared with placebo in participants with chronic neck pain (low quality, 36 participants; Cleland 2005). Two trials showed no differences between groups for manipulation when compared with an inactive control (very low, 22 participants; Krauss 2008) and when compared with same treatment in both arms (low quality, 82 participants; Saavedra‐Hernandez 2012CR).
Multiple sessions
Seven RCTs ‐ four with low and three with high risk of bias ‐ assessed the effects of thoracic manipulation provided at multiple sessions at three different follow‐up points (see Figure 2).
Immediate follow‐up: Two trials (low quality, 90 participants, pooled SMD ‐3.46, 95% CI ‐4.13 to ‐2.79; Fernandez 2009; Gonzalez‐Iglesias 2009 JO) looked at effects on acute pain and found that results favoured the treatment group. Two trials (low quality, 141 participants, pooled SMD ‐0.23, 95% CI ‐1.15 to 0.69; Cheung Lau 2011; Parkin‐Smith 1998) looked at chronic pain, and the results were heterogeneous (I2 = 81%).
Short‐term follow‐up: Four trials (moderate quality, 242 participants; Fernandez 2004 JWRD; Gonzalez‐Iglesias 2009 JO; Gonzalez‐Iglesias 2009 MT; Masaracchio 2013) that looked at acute and subacute neck pain, although assessed to be clinically similar, were statistically heterogeneous (I2 = 84%). Pooled results favoured the experimental group (SMD ‐1.46, ‐2.20 to ‐0.71; NNTB 4 to 7; magnitude of effect: small to medium). For chronic neck pain, one trial (111 participants; Cheung Lau 2011) looked at multiple sessions of thoracic manipulation compared with the same treatment in both arms. Results showed a decrease in pain in the experimental group.
Intermediate follow‐up: One trial (low quality, 111 participants; Cheung Lau 2011) favoured the experimental group when compared with the same treatment in both arms.
Function and disability
Six trials investigated the effects of thoracic manipulation when compared with a control.
Single session
One RCT with low risk of bias assessed the effects of single‐session thoracic manipulation (see Figure 2). This trial (low quality, 82 participants; Saavedra‐Hernandez 2012CR) found that thoracic manipulation significantly favoured the experimental group when function was assessed among participants with chronic neck pain.
Multiple sessions
Four RCTs assessed the effects of multiple sessions of thoracic manipulation at three follow‐up periods (see Figure 2).
Immediate follow‐up: Two trials (low quality, 141 participants, pooled SMD ‐0.52, 95% CI ‐0.85 to ‐0.18; Cheung Lau 2011; Parkin‐Smith 1998) looked at effects on function/disability and significantly favoured the experimental group for chronic neck pain.
Short‐term follow‐up: Four trials (moderate quality, 258 participants; NNTB 5, Cheung Lau 2011; NNTB 5, Gonzalez‐Iglesias 2009 JO; NNTB 5, Gonzalez‐Iglesias 2009 MT; NNTB 4, Masaracchio 2013) looked at the effects of thoracic manipulation among participants with acute, subacute and chronic neck pain. All four trials favoured or significantly favoured the experimental group (pooled SMD ‐1.40, 95% CI ‐2.24 to ‐0.55). The magnitude of effect was small to medium across varied outcome measures.
Intermediate follow‐up: One trial (low quality, 111 participants, NNTB 5, magnitude small; Cheung Lau 2011) looked at the effects of thoracic manipulation among participants with chronic neck pain and significantly favoured the experimental group.
Quality of life
One trial investigated the effects of thoracic manipulation when compared with a control.
Multiple sessions
One RCT with low risk of bias assessed the effects of multiple sessions of thoracic manipulation at immediate‐, short‐ and intermediate‐term follow‐up (see Figure 2). This trial (low quality, 111 participants; Cheung Lau 2011) significantly favoured the experimental group for chronic neck pain.
Subgroup analysis
Effects calculated in these meta‐analyses tended to overestimate the intervention effect, as suggested by the asymmetrical appearance of the funnel plots in Figure 3 (pain). Publication bias, a type of reporting bias, was possible and could not be ruled out. When considering disorder subtypes, all trials except one (Fernandez 2004 JWRD) (WAD 2 or 3) discussed neck pain. Therefore, subgroup analysis of this factor could not be formally conductied through meta‐regression. Very low‐quality evidence (one trial, 88 participants; Fernandez 2004 JWRD) supported thoracic manipulation as an adjunct to individualised physiotherapy care for pain reduction in acute/subacute WAD 2 or 3.
Manipulation alone of thoracic region versus mobilisation
Pain
Single session
One trial (moderate quality, 100 participants; Sillevis 2010) rated as having low risk of bias concluded that a single session of thoracic manipulation was comparable with thoracic mobilisation for immediate pain relief among participants with chronic non‐specific neck pain.
Manipulation alone of thoracic region versus mobilisation
Pain
Multiple sessions
One trial (very low quality, 41 participants; Savolainen 2004) with high risk of bias concluded that four sessions of thoracic manipulation over four weeks led to similar pain outcomes when compared with instructed exercise conducted over an undisclosed period for participants with neck pain of undefined duration at long‐term follow‐up.
Mobilisation alone of cervical region
Nine trials ‐ five with low (Coppieters 2003; David 1998; Hurwitz 2002; Kanlayanaphotporn 2009; Kanlayanaphotporn 2010a) and four with high risk of bias (Bitterli 1977; Cassidy 1992; Egwu 2008; Sterling 2001) ‐ met the inclusion criteria.
Mobilisation alone of cervical region versus inactive control
Two trials looked at mobilisation alone of the cervical region versus an inactive control. Both trials had high risk of bias (Bitterli 1977; Sterling 2010).
Pain
One trial (very low quality, 18 participants; Bitterli 1977) reported no additional pain relief when mobilisation was used as an adjunct to manipulation in participants with chronic CGH or degenerative changes immediately following the treatment period. In one trial (low quality, 39 participants; Sterling 2001), results favoured inactive control when compared with manual contact for participants with subacute/chronic neck pain ‐ WAD 2.
Mobilisation alone of cervical region versus medical injection
Pain
Multiple sessions
Lee 2013 (very low quality, 33 participants) concluded that mobilisation using the proprioceptive neuromuscular facilitation technique was more effective than trigger point intramuscular injection of lidocaine (SMD ‐1.05, 95% CI ‐1.96 to ‐0.15) for participants with neck pain with myofascial pain syndrome.
Function
No significant difference in function was found when this mobilisation approach was compared with intramuscular injection in one trial (very low quality, 33 participants; Lee 2013).
Mobilisation alone of cervical region versus mobilisation and other manual techniques
Pain
Single session
Three trials assessed the effect of one session of one mobilisation technique versus another at a randomly chosen segment in participants with chronic neck pain.
Mobilisation at most symptomatic segment versus mobilisation at randomly chosen segment (low quality, 48 participants; Aquino 2009).
Central posterior‐to‐anterior (PA) passive accessory movement mobilisation technique versus random PAs at the same segment (low quality, 60 participants; Kanlayanaphotporn 2010a).
Ipsilateral PAs versus random PAs at the same segment (low quality, 60 participants; Kanlayanaphotporn 2009).
Mobilisation perpendicular to the facet plane at the most symptomatic segment versus the same mobilisation three levels above or below (low quality, 126 participants; Schomacher 2009).
None of these studies demonstrated significant differences between groups for reducing neck pain. Two studies compared the effectiveness of one mobilisation technique versus another mobilisation technique in individuals with chronic neck pain (Kanlayanaphotporn 2009; Kanlayanaphotporn 2010a). One study showed no significant differences in pain reduction when an ipsilateral PA mobilisation was compared with one of three randomly selected mobilisation techniques: ipsilateral PA, central PA or contralateral PA (Kanlayanaphotporn 2009). Another study by the same authors demonstrated no significant change in pain when comparing central PA mobilisation versus one of the three random mobilisation techniques (Kanlayanaphotporn 2010a). Although statistically not significant, the mean achieved a minimal clinically important change, and post hoc analysis using an interaction plot favoured PA mobilisations over random mobilisation for neck pain during movement.
Multiple sessions
Seven trials assessed the effects of one mobilisation technique against another manual therapy technique. These studies reported the following varied results.
Massage ‐ light manual therapy (very low quality, 22 participants; Madson 2010; 36 participants, Youssef 2013): Youssef 2013 concluded that mobilisation was more effective than a massage regimen consisting of six phases at immediate follow‐up (SMD ‐2.89, 95% CI ‐3.85 to ‐1.93) for chronic CGH, and Madson 2010 noted no difference (SMD ‐0.52, 95% CI ‐1.35 to 0.32) when using effleurage, stroking and pétrissage for chronic neck pain.
One technique versus another ‐ anterior‐to‐posterior (AP) accessory movements, PA transverse and cervical rotational oscillatory techniques (low quality, 95 participants; Egwu 2008): Egwu 2008 concluded that use of an AP unilateral pressure technique was more effective for pain relief immediately post treatment when compared with rotation or transverse pressure (RR 0.36, 95% CI 0.18 to 0.72) after multiple sessions of mobilisation given twice a week for a maximum of four weeks.
Activator instrument (very low quality, 28 participants; Gemmell 2010): One trial (31 participants; Gemmell 2010) showed no significant difference between mobilisation and the Activator instrument for pain relief at immediate‐, short‐, intermediate‐ and long‐term follow‐up among those with subacute neck pain.
Manual therapy to the TMJ (very low quality, 38 participants; von Piekartz 2011): Study authors concluded that manual therapy to the TMJ among individuals with chronic CGH with a minimum of one of the four signs of a TMJ disorder was more effective than manual therapy to the cervical spine immediately post treatment (SMD 2.27, 95% CI 1.43 to 3.10, NNTB 2) and at intermediate‐term (SMD 3.55, 95% CI 2.50 to 4.61, NNTB 2) follow‐up.
Various multi‐modal approaches: Hurwitz 2002 (moderate quality, 133 participants) compared the effectiveness of mobilisation versus manipulation as an adjunct treatment to heat, manipulation plus electrical muscular stimulation (EMS) and manipulation plus heat and EMS. This study showed no significant differences in pain relief between treatment groups of participants with subacute or chronic neck pain at intermediate‐term follow‐up. Additionally, Cassidy 1992 (low quality, 100 participants) compared manipulation versus a muscle energy technique and reported no difference in pain measures immediately following the treatment period for chronic neck pain.
Function and disability
Single session
We found no trial.
Multiple sessions
The following four trials assessed the effects of mobilisation against various manual therapy approaches; three suggested no significant results at any time point, and one (von Piekartz 2011) favoured manual therapy to the TMJ.
Manual therapy to the TMJ (very low quality, 38 participants; von Piekartz 2011): Investigators found that manual therapy to the TMJ was more effective than manual therapy to the cervical spine immediately post treatment (SMD 1.35, 95% CI 0.64 to 2.06, NNTB 5) and at intermediate‐term (SMD 2.22, 95% CI 1.39 to 3.04, NNTB 4) follow‐up. Participants in this trial had cervicogenic headache with at least one sign or symptom of TMJ disorder.
Massage ‐ light manual therapy (very low quality, 23 participants; Madson 2010; 36 participants, Youssef 2013).
Activator instrument (very low quality, 31 participants; Gemmell 2010).
Global perceived effect
Two small trials compared the impact of one session of one PA mobilisation technique versus a random mobilisation technique on global perceived effect in individuals with chronic neck pain at immediate follow‐up (low quality, 120 participants; Kanlayanaphotporn 2009; Kanlayanaphotporn 2010a). Researchers reported no significant results for global perceived effect.
Mobilisation alone of cervical region versus exercise and other physical medicine modalities
Pain
Single session
One trial assessed the effect of one session of mobilisation against pulsed ultrasound (low quality, 20 participants; Coppieters 2003). Researchers investigated neural dynamic mobilisation in 20 participants with acute and chronic neck pain and found a non‐significant difference in pain reduction when compared with pulsed ultrasound. Although results were not statistically significant, the mean achieved a minimal clinically important difference (suggesting possible type 2 error).
Multiple sessions
Five trials assessed the effects of mobilisation against:
acupuncture (low quality, 51 participants; David 1998): no difference in pain reduction when mobilisation was compared with acupuncture for subacute or chronic neck pain including WAD at long‐term follow‐up;
exercise (very low quality, 20 participants; Ragonese 2009): no significant difference for cervical radiculopathy at immediate‐term follow‐up (Table 4);
TENS (very low quality, 87 participants; Escortell‐Mayor 2011): no significant difference for chronic neck pain.
shock wave therapy (very low quality, 33 participants; Lee 2013): cervical neuromuscular mobilisation technique possibly favoured over extracorporeal shock wave therapy at immediate post treatment for myofascial pain in the upper trapezius; and
cervical traction (very low quality, 26 participants; Shin 2006): Chuna manual therapy found more effective than cervical traction immediately post treatment for a herniated cervical disc.
Function and disability
None of the following trials (acupuncture: low quality, 51 participants; David 1998; exercise: very low quality, 20 participants; Ragonese 2009; TENS: very low quality, 87 participants; Escortell‐Mayor 2011; shock wave therapy: very low quality, 33 participants; Lee 2013) suggested significant results at any time point.
Patient satisfaction
One study (very low quality, 89 participants; Escortell‐Mayor 2011) assessed the effects of 10 sessions of mobilisation conducted over four weeks compared with utilisation of TENS at the cervical region. Investigators showed no significant results for utilisation of TENS at intermediate‐term (RR 1.09, 95% CI 0.96 to 1.23) follow‐up in terms of patient satisfaction among those with chronic neck pain.
Quality of life
One trial compared the effects of 10 sessions of mobilisation conducted over four weeks versus utilisation of TENS at the cervical region (very low quality, 83 participants; Escortell‐Mayor 2011). Researchers showed no differences at immediate‐ and intermediate‐term follow‐up for quality of life among those with chronic neck pain. David 1998 (low quality, 51 participants) showed no significant results when comparing mobilisation of the cervical region versus acupuncture at intermediate‐term (RR 1.07, 95% CI 0.48 to 2.35) follow‐up.
Other considerations
Adverse events
When researchers looked at mobilisation and manipulation versus an inactive control, they reported the number of participants experiencing side effects in 9.5% (2/18) of trials. One trial (Cheung Lau 2011) reported no side effects, and another trial (Saavedra‐Hernandez 2012CR) reported benign and transient side effects, including increased neck pain (one in the control group) or increased neck fatigue (one in the intervention group). The rate of rare but serious adverse events such as strokes or serious neurological deficits could not be established from our review data; the power to detect any serious events is too low in these RCTs, and strict RCT procedures might prevent occurrence of such serious complications. When investigators contrasted mobilisation and manipulation against another comparison treatment, they noted that 35% (12/34) of participants experienced adverse events. Ten trials reported benign and transient adverse events for manipulation (Bronfort 2012; Cassidy 1992; Chen 2007; Giles 1999; Haas 2004; Hurwitz 2002; Leaver 2010; Puentedura 2011; Saayman 2011; Shin 2006). Among participants receiving manipulation, 22% (105/469 participants) experienced adverse events. Four trials reported benign and transient adverse events for mobilisation (David 1998; Hurwitz 2002; Leaver 2010; Schomacher 2009). Among participants receiving mobilisation, 11% (42/390 participants) experienced adverse events. All adverse events reported for manipulation or mobilisation were benign and transient and were included for both interventions: increased neck pain, soreness, headache, stiffness, dizziness, nausea, paraesthesia, upper limb pain, fatigue, mid‐lower back pain and "unpleasant change in spinal posture".
Cost of care
The 51 trials included in this review reported no direct measures of the cost of care.
Discussion
Summary of main results
The objective of this literature review was to evaluate the effects of manipulation or mobilisation as a single treatment option versus a control intervention or versus other treatment interventions for neck pain. Review authors found support for use of thoracic manipulation versus control for neck pain, function and quality of life. Results for cervical manipulation and mobilisation versus control were few and diverse. We could not rule out publication bias. Findings suggest that manipulation and mobilisation produce similar results. Multiple cervical manipulation sessions provide slightly better improvement over certain medications such as varied combinations of non‐steroidal anti‐inflammatory drugs (NSAIDs), analgesics, opioids and muscle relaxants. In lieu of serious adverse event risk for manipulation and in the light of evidence suggesting that mobilisation and manipulation produce similar results, further high‐quality research exploring mobilisation is needed.
Overall completeness and applicability of evidence
How do we as meta‐analysts reconcile the various models of care? We noted that use of unimodal approaches was not common in clinical practice, although they are essential elements for teasing out which therapeutic item or combination works best. Typical conservative care takes a more holistic clinical approach and includes a treatment continuum (Jovey 2002) ‐ that is, physical, psychological and pharmacological ‐ starting with treatments that are most available, least expensive and least invasive and that produce the fewest side effects. Our review authors have acknowledged these diversities and have noted the following emerging questions.
How do we know when mobilisations will be effective? This remains unclear, as only two additional trials were discovered by this search. Meta‐analyses, subgroup analyses and sensitivity analyses continue to be hampered by the wide spectrum of comparisons, treatment characteristics and dosages. Until the number of high‐quality studies within individual subgroups of neck pain increases, we will not be able to provide strong conclusions about which groups benefit most from manipulation or mobilisation. Cleland 2007 and Puentedura 2012 developed clinical prediction rules for use of thoracic manipulation in the treatment of neck pain. Similar studies investigating clinical prediction rules for other mobilisations or manipulations in varied neck pain populations would help clinicians to determine when to manual therapy should be utilised.
What is the ideal mobilisation or manipulation?Our review showed that one technique was frequently compared with another in head‐to‐head comparisons of single techniques or combined treatment approaches. The answer to this question remains unclear, but evidence suggests that anterior‐posterior (AP) or posterior‐anterior (PA) mobilisations may be more effective for reducing pain than transverse or rotational mobilisations. We believe that continued research is needed to perform head‐to‐head comparisons between the most viable techniques or approaches.
What is the optimal "dosage"? What are the optimal "clinical parameters" for a given technique category? We still do not know how to answer these questions. Data on pain relief gathered to date reveal that the most commonly reported factors were frequency (total number of sessions) and duration (total number of weeks). We noted that levels of these two factors measured at various follow‐up periods were as follows: manipulation to cervical region alone: one to 18 sessions; one day to nine weeks; manipulation of thoracic region alone: one to 15 sessions; one day to three weeks; mobilisation of cervical region alone: one to six sessions; one day to six weeks. The ideal dosage for cervical manipulation, thoracic manipulation or cervical mobilisation for treatment of cervical pain could not be determined when existing controlled trials were evaluated. Pilot studies of mobilisation and manipulation exploring the minimally effective dose and the optimal dose should be conducted before a larger trial is undertaken. These pilot studies would serve a purpose similar to that of the small dose‐finding studies conducted as part of pharmaceutical trials used to establish a minimally effective dose. One such pilot study (Haas 2004) provided preliminary support for a larger trial assessing 12 sessions and nine sessions over three sessions of cervical manipulation.
A systematic review of adverse events (Carlesso 2010) noted that ascertainment bias may compromise the credibility of current studies. More trials are required to report on adverse events if meta‐analysis is to be useful for obtaining a summary estimate of minor adverse events. Two recent randomised trials have noted that transient minor side effects such as increased treatment soreness are common (Paanalahti 2014; Walker 2013). These studies and one systematic review support the theory that the occurrence of catastrophic events is rare (Carlesso 2010). Vertebrobasilar artery stroke following manipulation is a rare event (Cassidy 2008). Nevertheless, craniocervical arterial dissections as sequelae of cervical manipulation occur and should be managed (Albuquerque 2011; Rushton 2012). Conclusive evidence is lacking for a strong association between neck manipulation and stroke (Haynes 2012), and smaller randomised trials are unlikely to detect rare adverse events. From surveys and review articles, the risk of a serious irreversible complication (e.g. stroke) of cervical manipulations has been reported to vary from one adverse event in 3020 to one in 1,000,000 manipulations (Assendelft 1996; Gross 2002b). Reporting of serious adverse events continues to be required. As emerging literature shows that manipulation and mobilisation are valuable additions to patient care options, new trials are necessary to determine economic and risk advantages derived from using manipulation or mobilisation techniques to treat neck pain.
Quality of the evidence
The overarching limitation noted in this review is that only five of the 51 trials included a sample size of more than 100 participants. Many trials were extremely small (20 to 30 participants). The quality of evidence is strongly limited by the large number of small trials.
The randomisation technique was appropriate and was adequately described in 65% (33/51), and allocation concealment was sufficiently detailed and appropriate in 45% (23/51) of studies. These criteria are important for minimising selection bias, so that treatment is applicable to the general population. Without rates of randomisation and allocation concealment, it is unclear whether groups had baseline comparability, and whether study results are applicable to the general patient population.
Many biases (detection and performance biases) are inherent in trials and tend to overestimate the trial effect. A dominant bias in the studies included in this review was lack of blinding of participants (45/51) and therapists (100%). Blinding is difficult to perform in a randomised controlled trial examining manipulation or mobilisation versus control. Blinding of both participants and therapists minimises performance bias as the result of differences in actual treatment provided to groups and expectations of treatment. Given lack of blinding of participants and therapists, it is important to blind outcome assessors to ensure that no detection bias is present; however, only 12% of studies (6/51) blinded the assessor. This occurred in large part because many of the assessors were actually the participants themselves as required by the outcome measures (Neck Disability Index (NDI), visual analogue scale (VAS), Short Form (SF)‐36) used in various trials. Researchers can minimise this bias by integrating observer‐based outcomes, especially those pertaining to function and disability. Many pain trials use self reported outcomes; this makes it hard to protect against detection bias. Similarly, if one is to conclude that treatment effects in fact were due to the intervention, thereby reducing performance bias, it is important to avoid co‐interventions. Thirty‐one per cent (16/51) of the included studies explicitly avoided co‐interventions. Based on the relatively short nature of physiotherapeutic interventions, it would be crucial to avoid co‐interventions that otherwise may confound study results. Timing of outcome assessments is one of the dominant flaws leading to overestimation of the effects of care. In 37% (19/51) of trials, outcomes were assessed for single‐session trials, resulting in overestimation of the treatment effect size.
As this review is examining manipulation or mobilisation versus an inactive control or an active treatment, compliance with treatment must be evaluated if strong conclusions are to be provided. Of the 51 trials included in our review, compliance was monitored and acceptable in 45% (23/51). To ensure compliance, investigators had to track how often the participant came into the clinic to receive manipulation or mobilisation, and whether the participant received any other treatment during the entire length of the study. The most common method of tracking a patient’s treatment schedule is by using a diary. This method was rarely reported in the included trials.
Our group has observed three positive advances in recent years. Trials have become larger, have demonstrated lower risk of bias (20/51) and have used self reported ratings (e.g. pain, disability self report questionnaires, global perceived effect) as primary outcomes on a more consistent basis.
Most of our 51 trials were conducted immediately post treatment. With no long‐term follow‐up studies, it is hard for therapists to make a judgement in terms of using a particular technique in their practice. Single‐session trials using manipulation are few. Many of the benefits of a single manipulation are neurophysiological. Future investigators need to look at the optimal dosage to maximise the effects of manipulation or mobilisation. The very low to low quality of evidence for cervical manipulation and the moderate quality of evidence for thoracic manipulation in treating neck pain can leave a professional therapist with a level of uncertainty. The relevance of the evidence remains in question because (1) participants in manual therapy trials are not blinded as a result of the nature of the intervention being delivered; and (2) primary outcome measures are often self reported (i.e. pain), causing the participant to technically become ‘the outcome assessor’ who is not blinded to previous measures.
Potential biases in the review process
We used two independent review authors who were trained in the process and employed standardised forms. The effectiveness of this strategy was confirmed by strong agreement (kappa analysis) between review authors. We further attempted to limit systematic error by searching for both published and unpublished literature. Randomised controlled trials often go unpublished if they do not yield positive results. Searching the grey literature makes the results of systematic reviews more comprehensive.
Selection bias was avoided for citation screening and full‐text screening, as each phase was conducted in duplicate and with fair to good agreement. Language bias was avoided to the extent of including all languages during study selection; however, we did not search non‐English databases (i.e. Chinese databases). In this update, we captured one non‐English trial (Mansilla‐Ferragud 2008). It is also important to analyse the risks inherent in and the limitations of our systematic review update. A sweeping literature search is important for obtaining the full spectrum of results of applying manipulation or mobilisation for neck pain. Accordingly, it is important that an effort be made to search multiple language‐based databases.
In our grey literature search, one non‐published thesis (Khoury 2002) was uncovered but did not meet our selection criteria. Publication bias cannot be ruled out. The asymmetrical appearance of the funnel plot (see Figure 3) suggests the presence of publication bias. Publication bias was a matter of concern during the systematic review process. Many study authors tend to submit only trials with positive results for publication in peer‐reviewed journals. This can lead to overestimation of results. Fewer than 10 trials were included in each plot, further reducing the meaning of these data. Additionally, nine of 13 trials listed as ongoing trials (those conducted longer than five years ago) conducted during the period from 1995 to 2010 (Groeneweg 2010; Gudavalli 2006;Guerriero 1997; Kjellman 1997;Nagy 2000;Scott‐Dawkins 1997;Shammsuddin 2010; Stokke 1995;Tanaka 1995) may further support the notion of publication bias, especially if a “worse‐case scenario” that all trials are negative is considered. As we know, many negative trials never reach publication. Note that we did search the Internet and databases for all trials included in the ’ongoing’ list, and we wrote to each study author but received no response.
Sources of random error were limited by use of two independent review authors who used a standardised tool during the data extraction process. Reliability of the risk of bias tool was assessed by Graham 2012 for the Cervical Overview Group (COG) and was considered acceptable. Last, we predetermined our primary and secondary outcomes; this limited the random error associated with accepting articles that discussed a broad variety of outcomes.
Future updates of our review could benefit from addressing a diverse range of factors that may help to reduce systematic error. It may be appropriate, for example, to examine the pattern of results based on country of origin, and to explore why this pattern exists. Additional possibilities include examining results on the basis of therapist experience or provision of primary care as opposed to secondary care. Pooling of results according to type of neck disorder and length of injury may or may not be important for the magnitude of effects. Furthermore, risk of time lag bias means that positive trials may be published faster than negative trials. It is important to search the grey literature to find all trials. Future updates will be more informative if review authors can identify a greater number of trials related to the topic under review. Last, in the future, we must scrutinise studies on the basis of conflicts of interest due to funding from donors.
Agreements and disagreements with other studies or reviews
For acute whiplash‐associated disorder (WAD), we retrieved no evidence (0 trials; Shaw 2010). Although we assessed 15 trials on WAD, we found no trials that reported on mobilisation or manipulation provided as a single stand‐alone therapy compared with inactive treatment or other treatment interventions. For subacute WAD, weak evidence favoured manipulation in the short term; concerns regarding the rigor of methods used were noted (weak quality, one trial; Teasell 2010). Our findings are consistent with this evidence.
For cervical radiculopathy, no evidence was found on manipulation or mobilisation compared with inactive treatment. However, we found one trial (Ragonese 2009) suggesting that mobilisation alone is equal to exercise alone at short‐term follow‐up for pain. This very low quality of evidence statement is consistent with findings of the Thoomes 2013 systematic review on all forms of intervention for cervical radiculopathy.
For people with acute, subacute and chronic neck pain, manipulation more effectively reduced pain immediately following treatment when contrasted with inactive treatment (low to moderate quality, four trials; Clar 2014; Furlan 2012). Posadzki 2011 (one trial) compared one osteopathic manipulation versus a sham ultrasound and reported significant longitudinal change for individuals with chronic neck pain. We found eight trials assessing non‐specific neck pain and suggesting that a single manipulation reduces pain more effectively immediately post treatment or in the short term compared with a control. We suggest that evidence continues to be of lowor very lowquality, as trial results could not be pooled. Furthermore, when we compared the effectiveness of several sessions of manipulation versus several sessions of mobilisation, we found high‐ to moderate‐quality evidence showing that these two manual therapy interventions are equally effective in improving pain, function, quality of life, patient satisfaction and global perceived effect. These findings are consistent with those of the Neck Pain Task Force review (Hurwitz 2008) and Furlan 2012 systematic review. We found moderate‐quality evidence suggesting that manipulation is superior to medication (NSAIDs and analgesics) for pain relief at immediate‐, intermediate‐ and long‐term follow‐up based on findings of a large trial (Bronfort 2012) and two smaller trials (Giles 1999; Madson 2010). Our findings contrast with those of Furlan 2012, who concluded that manipulations are similar to medication in providing pain relief at short‐term follow‐up.
We agree with Scholten Peeters 2013 and Walser 2009 that thoracic manipulation is beneficial when contrasted with a placebo intervention, but we noted no differences from other treatment. We found one trial that favoured cervical manipulation over thoracic manipulation (Puentedura 2011) and two trials that showed thoracic manipulation to be equally effective when compared with thoracic mobilisation (Sillevis 2010) and with exercise (Savolainen 2004). The findings of Huisman 2013 were comparable with our own.
For participants with acute/subacute or chronic or mixed non‐specific neck pain, mobilisation reduced pain when contrasted with no treatment (low quality, three trials; Furlan 2012). However, no difference in chronic non‐specific neck pain was noted when mobilisation was contrasted with placebo (low quality, one trial; Furlan 2012). Contrary to this finding, our review found two trials (57 participants) provided low‐ or very low‐quality evidence showing no pain relief. Finally, we found that certain forms of mobilisation (AP) are superior to other forms (rotatory or transversal mobilisation) for providing pain relief at immediate follow‐up. To our knowledge, no other systematic review has reported this very low level of evidence finding.
Authors' conclusions
Implications for practice.
What is beneficial?For individuals with acute/subacute neck pain, thoracic manipulation provided short‐term neck pain relief, and for those with acute and chronic neck pain, it further improved function when contrasted with an inactive control. For acute/subacute neck pain, multiple sessions of cervical manipulation provided better pain relief and functional improvement than were attained with certain oral medications such as varied combinations of NSAIDs, analgesics, opioids and muscle relaxants at immediate‐, intermediate‐ and long‐term follow‐up.
What has a similar effect? For individuals with acute and chronic neck pain, cervical manipulation versus mobilisation produced similar results in neck pain reduction, functional improvement, quality of life and global perceived effect at immediate‐, short‐ and intermediate‐term follow‐up. A similar pattern was observed when thoracic mobilisations were contrasted with thoracic manipulation techniques in chronic neck pain. Given the risk of rare but devastating adverse events linked to cervical manipulation, cervical mobilisation may be the technique of choice when treatment of the cervical region is needed. As minor transient adverse events appeared to be similar in the thoracic region, both thoracic mobilisation and manipulation appear to be reasonable options for the treatment of patients with neck pain.
Implications for research.
Meta‐analysis of data across trials and sensitivity analysis were hampered by the wide spectrum of comparisons, treatment characteristics and dosages. Factorial designs would help determine active treatment agent(s) within a treatment mix. Phase II trials would help to identify the most effective treatment characteristics and dosages. Greater attention to methodological quality continues to be needed, as is protection against publication bias. Study designs of highest quality are needed to assess efficacy for mobilisation in neck pain. As manipulation has the potential to produce serious adverse effects, and as the present evidence shows no difference in effectiveness when compared with mobilisation, we suggest that additional trials on manipulation would be a matter of secondary priority.
What's new
| Date | Event | Description |
|---|---|---|
| 3 June 2014 | New citation required and conclusions have changed | We added 24 new trials from the June 2014 search, and we added 7 trials to the 'Awaiting classification' section from the June 2015 search update. We grouped controls into active controls and inactive controls |
| 3 June 2014 | New search has been performed | We added 24 new trials and a 'Summary of findings' table |
| 6 April 2010 | Amended | We added new references to 'Other references' (Karlberg 1996; Souvlis 2004), and we clarified the NNTB definition |
History
Protocol first published: Issue 1, 2003 Review first published: Issue 2, 2003
| Date | Event | Description |
|---|---|---|
| 25 November 2010 | New citation required and conclusions have changed | We changed conclusions because they dealt with results from trials that examined the effects of single modalities |
| 8 July 2009 | New search has been performed | We updated the literature search and changed the scope to include trials with manipulation or mobilisation as a single modality. We included in this update 32 publications, reporting on 27 trials |
| 25 November 2006 | New search has been performed | Review authors have added 15 new RCTs since the last review was published in 2004 |
| 25 November 2006 | New citation required and conclusions have changed | Evidence did not favour a course of manipulation or mobilisation alone or in combination with various other physical medicine agents for pain, function and global perceived effect. However, the combined effect of manipulation, mobilisation and soft tissue work may be beneficial for global perceived effect and patient satisfaction, at least over the short term. Mobilisation or manipulation combined with exercise, delivered as part of a programme, had lasting and clinically important benefit for pain relief, functional improvement and global perceived effect in subacute/chronic mechanical neck disorders with or without headache. The addition of thoracic manipulation may be beneficial for neck pain relief in (sub)acute whiplash‐associated disorders. It was not possible to determine which technique or dosage was most beneficial, or if certain subgroups benefited more from one form of care than another. Evidence was insufficient to allow conclusions regarding neck disorders based on radicular findings |
Acknowledgements
Funding was provided by the LIfeMark Centric Industry partnership grant. We are indebted to the many authors of primary studies for their support in retrieving original research. We thank our volunteers, translators, students, the Cochrane Back Review Group editors and Lisa Carlesso and Colleen McPhee for granting early access to their research. We would like to thank the members of the Cervical Overview Group for assistance and guidance provided during all phases of this update.
Appendices
Appendix 1. Search strategy
MEDLINE (Ovid)
Last Update November 2014; research librarian: Maurine Rice, McMaster University
1. neck/ or neck muscles/ or exp cervical plexus/ or exp cervical vertebrae/ or Atlanto‐Axial Joint/ or atlanto‐occipital joint/ or axis/ or atlas/ or spinal nerve roots/ or exp brachial plexus/ 2. (odontoid or cervical or occip: or atlant:).tw. 3. 1 or 2 4. exp arthritis/ or exp myofascial pain syndromes/ or fibromyalgia/ or spondylitis/ or exp spinal osteophytosis/ or spondylolisthesis/ 5. exp headache/ and cervic:.tw. 6. whiplash injuries/ or cervical rib syndrome/ or torticollis/ or cervico‐brachial neuralgia.ti,ab,sh. or exp radiculitis/ or polyradiculitis/ or polyradiculoneuritis/ or thoracic outlet syndrome/ 7. (monoradicul: or monoradicl:).tw. 8. 4 or 5 or 6 or 7 9. random:.ti,ab,sh. 10. randomised controlled trial.pt. 11. double‐blind method/ 12. single blind method/ 13. placebos/ 14. clinical trial.pt. 15. exp clinical trials/ 16. controlled clinical trial.pt. 17. (clin$ adj25 trial$).ti,ab. 18. ((singl$ or doubl$ or trebl$) adj25 (blind$ or mask$)).ti,ab. 19. placebo$.ti,ab. 20. or/9‐19 21. exp arthritis/rh,th or exp myofascial pain syndromes/rh,th or fibromyalgia/rh,th or spondylitis/rh,th or exp spinal osteophytosis/rh,th or spondylosis/rh,th or spondylolisthesis/rh,th 22. exp headache/rh,th and cervic:.tw. 23. whiplash injuries/rh,th or cervical rib syndrome/rh,th or thoracic outlet syndrome/rh,th or torticollis/rh,th or cervico‐brachial neuralgia/rh,th or exp radiculitis/rh,th or polyradiculitis/rh,th or polyradiculoneuritis/rh,th 24. or/21‐23 25. exp alternative medicine/ or chiropractic/ 26. (acupuncture or biofeedback or chiropract: or electric stimulation therapy or kinesiology or massage or traditional medicine or relaxation or therapeutic touch).tw. 27. or/25‐26 28. 3 and 24 29. 3 and 8 and 27 30. 28 or 29 31. 20 and 30
EMBASE (Ovid)
Last Updated November 2014; research librarian: Maurine Rice, McMaster Univesity
1. neck pain/
2. brachial plexus neuropathy/
3. neck injury/ or whiplash injury/
4. cervical pain.mp.
5. neckache.mp.
6. whiplash.mp.
7. cervicodynia.mp.
8. cervicalgia.mp.
9. brachialgia/
10. brachialgia.mp.
11. brachial neuritis.mp.
12. brachial neuralgia.mp.
13. neck pain.mp.
14. neck injur*.mp.
15. brachial plexus neuropath*.mp.
16. brachial plexus neuritis.mp.
17. thorax outlet syndrome/
18. torticollis/
19. cervico brachial neuralgia.ti,ab.
20. cervicobrachial neuralgia.ti,ab.
21. (monoradicul* or monoradicl*).tw.
22. or/1‐21
23. exp headache/ and cervic*.tw.
24. exp gynecologic disease/
25. genital disease*.mp.
26. exp *uterine cervix/
27. or/24‐26
28. 23 not 27
29. 22 or 28
30. neck/ or neck muscle/
31. cervical plexus/
32. cervical spine/
33. atlantoaxial joint/
34. atlantooccipital joint/
35. atlas/
36. "spinal root"/
37. brachial plexus/
38. (odontoid* or cervical or occip* or atlant*).tw.
39. odontoid process/
40. cervical vertebra.mp.
41. cervical vertebrae.mp.
42. cervical plexus.mp.
43. cervical spine.mp.
44. (neck adj3 muscles).mp.
45. (brachial adj3 plexus).mp.
46. (thoracic adj3 vertebra?).mp.
47. neck.mp.
48. (thoracic adj3 spine).mp.
49. (thoracic adj3 outlet).mp.
50. trapezius.mp.
51. cervical.mp.
52. cervico*.mp.
53. 51 or 52
54. exp gynecologic disease/
55. genital disease*.mp.
56. exp *uterine cervix/
57. 54 or 55 or 56
58. 53 not 57
59. 30 or 31 or 32 or 33 or 34 or 35 or 36 or 37 or 38 or 39 or 40 or 41 or 42 or 43 or 44 or 45 or 46 or 47 or 48 or 49 or 50 or 58
60. exp pain/
61. exp injury/
62. pain.mp.
63. ache.mp.
64. sore.mp.
65. stiff.mp.
66. discomfort.mp.
67. injur*.mp.
68. neuropath*.mp.
69. or/60‐68
70. radiculopathy/
71. temporomandibular joint disorder/
72. myofascial pain/
73. spondylosis/ or cervical spondylosis/
74. neuritis/
75. exp arthritis/
76. fibromyalgia/
77. exp spondylitis/
78. diskitis/
79. spondylolisthesis/
80. radiculopathy.mp.
81. radiculitis.mp.
82. temporomandibular.mp.
83. myofascial pain syndrome*.mp.
84. spinal osteophytosis.mp.
85. neuritis.mp.
86. spondylosis.mp.
87. spondylitis.mp.
88. spondylolisthesis.mp.
89. or/70‐88
90. 59 and 89
91. neck/
92. cervical spine/
93. neck.mp.
94. (thoracic adj3 vertebra?).mp.
95. cervical.mp.
96. cervico*.mp.
97. exp gynecologic disease/
98. genital disease*.mp.
99. exp *uterine cervix/
100. or/97‐99
101. 95 or 96
102. 101 not 100
103. (thoracic adj3 spine).mp.
104. cervical spine.mp.
105. 91 or 92 or 93 or 94 or 102 or 103 or 104
106. intervertebral disk/
107. (disc or discs).mp.
108. (disk or disks).mp.
109. 106 or 107 or 108
110. 105 and 109
111. herniat*.mp.
112. slipped.mp.
113. prolapse*.mp.
114. displace*.mp.
115. degenerat*.mp.
116. (bulge or bulged or bulging).mp.
117. 110 or 111 or 112 or 113 or 114 or 115 or 116
118. 110 and 117
119. intervertebral disk hernia/
120. intervertebral disk degeneration/
121. intervertebral disc degeneration.mp.
122. intervertebral disk degeneration.mp.
123. intervertebral disc displacement.mp.
124. intervertebral disk displacement.mp.
125. 119 or 120 or 121 or 122 or 123 or 124
126. 105 and 125
127. 59 and 69
128. 29 or 90 or 118 or 126 or 127
129. exp *neoplasm/
130. exp *penetrating trauma/
131. 129 or 130
132. 128 not 131
133. neck pain/rh, th
134. brachial plexus neuropathy/rh, th
135. neck injury/ or whiplash injury/rh, th
136. brachialgia/rh, th
137. thorax outlet syndrome/rh, th
138. Torticollis/rh, th
139. Radiculopathy/rh, th
140. temporomandibular joint disorder/rh, th
141. myofascial pain/rh, th
142. spondylosis/rh, th or cervical spondylosis/rh, th
143. neuritis/rh, th
144. exp arthritis/rh, th
145. Fibromyalgia/rh, th
146. exp spondylitis/rh, th
147. diskitis/rh, th
148. spondylolisthesis/rh, th
149. acupuncture/ or acupressure/ or acupuncture analgesia/
150. exp manipulative medicine/
151. massage.tw.
152. mobili?ation.tw.
153. (acupuncture or acu‐puncture or needling or acupressure or mox?bustion).tw.
154. ((neck or spine or spinal or cervical or chiropractic* or musculoskeletal* or musculo‐skeletal*) adj3 (adjust* or manipulat* or mobiliz* or mobilis*)).tw.
155. (manual adj therap*).tw.
156. (manipulati* adj (therap* or medicine)).tw.
157. (massag* or reflexolog* or rolfing or zone therap*).tw.
158. Nimmo.tw.
159. (vibration adj5 (therap* or treatment*)).tw.
160. (Chih Ya or Shiatsu or Shiatzu or Zhi Ya).tw.
161. (flexion adj2 distraction*).tw.
162. (myofascial adj3 (release or therap*)).tw.
163. muscle energy technique*.tw.
164. trigger point.tw.
165. proprioceptive Neuromuscular Facilitation*.tw.
166. cyriax friction.tw.
167. (lomilomi or lomi‐lomi or trager).tw.
168. aston patterning.tw.
169. (strain adj counterstrain).tw.
170. (craniosacral therap* or cranio‐sacral therap*).tw.
171. (amma or ammo or effleuurage or petrissage or hacking or tapotment).tw.
172. alternative medicine/
173. ((complement* or alternat* or osteopthic*) adj (therap* or medicine)).tw.
174. (Tui Na or Tuina).tw.
175. (swedish massage or rolfing).tw.
176. therapeutic touch.mp.
177. massotherapy.tw.
178. effleurage.mp.
179. or/149‐178
180. 132 and 179
181. 133 or 134 or 135 or 136 or 137 or 138
182. or/139‐148
183. 59 and 182
184. 180 or 181 or 183
185. randomized controlled trial/
186. controlled clinical trial/
187. (random* or sham or placebo*).tw.
188. placebo/
189. randomization/
190. single blind procedure/
191. double blind procedure/
192. ((singl* or doubl* or trebl* or tripl*) adj5 (blind* or dumm*or mask*)).ti,ab.
193. (rct or rcts).tw.
194. (control* adj2 (study or studies or tiral*)).tw.
195. or/185‐194
196. human/
197. nonhuman/
198. animal/
199. animal experiment/
200. or/197‐199
201. 200 not (200 and 196)
202. 195 not 201
203. 184 and 202
204. limit 203 to yr="2006 ‐Current"
205. limit 203 to yr="1928 ‐ 2005"
206. guidelines as topic/
207. practice guidelines as topic/
208. (guideline? or guidance or recommendations).ti.
209. consensus.ti.
210. or/206‐209
211. 184 and 210
212. limit 211 to yr="2006 ‐Current"
213. limit 211 to yr="1928 ‐ 2005"
214. meta analysis/
215. systematic review/
216. (meta analy* or metaanaly* or met analy* or metanaly*).tw.
217. (collaborative research or collaborative review* or collaborative overview*).tw.
218. (integrative research or integrative review* or intergrative overview*).tw.
219. (quantitative adj3 (research or review* or overview*)).tw.
220. (research integration or research overview*).tw.
221. (systematic* adj3 (review* or overview*)).tw.
222. (methodologic* adj3 (review* or overview*)).tw.
223. biomedical technology assessment/
224. (hta or thas or technology assessment*).tw.
225. ((hand adj2 search*) or (manual* adj search*)).tw.
226. ((electronic adj database*) or (bibliographic* adj database*)).tw.
227. ((data adj2 abstract*) or (data adj2 extract*)).tw.
228. (data adj3 (pooled or pool or pooling)).tw.
229. (analys* adj3 (pool or pooled or pooling)).tw.
230. mantel haenszel.tw.
231. (cochrane or Pubmed or pub med or medline or embase or psycinfo or psyclit or psychinfo or psychlit or cinahl or science citation index).ab.
232. or/214‐231
233. 184 and 232
234. limit 233 to yr="2006 ‐Current"
235. limit 233 to yr="1928 ‐ 2005"
236. (ae or co or si or to).fs.
237. (safe or safety or unsafe).tw.
238. (side effect* or side event*).tw.
239. ((adverse or undesirable or harm* or injurious or serious or toxic) adj3 (effect* or event* or reaction* or incident* or outcome*)).tw.
240. (abnormalit* or toxicit* or complication* or consequence* or noxious or tolerabilit*).tw.
241. or/236‐240
242. 184 and 241
243. limit 242 to yr="2006 ‐Current"
244. limit 242 to yr="1928 ‐ 2005"
245. limit 203 to em=201027‐201216
246. limit 211 to em=201027‐201216
247. limit 233 to em=201027‐201216
248. limit 242 to em=201027‐201216
CENTRAL (Ovid)
Last Update November 2014; research librarian: Maurine Rice, McMaster University
1 Neck Pain/
2 exp Brachial Plexus Neuropathies/
3 exp neck injuries/ or exp whiplash injuries/
4 cervical pain.mp.
5 neckache.mp.
6 whiplash.mp.
7 cervicodynia.mp.
8 cervicalgia.mp.
9 brachialgia.mp.
10 brachial neuritis.mp.
11 brachial neuralgia.mp.
12 neck pain.mp.
13 neck injur*.mp.
14 brachial plexus neuropath*.mp.
15 brachial plexus neuritis.mp.
16 thoracic outlet syndrome/ or cervical rib syndrome/
17 Torticollis/
18 exp brachial plexus neuropathies/ or exp brachial plexus neuritis/
19 cervico brachial neuralgia.ti,ab.
20 cervicobrachial neuralgia.ti,ab.
21 (monoradicul* or monoradicl*).tw.
22 or/1‐21
23 exp headache/ and cervic*.tw.
24 exp genital diseases, female/
25 genital disease*.mp.
26 or/24‐25
27 23 not 26
28 22 or 27
29 neck/
30 neck muscles/
31 exp cervical plexus/
32 exp cervical vertebrae/
33 atlanto‐axial joint/
34 atlanto‐occipital joint/
35 Cervical Atlas/
36 spinal nerve roots/
37 exp brachial plexus/
38 (odontoid* or cervical or occip* or atlant*).tw.
39 axis/ or odontoid process/
40 Thoracic Vertebrae/
41 cervical vertebrae.mp.
42 cervical plexus.mp.
43 cervical spine.mp.
44 (neck adj3 muscles).mp.
45 (brachial adj3 plexus).mp.
46 (thoracic adj3 vertebrae).mp.
47 neck.mp.
48 (thoracic adj3 spine).mp.
49 (thoracic adj3 outlet).mp.
50 trapezius.mp.
51 cervical.mp.
52 cervico*.mp.
53 51 or 52
54 exp genital diseases, female/
55 genital disease*.mp.
56 exp *Uterus/
57 54 or 55 or 56
58 53 not 57
59 29 or 30 or 31 or 32 or 33 or 34 or 35 or 36 or 37 or 38 or 39 or 40 or 41 or 42 or 43 or 44 or 45 or 46 or 47 or 48 or 49 or 50 or 58
60 exp pain/
61 exp injuries/
62 pain.mp.
63 ache.mp.
64 sore.mp.
65 stiff.mp.
66 discomfort.mp.
67 injur*.mp.
68 neuropath*.mp.
69 or/60‐68
70 59 and 69
71 Radiculopathy/
72 exp temporomandibular joint disorders/ or exp temporomandibular joint dysfunction syndrome/
73 myofascial pain syndromes/
74 exp "Sprains and Strains"/
75 exp Spinal Osteophytosis/
76 exp Neuritis/
77 Polyradiculopathy/
78 exp Arthritis/
79 Fibromyalgia/
80 spondylitis/ or discitis/
81 spondylosis/ or spondylolysis/ or spondylolisthesis/
82 radiculopathy.mp.
83 radiculitis.mp.
84 temporomandibular.mp.
85 myofascial pain syndrome*.mp.
86 thoracic outlet syndrome*.mp.
87 spinal osteophytosis.mp.
88 neuritis.mp.
89 spondylosis.mp.
90 spondylitis.mp.
91 spondylolisthesis.mp.
92 or/71‐91
93 59 and 92
94 exp neck/
95 exp cervical vertebrae/
96 Thoracic Vertebrae/
97 neck.mp.
98 (thoracic adj3 vertebrae).mp.
99 cervical.mp.
100 cervico*.mp.
101 99 or 100
102 exp genital diseases, female/
103 genital disease*.mp.
104 exp *Uterus/
105 or/102‐104
106 101 not 105
107 (thoracic adj3 spine).mp.
108 cervical spine.mp.
109 94 or 95 or 96 or 97 or 98 or 106 or 107 or 108
110 Intervertebral Disk/
111 (disc or discs).mp.
112 (disk or disks).mp.
113 110 or 111 or 112
114 109 and 113
115 herniat*.mp.
116 slipped.mp.
117 prolapse*.mp.
118 displace*.mp.
119 degenerat*.mp.
120 (bulge or bulged or bulging).mp.
121 115 or 116 or 117 or 118 or 119 or 120
122 114 and 121
123 intervertebral disk degeneration/ or intervertebral disk displacement/
124 intervertebral disk displacement.mp.
125 intervertebral disc displacement.mp.
126 intervertebral disk degeneration.mp.
127 intervertebral disc degeneration.mp.
