Abstract
Context: Although functional-performance tests are dynamic measures used to assess general lower body function, studies investigating these tests for ankle instability have yielded conflicting results.
Objective: To determine if a relationship exists between a measure of functional ankle instability and deficits in functional performance.
Design: A case-control study correlating subject performance on a set of lower extremity functional-performance tests with a measure of ankle instability.
Setting: University athletic training research laboratory.
Patients or Other Participants: We recruited 60 participants (43 females, 17 males, age = 22.4 ± 4.9 years, height = 169.9 ± 9.7 cm, mass = 72.6 ± 16.3 kg; 42 injured, 18 uninjured) to participate in the study. Six questions were used to determine if functional ankle instability was present in each participant. A point was added for each yes response to produce an index that represents a continuous variable of functional ankle instability.
Main Outcome Measure(s): Four unilateral hopping tests were used in this study: figure-of-8 hop, side hop, up-down hop, and single hop. For the first 3 tests, the total time was recorded with a handheld stopwatch to the nearest 0.01 second; for the single hop-for-distance test, the distance was recorded to the nearest 0.01 m. Correlations were computed with the functional ankle instability index and each of the 4 functional-performance tests.
Results: No relationship was revealed between the functional ankle instability index and single hop for distance or up-down hop, with r values of −.008 and .245, respectively. A significant relationship was found between the functional ankle instability index and the side hop (r = .35, P ≤ .01) and the figure-of-8 hop (r = .31, P ≤ .02).
Conclusions: A positive relationship existed between functional ankle instability and performance deficits on the side hop and figure-of-8 hop. Conversely, a relationship did not exist between functional ankle instability and frontal-plane functional-performance activities.
Keywords: side hop, figure-of-8 hop
Functional-performance tests are dynamic measures used to assess general lower body function. These tests are helpful because they combine multiple components, such as muscular strength, neuromuscular coordination, and joint stability, which could be affected after joint injury. Clinically, functional-performance tests are often used during the latter stages of rehabilitation and as criteria to determine return-to-participation status. More recently, the ability to detect functional-performance deficits in participants with knee1–3 or ankle4–7 joint injuries has been investigated.
In subjects with anterior cruciate ligament-deficient knees, the ability to detect dynamic impairments through functional-performance testing has varied. Functional tests that have been studied include the shuttle run,1,3 single hop for distance,1 timed hop,1 cocontraction semicircular maneuver,3 carioca maneuver,3 up-down hop,2 and figure-of-8 hop.1,2 The ability to detect these dynamic impairments in subjects with anterior cruciate ligament-deficient knees has changed depending on the test used and the number of tests included. Using 4 functional tests (figure-of-8 hop, side hop, up-down hop, and single hop for distance), Itoh et al2 found that deficits in at least one of the 4 tests appropriately classified 82% of anterior cruciate ligament-deficient knees.
Studies investigating ankle joint injuries have yielded conflicting results. When the single hop for distance,6 6-m hop for time,6 30-m agility hop,6 triple crossover hop for distance,4 shuttle run,4,7 cocontraction,7 or agility hop test7 were used, performance deficits were not found in participants with ankle instability. However, participants with a history of ankle injury performed significantly worse on a single-limb hopping course than their uninjured counterparts.5
Because of these conflicting results, we chose a myriad of tests that included both frontal- and sagittal-plane movement and separate tests for time or distance (or both). Therefore, our purpose was to determine if a relationship existed between a measure of functional ankle instability (FAI) and deficits in functional performance.
METHODS
Subjects
Sixty healthy college students (17 males, 43 females) from a large National Collegiate Athletic Association Division I institution participated in this study. Forty-two participants (age = 23.0 ± 5.5 years, height = 171.5 ± 8.8 cm, mass = 75.9 ± 16.6 kg) had various degrees of unilateral FAI, and 18 (age = 20.9 ± 2.3 years, height = 166.8 ± 11.1 cm, mass = 64.4 ± 12.8 kg) had no history of ankle injuries. Subjects were excluded from either group if they had a history of fractures or surgeries to the lower extremity. Functional ankle instability has been defined as a tendency for the foot to give way8 or a disabling loss of reliable static and dynamic support of a joint.9 We asked 6 dichotomous questions to determine the presence of FAI in each participant. These questions centered on the subjects' self-reported feeling of instability and consisted of (1) Have you ever sprained your ankle? (2) Does your ankle ever feel unstable while walking on a flat surface? (3) Does your ankle ever feel unstable while walking on uneven ground? (4) Does your ankle ever feel unstable during recreational or sport activity? (5) Does your ankle ever feel unstable while going up stairs? (6) Does your ankle ever feel unstable while going down stairs? A point was added for each yes response to provide a continuous variable of FAI. For example, uninjured participants answered no to all the questions and, thus, scored a 0 on the index. The use of a continuous variable to report the presence of FAI allowed us to portray the complexity and different severities of this condition. Day-to-day reliability of these items ranged from .86 (SEM = .184) to .70 (SEM = .368).10 With this index, we reproduced the inclusion criteria used in other studies by ensuring that all FAI subjects had both a history of previous ankle sprains and a feeling of instability in the ankle.11–15 Therefore, all FAI participants scored between a 2 and 6 on the index. The assumption was made that a feeling of instability during a greater number of these activities (walking on a flat surface, uneven surface, etc) potentially equated to more frequent instability and potentially a greater degree of FAI. An effort was also made to include a heterogeneous sample with relatively equal representation throughout the range of the index (18 subjects scored 0, 7 scored 2, 14 scored 3, 11 scored 4, 8 scored 5, and 2 scored 6). All participants were asymptomatic and active at the time of the study. Participants were excluded if they had a history of lower extremity fracture or surgery. The University's Human Investigation Committee approved the study, and all subjects read and signed a written informed consent form before the study.
Test Procedures
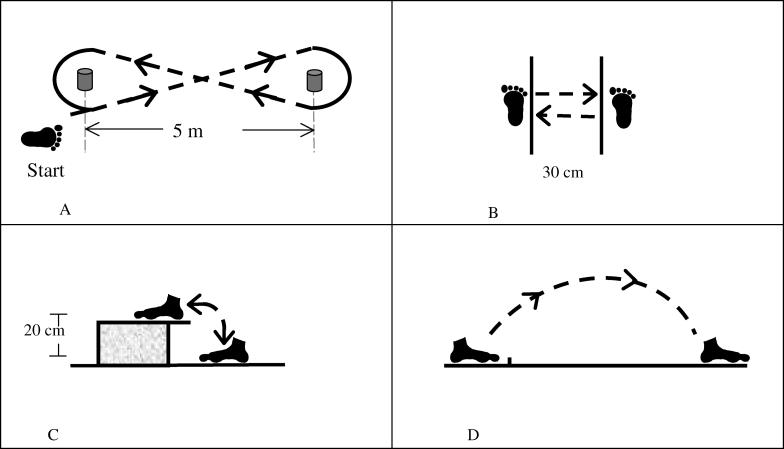
This project was done as part of a larger study assessing the proprioceptive changes in participants with ankle instability. Each participant came to the sports medicine research laboratory for all testing procedures. Four unilateral hopping tests were performed: figure-of-8 hop, side hop, up-down hop, and single hop. The functionally unstable ankle of the injured participants and a randomly selected ankle in the uninjured participants were identified as the test limbs before testing. The same percentages of right (approximately 60%) and left (approximately 40%) ankles were used in both the injured and uninjured participants. Testing procedures were similar to those in a previously published functional-performance study.2 All testing was performed with subjects barefoot. The figure-of-8 hop test was done on a 5-m course outlined by cones. Participants were instructed to hop as quickly as possible twice through the course (Figure). For the side-hop test, participants were instructed to hop laterally 30 cm and back for a total of 10 repetitions (see Figure). For the up-down hop test, a 20-cm step was used. Participants were instructed to hop vertically up and down on the step for a total of 10 repetitions (see Figure). For each test, the total time was recorded with a handheld stopwatch to the nearest 0.01 second. For the single-hop test, participants were instructed to hop forward as far as possible. The distance was recorded from the position of the toes on the starting line to the end of the jump to the nearest 0.01 m (see Figure). If the subject fell or was unable to maintain balance during the test period, the trial was discarded and repeated. Of the 60 subjects, 10 (6%) had at least 1 unacceptable trial. The unacceptable trials were typically due to the loss of balance during the up-down or side hop. Test order was counterbalanced among participants, and each test was conducted twice, with the best time or distance used for the analysis. A 30-second rest occurred between trials, with at least 1 minute of rest between tests. After each functional-performance test, the participant was asked, “Did you feel unstable during that activity?” The total number of times he or she answered yes to this question was also calculated.