128 123 or 124 or 125 or 126 or 127
129 109 and 128
130 28 or 70 or 93 or 122 or 129
131 animals/ not (animals/ and humans/)
132 130 not 131
133 exp *neoplasms/
134 exp *wounds, penetrating/
135 133 or 134
136 132 not 135
137 Neck Pain/rh, th [Rehabilitation, Therapy]
138 exp Brachial Plexus Neuropathies/rh, th
139 exp neck injuries/rh, th or exp whiplash injuries/rh, th
140 thoracic outlet syndrome/rh, th or cervical rib syndrome/rh, th
141 Torticollis/rh, th
142 exp brachial plexus neuropathies/rh, th or exp brachial plexus neuritis/rh, th
143 or/137‐142
144 Radiculopathy/rh, th
145 exp temporomandibular joint disorders/rh, th or exp temporomandibular joint dysfunction syndrome/rh, th
146 myofascial pain syndromes/rh, th
147 exp "Sprains and Strains"/rh, th
148 exp Spinal Osteophytosis/rh, th
149 exp Neuritis/rh, th
150 Polyradiculopathy/rh, th
151 exp Arthritis/rh, th
152 Fibromyalgia/rh, th
153 spondylitis/rh, th or discitis/rh, th
154 spondylosis/rh, th or spondylolysis/rh, th or spondylolisthesis/rh, th
155 or/144‐154
156 59 and 155
157 acupuncture/ or chiropractic/
158 exp Musculoskeletal Manipulations/
159 massage.tw.
160 mobili?ation.tw.
161 Acupuncture Therapy/
162 (acupuncture or acu‐puncture or needling or acupressure or mox?bustion).tw.
163 ((neck or spine or spinal or cervical or chiropractic* or musculoskeletal* or musculo‐skeletal*) adj3 (adjust* or manipulat* or mobiliz* or mobilis*)).tw.
164 (manual adj therap*).tw.
165 (manipulati* adj (therap* or medicine)).tw.
166 (massag* or reflexolog* or rolfing or zone therap*).tw.
167 Nimmo.mp.
168 exp Vibration/tu [Therapeutic Use]
169 (vibration adj5 (therap* or treatment*)).tw.
170 (Chih Ya or Shiatsu or Shiatzu or Zhi Ya).tw.
171 (flexion adj2 distraction*).tw.
172 (myofascial adj3 (release or therap*)).tw.
173 muscle energy technique*.tw.
174 trigger point.tw.
175 proprioceptive Neuromuscular Facilitation*.tw.
176 cyriax friction.tw.
177 (lomilomi or lomi‐lomi or trager).tw.
178 aston patterning.tw.
179 (strain adj counterstrain).tw.
180 (craniosacral therap* or cranio‐sacral therap*).tw.
181 (amma or ammo or effleuurage or petrissage or hacking or tapotment).tw.
182 Complementary Therapies/
183 ((complement* or alternat* or osteopthic*) adj (therap* or medicine)).tw.
184 (Tui Na or Tuina).tw.
185 or/157‐184
186 136 and 185
187 143 or 156 or 186
188 animals/ not (animals/ and humans/)
189 187 not 188
190 limit 189 to yr="2010 ‐ 2012"
CINAHL (EBSCO)
Last Update November 2014; research librarian: Maurine Rice, McMaster University
S139 S115 and S131 Limiters ‐ Published Date: 20121231‐20140330 S138 S115 and S131 S137 S109 and S131 Limiters ‐ Published Date: 20121231‐20140330 S136 S109 and S131 S135 S94 and S131 Limiters ‐ Published Date: 20121231‐20140330 S134 S94 and S131 S133 S91 and S131 Limiters ‐ Published Date: 20121231‐20140330 S132 S91 and S131 S131 S82 and S130 S130 S116 or S117 or S118 or S119 or S120 or S121 or S122 or S123 or S124 or S125 or S126 or S127 or S128 or S129 S129 TX ( ((complement* or alternat* or osteopthic*) N1 (therap* or medicine)) ) OR TX ( (Tui Na or Tuina) ) S128 TX (strain N1 counterstrain) OR TX ( (craniosacral therap* or cranio‐sacral therap*) ) OR TX ( (amma or ammo or effleuurage or petrissage or hacking or tapotment) ) S127 TX cyriax friction OR TX ( (lomilomi or lomi‐lomi or trager) ) OR TX aston patterning S126 TX muscle energy technique* OR TX trigger point OR TX proprioceptive Neuromuscular Facilitation* S125 TX ( (Chih Ya or Shiatsu or Shiatzu or Zhi Ya) ) OR TX (flexion N2 distraction*) OR TX ( (myofascial N3 (release or therap*)) ) S124 (MH "Vibration/TU") S123 TX ( (massag* or reflexolog* or rolfing or zone therap*) ) OR TX Nimmo OR TX ( (vibration N5 (therap* or treatment*)) ) S122 TX (manipulati* N1 (therap* or medicine)) S121 TX ((neck or spine or spinal or cervical or chiropractic* or musculoskeletal* or musculo‐skeletal*) N3 (adjust* or manipulat* or mobiliz* or mobilis*)) S120 TX mobili?ation OR TX ( (acupuncture or acu‐puncture or needling or acupressure or mox?bustion) ) OR TX manual therapy S119 (MH "Massage+") OR (MH "Deep Tissue Massage") OR (MH "Neuromuscular Massage") OR (MH "Sports Massage") OR (MH "Massage Therapists") OR (MH "Swedish Massage") S118 (MH "Manipulation, Chiropractic") OR (MH "Manual Therapy+") S117 (MH "Chiropractic+") OR (MH "Manipulation, Chiropractic") OR (MH "Chiropractic Practice") OR (MH "Chiropractors") S116 (MH "Acupuncture+") OR (MH "Acupuncture Points") OR (MH "Acupuncturists") S115 S110 or S111 or S112 or S113 or S114 S114 TX toxic reaction OR TX allergic reaction OR TX complications Limiters ‐ Published Date: 20100101‐20121231 S113 TX adverse outcome* OR TX adverse incident* Limiters ‐ Published Date: 20100101‐20121231 S112 TX adverse event* OR TX adverse effect* OR TX adverse reaction* Limiters ‐ Published Date: 20100101‐20121231 S111 TX ( (safe or safety or unsafe) ) OR TX ( (side effect* or side event*) ) Limiters ‐ Published Date: 20100101‐20121231 S110 (MH "Adverse Drug Event") Limiters ‐ Published Date: 20100101‐20121231 S109 S95 or S96 or S97 or S98 or S99 or S100 or S101 or S102 or S103 or S104 or S105 or S106 or S107 or S108 S108 TX PsycINFO or TX psycLIT or TX PsychINFO or TX psychLIT or TX CINAHL S107 TX cochrane or TX pubmed or TX pub med or TX medline or TX embase S106 TX mantel haenszel S105 TX data N2 pool* or TX analys* N2 pool* S104 TX data N2 abstract* or TX data N2 extract* S103 TX electronic N2 database* or TX bibliographic database* S102 TX hand N2 search* or TX manual N2 search S101 TX hta or TX htas or TX technology assessment* S100 TX methodologic* N3 review* or TX methodologic* N3 overview* S99 TX systematic* N3 review* or TX systematic* N3 overview* S98 TX quantitative research or TX quantitative review* or TX quantitative overview* S97 TX meta analy* or TX metaanaly* or TX met analy* or TX metanaly* S96 (MH "Meta Analysis") S95 PT systematic review S94 S92 or S93 S93 TI guideline* or TI guidance or TI recommendations or TI consensus S92 (MH "Practice Guidelines") S91 S83 or S84 or S85 or S86 or S87 or S88 or S89 or S90 S90 TX control* N2 study or TX control* N2 studies or TX control N2 trial* S89 TX RCT or TX RCTs S88 TX (singl* N1 (blind* OR dumm* OR mask*)) S87 (MH "Random Sample+") S86 (MH "Placebos") S85 TX random* or TX sham or TX placebo* S84 PT clinical trial or PT randomized controlled trial S83 (MH "Clinical Trials+") S82 S78 NOT S81 S81 S79 or S80 S80 (MM "Pregnancy+") S79 (MM "Abortion, Induced+") S78 S74 NOT S77 S77 S75 or S76 S76 (MM "Wounds, Penetrating+") S75 (MM "Neoplasms+") S74 S16 or S41 or S56 or S69 or S73 S73 S63 and S72 S72 S70 or S71 S71 TX intervertebral disk displacement or TX intervertebral disc displacement or TX intervertebral disk degeneration or TX intervertebral disc degeneration S70 (MH "Intervertebral Disk Displacement") S69 S67 and S68 S68 TX herniat* or TX slipped or TX prolapse* or TX displace* or TX degenerat* or TX ( bulged OR bulge OR bulging ) S67 S63 and S66 S66 S64 or S65 S65 TX disc or TX discs or TX disk or TX disks S64 (MH "Intervertebral Disk") S63 S61 NOT S62 S62 (MM "Genital Diseases, Female+") or ( (MM "Cervix") or (MM "Cervix Diseases") ) S61 S57 or S58 or S59 or S60 S60 TX thoracic N3 spine or TX cervical spine or TX cervico* S59 TX neck or TX thoracic N3 vertebr* S58 (MH "Thoracic Vertebrae") S57 (MH "Neck") S56 S34 and S55 S55 S42 or S43 or S44 or S45 or S46 or S47 or S48 or S49 or S50 or S51 or S52 or S53 or S54 S54 TX neuritis or TX spondylosis or TX spondylitis or TX spondylolisthesis S53 TX myofascial pain syndome* or TX thoracic outlet syndrome* or TX spinalosteophytosis S52 TX radiculopathy or TX radiculitis or TX temporomandibular S51 (MH "Spondylolysis") or (MH "Spondylolisthesis+") S50 (MH "Fibromyalgia") S49 (MH "Arthritis+") S48 (MH "Polyradiculopathy") S47 (MH "Neuritis+") S46 (MH "Spinal Osteophytosis") S45 (MH "Sprains and Strains+") S44 (MH "Myofascial Pain Syndromes+") S43 (MH "Temporomandibular Joint Diseases+") or (MH "Temporomandibular Joint Syndrome") S42 (MH "Radiculopathy") S41 S34 and S40 S40 S35 or S36 or S37 or S38 or S39 S39 (MH "Neuralgia") S38 TX stiff or TX discomfort or TX injur* or TX neuropath* S37 TX pain or TX ache* or TX sore S36 (MH "Wounds and Injuries+") S35 (MH "Pain+") S34 S33 NOT S32 S33 S17 or S18 or S19 or S20 or S21 or S22 or S23 or S24 or S25 or S26 or S27 or S28 or S29 or S30 or S31 S32 (MM "Genital Diseases, Female+") or ( (MM "Cervix") or (MM "Cervix Diseases") ) S31 TX trapezius or TX cervico* S30 TX thoracic N3 spine or TX thoracic N3 outlet S29 TX neck S28 TX thoracic N3 verteb* S27 TX brachial N3 plexus S26 TX neck n3 muscles S25 (MH "Thoracic Vertebrae") S24 TX ondontoid* or TX cervical or TX occip* or TX atlant* S23 (MH "Brachial Plexus+") S22 (MH "Spinal Nerve Roots+") S21 (MH "Atlanto‐Axial Joint") or (MH "Atlanto‐Occipital Joint") S20 (MH "Cervical Vertebrae+") or (MH "Cervical Atlas") S19 (MH "Cervical Plexus+") S18 (MH "Neck") S17 (MH "Neck Muscles+") S16 S10 or S15 S15 S11 NOT S14 S14 S12 or S13 S13 (MM "Cervix") or (MM "Cervix Diseases") S12 (MM "Genital Diseases, Female+") S11(MH "Headache+") and TX cervic* S10 S1 or S2 or S3 or S4 or S5 or S6 or S7 or S8 or S9 S9 (MH "Brachial Plexus Neuritis") S8 TX cervical brachial neuralgia S7 TX cervical rib sydrome* or TX cervico brachial neuralgia or TX cervicobrachial neuralgia or TX monoradicul* or TX monoradicl* S6 (MH "Thoracic Outlet Syndrome") or (MH "Torticollis") S5 TX brachial neuralgia or TX neck pain or TX neck injur* or TX brachial plexus neuropath* or TX brachial plexus neuralgia or TX brachial plexus neuritis S4 TX cervicalgia or TX brachialgia or TX brachial neuritis S3 TX cervical pain or TX neckache or TX neck ache or TX whiplash or TX cervicodynia S2 (MH "Neck Injuries+") S1 (MH "Neck Pain") or (MH "Brachial Plexus Neuropathies") or (MH "Brachial Plexus Neuritis")
MANTIS (Ovid)
Last update May 2014; librarian: Dela Shupe, Northwestern Health Science University
1 neck pain.mp. [mp=title, abstract, descriptors]
2 brachial plexus neuropathies.mp. [mp=title, abstract, descriptors]
3 neck injuries.mp. [mp=title, abstract, descriptors]
4 cervical pain.mp. [mp=title, abstract, descriptors]
5 neckache.mp. [mp=title, abstract, descriptors]
6 whiplash.mp. [mp=title, abstract, descriptors]
7 cervicodynia.mp. [mp=title, abstract, descriptors]
8 cervicalgia.mp. [mp=title, abstract, descriptors]
9 brachialgia.mp. [mp=title, abstract, descriptors]
10 brachial neuritis.mp. [mp=title, abstract, descriptors]
11 brachial neuralgia.mp. [mp=title, abstract, descriptors]
12 brachial plexus neuropath*.mp. [mp=title, abstract, descriptors]
13 brachial plexus neuritis.mp. [mp=title, abstract, descriptors]
14 (thoracic outlet syndrome or cervical rib syndrome).mp. [mp=title, abstract, descriptors]
15 torticollis.mp. [mp=title, abstract, descriptors]
16 cervico brachial neuralgia.mp. [mp=title, abstract, descriptors]
17 (monoradicul* or monoradicl*).tw.
18 or/1‐17
19 headache.mp. and cervic*.tw. [mp=title, abstract, descriptors]
20 genital diseases, female.mp. [mp=title, abstract, descriptors]
21 genital disease*.mp. [mp=title, abstract, descriptors]
22 or/20‐21
23 19 not 22
24 18 or 23
25 neck.mp. [mp=title, abstract, descriptors]
26 neck muscles.mp. [mp=title, abstract, descriptors]
27 cervical plexus.mp. [mp=title, abstract, descriptors]
28 cervical vertebrae.mp. [mp=title, abstract, descriptors]
29 atlanto‐axial joint.mp. [mp=title, abstract, descriptors]
30 atlanto‐occipital joint.mp. [mp=title, abstract, descriptors]
31 cervical atlas.mp. [mp=title, abstract, descriptors]
32 spinal nerve roots.mp. [mp=title, abstract, descriptors]
33 brachial plexus.mp. [mp=title, abstract, descriptors]
34 (odontoid* or cervical or occip* or atlant*).tw.
35 (axis or odontoid process).mp. [mp=title, abstract, descriptors]
36 thoracic vertebrae.mp. [mp=title, abstract, descriptors]
37 cervical vertebrae.mp. [mp=title, abstract, descriptors]
38 cervical plexus.mp. [mp=title, abstract, descriptors]
39 cervical spine.mp. [mp=title, abstract, descriptors]
40 (neck adj3 muscles).mp. [mp=title, abstract, descriptors]
41 (brachial adj3 plexus).mp. [mp=title, abstract, descriptors]
42 (thoracic adj3 vertebrae).mp. [mp=title, abstract, descriptors]
43 (thoracic adj3 spine).mp. [mp=title, abstract, descriptors]
44 (thoracic adj3 outlet).mp. [mp=title, abstract, descriptors]
45 trapezius.mp. [mp=title, abstract, descriptors]
46 cervical.mp. [mp=title, abstract, descriptors]
47 cervico*.mp. [mp=title, abstract, descriptors]
48 46 or 47
49 genital diseases, female.mp. [mp=title, abstract, descriptors]
50 genital disease*.mp. [mp=title, abstract, descriptors]
51 uterus.mp. [mp=title, abstract, descriptors]
52 49 or 50 or 51
53 48 not 52
54 25 or 26 or 27 or 28 or 29 or 30 or 31 or 32 or 33 or 34 or 35 or 36 or 37 or 38 or 39 or 40 or 41 or 42 or 43 or 44 or 45 or 53
55 pain.mp. [mp=title, abstract, descriptors]
56 injuries.mp. [mp=title, abstract, descriptors]
57 ache.mp. [mp=title, abstract, descriptors]
58 sore.mp. [mp=title, abstract, descriptors]
59 stiff.mp. [mp=title, abstract, descriptors]
60 discomfort.mp. [mp=title, abstract, descriptors]
61 injur*.mp. [mp=title, abstract, descriptors]
62 neuropath*.mp. [mp=title, abstract, descriptors]
63 or/55‐62
64 54 and 63
65 radiculopathy.mp. [mp=title, abstract, descriptors]
66 (temporomandibular joint disorders or temporomandibular joint dysfunction syndrome).mp. [mp=title, abstract, descriptors]
67 myofascial pain syndromes.mp. [mp=title, abstract, descriptors]
68 "sprains and strains".mp. [mp=title, abstract, descriptors]
69 spinal osteophytosis.mp. [mp=title, abstract, descriptors]
70 neuritis.mp. [mp=title, abstract, descriptors]
71 polyradiculopathy.mp. [mp=title, abstract, descriptors]
72 arthritis.mp. [mp=title, abstract, descriptors]
73 fibromyalgia.mp. [mp=title, abstract, descriptors]
74 (spondylitis or discitis).mp. [mp=title, abstract, descriptors]
75 (spondylosis or spondylolysis or spondylolisthesis).mp.,[mp=title, abstract, descriptors]
76 radiculitis.mp. [mp=title, abstract, descriptors]
77 tempomandibular.mp. [mp=title, abstract, descriptors]
78 myofascial pain syndrome*.mp. [mp=title, abstract, descriptors]
79 thoracic outlet syndrome*.mp. [mp=title, abstract, descriptors]
80 spinal osteophytosis.mp. [mp=title, abstract, descriptors]
81 neuritis.mp. [mp=title, abstract, descriptors]
82 spondylosis.mp. [mp=title, abstract, descriptors]
83 spondylitis.mp. [mp=title, abstract, descriptors]
84 spondylolisthesis.mp. [mp=title, abstract, descriptors]
85 or/65‐84
86 54 and 85
87 neck.mp. [mp=title, abstract, descriptors]
88 cervical vertebrae.mp. [mp=title, abstract, descriptors]
89 thoracic vertebrae.mp. [mp=title, abstract, descriptors]
90 (thoracic adj3 vertebrae).mp. [mp=title, abstract, descriptors]
91 cervical.mp. [mp=title, abstract, descriptors]
92 cervico*.mp. [mp=title, abstract, descriptors]
93 91 or 92
94 genital diseases, female.mp. [mp=title, abstract, descriptors]
95 genital disease*.mp. [mp=title, abstract, descriptors]
96 uterus.mp. [mp=title, abstract, descriptors]
97 or/94‐96
98 93 not 97
99 (thoracic adj3 spine).mp. [mp=title, abstract, descriptors]
100 cervical spine.mp. [mp=title, abstract, descriptors]
101 87 or 88 or 89 or 90 or 98 or 99 or 100
102 intervertebral disk.mp. [mp=title, abstract, descriptors]
103 (disc or discs).mp. [mp=title, abstract, descriptors]
104 (disk or disks).mp. [mp=title, abstract, descriptors]
105 102 or 103 or 104
106 101 and 105
107 herniat*.mp. [mp=title, abstract, descriptors]
108 slipped.mp. [mp=title, abstract, descriptors]
109 prolapse*.mp. [mp=title, abstract, descriptors]
110 displace*.mp. [mp=title, abstract, descriptors]
111 degenerat*.mp. [mp=title, abstract, descriptors]
112 (bulge or bulged or bulging).mp. [mp=title, abstract, descriptors]
113 107 or 108 or 109 or 110 or 111 or 112
114 106 and 113
115 intervertebral disk displacement.mp. [mp=title, abstract, descriptors]
116 intervertebral disc displacement.mp. [mp=title, abstract, descriptors]
117 intervertebral disk degeneration.mp. [mp=title, abstract, descriptors]
118 intervertebral disc degeneration.mp. [mp=title, abstract, descriptors]
119 115 or 116 or 117 or 118
120 101 and 119
121 24 or 64 or 86 or 106 or 114 or 120
122 (animals not (animals and humans)).mp. [mp=title, abstract, descriptors]
123 121 not 122
124 neoplasms.mp. [mp=title, abstract, descriptors]
125 wounds, penetrating.mp. [mp=title, abstract, descriptors]
126 124 or 125
127 123 not 126
128 rehabilitation.mp. [mp=title, abstract, descriptors]
129 therapy.mp. [mp=title, abstract, descriptors]
130 128 or 129
131 (neck pain or brachial plexus neuropathies or neck injuries or whiplash or thoracic outlet syndrome or cervical rib syndrome or torticollis
or brachial plexus neuritis).mp. [mp=title, abstract, descriptors]
132 (temporomandibular joint disorder or temporomandibular joint dysfunction syndrome).mp. [mp=title, abstract, descriptors]
133 (myofascial pain syndromes or "sprains and strains").mp. [mp=title, abstract, descriptors]
134 (radiculopathy or osteophytosis or neuritis or polyradiculopathy or arthritis or fibromyalgia or spondylitis or spondylosis or spondylolysis or spondylolisthesis).mp.
135 131 or 132 or 133 or 134
136 130 and 135
137 54 and 136
138 (acupuncture or chiropractic).mp. [mp=title, abstract, descriptors]
139 musculoskeletal manipulation*.mp. [mp=title, abstract, descriptors]
140 massage.mp. [mp=title, abstract, descriptors]
141 mobili?ation.mp. [mp=title, abstract, descriptors]
142 acupuncture therapy.mp. [mp=title, abstract, descriptors]
143 (acupuncture or acu‐puncture or needling or acupressure or mox?bustion).mp. [mp=title, abstract, descriptors]
144 ((neck or spine or spinal or cervical or chiropractic* or musculoskeletal*) adj3 (adjust* or manipulat* or mobiliz* or mobilis*)).mp. [mp=title, abstract, descriptors]
145 (manual adj therap*).mp. [mp=title, abstract, descriptors]
146 (manipulati* adj (therap* or medicine)).mp. [mp=title, abstract, descriptors]
147 (massag* or reflexolog* or rolfing or zone therap*).mp. [mp=title, abstract, descriptors]
148 Nimmo.mp. [mp=title, abstract, descriptors]
149 vibration therapy.mp. [mp=title, abstract, descriptors]
150 (vibration adj5 (therap* or treatment*)).mp. [mp=title, abstract, descriptors]
151 (ChihYa or Shiatsu or Shiatzu or ZhiYa).mp. [mp=title, abstract, descriptors]
152 (flexion adj2 distraction*).mp. [mp=title, abstract,descriptors]
153 (myofascial adj3 (release or therap*)).mp. [mp=title, abstract, descriptors]
154 muscle energy technique*.mp. [mp=title, abstract, descriptors]
155 trigger point.mp. [mp=title, abstract, descriptors]
156 proprioceptive neuromuscular facilitation*.mp. [mp=title, abstract, descriptors]
157 cyriax friction.mp. [mp=title, abstract, descriptors]
158 (lomilomi or lomi‐lomi or trager).mp. [mp=title, abstract, descriptors]
159 aston patterning.mp. [mp=title, abstract, descriptors]
160 (strain adj counterstrain).mp. [mp=title, abstract, descriptors]
161 (craniosacraltherap* or cranio‐sacral therap* or craniosacral therap*).mp. [mp=title, abstract, descriptors]
162 (amma or ammo or effleuurage or effleurage or petrissage or hacking or tapotment).mp. [mp=title, abstract, descriptors]
163 complementary therapies.mp. [mp=title, abstract, descriptors]
164 ((complement* or alternat* or osteopathic*) adj (therap* or medicine)).mp. [mp=title, abstract, descriptors]
165 (Tui Na or Tuina).mp. [mp=title, abstract, descriptors]
166 or/138‐165
167 127 and 166
168 136 or 137 or 167
169 (animals not (animals and humans)).mp. [mp=title, abstract, descriptors]
170 168 not 169
171 randomized controlled trial*.mp. [mp=title, abstract, descriptors]
172 controlled clinical trial*.mp. [mp=title, abstract, descriptors]
173 (random* or sham or placebo*).mp. [mp=title, abstract, descriptors]
174 placebos.mp. [mp=title, abstract, descriptors]
175 random allocation.mp. [mp=title, abstract, descriptors]
176 single blind method.mp. [mp=title, abstract, descriptors]
177 double blind method.mp. [mp=title, abstract, descriptors]
178 ((singl* or doubl* or trebl* or tripl*) adj25 (blind* or dumm* or mask*)).mp. [mp=title, abstract, descriptors]
179 (rct or rcts).mp. [mp=title, abstract, descriptors]
180 (control* adj2 (study or studies or trial*)).mp. [mp=title, abstract, descriptors]
181 or/171‐180
182 170 and 181
183 (guideline* or practice guideline*).mp. [mp=title, abstract, descriptors]
184 (guideline* or guidance* or recommendation*).ti.
185 consensus.ti.
186 183 or 184 or 185
187 170 and 186
188 meta‐analysis.mp. [mp=title, abstract, descriptors]
189 (metaanaly* or meta analy* or met analy* or metanaly*).mp. [mp=title, abstract, descriptors]
190 (collaborative research or collaborative review* or collaborative overview*).mp. [mp=title, abstract, descriptors]
191 (integrative research or integrative review* or integrative overview*).mp. [mp=title, abstract, descriptors]
192 (quantitative adj3 (research or review* or overview*)).mp. [mp=title, abstract, descriptors]
193 (research integration or research overview*).mp. [mp=title, abstract, descriptors]
194 (systematic* adj3 (review* or overview*)).mp. [mp=title, abstract, descriptors]
195 (methodologic* adj3 (review* or overview*)).mp. [mp=title, abstract, descriptors]
196 technology assessment biomedical.mp. [mp=title, abstract, descriptors]
197 (hta or thas or technology assessment*).mp. [mp=title, abstract, descriptors]
198 ((hand adj2 search*) or (manual* adj search*)).mp. [mp=title, abstract, descriptors]
199 ((electronic adj database*) or (bibliographic* adj database*)).mp. [mp=title, abstract, descriptors]
200 ((data adj2 abstract*) or (data adj2 extract*)).mp. [mp=title, abstract, descriptors]
201 (analys* adj3 (pool or pooled or pooling)).mp. [mp=title, abstract, descriptors]
202 mantel haenszel.mp. [mp=title, abstract, descriptors]
203 (cochrane or pubmed or pub med or medline or embase or psycinfo or psyclit or psychinfo or psychlit or cinahl or science citation index).ab.
204 or/188‐203
205 170 and 204
206 182 or 187 or 205 (
207 limit 206 to yr="2009 ‐Current"
Index to chiropractic literature
Jan 10 2014; Librarian: Dela Shupe, Northwestern Health Science University
S1 Subject: "BACK PAIN" OR "BACK INJURIES" OR "NECK INJURIES" OR "NECK PAIN" OR "SPINAL DISEASES" OR "SPINAL INJURIES" OR "SCIATICA" OR All Fields:backpain* or backache* OR "back pain" OR "back ache" OR "back pains" OR "back aches" OR neckpain* OR neckache* OR "neck pain" OR neck ache" OR "neck pains" OR "neck aches" OR All Fields:Spondylolys* or spondylolisthes* or Spondylisthes* or Discitis or diskitis or Spondylod* OR Sciatica OR ischialgia* OR cervicalgia OR Cervicodynia
S2 All Fields:whiplash* or "whip lash" OR "whip lashes" or radiculomyelopath* or "radiculo‐myelopathy" OR "radiculo‐myelopathies" OR All Fields:"failed back" or "back surgery syndrome" or "back surgery syndromes" or FBSS OR All Fields:lumbago or dorsalgia or "myofascial pain" OR "myofascial ache"
S3 All Fields:"cervical pain" OR "cervical ache" OR "vertebrogenic pain syndrome" OR "vertebrogenic pain syndromes" OR All Fields:"degenerated disk" OR "degenerative disk" OR "degenerated disks" OR "degenerative disks" OR All Fields:"degenerated disc" OR "degenerative disc OR "degenerated discs" OR "degenerative discs"
S4 All Fields:"prolapsed disk" OR "prolapsed disks" OR "prolapsed disc" OR "prolapsed discs" OR "disk prolapse" OR "disc prolapse" "herniated disk" OR "herniated disks" OR "herniated disc" OR "herniated discs" OR All Fields:"displaced disk" OR "displaced disks" OR "displaced disc" OR "displaced discs" OR "osteoporotic compression fracture" OR "osteoporotic compression fractures" OR All Fields::"lumbar stenosis" OR "lumbar stenoses" OR "spinal stenosis" OR "spinal stenoses" OR "cervicogenic headache" OR "cervicogenic headaches" OR "cervico‐genic headache" OR "cervico‐genic headaches"
S5 All Fields:radiculomyelopathy OR radiculomyelopathies OR "radiculo‐myelopathy" OR "radiculo‐myelopathies" OR All Fields:"Zygapophyseal joint syndrome" OR "Zygapophyseal joint syndromes" OR "Z‐joint syndrome" OR "Z‐joint syndromes" OR "facet joint syndrome" OR "facet joint syndromes" OR All Fields:"thoracic pain" OR "thoracic ache" OR "spinal pain" OR "spinal ache" OR "lumbar pain" OR "lumbar ache"
S6 S1 OR S2 OR S3 OR S4 OR S5
S7 Subject:"ACUPUNCTURE" OR "ACUPRESSURE" OR "ACUPUNCTURE THERAPY" OR "ELECTROACUPUNCTURE" OR "MANIPULATION, LUMBAR" OR "MANIPULATION, CERVICAL" OR "MANIPULATION, CHIROPRACTIC" OR "MANIPULATION, SPINAL" OR "MANIPULATION, THORACIC" OR Subject:"MASSAGE" OR "CHIROPRACTIC" OR All Fields:acupuncture or "acu‐puncture" or electroacupuncture or "electro‐acupuncture" or "electric acupuncture" or "electric acu‐puncture" or needling or acupressure or "acu‐pressure" or moxibustion or moxabustion
S8 All Fields:"manual therapy" OR "manual therapies" OR massag* or reflexolog* or rolfing or "zone therapy" or "zone therapies" OR All Fields:"Chih Ya" or Shiatsu or Shiatzu or "Zhi Ya" or "Flexion distraction" OR "Trigger point" OR "Trigger points" OR "Proprioceptive Neuromuscular Facilitation" OR "Proprioceptive Neuromuscular Facilitations" OR All Fields:"myofascial release" or "myofascial therapy" OR "myofascial therapies" OR "Muscle energy technique" OR "Muscle energy techniques" OR "Cyriax Friction"
S9 All Fields:: Lomilomi or "lomi‐lomi" or trager or "Aston patterning" or "Strain counterstrain" or "Alexander technique" or "Alexander techniques" or "Tui Na" or Tuina OR All Fields:Craniosacral Therapy" or "Craniosacral Therapies" or "Cranio‐sacral Therapy"or "Cranio‐sacral Therapies" or amma or ammo or Effleurage or Petrissage or hacking or Tapotment OR All Fields:manipulat* or mobiliz* or mobilis*
S10 All Fields:"complementary therapy" OR "complementary therapies" OR "complementary medicine" OR All Fields:"alternative therapy" OR "alternative therapies" OR "alternative medicine" OR All Fields:"osteopathic therapy" OR "osteopathic therapies" OR "osteopathic medicine"
S11 S7 OR S8 OR S9 OR S10
S12 S6 AND S11
S13 , Publication Type:Randomized Controlled Trial
S14 Subject:"RANDOMIZED CONTROLLED TRIALS AS TOPIC" OR "CONTROLLED CLINICAL TRIALS" OR "PLACEBOS" OR All Fields:random* or sham or placebo* or RCT or RCTs or CCT or CCTs OR All Fields:"controlled clinical trial" or "controlled clinical trials" or "controlled study" or "controlled studies" or "control study" or "controlled studies"
S15 S12 AND S14
S16 S13 OR S15
Appendix 2. Criteria for a judgement of yes for sources of risk of bias
1. Was the method of randomisation adequate?
Was a random (unpredictable) assignment sequence used? Examples of adequate methods are coin toss (for studies with two groups), rolling a dice (for studies with two or more groups), drawing of balls of different colours, drawing of ballots with study group labels from a dark bag, computer‐generated random sequence, pre‐ordered sealed envelopes, sequentially ordered vials, telephone call to a central office and pre‐ordered list of treatment assignments.
Examples of inadequate methods include alternation, birth date, social insurance/security number, date on which individuals are invited to participate in the study and hospital registration number.
2. Was treatment allocation concealed?
Was assignment generated by an independent person not responsible for determining the eligibility of individuals. This person has no information about persons included in the trial and has no influence on the assignment sequence nor on the decision about eligibility of patients for participation.
Was knowledge of the allocated interventions adequately prevented during the study?
3. Was the participant blinded to the intervention?
This item should be scored “yes” if index and control groups are indistinguishable for participants, or if blinding was tested among participants and was found to be successful.
4. Was the care provider blinded to the intervention?
This item should be scored “yes” if index and control groups are indistinguishable for care providers, or if blinding was tested among care providers and was found to be successful
5. Was the outcome assessor blinded to the intervention?
Adequacy of blinding should be assessed for primary outcomes. This item should be scored “yes” if blinding was tested among outcome assessors and was found to be successful or:
for patient‐reported outcomes for which the participant is the outcome assessor (e.g. pain, disability): The blinding procedure is adequate for outcome assessors if participant blinding is scored “yes”;
for outcome criteria assessed during scheduled visits that suppose a contact between participants and outcome assessors (e.g. clinical examination): The blinding procedure is adequate if participants are blinded, and if treatment or adverse effects of treatment cannot be noticed during clinical examination;
for outcome criteria that do not suppose a contact with participants (e.g. radiography, magnetic resonance imaging): The blinding procedure is adequate if treatment or adverse effects of treatment cannot be noticed when the main outcome is assessed;
for outcome criteria that are clinical or therapeutic events that will be determined by the interaction between participants and care providers (e.g. co‐interventions, hospitalization length, treatment failure), in which the care provider is the outcome assessor: The blinding procedure is adequate for outcome assessors if the item for care providers is scored “yes”; and
for outcome criteria that are assessed from data of the medical forms: The blinding procedure is adequate if treatment or adverse effects of treatment cannot be noticed in extracted data.
Were incomplete outcome data adequately addressed?
6. Was the dropout rate described and acceptable?
The number of participants who were included in the study but did not complete the observation period or were not included in the analysis must be described and reasons given. If the percentage of withdrawals and dropouts does not exceed 20% for short‐term follow‐up, and 30% for long‐term follow‐up, and does not lead to substantial bias, a 'yes' is scored. (N.B. These percentages are arbitrary and are not supported by the literature.)
7. Were all randomly assigned participants analysed in the group to which they were allocated?
All randomly assigned participants are reported/analysed in the group to which they were allocated by randomisation for the most important moments of effect measurement (minus missing values), irrespective of non‐compliance and co‐interventions.
8. Are reports of the study free of the suggestion of selective outcome reporting?
To assign a ‘yes’, the review author determines if all results from all pre‐specified outcomes have been adequately reported in the published report of the trial. This information can be obtained by comparing the protocol versus the report or, in the absence of the protocol, by assessing whether the published report includes enough information to permit this judgement.
Other sources of potential bias
9. Were the groups similar at baseline regarding the most important prognostic indicators?
To receive a “yes”, groups have to be similar at baseline regarding demographic factors, duration and severity of complaints, percentage of participants with neurological symptoms and value of main outcome measure(s).
10. Were co‐interventions avoided or similar?
This item should be scored “yes” if no co‐interventions were provided, or if they were similar between index and control groups.
11. Was compliance acceptable in all groups?
The review author determines whether compliance with the interventions is acceptable, based on reported intensity, duration, number and frequency of sessions for both index interventions and control interventions. For example, physiotherapy treatment is usually administered over several sessions; therefore it is necessary to assess how many sessions each participant attended. For single‐session interventions (e.g. surgery), this item is irrelevant.
12. Was timing of the outcome assessment similar in all groups?
Timing of outcome assessment should be identical for all intervention groups and for all important outcome assessments.
Note: These instructions are adapted from van Tulder 2003 and from the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011).
Appendix 3. Data imputation rules
The preliminary assumption made for imputation of missing values is that data were missing completely at random (Little 1987). In other words, it was assumed that data were not missing as the result of factors confounded by the treatment effect.
As information was available only on change scores:
change score treatment (T) is the difference between follow‐up treatment pain score (mFT) and baseline treatment pain score (mBT); and
change score control (C) is the difference between follow‐up control pain score (mFC) and pre‐baseline control pain score (mBC).
| Baseline | Follow‐up | Difference | |
| Treatment | mBT | mFT | T = mFT ‐ mBT |
| Control | mBC | mFC | C = mFC ‐ mBC |
| EB = mBT ‐ mBC | EF = mFT ‐ mFC | E = T ‐ C |
If EB = 0, then EF is equal to E.
The mean difference was calculated with the assumption that no baseline differences in scores were present (EB = 00). For the conversion, the mean postscore difference was assumed to be due to differences in postscore values (EF), and then equals the post‐follow‐up difference (E).
Appendix 4. Grading the quality of evidence ‐ definition of domains
Study design refers to type of study (i.e. randomised, observational study).
Limitations in design (quality) refers to the 12 risk of bias criteria noted in Appendix 2.
Consistency refers to similarity of results across studies. When all studies are included in the meta‐analysis, ‘consistency’ is defined as absence of statistical heterogeneity. In the case that not all studies are combined in a meta‐analysis, ‘consistency’ is defined when all studies for the specific outcome lead to the same decision or recommendation, and ‘inconsistency’ is present if the results of two or more studies lead to clinically different decisions or recommendations. Review authors use their judgement to decide whether inconsistency is present when only one study leads to clinically different decisions or recommendations.
Directness (generalisability) refers to the extent to which the people, interventions and outcome measures are similar to those of interest.
Precision of the evidence relates to the numbers of studies, participants and events considered for each outcome. Imprecise data are defined as:
only one study for an outcome, regardless of the sample size or the confidence interval;
multiple studies combined in a meta‐analysis: The confidence interval is sufficiently wide that the estimate is consistent with conflicting recommendations. For rare events, one should consider the confidence interval around the risk difference rather than the confidence interval around the relative risk; and
multiple studies not combined in a meta‐analysis: The total sample size is underpowered to detect a clinically important difference between those who received the index intervention compared with those who received the control intervention. In this case, a post hoc sample size calculation should be performed to determine adequate sample size for each outcome.
Reporting (publication) bias should be considered present only if actual evidence of reporting bias rather than only speculation about reporting bias is found. The Cochrane Reporting Bias Methods Group describes the following types of reporting bias and definitions.
Publication bias: publication or non‐publication of research findings, depending on the nature and direction of results.
Time lag bias: rapid or delayed publication of research findings, depending on the nature and direction of results.
Language bias: publication of research findings in a particular language, depending on the nature and direction of results.
Funding bias: reporting of research findings, depending on how results align with the aspirations of the funding body.
Outcome variable selection bias: selective reporting of some outcomes but not others, depending on the nature and direction of research findings.
Developed country biases: non‐publication or non‐indication of findings, depending on whether study authors were based in developed or developing countries.
Data and analyses
Comparison 1. Manipulation versus placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 PAIN: cervical manipulation vs placebo | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.1 Single session: immediate‐ or short‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 PAIN: thoracic manipulation vs placebo | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 2.1 Single session: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
1.1. Analysis.
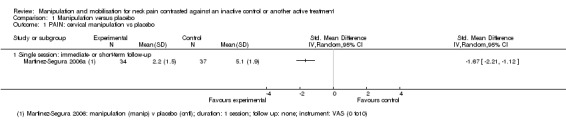
Comparison 1 Manipulation versus placebo, Outcome 1 PAIN: cervical manipulation vs placebo.
1.2. Analysis.
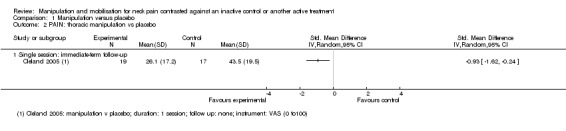
Comparison 1 Manipulation versus placebo, Outcome 2 PAIN: thoracic manipulation vs placebo.
Comparison 2. Manipulation versus control.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 PAIN: cervical manipulation vs control | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.1 Multiple sessions for chronic neck pain with HA: short‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 PAIN: cervical manipulation plus treatment vs same treatment in both arms | 2 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 2.1 Single session for subacute/chronic neck pain: immediate‐ or short‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Multiple sessions for subacute/chronic neck pain: short‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 PAIN: cervical manipulation vs same treatment in both arms | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 3.1 Single session for subacute/chronic neck pain with radicular findings and HA: short‐term follow‐up | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 PAIN: thoracic manipulation vs control | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.1 Single session for neck pain of not reported duration: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 PAIN: thoracic manipulation vs same treatment in both arms | 8 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 5.1 Multiple sessions for acute neck pain: immediate‐term follow‐up | 2 | 90 | Std. Mean Difference (IV, Random, 95% CI) | ‐3.46 [‐4.13, ‐2.79] |
| 5.2 Multiple sessions for chronic neck pain: immediate‐term follow‐up | 2 | 141 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.23 [‐1.15, 0.69] |
| 5.3 Single session for chronic neck pain: short‐term follow‐up | 1 | 82 | Std. Mean Difference (IV, Random, 95% CI) | 0.08 [‐0.36, 0.51] |
| 5.4 Multiple sessions for acute/subacute neck pain: short‐term follow‐up | 4 | 242 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.46 [‐2.20, ‐0.71] |
| 5.5 Multiple sessions for chronic neck pain: short‐term follow‐up | 1 | 104 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.60 [‐0.99, ‐0.20] |
| 5.6 Multiple sessions for chronic neck pain: intermediate‐term follow‐up | 1 | 103 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.64 [‐1.04, ‐0.25] |
| 6 PAIN: cervical and thoracic manipulation vs control | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6.1 Multiple sessions for chronic neck pain: long‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 FUNCTION: thoracic manipulation vs same treatment in both arms | 6 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 7.1 Multiple sessions for chronic neck pain: immediate‐term follow‐up | 2 | 141 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.52 [‐0.85, ‐0.18] |
| 7.2 Single session for chronic neck pain: short‐term follow‐up | 1 | 81 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.17 [‐0.61, 0.27] |
| 7.3 Multiple sessions for acute neck pain: short‐term follow‐up | 3 | 154 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.73 [‐2.68, ‐0.78] |
| 7.4 Multiple sessions for chronic neck pain: short‐term follow‐up | 1 | 104 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.50 [‐0.89, ‐0.10] |
| 7.5 Multiple sessions for chronic neck pain: intermediate‐term follow‐up | 1 | 103 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.38 [‐0.77, 0.01] |
| 8 FUNCTION: cervical manipulation vs same treatment in both arms | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 8.1 Multiple sessions for chronic neck pain: short‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 9 FUNCTION: cervical and thoracic manipulation vs control | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 9.1 Multiple sessions for chronic neck pain: long‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 10 QUALITY OF LIFE: thoracic manipulation vs control | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 10.1 Multiple sessions for chronic neck pain: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 10.2 Multiple sessions for chronic neck pain: short‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 10.3 Multiple sessions for chronic neck pain: intermediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 11 FUNNEL PLOT for pain: thoracic manipulation vs same treatment in both arms | 5 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 11.1 Multiple sessions for acute to chronic neck pain: short‐term follow‐up | 5 | 346 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.26 [‐1.86, ‐0.66] |
| 12 FUNNEL PLOT for function: thoracic manipulation vs same treatment in both arms | 4 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 12.1 Multiple sessions: short‐term follow‐up | 4 | 258 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.40 [‐2.24, ‐0.55] |
2.1. Analysis.
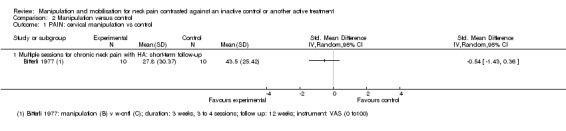
Comparison 2 Manipulation versus control, Outcome 1 PAIN: cervical manipulation vs control.
2.2. Analysis.
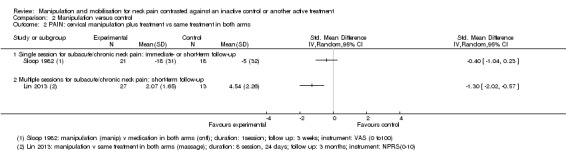
Comparison 2 Manipulation versus control, Outcome 2 PAIN: cervical manipulation plus treatment vs same treatment in both arms.
2.3. Analysis.
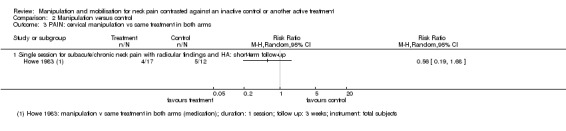
Comparison 2 Manipulation versus control, Outcome 3 PAIN: cervical manipulation vs same treatment in both arms.
2.4. Analysis.
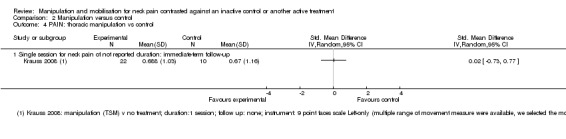
Comparison 2 Manipulation versus control, Outcome 4 PAIN: thoracic manipulation vs control.
2.5. Analysis.
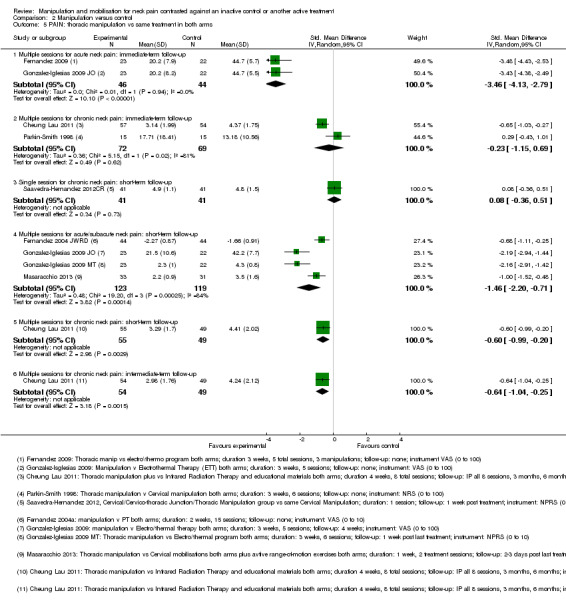
Comparison 2 Manipulation versus control, Outcome 5 PAIN: thoracic manipulation vs same treatment in both arms.
2.6. Analysis.
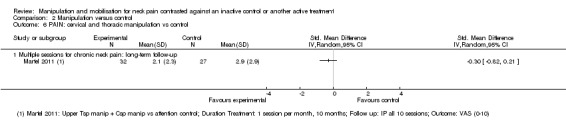
Comparison 2 Manipulation versus control, Outcome 6 PAIN: cervical and thoracic manipulation vs control.
2.7. Analysis.
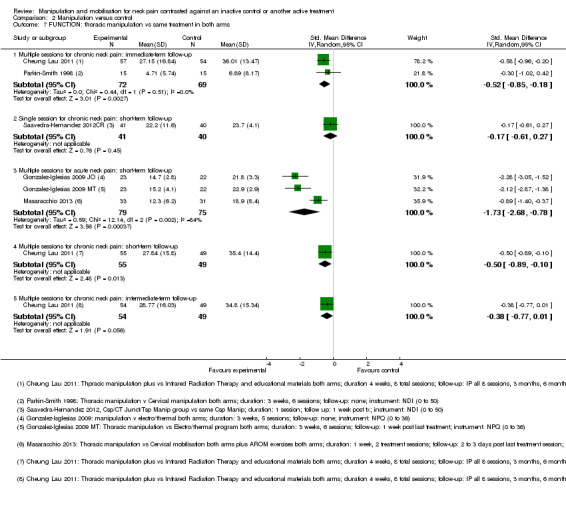
Comparison 2 Manipulation versus control, Outcome 7 FUNCTION: thoracic manipulation vs same treatment in both arms.
2.8. Analysis.
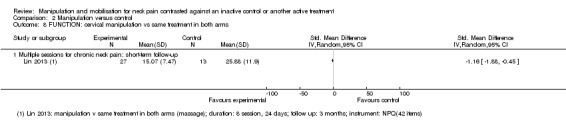
Comparison 2 Manipulation versus control, Outcome 8 FUNCTION: cervical manipulation vs same treatment in both arms.
2.9. Analysis.
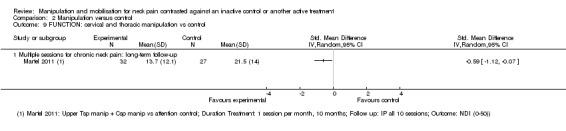
Comparison 2 Manipulation versus control, Outcome 9 FUNCTION: cervical and thoracic manipulation vs control.
2.10. Analysis.
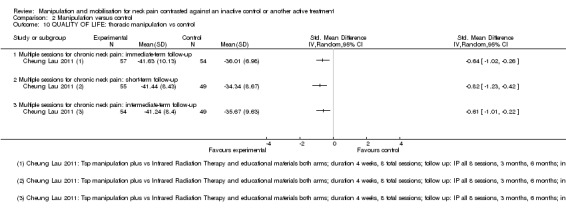
Comparison 2 Manipulation versus control, Outcome 10 QUALITY OF LIFE: thoracic manipulation vs control.
2.11. Analysis.
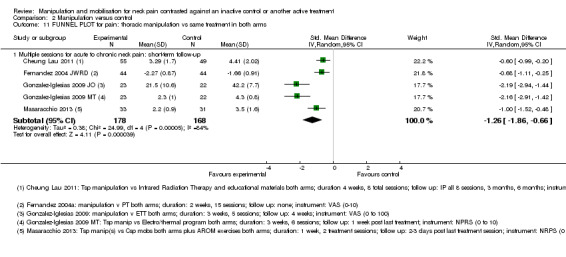
Comparison 2 Manipulation versus control, Outcome 11 FUNNEL PLOT for pain: thoracic manipulation vs same treatment in both arms.
2.12. Analysis.
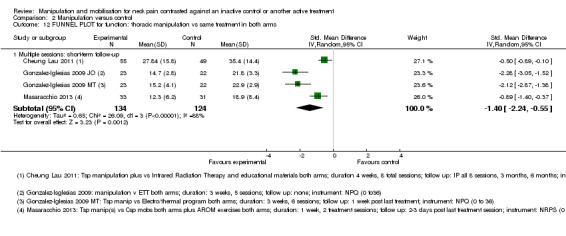
Comparison 2 Manipulation versus control, Outcome 12 FUNNEL PLOT for function: thoracic manipulation vs same treatment in both arms.
Comparison 3. Mobilisation versus control.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 PAIN: cervical mobilisation vs control | 2 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.1 Single session: intermediate post treatment | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Multiple sessions: short‐term follow‐up | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
3.1. Analysis.
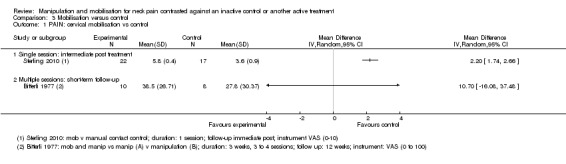
Comparison 3 Mobilisation versus control, Outcome 1 PAIN: cervical mobilisation vs control.
Comparison 4. Manipulation vs another treatment.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 PAIN: cervical manipulation vs mobilisation at immediate post treatment | 3 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.1 Single session for acute to chronic neck pain: immediate‐ or short‐term follow‐up | 2 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Multiple sessions for acute to subacute neck pain: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 PAIN: cervical manipulation vs mobilisation at intermediate‐term follow‐up | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 Multiple sessions for acute to chronic neck pain: intermediate‐term follow‐up | 2 | 446 | Mean Difference (IV, Random, 95% CI) | ‐0.07 [‐0.72, 0.59] |
| 3 PAIN: cervical manipulation vs massage | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.1 Multiple sessions for chronic CGH: short‐term follow‐up | 2 | 85 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.50 [‐0.93, ‐0.07] |
| 3.2 Multiple sessions for chronic CGH: intermediate‐term follow‐up | 1 | 36 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.79 [‐1.47, ‐0.11] |
| 4 PAIN: cervical manipulation vs medicine | 3 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.1 Multiple sessions for acute/subacute neck pain: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 Multiple sessions for acute/subacute neck pain: intermediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.3 Multiple sessions for acute/subacute neck pain: long‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.4 Multiple sessions for chronic neck pain: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.5 Multiple sessions for chronic neck pain: long‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 PAIN: cervical manipulation vs exercise | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 5.1 Multiple sessions for acute/subacute neck pain: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.2 Multiple sessions for acute/subacute neck pain: intermediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.3 Multiple sessions for acute/subacute neck pain: long‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 PAIN: cervical manipulation vs electrotherapy | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6.1 Multiple sessions for subacute to chronic CGH: short‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.2 Multiple sessions for subacute to chronic neck pain: short‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 PAIN: cervical manipulation vs acupuncture | 2 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 7.1 Multiple sessions for chronic neck pain: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.2 Multiple sessions for chronic neck pain: long‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 8 PAIN: cervical manipulation vs orthotic devices (K‐tape) | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 8.1 Single session for acute to chronic neck pain: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 9 PAIN: cervical manipulation vs varied multi‐modal approaches | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 9.1 Multiple sessions for chronic neck pain: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 10 PAIN: cervical manipulation ‐ 1 technique vs another technique | 4 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 10.1 Single session for acute to chronic neck pain: immediate‐ or short‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 10.2 Multiple sessions for chronic neck pain: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 10.3 Multiple sessions for subacute to chronic neck pain: short‐term follow‐up | 3 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 10.4 Multiple sessions for chronic neck pain: intermediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 11 PAIN: cervical manipulation ‐ varied dosage comparison | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 11.1 High vs low dosage ‐ multiple sessions for chronic CGH: short‐term follow‐up | 2 | 47 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.66 [‐1.81, 0.49] |
| 11.2 High vs low dosage ‐ multiple sessions for chronic CGH: intermediate‐term follow‐up | 2 | 50 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.40 [‐0.96, 0.16] |
| 12 PAIN: thoracic manipulation vs exercise | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 12.1 Multiple sessions for neck pain chronicity NR: long‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 13 FUNCTION: cervical manipulation vs mobilisation | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 13.1 Multiple sessions for acute/subacute neck pain: short‐term follow‐up | 1 | 176 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.06 [‐0.35, 0.24] |
| 13.2 Multiple sessions for acute to chronic neck pain: intermediate‐term follow‐up | 2 | 445 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.01 [‐0.21, 0.18] |
| 14 FUNCTION: cervical manipulation vs massage | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 14.1 Multiple sessions for chronic CGH: short‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 14.2 Multiple sessions for chronic CGH: intermediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 15 FUNCTION: cervical manipulation vs medicine | 3 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 15.1 Multiple sessions for acute/subacute neck pain: immediate‐term follow‐up | 1 | 181 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.35 [‐0.64, ‐0.06] |
| 15.2 Multiple sessions for chronic neck pain: immediate‐term follow‐up | 1 | 30 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.50 [‐1.30, 0.29] |
| 15.3 Multiple sessions for acute/subacute neck pain: intermediate‐term follow‐up | 1 | 181 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.30 [‐0.59, ‐0.00] |
| 15.4 Multiple sessions for acute/subacute neck pain: long‐term follow‐up | 1 | 181 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.11 [‐0.40, 0.18] |
| 15.5 Multiple sessions for chronic neck pain: long‐term follow‐up | 1 | 42 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.36 [‐0.97, 0.25] |
| 16 FUNCTION: cervical manipulation vs exercise | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 16.1 Multiple sessions for acute/subacute neck pain: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 16.2 Multiple sessions for acute/subacute neck pain: intermediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 16.3 Multiple sessions for acute/subacute neck pain: long‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 17 FUNCTION: cervical manipulation vs orthotic devices (K‐taping) | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 17.1 Single session for chronic neck pain: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 18 FUNCTION: cervical manipulation vs acupuncture | 2 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 18.1 Multiple sessions for subacute/chronic neck pain: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 18.2 Multiple sessions for chronic neck pain: long‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 19 FUNCTION: cervical manipulation vs varied multi‐modal approaches | 2 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 19.1 Multiple sessions for subacute/chronic neck pain: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 19.2 Multiple sessions for subacute/chronic neck pain: intermediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 20 FUNCTION: cervical manipulation ‐ 1 technique vs another technique | 3 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 20.1 Multiple sessions for subacute/chronic neck pain: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 20.2 Multiple sessions for acute/subacute neck pain: short‐term follow‐up | 2 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 20.3 Multiple sessions for neck pain chronicity NR: short‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 20.4 Multiple sessions for acute neck pain: intermediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 21 FUNCTION: cervical manipulation ‐ varied dosage comparison | 2 | 97 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.61 [‐1.09, ‐0.14] |
| 21.1 High vs low dosage ‐ multiple sessions for chronic CGH: short‐term follow‐up | 2 | 47 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.75 [‐1.71, 0.22] |
| 21.2 High vs low dosage ‐ multiple sessions for chronic CGH: intermediate‐term follow‐up | 2 | 50 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.61 [‐1.38, 0.17] |
| 22 PATIENT SATISFACTION: cervical manipulation vs mobilisation | 1 | 303 | Std. Mean Difference (IV, Random, 95% CI) | 0.02 [‐0.21, 0.24] |
| 22.1 Multiple sessions for subacute/chronic neck pain: short‐term follow‐up | 1 | 303 | Std. Mean Difference (IV, Random, 95% CI) | 0.02 [‐0.21, 0.24] |
| 23 PATIENT SATISFACTION: cervical manipulation vs varied multi‐modal approaches | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 23.1 Multiple sessions for subacute/chronic neck pain: short‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 24 GLOBAL PERCEIVED EFFECT: cervical manipulation vs mobilisation | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 24.1 Multiple sessions for acute/subacute neck pain: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 24.2 Multiple sessions for acute/subacute neck pain: intermediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 25 QUALITY OF LIFE: cervical manipulation vs mobilisation | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 25.1 Multiple sessions for acute/subacute neck pain: short‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 25.2 Multiple sessions for acute/subacute neck pain: intermediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 26 QUALITY OF LIFE: cervical manipulation vs medicine | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 26.1 Multiple sessions for acute/subacute neck pain: intermediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 26.2 Multiple sessions for acute/subacute neck pain: long‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 27 QUALITY OF LIFE: cervical manipulation vs exercise | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 27.1 Multiple sessions for acute/subacute neck pain: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 27.2 Multiple sessions for acute/subacute neck pain: intermediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 27.3 Multiple sessions for acute/subacute neck pain: long‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
4.1. Analysis.
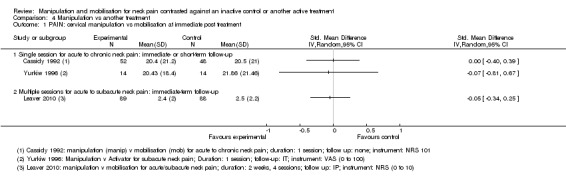
Comparison 4 Manipulation vs another treatment, Outcome 1 PAIN: cervical manipulation vs mobilisation at immediate post treatment.
4.2. Analysis.
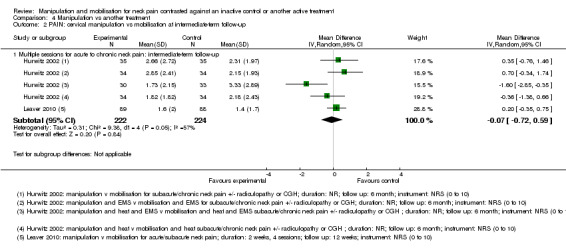
Comparison 4 Manipulation vs another treatment, Outcome 2 PAIN: cervical manipulation vs mobilisation at intermediate‐term follow‐up.
4.3. Analysis.
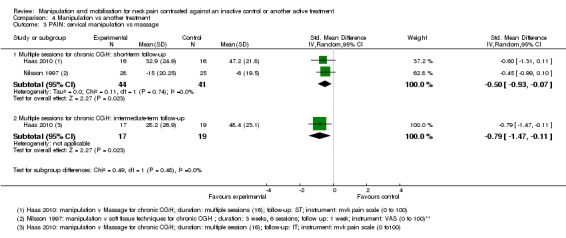
Comparison 4 Manipulation vs another treatment, Outcome 3 PAIN: cervical manipulation vs massage.
4.4. Analysis.
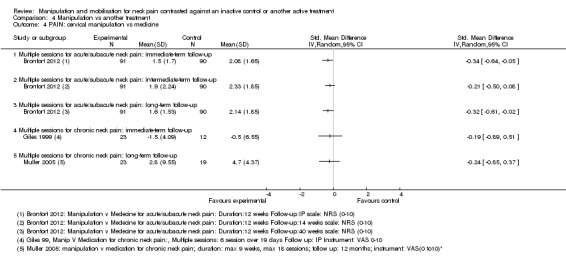
Comparison 4 Manipulation vs another treatment, Outcome 4 PAIN: cervical manipulation vs medicine.
4.5. Analysis.
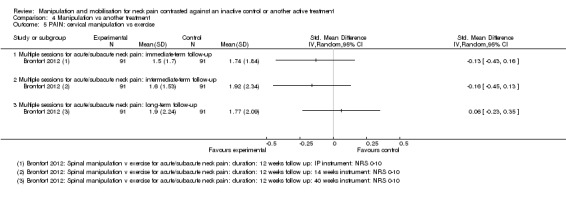
Comparison 4 Manipulation vs another treatment, Outcome 5 PAIN: cervical manipulation vs exercise.
4.6. Analysis.
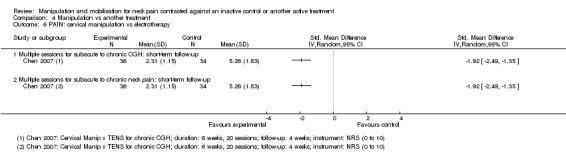
Comparison 4 Manipulation vs another treatment, Outcome 6 PAIN: cervical manipulation vs electrotherapy.
4.7. Analysis.
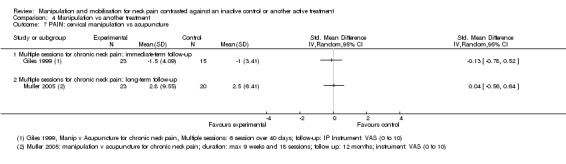
Comparison 4 Manipulation vs another treatment, Outcome 7 PAIN: cervical manipulation vs acupuncture.
4.8. Analysis.
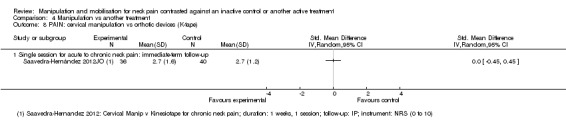
Comparison 4 Manipulation vs another treatment, Outcome 8 PAIN: cervical manipulation vs orthotic devices (K‐tape).
4.9. Analysis.
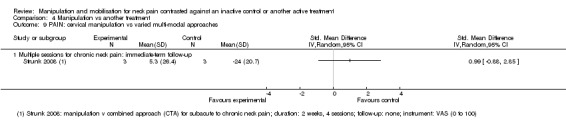
Comparison 4 Manipulation vs another treatment, Outcome 9 PAIN: cervical manipulation vs varied multi‐modal approaches.
4.10. Analysis.
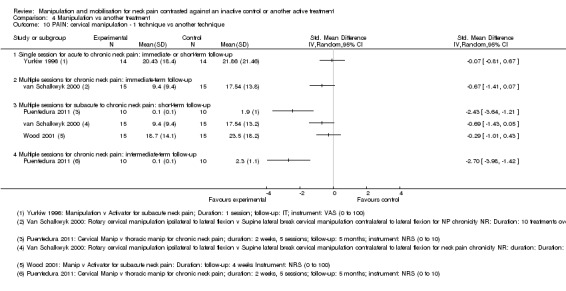
Comparison 4 Manipulation vs another treatment, Outcome 10 PAIN: cervical manipulation ‐ 1 technique vs another technique.
4.11. Analysis.
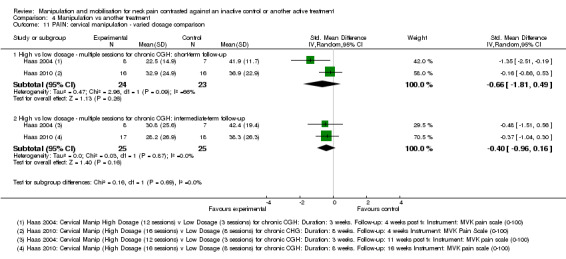
Comparison 4 Manipulation vs another treatment, Outcome 11 PAIN: cervical manipulation ‐ varied dosage comparison.
4.12. Analysis.
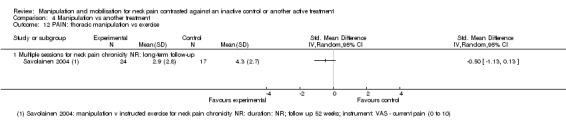
Comparison 4 Manipulation vs another treatment, Outcome 12 PAIN: thoracic manipulation vs exercise.
4.13. Analysis.
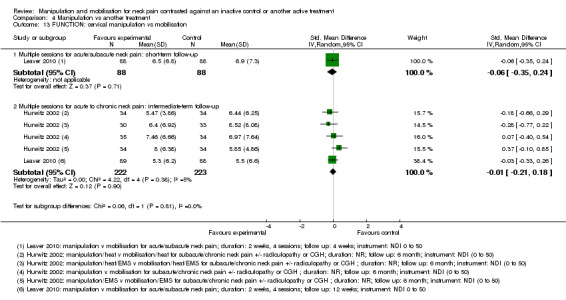
Comparison 4 Manipulation vs another treatment, Outcome 13 FUNCTION: cervical manipulation vs mobilisation.
4.14. Analysis.
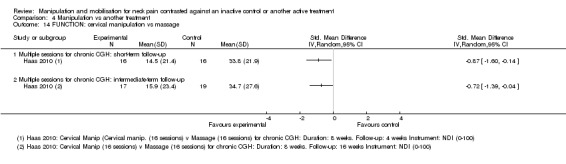
Comparison 4 Manipulation vs another treatment, Outcome 14 FUNCTION: cervical manipulation vs massage.
4.15. Analysis.
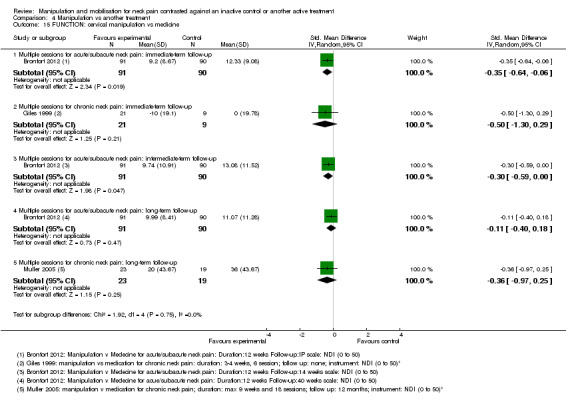
Comparison 4 Manipulation vs another treatment, Outcome 15 FUNCTION: cervical manipulation vs medicine.
4.16. Analysis.
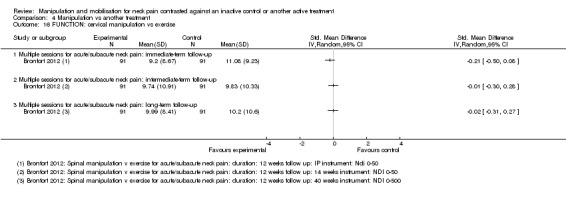
Comparison 4 Manipulation vs another treatment, Outcome 16 FUNCTION: cervical manipulation vs exercise.
4.17. Analysis.
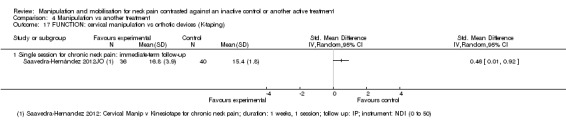
Comparison 4 Manipulation vs another treatment, Outcome 17 FUNCTION: cervical manipulation vs orthotic devices (K‐taping).
4.18. Analysis.
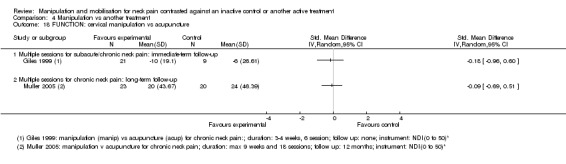
Comparison 4 Manipulation vs another treatment, Outcome 18 FUNCTION: cervical manipulation vs acupuncture.
4.19. Analysis.
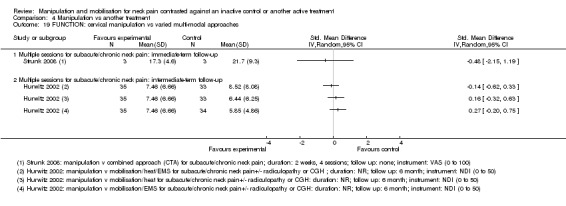
Comparison 4 Manipulation vs another treatment, Outcome 19 FUNCTION: cervical manipulation vs varied multi‐modal approaches.
4.20. Analysis.
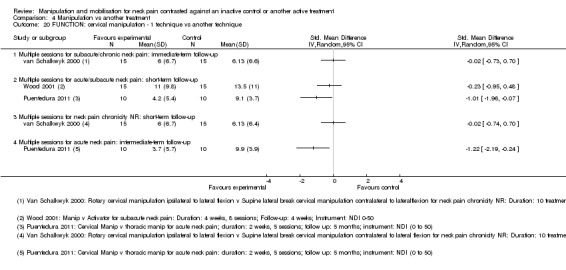
Comparison 4 Manipulation vs another treatment, Outcome 20 FUNCTION: cervical manipulation ‐ 1 technique vs another technique.
4.21. Analysis.
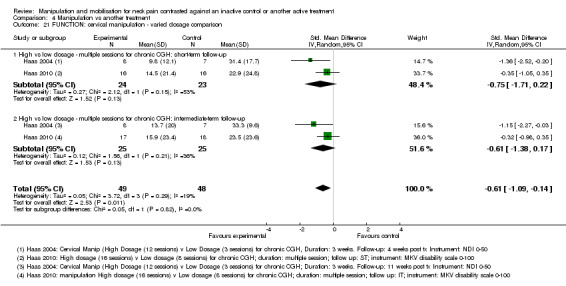
Comparison 4 Manipulation vs another treatment, Outcome 21 FUNCTION: cervical manipulation ‐ varied dosage comparison.
4.22. Analysis.
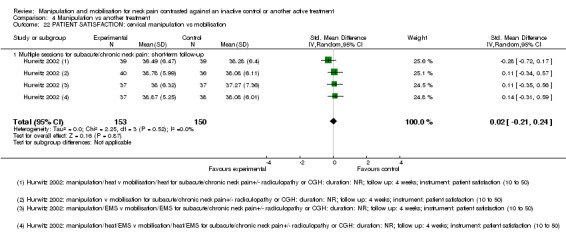
Comparison 4 Manipulation vs another treatment, Outcome 22 PATIENT SATISFACTION: cervical manipulation vs mobilisation.
4.23. Analysis.
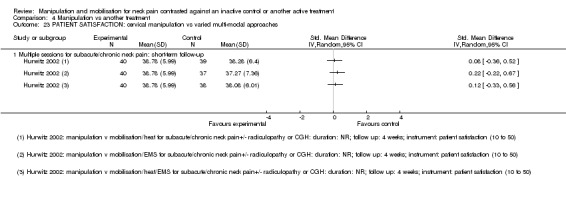
Comparison 4 Manipulation vs another treatment, Outcome 23 PATIENT SATISFACTION: cervical manipulation vs varied multi‐modal approaches.
4.24. Analysis.
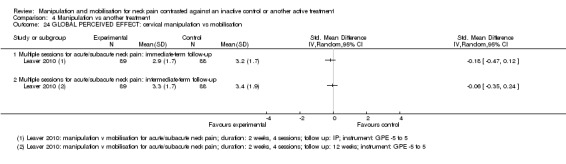
Comparison 4 Manipulation vs another treatment, Outcome 24 GLOBAL PERCEIVED EFFECT: cervical manipulation vs mobilisation.
4.25. Analysis.
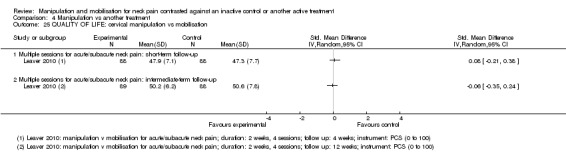
Comparison 4 Manipulation vs another treatment, Outcome 25 QUALITY OF LIFE: cervical manipulation vs mobilisation.
4.26. Analysis.
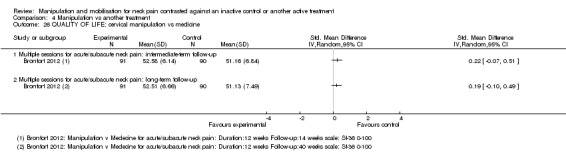
Comparison 4 Manipulation vs another treatment, Outcome 26 QUALITY OF LIFE: cervical manipulation vs medicine.
4.27. Analysis.
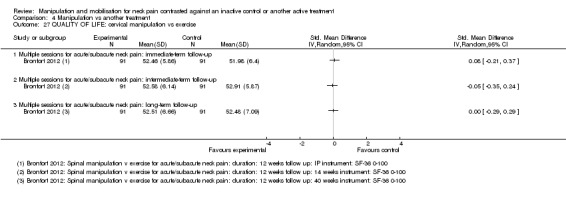
Comparison 4 Manipulation vs another treatment, Outcome 27 QUALITY OF LIFE: cervical manipulation vs exercise.
Comparison 5. Mobilisation versus another treatment.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 PAIN: cervical mobilisation vs medical injection ‐ trigger point | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.1 Multiple sessions for neck pain chronicity NR: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 PAIN: cervical mobilisation vs exercise | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 2.1 Multiple sessions for radiculopathy chronicity NR: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 PAIN: cervical mobilisation vs electrotherapy | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 3.1 Multiple sessions for chronic neck pain: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Multiple sessions for chronic neck pain: intermediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 PAIN: cervical mobilisation vs sonic devices ‐ ultrasound, shock wave therapy | 2 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.1 Single session for subacute/chronic neck pain: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 Multiple sessions for neck pain chronicity NR: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 PAIN: cervical mobilisation vs mechanical traction | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 5.1 Multiple sessions for neck pain chronicity NR: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 PAIN: cervical mobilisation vs acupuncture | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6.1 Multiple sessions for chronic neck pain: intermediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 PAIN: cervical mobilisation vs varied multi‐modal approaches | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 7.1 Multiple sessions for subacute/chronic neck pain ± radiculopathy or CGH: intermediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 8 PAIN: cervical mobilisation ‐ 1 technique vs another technique | 5 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 8.1 Single session for chronic neck pain: immediate‐term follow‐up | 2 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.2 Single session for chronic neck pain ± radiculopathy: immediate‐term follow‐up | 2 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.3 Multiple sessions for chronic CGH: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.4 Multiple sessions for chronic CGH: intermediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 9 PAIN: cervical mobilisation ‐ 1 technique vs another technique | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 9.1 PA vs other mobilisation for acute/subacute neck pain: multiple sessions: immediate‐term follow‐up | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 9.2 AP vs other mobilisation: multiple sessions: immediate‐term follow‐up | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 10 PAIN: cervical mobilisation vs massage | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 10.1 Multiple sessions for chronic neck pain: immediate‐term follow‐up | 2 | 58 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.56 [‐4.15, 1.03] |
| 10.2 Multiple sessions for chronic CGH: immediate‐term follow‐up | 1 | 36 | Std. Mean Difference (IV, Random, 95% CI) | ‐2.89 [‐3.85, ‐1.93] |
| 11 FUNCTION: cervical mobilisation vs medical injection ‐ trigger point | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 11.1 Multiple sessions for neck pain chronicity NR: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 12 FUNCTION: cervical mobilisation vs exercise | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 12.1 Multiple sessions for radiculopathy: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 13 FUNCTION: cervical mobilisation vs electrotherapy | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 13.1 Multiple sessions for neck pain chronicity NR: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 13.2 Multiple sessions for neck pain chronicity NR: intermediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 14 FUNCTION: cervical mobilisation vs sonic devices ‐ shock wave therapy | 2 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 14.1 Multiple sessions for neck pain chronicity NR: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 14.2 Multiple sessions for acute/subacute neck pain: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 15 FUNCTION: cervical mobilisation vs acupuncture | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 15.1 Multiple sessions for chronic neck pain: intermediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 16 FUNCTION: cervical mobilisation vs varied multi‐modal approaches | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 16.1 Multiple sessions for subacute/chronic neck pain ± radiculopathy or CGH: intermediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 17 FUNCTION: cervical mobilisation vs massage | 2 | 59 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.03 [‐0.90, 0.84] |
| 17.1 Multiple sessions for chronic neck pain: immediate‐term follow‐up | 1 | 23 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.52 [‐1.35, 0.32] |
| 17.2 Multiple sessions for subacute/chronic CGH: immediate‐term follow‐up | 1 | 36 | Std. Mean Difference (IV, Random, 95% CI) | 0.38 [‐0.28, 1.04] |
| 18 FUNCTION: cervical mobilisation ‐ 1 technique vs another technique | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 18.1 Multiple sessions for chronic CGH: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 18.2 Multiple sessions for chronic CGH: intermediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 19 QUALITY OF LIFE: mobilisation vs electrotherapy | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 19.1 Multiple sessions for neck pain chronicity NR: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 19.2 Multiple sessions for neck pain chronicity NR: intermediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 20 PATIENT SATISFACTION: cervical mobilisation vs varied multi‐modal approaches | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 20.1 Multiple sessions for subacute/chronic neck pain ± radiculopathy or CGH: short‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 21 PATIENT SATISFACTION: cervical mobilisation vs electrotherapy | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 21.1 Multiple sessions for neck pain chronicity NR: intermediate‐term follow‐up | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 22 GLOBAL PERCEIVED EFFECT: cervical mobilisation ‐ 1 technique vs another technique | 2 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 22.1 Single session for chronic neck pain: immediate‐term follow‐up | 2 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
5.1. Analysis.
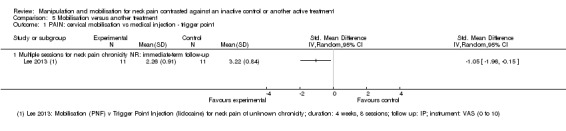
Comparison 5 Mobilisation versus another treatment, Outcome 1 PAIN: cervical mobilisation vs medical injection ‐ trigger point.
5.2. Analysis.
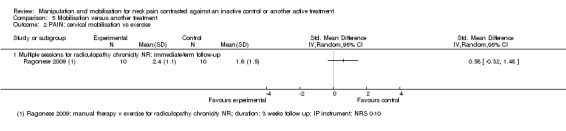
Comparison 5 Mobilisation versus another treatment, Outcome 2 PAIN: cervical mobilisation vs exercise.
5.3. Analysis.
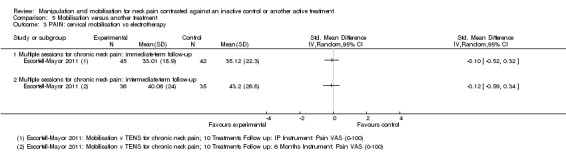
Comparison 5 Mobilisation versus another treatment, Outcome 3 PAIN: cervical mobilisation vs electrotherapy.
5.4. Analysis.
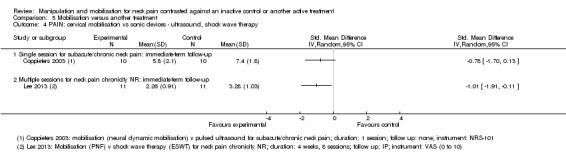
Comparison 5 Mobilisation versus another treatment, Outcome 4 PAIN: cervical mobilisation vs sonic devices ‐ ultrasound, shock wave therapy.
5.5. Analysis.
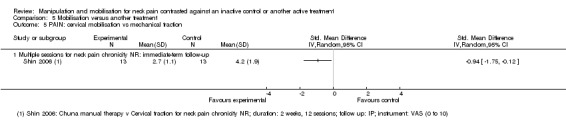
Comparison 5 Mobilisation versus another treatment, Outcome 5 PAIN: cervical mobilisation vs mechanical traction.
5.6. Analysis.
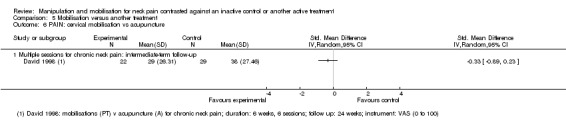
Comparison 5 Mobilisation versus another treatment, Outcome 6 PAIN: cervical mobilisation vs acupuncture.
5.7. Analysis.
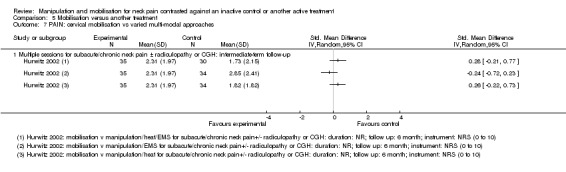
Comparison 5 Mobilisation versus another treatment, Outcome 7 PAIN: cervical mobilisation vs varied multi‐modal approaches.
5.8. Analysis.
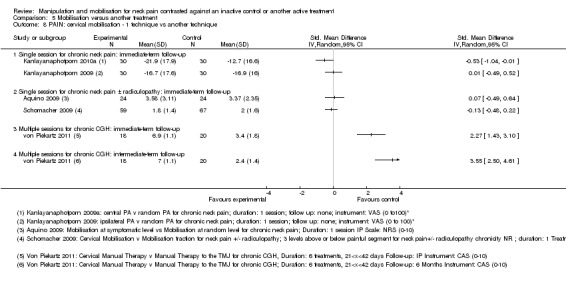
Comparison 5 Mobilisation versus another treatment, Outcome 8 PAIN: cervical mobilisation ‐ 1 technique vs another technique.
5.9. Analysis.
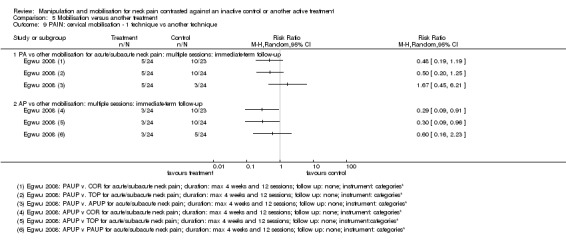
Comparison 5 Mobilisation versus another treatment, Outcome 9 PAIN: cervical mobilisation ‐ 1 technique vs another technique.
5.10. Analysis.
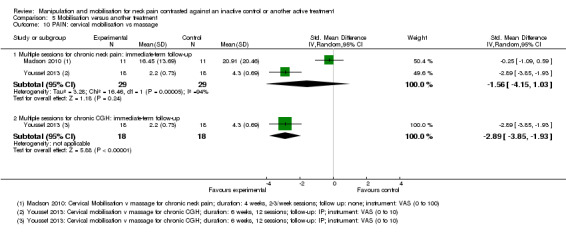
Comparison 5 Mobilisation versus another treatment, Outcome 10 PAIN: cervical mobilisation vs massage.
5.11. Analysis.
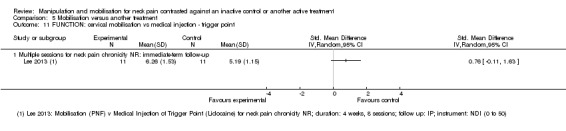
Comparison 5 Mobilisation versus another treatment, Outcome 11 FUNCTION: cervical mobilisation vs medical injection ‐ trigger point.
5.12. Analysis.
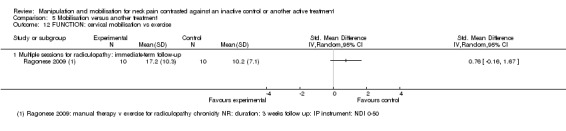
Comparison 5 Mobilisation versus another treatment, Outcome 12 FUNCTION: cervical mobilisation vs exercise.
5.13. Analysis.
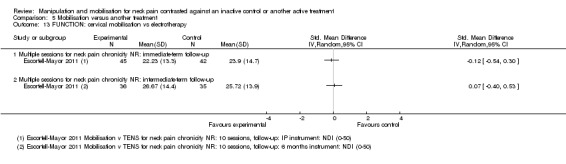
Comparison 5 Mobilisation versus another treatment, Outcome 13 FUNCTION: cervical mobilisation vs electrotherapy.
5.14. Analysis.
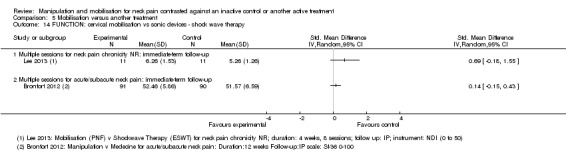
Comparison 5 Mobilisation versus another treatment, Outcome 14 FUNCTION: cervical mobilisation vs sonic devices ‐ shock wave therapy.
5.15. Analysis.
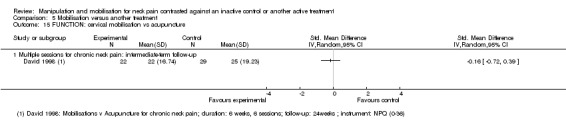
Comparison 5 Mobilisation versus another treatment, Outcome 15 FUNCTION: cervical mobilisation vs acupuncture.
5.16. Analysis.
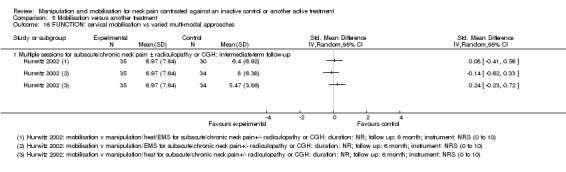
Comparison 5 Mobilisation versus another treatment, Outcome 16 FUNCTION: cervical mobilisation vs varied multi‐modal approaches.
5.17. Analysis.
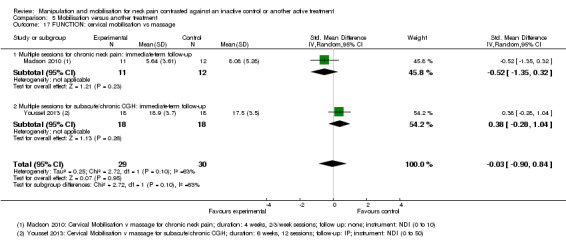
Comparison 5 Mobilisation versus another treatment, Outcome 17 FUNCTION: cervical mobilisation vs massage.
5.18. Analysis.
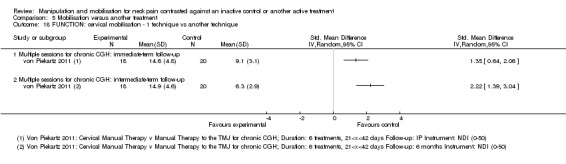
Comparison 5 Mobilisation versus another treatment, Outcome 18 FUNCTION: cervical mobilisation ‐ 1 technique vs another technique.
5.19. Analysis.
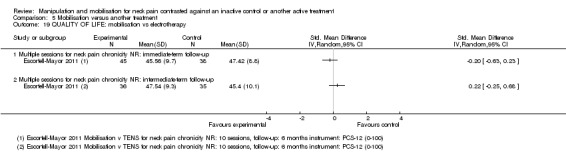
Comparison 5 Mobilisation versus another treatment, Outcome 19 QUALITY OF LIFE: mobilisation vs electrotherapy.
5.20. Analysis.
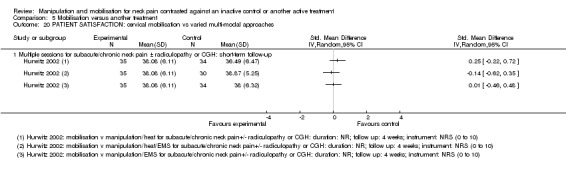
Comparison 5 Mobilisation versus another treatment, Outcome 20 PATIENT SATISFACTION: cervical mobilisation vs varied multi‐modal approaches.
5.21. Analysis.
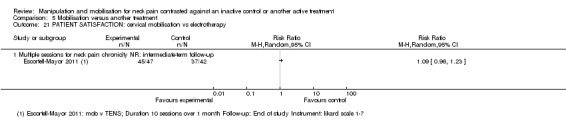
Comparison 5 Mobilisation versus another treatment, Outcome 21 PATIENT SATISFACTION: cervical mobilisation vs electrotherapy.
5.22. Analysis.
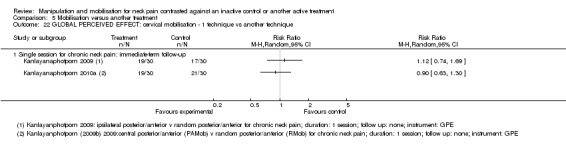
Comparison 5 Mobilisation versus another treatment, Outcome 22 GLOBAL PERCEIVED EFFECT: cervical mobilisation ‐ 1 technique vs another technique.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Aquino 2009.
| Methods | Type of trial: RCT Number analysed/randomly assigned: 48/48 Intention‐to‐treat analysis: calculated | |
| Participants | Chronic non‐specific cervical disorder | |
| Interventions | INDEX TREATMENT
Mobilisation at most symptomatic cervical vertebral level (B): technique: anterior central vertebral pressure, posterior‐anterior unilateral pressure and transversal vertebral pressure; technique selected at physiotherapist’s discretion, indications by Maitland et al.; timing: at baseline; frequency: 1 session; route: cervical spine COMPARISON TREATMENT Mobilisation randomly chosen at cervical vertebral level (A): technique: posterior‐anterior central vertebral pressure, posterior‐anterior unilateral pressure and transversal vertebral pressure; technique selected at physiotherapist’s discretion, indications by Maitland et al.; timing: at baseline; frequency: 1 session; route: cervical spine CO‐INTERVENTION: not applicable (N/A) Duration of treatment: 1 day, 1 session Duration of follow‐up: 0 days |
|
| Outcomes | PAIN (during most painful movement, 11‐point pain scale, 0 to 10) Baseline mean: A 6.2, B 6.04 End of study mean: A 3.58, B 3.37 Absolute benefit: A 2.62, B 2.67 Reported results: not significant SMD (A vs B): 0.07 (95% CI ‐0.49 to 0.64) FUNCTION: not reported (NR) GPE: NR PATIENT SATISFACTION: NR QoL: NR SIDE EFFECTS: NR COST OF CARE: NR |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not adequately designed; page 96, middle column, paragraph 2 |
| Allocation concealment (selection bias) | Unclear risk | Not adequately designed; page 96, middle column, paragraph 2 |
| Blinding of Participants (performance bias) | Unclear risk | Participant blinding not described but possible |
| Blinding of Personal (performance bias) | High risk | Study authors state that care providers were blinded; however, we believe this was not possible because treatment was provided at the discretion of the therapist |
| Blinding of the Outcome assessor (detection bias) | Unclear risk | Participant is the assessor |
| Incomplete outcome data (attrition bias) | Low risk | Pre‐post design; Figure 1 |
| Randomized Participants analysed were allocated (attrition bias) | Low risk | Pre‐post |
| Selective outcome (reporting bias) | Unclear risk | No protocol |
| Similar groups at baseline? | Low risk | Table 1 and Table 3 |
| co‐interventions avoided or similar? | Low risk | Pre‐post design |
| Compliance acceptable? | Low risk | Pre‐post design |
| Similar timing of outcome assessment? | Low risk | Pre‐post design |
Bitterli 1977.
| Methods | Type of trial: quasi‐RCT Number analysed/randomly assigned: 24/30 Intention‐to‐treat analysis: calculated | |
| Participants | Chronic neck pain with headache or degenerative changes (spondylogenic) | |
| Interventions | INDEX TREATMENT
Group A (A): technique: manipulation as described by Maigne; frequency: 1 session/wk; dose: mean 6.2 manipulations over 3.2 sessions; route: cervical spine Group B (B): technique: manipulation; frequency: 1 session/wk; dose: mean 7.2 manipulations over 3.8 sessions; route: cervical spine COMPARISON TREATMENT Group C (C): wait list control CO‐INTERVENTION: none Duration of treatment: 3 weeks, 3 to 4 sessions Duration of follow‐up: 12 weeks |
|
| Outcomes | PAIN (VAS, 0 to 100) Baseline mean: A 60.50, B 64.40, C 57.60 End of study mean: A 38.50, B 27.80, C 43.50 Absolute benefit: A 22.0, B 36.6, C 14.1 Reported results: not significant SMD (A vs C): ‐0.18 (95% CI‐1.12 to 0.75) (power 10%) SMD (A vs B): 0.36 (95% CI‐0.58 to 1.30) (power 7%) SMD (B vs C): ‐0.54 (95% CI‐1.43 to 0.36) (power 10%) FUNCTION: NR GPE: NR PATIENT SATISFACTION: NR QoL: NR SIDE EFFECTS: Manipulation and mobilisation were well tolerated, with the customary reaction of minimal benign reaction lasting less than 24 hours (RR 1.34, 95% CI 0.77 to 2.34) COST OF CARE: NR |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Draw lots; even chance of getting assigned to 1 of 3 groups |
| Allocation concealment (selection bias) | High risk | Not concealed |
| Blinding of Participants (performance bias) | High risk | VAS pain; not blind to participant |
| Blinding of Personal (performance bias) | High risk | Not blind |
| Blinding of the Outcome assessor (detection bias) | High risk | Participant is outcome assessor for VAS pain |
| Incomplete outcome data (attrition bias) | Low risk | See Table 1, page 260, for complete data |
| Randomized Participants analysed were allocated (attrition bias) | High risk | ITT not reported |
| Selective outcome (reporting bias) | Unclear risk | No previous protocol |
| Similar groups at baseline? | Low risk | Presented in text, page 260, 2nd column, 2nd paragraph. |
| co‐interventions avoided or similar? | Low risk | No co‐intervention was noted |
| Compliance acceptable? | High risk | Not assessed |
| Similar timing of outcome assessment? | Low risk | All groups were measured at similar time points |
Bronfort 2012.
| Methods | Type of trial: RCT Number analysed/randomly assigned: 147/272 Intension‐to‐treat analysis: calculated | |
| Participants | Acute/subacute mechanical neck pain (grade I or II according to Bone and Joint Decade 2000‐2010 Task on Neck Pain and Its Associated Disorders classification) | |
| Interventions | INDEX TREATMENT
Spinal manipulation therapy (A): technique: low‐amplitude spinal adjustments (high‐velocity type of joint thrust manipulation) and mobilisation. Specific spinal level to be treated was left to the discretion of the provider. Light‐soft massage, assisted stretching and cold and hot packs to facilitate manipulation treatment; timing: at baseline; frequency: left to the provider's discretion (mean visits = 15.3); duration: 15 to 20 minutes; route: cervical spine and thoracic spine COMPARISON TREATMENT Medication (B): technique: NSAID, acetaminophen or both. Second line of therapy for those who did not respond was narcotic medication. Muscle relaxants were also used (choice made by the physician); timing: at baseline; frequency: left to the physician's discretion (mean visits = 4.8); dose: choice made by the physician; duration: 15 to 20 minutes (included brief history and examination); route: oral Home exercise (C): technique: self mobilisation exercise (gentle controlled movement) of the neck and shoulder (neck retraction, rotation, extension, flexion, lateral bending motions and scapular retraction with no resistance); timing: at baseline; frequency: 6 to 8 times per day; dose: 5 to 10 rep/exercise; route: cervical and shoulder joint CO‐INTERVENTION: avoided in trial design: additional treatment for neck pain from non‐study healthcare providers, 4 participants (n = 3 in the medication group and n = 1 in the HEA group) reported to visit other healthcare providers during 12‐week interventions; by week 52, participants in each treatment group sought additional health care after completing the treatment phase (n = 18 in the SMT group, n = 14 in the medication group, n = 17 in the HEA group) Duration of treatment: maximum 12 weeks; number of treatment sessions was left to the discretion of the provider Duration of follow‐up: 40 weeks |
|
| Outcomes | PAIN (NRS, 0 to 10) Baseline mean: A 5.27, B 4.93, C 5.05 End of study mean: A 1.60, B 2.14, C 1.92 Absolute benefit: A 3.67, B 2.79, C 3.13 Reported results: significant favouring A over B at IP and LT SMD (A vs C): IP ‐0.13 (95% CI ‐0.43 to 0.16), IT ‐0.16 (95% CI ‐0.45 to 0.13), LT 0.06 (95% CI ‐0.23 to 0.35) SMD (A vs B): IP ‐0.34 (95% CI ‐0.64 to ‐0.05), IT ‐0.21 (95% CI ‐0.50 to 0.08), LT ‐0.32 (95% CI ‐0.61 to ‐0.02); NNTB 12 FUNCTION (NDI, 0 to 50) Baseline mean: A 24.22, B 25.12, C 25.12 End of study mean: A 9.99, B 11.07, C 10.20 Absolute benefit: A 14.23, B 14.05, C 14.92 Reported results: significant favouring A over B at IP and IT SMD (A vs C): IP ‐0.21 (95% CI ‐0.50 to 0.08), IT ‐0.01 (95% CI ‐0.30 to 0.28), LT ‐0.02 (95% CI ‐0.31 to 0.27) SMD (A vs B): IP ‐0.35 (95% CI ‐0.64 to ‐0.06), IT ‐0.30 (95% CI ‐0.59 to ‐0.00), LT ‐0.11 (95% CI ‐0.40 to 0.18); NNTB 15 GPE (9‐point scale, 1 to 9) End of study mean: A 2.22, B 2.57, C 2.43 Reported results: significant improvement favouring A over B PATIENT SATISFACTION (7‐point scale, 1 to 7) End of study mean: A 1.67, B 2.48, C 2.06 Reported results: significant improvement favouring A over B QoL (PCS component of SF‐36, 0 to 100) Baseline mean: A 43.36, B 46.27, C 45.31 End of study mean: A 52.51, B 51.13, C 52.48 Absolute benefit: A 9.15, B 4.86, C 7.17 Reported results: not significant SMD (A vs C): IP 0.08 (95% CI ‐0.21 to 0.37), IT ‐0.05 (95% CI ‐0.35 to 0.24), LT 0.00 (95% CI ‐0.29 to 0.29) SMD (A vs B): IP 0.14 (95% CI ‐0.15 to 0.43), IT 0.22 (95% CI ‐0.07 to 0.51), LT 0.19 (95% CI ‐0.10 to 0.49) SIDE EFFECTS Aggravation of pain: A 28/91, B 0/90, C 37/91 Headache: A 5/91, B 0/90, C 3/91 Stiffness: A 5/91, B 0/90, C 4/91 Not specified: A 4/91, B 5/90, C 0/91 Paraesthesia: A 2/91, B 0/90, C 3/91 Nausea: A 1/91, B 5/90, C 1/91 Crepitus: A 0/91, B 0/90, C 3/91 Increased blood pressure: A 0/91, B 1/90, C 0/91 Stress incontinence: A 0/91, B 1/90, C 0/91 Disturbed sleep: A 0/91, B 4/90, C 0/91 Congestion: A 0/91, B 6/90, C 0/91 Rash: A 0/91, B 7/90, C 0/91 Cognitive symptoms: A 0/91, B 10/90, C 0/91 Dry mouth: A 0/91, B 10/90, C 0/91 Gastrointestinal symptoms: A 0/91, B 17/90, C 0/91 Drowsiness: A 0/91, B 18/90, C 0/91 COST OF CARE: NR |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Page 2, left column, at the bottom |
| Allocation concealment (selection bias) | Low risk | Page 2, right column, at the top |
| Blinding of Participants (performance bias) | High risk | Not possible owing to design |
| Blinding of Personal (performance bias) | High risk | Not possible owing to design |
| Blinding of the Outcome assessor (detection bias) | High risk | Not possible owing to design |
| Incomplete outcome data (attrition bias) | Unclear risk | Study flow diagram is unclear – are long‐term dropouts 31 or 52 (short term + long term). Also, long‐term dropout in medication group is 34.4%. Unclear whether dropouts in each week of diagram are the same participants |
| Randomized Participants analysed were allocated (attrition bias) | Low risk | Page 3, right column, paragraph 3 |
| Selective outcome (reporting bias) | Low risk | Page 2, right column, paragraph 2 – similar to Evans 2003 pilot |
| Similar groups at baseline? | Low risk | Table 1 |
| co‐interventions avoided or similar? | High risk | Table 2 – Variety of co‐interventions were provided to SMT group; types of other interventions used by each group are not reported |
| Compliance acceptable? | Unclear risk | Unsure whether participants were compliant with home exercises |
| Similar timing of outcome assessment? | Low risk | Page 3, right column, paragraph 2 |
Cassidy 1992.