A, Figure-of-8 hop test.
B, Side-hop test. C, Up-down hop test. D, Single-hop test
Statistical Analysis
All data were imported into a statistical program. Using a continuous variable of FAI, we were able to evaluate the instability throughout the range of FAI versus grouping all FAI participants together, regardless of instability severity. Therefore, Pearson product moment correlations were calculated to determine the relationship between the FAI index and performance on each functional test. A correlation was also computed between the FAI index and subject responses to “Did you feel unstable during that activity?” Alpha for all analyses was set at P < .05.
RESULTS
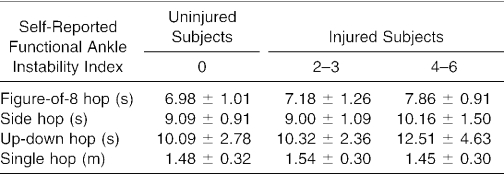
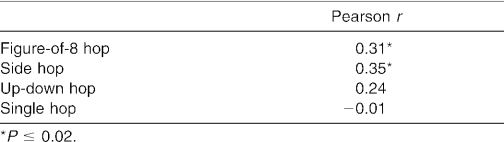
Means and standard deviations for the functional-performance tests are shown in Table 1, and the Pearson r correlations for each test are shown in Table 2. Pearson r correlations revealed a significant positive relationship between the FAI index and the side hop (r = .35, df = 59, P < .01) and FAI index and the figure-of-8 hop (r = .31, df = 59, P < .02). No significant relationship was revealed for the single hop for distance or the up-down hop. A significant positive correlation was also noted between the FAI index and the total yes responses to feeling unstable during the functional-performance testing (r = .43, df = 59, P < .01).
Table 1. Results (Mean ± SD) for Each Functional-Performance Test (n = 60).
Table 2. Correlations Between Ankle Instability and Functional-Performance Tests.
DISCUSSION
Our data suggest that those participants who scored higher on the FAI index had greater performance deficits on the figure-of-8 hop and side hop. Although these correlations by athletic training conventions may be considered weak, we believe they represent clinically significant relationships for at least 3 reasons. First, most correlation coefficients generated in athletic training research are calculated as part of reliability studies. These studies are conducted under very controlled conditions for the express purpose of minimizing extraneous variance and maximizing measurement stability. Our study was nonexperimental in design and used an existing clinical population. Under these conditions, it is not reasonable to expect correlations typically considered moderate to high. Second, we believe that a multifactor model, yet to be determined, will best describe FAI. Previous researchers have shown that other proprioceptive measures and constructs (eg, balance) are related to FAI.5,16–19 Based on these findings, we suspect that these functional-performance tests are detecting important but select aspects of FAI, thus accounting for a limited portion of the variance. Finally, in terms of effect size, our correlations are comparable with mean differences found in the functional-performance test literature. It is possible to equate our correlations to mean differences using effect sizes.20 For example, in terms of effect size, our correlations are considered to be moderate. By converting the Cohen effect size r to the effect size d for mean comparisons, d = .50 for our correlations. This is interpreted as a difference between means equal to one half of a standard deviation.21 Other researchers22 using similar functional-performance tests have reported significant mean differences with effect sizes of d = .25, less than half of our effect size. Therefore, we believe that our findings are well within the established limits of meaningful effect sizes.