| Methods | Type of trial: RCT Number analysed/randomly assigned: 100/100 Intention‐to‐treat analysis: conducted | |
| Participants | Acute, subacute, chronic neck pain with varied degenerative changes (spondylosis) | |
| Interventions | INDEX TREATMENT
Manipulation (A): technique: rotation manipulation away from the direction of pain; frequency: 1 session; dose: 1 manipulation; route: cervical spine COMPARISON TREATMENT Mobilisation (B): technique: muscle energy technique described by Bourdillon, an isometric contraction localised to the involved level, held for 5 seconds, repeated 4 times with increasing rotation or lateral flexion at localised levels; frequency: 1 session; route: cervical spine CO‐INTERVENTION: none Duration of treatment: 1 session Duration of follow‐up: none |
|
| Outcomes | PAIN (NRS, 0 to 100) Baseline mean: A 37.7, B 31.0 End of study mean: A 20.4, B 20.5 Absolute benefit: A 17.3, B 10.5 Reported results: not significant SMD (A vs B): 0.00 (95% CI ‐0.40 to 0.39) (power 16%) FUNCTION: NR PATIENT SATISFACTION: NR GPE: NR QoL: NR SIDE EFFECTS: no complications; 3 participants in each group reported more pain after intervention (RR 0.97, 95% CI 0.47 to 2.03) COST OF CARE: NR |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Mentioned in letter to editor, 1993, page 279 |
| Allocation concealment (selection bias) | Low risk | Mentioned in letter to editor, 1993, page 279 |
| Blinding of Participants (performance bias) | High risk | Not possible owing to design |
| Blinding of Personal (performance bias) | High risk | Not possible owing to design |
| Blinding of the Outcome assessor (detection bias) | High risk | Not possible owing to design |
| Incomplete outcome data (attrition bias) | Low risk | Pre‐post design |
| Randomized Participants analysed were allocated (attrition bias) | Low risk | Pre‐post design |
| Selective outcome (reporting bias) | Unclear risk | No previous protocol found |
| Similar groups at baseline? | High risk | Mentioned in letter to editor, 1993, page 279 |
| co‐interventions avoided or similar? | Low risk | Pre‐post design |
| Compliance acceptable? | Low risk | Pre‐post design |
| Similar timing of outcome assessment? | Low risk | Pre‐post design |
Chen 2007.
| Methods | Type of trial: quasi‐RCT Number analysed/randomly assigned: 65/70 Intention‐to‐treat analysis: not calculated | |
| Participants | Chronic cervicogenic headache from degenerative changes | |
| Interventions | INDEX TREATMENT
Manipulation (A): technique: manipulation; frequency: 10 sessions, every other day; dose: 20‐ to 30 minute‐treatment; route: cervical spine COMPARISON TREATMENT Transcutaneous electrical nerve stimulation (B): technique: TENS Perimedic, 10 Hz, 250 ns; frequency: 10 sessions every other day; dose: 20‐minute duration; route: NR CO‐INTERVENTION: NR Duration of therapy period: 10 sessions Duration of follow‐up: 4 weeks |
|
| Outcomes | PAIN (NRS, 0 to 10) Baseline mean: A 7.45, B 7.86 End of study mean: A 2.31, B 5.26 Absolute benefit: A 5.14, B 2.6 Reported results: significant favouring manipulation SMD (A vs B): ‐1.92 (95% CI ‐2.49 to ‐1.35); NNTB 7 FUNCTION: NR PATIENT SATISFACTION: NR GPE: NR QoL: NR SIDE EFFECTS: none COST OF CARE: NR |
|
| Notes | Chinese translation: Kein Trinh | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Page 404, right column, paragraph 1 |
| Allocation concealment (selection bias) | High risk | Page 404, right column, paragraph 1 |
| Blinding of Participants (performance bias) | High risk | Blinding not mentioned in the paper but really not possible, as 2 treatment methods are very different |
| Blinding of Personal (performance bias) | High risk | Page 404, left column, paragraph 2 |
| Blinding of the Outcome assessor (detection bias) | High risk | Page 404, right column, 1.3 and 1.4 sections. Describe subjective rating system of treatment effectiveness and pain score. Scores are given by participant, so outcome assessor is not blinded |
| Incomplete outcome data (attrition bias) | Low risk | Page 404, right column, lines 5 to 7 |
| Randomized Participants analysed were allocated (attrition bias) | High risk | Table 2, page 405 |
| Selective outcome (reporting bias) | Unclear risk | No previous protocol published |
| Similar groups at baseline? | Low risk | Page 405, section 2.1; also Tables 1 and 2, baseline data |
| co‐interventions avoided or similar? | Low risk | Not mentioned |
| Compliance acceptable? | Low risk | Page 405, section 2.1 |
| Similar timing of outcome assessment? | Low risk | Page 404, right column, section 1.4 |
Cheung Lau 2011.
| Methods | Type of trial: RCT
Number analysed/randomly assigned: 60/60
Intention‐to‐treat analysis: calculated Location of study: Hong Kong |
|
| Participants | Chronic (> 3 months) mechanical neck pain | |
| Interventions | INDEX TREATMENT
Manipulation group (manipulation plus cntl): technique: supine technique performed anterior‐posterior, high‐velocity low‐amplitude thoracic manipulation plus infrared radiation therapy and educational materials (pathology, advice, exercise) provided; frequency: 2 sessions per week for 4 weeks, 8 sessions total; dose: 1 to 2 manipulations per segment; duration: infrared radiation therapy applied for 15 minutes; route: thoracic spine manipulation to identified restricted segment, infrared radiation therapy applied over painful site COMPARISON TREATMENT Control group (cntl): Infrared radiation therapy group received the same educational materials as were given to the manipulation group (CG): technique: infrared radiation therapy; frequency: 2 sessions per week for 4 weeks, 8 sessions total; dose: 15 minutes per session; route: applied over painful site CO‐INTERVENTION: NR Duration of therapy period: 4 weeks Duration of follow‐up: immediately post treatment, 3 months, 6 months |
|
| Outcomes | PAIN (NPRS, 0 to 10) Baseline mean: manip plus cntl 5.02, cntl 5.05 End of study mean: manip plus cntl 2.98, cntl 4.24 Absolute benefit: manip plus cntl 2.04, cntl 0.81 Reported results: significant favouring manipulation SMD (6 months): ‐0.64 (95% CI ‐1.04 to ‐0.25); NNTB 4 FUNCTION: NPQ, 0 to 100% Baseline mean: manip plus cntl 39.15, cntl 41.86 End of study mean: manip plus cntl 28.77, cntl 34.80 Absolute benefit: manip plus cntl 10.38, cntl 7.06 Reported results: significant favouring manipulation SMD: ‐0.38 (95% CI ‐0.77 to 0.01); NNTB 5 PARTICIPANT SATISFACTION: NR GPE: NR QoL: SF‐36 PCS and MCS PCS Baseline mean: manip plus cntl 38.35, cntl 35.35 End of study mean: manip plus cntl 41.24, cntl 35.67 Absolute benefit: manip plus cntl 2.89, cntl 0.32 Reported results: significant favouring manipulation SMD: ‐0.64 (95% CI ‐1.02 to ‐0.26) SIDE EFFECTS: none COST OF CARE: NR |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Page 142, left column, paragraphs 3 and 4 |
| Allocation concealment (selection bias) | Low risk | Page 142, left column, paragraphs 3 and 4 |
| Blinding of Participants (performance bias) | High risk | Not possible owing to intervention |
| Blinding of Personal (performance bias) | High risk | Not possible owing to intervention |
| Blinding of the Outcome assessor (detection bias) | High risk | Not possible owing to intervention |
| Incomplete outcome data (attrition bias) | Low risk | Figure 1 |
| Randomized Participants analysed were allocated (attrition bias) | Low risk | Figure 1 |
| Selective outcome (reporting bias) | Unclear risk | No protocol |
| Similar groups at baseline? | Low risk | Table 1 |
| co‐interventions avoided or similar? | Unclear risk | Not described |
| Compliance acceptable? | Unclear risk | Home exercise compliance not reported |
| Similar timing of outcome assessment? | Low risk | Baseline, immediate, 3 months, 6 months. Figure 1; page 142, right column, paragraph 4 |
Cleland 2005.
| Methods | Type of trial: RCT Number analysed/randomly assigned: 36/36 Intention‐to‐treat analysis: not applicable (NA) | |
| Participants | Chronic neck pain | |
| Interventions | INDEX TREATMENT
Manipulation (manip): technique: thoracic manip; frequency: 1 session; dose: 1 to 2 manip per segment, average 3.7 manip per participant; route: thoracic spine to each restricted segment COMPARISON TREATMENT Placebo manip (cntl): technique: use of flat open hand on participant naive to manip; frequency: 1 session; dose: average 3 placebo manip per participant; route: thoracic spine COINTERVENTION: NR Duration of therapy period: 1 session Duration of follow‐up: none |
|
| Outcomes | PAIN (VAS, 0 to 100) Baseline mean: manip 41.6, placebo 47.7 End of study mean: manip 26.1, cntl 43.5 Absolute benefit: manip 15.5, cntl 4.2 Reported results: significant favouring manipulation SMD: ‐0.93 (95% CI ‐1.62 to ‐0.24); NNTB 2; treatment advantage 29% FUNCTION: NR PARTICIPANT SATISFACTION: NR GPE: NR QoL: NR SIDE EFFECTS: none COST OF CARE: NR |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Page 129, column 1, paragraph 3 |
| Allocation concealment (selection bias) | Low risk | Page 129, column 1, paragraph 3 |
| Blinding of Participants (performance bias) | Low risk | Page 130, column 2, paragraph 2 |
| Blinding of Personal (performance bias) | High risk | Not possible owing to design |
| Blinding of the Outcome assessor (detection bias) | High risk | Not possible owing to design |
| Incomplete outcome data (attrition bias) | Low risk | Page 130, column 2, paragraph 2 |
| Randomized Participants analysed were allocated (attrition bias) | High risk | Not reported |
| Selective outcome (reporting bias) | Low risk | Protocol available |
| Similar groups at baseline? | Low risk | Table 1, page 131 |
| co‐interventions avoided or similar? | Low risk | Table 1, page 131 |
| Compliance acceptable? | Low risk | Pre‐test/Post‐test design |
| Similar timing of outcome assessment? | Low risk | Pre‐test/Post‐test design |
Coppieters 2003.
| Methods | Type of trial: RCT Number analysed/randomly assigned: 20/20 Intention‐to‐treat analysis: calculated | |
| Participants | Subacute/chronic neck pain | |
| Interventions | INDEX TREATMENT
Mobilisation (A): technique: Mobilisations included lateral glide techniques described by Elvey 1986 and Vicenzino et al 1999; the arm is progressively positioned from an unloaded toa preloaded position; frequency: 1 session; dose: mean 4.5‐minute treatment duration, session 1 grade 2 technique, session 2 to 3, grade 3 technique; route: C5 and C6 most frequently treated COMPARISON TREATMENT US (B): pulsed ultrasound CO‐INTERVENTION: NR Duration of therapy period: 1 session Duration of follow‐up: none |
|
| Outcomes | PAIN (NRS, 0 to 10) Baseline mean: A 7.3, B 7.7 End of study mean: A 5.8, B 7.4 Absolute benefit: A 1.5, B 0.3 Reported results: positive immediate effect favouring mobilisations: SMD (A vs B) ‐0.78, 95% CI‐1.70 to 0.13 (power 58%) FUNCTION: NR PARTICIPANT SATISFACTION: NR GPE: NR QoL: NR SIDE EFFECTS: NR COST OF CARE: NR |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomisation technique not specified |
| Allocation concealment (selection bias) | Unclear risk | Opaque sealed envelopes, not numbered |
| Blinding of Participants (performance bias) | High risk | Not possible owing to design |
| Blinding of Personal (performance bias) | High risk | Not possible owing to design |
| Blinding of the Outcome assessor (detection bias) | High risk | Not possible owing to design |
| Incomplete outcome data (attrition bias) | Low risk | Pre‐post design |
| Randomized Participants analysed were allocated (attrition bias) | Low risk | Pre‐post design |
| Selective outcome (reporting bias) | Unclear risk | No protocol published |
| Similar groups at baseline? | Low risk | Table 1 |
| co‐interventions avoided or similar? | Low risk | Pre‐post design |
| Compliance acceptable? | Low risk | Pre‐post design |
| Similar timing of outcome assessment? | Low risk | Pre‐post design |
David 1998.
| Methods | Type of trial: RCT Number analysed/randomly assigned: 51/70 Intention‐to‐treat analysis: NR | |
| Participants | Subacute, chronic neck pain with degenerative changes (i.e. cervical spondylosis), whiplash‐associated disorder (WAD) | |
| Interventions | INDEX TREATMENT
Physiotherapy (A): technique: standard localised mobilisation described by Maitland, rotation, posterior‐anterior oscillations, longitudinal traction; frequency: 1 session/wk; route: cervical spine COMPARISON TREATMENT Acupuncture (B): technique: local needling of trigger point, regional needling (GB21‐supraspinatus tender area), distal needling (LI4‐web space between thumb and first finger); frequency: 1 session/wk; dose: needle left in situ for 15 minutes; route: as described under technique CO‐INTERVENTION: NR Duration of treatment: 6 weeks, 6 sessions maximum Duration of follow‐up: 24 weeks |
|
| Outcomes | PAIN (VAS, 0 to 100) Baseline mean: A 51, B 51 End of study mean: A 22, B 28 Absolute benefit: A 29, B 23 Reported results: not significant SMD (A vs B): ‐0.33 (95% CI ‐0.89 to 0.23) (power 24%) FUNCTION (NPQ, 0 to 36) Baseline mean: A 36, B 36 End of study mean: A 22, B 25 Absolute benefit: A 14, B 11 Reported results: not significant SMD (A vs B): ‐0.16 (95% CI ‐0.72 to 0.39) (power 15%) PARTICIPANT SATISFACTION: NR GPE: NR QoL (GHQ 28, 0 to 28) Reported results: not significant RR (A vs B): 1.07 (95% CI 0.48 to 2.35) SIDE EFFECTS: no side effects with acupuncture COST OF CARE: NR |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomisation technique not specified |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of Participants (performance bias) | High risk | Not possible owing to study design |
| Blinding of Personal (performance bias) | High risk | Not possible owing to study design |
| Blinding of the Outcome assessor (detection bias) | High risk | Not possible owing to study design |
| Incomplete outcome data (attrition bias) | High risk | Page 1119, right column 2, dropout not described and exceeds 30% long term |
| Randomized Participants analysed were allocated (attrition bias) | High risk | Table 1: Numbers do not add up |
| Selective outcome (reporting bias) | Unclear risk | No published protocol |
| Similar groups at baseline? | Low risk | Figures 1, 2 and 3 |
| co‐interventions avoided or similar? | Unclear risk | Not described |
| Compliance acceptable? | Unclear risk | Not described |
| Similar timing of outcome assessment? | Low risk | Baseline, 6 weeks, 6 months |
Egwu 2008.
| Methods | Type of trial: quasi‐RCT Number analysed/randomly assigned: 95/96 Intention‐to‐treat analysis: not calculated | |
| Participants | Acute or subacute neck pain with degenerative changes ‐ cervical spondylosis of C5/6 | |
| Interventions | INDEX TREATMENT GROUPS
Posterior‐anterior‐unilateral pressure (A): technique: posterior‐anterior oscillatory pressure on the side of symptoms (Maitland); frequency: 3 times/wk; dose: 10 oscillations in 60 seconds; route: transverse processes of C5/6 Anterior‐posterior‐unilateral pressure (B): technique: anterior‐posterior oscillatory pressure on the side of symptoms (Maitland); frequency: 3 times/wk; dose: 10 oscillations in 60 seconds; route: transverse processes of C5/6 Cervical oscillatory rotation (C): technique: rotation oscillation by turning head and neck to the opposite side from the pain until pain is just elicited and then oscillations are given (Maitland); frequency: 3 times/wk; dose: 10 oscillations in 60 seconds; route: rotation performed with hands on jaw and occiput Transverse oscillatory pressure (D): technique: transverse oscillation produced by a push‐relax sequence on the spinous process using the thumbs to produce movement (Maitland); frequency: 3 times/wk; dose: 10 oscillations in 60 seconds; route: spinous processes of C5/6 CO‐INTERVENTION: NR Duration of treatment: 4 weeks or until pain was absent, 12 sessions maximum Duration of follow‐up: 0 days |
|
| Outcomes | PAIN STATUS (5 categories, pain free to worse) Reported results: NR RR (B vs A): 0.60 (95% CI 0.16 to 2.23) RR (B vs C): 0.29 (95% CI 0.09 to 0.91) RR (B vs D): 0.30 (95% CI 0.09 to 0.96) RR (A vs C): 0.48 (95% CI 0.19 to 1.19) RR (A vs D): 0.50 (95% CI 0.20 to 1.25) RR (A vs B): 1.67 (95% CI 0.45 to 6.21) MEAN TREATMENT TIME (minutes) Mean: A 161, B 130, C 201, D 221 Reported results: not significant RELAPSE AFTER 3 MONTHS (number reported) A 0, B 0, C 3, D 2 Reported results: NR FUNCTION: NR GPE: NR PARTICIPANT SATISFACTION: NR QoL: NR SIDE EFFECTS: NR COST OF CARE: NR |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Sequential ordering into groups, page 104 |
| Allocation concealment (selection bias) | High risk | Not possible with consecutive allocation. |
| Blinding of Participants (performance bias) | High risk | Not described as blinded in paper |
| Blinding of Personal (performance bias) | High risk | Not described as blinded in paper |
| Blinding of the Outcome assessor (detection bias) | High risk | Not described as blinded in paper |
| Incomplete outcome data (attrition bias) | High risk | Page 106, 13 dropouts were not described |
| Randomized Participants analysed were allocated (attrition bias) | Unclear risk | 13 dropouts were not described, but Table 1 seems to include all participants |
| Selective outcome (reporting bias) | Unclear risk | No protocol available |
| Similar groups at baseline? | Unclear risk | Data other than age not given |
| co‐interventions avoided or similar? | Unclear risk | Not stated |
| Compliance acceptable? | Unclear risk | Not mentioned |
| Similar timing of outcome assessment? | Unclear risk | Not clear when outcomes were taken |
Escortell‐Mayor 2011.
| Methods | Type of trial: RCT Number analysed/randomly assigned: 71/90 Intention‐to‐treat analysis: calculated | |
| Participants | Chronic non‐specific cervical disorder | |
| Interventions | INDEX TREATMENT
Manual therapy (A): technique: neuromuscular technique, post‐isometric, stretching, spray and stretching (Jones technique); timing: at baseline; frequency: 10 treatments on alternate days; duration: 30 minutes COMPARISON TREATMENT TENS (B): technique: TENS electrodes were placed in painful area, in the metamere or in the pathway of the nerve; timing: at baseline; frequency: 10 treatments; dose: 80 Hz at ≤ 150 μs; duration: 30 minutes CO‐INTERVENTION: not avoided: medication; avoided in trial design: other health professionals Duration of treatment: 1 month, 10 sessions Duration of follow‐up: 6 months, not specified for participant satisfaction |
|
| Outcomes | PAIN (VAS, 0 to 100 mm) Baseline mean: A 54.91, B 56.45 End of study mean: A 33.01, B 35.12 Absolute benefit: A 21.90, B 21.33 Reported results: not significant SMD (A vs B): IP ‐0.10 (95% CI ‐0.52 to 0.32), IT ‐0.12 (95% CI ‐0.59 to 0.34) FUNCTION (NDI, 0 to 50) Baseline mean: A 31.63, B 34.38 End of the study mean: A 22.23, B 23.90 Absolute benefit: A 9.40, B 10.48 Reported results: not significant SMD (A vs B): IP ‐0.12 (95% CI ‐0.54 to 0.30), IT 0.07 (95% CI ‐0.40 to 0.53) PATIENT SATISFACTION (Likert scale, 1 to 7) End of the study mean: unsatisfied: A 2, B 3, indifferent: A 0, B 2, satisfied: A 45, B 37 Reported results: not significant RR (A vs B): 1.09 (95% CI 0.96 to 1.23) GPE: NR QoL (PCS component of the SF‐12, 0 to 100) Baseline mean: A 43.26, B 42.66 End of the study mean: A 45.56, B 47.42 Absolute benefit: A 2.30, B 4.76 Reported results: not significant SMD (A vs B): IP ‐0.20 (95% CI ‐0.63 to 0.23), IT 0.22 (95% CI ‐0.25 to 0.68) SIDE EFFECTS: NR COST OF CARE: NR |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of block randomisation is not clearly stated; it is not clear whether complete blocks were done at each centre |
| Allocation concealment (selection bias) | Unclear risk | Envelopes were not numbered |
| Blinding of Participants (performance bias) | High risk | Not possible owing to design |
| Blinding of Personal (performance bias) | High risk | Not possible owing to design |
| Blinding of the Outcome assessor (detection bias) | High risk | Not possible owing to design |
| Incomplete outcome data (attrition bias) | Low risk | Figure 1 |
| Randomized Participants analysed were allocated (attrition bias) | Low risk | Page 69, paragraph 2 |
| Selective outcome (reporting bias) | Unclear risk | No protocol |
| Similar groups at baseline? | Low risk | Table 1 |
| co‐interventions avoided or similar? | Unclear risk | Not reported |
| Compliance acceptable? | Unclear risk | Home exercise compliance not reported |
| Similar timing of outcome assessment? | Low risk | Baseline, 1 month, 6 months |
Fernandez 2004 JWRD.
| Methods | Type of trial: RCT Number analysed/randomly assigned: 88/88 Intention‐to‐treat analysis: NA | |
| Participants | Acute, subacute neck pain ‐ WAD II or III | |
| Interventions | INDEX TREATMENT
Thoracic manipulation + active control (A): technique: thoracic manipulation and active control (same as comparison treatment); frequency: 2 manipulations over 2 weeks; 15 sessions over 3 weeks of control treatment; route: thoracic spine COMPARISON TREATMENT Ultrasound + active control (B): technique: ultrasound to neck, active exercises at home, muscle stretching, massage, multi‐modal care, electrotherapy, manual therapies; frequency: 15 sessions over 3 weeks CO‐INTERVENTION: NR Duration of treatment: 3 weeks, 15 sessions Duration of follow‐up: 0 days |
|
| Outcomes | PAIN (VAS, 0 to 10) Baseline mean: NR End of study mean: NR Absolute benefit: A 2.27, B 1.66 Reported results: significant favouring group A SMD:‐0.68 (95% CI ‐1.11 to ‐0.25); NNTB can calculate no baseline values FUNCTION: NR PARTICIPANT SATISFACTION: NR GPE: NR QoL: NR SIDE EFFECTS: NR COST OF CARE: NR |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Page 59, paragraph 3 |
| Allocation concealment (selection bias) | High risk | Not reported |
| Blinding of Participants (performance bias) | High risk | Not possible owing to design |
| Blinding of Personal (performance bias) | High risk | Not possible owing to design |
| Blinding of the Outcome assessor (detection bias) | High risk | Not possible owing to design |
| Incomplete outcome data (attrition bias) | Low risk | Page 56 |
| Randomized Participants analysed were allocated (attrition bias) | Low risk | Page 59, paragraph 3 |
| Selective outcome (reporting bias) | Unclear risk | No protocol reported |
| Similar groups at baseline? | High risk | Reported only male/female and mean age |
| co‐interventions avoided or similar? | High risk | Not reported |
| Compliance acceptable? | Low risk | Short‐term follow‐up |
| Similar timing of outcome assessment? | Low risk | Baseline, 3 weeks |
Fernandez 2009.
| Methods | Type of trial: RCT Number analysed/randomly assigned: 45/45 Intention‐to‐treat analysis: NA | |
| Participants | Acute mechanical neck pain | |
| Interventions | INDEX TREATMENT
Group A: technique: mid‐thoracic distraction manipulation plus electro/thermotherapy programme (same as comparison treatment); frequency: 5 sessions over 3 weeks; dose: 3 manipulations over 3 weeks; route: thoracic spine COMPARISON TREATMENT Group B: (electro/thermotherapy programme) type: infrared lamp dose: 250 watts; duration: 15 minutes, route: 50 cm from neck. type: transcutaneous electrical nerve stimulation; dose: 100 Hz and 50 microsecond pulse; duration: 20 minutes; frequency: 5 sessions over 3 weeks CO‐INTERVENTION: NR Duration of treatment: 3 weeks, 5 sessions Duration of follow‐up: immediate post intervention |
|
| Outcomes | PAIN (VAS, 0 to 100) Baseline mean: group A 54.7, group B 52.7 End of study mean: group A 20.2, group B 44.7 Absolute benefit: group A 24.5, group B 8 Reported results: significant favouring group A SMD: ‐3.48 (95% CI ‐4.43 to ‐2.53); NNTB 4 FUNCTION: NR PATIENT SATISFACTION: NR GPE: NR QoL: NR SIDE EFFECTS: NR COST OF CARE: NR |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Page 155, column 3, paragraph 2 |
| Allocation concealment (selection bias) | Low risk | Page 155, column 3, paragraph 2 |
| Blinding of Participants (performance bias) | High risk | Not possible owing to differences between interventions |
| Blinding of Personal (performance bias) | High risk | Not possible |
| Blinding of the Outcome assessor (detection bias) | High risk | Not possible owing to differences between interventions |
| Incomplete outcome data (attrition bias) | Low risk | Figure 1, page 157, middle of paragraph 2 |
| Randomized Participants analysed were allocated (attrition bias) | Low risk | No dropouts |
| Selective outcome (reporting bias) | High risk | No reporting of Norwick follow‐up scores but measured at baseline |
| Similar groups at baseline? | Low risk | Table 1 |
| co‐interventions avoided or similar? | Unclear risk | Not reported |
| Compliance acceptable? | Low risk | Page 156, column 3, paragraph 1 |
| Similar timing of outcome assessment? | Low risk | No dropouts |
Gemmell 2010.
| Methods | Type of trial: RCT Number analysed/randomly assigned: 36/47 Intention‐to‐treat analysis: calculated | |
| Participants | Subacute mechanical neck pain | |
| Interventions | INDEX TREATMENT
Manipulation (A): technique: high velocity, low amplitude; timing: at baseline; frequency: 2 treatments/wk for 3 weeks; dose: 1 or 2 dynamic thrust; duration: 10 to 15 minutes; route: 1 or more restricted upper thoracic or cervical spine segments Mobilisation (B): technique: posterior‐anterior and transverse oscillations to the articular pillar and spinous process; timing: at baseline; frequency: 2 treatments/wk for 3 weeks; dose: grade III mobilisation; duration: 10 to 15 minutes; route: 1 or more restricted upper thoracic or cervical spine segments COMPARISON TREATMENT Activator instrument (C): technique: application of the instrument over the articular pillar in line with the facet joint, with the patient prone and with a setting of 1 for the Atlas and 2 for the cervical and upper thoracic segments; timing: at baseline; frequency: 2 treatments/wk for 3 weeks; dose: 1 thrust; duration: 10 to 15 minutes; route: 1 or more restricted upper thoracic or cervical spine segments CO‐INTERVENTION: not avoided: medication (specify: paracetamol 500 mg was allowed as rescue medication); avoided in trial design: other health professional (specify: Participant agreed not to take medication or receive other treatment for neck pain during the course of the study); comparable between index and control groups: package of care (specify: trigger point pressure release to active trigger points; post‐isometric relaxation stretching; exercise and ergonomic advice, use of rescue medication) Duration of treatment: 3 weeks or until symptom free, 6 sessions maximum Duration of follow‐up: 12 months |
|
| Outcomes | PAIN (11‐point pain scale, 0 to 10) Reported results (as reported in the article): no significant differences between groups at any follow‐up points FUNCTION (Neck Bournemouth Questionnaire, 0 to 70) Reported results (as reported in the article): no significant differences between groups at any follow‐up points PATIENT SATISFACTION: NR GPE (PGIC, 7‐point scale) Reported results (as reported in the article): no significant differences between groups for any follow‐up points QoL (PCS component of SF‐36, 0 to 100) Reported results (as reported in the article): no significant differences between groups at any follow‐up points SIDE EFFECTS Mildly increased neck pain: A 4/16, B 2/15, C 7/16 Mild radiating pain: A 2/16, B 1/15, C 5/16 Mild arm weakness: A 0/16, B 0/15, C 1/16 Mild arm numbness: A 0/16, B 0/15, C 1/16 Mild headache: A 3/16, B 4/15, C 3/16 Mild fatigue: A 3/16, B 0/15, C 3/16 Mild dizziness: A 1/16, B 1/15, C 1/16 Mild muscle twitching: A 1/16, B 0/15, C 0/16 COST OF CARE: NR |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Page 3, left column, paragraph 2 |
| Allocation concealment (selection bias) | Low risk | Page 3, left column, paragraph 2 |
| Blinding of Participants (performance bias) | High risk | Not possible owing to perceptible differences between interventions |
| Blinding of Personal (performance bias) | High risk | Not possible owing to perceptible differences between interventions |
| Blinding of the Outcome assessor (detection bias) | High risk | Not possible owing to perceptible differences between interventions |
| Incomplete outcome data (attrition bias) | Unclear risk | Not adequately described |
| Randomized Participants analysed were allocated (attrition bias) | Low risk | Page 5, left column, paragraph 2 |
| Selective outcome (reporting bias) | Unclear risk | No protocol |
| Similar groups at baseline? | High risk | Table 1 |
| co‐interventions avoided or similar? | Unclear risk | Not reported |
| Compliance acceptable? | Unclear risk | Not reported |
| Similar timing of outcome assessment? | Low risk | Baseline, 3, 6, 12 months |
Giles 1999.
| Methods | Type of trial: RCT Number analysed/randomly assigned: 98/157 for all spinal patients; 62/x for neck subgroup Intention‐to‐treat analysis: NR | |
| Participants | Chronic neck pain with degenerative changes | |
| Interventions | INDEX TREATMENT
Manipulation (A): technique: high‐velocity low‐amplitude manipulation; frequency: 6 sessions/median 19 days; dose: 15‐ to 20‐minute appointment; route: cervical spine COMPARISON TREATMENT Acupuncture (B): technique: 8 to 10 needles with low‐volt electrical stimulation to tender points; frequency: 6 sessions/median 40 days Medication (C): tenoxicam (NSAID) with ranitidine, median 15 days CO‐INTERVENTION: NR Duration of treatment: 3 to 4 weeks, 6 sessions Duration of follow‐up: none |
|
| Outcomes | PAIN (neck pain change scores, VAS, 0 to 10) Baseline median: A 4.5, B 2.0, C 4.0 Absolute benefit: A 1.5, B 1.0, C 0.5 Reported results: not clear SMD (A vs C): ‐0.19 (95% CI ‐0.89 to 0.51) SMD (A vs B): ‐0.13 (95% CI ‐0.78 to 0.52) FUNCTION (NDI, 0 to 50) Baseline median: A 32, B 40, C 28 Absolute benefit: A 10.0, B 6.0, C 0.0 Reported results: not clear SMD (A vs C): ‐0.50 (95% CI ‐1.30 to 0.29) SMD (A vs B): ‐0.18 (95% CI ‐0.96 to 0.60) PATIENT SATISFACTION: NR GPE: NR QoL: NR SIDE EFFECTS: no side effects seen with acupuncture or manipulation COST OF CARE: NR |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Page 377, left column, paragraph 3 |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of Participants (performance bias) | High risk | Not possible owing to design |
| Blinding of Personal (performance bias) | High risk | Not possible owing to design |
| Blinding of the Outcome assessor (detection bias) | High risk | Not possible owing to design |
| Incomplete outcome data (attrition bias) | High risk | Page 378, left column, paragraph 2 |
| Randomized Participants analysed were allocated (attrition bias) | High risk | Numbers in Table 1 and Table 2 do not add up |
| Selective outcome (reporting bias) | Unclear risk | No reported protocol |
| Similar groups at baseline? | High risk | Table 1 |
| co‐interventions avoided or similar? | Unclear risk | Not described |
| Compliance acceptable? | Unclear risk | Not described |
| Similar timing of outcome assessment? | Low risk | Baseline, 4 weeks |
Gonzalez‐Iglesias 2009 JO.
| Methods | Type of trial: RCT
Number analysed/randomly assigned: 45/45
Intention‐to‐treat analysis: NA Protocol: The protocol for this study was approved by the Human Research Committee of the Escuela de Osteopatía de Madrid |
|
| Participants | Acute neck pain | |
| Interventions | INDEX TREATMENT
Thoracic spine thrust manipulation (TSM): technique: seated distraction manipulation ‐ participant had arms across chest, therapist gently flexed the thoracic spine until tension was felt, and then a distraction thrust manipulation was applied. If no pop was heard, a second attempt was made; frequency: 1 session/wk; dose: grade 5 manipulation; route: thoracic spine Electrothermal therapy (ETT): type: infrared lamp and TENS; frequency: 2 sessions/wk; dose: infrared 250 W for 15 minutes, TENS 100 Hz for 20 minutes; route: infrared lamp 50 cm from the participant's neck, TENS applied to each side of C7 COMPARISON TREATMENT Electrothermal therapy (ETT): type: infrared lamp and TENS; frequency: 2 sessions/wk; dose: infrared 250 W for 15 minutes, TENS 100 Hz for 20 minutes; route: infrared lamp 50 cm from the participant's neck, TENS applied to each side of C7 CO‐INTERVENTION: NR Duration of treatment: 3 weeks, 5 sessions Duration of follow‐up: 4 weeks |
|
| Outcomes | PAIN (intensity at rest change score, VAS, 0 to 100) Baseline mean: TSM + ETT 54.7, ETT 52.7 IP treatment mean: TSM + ETT 20.2, ETT 44.7 2‐Week follow‐up mean: TSM + ETT 26.4, ETT 41.2 4‐Week follow‐up mean: TSM + ETT 21.5, ETT 42.2 Reported results: significant for comparisons at all time points IP treatment SMD (TSM + ETT vs ETT): ‐3.43 (95% CI ‐4.38 to ‐2.49) 4‐Week follow‐up SMD (TSM + ETT vs ETT): ‐2.19 (95% CI‐2.94 to ‐1.44); NNTB 7 FUNCTION (Northwich Park Pain Questionnaire, 0 to 36) Baseline mean: TSM + ETT 27.9, ETT 27.0 IP treatment mean: TSM + ETT 15.2, ETT 23.1 2‐Week follow‐up mean: TSM + ETT 14.7, ETT 21.8 Reported results: significant for comparisons at all time points IP treatment SMD (TSM + ETT vs ETT): ‐2.17 (95% CI ‐2.92 to ‐1.42) 2‐Week follow‐up SMD (TSM + ETT vs ETT): ‐2.28 (95% CI ‐3.05 to ‐1.52); NNTB 5 4‐Week follow‐up: not collected GPE: NR PATIENT SATISFACTION: NR QoL: NR SIDE EFFECTS: NR COST OF CARE: NR |
|
| Notes | For 4‐week disability (NPPQ) data: "We only collected changes in disability up to the 2‐week follow‐up period. It would have been beneficial to see if these benefits remain at 1‐month, similar to the improvements in pain" | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Page 21, column 3, paragraph 3 |
| Allocation concealment (selection bias) | Low risk | Page 21, column 3, paragraph 3 |
| Blinding of Participants (performance bias) | High risk | Participants in control did not receive sham or placebo |
| Blinding of Personal (performance bias) | High risk | Not possible owing to intervention |
| Blinding of the Outcome assessor (detection bias) | High risk | Not possible as participant was assessor of pain |
| Incomplete outcome data (attrition bias) | Low risk | No dropouts |
| Randomized Participants analysed were allocated (attrition bias) | Low risk | No dropouts |
| Selective outcome (reporting bias) | Unclear risk | No reported protocol |
| Similar groups at baseline? | Low risk | |
| co‐interventions avoided or similar? | Unclear risk | Not mentioned |
| Compliance acceptable? | Unclear risk | Not mentioned |
| Similar timing of outcome assessment? | Low risk | |
Gonzalez‐Iglesias 2009 MT.
| Methods | Type of trial: RCT
Number analysed/randomly assigned: 45/45
Intention‐to‐treat analysis: calculated Location of study: Spain |
|
| Participants | Acute mechanical neck pain | |
| Interventions | INDEX TREATMENT
Thoracic spine thrust manipulation plus control (EG: TSM + ETT): technique: seated distraction manipulation ‐ participant had arms across chest, therapist gently flexed the thoracic spine until tension was felt, and then a distraction thrust manipulation was applied. If no pop was heard, a second attempt was made; frequency: 1 session/wk for 3 weeks; dose: grade 5 manipulation; route: thoracic spine Electrothermal therapy (ETT): type: infrared lamp and TENS; frequency: 2 sessions/wk for 3 weeks; dose: infrared 250 W for 15 minutes, TENS 100 Hz for 20 minutes; route: infrared lamp 50 cm from the participant's neck, TENS applied bilaterally to spinous process of C7 COMPARISON TREATMENT Electrothermal therapy (CG: ETT): type: infrared lamp and TENS; frequency: 2 sessions/wk for 3 weeks; dose: infrared 250 W for 15 minutes, TENS 100 Hz for 20 minutes; route: infrared lamp 50 cm from the participant's neck, TENS applied bilaterally to spinous process of C7 CO‐INTERVENTION: NR Duration of treatment: 3 weeks, 6 sessions Duration of follow‐up: 1 week post last treatment |
|
| Outcomes | PAIN INTENSITY NRPS (0 to 10) Baseline mean: EG 5.6, CG 5.37 End of study mean: EG 2.3, CG 4.3 Absolute benefit: EG 3.3, CG 1.07 Reported results: significant favouring EG SMD: ‐2.16 (95% CI ‐2.91 to ‐1.42); NNTB 5 FUNCTION (NPQ, 0 to 36) Baseline mean: EG 27.8, CG 27.1 End of study mean: EG 15.2, CG 22.9 Absolute benefit: EG 12.6, CG 4.2 Reported results: significant favouring EG SMD: ‐2.12 (95% CI ‐2.87 to ‐1.38); NNTB 4 PATIENT SATISFACTION: NR QoL: NR GPE: NR SIDE EFFECTS: NR COST OF CARE: NR |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Page 308, column 1, paragraph 4 |
| Allocation concealment (selection bias) | Low risk | Page 308, column 1, paragraph 4 |
| Blinding of Participants (performance bias) | Low risk | Not possible owing to design |
| Blinding of Personal (performance bias) | High risk | Not possible owing to design |
| Blinding of the Outcome assessor (detection bias) | Low risk | Not possible owing to design |
| Incomplete outcome data (attrition bias) | Low risk | Page 309, Figure 2 |
| Randomized Participants analysed were allocated (attrition bias) | Low risk | Page 309, Figure 2 |
| Selective outcome (reporting bias) | Unclear risk | Not reported |
| Similar groups at baseline? | Low risk | Page 310, Table 1 |
| co‐interventions avoided or similar? | Low risk | Pre‐post design |
| Compliance acceptable? | Low risk | Pre‐post design |
| Similar timing of outcome assessment? | Low risk | Baseline, 1 week after discharge |
Haas 2004.
| Methods | Type of trial: RCT Number analysed/randomly assigned: 25/26 Intention‐to‐treat analysis: calculated | |
| Participants | Chronic neck pain with headache | |
| Interventions | INDEX TREATMENT
Group 4 sessions/wk (12s): technique: manipulation: high‐velocity low‐amplitude manipulation; frequency: 4 sessions/wk; route: cervical spine Group 3 sessions/wk (9s): technique: manipulation: high‐velocity low‐amplitude manipulation; frequency: 3 sessions/wk; route: cervical spine COMPARISON TREATMENT Group 1 session/wk (3s): technique: high‐velocity low‐amplitude manipulation; frequency: 1 session/wk; route: cervical spine CO‐INTERVENTION: comparable between groups: heat, soft tissue therapy with massage, trigger point therapy, education (modification of ADLs), rehabilitation exercises Duration of treatment: 3 weeks, 9 to 12 sessions Duration of follow‐up: 1 week post treatment, 9 weeks post treatment |
|
| Outcomes | PAIN (neck pain, modified von Korff scale, 0 to 100)
Baseline mean: 12s 49.6, 9s 58.7, 3s 61.0
Absolute benefit: 12s 18.8, 9s 31.7, 3s 18.6
Reported results: Findings give preliminary support for larger doses at 9 to 12 sessions
SMD (12s vs 3s): ST ‐1.35 (95% CI ‐2.51 to ‐0.19); NNTB 12, treatment advantage 23%
SMD (12s vs 3s): IT ‐0.48 (95% CI ‐1.51 to 0.56)
SMD (12s vs 9s): 0.17 (95% CI ‐0.81 to 1.16) (power 60%)
SMD (9s vs 3s): ‐0.90 (95% CI ‐1.98 to 0.18) (power 69%) FUNCTION (neck disability modified von Korff scale, 0 to 100) Baseline mean: 12s 33.8, 9s 35.7, 3s 46.7 Absolute benefit: 12s 20.1, 9s 22.5, 3s 13.4 Reported results: Findings give preliminary support for larger doses at 9 to 12 sessions SMD (12s vs 3s): ST ‐1.36 (95% CI ‐2.52 to ‐0.20); NNTB 12, treatment advantage 23% SMD (12s vs 3s): IT ‐1.15 (95% CI ‐2.27 to ‐0.03) SMD (12s v 9s): ‐0.03 (95% CI ‐1.01 to 0.95) (power 56%) SMD (9s vs 3s): ‐1.47 (95% CI ‐2.65 to ‐0.28) PATIENT SATISFACTION: NR GPE: NR QoL: NR SIDE EFFECTS: none COST OF CARE: NR |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Page 548, under design |
| Allocation concealment (selection bias) | Unclear risk | Opaque sealed envelopes, not numbered |
| Blinding of Participants (performance bias) | High risk | Not possible owing to design |
| Blinding of Personal (performance bias) | High risk | Not possible owing to design |
| Blinding of the Outcome assessor (detection bias) | High risk | Not possible owing to design |
| Incomplete outcome data (attrition bias) | Low risk | Page 550, compliance and dropout |
| Randomized Participants analysed were allocated (attrition bias) | High risk | One participant lost for analysis |
| Selective outcome (reporting bias) | Unclear risk | No reported protocol |
| Similar groups at baseline? | High risk | Table 2 |
| co‐interventions avoided or similar? | High risk | Table 3 |
| Compliance acceptable? | Low risk | Page 550, right column, paragraph 2 |
| Similar timing of outcome assessment? | Low risk | Baseline, 4 weeks, 12 weeks |
Haas 2010.
| Methods | Type of trial: RCT Number analysed/randomly assigned: 72/80 Intention‐to‐treat analysis: calculated | |
| Participants | Chronic cervicogenic headache (migraine + tension type concomitant) | |
| Interventions | INDEX TREATMENT
Manipulation 8 treatments (A): technique: high‐velocity low‐amplitude spinal manipulation with light massage (2 minutes) before treatment; timing: at baseline; frequency: 1×/wk for 8 weeks (+ 1 assessment/wk); duration: 10 minutes; route: cervical spine and upper thoracic Manipulation 16 treatments (B): technique: high‐velocity low‐amplitude spinal manipulation with light massage (2 minutes) before treatment; timing: at baseline; frequency: 2×/wk for 8 weeks; duration: 10 minutes; route: cervical spine and upper thoracic COMPARISON TREATMENT Massage 8 treatments (C): technique: low‐intensity manual therapy consisting of gentle effleurage (gliding) and gentle pétrissage (kneading); timing: at baseline; frequency: 1×/wk for 8 weeks (+ 1 assessment/wk); duration: 10 minutes; route: neck and shoulder muscles Massage 16 treatments (D): technique: low‐intensity manual therapy consisting of gentle effleurage (gliding) and gentle pétrissage (kneading); timing: at baseline; frequency: 2×/wk for 8 weeks; duration: 10 minutes; route: neck and shoulder muscles CO‐INTERVENTION Not avoided: alternative health care avoided in inclusion criteria, but 10 participants had recourse to other professionals during treatment (outside care visits were balanced across groups and were not correlated with pain improvement at between four and 24 weeks); comparable between index and control groups: palliative drug use, application of heat pack (5 minutes) before treatment Duration of treatment: 8 weeks, maximum 16 sessions Duration of follow‐up: 16 weeks |
|
| Outcomes | PAIN (VAS, 0 to 100)
Baseline mean: A 53.3, B 53.0, C 60.5, D 59.0
End of study mean: A 38.3, B 28.2, C 42.8, D 48.4
Absolute benefit: A 15.0, B 24.8, C 17.7, D 10.6
Reported results: significant favouring B over D at intermediate term SMD (B vs A): ST ‐0.16 (95% CI ‐0.86 to 0.53), IT ‐0.37 (95% CI ‐1.04 to 0.30) SMD (B vs D): ST ‐0.60 (95% CI ‐1.31 to 0.11), IT ‐0.79 (95% CI ‐1.47 to ‐0.11); NNTB 5, treatment advantage 29% FUNCTION (neck pain, modified von Korff scale, 0 to 100) Baseline mean: A 46.3, B 36.2, C 48.5, D 41.6 End of study mean: A 23.5, B 15.9, C 28.3, D 34.7 Absolute benefit: A 22.8, B 20.3, C 20.2, D 6.9 Reported results: significant favouring B over D at short and intermediate term SMD (B vs A): ST ‐0.35 (95% CI ‐1.05 to 0.35), IT ‐0.32 (95% CI ‐0.98 to 0.35) SMD (B vs D): ST ‐0.87 (95% CI ‐1.60 to ‐0.14), NNTB 5; treatment advantage 29% SMD (B vs D): IT ‐0.72 (95% CI ‐1.39 to ‐0.04); NNTB 5, treatment advantage 39% GPE: NR PATIENT SATISFACTION: NR QoL: NR SIDE EFFECTS: NR COST OF CARE: NR |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Page 118, right column, paragraph 4 |
| Allocation concealment (selection bias) | Low risk | Page 118, right column, paragraph 4 |
| Blinding of Participants (performance bias) | High risk | Not possible owing to design |
| Blinding of Personal (performance bias) | High risk | Not possible owing to design |
| Blinding of the Outcome assessor (detection bias) | High risk | Not possible owing to design |
| Incomplete outcome data (attrition bias) | Low risk | Figure 1, page 121, right column, paragraph 1 |
| Randomized Participants analysed were allocated (attrition bias) | Low risk | Tables 2 and 3 legends |
| Selective outcome (reporting bias) | Unclear risk | No protocol available |
| Similar groups at baseline? | High risk | Disabilities for CGH and neck pain were clinically different |
| co‐interventions avoided or similar? | Low risk | Page 122, left column, paragraph 1 |
| Compliance acceptable? | Low risk | Page 118, right column, paragraph 5 |
| Similar timing of outcome assessment? | Low risk | Abstract |
Howe 1983.
| Methods | Type of trial: RCT Number analysed/randomly assigned: 44/52 Intention‐to‐treat analysis: calculated | |
| Participants | Subacute, chronic neck pain with radicular findings and headache | |
| Interventions | INDEX TREATMENT
Manipulation (A): technique: manipulation and azapropazone; frequency: 1 session; dose: up to 3 manipulations; route: cervical spine COMPARISON TREATMENTS Medication (B): type: azapropazone; dose: NR CO‐INTERVENTION: 2 participants in manipulation group had lignocaine‐hydrocortisone injections Duration of treatment: 1 session Duration of follow‐up: 3 weeks |
|
| Outcomes | PAIN (count, neck/shoulder/arm/hand pain and headache present)
Baseline mean: NR
Reported results: significant favouring A
RR: 0.56 (95% CI 0.19 to 1.68) (power 18%) FUNCTION: NR PARTICIPANT SATISFACTION: NR GPE: NR QoL: NR SIDE EFFECTS: NR COST OF CARE: NR |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Page 574, column 2, paragraph 3 |
| Allocation concealment (selection bias) | Low risk | Page 574, column 2, paragraph 3 |
| Blinding of Participants (performance bias) | High risk | Not possible owing to design |
| Blinding of Personal (performance bias) | High risk | Not possible owing to design |
| Blinding of the Outcome assessor (detection bias) | Low risk | Page 574, column 2, paragraph 3 |
| Incomplete outcome data (attrition bias) | High risk | Page 578, Table 4 |
| Randomized Participants analysed were allocated (attrition bias) | High risk | Not reported |
| Selective outcome (reporting bias) | Unclear risk | No reported protocol |
| Similar groups at baseline? | High risk | Page 575, Table 2 |
| co‐interventions avoided or similar? | High risk | Not reported |
| Compliance acceptable? | High risk | Not reported |
| Similar timing of outcome assessment? | Low risk | Baseline, 1 week, 3 weeks |
Hurwitz 2002.
| Methods | Type of trial: RCT (2 × 2 × 2 factorial design) Number analysed/randomly assigned: 269/336 Intention‐to‐treat analysis: done by design | |
| Participants | Subacute chronic neck pain with or without radicular symptoms and headache | |
| Interventions | INDEX TREATMENTS
Manipulation (Manip): technique: controlled, dynamic thrust applied with high‐velocity low‐amplitude force with minimal extension and rotation; frequency: NR; dose: at least 1 manipulation; route: directed at 1 or more restricted upper thoracic or cervical spine joint segments Manipulation with heat (Manip + H): 10‐minute moist heat application before manipulation Manipulation with EMS (Manip + EMS): 10‐minute application of this modality before manipulation; parameters NR Mobilisation (Mob): technique: low‐velocity variable‐amplitude movements applied within the individual's passive range of motion directed to 1 or more restricted upper thoracic or cervical spine joint segments; frequency: NR; route: cervical spine and thoracic spine Mobilisation with heat (Mob + H): 10‐minute moist heat application before mobilisation Mobilisation with EMS (Mob + EMS): 10‐minute application of this modality before mobilisation; parameters NR COMPARISON TREATMENTS Any of the above noted treatment combinations CO‐INTERVENTION: All participants received information on posture and body mechanics and 1 or more of the following ‐ stretching, flexibility or strengthening exercises ‐ and advice about ergonomic and workplace modifications. Duration of treatment: NR Duration of follow‐up: 6 months |
|
| Outcomes | PAIN INTENSITY (average pain during previous week, most severe pain, NRS, 0 to 10)
Baseline mean: NR for each subgroup
End of study mean: NR for each subgroup
Reported results: no significant differences, heat therapies: condition improved slightly more, and differences were clinically negligible (=?). Significant favouring the combination of manipulation, electrical stimulation and heat over mobilisation, electrical stimulation and heat
SMD (Manip vs Mob): 0.15 (95% CI: ‐0.32 to 0.61) SMD (Manip + EMS vs Mob + EMS): 0.32 (95% CI ‐0.16 to 0.8) SMD (Manip + EMS + H vs Mob + EMS + H): ‐0.62 (95% CI ‐1.12 to ‐0.11) SMD (Manip + H vs Mob + H): ‐0.17 (95% CI ‐0.64 to 0.31) RR (heat vs no heat): 1.14 (95% CI mixed: 0.95 to 1.37) RR (EMS vs no EMS): 0.90 (95% CI mixed: 0.73 to 1.13) FUNCTION (NDI, 0 to 50) Baseline mean: NR for each subgroup End of study mean: NR for each subgroup Reported results: no significant difference SMD (Manip vs Mob): 0.07 (95% CI ‐0.40 to 0.54) (power 66%) SMD (Manip + EMS + H vs Mob + EMS + H): ‐0.28 (95% CI ‐0.77 to 0.22) SMD (Manip + EMS vs Mob + EMS): 0.37 (95% CI ‐0.10 to 0.85) SMD (Manip + H vs Mob + H): ‐0.18 (95% CI ‐0.66 to 0.29) RR (heat vs no heat): 1.14 (95% CI mixed: 0.94 to 1.38) RR (EMS vs no EMS): 0.87 (95% CI mixed: 0.69 to 1.10) SATISFACTION (10 to 50 scale; at 4w of care) SMD (Manip vs Mob): 0.11 (95% CI ‐0.34 to 0.57) SMD (Manip + EMS + H vs Mob + EMS + H): 0.14 (95% CI ‐0.31 to 0.59) SMD (Manip + EMS vs Mob + EMS): 0.11 (95% CI ‐0.35 to 0.56) SMD (Manip + H vs Mob + H): ‐0.28 (95% CI ‐0.72 to 0.17) GPE: NR QoL: NR PATIENT SATISFACTION: NR SIDE EFFECTS: interviewed at 4 weeks of care, no known study‐related adverse events; manipulation group had statistically significant more transient minor discomfort (16%) vs mobilisation group (8.7%) COST OF CARE: number of disability days not significantly different between groups |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Page 1634, middle column, paragraph 2 |
| Allocation concealment (selection bias) | Low risk | Page 1634, middle column, paragraph 2 |
| Blinding of Participants (performance bias) | High risk | Not possible owing to differences in treatment methods |
| Blinding of Personal (performance bias) | High risk | Not possible |
| Blinding of the Outcome assessor (detection bias) | High risk | Subjective rating of pain |
| Incomplete outcome data (attrition bias) | Low risk | Page 1636, paragraph 2 |
| Randomized Participants analysed were allocated (attrition bias) | Unclear risk | Intention‐to‐treat not described |
| Selective outcome (reporting bias) | Unclear risk | Not described |
| Similar groups at baseline? | Low risk | Table 1 |
| co‐interventions avoided or similar? | Unclear risk | Not described |
| Compliance acceptable? | Unclear risk | Not described |
| Similar timing of outcome assessment? | Low risk | Baseline, 2 weeks, 6 weeks, 3 months, 6 months |
Kanlayanaphotporn 2009.
| Methods | Type of trial: RCT Number analysed/randomly assigned: 60/60 Intention‐to‐treat analysis: NA | |
| Participants | Chronic neck pain | |
| Interventions | INDEX TREATMENT
Preferred mobilisation (A): technique: posterior‐anterior pressure on the side of symptoms; frequency: 1 session; dose: 2 × 1 minute mobilisations graded 1 to 2 for pain and 3 to 4 for stiffness; route: articular processes of cervical spine COMPARISON TREATMENT Random mobilisation (B): technique: 1 of 3 techniques selected (1) central posterior‐anterior pressure, (2) ipsilateral posterior‐anterior pressure, (3) contralateral posterior‐anterior pressure; frequency: 1 session; dose 2 × 1 minute mobilisations; route: articular processes of cervical spine CO‐INTERVENTION: NR Duration of treatment: 1 session Duration of follow‐up: none |
|
| Outcomes | PAIN (intensity with most painful movement, VAS, 0 to 100)
Baseline mean: A 59.5, B 61.6
Absolute benefit: A 16.7, B 16.9
Reported results: not significant
SMD (A vs B): 0.01 (95% CI ‐0.49 to 0.52) FUNCTION: NR GPE (1 to 7) Reported results: not significant RR (A vs B): 1.12 (95% CI 0.74 to 1.6) PATIENT SATISFACTION: NR QoL: NR SIDE EFFECTS: NR COST OF CARE: NR |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Page 189, right column, paragraph 2 |
| Allocation concealment (selection bias) | Low risk | Page 189, right column, paragraph 2 |
| Blinding of Participants (performance bias) | Low risk | Different treatments were not perceptually different to participants |
| Blinding of Personal (performance bias) | High risk | Not possible owing to design |
| Blinding of the Outcome assessor (detection bias) | Low risk | Participant is the assessor and is blinded |
| Incomplete outcome data (attrition bias) | Low risk | No dropouts |
| Randomized Participants analysed were allocated (attrition bias) | Low risk | Pre‐post design |
| Selective outcome (reporting bias) | Unclear risk | No pilot study available |
| Similar groups at baseline? | Low risk | Table 1 |
| co‐interventions avoided or similar? | Low risk | Pre‐post study, no opportunity for co‐intervention |
| Compliance acceptable? | Low risk | Pre‐post study |
| Similar timing of outcome assessment? | Low risk | Pre‐post study |
Kanlayanaphotporn 2010a.
| Methods | Type of trial: RCT Number analysed/randomly assigned: 60/60 Intention‐to‐treat analysis: NA | |
| Participants | Chronic neck pain | |
| Interventions | INDEX TREATMENT
Central posterior‐anterior mobilisation (A): technique: posterior‐anterior pressure over the spinous process of restricted segments; frequency: 1 session; dose: 2 × 1 minute mobilisations graded 1 to 2 for pain and 3 to 4 for stiffness; route: spinous processes of cervical spine COMPARISON TREATMENT Random mobilisation (B): technique: 1 of 3 techniques selected: (1) central posterior‐anterior pressure, (2) ipsilateral posterior‐anterior pressure, (3) contralateral posterior‐anterior pressure; frequency: 1 session; dose: 2 × 1 minute mobilisations; route: articular processes of cervical spine CO‐INTERVENTION: NR Duration of treatment: 1 session Duration of follow‐up: none |
|
| Outcomes | PAIN (intensity with most painful movement change score, VAS, 0 to 100)
Baseline mean: A 60.8, B 59.8
Absolute benefit: A 21.9, B 12.7
Reported results: significant favouring A
SMD (A vs B): ‐0.53 (95% CI ‐1.04 to ‐0.01) FUNCTION: NR GPE (1 to 7) Reported results: not significant RR (A vs B): 0.90 (95% CI 0.63 to 1.30) PATIENT SATISFACTION: NR QoL: NR SIDE EFFECTS: NR COST OF CARE: NR |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Page 624, right column, paragraph 2 |
| Allocation concealment (selection bias) | Low risk | Page 624, right column, paragraph 2 |
| Blinding of Participants (performance bias) | Low risk | Page 624, right column, paragraphs 3 and 4 |
| Blinding of Personal (performance bias) | High risk | Not possible owing to design |
| Blinding of the Outcome assessor (detection bias) | Low risk | Page 624, right column, paragraphs 3 and 4 |
| Incomplete outcome data (attrition bias) | Low risk | Pre‐post design |
| Randomized Participants analysed were allocated (attrition bias) | Low risk | Pre‐post design |
| Selective outcome (reporting bias) | Unclear risk | No reported protocol available |
| Similar groups at baseline? | Low risk | Table 1 |
| co‐interventions avoided or similar? | Low risk | Pre‐post design |
| Compliance acceptable? | Low risk | Pre‐post design |
| Similar timing of outcome assessment? | Low risk | Pre‐post design |
Krauss 2008.
| Methods | Type of trial: RCT Number analysed/randomly assigned: 32/32 Intention‐to‐treat analysis: NA | |
| Participants | Neck pain (duration of symptoms NR) | |
| Interventions | INDEX TREATMENT
Thoracic spine manipulation (TSM): technique: bilateral translatoric facet joint traction manipulation to the upper thoracic intervertebral segment performed; frequency: 1 session; dose: grade 5 manipulation; route: thoracic spine COMPARISON TREATMENT No treatment (NT): no treatment provided CO‐INTERVENTION: NR Duration of treatment: 1 session Duration of follow‐up: no follow‐up |
|
| Outcomes | PAIN (intensity with left rotation, 9 point faces pain scale)
Baseline mean: TSM 3.73, NT 2.50
Absolute benefit: TSM 0.688, NT 0.667
Reported results: not significant
SMD (TSM vs NT): 0.02 (95% CI ‐0.73 to 0.77) PAIN (intensity with right rotation, 9 point faces pain scale) Baseline mean: TSM 2.75, NT 2.80 Absolute benefit: TSM 1.5, NT ‐0.1 Reported results: not significant SMD (TSM vs NT): 0.65 (95% CI ‐0.12 to 1.41) FUNCTION: NR GPE: NR PATIENT SATISFACTION: NR QoL: NR SIDE EFFECTS: NR COST OF CARE: NR |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Page 95, left column, paragraph 4 |
| Allocation concealment (selection bias) | High risk | Unsure whether envelopes were opaque, questions about allocation numbers |
| Blinding of Participants (performance bias) | High risk | Not possible owing to intervention |
| Blinding of Personal (performance bias) | High risk | Not possible owing to intervention |
| Blinding of the Outcome assessor (detection bias) | High risk | Not possible owing to intervention |
| Incomplete outcome data (attrition bias) | Low risk | Pre‐post design |
| Randomized Participants analysed were allocated (attrition bias) | Low risk | Pre‐post design |
| Selective outcome (reporting bias) | Unclear risk | No protocol reported |
| Similar groups at baseline? | High risk | Not enough baseline data available |
| co‐interventions avoided or similar? | Low risk | Pre‐post design |
| Compliance acceptable? | Low risk | Pre‐post design |
| Similar timing of outcome assessment? | Low risk | Pre‐post design |
Leaver 2010.
| Methods | Type of trial: RCT Number analysed/randomly assigned: 177/182 Intention‐to‐treat analysis: calculated | |
| Participants | Acute/subacute non‐specific cervical disorder | |
| Interventions | INDEX TREATMENT
Manipulation (A): technique: high‐velocity low‐amplitude thrust, particular technique according to clinical judgement; timing: at baseline; frequency: 4 treatments over 2 weeks; route: cervical spine COMPARISON TREATMENT Mobilisation (B): technique: low‐velocity oscillating passive movement, particular technique according to clinical judgement; timing: at baseline; frequency: 4 treatments over 2 weeks; route: cervical spine CO‐INTERVENTION Not avoided: possibility of other treatment during follow‐up, option to continue existing exercise programme during treatment, use of other manipulations or mobilisation at different body locations during treatment not constrained Duration of treatment: 2 weeks, 4 sessions Duration of follow‐up: 10 weeks |
|
| Outcomes | PAIN (NRS, 0 to 10)
Baseline mean: A 6.1, B 5.9
End of study mean: A 1.6, B 1.4
Absolute benefit: A 4.5, B 4.5
Reported results: not significant SMD (A vs B): IP ‐0.05 (95% CI ‐0.34 to 0.25), IT 0.11 (‐0.19 to 0.40) FUNCTION (NDI, 0 to 50) Baseline mean: A 16.1, B 14.8 End of study mean: A 5.3, B 5.5 Absolute benefit: A 10.8, B 9.3 Reported results: not significant SMD (A vs B): ST ‐0.06 (95% CI ‐0.35 to 0.24), IT ‐0.03 (95% CI ‐0.33 to 0.26) GPE (5‐point scale, ‐5 to 5) End of study mean: A 3.3, B 3.4 Reported results: not significant SMD (A vs B): IP ‐0.18 (95% CI ‐0.47 to 0.12), IT ‐0.06 (95% CI ‐0.35 to 0.24) PATIENT SATISFACTION: NR QoL (PCS component of the SF‐12, 0 to 100) Baseline mean: A 42.9, B 43.6 End of study mean: A 50.2, B 50.6 Absolute benefit: A 7.3, B 7.0 Reported results: not significant SMD (A vs B): ST 0.08 (95% CI ‐0.21 to 0.38), IT ‐0.06 (95% CI ‐0.35 to 0.24) SIDE EFFECTS Additional neck pain: A 28/91, B 24/91 Headache: A 22/91, B 17/91 Dizziness/vertigo: A 7/91, B 6/91 Nausea: A 4/91, B 7/91 Paraesthesia: A 8/91, B 5/91 Other (upper limb pain, neck stiffness, fatigue, mid‐lower back pain, unpleasant change in spinal posture): A 7/91, B 3/91 COST OF CARE: NR |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Page 1314, right column, paragraph 2 and page 1315, right column |
| Allocation concealment (selection bias) | Low risk | Page 1314, right column, paragraph 2 and page 1315, right column |
| Blinding of Participants (performance bias) | High risk | Not possible |
| Blinding of Personal (performance bias) | High risk | Not possible |
| Blinding of the Outcome assessor (detection bias) | High risk | Participant is the assessor |
| Incomplete outcome data (attrition bias) | Low risk | Figure 1 |
| Randomized Participants analysed were allocated (attrition bias) | High risk | 5 participants not analysed in secondary analysis |
| Selective outcome (reporting bias) | Unclear risk | No protocol |
| Similar groups at baseline? | Low risk | Table 1 |
| co‐interventions avoided or similar? | Unclear risk | Co‐interventions not reported |
| Compliance acceptable? | Low risk | Page 1315, left column |
| Similar timing of outcome assessment? | Low risk | Baseline, 2, 4, 12 weeks |
Lee 2013.
| Methods | Type of trial: RCT Number analysed/randomly assigned: 33/33 Intention‐to‐treat analysis: NR | |
| Participants | Non‐specific cervical disorder (myofascial pain syndrome of the upper trapezius), duration NR | |
| Interventions | INDEX TREATMENT
PNF (A): technique: upper trapezius muscle relaxation therapy (PNF hold‐relax technique) with the participant in a sitting position; timing: at baseline; frequency: 2 treatments/wk for 4 weeks; dose: 5 repetitions of the technique at each session; route: upper trapezius COMPARISON TREATMENT EWST (B): technique: extracorporeal shock wave therapy applied to trigger points with 17‐mm gun and low power; timing: at baseline; frequency: 2 sessions/wk for 4 weeks; dose: 1000 impulsions, 5 Hz; route: upper trapezius TPI (C): technique: trigger point injection of 0.2 mL of 0.3% lidocaine (Travell method); timing: at baseline; frequency: 2 sessions/wk for 4 weeks; dose: 1 injection/trigger point; route: upper trapezius CO‐INTERVENTION Comparable between index and control groups: Each participant received hot pack therapy for 20 minutes and US for 5 minutes Duration of treatment: 4 weeks, 8 sessions Duration of follow‐up: 0 days |
|
| Outcomes | PAIN (NRS, 0 to 10)
Baseline mean: A 7.09, B 7.18, C 7.36
End of study mean: A 2.26, B 3.28, C 3.22
Absolute benefit: A 4.83, B 3.9, C 4.14
Reported results: significant favouring A over B and C SMD (A vs B): IP ‐1.01 (95% CI ‐1.91 to ‐0.11) SMD (A vs C): IP ‐1.05 (95% CI ‐1.96 to ‐0.15) FUNCTION (NDI, 0 to 50) Baseline mean: A 24.45, B 28.00, C 26.73 End of study mean: A 6.26, B 5.26, C 5.19 Absolute benefit: A 18.19, B 22.74, C 21.54 Reported results: not significant SMD (A vs B): IP 0.69 (95% CI ‐0.18 to 1.55) SMD (A vs C): IP 0.76 (95% CI ‐0.11 to 1.63) GPE: NR PATIENT SATISFACTION: NR QoL: NR SIDE EFFECTS: NR COST OF CARE: NR |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of Participants (performance bias) | High risk | Not possible owing to differences in interventions |
| Blinding of Personal (performance bias) | High risk | Not possible owing to differences in interventions |
| Blinding of the Outcome assessor (detection bias) | High risk | Not possible owing to differences in interventions |
| Incomplete outcome data (attrition bias) | Low risk | No dropouts |
| Randomized Participants analysed were allocated (attrition bias) | Low risk | No dropouts |
| Selective outcome (reporting bias) | Unclear risk | No protocol or registration |
| Similar groups at baseline? | Low risk | Tables 1 and 2 |
| co‐interventions avoided or similar? | Unclear risk | P343L medication may have increased effects of specific techniques |
| Compliance acceptable? | Unclear risk | Not described |
| Similar timing of outcome assessment? | Unclear risk | Baseline, 4 weeks for intervention but no description of when follow‐up was performed |
Lin 2013.
| Methods | Type of trial: RCT Number analysed/randomly assigned: 63/63 Intention‐to‐treat analysis: NA | |
| Participants | Chronic mechanical neck pain | |
| Interventions | INDEX TREATMENT
Long's manipulation plus traditional Chinese massage (control) (A): technique: high‐velocity low‐amplitude thrust; frequency: 8 sessions, 1 session every 3 days for 24 days; route: cervical spine COMPARISON TREATMENT Traditional Chinese massage (B): technique: massage technique such as stroking, rubbing, shaking, pinching, plucking, clapping and acupressure; frequency: 8‐ to 20‐minute sessions, 1 session every 3 days for 24 days; route: cervical spine CO‐INTERVENTION Duration of treatment: 24 days, 8 sessions Duration of follow‐up: 3 months |
|
| Outcomes | PAIN (NPRS, 0 to 10 mm)
Baseline mean: A 5.79, B 5.63 End of study mean: A 2.06, B 4.54 Absolute benefit: A 3.72, B 1.09 Reported results: statistically significant decrease SMD (A vs B): ‐1.30 (‐2.02 to ‐0.57) FUNCTION (NPQ, 42 items) Baseline mean: A 35.44, B 36.14 End of study mean: A 15.07, B 25.88 Absolute benefit: A 20.37, B 10.26 Reported results: significant decrease SMD (A vs B): ‐1.16 (‐1.88 to ‐0.45) GPE: NR PATIENT SATISFACTION: NR QoL: NR SIDE EFFECTS: NR COST OF CARE: NR |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Page 310, column 2, paragraph 1 |
| Allocation concealment (selection bias) | Low risk | Page 310, column 2, paragraph 1 |
| Blinding of Participants (performance bias) | High risk | Not possible owing to design |
| Blinding of Personal (performance bias) | High risk | Not possible owing to design |
| Blinding of the Outcome assessor (detection bias) | High risk | Not possible owing to design |
| Incomplete outcome data (attrition bias) | High risk | Figure 2 |
| Randomized Participants analysed were allocated (attrition bias) | Low risk | Figure 2 |
| Selective outcome (reporting bias) | Unclear risk | No protocol |
| Similar groups at baseline? | Low risk | Table 1 |
| co‐interventions avoided or similar? | Unclear risk | Not described |
| Compliance acceptable? | Unclear risk | Not described |
| Similar timing of outcome assessment? | Low risk | Baseline, 3‐month follow‐up |
Madson 2010.
| Methods | Type of trial: RCT Number analysed/randomly assigned: 23/23 Intention‐to‐treat analysis: not calculated | |
| Participants | Chronic non‐specific cervical disorder | |
| Interventions | INDEX TREATMENT
Joint mobilisation (A): technique: non‐thrust, oscillatory techniques (transverse glide, posterior‐anterior glides and rotational); timing: at baseline; frequency: 2 or 3 treatments/wk for 4 weeks; dose: low grade (I to IV); duration: 30 minutes (after application of the moist heat pack); route: 1 or more restricted cervical spine segments COMPARISON TREATMENT Massage (B): technique: effleurage, stroking and pétrissage; timing: at baseline; frequency: 2 or 3 treatments/wk for 4 weeks; duration: 30 minutes; route: neck and upper back muscles CO‐INTERVENTION Not avoided: Participants were allowed to continue taking prescribed pain medication; avoided in trial design: other therapeutic interventions and modalities; comparable between groups: application of moist heat packs to the neck and upper back for 20 to 30 minutes before treatment Duration of treatment: 4 weeks, maximum 12 sessions Duration of follow‐up: 0 days |
|
| Outcomes | PAIN (VAS, 0 to 100 mm)
Baseline mean: A 40.91, B 29.42
End of study mean: A 16.45, B 20.91
Absolute benefit: A 24.46, B 8.51
Reported results: not significant SMD (A vs B): ‐0.25 (95% CI ‐1.09 to 0.59) FUNCTION (NDI, 0 to 50) Baseline mean: A 13.54, B 12.75 End of study mean: A 5.64, B 8.08 Absolute benefit: A 7.90, B 4.67 Reported results: not significant SMD (A vs B): ‐0.52 (95% CI ‐1.35 to 0.32) GPE: NR PATIENT SATISFACTION: NR QoL: NR SIDE EFFECTS: NR COST OF CARE: NR |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Page 645, right column |
| Allocation concealment (selection bias) | Low risk | Page 645, right column |
| Blinding of Participants (performance bias) | High risk | Not possible |
| Blinding of Personal (performance bias) | High risk | Not possible |
| Blinding of the Outcome assessor (detection bias) | High risk | Not possible |
| Incomplete outcome data (attrition bias) | Low risk | Figure 1 – no dropouts |
| Randomized Participants analysed were allocated (attrition bias) | Low risk | No dropouts |
| Selective outcome (reporting bias) | Unclear risk | No protocol |
| Similar groups at baseline? | High risk | Table 1, Table 2 |
| co‐interventions avoided or similar? | Unclear risk | Not described |
| Compliance acceptable? | Unclear risk | Exercise compliance not reported. |
| Similar timing of outcome assessment? | Low risk | Page 648, left column, paragraph 1 |
Martel 2011.
| Methods | Type of trial: RCT Number analysed/randomly assigned: 65/59 Intention‐to‐treat analysis: calculated | |
| Participants | Chronic (> 3 months) mechanical neck pain | |
| Interventions | INDEX TREATMENT
Spinal manipulation therapy group (SMT): technique: supine technique with 4 high‐velocity low‐amplitude manipulations in upper thoracic and cervical areas: frequency: 1 session/mo for 10 months, 10 sessions total; dose: 1 to 2 manipulations/segment (maximum 4) COMPARISON TREATMENT 10‐Month attention‐control group (AC); frequency: participants attended the clinic once every 2 months for 20 to 30 minutes for 10 months, 5 sessions in total CO‐INTERVENTION: NR Duration of therapy period: 10 months Duration of follow‐up: baseline, initiation of RCT, mid‐trial, end of trial at 10 months |
|
| Outcomes | PAIN (VAS, 0 to 10 cm)
Baseline mean: AC 3.8, SMT 3.3
End of study mean: AC 2.9, SMT 2.1
Absolute benefit: AC 0.9, SMT 1.2
Reported results: no significant difference
SMD: ‐0.30 (95% CI ‐0.82 to 0.21) FUNCTION (NDI, 0 to 50) Baseline mean: AC 26.1, SMT 21.5 End of study mean: AC 21.5, SMT 13.7 Absolute benefit: AC 4.6, SMT 7.8 Reported results: significant favouring experimental differences SMD: ‐0.59 (95% CI ‐1.12 to ‐0.07); NNTB 10 PATIENT SATISFACTION: NR GPE: NR QoL: NR SIDE EFFECTS: none COST OF CARE: NR |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Page 2, left column |
| Allocation concealment (selection bias) | Low risk | Page 3, left column |
| Blinding of Participants (performance bias) | High risk | Not possible owing to intervention |
| Blinding of Personal (performance bias) | High risk | Not possible owing to intervention |
| Blinding of the Outcome assessor (detection bias) | High risk | Not possible owing to intervention |
| Incomplete outcome data (attrition bias) | Low risk | Figure 1 |
| Randomized Participants analysed were allocated (attrition bias) | High risk | Not all randomly assigned participants were included; Figure 1 |
| Selective outcome (reporting bias) | Unclear risk | No protocol |
| Similar groups at baseline? | Low risk | Table 1 |
| co‐interventions avoided or similar? | High risk | Page 7, right column |
| Compliance acceptable? | High risk | Page 7, left column |
| Similar timing of outcome assessment? | Low risk | Baseline, 12 months; mid‐trial data unclear; however, we believe long‐term follow‐up data are more important |
Martinez‐Segura 2006a.
| Methods | Type of trial: RCT Number analysed/randomly assigned: 71/71 Intention‐to‐treat analysis: NR | |
| Participants | Subacute chronic neck pain, no radiculopathy | |
| Interventions | INDEX TREATMENT
Cervical high‐velocity low‐amplitude technique group (manip): technique: manipulation ipsilateral side flexion, contralateral rotation; frequency: 1 session; route: cervical spine COMPARISON TREATMENT Sham/Control group (cntl): technique: neck positioned into ipsilateral side flexion, contralateral rotation, position held for 30 seconds, the side of manual contact was randomly assigned; frequency: 1 session CO‐INTERVENTION: NR Duration of treatment: 1 session Duration of follow‐up: none |
|
| Outcomes | PAIN INTENSITY (VAS, 0 to 10 cm)
Baseline mean: manip 5.7, cntl 5.5
End of study mean: manip 2.2, cntl 5.1
Absolute benefit: manip 3.5, cntl 0.4
Reported results: significant favouring manipulation
SMD: ‐1.67 (95% CI ‐2.21 to ‐1.12); NNTB: 2; treatment advantage 54% FUNCTION: NR PATIENT SATISFACTION: NR GPE: NR QoL: NR SIDE EFFECTS: NR COST OF CARE: NR |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Not reported |
| Allocation concealment (selection bias) | High risk | Not reported |
| Blinding of Participants (performance bias) | High risk | Not reported |
| Blinding of Personal (performance bias) | High risk | Not possible owing to design |
| Blinding of the Outcome assessor (detection bias) | High risk | Not possible owing to design |
| Incomplete outcome data (attrition bias) | Low risk | Pre‐post design |
| Randomized Participants analysed were allocated (attrition bias) | Low risk | Pre‐post design |
| Selective outcome (reporting bias) | Unclear risk | No reported protocol |
| Similar groups at baseline? | Low risk | Page 513, Table 1 |
| co‐interventions avoided or similar? | Low risk | Pre‐post design |
| Compliance acceptable? | Low risk | Pre‐post design |
| Similar timing of outcome assessment? | Low risk | Pre‐post design |
Masaracchio 2013.
| Methods | Type of trial: RCT
Number analysed/randomly assigned: 64/66
Intention‐to‐treat analysis: calculated Location of study: USA |
|
| Participants | Mechanical neck pain < 3 months (acute and subacute) | |
| Interventions | INDEX TREATMEAT Experimental group (EG): thoracic spine manipulations plus cervical non‐thrust manipulations plus cervical spine active range of motion exercises (thoracic spine manip plus control vs control): technique: 2 upper thoracic spine thrust manipulations and 2 middle thoracic spine thrust manipulations plus cervical spine posterior‐anterior non‐thrust manipulations; frequency: 10 reps for non‐thrust manip; dose: 1 to 2 attempts for thrust manip; duration: 2 treatment sessions; routes: T1‐3 and T4‐7 and C2‐7; duration of follow‐up: 1 week, 2 to 3 days following last treatment session COMPARISON TREATMENT Comparison group (CG): cervical posterior‐anterior non‐thrust manipulation to the segment spinous processes plus cervical active range of motion exercises; frequency: 10 reps followed by 10‐second rest between segments; dose: grade 3; duration: 2 treatment sessions; route: spinous process of C2‐C7; duration of follow‐up: 1 week, 2 to 3 days following last treatment session CO‐INTERVENTION: NR Duration of therapy period: 1 week Duration of follow‐up: baseline, 1 week |
|
| Outcomes | PAIN INTENSITY (NPRS, 0 to 10)
Baseline mean: EG 5.1, CG 4.9
End of study mean: EG 2.2, CG 3.5
Absolute benefit: EG 2.9, CG 1.4
Reported results: significant favouring EG
SMD: ‐1.00 (95% CI ‐1.52 to ‐0.48); NNTB 4 FUNCTION (NDI, 0 to 50) Baseline mean: EG 28.5, CG 26.3 End of study mean: EG 12.3, CG 18.9 Absolute benefit: EG 16.2, CG 7.4 Reported results: significant favouring EG SMD: ‐0.89 (95% CI ‐1.40 to ‐0.37); NNTB 4 PATIENT SATISFACTION: NR QoL: NR GPE: NR SIDE EFFECTS: NR COST OF CARE: NR |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Page 120, column 3, paragraph 2 |
| Allocation concealment (selection bias) | Unclear risk | Did not follow adequate level of allocation concealment |
| Blinding of Participants (performance bias) | High risk | Not possible owing to design |
| Blinding of Personal (performance bias) | High risk | Not possible owing to design |
| Blinding of the Outcome assessor (detection bias) | High risk | Not possible owing to design |
| Incomplete outcome data (attrition bias) | Low risk | Figure 5, page 122 |
| Randomized Participants analysed were allocated (attrition bias) | Low risk | Page 122, column 2, paragraph 1 |
| Selective outcome (reporting bias) | Unclear risk | No protocol |
| Similar groups at baseline? | Low risk | Page 123, Table 2 |
| co‐interventions avoided or similar? | Unclear risk | Not reported |
| Compliance acceptable? | Unclear risk | Not reported |
| Similar timing of outcome assessment? | Low risk | Baseline, 1 week |
Muller 2005.
| Methods | Type of trial: RCT Number analysed/randomly assigned: 69/115 Intention‐to‐treat analysis: calculated | |
| Participants | Chronic neck pain | |
| Interventions | INDEX TREATMENT
Spinal manipulation (A): technique: high‐velocity low‐amplitude thrust on the level of involvement; frequency: 2 sessions/wk; dose: grade 5 manipulation; duration: 20 minute visits; route: affected segments of cervical spine COMPARISON TREATMENT Medication (B): type: Celebrex‐celacoxin (27 participants), Vioxx‐rofecoxib (11 participants), paracetamol (5 participants); frequency: fortnightly 20‐minute office visits until asymptomatic or sufficient pain relief achieved; dose Celebrex‐celacoxin 200 to 400 mg/d, Vioxx‐rofecoxib 12.5 to 25 mg/d, paracetamol 1000 to 3000 mg/d; route: oral Acupuncture (C): technique: 8 to 10 needles placed in local paraspinal and intramuscular pain areas, 5 needles placed in distal point meridians; frequency: 2 sessions/wk until asymptomatic or acceptable pain relief achieved; dose: 20 minutes with turning or flicking needles every 5 minutes if tolerated; route: sterile HWATO Chinese acupuncture guide tube needles (50 mm length, 0.25 mm gauge) CO‐INTERVENTION: not avoided Duration of treatment: 9 weeks or until asymptomatic, maximum 18 sessions Duration of follow‐up: 12 months |
|
| Outcomes | PAIN (intensity, VAS, 0 to 10)
Baseline median: A 6, B 4, C 7
12‐Month median: A 2.8, B 4.7, C 2.5 Absolute benefit: A 3.2, B ‐0.7, C 4.5 Reported results: significance between groups NR, significance for A and C within‐group data SMD (A vs B): ‐0.24 (95% CI ‐0.85 to 0.37) SMD (A vs C): 0.04 (95% CI ‐0.56 to 0.64) FUNCTION (NDI, 0 to 50) Baseline median: A 28, B 42, C 36 12‐Month median: A 20, B 36, C 24 Absolute benefit: A 8, B 6, C 12 Reported results: significance between groups NR, significance within A and C groups SMD (A vs B): ‐0.36 (95% CI ‐0.97 to 0.25) SMD (A vs C): ‐0.09 (95% CI ‐0.69 to 0.51) GPE: NR PATIENT SATISFACTION: NR QoL: NR for neck group alone SIDE EFFECTS: NR COST OF CARE: NR |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Randomisation technique not adequate |
| Allocation concealment (selection bias) | Unclear risk | Envelopes not sequentially numbered |
| Blinding of Participants (performance bias) | High risk | Not possible owing to study design |
| Blinding of Personal (performance bias) | High risk | Not possible owing to study design |
| Blinding of the Outcome assessor (detection bias) | High risk | Not possible owing to study design |
| Incomplete outcome data (attrition bias) | High risk | Dropout rate > 50%, only compliers used |
| Randomized Participants analysed were allocated (attrition bias) | High risk | Page 6 ‐ improper Intention‐to‐treat technique; only responders included |
| Selective outcome (reporting bias) | Unclear risk | No reported protocol |
| Similar groups at baseline? | Unclear risk | NDI and Oswestry data not given; data for only 62 participants given |
| co‐interventions avoided or similar? | High risk | Page 8, left column, paragraph 2 |
| Compliance acceptable? | High risk | Page 8, left column, paragraph 2 |
| Similar timing of outcome assessment? | Low risk | Baseline, 12‐month follow‐up |
Nilsson 1997.
| Methods | Type of trial: RCT Number analysed/randomly assigned: 53/54 Intention‐to‐treat analysis: NR | |
| Participants | Chronic neck pain with headache | |
| Interventions | INDEX TREATMENT
Manipulation (A): technique: manipulation‐toggle recoil for upper cervical spine, diversified technique for mid‐ and lower cervical spine; high‐velocity low‐amplitude thrust at end point of passive range of motion; frequency: 2 sessions/wk; dose: 12 toggle recoil, 10 diversified manipulation; route: cervical spine COMPARISON TREATMENT Soft tissue massage (B): technique: massage, deep frictions and trigger point treatment of posterior muscles of shoulder girdle, upper thoracic and lower cervical, and placebo laser applied to upper cervical region; frequency: 2 sessions/wk; route: cervical and thoracic spines CO‐INTERVENTION: NR Duration of treatment: 3 weeks, 6 sessions Duration of follow‐up: 1 week |
|
| Outcomes | PAIN (headache intensity per episode; VAS, 0 to 100)
Baseline median: A 48, B 37
End of study median: A 15, B 6
Absolute benefit: A 33, B 31
Reported results: not significant
SMD: ‐0.45 (95% CI ‐0.99 to 0.10) (power 16%) FUNCTION: NR PATIENT SATISFACTION: NR GPE: NR QoL: NR SIDE EFFECTS: NR COST OF CARE: NR |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Page 327, right column, paragraph 1 |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of Participants (performance bias) | High risk | Not possible owing to design |
| Blinding of Personal (performance bias) | High risk | Not possible owing to design |
| Blinding of the Outcome assessor (detection bias) | High risk | Not possible owing to design |
| Incomplete outcome data (attrition bias) | Low risk | Page 328, left column, paragraph 1 |
| Randomized Participants analysed were allocated (attrition bias) | High risk | One participant lost for analysis |
| Selective outcome (reporting bias) | Unclear risk | No reported protocol |
| Similar groups at baseline? | Low risk | Tables 2 and 3 |
| co‐interventions avoided or similar? | High risk | Unsure whether co‐interventions were similar between groups |
| Compliance acceptable? | Unclear risk | Diary described, but no data on compliance with treatment |
| Similar timing of outcome assessment? | Low risk | Figure 1 |
Parkin‐Smith 1998.
| Methods | Type of trial: RCT Number analysed/randomly assigned: 30/30 Intention‐to‐treat analysis: not calculated | |
| Participants | Neck pain, duration not reported (NR) | |
| Interventions | INDEX TREATMENT
Group A: technique: manipulation; route: cervical spine COMPARISON TREATMENT Group B: technique: manipulation; route: cervical and thoracic spines CO‐INTERVENTION: not specified Duration of treatment: 3 weeks, 6 sessions Duration of follow‐up: none |
|
| Outcomes | PAIN INTENSITY (NRS‐101, 0 to 100)
Baseline mean: A 33.89, B 33.00
End of study mean: A 17.17, B 13.18
Absolute benefit: A 16.72, B 19.82
Reported results: not significant
SMD: 0.29 (95% CI ‐0.43 to 1.01) (power 94%) FUNCTION (NDI, 0 to 50) Baseline mean: A 18.24, B 17.64 End of study mean: A 6.89, B 4.71 Absolute benefit: A 11.35, B 12.93 Reported results: not significant SMD: 0.30 (95% CI ‐0.42 to 1.02) (power 100%) PATIENT SATISFACTION: NR GPE: NR QoL: NR SIDE EFFECTS: NR COST OF CARE: NR |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Not reported |
| Allocation concealment (selection bias) | High risk | Not reported |
| Blinding of Participants (performance bias) | High risk | Not possible owing to design |
| Blinding of Personal (performance bias) | High risk | Not possible owing to design |
| Blinding of the Outcome assessor (detection bias) | High risk | Not possible owing to design |
| Incomplete outcome data (attrition bias) | High risk | Not reported |
| Randomized Participants analysed were allocated (attrition bias) | High risk | Not reported |
| Selective outcome (reporting bias) | Unclear risk | No reported protocol |
| Similar groups at baseline? | Low risk | Page 329, Table 21 |
| co‐interventions avoided or similar? | High risk | Not reported |
| Compliance acceptable? | High risk | Not Reported |
| Similar timing of outcome assessment? | Low risk | Baseline, 4 weeks |
Puentedura 2011.
| Methods | Type of trial: RCT Number analysed/randomly assigned: 20/24 Intention‐to‐treat analysis: calculated | |
| Participants | Acute mechanical neck pain (with or without unilateral upper extremity symptoms) | |
| Interventions | INDEX TREATMENT Cervical thrust manipulation (A): technique: during first 2 sessions: mid‐range high‐velocity low‐amplitude thrust into rotation to both sides of cervical segment directed up towards the participant's contralateral eye (participant in supine position with cervical spine rotation and side bending); timing: at baseline; frequency: 3× for first week and 2× during second week, 5 treatment sessions; dose: maximum of 2 thrusts for each manipulation technique; route: cervical spine COMPARISON TREATMENT Thoracic thrust manipulation (B): technique: application of 3 different thoracic spine manipulation techniques during first 2 sessions; mid‐range high‐velocity upward distraction thrust to lower thoracic spine (participant in a sitting position) and end‐range high‐velocity low‐amplitude anterior‐posterior thrust to mid‐thoracic and lower thoracic spines with cervicothoracic flexion (participant in supine position); timing: at baseline; frequency: 3× for the first week and 2× during the second week, 5 treatment sessions; dose: maximum 2 thrusts for each manipulation technique; route : thoracic spine CO‐INTERVENTION: comparable between groups: during last 3 therapy sessions, participants from both groups performed a standardised exercise programme to improve ROM and strength (3 times 10 reps, 3 to 4×/d) and did not receive further manipulation Duration of treatment: 2 weeks, 5 sessions Duration of follow‐up: 22 weeks |
|
| Outcomes | PAIN (NRS, 0 to 10)
Baseline mean: A 4.6, B 3.6
End of study mean: A 0.1, B 2.3
Absolute benefit: A 4.5, B 1.3
Reported results: significant favouring A at short and intermediate terms SMD (A vs B): ST ‐2.43 (95% CI ‐3.64 to ‐1.21); NNTB 12 IT ‐2.70 (95% CI ‐3.98 to ‐1.42); NNTB 6 FUNCTION (NDI, 0 to 50) Baseline mean: A 13.4, B 12.6 End of study mean: A 3.7, B 9.9 Absolute benefit: A 9.7, B 2.7 Reported results: significant favouring A at short and intermediate terms SMD (A vs B): ST ‐1.01 (95% CI ‐1.96 to ‐0.07); NNTB 5 IT ‐1.22 (95% CI ‐2.19 to ‐0.24); NNTB 4 GPE: NR PATIENT SATISFACTION: NR QoL: NR SIDE EFFECTS: reported A 1/14 reported minor increased neck pain after first treatment B 8/10 in thoracic group after first treatment and 7/10 after second treatment reported minor increased neck pain, fatigue, headache or upper back pain that resolved within 24 hours of onset COST OF CARE: NR |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Page 210, right column, paragraph 1 |
| Allocation concealment (selection bias) | Unclear risk | Envelopes not numbered |
| Blinding of Participants (performance bias) | High risk | Interventions perceptibly different |
| Blinding of Personal (performance bias) | High risk | Interventions perceptibly different |
| Blinding of the Outcome assessor (detection bias) | High risk | Interventions perceptibly different |
| Incomplete outcome data (attrition bias) | High risk | High dropout rate in cervical manipulation group; all dropouts were in this group |
| Randomized Participants analysed were allocated (attrition bias) | Low risk | Page 212, middle column, paragraph 2 and Figure 5 |
| Selective outcome (reporting bias) | Unclear risk | No protocol |
| Similar groups at baseline? | Unclear risk | Duration different between groups, see page 217 for study author comments on this |
| co‐interventions avoided or similar? | Unclear risk | Not reported |
| Compliance acceptable? | Unclear risk | Not reported |
| Similar timing of outcome assessment? | Low risk | Baseline, 1 week, 4 weeks, 6 months |
Ragonese 2009.
| Methods | Type of trial: RCT Number analysed/randomly assigned: 20/20 Intention‐to‐treat analysis: not calculated | |
| Participants | Neck disorder with radiculopathy (radicular symptoms or signs), duration NR | |
| Interventions | INDEX TREATMENT Manual therapy (A): technique: cervical lateral glide in supine position of all cervical segments (C2 to C7), PAs in prone position of hypomobile segment of the thoracic spine and sliding neural dynamic technique of the median nerve (as described by Butler); timing: at baseline; frequency: 3 times/wk for 3 weeks; dose: grade III to IV oscillatory movements as described by Maitland for cervical glide and thoracic mobilisation and unknown for the neural dynamic technique; route: cervical spine, thoracic spine and upper extremity of the affected side COMPARISON TREATMENT Exercises (B): technique: deep neck flexor strengthening in supine position, lower and middle trapezius strengthening in prone position and serratus anterior strengthening in standing position. No home programme was prescribed; timing: at baseline; frequency: 3 times/wk for 3 weeks; dose: 10 × 10 seconds for neck flexor, 2 × 15 reps (with or without dumbbells) for trapezius and serratus anterior; route: cervical spine, thoracic spine and upper extremity of affected side CO‐INTERVENTION: NR Duration of treatment: 3 weeks, 9 sessions Duration of follow‐up: 0 days |
|
| Outcomes | PAIN (NRS, 0 to 0)
Baseline mean: A 5.3, B 4.9
End of study mean: A 2.4, B 1.6
Absolute benefit: A 2.9, B 3.3
Reported results: not significant SMD (A vs B): 0.58 (95% CI ‐0.32 to 1.48) FUNCTION (NDI, 0 to 50) Baseline mean: A 39.6, B 28.7 End of study mean: A 17.2, B 10.2 Absolute benefit: A 22.4, B 18.5 Reported results: not significant SMD (A vs B): 0.76 (95% CI ‐0.16 to 1.67) GPE: NR PATIENT SATISFACTION: NR QoL: NR SIDE EFFECTS: NR COST OF CARE: NR |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Unclear for sequence |
| Allocation concealment (selection bias) | Unclear risk | Unclear for sequence |
| Blinding of Participants (performance bias) | High risk | Not possible owing to design |
| Blinding of Personal (performance bias) | High risk | Not possible owing to design |
| Blinding of the Outcome assessor (detection bias) | High risk | Not possible owing to design |
| Incomplete outcome data (attrition bias) | Unclear risk | Not reported |
| Randomized Participants analysed were allocated (attrition bias) | Low risk | Table 4 |
| Selective outcome (reporting bias) | Unclear risk | Not reported |
| Similar groups at baseline? | High risk | Tables 2 and 3, initial NDI difference |
| co‐interventions avoided or similar? | Unclear risk | Not reported |
| Compliance acceptable? | Unclear risk | Not reported |
| Similar timing of outcome assessment? | Unclear risk | Not clear when outcomes were performed each week |
Saavedra‐Hernandez 2012CR.
| Methods | Type of trial: RCT Number analysed/randomly assigned: 81/82 Intention‐to‐treat analysis: calculated | |
| Participants | Chronic mechanical neck pain | |
| Interventions | INDEX TREATMENT Full manipulation group (A): technique: high‐velocity low‐amplitude thrust, (1) cervical spine: manipulation directed upward and medially in the direction of the participant's contralateral eye, participant in supine position with the cervical spine in a neutral position, (2) cervicothoracic junction: thrust applied toward the participant's right or left side, thrust applied bilaterally, participant prone with head and neck rotated, (3) upper thoracic spine: distraction thrust manipulation directed in an upward direction, participant in supine position with arms crossed; timing: at baseline; frequency: 1 session; dose: 1 to 2 thrusts per area; route: cervical spine, cervicothoracic junction, upper thoracic spine, symptomatic level COMPARISON TREATMENT Cervical manipulation group (B): technique: high‐velocity low‐amplitude thrust manipulation directed upward and medially in the direction of the participant's contralateral eye, participant in supine position with the cervical spine in a neutral position; timing: at baseline; frequency: 1 treatment session; dose: 1 to 2 thrusts; route: cervical spine, symptomatic level CO‐INTERVENTION: N/A Duration of treatment: 1 day, 1 session Duration of follow‐up: 1 week post treatment |
|
| Outcomes | PAIN (NPRS, 0 to 10)
Baseline mean: A 4.9, B 4.8
End of study mean: A 2.7, B 2.7
Absolute benefit: A 2.2, B 2.1
Reported results: equally effective, no significant differences between groups SMD: 0.08 (95% CI ‐0.36 to 0.51) FUNCTION (NDI, 0 to 50) Baseline mean: A 22.2, B 23.7 End of study mean: A 11.6, B 16.8 Absolute benefit: A 10.6, B 6.9 Reported results: statistically significant favouring A SMD: ‐0.17 (95% CI ‐0.61 to 0.27) GPE: NR PATIENT SATISFACTION: NR QoL: NR SIDE EFFECTS: reported Minor increase in neck pain or fatigue after manipulation(s): A 1/41, B 1/40 COST OF CARE: NR |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Page 3, column 2, paragraph 1 |
| Allocation concealment (selection bias) | Low risk | Page 3, column 2, paragraph 1 |
| Blinding of Participants (performance bias) | High risk | Not possible owing to design |
| Blinding of Personal (performance bias) | High risk | Not possible owing to design |
| Blinding of the Outcome assessor (detection bias) | High risk | Not possible owing to design |
| Incomplete outcome data (attrition bias) | Low risk | Figure 4, page 4 |
| Randomized Participants analysed were allocated (attrition bias) | Low risk | Figure 4, page 4 |
| Selective outcome (reporting bias) | Unclear risk | Not reported |
| Similar groups at baseline? | Low risk | Table 1, page 5 |
| co‐interventions avoided or similar? | Unclear risk | Not reported |
| Compliance acceptable? | Low risk | Short‐term follow‐up |
| Similar timing of outcome assessment? | Low risk | Baseline, 7‐day follow‐up |
Saavedra‐Hernández 2012JO.
| Methods | Type of trial: RCT Number analysed/randomly assigned: 76/80 Intention‐to‐treat analysis: calculated | |
| Participants | Chronic mechanical neck pain | |
| Interventions | INDEX TREATMENT
Cervical manipulation (A): technique: high‐velocity low‐amplitude thrust at mid‐cervical spine directed upward and medially in the direction of the participant's contralateral eye, participant in supine position with cervical spine in neutral position. For cervicothoracic junction, thrust was applied bilaterally toward the participant's left and right sides, participant prone with head and neck rotated; timing: at baseline; dose: 1 thrust per manipulation technique; route: thoracic spine and cervical spine COMPARISON TREATMENT Kinesio‐tape (B): technique: tape with width of 5 cm and thickness of 0.5 mm. Each tail of the first strip (blue Y‐strip, 2‐tailed) was applied with the participant's neck in a position of cervical contralateral side bending and rotation. Tape was first placed from T1‐T2 to C1‐C2. Overlying strip (black) was a space‐tape (opening) placed perpendicular to the Y‐strip, over C3‐C6, with the participant's cervical spine in flexion to apply tension to posterior structures; timing: at baseline; duration: tape worn for 7 days; route: thoracic spine and cervical spine CO‐INTERVENTION: N/A Duration of treatment: 1 day, 1 session Duration of follow‐up: 0 day |
|
| Outcomes | PAIN (NPRS, 0 to 10)
Baseline mean: A 5.0, B 5.2
End of study mean: A 2.7, B 2.7
Absolute benefit: A 2.3, B 2.5
Reported results: not significant SMD (A vs B): 0.00 (95% CI ‐0.45 to 0.45) FUNCTION (NDI, 0 to 50) Baseline mean: A 22.5, B 21.4 End of study mean: A 16.8, B 15.4 Absolute benefit: A 5.7, B 6.0 Reported results: significant favouring B SMD (A vs B): 0.46 (95% CI 0.01 to 0.92) GPE: NR PATIENT SATISFACTION: NR QoL: NR SIDE EFFECTS: reported Minor increase in neck pain or fatigue after manipulation: A 3/36, B 0/40 Cutaneous irritation related to tape application: A 0/36, B 2/40 COST OF CARE: NR |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Pages 725 to 726 |
| Allocation concealment (selection bias) | Low risk | Pages 725 to 726 |
| Blinding of Participants (performance bias) | High risk | Not possible owing to intervention |
| Blinding of Personal (performance bias) | High risk | Not possible owing to intervention |
| Blinding of the Outcome assessor (detection bias) | High risk | Not possible owing to intervention |
| Incomplete outcome data (attrition bias) | Low risk | Figure 4 |
| Randomized Participants analysed were allocated (attrition bias) | Unclear risk | Unclear whether ITT was properly performed – see manipulation group numbers in Table 1 |
| Selective outcome (reporting bias) | Unclear risk | No protocol |
| Similar groups at baseline? | Low risk | Table 1 |
| co‐interventions avoided or similar? | Unclear risk | Not reported |
| Compliance acceptable? | Unclear risk | Not reported whether participants in kinesiotape group kept it on for 7 days |
| Similar timing of outcome assessment? | Low risk | Baseline, 7 days |
Saayman 2011.