We believe that the figure-of-8 hop and side hop produced deficits because they forced the participants to move laterally, placing stress on the structures on the lateral aspect of the leg, including the lateral ligaments and peroneus muscle complex. Additionally, the figure-of-8 test seems to force a rotational stress on the ankle and lower leg. Conversely, the up-down hop and single-hop tests, which did not reveal a relationship with the FAI index, are done primarily in the sagittal plane. Clinically, a typical mechanism of injury for an ankle sprain is lateral movement causing hypersupination of the ankle.23 Thus, these findings suggest that functional tests that place lateral or rotational stress on the ankle reveal performance deficits in participants with FAI.
These findings conflict with other functional-performance investigations done on the ankle.4,6,7 Although we studied a heterogeneous sample that ranged from participants with no ankle injuries to participants with various amounts of instability, earlier investigators4,6 performed a different comparison by using the contralateral, uninjured limb of the FAI subject as the normal comparison for functional-performance testing. With this contralateral comparison, it is not surprising that no significant difference was identified. Researchers looking at postural-stability differences between unstable ankles and contralateral normal ankles have also failed to note differences. For example, Tropp11 found no difference in postural stability between the injured and the contralateral uninjured limbs; however, both limbs had significantly higher stabilometric values compared with subjects who had never sustained an ankle injury to either limb. He suggested that the increase in postural stability bilaterally may represent a preexisting condition or a central organizational change due to pain and immobilization.11 Therefore, as in our current study, utilizing different subjects for the injured and uninjured groups may be a better model to determine if functional deficits exist.
Additionally, investigators who failed to find functional-performance deficits in participants with FAI used tests that stressed the quadriceps and hamstrings instead of the lower leg musculature.4,7 These authors borrowed methods from studies that evaluated functional deficits in participants with knee injuries.1,3,24–26 Tests such as the shuttle run and cocontraction, which did not produce differences in ankle studies,4,7 were successfully used in studies of subjects with anterior cruciate ligament deficiency,1,3 indicating that these tests tax knee stability but not ankle stability.
In support of our findings, Jerosch and Bischof5 found that, when rotational stress was placed on the structures around the ankle, participants with a history of ankle instability had performance deficits. They used a slanted hopping course that combined frontal and rotational stress on an uneven surface. The surface was slanted up, down, and laterally at several points in the course. Performance on the course was evaluated by the amount of time it took for them to complete the task, and penalty seconds were added if they deviated from the course.
In contrast, the lack of relationship between either the up-down hop or the single hop and the FAI index was probably due to the nature of the functional tests. These tests are performed in the sagittal plane and place little stress on the lateral structures of the ankle. Worrell et al6 were also unsuccessful in finding significant differences at the ankle when using sagittal-plane activities. In that investigation, participants performed the single hop for distance and the single-leg 6-m hop for time.6 Clinically, this is similar to a patient being asymptomatic during straight-ahead running but complaining of instability during change-of-direction activities.
Additional research is necessary to evaluate muscular activity during a variety of functional-performance tests. Electromyographic analysis could confirm which functional-performance tests are best at stressing specific muscles, thereby focusing ankle instability investigators on tests that specifically tax the lower leg muscles. Further research is necessary on other functional-performance tests that incorporate both lateral and rotational movement. Functional-performance tests that could be considered include the lower extremity functional test, spiral-staircase run, 30-m single-leg agility hop, triple crossover hop for distance, multiple single-leg hop-stabilization test, and functional hop test.
Perceived Deficits
Previous researchers4,7 have reported that a perceived deficit may exist in subjects with FAI even though actual performance was not affected. However, because these authors did not ask the subjects if they felt unstable during the functional-performance tasks, a perceived deficit could only be considered as a possible explanation. Therefore, in our study, after every functional test, we asked the participants if they felt unstable during the activity. We found a significant correlation between FAI index and the total number of yes responses after each functional-performance test. We found that 76% of the FAI subjects (32 of 42) reported that they felt unstable in at least 1 of the functional performance tasks. We further categorized the subjects according to the functional-performance test on which each subject felt unstable. A total of 33% (14 of 42 FAI subjects) reported instability in the figure-of-8 hop, 60% (25 of 42 FAI subjects) in the up-down hop, 60% (25 of 42 FAI subjects) in the side hop, and 14% (6 of 42 FAI subjects) in the single hop. Because we found a performance deficit only on the side hop and the figure-of-8 hop, the large number of yes responses on the up-down hop was an unexpected finding. This test should be further evaluated to identify why a perceived deficit may be present without an actual performance deficit.