| Methods | Type of trial: RCT Number analysed/randomly assigned: 56/60 Intention‐to‐treat analysis: calculated | |
| Participants | Subacute/chronic mechanical neck pain (facet joint dysfunction/syndrome) | |
| Interventions | INDEX TREATMENT
Chiropractic manipulation (A): technique: specific short‐lever, high‐velocity low‐amplitude diversified techniques of cervical manipulation. Maximum of 3 most painful dysfunctional joints treated per session; timing: at baseline; frequency: 2 treatment sessions/wk; dose: 6 treatments over 3 weeks; duration: 30 minutes; route: cervical spine COMPARISON TREATMENT Low‐level laser therapy (B): technique: use of a Uni‐Laser 201 830‐nm gallium aluminium arsenide with handheld probe. Output ranged from 14 to 19 mW. Minimum of 3 joints per treatment session; timing: at baseline; frequency: 2 sessions/wk over 3 weeks; dose: 5.57 to 7.56 J/cm2; duration: 50 seconds; route: cervical spine Combination of CMT and LLLT (C): technique: combination of the 2 interventions mentioned before. Manipulative procedures completed first. Protocols were the same; timing: at baseline; frequency: 6 sessions over 3 weeks; duration: 30 minutes; see groups A and B for other dosage parameters CO‐INTERVENTION: avoided in trial design: participants requested not to take analgesic or NSAID or any other form of physical treatment to the neck, nor to partake in activities that would exacerbate the pain for the duration of the study Duration of treatment: 3 weeks, 6 sessions Duration of follow‐up: 1 week |
|
| Outcomes | PAIN (NRS, 0 to 10)
Baseline mean: A 6, B 6, C 6
End of study mean: A 4, B 4, C 2
Absolute benefit: A 2, B 2, C 4
Reported results: significant favouring combination of CMT + LLLT FUNCTION (NDI, 0 to 50, converted in 100%) Baseline mean: A 24, B 23.5, C 26 End of study mean: A 17, B 18, C 11.5 Absolute benefit: A 7, B 5.5, C 14.5 Reported results: significant favouring combination of CMT + LLLT GPE: NR PATIENT SATISFACTION: NR QoL: NR SIDE EFFECTS: reported: no adverse serious effects in any study groups COST OF CARE: NR |
|
| Notes | Wrote study author in 2015 to request additional data (SD) for week 4 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Page 154, right column, paragraph 4 |
| Allocation concealment (selection bias) | Low risk | Page 154, right column, paragraph 4 |
| Blinding of Participants (performance bias) | High risk | Not possible owing to differences between interventions |
| Blinding of Personal (performance bias) | High risk | Not possible owing to differences between interventions |
| Blinding of the Outcome assessor (detection bias) | High risk | Not possible owing to differences between interventions |
| Incomplete outcome data (attrition bias) | Low risk | Figure 3 |
| Randomized Participants analysed were allocated (attrition bias) | Low risk | Figure 3 |
| Selective outcome (reporting bias) | Unclear risk | No protocol |
| Similar groups at baseline? | Low risk | Table 1 |
| co‐interventions avoided or similar? | Unclear risk | Co‐interventions not reported |
| Compliance acceptable? | Unclear risk | Compliance not reported |
| Similar timing of outcome assessment? | Low risk | Baseline, 2 weeks, 3 weeks, 4 weeks (see abstract) |
Savolainen 2004.
| Methods | Type of trial: RCT Number analysed/randomly assigned: 41/75 Intention‐to‐treat analysis: NR | |
| Participants | Neck pain, duration NR | |
| Interventions | INDEX TREATMENT
Thoracic manipulation (A): technique: manipulation of the upper thoracic spine by a physiatrist; frequency: 1 session/wk; dose: 4 manipulations; route: thoracic spine COMPARISON TREATMENT Instructed exercise (B): duration unclear CO‐INTERVENTION: NR Duration of treatment: 4 weeks for manipulation group, unknown for control group Duration of follow‐up: 52 weeks |
|
| Outcomes | PAIN (neck pain intensity (pain right now); VAS, 0 to 10)
Baseline mean: A 3.7, B 3.8
Absolute benefit: A 0.8, B ‐0.5
Results: significant favouring thoracic manipulation for worst perceived pain, no other significant results between groups for pain right now and for average pain
SMD (A vs B): ‐0.50 (95% CI ‐1.13 to 0.13) (power 69%) FUNCTION: NR PATIENT SATISFACTION: NR GPE: NR QoL: NR SIDE EFFECTS: NR COST OF CARE: NR |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of Participants (performance bias) | High risk | Not possible owing to study design |
| Blinding of Personal (performance bias) | High risk | Not possible owing to study design |
| Blinding of the Outcome assessor (detection bias) | High risk | Not possible owing to study design |
| Incomplete outcome data (attrition bias) | High risk | Table 1 |
| Randomized Participants analysed were allocated (attrition bias) | High risk | Table 1 |
| Selective outcome (reporting bias) | Unclear risk | No reported protocol |
| Similar groups at baseline? | Low risk | Tables 1 and 2 |
| co‐interventions avoided or similar? | Unclear risk | Not described |
| Compliance acceptable? | Unclear risk | Not described |
| Similar timing of outcome assessment? | Low risk | Baseline, 6 weeks, 12 months |
Schomacher 2009.
| Methods | Type of trial: RCT Number analysed/randomly assigned: 126/126 Intention‐to‐treat analysis: calculated | |
| Participants | Neck disorder ± radicular symptoms or signs (inclusion criteria; patient with or without irradiation into the arm(s) that changed with movements between C2 and C7), duration NR | |
| Interventions | INDEX TREATMENT
Mobilisation (A): technique: intermittent translatoric (perpendicular to the facet plane) traction at the most painful joint between C2 and C7; timing: at baseline; frequency: 1 session; dose: grade II, 6 to 7/Hz and changed as needed at 30 seconds; duration: 4 minutes; route: cervical spine COMPARISON TREATMENT Mobilisation 3 levels below or above (B): technique: intermittent translatoric (perpendicular to the facet plane) traction 3 levels below or above the most painful joint between C2 and C7; timing: at baseline; frequency: 1 session; dose: grade II, 6 to 7 Hz and changed as needed at 30 seconds; duration: 4 minutes; route: cervical spine CO‐INTERVENTION: not specified. Duration of treatment: 1 day, 1 session Duration of follow‐up: 0 days |
|
| Outcomes | PAIN (NRS, 0 to 10)
Baseline mean: A 3.1, B 3.7
End of study mean: A 1.8, B 2.0
Absolute benefit: A 1.3, B 1.7
Reported results: not significant SMD (A vs B): ‐0.13 (95% CI ‐0.48 to 0.22) FUNCTION: NR GPE: NR PATIENT SATISFACTION: NR QoL: NR SIDE EFFECTS Allodynia: A 1/59, B 1/67 COST OF CARE: NR |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not adequately described |
| Allocation concealment (selection bias) | Unclear risk | Not adequately described |
| Blinding of Participants (performance bias) | Low risk | Our group believes that the participant would not be able to perceive differences between the 2 interventions |
| Blinding of Personal (performance bias) | High risk | Page 103, middle column, paragraph 1 and page 107, left column, paragraph 2 |
| Blinding of the Outcome assessor (detection bias) | Low risk | Participant is the assessor |
| Incomplete outcome data (attrition bias) | Low risk | Only 2 dropouts due to allodynia |
| Randomized Participants analysed were allocated (attrition bias) | High risk | 2 dropouts not analysed |
| Selective outcome (reporting bias) | Unclear risk | No protocol |
| Similar groups at baseline? | Low risk | Page 104 |
| co‐interventions avoided or similar? | Low risk | Pre‐post design |
| Compliance acceptable? | Low risk | Pre‐post design |
| Similar timing of outcome assessment? | Low risk | Pre‐post design |
Shin 2006.
| Methods | Type of trial: RCT Number analysed/randomly assigned: 26/26 Intention‐to‐treat analysis: not specified | |
| Participants | Specific cervical disorder: herniated cervical disc (MRI diagnosis), duration NR | |
| Interventions | INDEX TREATMENT Chuna manual therapy (A): technique: soft tissue manipulation and thrust technique analogous to chiropractic manipulation, in which the practitioner’s hands apply focused and forceful movements to various areas of the body; timing: at baseline; frequency : 1 session/d for 2 weeks; duration: 20 minutes; route: various areas of the body COMPARISON TREATMENT Traction (B): technique: cervical traction treatment; timing: at baseline; frequency: 1 session/d for 2 weeks; duration: 20 minutes; route: cervical spine CO‐INTERVENTION: not specified Duration of treatment: 2 weeks, 12 sessions Duration of follow‐up: 0 days |
|
| Outcomes | PAIN (VAS, 0 to 10)
Baseline mean: A 7.5, B 7.2
End of study mean: A 2.7, B 4.2
Absolute benefit: A 4.8, B 3.0
Reported results: significant favouring A SMD (A vs B): ‐0.94 (95% CI ‐1.75 to ‐0.12) FUNCTION: NR GPE: NR PATIENT SATISFACTION: NR QoL: NR SIDE EFFECTS: reported (no adverse effects occurred) COST OF CARE: NR |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not adequately described |
| Allocation concealment (selection bias) | Unclear risk | Not adequately described |
| Blinding of Participants (performance bias) | High risk | Not possible owing to differences between interventions |
| Blinding of Personal (performance bias) | High risk | Not possible owing to differences between interventions |
| Blinding of the Outcome assessor (detection bias) | High risk | Not possible owing to differences between interventions |
| Incomplete outcome data (attrition bias) | Low risk | No dropouts |
| Randomized Participants analysed were allocated (attrition bias) | Low risk | No dropouts |
| Selective outcome (reporting bias) | Unclear risk | No protocol |
| Similar groups at baseline? | Unclear risk | Data were given only for age and pain; missing for other characteristics |
| co‐interventions avoided or similar? | Unclear risk | Not described |
| Compliance acceptable? | Low risk | Table 1 – appears that all received 12 treatments. |
| Similar timing of outcome assessment? | Low risk | Baseline, 2 weeks |
Sillevis 2010.
| Methods | Type of trial: RCT Number analysed/randomly assigned: 100/101 Intention‐to‐treat analysis: not specified | |
| Participants | Chronic non‐specific neck pain | |
| Interventions | INDEX TREATMENT
Thoracic manipulation (A): technique: high‐velocity mid‐range and anterior‐to‐posterior force to the upper thoracic segment. Participant in supine position, arms crossed over the chest; timing: at baseline; frequency: 1 treatment session; dose: 1 thrust; route: thoracic spine (T3 to T4) COMPARISON TREATMENT Thoracic mobilisation (B): technique: described by Cleland et al. Practitioner’s flat hand placed under T4 segment, participant in the same position as described in group A. Application of a light 3‐second compression of the participant's arm to the chest; timing: at baseline; frequency: 1 treatment session; dose: 1 mobilisation; route: thoracic spine (T3 to T4) CO‐INTERVENTION: avoided in trial design; no medication that alters the functioning of the autonomic nervous system less than 24 hours before the study, and no caffeinated drinks, smoke or food less than 12 hours before the study Duration of treatment: 1 day, 1 session Duration of follow‐up: 0 days |
|
| Outcomes | PAIN (VAS, 0 to 100)
Baseline mean: A 38, B 33
End of study mean: A 32, B 28
Absolute benefit: A 6, B 5
Reported results: not significant FUNCTION: NR GPE: NR PATIENT SATISFACTION: NR QoL: NR SIDE EFFECTS: NR COST OF CARE: NR |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Page 184, left column, paragraph 2 |
| Allocation concealment (selection bias) | Low risk | Page 184, left column, paragraph 2 |
| Blinding of Participants (performance bias) | Unclear risk | Unsure whether control was a true sham manipulation |
| Blinding of Personal (performance bias) | High risk | Not possible owing to design |
| Blinding of the Outcome assessor (detection bias) | Unclear risk | Unsure whether control was a true sham manipulation |
| Incomplete outcome data (attrition bias) | Low risk | 1 dropout |
| Randomized Participants analysed were allocated (attrition bias) | High risk | Figure 3 and Table 1 do not add up to 101 analysed |
| Selective outcome (reporting bias) | Unclear risk | No protocol |
| Similar groups at baseline? | Low risk | Table 1 |
| co‐interventions avoided or similar? | Low risk | Pre‐post design |
| Compliance acceptable? | Low risk | Pre‐post design |
| Similar timing of outcome assessment? | Low risk | Pre‐post design |
Sloop 1982.
| Methods | Type of trial: RCT cross‐over design Number analysed/randomly assigned: 39/39 Intention‐to‐treat analysis: calculated | |
| Participants | Subacute chronic neck pain with variable degenerative changes (cervical spondylosis) | |
| Interventions | INDEX TREATMENT
Manipulation group (manip): technique: manipulation described by Cyriax, Maigne, Maitland, Matthews, muscle relaxant; frequency: 1 session; route: cervical spine COMPARISON TREATMENT Control treatment (cntl): muscle relaxant CO‐INTERVENTION: "other medical management was not restricted during the study" Duration of treatment: 1 session Duration of follow‐up: 3 weeks (then cross‐over occurs) |
|
| Outcomes | PAIN (neck pain intensity; VAS, 0 to 100)
Baseline: NR
Absolute benefit: manip 18, cntl 5
Reported results: not significant
SMD: 0.40 (95% CI ‐1.04 to 0.23) (power 5%) FUNCTION (selected daily activities; VAS, 0 to 100) Baseline: NR Reported results: not significant PATIENT SATISFACTION: NR QoL: NR GPE [patient perceived effect, 0 (completely well) to 8 (worst possible), collapsed to dichotomous response (improved/not improved) Reported results: not significant RR: 0.59 (95% CI 0.34 to 1.05) SIDE EFFECTS: 2 people had superficial phlebitis following diazepam injection and recovered uneventfully; 2 people in the manipulation group reported new discomfort in their neck followed by improvement in their chronic neck pain RR: 1.0 (95% CI 0.4 to 2.4) COST OF CARE: NR |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Page 533, column 1, paragraph 1 |
| Allocation concealment (selection bias) | Low risk | Page 533, column 2, paragraph 2 |
| Blinding of Participants (performance bias) | Low risk | Cross‐over design |
| Blinding of Personal (performance bias) | High risk | Not possible owing to design |
| Blinding of the Outcome assessor (detection bias) | Low risk | Page 533, column 2, paragraph 3 |
| Incomplete outcome data (attrition bias) | Low risk | Page 534, column 1, paragraph 1 |
| Randomized Participants analysed were allocated (attrition bias) | Low risk | Cross‐over design |
| Selective outcome (reporting bias) | Unclear risk | No reported protocol |
| Similar groups at baseline? | Low risk | Page 533, column 1, paragraph 5 |
| co‐interventions avoided or similar? | High risk | Not reported |
| Compliance acceptable? | Low risk | Cross‐over design |
| Similar timing of outcome assessment? | Low risk | Baseline, 3 weeks, 12 weeks |
Sterling 2010.
| Methods | Type of trial: RCT Number analysed/randomly assigned: 39/39 Intention‐to‐treat analysis: calculated | |
| Participants | Subacute chronic neck pain > 3 months WAD II | |
| Interventions | INDEX TREATMENT
Cervical SMT group: lateral glide mobilisation technique; frequency of treatment: 1 session Dose of treatment: 3 sets of 1 minute; 5 minutes total: 3 minutes of treatment with 1 minute rest between sets Duration of treatment: 1 session Route: C5/6 Duration of follow‐up: 0 days CONTROL TREATMENT Manual contact CO‐INTERVENTION: avoided in trial designs |
|
| Outcomes | PAIN (neck pain intensity; VAS, 0 to 10) Baseline mean: SMT 6.2, cntl 4.5 End of study mean: SMT 5.8, cntl 3.6 Absolute benefit: SMT 0.4, cntl 0.9 Reported results: favours control SMD: SMT vs cntl: 2.2 (95% CI 1.74 to 2.66) FUNCTION: NR PATIENT SATISFACTION: NR QoL: NR GPE: NR SIDE EFFECTS: NR COST OF CARE: NR |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Page 151, left column, paragraph 2 |
| Allocation concealment (selection bias) | Unclear risk | Page 151, left column, paragraph 2 |
| Blinding of Participants (performance bias) | High risk | Stated participant not blinded, page 153, left column, paragraph 3 |
| Blinding of Personal (performance bias) | High risk | Not possible |
| Blinding of the Outcome assessor (detection bias) | High risk | Stated participant not blinded, page 153, left column, paragraph 3 |
| Incomplete outcome data (attrition bias) | Low risk | Pre‐post design |
| Randomized Participants analysed were allocated (attrition bias) | High risk | ITT not done for NFR |
| Selective outcome (reporting bias) | Unclear risk | No protocol |
| Similar groups at baseline? | High risk | VAS different between groups |
| co‐interventions avoided or similar? | Low risk | Pre‐post design |
| Compliance acceptable? | Low risk | Pre‐post design |
| Similar timing of outcome assessment? | Low risk | Pre‐post design |
Strunk 2008.
| Methods | Type of trial: RCT Number analysed/randomly assigned: 5/6 Intention‐to‐treat analysis: calculated | |
| Participants | Subacute or chronic neck pain | |
| Interventions | INDEX TREATMENT Cervical manipulation (A): technique: high‐velocity low‐amplitude manipulation of hypomobile segment of the cervical spine; frequency: 2 sessions/wk; dose: grade 5 manipulation; route: hypomobile segments identified from C0 to C7 COMPARISON TREATMENT Thoracic and sacroiliac manipulation + muscle energy technique (B): For thoracic spine and sacroiliac joint manipulation: technique: high‐velocity low‐amplitude spinal manipulation; frequency: 2 sessions/wk; dose: grade 5 manipulation; route: thoracic spine and sacroiliac joint. Muscle energy: technique: post‐isometric relaxation technique to hypertonic muscles according to Lewis procedures; frequency: 2 sessions/wk; dose: 2 sets of 3 reps; route: left or right scalenes, upper fibres of trapezius, levator scapulae, suboccipital muscles based on assessment findings CO‐INTERVENTION: NR Duration of treatment: 2 weeks, 4 sessions Duration of follow‐up: 0 days |
|
| Outcomes | PAIN (VAS, 0 to 100)
Baseline median: A 29, B 35
2‐Week median: A 27, B 65 Absolute benefit: A 2, B ‐30 Reported results: not significant SMD (A vs B): 0.99 (95% CI ‐0.88 to 2.85) FUNCTION (NDI, 0 to 100%) Baseline median: A 24, B 34 2‐Week median: A 20, B 26 Absolute benefit: A 4, B 8 Reported results: not significant SMD (A vs B): ‐0.48 (95% CI ‐2.15 to 1.19) GPE: NR PATIENT SATISFACTION: NR QoL: NR SIDE EFFECTS Discomfort: A and B combined 3/5 Neck pain/stiffness (lasting < 10 minutes): A 0/3, B 1/2 Dizziness/imbalance: A 0/3, B 1/2 Neck pain/stiffness (onset > 24 hours post treatment, duration > 24 hours): A 1/3, B 0/2 COST OF CARE: NR |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Page 3, left and right columns |
| Allocation concealment (selection bias) | Low risk | Page 3, left and right columns |
| Blinding of Participants (performance bias) | High risk | Not possible owing to study design |
| Blinding of Personal (performance bias) | High risk | Not possible owing to study design |
| Blinding of the Outcome assessor (detection bias) | High risk | Not possible owing to study design |
| Incomplete outcome data (attrition bias) | Low risk | No dropouts |
| Randomized Participants analysed were allocated (attrition bias) | Low risk | Table 2, no dropouts |
| Selective outcome (reporting bias) | Unclear risk | No reported protocol |
| Similar groups at baseline? | High risk | NDI scores different between groups |
| co‐interventions avoided or similar? | Unclear risk | No data available for measurement |
| Compliance acceptable? | Low risk | Page 5, right column, paragraph 2 |
| Similar timing of outcome assessment? | Low risk | Baseline, 2 weeks |
van Schalkwyk 2000.
| Methods | Type of trial: quasi‐RCT Number analysed/randomly assigned: 30/30 Intention‐to‐treat analysis: NR | |
| Participants | Neck pain, duration NR | |
| Interventions | INDEX TREATMENT
Cervical rotary break manipulation (A): technique: manipulation with contact taken on the ipsilateral side, described by Szaraz; frequency: 10 sessions over 4 weeks; route: cervical spine COMPARISON TREATMENT Lateral break manipulation (B): technique: manipulation with contact taken on the contralateral side, described by Szaraz; frequency: 10 sessions over 4 weeks; route: cervical spine CO‐INTERVENTION: NR Duration of treatment: 4 weeks, 10 sessions Duration of follow‐up: 4 weeks |
|
| Outcomes | PAIN INTENSITY (NRS, 0 to 100)
Baseline mean: A 38.28, B 33.25
End of study mean: A 9.40, B 17.54
Absolute benefit: A 28.88, B 15.71
Reported results: not significant SMD (A vs B): IP ‐0.67 (95% CI ‐1.41 to 0.07), ST SMD (A vs B): ‐0.69 (95% CI ‐1.43 to 0.05) FUNCTION (NDI, 0 to 50) Baseline mean: A 22.53, B 16.4 End of study mean: A 6.00, B 6.13 Absolute benefit: A 16.53, B 10.27 Reported results: not significant SMD (A vs B): IP ‐0.02 (95% CI ‐0.73 to 0.70), ST ‐0.02 (95% CI ‐0.74 to 0.70) PATIENT SATISFACTION: NR GPE: NR QoL: NR SIDE EFFECTS: NR COST OF CARE: NR |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Page 327, right column, paragraph 1 |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of Participants (performance bias) | High risk | Not possible owing to design |
| Blinding of Personal (performance bias) | High risk | Not possible owing to design |
| Blinding of the Outcome assessor (detection bias) | High risk | Not possible owing to design |
| Incomplete outcome data (attrition bias) | Unclear risk | Not described |
| Randomized Participants analysed were allocated (attrition bias) | Unclear risk | Not described |
| Selective outcome (reporting bias) | Unclear risk | No reported protocol |
| Similar groups at baseline? | Low risk | Table 14 |
| co‐interventions avoided or similar? | Unclear risk | Not described |
| Compliance acceptable? | Unclear risk | Not described |
| Similar timing of outcome assessment? | Unclear risk | Unclear description, page 328, left column, paragraph 3 |
von Piekartz 2011.
| Methods | Type of trial: RCT Number analysed/randomly assigned: 38/43 Intention‐to‐treat analysis: not specified | |
| Participants | Chronic cervicogenic headache (diagnosed according to ICDH‐II); other (minimum of 1 of the 4 signs of TMD: joint sounds, deviation during mouth opening, extraoral muscle pain at a minimum of 2 tender points and pain during passive mouth opening) | |
| Interventions | INDEX TREATMENT Manual therapy to cervical spine (A): technique: manual therapy, therapist decision; timing: at baseline; frequency: depended on therapist decision; dose: 6 treatments; duration: 30 minutes; route: cervical spine COMPARISON TREATMENT Manual therapy to the TMJ (B): technique: accessory (translatory) movements of the temporomandibular region and/or masticatory muscle techniques (tender‐trigger point treatment and muscle stretching), active and passive movement of cranial nerve tissue, co‐ordination exercises, home exercises and treatment of the cervical region when necessary; timing: at baseline; frequency: depended on therapist decision; dose: 6 sessions; duration: 30 minutes; route: TM region and cervical spine CO‐INTERVENTION: not specified Duration of treatment: minimum 21 and maximum 42 days, 6 sessions Duration of follow‐up: 6 months |
|
| Outcomes | PAIN (CGH pain, CAS, 0 to 10)
Baseline mean: A 7.1, B 7.3
End of study mean: A 7.0, B 2.4
Absolute benefit: A 0.1, B 4.9
Reported results: significant favouring B SMD (A vs B): IP 2.27 (95% CI 1.43 to 3.10); NNTB 2, IT 3.55 (95% CI 2.50 to 4.61); NNTB 2 FUNCTION (NDI, 0 to 50) Baseline mean: A 15.4, B 15.6 End of study mean: A 14.9, B 6.3 Absolute benefit: A 0.5, B 9.3 Reported results: significantfavouring B SMD (A vs B): IP 1.35 (95% CI 0.64 to 2.06); NNTB 5, IT 2.22 (95% CI 1.39 to 3.04); NNTB 4 GPE: NR PATIENT SATISFACTION: NR QoL: NR SIDE EFFECTS: NR COST OF CARE: NR |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Page 3, left column, paragraph 1 |
| Allocation concealment (selection bias) | Unclear risk | Concealment not described |
| Blinding of Participants (performance bias) | High risk | Not possible owing to differences between interventions |
| Blinding of Personal (performance bias) | High risk | Not possible owing to differences between interventions |
| Blinding of the Outcome assessor (detection bias) | High risk | Not possible owing to differences between interventions |
| Incomplete outcome data (attrition bias) | Low risk | Page 5, right column, paragraph 3 |
| Randomized Participants analysed were allocated (attrition bias) | High risk | Intention‐to‐treat not done; Figure 1 shows numbers; page 5, right column, paragraph 3 |
| Selective outcome (reporting bias) | Unclear risk | No protocol |
| Similar groups at baseline? | Low risk | Table 3 |
| co‐interventions avoided or similar? | Unclear risk | Not reported |
| Compliance acceptable? | Unclear risk | Home exercise compliance not reported |
| Similar timing of outcome assessment? | Low risk | Baseline, 3 months, 6 months |
Wood 2001.
| Methods | Type of trial: quasi‐RCT Number analysed/randomly assigned: 30/30 Intention‐to‐treat analysis: calculated | |
| Participants | Subacute neck pain | |
| Interventions | INDEX TREATMENT
Manual manipulation (A): technique: high‐velocity low‐amplitude manual adjustment; frequency: 2 to 3 sessions/wk; route: cervical spine COMPARISON Manipulation with Activator II (B): technique: manipulation using Activator II adjusting Instrument, mechanical force, manually assisted; frequency: 2 to 3 sessions/wk; route: cervical spine CO‐INTERVENTION: no medication ≥ 1 month; no other treatment modalities, exercises or education prescribed Duration of treatment: 4 weeks, 8 sessions Duration of follow‐up: 4 weeks |
|
| Outcomes | PAIN INTENSITY (NRS, 0 to 100)
Baseline mean: A 48.0, B 52.5
End of study mean: A 18.7, B 23.5
Absolute benefit: A 29.3, B 29.0
Reported results: not significant
SMD (A vs B): ‐0.29 (95% CI ‐1.01 to 0.43) FUNCTION (NDI, 0 to 50) Baseline mean: A 26.8, B 31.8 End of study mean: A 11.0, B 13.5 Absolute benefit: A 15.8, B 18.3 Reported results: not significant SMD (A vs B): ‐0.23 (95% CI ‐0.95 to 0.48) PATIENT SATISFACTION: NR GPE: NR QoL: NR SIDE EFFECTS: NR COST OF CARE: NR |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Page 261, right column, paragraph 1 |
| Allocation concealment (selection bias) | Unclear risk | Unsure whether opaque and sealed envelopes were used |
| Blinding of Participants (performance bias) | High risk | Not possible owing to design |
| Blinding of Personal (performance bias) | High risk | Not possible owing to design |
| Blinding of the Outcome assessor (detection bias) | High risk | Not possible owing to design |
| Incomplete outcome data (attrition bias) | Unclear risk | Not described |
| Randomized Participants analysed were allocated (attrition bias) | Unclear risk | Not described |
| Selective outcome (reporting bias) | Unclear risk | No reported protocol |
| Similar groups at baseline? | Low risk | Table 5 |
| co‐interventions avoided or similar? | Unclear risk | Not described in Results section |
| Compliance acceptable? | Unclear risk | Not described |
| Similar timing of outcome assessment? | Low risk | Baseline, 4 weeks, 8 weeks |
Youssef 2013.
| Methods | Type of trial: RCT Number analysed/randomly assigned: 36/38 Intention‐to‐treat analysis: not specified | |
| Participants | Subacute/Chronic cervicogenic headache with neck pain | |
| Interventions | INDEX TREATMENT Mobilisation (A): technique: low‐velocity high‐amplitude passive spinal mobilisation (posterior‐anterior central vertebral pressure; unilateral and bilateral posterior‐anterior vertebral pressure; transverse vertebral pressure); timing: at baseline; frequency: 2 sessions/wk for 6 weeks; duration: 30 to 40 minutes; route: C1 to C3 cervical segment COMPARISON TREATMENT Massage (B): technique: massage regimen consisted of 6 phases: warm‐up, myofascial release, manual cervical traction, trigger point therapy procedure, facilitated stretching techniques and session closure; timing: at baseline; frequency: 2 sessions/wk for 6 weeks; duration: 30 to 40 minutes; route: C‐spine and upper limb/cervical musculature CO‐INTERVENTION: avoided in trial design: therapeutic treatment for neck pain or headache during previous 6 months; comparable between index and control groups: All participants underwent active neck range of motion, isometric and dynamic strengthening and endurance exercises in 2 sessions/wk for 6 weeks Duration of treatment: 6 weeks, 12 sessions Duration of follow‐up: 0 days |
|
| Outcomes | PAIN (CGH pain, NRS, 0 to 10)
Baseline mean: A 7.1, B 6.8
End of study mean: A 2.2, B 4.3
Absolute benefit: A 4.9, B 2.5
Reported results: significant favouring A SMD (A vs B): IP ‐2.89 (95% CI ‐3.85 to ‐1.93) FUNCTION (NDI, 0 to 50) Baseline mean: A 46.7, B 48.3 End of study mean: A 18.9, B 17.5 Absolute benefit: A 27.8, B 30.8 Reported results: not significant SMD (A vs B): IP 0.38 (95% CI ‐0.28 to 1.04) GPE: NR PATIENT SATISFACTION: NR QoL: NR SIDE EFFECTS: NR COST OF CARE: NR |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer generated |
| Allocation concealment (selection bias) | Unclear risk | Envelopes not numbered |
| Blinding of Participants (performance bias) | High risk | Not possible owing to differences in interventions |
| Blinding of Personal (performance bias) | High risk | Not possible owing to differences in interventions |
| Blinding of the Outcome assessor (detection bias) | High risk | Not possible owing to differences in interventions |
| Incomplete outcome data (attrition bias) | Low risk | Page 19, left column, paragraph 2 |
| Randomized Participants analysed were allocated (attrition bias) | Unclear risk | 2 dropouts apparently not analysed, but unclear |
| Selective outcome (reporting bias) | Unclear risk | No protocol or registration |
| Similar groups at baseline? | Low risk | Table 4 |
| co‐interventions avoided or similar? | Unclear risk | Not reported |
| Compliance acceptable? | Unclear risk | Not reported |
| Similar timing of outcome assessment? | Low risk | Baseline, 7 weeks |
Yurkiw 1996.
| Methods | Type of trial: RCT Number analysed/randomly assigned: 28/28 Intention‐to‐treat analysis: NA | |
| Participants | Subacute neck pain | |
| Interventions | INDEX TREATMENT
Spinal manipulation therapy (A): technique: high‐velocity low‐amplitude manual adjustment (described by Haldeman 1992). Diversified techniques, applied 1 technique to lower cervical vertebrae (C3 to C7); frequency: 1 session; route: cervical spine COMPARISON Mechanically assisted device (B): technique: manipulation using Activator adjusting Instrument (described by Petterson), participant in prone position, instrument in "2 ring" setting, applied to posterior pillar of restricted lower cervical vertebrae, 1‐click application given; frequency: 1 session; route: cervical spine CO‐INTERVENTION: avoided Duration of treatment: 1 session Duration of follow‐up: 0 days |
|
| Outcomes | PAIN INTENSITY (VAS, 0 to 100)
Baseline mean: A 32.9, B 32.9
End of study mean: A 20.4, B 21.9
Absolute benefit: A 12.5, B 11.0
Reported results: no significant differences
SMD: ‐0.07 (95% CI ‐0.81 to 0.67) (power 61%) FUNCTION: NR PATIENT SATISFACTION: NR GPE: NR QoL: NR SIDE EFFECTS: NR COST OF CARE: NR |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Page 158, left column, paragraph 4 |
| Allocation concealment (selection bias) | High risk | Page 158, left column, paragraph 4, considered high risk of bias according to scale |
| Blinding of Participants (performance bias) | High risk | Not possible owing to design |
| Blinding of Personal (performance bias) | High risk | Not possible owing to design |
| Blinding of the Outcome assessor (detection bias) | High risk | Not possible owing to design |
| Incomplete outcome data (attrition bias) | Low risk | Pre‐post design |
| Randomized Participants analysed were allocated (attrition bias) | Low risk | Pre‐post design |
| Selective outcome (reporting bias) | Unclear risk | No reported protocol |
| Similar groups at baseline? | Unclear risk | Page 259, statistical analysis section |
| co‐interventions avoided or similar? | Low risk | Pre‐post design |
| Compliance acceptable? | Low risk | Pre‐post design |
| Similar timing of outcome assessment? | Low risk | Pre‐post design |
-
Record of personal communications/Unpublished data.
- Allison 2001 provided an early manuscript and data clarification.
- Brodin 1985 provided additional raw data to facilitate study selection and calculation of effect measures.
- Bronfort 2000 provided his manuscript before publication in Spine and included raw data on range, muscle strength and endurance.
- Coppieter 2001 provided 2 early manuscripts and raw data.
- Hoving 2002 provided an early manuscript and clarification of data.
- Hurwitz 2002 provided an early manuscript.
- Jull 2001 provided an early manuscript and additional unpublished data.
- Koes 1992 provided additional raw data on the neck disorder subgroup to facilitate calculation of effect measures.
- Sloop 1982 communicated that additional information on raw data was not available.
- Definitions of terms.
-
Acute ≤ 30 days (1 month, 4 weeks).
- Subacute = 30 days (1 month, 4 weeks) to 90 days (3 months, 12 weeks).
- Chronic ≥ 90 days (3 months, 12 weeks).
-
Timing of outcomes.
- IP = immediate post‐treatment follow‐up < 1 dayIT = intermediate‐term follow‐up ≥ 3 months and < 1 year.
- LT = long‐term follow‐up ≥ 1 year.
- ST = short‐term follow‐up ≥ 1 day and < 3 months.
-
Types of controls.
- AC = attention control.
- cntl = control group.
- Manual therapy placebo.
- Non‐manual therapy placebo.
- NT = no treatment control.
- Same other treatment control.
- Sham.
- Wait list control.
-
-
Short forms commonly used in text.
-
Clinical terms.
- AROM = active range of motion.
- CGH = cervicogenic headache.
- DT = drug therapy.
- ED = education.
- EMS = electrical muscle stimulation.
- ETT = electrothermal therapy.
- H = heat.
- Kinesio‐tape = an elastic therapeutic sports taping product applied to the neck, thorax and shoulder placed on the skin.
- manip = manipulation.
- MNP = mechanical neck pain.
- mob = mobilisation.
- MT = manual therapy
- PEMT = pulsed electromagnetic therapy.
- PMM = physical medicine methods.
- PROM = passive range of motion.
- PSWD = pulsed short‐wave diathermy.
- SMT = spinal manipulation therapy.
- TENS = transcutaneous electrical nerve stimulation.
- TSM = thoracic spinal thrust manipulation.
- TTM = thoracic thrust manipulation.
- US = ultrasound
- W = watts.
-
- Outcome measures.
- EuroQ = Euro Quality of Life scale, 0 to 100‐point scale.
- GHQ 28 = General Health Questionnaire 28.
- GPE = global perceived effect.
- GRC = global rating of change.
- MCID = minimal clinically important difference.
- MDC = minimal detectable change.
- NDI = Neck Disability Index.
- NPQ = Northwick Park neck pain Questionnaire.
- NPRS = Numerical Pain Rating Scale.
- NRS‐101 = Numerical Rating Scale 101, 0 to 100‐point scale.
- PCS = physical component score.
- PPT = pain pressure threshold, measured by algometry.
- QoL = quality of life measures.
- SF‐12 = Short‐Form 12, short form with 12 questions, yielding an 8‐scale health profile.
- SF‐36 = Short‐Form 36, short form with 36 questions yielding an 8‐scale health profil
- VAS = visual analogue scale.
- WHYMPI = West Haven‐Yale Multidimensional Pain Inventory (subscale of pain severity).
-
Statistical terms.
- ANCOVA = analysis of co‐variance.
- ANOVA = analysis of variance.
- 95% CI = 95% confidence interval.
- IQR = interquartile range.
- ITT = intention‐to‐treat analysis.
- MANOVA = multi‐variate analysis of variance.
- MD = mean difference.
- NNTB = number needed to treat for an additional beneficial outcome.
- RR = risk ratio.
- SD = standard deviation.
- SE = standard error.
- SMD = standard mean difference.
-
Other.
- m = months.
- N/A = not applicable.
- NR = not reported.
- RCT = randomised controlled trial.
- v = versus.
- w = weeks.
- y = years.
-
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Allan 2003 | Intervention: manipulation received in all arms |
| Allison 2002 | Intervention: multi‐modal approach |
| Bablis 2008 | Design: quasi‐RCT sequential allocation cohort |
| Björklund 2012 | Intervention: multi‐modal approach |
| Bonk 2000 | Intervention: multi‐modal approach |
| Borman 2008 | Intervention: mechanical traction |
| Borusiak 2010 | Population: study included only children |
| Bosmans 2011 | Intervention: behavioural exercise programme vs manual therapy |
| Boyles 2010 | Design: this was a secondary analysis in which participants were not randomly assigned |
| Briem 2007 | Intervention: intervention technique was not mobilisation nor manipulation |
| Brodin 1985 | Intervention: multi‐modal approach |
| Brønfort 2001 | Intervention: multi‐modal approach |
| Chiu 2011 | Intervention: participants received mechanical traction using the Tru‐Trac series 92B machine under the supervision of a physiotherapist |
| Cleland 2007a | Design: not an RCT |
| Cleland 2009 | Intervention: aimed at therapist, not at study population |
| Cleland 2010 | Intervention: manipulation and exercise |
| Conforti 2013 | Intervention: multi‐modal |
| Cross 2011 | Design: article is a systematic review, not an RCT |
| Cunha 2008 | Intervention: both groups underwent manual therapy |
| De Hertogh 2009 | Population: tenstion ‐type headache and migraine |
| Donkin 2002 | Population: tension‐type headache |
| Dostal 1997 | Intervention: manipulation was used in combination with ibuprofen as a control |
| Durianova 1977 | Outcome: outcome measure used was not clearly stated |
| Dziedzic 2005 | Intervention: multi‐modal approach |
| Evans 2012 | Intervention: multi‐modal approach |
| Fang 2010 | Population: cervical vertigo |
| Fernandez 2004 JWR | Intervention: multi‐modal approach |
| Fernandez 2008 | Population: asymptomatic individuals |
| Fitz‐Ritson 1994 | Population: unsure, sample not adequately described (query whiplash‐associated neck disorder) |
| Gemmell 2008 | Intervention: ischaemic compression and trigger point pressure release on neck pain |
| Giebel 1997 | Intervention: multi‐modal approach |
| Giles 2003 | Population: unable to split spinal data. Attempts to contact study author resulted in no response |
| Goldie 1970 | Intervention: manual therapy in active and control groups |
| Grunnet‐Nilsson 1999 | Population: did not meet review inclusion criteria |
| Gustavsson 2006 | Intervention: Control treatment was individualised care (acupuncture, massage, mobs, hot pack, TENS, US, exercise), and we were not able to elucidate the exact treatment mix for the "treat as usual" group |
| Haas 2003 | Design: phase IV diagnostic trial, not an efficacy trial |
| Hakkinen 2007 | Intervention: multi‐modal approach |
| Hemmila 2005 | Intervention: multi‐modal approach |
| Hodgson 2006 | Intervention: did not consist of mobilisation nor manipulation |
| Hong 2005 | Outcome: included only measures of blood flow |
| Hoving 2002 | Intervention: multi‐modal approach |
| Hurwitz 2005 | Outcomes: excluded on basis of outcomes |
| Hurwitz 2006 | Outcome: psychosocial outcome measure |
| Jahanshahi 1991 | Population: no sample with neck disorder meeting inclusion criteria (torticollis) |
| Jensen 1990 | Intervention: multi‐modal approach |
| Jensen 1995 | Intervention: no manual therapy intervention |
| Jensen 2009 | Design: observational study |
| Jiang 2012 | Intervention: manual/mechanical traction |
| Jing 2006 | Intervention: Shiatsu type of manipulation |
| Jordan 1998 | Intervention: multi‐modal approach |
| Jull 2001 | Intervention: multi‐modal approach |
| Jull 2007 | Intervention: multi‐modal approach |
| Karlberg 1996 | Intervention: multi‐modal approach |
| Khoury 2002 | Intervention: co‐intervention inconsistencies Design: quasi‐RCT |
| Ko 2010 | Intervention: Control group performed craniocervical flexor exercises Design: method of randomisation unclear |
| Koes 1992 | Intervention: multi‐modal approach |
| Kogstad 1978 | Intervention: multi‐modal approach |
| Kongsted 2007 | Interventions: no manual therapy |
| Krugh 2010 | Population: mixed headache |
| Langevin 2012 | Intervention: Mobilisations were combined with exercises |
| Leboeuf 1987 | Population: no sample with neck disorder meeting inclusion criteria (repetitive strain injury of upper limb) |
| Lee 2010 | Design: case study (not an RCT) |
| Levoska 1993 | Intervention: manual therapy in treatment and control groups |
| Li 2006 | Population: canal spinal stenosis unclear; long tract signs Intervention: local point traction manipulation |
| Lindell 2008 | Population: unable to split data into neck pain‐only group |
| Linton 2001 | Population: unable to split data into neck pain‐only group |
| Maduro de Camargo 2011 | Outcome: PPT was not an outcome of interest in this review |
| Maiers 2007 | Intervention: manipulation plus exercise |
| Maiers 2013 | Population: seniors |
| Manca 2007 | Intervention: no manual therapy included |
| Mansilla‐Feragut 2009 | Outcome was PPT and mouth ROM |
| Mansilla‐Ferragud 2008 | Outcome: PPT was not an outcome of interest in this review |
| McClatchie 2009 | Population: asymptomatic cervical spine; outcomes: no outcomes measuring cervical spine or related disability |
| McKinney 1989 | Intervention: multi‐modal approach |
| McReynolds 2005 | Intervention: multi‐modal approach |
| Mealy 1986 | Intervention: multi‐modal approach |
| Metcalfe 2006 | Outcome: Muscle strength measure was not part of our inclusion outcomes |
| Mezaki 1995 | Design: unsure RCT Population: no participants with neck disorder meeting inclusion criteria (spasmodic torticollis) |
| Moodley 2002 | Intervention: multi‐modal approach |
| Murphy 2010 | Intervention: multi‐modal approach including myofascial trigger point and mobilisation techniques |
| Nagrale 2010 | Intervention: integrated neuromuscular inhibition technique (INIT) |
| Nee 2012 | Intervention: multi‐modal approach |
| Nordemar 1981 | Intervention: multi‐modal approach |
| Palmgren 2006 | Intervention: multi‐modal approach |
| Persson 2001 | Intervention: multi‐modal approach |
| Pool 2006 | Intervention: behavioural exercise programme |
| Pool 2010 | Intervention: behavioural exercise programme |
| Provinciali 1996 | Intervention: multi‐modal approach |
| Reginiussen 2000 | Intervention: multi‐modal approach |
| Reid 2014 | Intervention: mobilisation plus exercise |
| Rubinstein 2007 | Design: not a randomised controlled trial |
| Rupert 2002 | Population: rat study; not human study |
| Schenk 1994 | Population: no sample with neck disorder meeting inclusion criteria (normal cervical spine) |
| Scholten‐Peeters 2003 | Intervention: multi‐modal approach |
| Schwerla 2008 | Intervention: multi‐modal approach |
| Skargren 1998 | Intervention: multi‐modal approach |
| Snyder 1996 | Population: Study population did not meet inclusion criteria for the review |
| Sterling 2001 | Design: a mechanistic trial |
| Strunk 2009 | Design: not an RCT but a single‐group study |
| Tuchin 2000 | Population: individuals with migraine |
| Vasseljen 1995 | Intervention: multi‐modal approach |
| Vernon 1990 | Outcome: PPT was not an outcome of interest in this review |
| Walker 2013 | Intervention: multi‐modal Outcome: adverse effects |
| Whittingham 2001 | Outcome: range of motion data only; study does not meet our inclusion criteria |
| Williams 2003 | Outcome: outcomes for neck and back pain combined |
| Yin 2006 | Intervention: injection‐type manipulation |
| Ylinen 2003 | Intervention: multi‐modal approach |
| Ylinen 2007 | Intervention: multi‐modal approach |
| Young 2009 | Intervention: traction + MT/Ex vs MT/Ex |
| Zaproudina 2007 | Intervention: multi‐modal approach ‐ traditional bone setting ‐ mobilisation and manipulation |
| Zhi 2008 | Intervention: acupuncture |
Characteristics of studies awaiting assessment [ordered by study ID]
Casanova‐Mendez 2014.
| Methods | RCT |
| Participants | Chronic non‐specific neck pain |
| Interventions | Dog technique vs toggle‐recoil technique |
| Outcomes | Self reported neck pain (visual analogue scale); neck mobility (cervical range of motion); pressure pain threshold at cervical and thoracic levels (C4 and T4 spinous process) and over the site described for location of tense bands of the upper trapezius muscle |
| Notes |
Cleland 2007b.
| Methods | RCT |
| Participants | Primarily neck pain with and without upper extremity symptoms |
| Interventions | Thrust vs non‐thrust manipulation/Mobilisation |
| Outcomes | NDI, NRS, fear avoidance |
| Notes | Clarify population |
El Soleny 2014.
| Methods | RCT |
| Participants | Patients with cervical spine disorders |
| Interventions | SNAGs group vs manipulation group vs exercise group |
| Outcomes | Cervical range of motion (CROM) was measured using CROM device, with pain assessed using the visual analogue scale (VAS), and grade of functional recovery measured using the Neck Disability Index (NDI) |
| Notes |
Izquierdo‐Perez 2014.
| Methods | RCT |
| Participants | Chronic neck pain |
| Interventions | High velocity low amplitude (HVLA) vs mobilisation (Mob) vs sustained natural apophyseal glide (SNAG) |
| Outcomes | Visual analogue scale (VAS), Neck Disability Index (NDI), Global Rating of Change (GROC) and cervical range of motion (CROM) |
| Notes |
Karas 2014.
| Methods | RCT |
| Participants | Cervical spine pain |
| Interventions | Seated thoracic manipulation vs targeted supine thoracic manipulation group |
| Outcomes | Pain and flexion ROM measures |
| Notes |
Leonelli 2013.
| Methods | RCT |
| Participants | Radiculopathy |
| Interventions | Neurodynamic technique |
| Outcomes | Pain, NDI |
| Notes | Spanish translation needed |
Moretti 2004.
| Methods | RCT |
| Participants | Benign cervicobrachialgia of mechanical origin |
| Interventions | Manipulative therapy |
| Outcomes | Pain |
| Notes | Interlibrary loan ordered ‐ access to article pending |
Characteristics of ongoing studies [ordered by study ID]
Demircio 2011.
| Trial name or title | Comparison of the Effectiveness of Manual Therapy and Physical Therapy in Patients with Neck Pain |
| Methods | RCT |
| Participants | Patients with chronic neck pain |
| Interventions | Exercice + manual therapy; Exercise + physical therapy; Exercise |
| Outcomes | Pain (VAS) Function (NDI) Quality of life (SF‐36) Global perceived effect |
| Starting date | Unknown |
| Contact information | None |
| Notes |
Groeneweg 2010.
| Trial name or title | Effectiveness and Cost Evaluation of Manual Therapy and Physical Therapy in Patients with Subacute and Chronic Non‐specific Neck Pain: Rationale and Design of a Randomised Controlled Trial (RCT) |
| Methods | Type of trial: RCT protocol
Number analysed/randomly assigned: NR intention‐to‐treat analysis: calculated Power analysis: calculated 80% pre‐hoc (specify beta value per comparison: 0.2) |
| Participants | Subacute/Chronic non‐specific cervical; patients may have received radiation to the elbow and may have CGH (inclusion criteria) |
| Interventions | INDEX TREATMENT
Utrecht manual therapy (A): technique: very gentle mobilisation, without high‐velocity thrust technique at the participant's joint. In MTU, it is common to give advice and recommend exercise. 3D passive movements with low velocity and high accuracy executed repeatedly in the joint in the direction of preferred movement; timing: at baseline; frequency: maximum 6 sessions once or twice a week; duration: 30 to 60 minutes; route: spine and extremity joints COMPARISON TREATMENT Physical therapy (B): technique: active exercise, manual traction or stretching and massage. Minimum 20 minutes on active exercise therapy combined with instruction in each session; timing: at baseline; frequency: maximum 9 sessions once or twice a week; duration: 30 minutes CO‐INTERVENTION Not avoided: Participants are free to use medication prescribed by a physician or of their own choice; avoided in trial design: Participant will not receive treatment other than treatments allocated in the trial Duration of treatment: 6 weeks, maximum 6 (UMT) and 9 (PT) treatment sessions Duration of follow‐up: 52 weeks |
| Outcomes | Pain (NRS), function (NDI), GPE (7‐point ordinal scale) and QoL (PCS and MCS components of SF‐36) |
| Starting date | 2008 |
| Contact information | The Netherlands r.groeneweg@iq.umcn.nl |
| Notes |
Gudavalli 2006.
| Trial name or title | Randomised Clinical Trial Comparing Non‐operative Conservative Medical Care, Chiropractic Cervical Distraction and a Combination of Both for Chronic Neck Pain Health Resources and Services Administration Grant # R18 HP 10001 |
| Methods | RCT |
| Participants | Chronic neck pain with or without associated arm symptoms or headache |
| Interventions | Non‐operative conservative medical care ‐ active exercise programme to stabilise neck muscles and decrease anterior head carriage Application of flexion and traction to specific regions in the cervical spine on a specifically designed table in prone lying Combination therapy with both care processes noted above |
| Outcomes | NDI, VAS pain intensity over previous week |
| Starting date | Study is currently in manuscript phase |
| Contact information | Palmer Center for Chiropractic Research |
| Notes |
Guerriero 1997.
| Trial name or title | Comparative Effects of Manipulation and Physical Therapy on Motion in the Cervical Spine |
| Methods | RCT |
| Participants | Chronic neck pain |
| Interventions | Cervical spine manipulation vs sham treatment vs cervical spine manipulation, ischaemic compression of myofascial trigger points, PNF, interferential therapy |
| Outcomes | Cervical ROM |
| Starting date | |
| Contact information | Palmer Institute of Graduate Studies and Research, Davenport, Iowa. |
| Notes |
Kjellman 1997.
| Trial name or title | Comparison of Treatment of Neck Pain |
| Methods | RCT |
| Participants | Neck pain |
| Interventions | Not specified |
| Outcomes | Not specified |
| Starting date | |
| Contact information | Department of Neuroscience and Locomotion, Physiotherapy, Faculty of Health Sciences, Linkopings Universitet, Sweden |
| Notes |
Langevin 2015.
| Trial name or title | Cervical Radiculopathy: Study Protocol of a Randomised Clinical Trial Evaluating the Effects of Mobilisations and Exercises Targeting the Opening of Intervertebral Foramen (NCT01500044) |
| Methods | RCT |
| Participants | Cervical radiculopathy |
| Interventions | One group will receive a 4‐week rehabilitation programme targeting opening of the intervertebral foramen; the second group will receive a 4‐week conventional rehabilitation programme |
| Outcomes | Primary outcome measure will be the validated Neck Disability Index questionnaire. Secondary outcome measures will include the short version of the Disabilities of the Arm, Shoulder and Hand Questionnaire, a numerical pain rating scale, cervicothoracic mobility and participants' perceived global rating of change |
| Starting date | 2012 |
| Contact information | pierre.langevin@fmed.ulaval.ca |
| Notes |
Nagy 2000.
| Trial name or title | Randomised Placebo Controlled Trial for Cervicobrachial Pain Syndrome Using Manual Therapy |
| Methods | RCT |
| Participants | Cervicobrachial pain syndrome |
| Interventions | Manipulative therapy vs placebo physiotherapy vs control |
| Outcomes | EMG muscle onset, pain, functional disability |
| Starting date | |
| Contact information | B Nagy, The Centre for Musculoskeletal Studies, University Department of Surgery, The University of Western Australia, Australia email: gta@cms.uwa,edu.au |
| Notes |
Scott‐Dawkins 1997.
| Trial name or title | Comparative Effectiveness of Adjustments vs Mobilisation in Chronic Mechanical Neck Pain |
| Methods | RCT |
| Participants | Chronic mechanical neck pain |
| Interventions | Adjustments (diversified) vs mobilisation (muscle energy technique) |
| Outcomes | Cervical ROM, NRS, short form McGill Pain Questionnaire, NDI |
| Starting date | |
| Contact information | Technikon Natal College of Chiropractic, Durban, South Africa |
| Notes |
Shammsuddin 2010.
| Trial name or title | Effectiveness of Thoracic Spine Manipulation on Pain and Disability in Patients with Neck Pain: A Pilot Randomised Clinical Trial |
| Methods | Participants were randomly assigned to receive MNP only or MNP + TTM for a maximum of 12 sessions 2×/wk. Primary outcomes were an 11‐point Numerical Pain Rating Scale (NPS), the Neck Disability Index (NDI), and a 15‐point Global Rating of Change (GRC) scale to measure perceived change in health status. Neck active range of motion (AROM) was a secondary outcome. Outcomes were collected at baseline and at 2, 4 and 6 weeks (GRC was not collected at baseline). As the goal of the study was to prepare parameter estimates, hypothesis testing was not done. We determined clinically important changes by comparing point estimates of within‐participant changes for NPS and NDI vs their established minimal clinically important differences (MCIDs). MCIDs for NPS and NDI are 2 points and 10% change, respectively. We calculated the percentage of participants in each group who reported moderate or higher improvement on the GRC at each follow‐up. For neck AROM, changes greater than published values of minimal detectable change (MDC) were considered noticeable changes. Between‐group differences at 6 weeks in primary outcomes were used to estimate sample size |
| Participants | Mechanical neck pain |
| Interventions | Multi‐modal neck programme (MNP) that includes electrothermal modalities, active exercises and some form of manual therapy (commonly non‐thrust) directed at the cervical spine vs thoracic thrust manipulation (TTM) |
| Outcomes | Pain, disability, AROM, global rating of improvement |
| Starting date | 2010 |
| Contact information | Shamsuddin Khoja, Samannaaz, Daliman, Daniel, Regina Sara, Piva |
| Notes |
Snodgrass 2012.
| Trial name or title | Dose Optimisations for Spinal Treatment Effectiveness (the Dose Study): Higher Applied Mobilisation Force Associated with Reduced Pain and Spinal Stiffness in Patients with Chronic Neck Pain |
| Methods | RCT |
| Participants | Chronic non‐specific neck pain |
| Interventions | Posterior‐to‐anterior mobilisation vs placebo (de‐tuned laser) |
| Outcomes | Pain, PPT, ROM and spinal stiffness |
| Starting date | |
| Contact information | Australia |
| Notes |
Stokke 1995.
| Trial name or title | Randomised Comparison of Chiropractic and Physiotherapy Treatment for Neck Pain of Functional (Mechanical) Origins. A Controlled Clinical Trial |
| Methods | RCT |
| Participants | Neck pain, neck and head pain, neck and shoulder pain |
| Interventions | Chiropractic spinal manipulation vs physiotherapy vs medication |
| Outcomes | NDI, pain intensity VAS |
| Starting date | |
| Contact information | Institute of Community Medicine, School of Medicine, University of Tromso, 9037 Tromso, Norway |
| Notes |
Tanaka 1995.
| Trial name or title | Chiropractic Therapy Compared to Medical Therapy for Chronic Cervical Pain |
| Methods | RCT |
| Participants | Chronic cervical spine pain |
| Interventions | Chiropractic care: (lateral flexion) manipulation, exercise plus heat vs medical care: heat, exercise, acetaminophen |
| Outcomes | McGill Pain Questionnaire, NDI, cervical ROM, cervical muscle strength (Cybex), SF‐36 |
| Starting date | Start: November 1994 Complete: June 1995 |
| Contact information | Colorado Prevention Centre, Denver, Colorado, USA |
| Notes |
Vihstadt 2014.
| Trial name or title | Short‐Term Treatment vs Long‐Term Management of Neck and Back Disability in Older Adults Utilising Spinal Manipulative Therapy and Supervised Exercise: A Parallel‐Group Randomised Clinical Trial Evaluating Relative Effectiveness and Harms |
| Methods | RCT |
| Participants | Back and neck disability |
| Interventions | 12 weeks SMT + SRE or 36 weeks SMT + SRE |
| Outcomes | Self report questionnaires administered at 2 baseline visits and at 4, 12, 24, 36, 52 and 78 weeks post randomisation. Primary outcomes include back and neck disability, measured by the Oswestry Disability Index and the Neck Disability Index. Secondary outcomes include pain, general health status, improvement, self efficacy, kinesiophobia, satisfaction and medication use. Functional outcome assessment occurs at baseline and at week 37 for hand grip strength, short physical performance battery and accelerometry. Individual qualitative interviews are conducted when treatment ends |
| Starting date | 2014 |
| Contact information | Northwestern Health Sciences University, Wolfe‐Harris Center for Clinical Studies, 2501 W. 84th Street, Bloomington, MN 55431, USA |
| Notes |
We have attempted to find most of these study authors over the Internet; however, we have not been able to make contact with many of them, especially authors of older trials.
Differences between protocol and review
Our protocol was published in 2002. We have noted some differences from our original protocol.
The term for type of participant as 'neck disorder with headache' was changed to 'cervicogenic headache'. Diagnostic criteria remain the same. Mechanical neck disorder was changed to neck pain, but the criteria remained the same.
Interventions were subgrouped by region of the body manipulated. Emerging evidence has revealed differences per region. This information was obtained by sensitivity analysis.
We added a grey literature search: clinicaltrials.gov.
A research librarian was hired and developed sensitive and specific search strategies.
Primary outcome categories remain the same, but specific outcomes have evolved over the years.
The body of evidence was assessed by the Strength of Evidence assessment, which has been changed to the GRADE system.
Original methods used the Jadad Scale. The risk of bias system is now used, as recommended by the Cochrane Handbook for Systematic Reviews of Interventions.
The post hoc power analysis for meaningful SMD was discontinued.
Contributions of authors
This is one review of a series conducted by the Cervical Overview Group (COG): Gross AR, Goldsmith CH, Graham N, Santaguida PL, Burnie SJ, Miller J, Peloso P, Kay T, Kroeling P, Trinh K, Langevin P, Santaguida PL, Patel K, Haines T, Haraldsson B, Radylovick Z, Forget M, Szeto G, LeBlanc F, Ezzo J, Morien A, Rice M, Perry L, Fraser M, Cameron I, Wang Z, Lilge L, White R, Bronfort G, Hoving J, Jelley J, Empey B, Lalonde P.
Primary review authors ‐ Gross AR, Langevin P, Burnie SJ, Bédard‐Brochu MS, Empey B, Dugas E, Faber‐Dobrescu M, Andres C, Goldsmith CH, Graham N, Bronfort G, Hoving J, LeBlanc F. Student members of this review: Bédard‐Brochu MS, Empey B, Dugas E, Faber‐Dobrescu M, Andres C, Boudreau M. Statistician ‐ Goldsmith C. Methodological quality assessment ‐ Burnie SJ, Forget M, Goldsmith CH, LeBlanc F, Empey B, Szeto G, Jelley G, Lalonde P. Study identification and selection ‐ Graham N, Brunarski D, Haines T, Gross AR. Research librarian ‐ Rice M. Data abstraction, synthesis, manuscript preparation, public responsibility, grants, administration ‐ Gross AR, Langevin P, Bédard‐Brochu MS, Empey B, Dugas E, Faber‐Dobrescu M, Andres C, Boudreau M. Final synthesis ‐ Gross AR, Langevine P, Burnie SJ, Bronfort G, Hoving J, Bédard‐Brochu MS, Empey B, Dugas E, Faber‐Dobrescu M, Andres C, Boudreau M. Grant writing ‐ Santaguida PL, Gross AR, Graham N. Conference presentation ‐ Empey B, Gross AR, Burnie SJ, Graham N.
Sources of support
Internal sources
McMaster University, Department of Clinical Epidemiology and Biostatistics; School of Rehabilitation Sciences; Occupational Health Program, Canada.
Centric Health, Lifemark Physiotherapy, Canada.
Vrije Universiteit Amsterdam, Academic Medical Centre, Coronel Institute of Occupational Health, Netherlands.
Sunnybrook & Women's College Health Sciences Centre, Physiotherapy Department, Canada.
LAMP Occupational Health Program, Canada.
Northwestern Health Sciences University, Minnesota, USA.
Royal Canadian Chiropractic College, Canada.
External sources
Problem‐based Research Award; Sunnybrook and Women's College Health Sciences Foundation, Canada.
Consortial Center for Chiropractic Research ‐ National Institutes of Health, Bethesda, MD, USA.
Hamilton Hospital Association, Canada.
University of Saskatchewan, Clinical Teaching and Research Award, Canada.
Hamilton Health Sciences Corporation, Chedoke‐McMaster Foundation, Canada.
Declarations of interest
Two of our review authors are authors of included studies. Although Jan Hoving and Gert Bronfort were review authors, they were not involved in decisions about study inclusion, risk of bias assessment or extraction of data from their studies.
New search for studies and content updated (conclusions changed)
References
References to studies included in this review
Aquino 2009 {published data only}
- Aquino RL, Caires PM, Furtado FC, Loureiro AV, Ferreira PH, Ferreira ML. Applying joint mobilization at different cervical vertebral levels does not influence immediate pain reduction in patients with chronic neck pain: a randomized clinical trial. Journal of Manual & Manipulative Therapy 2009;17(2):95‐100. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bitterli 1977 {published data only}
- Bitterli J, Graf R, Robert F, Adler R, Mumenthaler M. The objective of manual‐therapeutic treatment for spondylogenic headache [Zur objectivierung der manualtherapeutischen beeinflussbarkeit des spondylogenen kopfschmerzes (German)]. Nervenarzt 1977;48:259‐62. [PubMed] [Google Scholar]
Bronfort 2012 {published data only}
- Bronfort G, Evans R, Anderson AV, Svendsen KH, Bracha Y, Grimm RH. Spinal manipulation, medication, or home exercise with advice for acute and subacute neck pain: a randomized trial. Annals of Internal Medicine 2012;156:1‐10. [DOI] [PubMed] [Google Scholar]
- Leininger BD, Evans R, Bronfort G. Exploring patient satisfaction: a secondary analysis of a trial of a randomized clinical trial of spinal manipulation, home exercise, and medications for acute and subacute neck pain. Journal of Manipulative Physiological Therapeutics 2014;37:593‐601. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cassidy 1992 {published data only}
- Cassidy J [letter]. The immediate effect on manipulation vs mobilisation pain and range of motion in the cervical spine: a randomized controlled trial. Journal of Manipulative and Physiological Therapeutics 1993;16(4):279‐80. [PubMed] [Google Scholar]
- Cassidy JD, Lopes AA, Yong‐Hing K. The immediate effect of manipulation versus mobilization on pain and range of motion in the cervical spine: a randomized controlled trial. Journal of Manipulative and Physiological Therapeutics 1992;15(9):570‐5. [PubMed] [Google Scholar]
Chen 2007 {published data only}
- Chen L, Zhang XL, Ding H, Tao YQ, Zhan HS. Comparative study on effects of manipulation treatment and transcutaneous electrical nerve stimulation on patients with cervicogenic headache. Journal of Chinese Integrative Medicine 2007;5(4):403‐6. [DOI] [PubMed] [Google Scholar]
Cheung Lau 2011 {published data only}
- Cheung Lau HM, Wing Chiu TT, Lam T. The effectiveness of thoracic manipulation on patients with chronic mechanical neck pain ‐ a randomized controlled trial. Manual Therapy 2011;16:141‐7. [DOI] [PubMed] [Google Scholar]
Cleland 2005 {published data only}
- Cleland JA, Childs JD, McRae M, Palmer JA, Stowell T. Immediate effects of a thoracic manipulation in patients with neck pain: a randomized clinical trial. Manual Therapy 2005;10:127‐35. [DOI] [PubMed] [Google Scholar]
Coppieters 2003 {published data only}
- Coppieters MW, Stappaerts KH. The immediate effects of manual therapy in patients with cervicobrachial pain on neural origin: a pilot study. IFOMT 2000: International Federation of Orthopaedic Manipulative Therapists in Conjunction With the 11th Biennial Conference of the Manipulative Physiotherapists Association of Australia. Perth: The University of Western Australia, 2000:Poster 7.
- Coppieters MW, Stappaerts KH, Wouters LL, Janssens K. Aberrant protective force generation during neural provocation testing and the effect of treatment in patients with neurogenic cervicogenic pain. Journal of Manipulative and Physiological Therapeutics 2003;26(2):99‐106. [DOI] [PubMed] [Google Scholar]
- Coppieters MW, Stappaerts KH, Wouters LL, Janssens K. The immediate effects of a cervical lateral glide treatment technique in patients with neurogenic cervicobrachial pain. Journal of Orthopedic and Sports Physical Therapy 2003;33:369‐78. [DOI] [PubMed] [Google Scholar]
David 1998 {published data only}
- David J, Modi S, Aluko AA, Robertshaw C, Farebrother J. Chronic neck pain: a comparison of acupuncture treatment and physiotherapy. British Journal of Rheumatology 1998;37:118‐22. [DOI] [PubMed] [Google Scholar]
Egwu 2008 {published data only}
- Eqwu MO. Relative therapeutic efficacy of some vertebral mobilization techniques in the management of unilateral cervical spondylosis: a comparative study. Journal of Physical Therapy and Science 2008;20:103‐8. [Google Scholar]
Escortell‐Mayor 2011 {published data only}
- Elustondo SG, Fuertes RR, Mayor EE, Barco AA, Martín YP, Castro BM. Satisfaction of patients with mechanical neck disorders attended to by primary care physical therapists. Journal of Evaluation Clinical Practice 2010;16(3):445‐50. [DOI] [PubMed] [Google Scholar]
- Escortell ME, Lebrijo PG, Perez MY, Asunsolo del Barco A, Riesego FR, Saa Requejo C, et al. Randomized clinical trial for primary care patients with neck pain: manual therapy versus electrical stimulation [Ensayo clinico aleatorizado en pacientes con cervicalgia mecanica en atencion primaria: terapia manual frente a electrostimulacion nerviosa transcutanea (Spanish)]. Atencion Primaria 2008;40(7):337‐43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Escortell‐Mayor E, Riesgo‐Fuertes R, Garrido‐Elustondo S, Asúnsolo‐del Barco A, Díaz‐Pulido B, Blanco‐Díaz M, et al. Primary care randomized clinical trial: manual therapy effectiveness in comparison with TENS in patients with neck pain. Manual Therapy 2011;16:66‐73. [DOI] [PubMed] [Google Scholar]
Fernandez 2004 JWRD {published data only}
- Fernandez‐de‐las‐Penas C, Fernandez‐Carnero J, Plaza Fernandez A, Lomas‐Vega R, Miangolarra‐Page JC. Dorsal manipulation in whiplash injury treatment: a randomized controlled trial. Journal of Whiplash & Related Disorders 2004;3:55‐71. [Google Scholar]
Fernandez 2009 {published data only}
- Fernandez‐de‐las‐Penas C, Cleland J, Huijbregts P, Palomeque‐Del‐Cerro, Gonzalez‐Iglesias J. Repeated applications of thoracic spine thrust manipulation do not lead to tolerance in patients presenting with acute mechanical neck pain: a secondary anaylsis. Journal of Manual & Manipulative Therapy 2009;17(3):154‐62. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gemmell 2010 {published data only}
- Gemmell H, Miller P. Relative effectiveness and adverse effects of cervical manipulation, mobilisation and the activator instrument in patients with sub‐acute non‐specific neck pain: results from a stopped randomised trial. Chiropractic & Osteopathy 2010;18(20):1‐14. [DOI] [PMC free article] [PubMed] [Google Scholar]
Giles 1999 {published data only}
- Giles LGF, Muller R. Chronic spinal pain syndromes: a clinical pilot trial comparing acupuncture, a nonsteroidal anti‐inflammatory drug, and spinal manipulation. Journal of Manipulative and Physiological Therapeutics 1999;22(6):376‐81. [DOI] [PubMed] [Google Scholar]
Gonzalez‐Iglesias 2009 JO {published data only}
- Gonzalez‐Iglesias J, Fernandez‐De‐Las‐Penas C, Cleland JA, Rosario Gutierrez‐Vega M. Thoracic spine manipulation for the management of patients with neck pain: a randomized clinical trial. Journal of Orthopaedic and Sports Physical Therapy 2009;39(1):20‐7. [DOI] [PubMed] [Google Scholar]
Gonzalez‐Iglesias 2009 MT {published data only}
- Gonzalez‐Iglesias J, Fernandez‐de‐las‐Penas C, Cleland J, Alburquerque‐Sendin F, Palomeque‐del‐Cerro L. Inclusion of thoracic spine thrust manipulation into a electro‐therapy/thermal program for the management of patients with acute mechanical neck pain: a randomized clinical trial. Manual Therapy 2009;14:306‐13. [DOI] [PubMed] [Google Scholar]
Haas 2004 {published data only}
- Haas M, Groupp E, Aickin M, Fairweather A, Ganger B, Attwood M, et al. Dose response for chiropractic care of chronic cervicogenic headache and associated neck pain: a randomized pilot study. Journal of Manipulative and Physiological Therapeutics 2004;27:547‐53. [DOI] [PubMed] [Google Scholar]
Haas 2010 {published data only}
- Haas M, Spegman A, Peterson D, Aickin M, Vavrek D. Dose response and efficacy of spinal manipulation for chronic cervicogenic headache: a pilot randomization controlled trial. The Spine Journal 2010;10:117‐28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vavrek D, Haas M, Peterson D. Physical examination and self‐reported pain outcomes from a randomized trial on chronic cervicogenic headache. Journal of Manipulative and Physiological Therapeutics 2010;33(5):338‐48. [DOI] [PMC free article] [PubMed] [Google Scholar]
Howe 1983 {published data only}
- Howe DH, Newcombe RG, Wade MT. Manipulation of the cervical spine ‐ a pilot study. Journal of the Royal College of General Practitioners 1983;33:574‐9. [PMC free article] [PubMed] [Google Scholar]
Hurwitz 2002 {published data only}
- Hurwitz EL, Morgenstern H, Harber P, Kominski GF, Yu F, Adams AH. A randomized trial of chiropractic manipulation and mobilization for patients with neck pain: clinical outcomes from the UCLA Neck‐Pain Study. Research and Practice 2002;92(10):1634‐41. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kanlayanaphotporn 2009 {published data only}
- Kanlayanaphotporn R, Chiradejnant A, Vachalathiti R. The immediate effects of mobilization technique on pain and range of motion in patients presenting with unilateral neck pain: a randomized controlled trial. Archives of Physical Medicine and Rehabilitation 2009;90:187‐92. [DOI] [PubMed] [Google Scholar]
Kanlayanaphotporn 2010a {published data only}
- Kanlayanaphotporn R, Chiradejnant A, Vachalathiti R. Immediate effects of the central posteroanterior mobilization technique on pain and range of motion in patients with mechanical neck pain. Disability and Rehabilitation 2010;32(8):622‐8. [DOI] [PubMed] [Google Scholar]
Krauss 2008 {published data only}
- Krauss J, Creighton D, Ely JD, Podlewska‐Ely J. The immediate effects of upper thoracic translatoric spinal manipulation on cervical pain and range of motion: a randomized clinical trial. Journal of Manual and Manipulative Therapy 2008;16(2):93‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Leaver 2010 {published data only}
- Leaver AM, Maher CG, Herbert RD, Latimer J, McAuley JH, Jull G, et al. A randomized controlled trial comparing manipulation with mobilization for recent onset neck pain. Archives Physical Medicine Rehabilitation 2010;91:1313‐8. [DOI] [PubMed] [Google Scholar]
Lee 2013 {published data only}
- Lee JH, Han EY. A comparison of the effect of PNF, ESWT and TPI on pain and function of patients with myofascial pain syndrome. Journal of Physical Therapy Science 2013;25:341‐4. [Google Scholar]
Lin 2013 {published data only}
- Lin JH, Shen T, Chung RCK, Chiu TTY. The effectiveness of Long’s manipulation on patients with chronic mechanical neck pain: a randomized controlled trial. Manual Therapy 2013;18:308‐15. [DOI] [PubMed] [Google Scholar]
Madson 2010 {published data only}
- Madson TJ, Cieslak KR, Gay RE. Joint mobilization vs massage for chronic mechanical neck pain: a pilot study to assess recruitment strategies and estimate outcome measure variability. Journal of Manipulative and Physiological Therapeutics 2010;33(9):644‐51. [DOI] [PubMed] [Google Scholar]
Martel 2011 {published data only}
- Martel J, Dugas C, Dubois J, Descarreaux M. A randomised control trial of preventive spinal manipulation with and without a home exercise program for patients with chronic neck pain. BMC Musculoskeletal Disorders 2011;12:41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thistle S. Preventive spinal manipulation for patient with chronic neck pain. Dynamic Chiropractic 2011;29(19):1‐7. [Google Scholar]
Martinez‐Segura 2006a {published data only}
- Martinez‐Segura R, Fernandez‐de‐las‐Penas C, Ruiz‐Saez M, Lopez‐Jimenez C, Rodriguez‐Blanco C. Immediate effects on neck pain and active range of motion after a single cervical high‐velocity low amplitude manipulation in subjects presenting with mechanical neck pain: a randomized controlled trial. Journal of Manipulative and Phyiological Therapeutics 2006;29:511‐7. [DOI] [PubMed] [Google Scholar]
Masaracchio 2013 {published data only}
- Masaracchio M, Cleland J, Hellman M, Hagins M. Short‐term combined effects of thoracic spine thrust manipulation and cervical spine nonthrust manipulation in individuals with mechanical neck pain: a randomized clinical trial. Journal of Orthopaedic & Sports Physical Therapy 2013;43(3):118‐27. [DOI] [PubMed] [Google Scholar]
Muller 2005 {published data only}
- Muller R, Giles LGF. Long‐term follow‐up of a randomized clinical trial assessing the efficacy of medication, acupuncture, and spinal manipulation for chronic mechanical spinal pain syndromes. Journal of Manipulative and Physiological Therapeutics 2005;28:3‐11. [DOI] [PubMed] [Google Scholar]
Nilsson 1997 {published data only}
- Nilsson N. A randomized controlled trial of the effect of spinal manipulation in the treatment of cervicogenic headache. Journal of Manipulative and Physiological Therapeutics 1995;18(7):435‐40. [PubMed] [Google Scholar]
- Nilsson N, Christensen HW, Hartvigsen J. Lasting changes in passive range of motion after spinal manipulation: a randomized, blind, controlled trial. Journal of Manipulative and Physiological Therapeutics 1996;19(3):165‐8. [PubMed] [Google Scholar]
- Nilsson N, Christensen HW, Hartvigsen J. The effect of spinal manipulation in the treatment of cervicogenic headache. Journal of Manipulative and Physiological Therapeutics 1997;20(5):326‐30. [PubMed] [Google Scholar]
Parkin‐Smith 1998 {published data only}
- Parkin‐Smith GF, Penter CS. A clinical trial investigating the effect of two manipulative approaches in the treatment of mechanical neck pain: a pilot study. Journal of the Neuromusculoskeletal System 1998;6(1):6‐16. [Google Scholar]
Puentedura 2011 {published data only}
- Puentedura EJ, Landers MR, Cleland JA, Mintken PE, Huijbregts P, Fernández‐de‐Las‐Peñas C. Thoracic spine thrust manipulation versus cervical spine thrust manipulation in patients with acute neck pain: a randomized clinical trial. Journal of Orthopaedic Sports Physical Therapy 2011;41(4):208‐20. [DOI] [PubMed] [Google Scholar]
Ragonese 2009 {published data only}
- Ragonese J. A randomized trial comparing manual physical therapy to therapeutic exercises, to a combination of therapies, for the treatment of cervical radiculopathy. Orthopaedic Practice 2009;21(3):71‐7. [Google Scholar]
Saavedra‐Hernandez 2012CR {published data only}
- Saavedra‐Hernandez M, Arroyo‐Morales M, Cantarero‐Villanueva I, Fernandez‐Lao C, Castro‐Sanchez A, Puentedura E, et al. Short‐term effects of spinal thrust manipulation in patients with chronic neck pain: a randomized clinical trial. Clinical Rehabilitation November 2012:1‐9. [DOI] [PubMed] [Google Scholar]
Saavedra‐Hernández 2012JO {published data only}
- Saavedra‐Hernández M, Castro‐Sánchez AM, Arroyo‐Morales M, Cleland JA, Lara‐Palomo IC, Fernández‐de‐Las‐Peñas C. Short‐term effects of kinesiotaping versus cervical thrust manipulation in patients with mechanical neck pain: a randomized clinical trial. Journal Orthopaedic & Sports Physical Therapy 2012;42(8):724‐30. [DOI] [PubMed] [Google Scholar]
Saayman 2011 {published data only}
- Saayman L, Hay C, Abrahamse H. Chiropractic manipulative therapy and low‐level laser therapy in the management of cervical facet dysfunction: a randomized controlled study. Journal of Manipulative and Physiological Therapeutics 2011;34(3):153‐63. [DOI] [PubMed] [Google Scholar]
Savolainen 2004 {published data only}
- Savolainen A, Ahlberg J, Nummila H, Nissinen M. Active or passive treatment for neck‐shoulder pain in occupational health care? A randomized controlled trial. Occupational Medicine 2004;54:422‐4. [DOI] [PubMed] [Google Scholar]
Schomacher 2009 {published data only}
- Schomacher J. The effect of an analgesic mobilization technique when applied at symptomatic or asymptomatic levels of the cervical spine in subjects with neck pain: a randomized controlled trial. Journal of Manual and Manipulative Therapy 2009;17(2):101‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Shin 2006 {published data only}
- Shin BC, Kim SD, Lee MS [Letter to the editor]. Comparison between the effects of Chuna manipulation therapy and cervical disc traction treatment on pain in patients with herniated cervical disc: a randomized clinical pilot trial. American Journal of Chinese Medicine 2006;34(5):923‐5. [DOI] [PubMed] [Google Scholar]
Sillevis 2010 {published data only}
- Sillevis R, Cleland J. Immediate effects of the audible pop from a thoracic spine thrust manipulation on the autonomic nervous system and pain: a secondary analysis of a randomized clinical trial. Journal of Manipulative and Physiological Therapeutics 2011;34(1):37‐45. [DOI] [PubMed] [Google Scholar]
- Sillevis R, Cleland J, Hellman M, Beekhuizen K. Immediate effects of a thoracic spine thrust manipulation on the autonomic nervous system: a randomized clinical trial. Journal of Manual and Manipulative Therapy 2010;18(4):181‐90. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sloop 1982 {published data only}
- Sloop PR, Smith DS, Goldenberg E, Dore C. Manipulation for chronic neck pain: a double‐blind controlled study. Spine 1982;7(6):532‐5. [DOI] [PubMed] [Google Scholar]
Sterling 2010 {published data only}
- Sterling M, Pedler A, Chan C, Puglisi M, Vuvan V, Vicenzino B. Cervical lateral glide increases nociceptive flexion reflex threshold but not pressure or thermal pain thresholds in chronic whiplash associated disorders: a pilot randomised controlled trial. Manual Therapy 2010;15:149‐53. [DOI] [PubMed] [Google Scholar]
Strunk 2008 {published data only}
- Strunk RG, Hondras MA. A feasibility study assessing manual therapies to different regions of the spine for patients with subacute or chronic neck pain. Journal of Chiropractic Medicine 2008;7:1‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
van Schalkwyk 2000 {published data only}
- Schalkwyk R, Parkin‐Smith GF. A clinical trial investigating the possible effect of the supine cervical rotatory manipulation and the supine lateral break manipulation in the treatment of mechanical neck pain: a pilot study. Journal of Manipulative and Physiological Therapeutics 2000;23(5):324‐31. [DOI] [PubMed] [Google Scholar]
von Piekartz 2011 {published data only}
- Piekartz H, Lüdtke K. Effect of treatment of temporomandibular disorders (TMD) in patients with cervicogenic headache: a single‐blind, randomized controlled study. Journal of Craniomandibular Practice 2011;29(1):1‐14. [DOI] [PubMed] [Google Scholar]
Wood 2001 {published data only}
- Wood TG, Colloca CJ, Matthews R. A pilot randomized clinical trial on the relative effect of instrumental (MFMA) versus manual (HVLA) manipulation in the treatment of cervical spine dysfunction. Journal of Manipulative and Physiological Therapeutics 2001;24(4):260‐71. [DOI] [PubMed] [Google Scholar]
Youssef 2013 {published data only}
- Youssef EF, Al ‐Sayed AS. Mobilization versus massage therapy in the treatment of cervicogenic headache: a clinical study. Journal of Back and Musculoskeletal Rehabilitation 2013;26:17‐24. [DOI] [PubMed] [Google Scholar]
Yurkiw 1996 {published data only}
- Yurkiw D, Mior S. Comparison of two chiropractic techniques on pain and lateral flexion in neck pain patients: a pilot study. Chiropractic Technique 1996;8(4):155‐62. [Google Scholar]
References to studies excluded from this review
Allan 2003 {published data only}
- Allan M, Brantingham JW, Menezes A. Stretching as an adjunct to chiropractic manipulation of chronic neck pain ‐ before, after, or not at all? A perspective, randomized controlled clinical trial. European Journal of Chiropractic 2003;50:41‐52. [Google Scholar]
Allison 2002 {published data only}
- Allison GT, Nagy BM, Hall T. A randomized clinical trial of manual therapy for cervico‐brachial pain syndrome ‐ a pilot study. Manual Therapy 2002;7(2):95‐102. [DOI] [PubMed] [Google Scholar]
Bablis 2008 {published data only}
- Bablis P, Pollard H, Bonello R. Neuro emotional technique for the treatment of trigger point sensitivity in chronic neck pain sufferers: a controlled clinical trial. Chiropractic & Osteopathy 2008;16(4). [DOI] [PMC free article] [PubMed] [Google Scholar]
Björklund 2012 {published data only}
- Björklund M, Djupsjöbacka M, Svedmark A, Häger C. Effects of tailored neck‐shoulder pain treatment based on a decision model guided by clinical assessments and standardized functional tests. A study protocol of a randomized controlled trial. BMC Musculoskeletal Disorders 2012;13(75):1‐14. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bonk 2000 {published data only}
- Bonk AD, Ferrari R, Giebel GD, Edelmann M, Huser R. Prospective randomized controlled study of activity versus collar and the natural history for whiplash injury in Germany. Journal of Musculoskeletal Pain 2000;8(1‐2):123‐32. [Google Scholar]
Borman 2008 {published data only}
- Borman P, Keskin D, Ekici B. The efficacy of intermittent cervical traction in patients with chronic neck pain. Clinical Rheumatology 2008;27:1249‐53. [DOI] [PubMed] [Google Scholar]
Borusiak 2010 {published data only}
- Borusiak P, Biedermann H, Boberhoff S, Opp J. Lack of efficacy of manual therapy in children and adolescents with suspected cervicogenic headache: result of a prospective, randomized, placebo‐controlled and blinded trial. Headache 2010;50:224‐30. [DOI] [PubMed] [Google Scholar]
Bosmans 2011 {published data only}
- Bosmans JE, Pool JJM, Vet HCW, Tulder MW, Oselo RWJG. Is behavioural graded activity cost‐effective in comparison with manual therapy for patients with subacute neck pain? An economic evaluation alongside a randomized clinical trial. Spine 2011;36(18):E1179‐86. [DOI] [PubMed] [Google Scholar]
Boyles 2010 {published data only}
- Boyles RE, Walker MJ, Young BA, Strunce JB, Wainner RS. The addition of cervical thrust manipulations to a manual physical therapy approach in patients treated for mechanical neck pain: a secondary analysis. Journal of Orthopaedic & Sports Physical Therapy March 2010;40(3):133‐40. [DOI] [PubMed] [Google Scholar]
Briem 2007 {published data only}
- Briem K, Huijbregts P, Thorsteinsdottir M. Immediate effects of inhibitive distraction on active range of cervical flexion in patients with neck pain: a pilot study. Journal of Manual and Manipulative Therapy 2007;15(2):82‐92. [DOI] [PMC free article] [PubMed] [Google Scholar]
Brodin 1985 {published data only}
- Brodin H. Cervical pain and mobilization. International Journal of Rehabilitation Research 1984;7(2):190‐1. [DOI] [PubMed] [Google Scholar]
- Brodin H. Cervical pain and mobilization. Manual Medicine 1985;2:18‐22. [Google Scholar]
Brønfort 2001 {published data only}
- Brønfort G, Evan R, Nelson B, Aker PD, Goldsmith CH, Vernon H. A randomized clinical trial of exercise and spinal manipulation for patients with chronic neck pain. Spine 2001;26(7):788‐99. [DOI] [PubMed] [Google Scholar]
- Evans R, Brønfort G, Nelson B, Goldsmith C. Two‐year follow‐up of a randomized clinical trial of spinal manipulation and two types of exercise for patients with chronic neck pain. Spine 2002;27:2383‐9. [DOI] [PubMed] [Google Scholar]
Chiu 2011 {published data only}
- Chiu T, Ng J, Walther‐Zhang B, Lin R, Ortelli L, Chua SW. A randomized controlled trial on the efficacy of intermittent cervical traction for patients with chronic neck pain. Clinical Rehabilitation 2011;25(9):814‐22. [DOI] [PubMed] [Google Scholar]
Cleland 2007a {published data only}
- Cleland J, Flynn T, Childs J, Eberhart S. The audible pop from thoracic spine thrust manipulation and its relation to short‐term outcomes in patients with neck pain. Journal of Manual & Manipulative Therapy 2007;15(3):143‐54. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cleland 2009 {published data only}
- Cleland JA, Fritz JM, Brennan GP, Magel J. Does continuing education improve physical therapists' effectiveness in treating neck pain? A randomized clinical trial. Physical Therapy 2009;89(1):38‐47. [DOI] [PubMed] [Google Scholar]
Cleland 2010 {published data only}
- Cleland J, Mintken P, Christopher K, Fritz J, Glynn P, Whitman J, et al. Examination of a clinical prediction rule to Identify patients with neck pain likely to benefit from thoracic spine thrust manipulation and a general cervical range of motion exercise: multi‐centre randomized clinical trial. Physical Therapy 2010;90(9):1239‐53. [DOI] [PubMed] [Google Scholar]
Conforti 2013 {published data only}
- Conforti M. High power laser therapy treatment compared to simple segmental physical rehabilitation in whiplash injuries (1° and 2° grade of the Quebec Task Force classification) involving muscles and tendons. Muscles Ligaments and Tendons Journal 2013;3(2):106‐11. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cross 2011 {published data only}
- Cross K, Kuenze C, Grindstaff T, Hertel J. Thoracic spine thrust manipulation improves pain, range of motion, and self‐reported function in patients with mechanical neck pain: a systematic review. Journal of Orthopaedic & Sports Physical Therapy 2011;41(9):633‐42. [DOI] [PubMed] [Google Scholar]
Cunha 2008 {published data only}
- Cunha ACV, Burke TN, Franca FJR, Marques AP. Effect of global posture re‐education and of static stretching on pain, range of motion, and quality of life in women with chronic neck pain: a randomized clinical trial. Clinics 2008;63(6):763‐70. [DOI] [PMC free article] [PubMed] [Google Scholar]
De Hertogh 2009 {published data only}
- Hertogh W, Vaes P, Devroey D, Louis P, Carpay H, Truijen S. Preliminary results, methodological considerations and recruitment difficulties of a randomised clinical trial comparing two treatment regimens for patients with headache and neck pain. BMC Musculoskeletal Disorders 2009;10(115). [DOI] [PMC free article] [PubMed] [Google Scholar]
Donkin 2002 {published data only}
- Donkin RD, Parkin‐Smith GF, Gomes AN. Possible effect of chiropractic manipulation and combined manual traction and manipulation on tension‐type headache: a pilot study. Journal of the Neuromusculoskeletal System 2002;10(3):89‐97. [Google Scholar]
Dostal 1997 {published data only}
- Dostal C, Pavelka K, Lewit K. Ibuprofen in the treatment of the cervico‐cranial syndrome in combination with manipulative therapy. Fysiatrickay a Reumatologickay Vestniak [Czech] 1997;56:258‐63. [PubMed] [Google Scholar]
Durianova 1977 {published data only}
- Durianova J. Functional muscle changes and their influence by physiatric means. Fysiat Revmatol Vestn [Slovak] 1977;55:16‐21. [PubMed] [Google Scholar]
Dziedzic 2005 {published data only}
- Dziedzic K, Hill J, Lewis M, Sim J, Daniels J, Hay E. Effectiveness of manual therapy or pulsed shortwave diathermy in addition to advice and exercise for neck disorders: a pragmatic randomized controlled trial in physical therapy clinics. American College of Rheumatology 2005;53:214‐22. [DOI] [PubMed] [Google Scholar]
Evans 2012 {published data only}
- Evans J, Bronfort G, Schulz C, Maiers M, Branda Y, Svendsen K, et al. Supervised exercise with and without spinal manipulation performs similarly and better than home exercise for chronic neck pain: a randomized controlled trial. Spine 2012;15(37):903‐14. [DOI] [PubMed] [Google Scholar]
Fang 2010 {published data only}
- Fang J. Observation of curative effect on fixed spin reduction of spinal manipulation therapy for cervical vertigo. Zhongguo Gu Shang 2010;23(2):99‐101. [PubMed] [Google Scholar]
Fernandez 2004 JWR {published data only}
- Fernandez‐de‐las‐Penas C, Fernandez‐Carnero J, Palomeque del Cerro L, Miangolarra‐Page JC. Manipulative treatment vs. conventional physiotherapy treatment in whiplash injury: a randomized controlled trial. Journal of Whiplash & Related Disorders 2004;3:73‐90. [Google Scholar]
Fernandez 2008 {published data only}
- Fernández‐de‐las‐Peñas C, Alonso‐Blanco C, Cleland JA, Rodríguez‐Blanco C, Alburquerque‐Sendín F. Changes in pressure pain thresholds over C5‐C6 zygapophyseal joint after a cervicothoracic junction manipulation in healthy subjects. Journal of Manipulative and Physiological Therapeutics 2008;31(5):332‐7. [DOI] [PubMed] [Google Scholar]
Fitz‐Ritson 1994 {published data only}
- Fitz‐Ritson D. Efficacy of low energy laser therapy for extensor neck muscles and sleep pattern improvement after "whiplash" injury. Journal of Manipulative and Physiological Therapeutics 1994;17(4):277‐8. [Google Scholar]
Gemmell 2008 {published data only}
- Gemmell H, Allen A. Relative immediate effect of Ischaemic compression and activator trigger point, therapy on active upper trapezius points: a randomised trial. Clinical Chiropractics 2008;11(4):174‐81. [Google Scholar]
Giebel 1997 {published data only}
- Giebel GD, Edelmann M, Huser R. Cervical disc derangement: early function vs immobilizing treatment [Die distorsion der halswirbelsaule: Fruhfunktionalle vs. ruhigstellende behandlung (German)]. Zentralbl Chir 1997;122:517‐21. [PubMed] [Google Scholar]
Giles 2003 {published data only}
- Giles LGF, Muller R. Chronic spinal pain: a randomized clinical trial comparing medication, acupuncture, and spinal manipulation. Spine 2003;28(14):1490‐502. [DOI] [PubMed] [Google Scholar]
Goldie 1970 {published data only}
- Goldie I, Landquist A. Evaluation of the effects of different forms of physiotherapy in cervical pain. Scandanavian Journal of Rehabilatation Medicine 1970;2(3):117‐21. [PubMed] [Google Scholar]
Grunnet‐Nilsson 1999 {published data only}
- Grunnet‐Nilson N, Bove G. Manipulation of episodic neck pain [Manipulationsbehandling af episodisk spaendings‐type‐hovedpine (Dutch)]. Ugeskr Laeger 2000;162:174‐7. [PubMed] [Google Scholar]
Gustavsson 2006 {published data only}
- Gustavsson C, Koch L. Applied relaxation in the treatment of long‐lasting neck pain: a randomized controlled pilot study. Journal of Rehabilitation Medicine 2006;38:100‐7. [DOI] [PubMed] [Google Scholar]
Haas 2003 {published data only}
- Haas M, Groupp E, Panzer D, Parna L, Lumsden S, Aickin M. Efficacy of cervical end‐play assessment as an indicator for spinal manipulation. Spine 2003;28(11):1091‐8. [DOI] [PubMed] [Google Scholar]
Hakkinen 2007 {published data only}
- Hakkinen A, Salo P, Tarvainen U, Wiren K, Ylinen J. Effect of manual therapy and stretching on neck muscle strength and mobility in chronic neck pain. Journal of Rehabilitation Medicine 2007;39:575‐9. [DOI] [PubMed] [Google Scholar]
Hemmila 2005 {published data only}
- Hemmila HM. Bone setting for prolonged neck pain: a randomized clinical trial. Journal of Manipulative and Physiological Therapeutics 2005;28:508‐15. [DOI] [PubMed] [Google Scholar]
Hodgson 2006 {published data only}
- Hodgson L, Fryer G. The effect of manual pressure release on myofascial trigger points in the upper trapezius muscle. International Journal of Osteopathic Medicine 2006;9:27‐46. [Google Scholar]
Hong 2005 {published data only}
- Hong ES, Deng MY, Cheng LH, Zhou S, Wang B, Zhang A, et al. Effect of vertebral manipulation therapy on vertebro‐basilar blood flow in cervical spondylosis of vertebral artery type. Zhongguo Zhong Xi Yi Jie He Za Zhi 2005;25(8):742‐4. [PubMed] [Google Scholar]
Hoving 2002 {published data only}
- Hoving JL, Koes BW, Vet HCW, Windt DAWM, Assendelft WJJ, Mameren H, et al. Manual therapy, physical therapy, or continued care by a general practitioner for patients with neck pain. Annals of Internal Medicine 2002;136(10):713‐59. [DOI] [PubMed] [Google Scholar]
- Hoving JL, Koes BW, Vet HCW, Windt DAWM, Assendelft WJJ, Mameren H, et al. Manual therapy, physical therapy, or continued care by a general practitioner for patients with neck pain: long‐term results from a pragmatic randomized clinical trial. Clinical Journal of Pain 2006;22(4):370‐7. [DOI] [PubMed] [Google Scholar]
- Hoving JL, Vet HCW, Koes BW, Mameren H, Deville WJLM, Windt DAWM, et al. Manual therapy, physical therapy, or continued care by the general practitioner for patients with neck pain: long‐term results from a pragmatic randomized trial. In: Hoving JL editor(s). Thesis. 1st Edition. Wageningen: Pons & Looijen bv, 2001:59‐73. [Google Scholar]
- Korthals‐de Bos IBC, Hoving JL, Tulder MW, Rutten‐van Molken MPMH, Ader HJ, Vet HC, et al. Cost effectiveness of physiotherapy, manual therapy, and general practitioner care for neck pain: economic evaluation alongside a randomized controlled trial. British Medical Journal 2003;326:1‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korthals‐de Bos IBC, Hoving JL, Tulder MW, Rutten‐van Molken MPMH, Ader HJ, Vet HC, et al. Manual therapy is more cost‐effective than physical therapy and GP care for patients with neck pain. Thesis. 1st Edition. Wageningen: Pons & Looijen bv, 2001:75‐89. [Google Scholar]
Hurwitz 2005 {published data only}
- Hurwitz EL, Morgenstern H, Vassilaki M, Chiang LM. Frequency and clinical predictors of adverse reactions to chiropractic care in the UCLA neck pain study. Spine 2005;30(13):1477‐84. [DOI] [PubMed] [Google Scholar]
Hurwitz 2006 {published data only}
- Hurwitz EL, Goldstein MS, Morgenstern H, Chiang LM. The impact of psychosocial factors on neck pain and disability outcomes among primary care patients: results from the UCLA Neck Pain Study. Disability and Rehabilitation 2006;28(21):1319‐29. [DOI] [PubMed] [Google Scholar]
Jahanshahi 1991 {published data only}
- Jahanshahi M, Sartory G, Marsden CD. EMG biofeedback treatment of torticollis: a controlled outcome study. Biofeedback and Self Regulation 1991;16:413‐48. [DOI] [PubMed] [Google Scholar]
Jensen 1990 {published data only}
- Jensen OK, Nielsen FF, Vosmar L. An open study comparing manual therapy with the use of cold packs in the treatment of post‐traumatic headache. Cephalgia 1990;10:241‐50. [DOI] [PubMed] [Google Scholar]
Jensen 1995 {published data only}
- Jensen I, Nygren A, Goldie I, Westerholm P, Jonsson E. The role of the psychologist in multidisciplinary treatments for chronic neck and shoulder pain: a controlled cost‐effectiveness study. Scandanavian Journal of Rehabilitation Medicine 1995;27(1):19‐26. [PubMed] [Google Scholar]
Jensen 2009 {published data only}
- Jensen IB, Busch H, Bodin L, Hagberg J, Nygren A, Bergstrom G. Cost effectiveness of two rehabilitation programmes for neck pain and back pain patients: a seven year follow‐up. Pain 2009;142:202‐8. [DOI] [PubMed] [Google Scholar]
Jiang 2012 {published data only}
- Jiang CB, Wang J, Zheng ZX, Hou JS, Ma L, Sun T. Efficacy of cervical fixed‐point traction manipulation for cervical spondylotic radiculopathy: a randomized controlled trial. Journal of Chinese Integrative Medicine 2012;10(1):54‐8. [DOI] [PubMed] [Google Scholar]
Jing 2006 {published data only}
- Jing FJ, Zhang J. Clinical effect of Yi‐Nao manipulation in the treatment of cervical spondylosis of vertebral artery type. Chinese Journal of Clinical Rehabilitation 2006;10(39):27‐9. [Google Scholar]
Jordan 1998 {published data only}
- Jordan A, Bendix T, Nielsen H, Hansen FR, Host D, Winkel A. Intensive training, physiotherapy, or manipulation for patients with chronic neck pain: a prospective single‐blind randomized clinical trial. Spine 1998;23(3):311‐9. [DOI] [PubMed] [Google Scholar]
Jull 2001 {unpublished data only}
- Jull G, Trott P, Potter H, Zito G, Niere K, Shirley D, et al. A randomized controlled trial of exercise and manipulative therapy for cervicogenic headache. Spine 2001;27(17):1845‐3. [DOI] [PubMed] [Google Scholar]
Jull 2007 {published data only}
- Jull G, Sterling M, Kenardy J, Beller E. Does the presence of sensory hypersensitivity influence outcomes of physical rehabilitation for chronic whiplash? A preliminary RCT. Pain 2007;129:28‐34. [DOI] [PubMed] [Google Scholar]
Karlberg 1996 {published data only}
- Karlberg M, Magnusson M, Eva‐Maj M, Melander A, Moritz U. Postural and symptomatic improvement after physiotherapy in patients with dizziness of suspected cervical origin. Archives of Physical Medicine and Rehabilitation 1996;77:874‐82. [DOI] [PubMed] [Google Scholar]
Khoury 2002 {published data only}
- Khoury MA, Deall AJ. A comparative study to determine the most effective chiropractic treatment protocol in the management of cervicogenic headache. European Journal of Chiropractic 2002;49:104‐5. [Google Scholar]
Ko 2010 {published data only}
- Ko T, Jeong U, Lee K. Effects of the inclusion thoracic mobilization into cranio‐cervical flexor exercise in patients with chronic neck pain. Journal of Physical Therapy Science 2010;22:87‐91. [Google Scholar]
Koes 1992 {published data only}
- Koes B, Bouter LM, Knipshild PG. The effectiveness of manual therapy, physiotherapy and continued treatment by general practitioner for chronic nonspecific back and neck complaints. Journal of Manipulative and Physiological Therapeutics 1991;14:498‐502. [PubMed] [Google Scholar]
- Koes BW. Efficacy of manual therapy and physiotherapy for back and neck complaints (thesis). den Haag: Cip‐Gegevens Koninklijke Bibliotheek, 1992a. [Google Scholar]
- Koes BW, Bouter LM, Mameren H, Esser AH, Verstegen GH, Hofhuizen DM, et al. Randomized clinical trial of manual therapy and physiotherapy for persistent back and neck complaints. Manual Therapy in the Netherlands 1992d;1:7‐12. [Google Scholar]
- Koes BW, Bouter LM, Mameren H, Esser AH, Verstegen GM, Hofhuizen DM, et al. A blind randomized clinical trial of manual therapy and physiotherapy for chronic back and neck complaints: physical outcome measures. Journal of Manipulative Physiological Therapeutics 1992e;15(1):16‐23. [PubMed] [Google Scholar]
- Koes BW, Bouter LM, Mameren H, Esser AH, Verstegen GM, Hofhuizen DM, et al. Randomized clinical trial of manipulative therapy and physiotherapy for persistent back and neck complaints: results of one year follow‐up. British Medical Journal 1992b;304:601‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koes BW, Bouter LM, Mameren H, Esser AHM, Verstegen GJMG, Hofhuizen DM, et al. A randomized clinical trial of manual therapy and physiotherapy for persistent back and neck complaints. Subgroup analysis and relationship between outcomes measures. Journal of Manipulative and Physiological Therapeutics 1993;16(4):211‐9. [PubMed] [Google Scholar]
- Koes BW, Bouter LM, Mameren H, Essers AH, Verstegen GM, Hofhuizen DM, et al. The effectiveness of manual therapy, physiotherapy, and treatment by the general practitioner for nonspecific back and neck complaints. Spine 1992c;17(1):28‐35. [DOI] [PubMed] [Google Scholar]
Kogstad 1978 {published data only}
- Kogstad OA, Karterud S, Gudmundsen J. Cervicobrachialgia. A controlled trial with conventional treatment and manipulation [Cervicobrachialgi (Danish)]. Tidiskr Nor Loegeforen 1978;98(16):845‐8. [PubMed] [Google Scholar]
Kongsted 2007 {published data only}
- Kongsted A, Qerama E, Kasch H, Bendix T, Winther F, Korsholm L, et al. Neck collar, "act‐as‐usual" or active mobilization for whiplash injury?. Spine 2007;32(6):618‐26. [DOI] [PubMed] [Google Scholar]
Krugh 2010 {published data only}
- Krugh JS, Olson LE. Efficacy of orthopaedic manual physical therapy and exercise in the treatment of cervicogenic headache with concurrent headache types: a pilot study. Journal of Manual & Manipulative Therapy 2010;18(4):211‐7. [Google Scholar]
Langevin 2012 {published data only}
- Langevin P, Roy JS, Desmeules F. Cervical radiculopathy: study protocol of a randomised clinical trial evaluating the effect of mobilisations and exercises targeting the opening of intervertebral foramen. BMC Musculoskeletal Disorders 2012;13(10). [DOI] [PMC free article] [PubMed] [Google Scholar]
Leboeuf 1987 {published data only}
- Leboeuf C, Grant BR, Maginnes GS. Chiropractic treatment of repetitive stress injuries: a preliminary prospective outcome study of SMT versus SMT combined with massage. Journal of the Australian Chiropractors Association 1987;17(1):11‐4. [Google Scholar]
Lee 2010 {published data only}
- Lee MJ. Impairment based treatment of neck pain with trunk strengthening following inefficacious manual therapy intervention. Journal of Manual and Manipulative Therapy 2010;18(4):229‐30. [Google Scholar]
Levoska 1993 {published data only}
- Levoska S, Keinanen‐Kiukaanneimi S. Active or passive physiotherapy for occupational cervicobrachial disorders? A comparison of two treatment methods with a 1‐year follow‐up. Archives of Physical Medicine and Rehabilitation 1993;74:425‐30. [PubMed] [Google Scholar]
Li 2006 {published data only}
- Li DJ, Wang J, Gao Q, Hou JS. Interventional effects of cervical local‐point traction, manipulation plus silver needle heat conductive treatment for cervical spinal canal stenosis. Chinese Journal of Clinical Rehabilitation 2006;10(43):7‐10. [Google Scholar]
Lindell 2008 {published data only}
- Lindell O, Johansson SE, Strender LE. Subacute and chronic, non‐specific back and neck pain: cognitive‐behavioural rehabilitation versus primary care. A randomized controlled trial. BMC Musculoskeletal Disorders 2008;9:59‐63. [DOI] [PMC free article] [PubMed] [Google Scholar]
Linton 2001 {published data only}
- Linton SL, Ryberg M. A cognitive‐behavioural group intervention as prevention for persistent neck and back pain in a non‐patient population: a randomized controlled trial. Pain 2001;90:83‐90. [DOI] [PubMed] [Google Scholar]
Maduro de Camargo 2011 {published data only}
- Maduro de Camargo V, Alburquerque‐Sendin F. Immediate effects of electromyographic activity and pressure pain thresholds after a cervical manipulation in mechanical neck pain: a randomized controlled trial. Journal of Manipulative and Physiological Therapeutics 2011;34(4):211‐9. [DOI] [PubMed] [Google Scholar]
Maiers 2007 {published data only}
- Maiers MJ, Hartvigsen J, Schulz C, Schulz K, Evans RL, Bronfort G. Chiropractic and exercise for seniors with low back pain or neck pain: the design of two randomized clinical trials. BMC Musculoskeletal Disorders 2007;8(94):1‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Maiers 2013 {published data only}
- Maiers M, Bronfort G, Evans R, Hartvigsen J, Svendsen K, Bracha Y, et al. Spinal manipulative therapy and exercise for seniors with chronic neck pain. The Spine Journal 2013;10:5‐10. [DOI] [PubMed] [Google Scholar]
Manca 2007 {published data only}
- Manca A, Dumville JC, Torgerson DJ, Klaber Moffett JA, Mooney MP, Jackson DA, et al. Randomized trial of two physiotherapy interventions for primary care back and neck patients: cost‐effectiveness analysis. Rheumatology 2007;46:1495‐501. [DOI] [PubMed] [Google Scholar]
Mansilla‐Feragut 2009 {published data only}
- Mansilla‐Ferragut P, Fernández‐de‐las Peñas C, Alburquerque‐Sendín F, Cleland JA, Boscá‐ Gandía JJ. Immediate effects of atlanta‐occipital joint manipulation on active mouth opening and pressure pain sensitivity in women with mechanical neck pain. Journal of Manipulative and Physiological Therapeutics 2009;32:101‐6. [DOI] [PubMed] [Google Scholar]
Mansilla‐Ferragud 2008 {published data only}
- Mansilla‐Ferragud P, Bosca Gandia JJ. Effect of the manipulation of the occipito‐atlanto‐axial joint complex on mouth opening [Efecto de la manipulacion de la charnela occipito‐atlo‐axiodea en la apertura de la boca (Spanish)]. Osteopathia Cientifica 2008;3(2):45‐51. [Google Scholar]
McClatchie 2009 {published data only}
- Mcclatchie L, Laprade J, Martis S, Jaglal SD, Richardson D. Mobilizations of the asymptomatic cervical spine can reduce signs of shoulder dysfunction in adults. Manual Therapy 2009;14(4):369‐74. [DOI] [PubMed] [Google Scholar]
McKinney 1989 {published data only}
- McKinney LA. Early mobilisation and outcome in acute sprains of the neck. British Medical Journal 1989b;299:1006‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKinney LA, Dornan JO, Ryan M. The role of physiotherapy in the management of acute neck sprains following road‐traffic accidents. Archives of Emergency Medicine 1989a;6(1):27‐33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKinney MB. Treatment of dislocations of the cervical vertebrae in so‐called "whiplash injuries" [Behandlung der HWS‐Distorsionen bei sog "Schleuderverletzungen"]. Orthopade 1994;23(4):287‐90. [PubMed] [Google Scholar]
McReynolds 2005 {published data only}
- McReynolds TM, Sheridan BJ. Intramuscular Ketorolac versus osteopathic manipulative treatment in the management of acute neck pain in the emergency department: a randomized clinical trial. Journal of American Osteopathic Association 2005;105(2):57‐68. [PubMed] [Google Scholar]
Mealy 1986 {published data only}
- Mealy K, Brennan H, Fenelon GC. Early mobilisation of acute whiplash injuries. British Medical Journal 1986;92:656‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Metcalfe 2006 {published data only}
- Metcalfe S, Reese H, Sydenham R. Effect of high‐velocity low‐amplitude manipulation on cervical spin muscle strength: a randomized clinical trial. Journal of Manual & Manipulative Therapy 2006;14(3):152‐8. [Google Scholar]
Mezaki 1995 {published data only}
- Mezaki T, Kaji R, Kimura J, Mannen T. Dose‐response relationship in the treatment of cervical dystonia with botulinum toxin type A (AGN 191622): a phase II study. Brain and Nerve 1995;4:857‐62. [PubMed] [Google Scholar]
- Mezaki T, Kaji R, Kimura J, Osame M, Mizuno Y, Hirayama K, et al. The clinical usefulness of botulinum toxin type A for spasmodic torticollis and facial spasm. Brain and Nerve 1995;47:749‐54. [PubMed] [Google Scholar]
Moodley 2002 {published data only}
- Moodley M, Brantingham JW. The relative effectiveness of spinal manipulation and ultrasound in mechanical pain: pilot study. Journal of Chiropractic Medicine 2002;1(4):184‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Murphy 2010 {published data only}
- Murphy B, Taylor H, Marshall P. The effect of spinal manipulation on the efficacy of a rehabilitation protocol for patients with chronic neck pain: a pilot study. Journal of Manipulative and Physiological Therapeutics 2010;33(3):168‐77. [DOI] [PubMed] [Google Scholar]
Nagrale 2010 {published data only}
- Nagrale A, Glynn P, Joshi A, Ramteke G. The efficacy of an integrated neuromuscular inhibition technique on upper trapezius trigger points in subjects with non‐specific neck pain: a randomized controlled trial. Journal of Manual and Manipulative Therapy 2010;18(1):37‐43. [DOI] [PMC free article] [PubMed] [Google Scholar]
Nee 2012 {published data only}
- Nee RJ, Vicenzino B, Jull GW, Cleland JA, Coppieters MW. Neural tissue management provides immediate clinically relevant benefits without harmful effects for patients with nerve‐related neck and arm pain: a randomised trial. Journal of Physiotherapy 2012;58:23‐31. [DOI] [PubMed] [Google Scholar]
Nordemar 1981 {published data only}
- Nordemar R, Thorner C. Treatment of acute cervical pain ‐ a comparative group study. Pain 1981;10:93‐101. [DOI] [PubMed] [Google Scholar]
Palmgren 2006 {published data only}
- Palmgren PJ, Sandstrom PJ, Lundqvist FJ, Heikkila H. Improvement after chiropractic care in cervicocephalic kinesthetic sensibility and subjective pain intensity in patients with nontraumatic chronic neck pain. Journal of Manipulative and Physiological Therapeutics 2006;29:100‐6. [DOI] [PubMed] [Google Scholar]
Persson 2001 {published data only}
- Persson L, Karlberg M, Magnusson M. Effects of different treatments on postural performance in patients with cervical root compression. A randomized prospective study assessing the importance of the neck in postural control. Journal of Vestibular Research 1996;6(6):439‐53. [PubMed] [Google Scholar]
- Persson LCG, Carlsson CA, Carlsson JY. Long‐lasting cervical radicular pain managed with surgery, physiotherapy, or a cervical collar. A prospective, randomized study. Spine 1997;22(7):751‐8. [DOI] [PubMed] [Google Scholar]
- Persson LCG, Lilja A. Pain, coping, emotional state and physical function in patients with chronic radicular neck pain. A comparison between patients treated with surgery, physiotherapy or neck collar ‐ a blinded, prospective randomized study. Disability and Rehabilitation 2001;23(8):325‐35. [DOI] [PubMed] [Google Scholar]
- Persson LCG, Moritz U, Brandt L, Carlsson CA. Cervical radiculopathy: pain, muscle weakness and sensory loss in patients with cervical radiculopathy treated with surgery, physiotherapy or cervical collar. A prospective, controlled study. European Spine Journal 1994;6(4):256‐66. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pool 2006 {published data only}
- Pool JJM, Ostelo RWJG, Koke AJ, Bouter LM, Vet HCW. Comparison of the effectiveness of a behavioural graded activity program and manual therapy in patients with sub‐acute neck pain: design of a randomized clinical trial. Manual Therapy 2006;11:297‐305. [DOI] [PubMed] [Google Scholar]
Pool 2010 {published data only}
- Pool JJ, Ostelo RW, Knol DL, Vlaeyen JW, Bouter LM, Vet HC. Is a behavioural graded activity program more effective than manual therapy in patients with subacute neck pain? Results of a randomized clinical trial. Spine 2010;35(10):1017‐24. [DOI] [PubMed] [Google Scholar]
Provinciali 1996 {published data only}
- Provinciali L, Baroni M, Illuminati L, Ceravolo MG. Multimodal treatment to prevent the late whiplash syndrome. Scandinavian Journal of Rehabilitation Medicine 1996;28:105‐11. [PubMed] [Google Scholar]
Reginiussen 2000 {published data only}
- Reginiussen T, Johnsen R, Torstensen TA. Efficiency of manual therapy on patients with cervicogenic headache: a randomized single blinded controlled trial. International Federation of Manipulation Therapy, 7th Scientific Conference. Perth: University of Western Australia, 2000:Abstract 105.