CONCLUSIONS
A positive relationship existed between the FAI index and performance deficits in the figure-of-8 hop and side hop. Participants with FAI, as we defined it, performed worse on these 2 functional tasks that potentially place greater stress on the lateral structures. Conversely, no relationship existed during sagittal-plane activities. Continued research is necessary to determine if other functional-performance tests yield the same results and if these tests can be used to predict participants who may be predisposed to ankle instability. Finally, because ankle instability is a difficult phenomenon to assess, deficits in performing these tests could also be incorporated into the evaluation of injuries. Additional research needs to be conducted on a large number of normal subjects to identify normative values on these functional-performance tests. This would also allow us to demonstrate the diagnostic capability of these tests in determining FAI.
REFERENCES
- Barber SD, Noyes FR, Mangine RE, McCloskey JW, Hartman W. Quantitative assessment of functional limitations in normal and anterior cruciate ligament-deficient knees. Clin Orthop. 1990;255:204–214. [PubMed] [Google Scholar]
- Itoh H, Kurosaka M, Yoshiya S, Ichihashi N, Mizuno K. Evaluation of functional deficits determined by four different hop tests in patients with anterior cruciate ligament deficiency. Knee Surg Sports Traumatol Arthrosc. 1998;6:241–245. doi: 10.1007/s001670050106. [DOI] [PubMed] [Google Scholar]
- Lephart SM, Perrin DH, Fu FH, Gieck JH, McCue FC, Irrgang JJ. Relationship between selected physical characteristics and functional capacities in the anterior cruciate ligament-insufficient athlete. J Orthop Sports Phys Ther. 1992;16:174–181. doi: 10.2519/jospt.1992.16.4.174. [DOI] [PubMed] [Google Scholar]
- Munn J, Beard D, Refshauge K, Lee RJ. Do functional-performance tests detect impairment in subjects with ankle instability? J Sport Rehabil. 2002;11:40–50. [Google Scholar]
- Jerosch J, Bischof M. Proprioceptive capabilities of the ankle in stable and unstable joint. Sports Exerc Inj. 1996;2:167–171. [Google Scholar]
- Worrell T, Booher LD, Hench KM. Closed kinetic chain assessment following inversion ankle sprain. J Sport Rehabil. 1994;3:97–203. [Google Scholar]
- Demeritt KM, Shultz SJ, Docherty CL, Gansneder BM, Perrin DH. Chronic ankle instability does not affect lower extremity functional performance. J Athl Train. 2002;37:507–511. [PMC free article] [PubMed] [Google Scholar]
- Freeman MAR. Instability of the foot after injuries to the lateral ligament of the ankle. J Bone Joint Surg Br. 1965;47:669–677. [PubMed] [Google Scholar]
- Vaes PH, Duquet W, Casteleyn PP, Handelberg F, Opdecam P. Static and dynamic roentgenographic analysis of ankle stability in braced and nonbraced stable and functionally unstable ankles. Am J Sports Med. 1998;26:692–702. doi: 10.1177/03635465980260051601. [DOI] [PubMed] [Google Scholar]
- Docherty CL, Gansender BM, Arnold BL, Hurwitz S. Reliability and validity of an ankle instability instrument [abstract] J Athl Train. 2003;38:S-12. (suppl) [PMC free article] [PubMed] [Google Scholar]
- Tropp H. Pronator muscle weakness in functional instability of the ankle joint. Int J Sports Med. 1986;7:291–294. doi: 10.1055/s-2008-1025777. [DOI] [PubMed] [Google Scholar]