Reid 2014 {published data only}
- Reid SA, Rivett DA, Katekar MG, Callister R. Comparison of Mulligan sustained natural apophyseal glides and Maitland mobilizations for treatment of cervicogenic dizziness: a randomized controlled trial. Physical Therapy 2010;94(4):466‐77. [DOI] [PubMed] [Google Scholar]
Rubinstein 2007 {published data only}
- Rubinstein SM, Leboeuf‐Yde C, Knol DL, Koekkoek TE, Pfeifle CE, Tulder MW. The benefits outweigh the risks for patients undergoing chiropractic care for neck pain: a prospective, multicenter, cohort study. Journal of Manipulative and Physiological Therapeutics 2007;30(6):408‐18. [DOI] [PubMed] [Google Scholar]
Rupert 2002 {published data only}
- Rupert R, Xuejun S, Giggleman G, Wang Z. Physiological changes resulting form soft tissue manipulation. Proceedings of the 2002 International Conference on Spinal Manipulation. Toronto, Ontario, Canada: Foundation for Chiropractic Education, 2002.
Schenk 1994 {published data only}
- Schenk R, Adelman K, Rousselle J. The effects of muscle energy technique on cervical range of motion. Journal of Manual & Manipulative Therapy 1994;2(4):149‐55. [Google Scholar]
Scholten‐Peeters 2003 {published data only}
- Scholten‐Peeters GGM, Verhagen AP, Neeleman‐van der Steen, Hurkmans JCAM, Wams RWA, Oosterdorp RAB. Randomized clinical trial of conservative treatment for patients with whiplash‐associated disorders: considerations for the design and dynamic treatment protocol. Journal of Manipulative Physiological Therpeutics 2003;26:412‐20. [DOI] [PubMed] [Google Scholar]
Schwerla 2008 {published data only}
- Schwerla F, Bischoff A, Nurnberger A, Genter P, Guillaume JP, Resch KL. Osteopathic treatment of patients with chronic non‐specific neck pain: a randomised controlled trial of efficacy. Forsch Komplementmed 2008;15:138‐45. [DOI] [PubMed] [Google Scholar]
Skargren 1998 {published data only}
- Skargren EI, Carlsson PG, Oberg BE. One‐year follow‐up comparison of the cost and effectiveness of chiropractic and physiotherapy as primary management for back pain. Spine 1998;23(17):1875‐84. [DOI] [PubMed] [Google Scholar]
- Skargren EI, Oberg BE. Predictive factors for 1‐year outcome of low‐back and neck pain in patients treated in primary care: comparison between the treatment strategies chiropractic and physiotherapy. Pain 1998;77:201‐7. [DOI] [PubMed] [Google Scholar]
- Skargren EI, Oberg BE, Carlsson PG, Gade M. Cost and effectiveness analysis of chiropractic and physiotherapy treatment for low back and neck pain: six‐month follow‐up. Spine 1997;22(18):2167‐71. [DOI] [PubMed] [Google Scholar]
Snyder 1996 {published data only}
- Snyder BJ, Sanders GE. Evaluation of the Toftness system of chiropractic adjusting for subjects with chronic back pain, chronic tension headaches, or primary dysmenorrhoea. Chiropractic Technique 1996;8(1):3‐9. [Google Scholar]
Sterling 2001 {published data only}
- Sterling M, Jull G, Wright A. Cervical mobilisation: concurrent effects on pain, sympathetic nervous system activity and motor activity. Manual Therapy 2001;6(2):72‐81. [DOI] [PubMed] [Google Scholar]
Strunk 2009 {published data only}
- Strunk RG, Hawk C. Effects of chiropractic care on dizziness, neck pain and balance: a single group pre‐experimental, feasibility study. Journal of Chiropractic Medicine 2009;8:156‐64. [DOI] [PMC free article] [PubMed] [Google Scholar]
Tuchin 2000 {published data only}
- Tuchin PJ, Pollard H, Bonello P. A randomized controlled trial of chiropractic spinal manipulation therapy for migraines. Journal of Manipulative and Physiological Therapeutics 2000;23:91‐5. [PubMed] [Google Scholar]
Vasseljen 1995 {published data only}
- Vasseljen O, Johansen BM, Westgaard RH. The effect of pain reduction on perceived tension and EMG‐recoded trapezius muscle activity in workers with shoulder and neck pain. Scandinavian Journal of Rehabilitation Medicine 1995;27:243‐52. [PubMed] [Google Scholar]
Vernon 1990 {published data only}
- Vernon HT, Aker P, Burns S, Viljakaanen S, Short L. Pressure pain threshold evaluation of the effect of spinal manipulation in the treatment of chronic neck pain: a pilot study. Journal of Manipulative and Physiological Therapeutics 1990;13(1):13‐6. [PubMed] [Google Scholar]
Walker 2013 {published data only}
- Walker BF, Hebert JJ, Stomski NJ, Clarke BR, Bowden RS, Mathematics M, et al. Outcomes of usual chiropractic. The OUCH randomized controlled trial of adverse events. Spine 2013;38(20):1723‐9. [DOI] [PubMed] [Google Scholar]
- Walker BF, Losco B, Clarke BR, Hebert J, French S, Stomski NJ. Outcomes of usual chiropractic, harm & efficacy ‐ the OUCH study: study protocol for a randomized controlled trial [study protocol]. Trials Journal 2011;12(235). [DOI] [PMC free article] [PubMed] [Google Scholar]
Whittingham 2001 {published data only}
- Whittingham W, Nilsson N. Active range of motion in the cervical spine increases after spinal manipulation. Journal of Manipulative and Physiological Therapeutics 2001;24(9):552‐5. [DOI] [PubMed] [Google Scholar]
Williams 2003 {published data only}
- Williams NH, Wilkinson C, Russell I, Edwards RT, Hibbs R, Linck P, et al. Randomized osteopathic manipulation study (ROMANS): pragmatic trial for spinal pain in primary care. Family Practice 2003;20(6):662‐9. [DOI] [PubMed] [Google Scholar]
Yin 2006 {published data only}
- Yin ZJ, Chen XM. Effect of clinosatic manipulation on blood flow velocity of patients with cervical spondylosis of vertebral artery type in supine position. Chinese Journal of Clinical Rehabilitation 2006;10(35):90‐1. [Google Scholar]
Ylinen 2003 {published data only}
- Ylinen J, Takala EP, Nykanen M, Hakkinen A, Malkia E, Pohjolainen T, et al. Active neck muscle training in the treatment of chronic neck pain in women. JAMA 2003;289(19):2509‐16. [DOI] [PubMed] [Google Scholar]
Ylinen 2007 {published data only}
- Ylinen J, Kautiainen H, Wiren K, Hakkinen A. Stretching exercises vs manual therapy in treatment of chronic neck pain: a randomized, controlled cross‐over trial. Journal of Rehabilitation Medicine 2007;39:126‐32. [DOI] [PubMed] [Google Scholar]
Young 2009 {published data only}
- Young IA, Michener LA, Cleland JA, Aguilera AJ, Snyder AR. Manual therapy, exercise, and traction for patients with cervical radiculopathy: a randomised clinical trial. Physical Therapy 2009;89:632‐42. [DOI] [PubMed] [Google Scholar]
Zaproudina 2007 {published data only}
- Zaproudina N, Hanninen OOP, Airaksinen O. Effectiveness of traditional bone setting in chronic neck pain: randomized clinical trial. Journal of Manipulative and Physiological Therapeutics 2007;30(6):432‐7. [DOI] [PubMed] [Google Scholar]
Zhi 2008 {published data only}
- Zhi LX, Feng CW, Tu CY. Controlled randomized clinical trail on the therapeutic effect of acupotomy‐injection combined with Feng's spinal manipulation (FSM) for cervical spondylotic radiculopathy. China Journal of Orthopaedics and Trauma 2008;21(6):421‐4. [PubMed] [Google Scholar]
References to studies awaiting assessment
Casanova‐Mendez 2014 {published data only}
- Casanova‐Méndez A, Oliva‐Pascual‐Vaca A, Rodriguez‐Blanco C, Heredia‐Rizo AM, Gogorza‐Arroitaonandia K, Almazán‐Campos G. Comparative short‐term effects of two thoracic spinal manipulationtechniques in subjects with chronic mechanical neck pain: a randomized controlled trial. Manual Therapy 2014;19(4):331‐7. [DOI] [PubMed] [Google Scholar]
Cleland 2007b {published data only}
- Cleland JA, Glynn P, Whitman JM, Eberhart SL, MacDonald C, Childs JD. Short‐term effects of thrust versus nonthrust mobilization/manipulation directed at the thoracic spine in patients with neck pain: a randomized clinical trial. Physical Therapy 2007;87:431‐40. [DOI] [PubMed] [Google Scholar]
El Soleny 2014 {published data only}
- El‐Sodany AM, Alayat MSM, Zafer AMI. Sustained natural apophyseal glides mobilization versus manipulation in the treatment of cervical spine disorders: a randomized controlled trial. International Journal of Advanced Research 2014;2(6):274‐80. [Google Scholar]
Izquierdo‐Perez 2014 {published data only}
- Pérez HP, Perez JLA, Martinez AG, Touche R, Lerma‐Lara S, Gonzalez NC, et al. Is one better than another? A randomized clinical trial of manual therapy for patients with chronic neck pain. Manual Therapy 2014;19:215‐21. [DOI] [PubMed] [Google Scholar]
Karas 2014 {published data only}
- Karas S, Olson‐Hunt MJ. A randomized clinical trial to compare the immediate effects of seated thoracic manipulation and targeted supine thoracic manipulation on cervical spine flexion range of motion and pain. Journal of Manual and Manipulative Therapy 2015;22(2):108‐14. [DOI] [PMC free article] [PubMed] [Google Scholar]
Leonelli 2013 {published data only}
- Leonelli C, Zucchini E, Messora A, Sartini S, Fontana L, Parazza S. Neurodynamic technique benefits in patients with chronic radiculopathy: a pilot study. Scienza Riabilitativa 2013;15(4):19‐28. [Google Scholar]
Moretti 2004 {published data only}
- Moretti B, Vetro A, Garofalo R. Manipulative therapy in the treatment of benign cervicobrachialgia of mechanical origin. La Chirurgia degli Organi di Movimento 2004;89:81‐6. [PubMed] [Google Scholar]
References to ongoing studies
Demircio 2011 {published data only}
- Demircio O, Imaz FY, Baflflerdem B, Kuran B. The comparison of the effectiveness of manual therapy and physical therapy in patients with neck pain. Turkish Journal of Physical Medicine and Rehabilitation 2011;57:1‐334. [Google Scholar]
Groeneweg 2010 {published data only}
- Groeneweg R, Kropman H, Leopold H, Assen L, Mulder J, Tulder MW, et al. The effectiveness and cost‐evaluation of manual therapy and physical therapy in patients with sub‐acute and chronic non specific neck pain. Rationale and design of a randomized controlled trial (RCT) [study protocol]. BMC Musculoskeletal Disorders 2010;11(14). [DOI] [PMC free article] [PubMed] [Google Scholar]
Gudavalli 2006 {published data only}
- Gudavalli MR, Cambron J, Long C, McGregor M, Jedlicka J, Keenum M, et al. A randomized clinical trial comparing non‐operative conservative medical care, chiropractic cervical distraction, and a combination of both for chronic neck pain. The Week in Chiropractic 2005;11(37):1. [Google Scholar]
Guerriero 1997 {published data only}
- Guerriero D. Comparative effects of manipulation and physical therapy on motion in the cervical spine. Proceedings of the International Conference on Spinal Manipulation [Abstract]. Arlington, VA; USA, April 12‐13, 1991.
Kjellman 1997 {published data only}
- Kjellman G, Oberg B, Skargren E. Comparison of treatment in neck pain. The Second International Forum for Primary Care Research on Low Back Pain [Abstract]. The Hague, The Netherlands, May 30‐31, 1997.
Langevin 2015 {published data only}
- Langevin P, Roy JS, Desmeules F. Cervical radiculopathy: study protocol of a randomised clinical trial evaluating the effect of mobilisations and exercises targeting the opening of intervertebral foramen [NCT01500044]. BMC Musculoskeletal Disorders 2012;13:1‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Nagy 2000 {published data only}
- Nagy B, Allison GT, Hall T. Randomised placebo controlled trail for cervicobrachial pain syndrome using manual therapy. International Federation of Manipulative Therapy, 7th Scientific Conference. Perth: The University of Western Australia, November 2000:Abstract 72.
Scott‐Dawkins 1997 {published data only}
- Scott‐Dawkins C. The comparative effectiveness of adjustments versus mobilisation in chronic mechanical neck pain. Proceedings of the Scientific Symposium. Tokyo, Japan, June 2‐8, 1997.
Shammsuddin 2010 {published data only}
- Shamsuddin K. The effectiveness of thoracic spine manipulation on pain and disability in patients with neck pain: a pilot randomized clinical trial (abstract). Arthritis and Rheumatology 2010;62(10):2060. [Google Scholar]
Snodgrass 2012 {published data only}
- Snodgrass S, Rivett D, Vicenzino B, Sterling M. Dose optimization for spinal treatment effectiveness (the dose study): higher applied mobilization force associated with reduced pain and spinal stiffness in patients with chronic neck pain [Abstract]. The International Federation of Orthopaedic Manipulative Physical Therapists 2012.
- Snodgrass SJ, Rivett DA, Sterling M, Vicenzino B. Dose optimisation for spinal treatment effectiveness: a randomised controlled trial investigating the effects of high and low mobilisation forces in patients with neck pain. Journal of Orthopaedic & Sports Physical Therapy 2014;44(3):141‐52. [DOI] [PubMed] [Google Scholar]
Stokke 1995 {published data only}
- Stokke O. A randomized comparison of chiropractic and physiotherapy treatment for neck pain of functional (mechanical) origins: a controlled clinical trial. Conference Proceedings of the Chiropractic Centennial Foundation [Abstract]. July 1995:372‐3.
Tanaka 1995 {published data only}
- Tanaka, D. Pilot study of chiropractic therapy compared to medical therapy for chronic cervical pain. Conference Proceedings of the Chiropractic Centennial Foundation [Abstract]. 1995:374‐5.
Vihstadt 2014 {published data only}
- Vihstadt C, Maiers M, Westrom K, Bronfort G, Evans R, Hartvigsen J, et al. Short term treatment versus long term management of neck and back disability in older adults utilizing spinal manipulative therapy and supervised exercise: a parallel‐group randomized clinical trial evaluating relative effectiveness and harms. Chiropractic & Manual Therapies 2014;22:1‐15. [DOI] [PMC free article] [PubMed] [Google Scholar]
Additional references
Albuquerque 2011
- Albuquerque FC, Hu YC, Dashti SR, Abla AA, Clark JC, Alkire B, et al. Craniocervical arterial dissections as sequelae of chiropractic manipulation: patterns of injury and management. Journal Neurosurgery 2011;115:1197–205. [DOI] [PubMed] [Google Scholar]
Assendelft 1996
- Assendelft WJ, Bouter LM, Knipschild PG. Complications of spinal manipulation: a comprehensive review of the literature. Journal of Family Practice 1996;42(5):475‐80. [PubMed] [Google Scholar]
Basmajian 1993
- Basmajian JV. Rational Manual Therapies. 1st Edition. Baltimore, MD: Williams & Wilkins, 1993. [Google Scholar]
Beattie 2001
- Beattie P. Measurement of health outcomes in the clinical setting: applications to physiotherapy. Physiotherapy Theory and Practice 2001;17:173‐85. [Google Scholar]
Bialosky 2009
- Bialosky JE, Bishop MD, Price DD, Robinson ME, George SZ. The mechanisms of manual therapy in the treatment of musculoskeletal pain: a comprehensive model. Manual Therapy 2009;14:531‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Borghouts 1998
- Borghouts JAJ, Koes BW, Bouter LM. The clinical course and prognostic factors of non‐specific neck pain: a systematic review. Pain 1998;77:1‐13. [DOI] [PubMed] [Google Scholar]
Boyles 2011
- Boyles R, Toy P, Mellon J, Hayes M, Hammer B. Effectiveness of manual physical therapy in the treatment of cervical radiculopathy: a systematic review. Journal of Manipulative and Physiological Therapeutics 2011;19(3):135‐42. [DOI] [PMC free article] [PubMed] [Google Scholar]
Butler 2000
- Butler DS. The Sensitive Nervous System. 1st Edition. Adelaide City: Noigroup Publication, 2000. [Google Scholar]
Calloca 2006
- Colloca CJ, Keller TS, Harrison DE, Moore RJ, Bunzburg R, Harrison DD. Spinal manipulation force and duration affect vertebral movement and neuromuscular responses. Clinical Biomechanics (Bristol, Avon) 2006;21:254‐62. [DOI] [PubMed] [Google Scholar]
Carlesso 2010
- Carlesso LC, Gross AR, Santaguida PL, Burnie SJ, Voth S, Sadi J. Adverse events associated with the use of cervical manipulation and mobilization for the treatment of neck pain in adults: a systematic review. Manual Therapy 2010;15:434‐44. [DOI] [PubMed] [Google Scholar]
Cassidy 2008
- Cassidy DJ, Boyle E, Cote P, He Y, Hogg‐Johnson S, Silver FL, et al. Risk of vertebrobasilar stroke and chiropractic care: results of a population based case‐control and case‐crossover study. Spine 2008;33(45):S176‐83. [DOI] [PubMed] [Google Scholar]
Chaibi 2012
- Chaibi A, Russell M. Manual therapies for cervicogenic headache: a systematic review. Journal of Headache and Pain 2012;13(5):351‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cicchetti 1976
- Cicchetti DV. Assessing inter‐rater reliability for rating scales: resolving some basic issues. British Journal of Psychiatry 1976;129:452‐6. [DOI] [PubMed] [Google Scholar]
Clar 2014
- Clar C, Tsertsvadze A, Court R, Hundt GL, Clarke A, Sutcliffe P. Clinical effectiveness of manual therapy for the management of musculoskeletal and nonmusculoskeletal conditions: systematic review and update of UK evidence report. Chiropractic and Manual Therapies 2014;22(12):1‐34. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cleland 2007
- Cleland JA, Childs JD, Fritz JM, Whitman JM, Eberhart SL. Development of a clinical prediction rule for guiding treatment of a subgroup of patients with neck pain: use of thoracic spine manipulation, exercise, and patient education. Physical Therapy 2007b;87(1):9‐23. [DOI] [PubMed] [Google Scholar]
Cleland 2008
- Cleland JA, Childs JD, Whitman JM. Psychometric properties of the Neck Disability Index and Numeric Pain Rating Scale in patients with mechanical neck pain. Archives of Physical Medicine Rehabilitation 2008;89:69‐74. [DOI] [PubMed] [Google Scholar]
Cohen 1988
- Cohen J. Statistical Power Analysis for the Behavioural Sciences. Second Edition. Hilldale, NJ: Lawrence Erlbaum Associates, 1988. [Google Scholar]
Côté 2008
- Côté P, Kristman V, Vidmar M, Eerd D, Hogg‐Johnson S, Beaton D, et al. The prevalence and incidence of work absenteeism involving neck pain: a cohort of Ontario lost‐time claimants. Spine 2008;33(4 Suppl):S192‐8. [DOI] [PubMed] [Google Scholar]
Côté, 2008
- Côté P, Carroll LJ, Carragee EJ, Nordin M, Guzman J. The burden and determinants of neck pain in workers: results of the Bone and Joint Decade 2000‐2010 Task Force on Neck Pain and Its Associated Disorders. Spine 2008;33(4S):S60‐74. [DOI] [PubMed] [Google Scholar]
D'Sylva 2010
- D'Sylva J, Miller J, Gross AR, Burnie SJ, Goldsmith CH, Graham N, et al. Manual therapy with or without physical medicine modalities for neck pain: a systematic review. Manual Therapy 2010;15:415‐33. [DOI] [PubMed] [Google Scholar]
Davis 2012
- Davis MA, Onega T, Weeks WB, Lurie JD. Where the United States spends its spine dollars expenditures on different ambulatory services for the management of back and neck conditions. Spine 2012;37(19):1693‐701. [DOI] [PMC free article] [PubMed] [Google Scholar]
Farrar 2001
- Farrar JT, Young JP Jr, LaMoureaux L, Worth JL, Poole RM. Clinical importance of changes in chronic pain intensity measured on an 11‐point numerical rating scale. Pain 2001;94:149‐58. [DOI] [PubMed] [Google Scholar]
Felson 1995
- Felson DT, Anderson JJ, Boers M, Bombardier C, Furst D, Goldsmith C, et al. American College of Rheumatology: Preliminary definition of improvement in rheumatoid arthritis. Arthritis and Rheumatism 1995;38(6):727‐35. [DOI] [PubMed] [Google Scholar]
Finch 2002
- Finch E, Brooks D, Stratford P, Mayo N. Physical rehabilitation outcome measures: A guide to enhanced. Physical Rehabilitation Outcome Measures: A Guide to Enhanced Clinical Decision Making. Second Edition. Baltimore, MD: Lippincott Williams and Wilkins, 2002. [Google Scholar]
Fritz 2011
- Fritz JM, Koppenhaver SL, Kawchuk GN, Teyhen DS, Hebert JJ, Child JD. Preliminary investigation of the mechanisms underlying the effects of manipulation: exploration of a multivariate model Including spinal stiffness, multifidus recruitment, and clinical findings. Spine 2011;36(21):1772‐81. [DOI] [PMC free article] [PubMed] [Google Scholar]
Furlan 2009
- Furlan AD, Pennick V, Bombardier C, Tulder M, Editorial Board, Cochrane Back Review Group. 2009 updated method guidelines for systematic reviews in the Cochrane Back Review Group. Spine 2009;34(18):1929‐41. [DOI] [PubMed] [Google Scholar]
Furlan 2012
- Furlan AD, Yazdi F, Tsertsvaze A, Gross A, Tulder M, Santaguida L, et al. A systematic review and meta‐analysis of efficacy, cost‐effectiveness, and safety of selected complementary and alternative medicine for neck and low‐back pain. Evidence‐based Complementary and Alternative Medicine 2012;2012:953139. [DOI: 10.1155/2012/953139] [DOI] [PMC free article] [PubMed] [Google Scholar]
Goldsmith 1993
- Goldsmith CH, Boers M, Bombardier C, Tugwell P. Criteria for clinically important changes in outcomes. Development, scoring and evaluation of rheumatoid arthritis patients and trial profiles. Journal of Rheumatology 1993;20(3):561‐5. [PubMed] [Google Scholar]
Graham 2012
- Graham N, Haines T, Goldsmith CH, Gross AR, Burnie SJ, Shahzadu U, et al. Reliability of three assessment tools used to evaluate randomized controlled trials for treatment of neck pain. Spine 2012;37(6):515‐22. [DOI] [PubMed] [Google Scholar]
Grieve 1988
- Grieve GP. Common Vertebral Joint Problems. 2nd Edition. London: Churchill Livingstone, 1988. [Google Scholar]
Gross 2002b
- Gross AR, Kay T, Kennedy C, Gasner D, Hurley L, Yardley K, et al. Clinical practice guideline on the use of manipulation or mobilization in the treatment of adults with mechanical neck disorder. Manual Therapy 2002;7(4):193‐205. [DOI] [PubMed] [Google Scholar]
Guyatt 2010
- Guyatt G, Oxman A, Aklm E, Kunzd R, Vistc G, Brozeka J, et al. GRADE guidelines 1. Introduction to GRADE evidence profiles and summary of findings tables. Journal of Clinical Epidemiology 2010 Dec 31 [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
Guzman 2008
- Guzman J, Hurwitz EL, Carroll LJ, Haldeman S, Côté P, Carragee EJ, et al. A new conceptual model of neck pain: linking onset, course, and care: the Bone and Joint Decade 2000‐2010 Task Force on Neck Pain and Its Associated Disorders. Spine 2008;33(4S):S14‐23. [DOI] [PubMed] [Google Scholar]
Haavik 2012
- Haavik H, Murphy B. The role of spinal manipulation in addressing disordered sensorimotor integration and altered motor control. Journal of Electromyography and Kinesiology 2012;22(5):768‐76. [DOI] [PubMed] [Google Scholar]
Haldeman 2008
- Haldeman S, Schubert S. The Bone and Joint Decade 2000‐2010 Task Force on Neck Pain and Its Associated Disorders. Spine 2008;33(4S):S5‐7. [DOI] [PubMed] [Google Scholar]
Haynes 2012
- Haynes MJ, Vincent K, Bremner AP, Lanlo O, Hankey GJ. Assessing the risk of stroke from neck manipulation: a systematic review. International Journal of Clinical Practice 2012;66(10):940‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions. Version 5.1.0 [updated March 2011]. www.cochrane‐handbook.org. The Cochrane Collaboration., 2011.
Hogg‐Johnson 2008
- Hogg‐Johnson S, Velde G, Carroll LJ, Holm LW, Cassidy JD, Guzman J, et al. The burden and determinants of neck pain in the general population: results of the Bone and Joint Decade 2000‐2010 Task Force on Neck Pain and Its Associated Disorders. Spine 2008;33(4S):S39‐51. [DOI] [PubMed] [Google Scholar]
Huisman 2013
- Huisman PA, Speksnijder CM, Wijer A. The effect of thoracic spine manipulation on pain and disability in patients with non‐specific neck pain: a systematic review. Disability and Rehabilitation January 2013;Early Online:1‐9. [DOI] [PubMed] [Google Scholar]
Hurwitz 2008
- Hurwitz EL, Carragee JEJ, Velde G, Carroll LJ, Nordin M, Guzman J, et al. Treatment of neck pain: noninvasive interventions: results of the Bone and Joint Decade 2000‐2010 Task Force on Neck Pain and Its Associated Disorders. Spine 2008;33(4S):S123‐52. [DOI] [PubMed] [Google Scholar]
Jennum 2013
- Jennum P, Kjellberg J, Ibsen R, Bendix T. Health, social, and economic consequences of neck injuries: a controlled national study evaluating societal effects on patients and their partners. Spine 2013;38:449‐57. [DOI] [PubMed] [Google Scholar]
Jovey 2002
- Jovey RD. General principles of pain management. In: Jovey RD editor(s). Managing Pain. 1st Edition. Toronto: Healthcare and Financial Publishing, Rogers Media, 2002:15‐20. [Google Scholar]
Karason 2003
- Karason AB, Drysdale IP. Somatovisceral response following osteopathic HVLAT: a pilot study on the effect of unilateral lumbosacral high‐velocity low‐amplitude thrust technique on the cutaneous blood flow in the lower limb. Journal of Manipulative and Physiological Therapeutics 2003;26:220‐5. [DOI] [PubMed] [Google Scholar]
Kendal 1963
- Kendal MG, Stuart A. The Advanced Theory of Statistics. Second Edition. Vol. 1, New York: Hofner Publishing Co., 1963. [Google Scholar]
Lee 2001
- Lee CE, Simmonds MJ, Novy DM, Jones S. Self‐reports and clinician‐measured physical function among patients with low back pain: a comparison. Archives of Physical Medicine and Rehabilitation 2001;82:227‐31. [DOI] [PubMed] [Google Scholar]
Lin 2012
- Lin JH, Chiu TTW, Hu J. Chinese manipulation for mechanical neck pain: a systematic review. Clinical Rehabilitation 2012;26(11):963‐73. [DOI] [PubMed] [Google Scholar]
Linton 1998
- Linton SJ, Hellsing AL, Hallden K. A population‐based study of spinal pain among 35‐45 year old individuals. Prevalence, sick leave and health care use. Spine 1998;23(13):1457‐63. [DOI] [PubMed] [Google Scholar]
Little 1987
- Little RJA, Rubin DB. Statistical Analysis With Missing Data. Toronto: J. Wiley & Sons Inc., 1987. [Google Scholar]
MacDermid 2009
- MarDermid JC, Walton DM, Avery S, Blanchard A, Etruw E, McAlpine C, et al. Measurement properties of the neck disability index: a systematic review. Journal of Orthopaedic and Sports Physical Therapy 2009;39(5):400‐17. [DOI] [PubMed] [Google Scholar]
Martinez‐Segura 2006
- Martinez‐Segura R, Fernandez‐de‐las‐Penas C, Ruiz‐Saez M, Lopez‐Jimenez C, Rodriguez‐Blanco C. Immediate effects of neck pain and active range of motion after a single cervical high‐velocity low‐amplitude manipulation in subjects presenting with mechanical neck pain: a randomized controlled trial. Journal of Manipulative Physiological Therapeutics 2006;29:511‐7. [DOI] [PubMed] [Google Scholar]
Millan 2012
- Millan M, Leboeuf YC, Budgell B, Descarreaux M, Amorim MA. The effect of spinal manipulative therapy on spinal range of motion: a systematic literature review. Chiropractic & Manual Therapies 2012;20(1):23. [DOI] [PMC free article] [PubMed] [Google Scholar]
Miller 2010
- Miller J, Gross AR, D'Sylva J, Burnie SJ, Goldsmith CH, Graham N, et al. Manual therapy and exercise for neck pain: a systematic review. Manual Therapy 2010;15(4):334‐54. [PubMed] [Google Scholar]
Olesen 1988
- Olesen J. Classification and diagnostic criteria for headache disorders, cranial neuralgias and facial pain. Cephalgia 1988;8(7):61‐2. [PubMed] [Google Scholar]
Olesen 1997
- Olesen J, Gobel H. ICD‐10 Guide for Headaches. Guide to the classification, diagnosis and assessment of headaches in accordance with the Tenth Revision of the International Classification of Diseases and Related Health Problems and its application to neurology. Cephalalgia 1997;17(Suppl 19):29‐30. [Google Scholar]
Paanalahti 2014
- Paanalahti K, Holm LW, Nordin M, Asker M, Lyander J, Skillgate E. Adverse events after manual therapy among patients seeking care for neck and/or back pain: a randomized controlled trial. BMC Musculoskeletal Disorders 2014;15:77. [DOI] [PMC free article] [PubMed] [Google Scholar]
Perry 2008
- Perry J, Green A. An investigation into the effects of a unilaterally applied lumbar mobilization technique on peripheral sympathetic nervous system activity in the lower limbs. Manual Therapy 2008;13:492‐9. [DOI] [PubMed] [Google Scholar]
Pickar 2002
- Pickar JG. Neurophysiological effects of spinal manipulation. Spine Journal 2002;2:357‐71. [DOI] [PubMed] [Google Scholar]
Posadzki 2011
- Posadzki P, Ernst E. Osteopathy for musculoskeletal patients: a systematic review of randomized controlled trials. Clinical Rheumatology 2011;30:285‐91. [DOI] [PubMed] [Google Scholar]
Puentedura 2012
- Puentedura EJ, Cleland JA, Landers MR, Mintken P, Louw A, Fernandez‐de‐las‐Penas C. Development of a clinical prediction rule to identify patients with neck pain likely to benefit from thrust joint manipulation to the cervical spine. Journal of Orthopaedic and Sports Physical Therapy 2012;42(7):577‐92. [DOI] [PubMed] [Google Scholar]
Racicki 2013
- Racicki S, Gerwin S, CiClaudio S, Reinmann S, Donaldson M. Conservative physiotherapy management for the treatment of cervicogenic headache: a systematic review. Journal of Manual & Manipulative Therapy 2013;21(2):113‐24. [DOI] [PMC free article] [PubMed] [Google Scholar]
RevMan 2014 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan). Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Rodine 2012
- Rodine RJ, Vernon H. Cervical radiculopathy: a systematic review on treatment by spinal manipulation and measurement with the Neck Disability Index. Journal of Canadian Chiropractic Association 2012;56(1):18‐28. [PMC free article] [PubMed] [Google Scholar]
Rushton 2012
Schmid 2008
- Schmid A, Brunner F, Wright A, Bachmann L. Paradigm shift in manual therapy? Evidence for a central nervous system component in the response to passive cervical joint mobilisation. Manual Therapy 2008;13(5):387‐96. [DOI] [PubMed] [Google Scholar]
Scholten Peeters 2013
- Scholten‐Peeters GGM, Thoomes E, Konings S, Beijer M, Verkerk K, Koes BW, et al. Is manipulative therapy more effective than sham manipulation in adults? A systematic review and meta‐analysis. Chiropractic and Manual Therapies 2013;21(34):1‐19. [DOI] [PMC free article] [PubMed] [Google Scholar]
Schumacher 1993
- Schumacher HR, Klippel JH, Koopman WJ (eds). Primer on the Rheumatic Diseases. Tenth. Atlanta: Arthritis Foundation, 1993. [Google Scholar]
Shaw 2010
- Shaw L, Descarreau M, Bryans R, Duranleau M, Marcoux H, Potter B, et al. A systematic review of chiropractic management of adults with whiplash‐associated disorders: recommendations for advancing evidence‐based practice and research. Work ‐ Journal of Prevention Assessment and Rehabilitation 2010;35(3):369‐94. [DOI] [PubMed] [Google Scholar]
Sjaastad 1990
- Sjaastad O, Fredriksen TA, Pfaffenrath V. Cervicogenic headache: diagnostic criteria. Headache 1990;30:725‐6. [DOI] [PubMed] [Google Scholar]
Souvlis 2004
- Souvlis T, Vicenzino B, Wright A. Neurophysiological effects of spinal manual therapy. In: Boyling JD, Jull GA editor(s). Grieve's Modern Manual Therapy, The Vertebral Column. 3rd Edition. Edinburgh: Churchill Livingstone, 2004:367‐80. [ISBN 0443 071551] [Google Scholar]
Spitzer 1987
- Spitzer WO, Leblanc FE, Dupuis M. Scientific approach to the assessment and management of activity related spinal disorders. Spine 1987;7:S1‐59. [PubMed] [Google Scholar]
Spitzer 1995
- Spitzer WO, Skovron ML, Salmi LR, Cassidy JD, Duranceau J, Suissa S, et al. Scientific monograph of the Quebec Task Force on Whiplash‐Associated Disorders: redefining "whiplash" and its management. Spine 1995;20:S1‐73. [PubMed] [Google Scholar]
Stratford 1999
- Stratford PW, Riddle DL, Binkley JM, Spadoni G, Westaway MD, Padfield B. Using the Neck Disability Index to make decisions concerning individual patients. Physiotherapy Canada 1999;Spring:107‐19. [Google Scholar]
Teasell 2010
- Teasell RW, McClure JA, Walton D, Pretty J, Salter K, Meyer M, et al. A research synthesis of therapeutic interventions for whiplash‐associated disorders (WAD): Part 3 – interventions for subacute WAD. Pain Research & Management 2010;15(5):305‐12. [DOI] [PMC free article] [PubMed] [Google Scholar]
Thoomes 2013
- Thoomes EJ, Scholten‐Peeters W, Koes B, Falla D, Verhagen AP. The effectiveness of conservative treatment for patients with cervical radiculopathy. Clinical Journal of Pain 2013;29(12):1073‐86. [DOI] [PubMed] [Google Scholar]
van Tulder 2003
- Tulder MW, Furlan A, Bombardier C, Bouter L, Editorial Board of the Cochrane Collaboration Back Review Group. Updated Method Guidelines for systematic reviews in the Cochrane Collaboration Back Review Group. Spine 2003;28(12):1290‐9. [DOI] [PubMed] [Google Scholar]
Verbeek 2012
- Verbeek J, Ruotsalainen J, Hoving JL. Synthesizing study results in a systematic review. Scandinavian Journal of Work, Environment & Health 2012;38(3):282‐90. [DOI] [PubMed] [Google Scholar]
Vincent 2013
- Vincent K, Maigne JY, Fischhoff C, Lanlo O, Dagenais S. Systematic review of manual therapies for nonspecific neck pain. Joint, Bone, Spine 2013;80:508‐15. [DOI] [PubMed] [Google Scholar]
Vincenzino 1996
- Vincenzino B, Collins D, Wright A. The initial effects of a cervical spine manipulative physiotherapy treatment on the pain and dysfunction of lateral epicondylalgia. Pain 1996;68:69‐74. [DOI] [PubMed] [Google Scholar]
Walser 2009
- Walser RF, Meserve BB, Boucher TR. The effectiveness of thoracic spine manipulation for the management of musculoskeletal conditions: a systematic review and meta‐analysis of randomized clinical trials. Journal of Manual and Manipulative Therapy 2009;17(4):237‐46. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to other published versions of this review
Gross 1996
- Gross AR, Aker PD, Goldsmith CH, Peloso P. Conservative management of neck disorders. A systematic overview and meta‐analysis. Online Journal of Current Clinical Trials 1996:Doc No. 200‐201. [PubMed] [Google Scholar]
Gross 2002a
- Gross AR, Kay T, Hondras M, Goldsmith C, Haines T, Peloso P, et al. Manual therapy for mechanical neck disorders: a systematic review. Manual Therapy 2002a;7(3):131‐49. [DOI] [PubMed] [Google Scholar]
Gross 2004a
- Gross AR, Bronfort G, Hoving J, Goldsmith CH, Haines T, Aker P, et al. Manipulation and mobilisation for mechanical neck disorders. Cochrane Database of Systematic Reviews 2004, Issue 1. [DOI: 10.1002/14651858.CD004249.pub2] [DOI] [PubMed] [Google Scholar]
Gross 2004b
- Gross AR, Hoving JL, Haines TA, Goldsmith CH, Kay T, Aker P, et al. Cervical Overview Group. A Cochrane review of manipulation and mobilization for mechanical neck disorders. Spine 2004;29(14):1541‐8. [DOI] [PubMed] [Google Scholar]
Gross 2007
- Gross AR, Goldsmith CH, Hoving JL, Haines T, Peloso P, Aker P, et al. Conservative management of mechanical neck disorders: a systematic review. Journal of Rheumatology 2007;34(5):183‐202. [PubMed] [Google Scholar]
Gross 2010
- Gross AR, Miller J, D'Sylva J, Burnie SJ, Goldsmith CH, Graham N, et al. Manipulation or mobilisation for neck pain. Cochrane Database of Systematic Reviews 2010, Issue 1. [DOI: 10.1002/14651858.CD004249.pub3] [DOI] [PubMed] [Google Scholar]