- Hartsell HD, Spaulding SJ. Eccentric/concentric ratios at selected velocities for the invertor and evertor muscles of the chronically unstable ankle. Br J Sports Med. 1999;33:255–258. doi: 10.1136/bjsm.33.4.255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gauffin H, Tropp H, Odenrick P. Effect of ankle disk training on postural control in patients with functional instability of the ankle joint. Int J Sports Med. 1988;9:141–144. doi: 10.1055/s-2007-1024996. [DOI] [PubMed] [Google Scholar]
- Wilkerson GB, Pinerola JJ, Caturano RW. Invertor vs. evertor peak torque and power deficiencies associated with lateral ankle ligament injury. J Orthop Sports Phys Ther. 1997;26:78–86. doi: 10.2519/jospt.1997.26.2.78. [DOI] [PubMed] [Google Scholar]
- Rozzi SL, Lephart SM, Sterner R, Kuligowski L. Balance training for persons with functionally unstable ankles. J Orthop Sports Phys Ther. 1999;29:478–486. doi: 10.2519/jospt.1999.29.8.478. [DOI] [PubMed] [Google Scholar]
- Konradsen L, Magnusson P. Increased inversion angle replication error in functional ankle instability. Knee Surg Sports Traumatol Arthrosc. 2000;8:246–251. doi: 10.1007/s001670000124. [DOI] [PubMed] [Google Scholar]
- Olmsted L, Carcia C, Hertel J, Shultz S. Efficacy of the Star Excursion Balance Tests in detecting reach deficits in subjects with chronic ankle instability. J Athl Train. 2002;37:501–506. [PMC free article] [PubMed] [Google Scholar]
- Lentell G, Baas B, Lopez D, McGuire L, Sarrels M, Snyder P. The contributions of proprioceptive deficits, muscle function, and anatomic laxity to functional instability of the ankle. J Orthop Sports Phys Ther. 1995;21:206–215. doi: 10.2519/jospt.1995.21.4.206. [DOI] [PubMed] [Google Scholar]
- Forkin DM, Koczur C, Battle R, Newton RA. Evaluation of kinesthetic deficits indicative of balance control in gymnasts with unilateral chronic ankle sprains. J Orthop Sports Phys Ther. 1996;23:245–250. doi: 10.2519/jospt.1996.23.4.245. [DOI] [PubMed] [Google Scholar]
- Cohen J. The significance of a product moment rs. In: Statistical Power Analysis for the Behavioral Sciences. 2nd ed. Hillsdale, NJ: Lawrence Erlbaum Assoc; 1988:75–107.
- Cohen J. The t test for means. In: Statistical Power Analysis for the Behavioral Sciences. 2nd ed. Hillsdale, NJ: Lawrence Erlbaum Assoc; 1988:19–74.
- Risberg MA, Ekeland A. Assessment of functional tests after anterior cruciate ligament surgery. J Orthop Sports Phys Ther. 1994;19:212–217. doi: 10.2519/jospt.1994.19.4.212. [DOI] [PubMed] [Google Scholar]
- Hertel J. Functional instability following lateral ankle sprain. Sports Med. 2000;29:361–371. doi: 10.2165/00007256-200029050-00005. [DOI] [PubMed] [Google Scholar]
- Noyes FR, Barber SD, Mangine RE. Abnormal lower limb symmetry determined by function hop tests after anterior cruciate ligament rupture. Am J Sports Med. 1991;19:513–518. doi: 10.1177/036354659101900518. [DOI] [PubMed] [Google Scholar]
- Lephart SM, Perrin D, Fu FH, Moberg E. Functional performance tests for the anterior cruciate ligament insufficient athlete. J Athl Train. 1991;26:44–50. [Google Scholar]
- Lephart SM, Kocher MS, Harner CD, Fu FH. Quadriceps strength and functional capacity after anterior cruciate ligament reconstruction: patellar tendon autograft versus allograft. Am J Sports Med. 1993;21:738–743. doi: 10.1177/036354659302100519. [DOI] [PubMed] [Google Scholar]