Abstract
A plasmacytoma is a cancerous growth of abnormal plasma cells that arise within osseous or soft tissue structures. In soft tissue structures, plasmacytomas can present as solitary or multiple masses in the absence of systemic involvement. Solitary plasmacytomas can be subcategorized as extramedullary plasmacytoma (derived from plasma cells located in soft tissues) or osseous plasmacytoma (derived from plasma cells located in the bone marrow). Infrequently, these tumors can arise as extramedullary lesions from the pancreas and present similarly to other tumors, such as pancreatic neuroendocrine tumors (PNETs). In this article, we report the case of a 62-year-old male with a diagnosis of solitary plasmacytoma of the pancreas. We focus on optimizing diagnosis and management through the application of radiological imaging modalities, specifically computed tomography (CT) scans and positron emission tomography-computed tomography (PET-CT) scans.
Keywords: Pancreatic plasmacytomas, Extramedullary plasmacytomas, Axial skeleton, Computed tomography, Ultrasound-guided fine-needle aspiration
Introduction
Solitary extramedullary plasmacytoma is an extremely rare plasma cell neoplasm involving organs external to the bone marrow, occurring in fewer than 5% of plasma cell tumors [1]. Even more rare is pancreatic involvement by plasma cell neoplasms, comprising less than 0.1% of all pancreatic masses [2]. Hefferman reported the first pancreatic plasmacytoma case in 1947 [3], and since then, fewer than 0.1% of all pancreatic tumors seen are primary pancreatic plasmacytomas, without associated multiple myeloma (MM) of the bone marrow [2]. Pancreatic plasmacytomas pose a unique radiological challenge, given their similarity to other pancreatic neoplasms such as pancreatic neuroendocrine tumors (PNETs), lymphomas, and adenocarcinomas [1]. Here, we report a rare case of a 62-year-old male who presented with abdominal pain, nausea, and vomiting that was eventually diagnosed as a solitary plasmacytoma of the pancreas.
Case presentation
A 62-year-old African American male with a past medical history of hypertension presented to the emergency department with nausea, vomiting, and abdominal pain. Upon physical examination, the patient's abdomen was soft and distended with epigastric tenderness to palpation. Initial complete blood count, urinalysis, and lipase levels were unremarkable. Subsequently, the patient underwent a CT scan of the abdomen and pelvis with IV contrast, which displayed a heterogeneous exophytic lobulated solid mass in the region of the pancreatic head/uncinate process measuring 7.7 × 7.2 × 6.5 cm with mild pancreatic ductal dilatation along with an adjacent eccentric nodal mass. Two days later, a pancreatic protocol CT scan with IV contrast revealed that the mass occluded the superior mesenteric vein (SMV) and involved the superior mesenteric artery (SMA) and main portal vein to less than 180 degrees (Figs. 1A–D). The mass was suggestive of a neuroendocrine tumor due to prominent vascularity. In addition, the mass extended downward and was inseparable from the duodenum. An adjacent peritoneal 1.5 cm nodule suggested nodal disease and isolated distended distal small bowel loops were present.
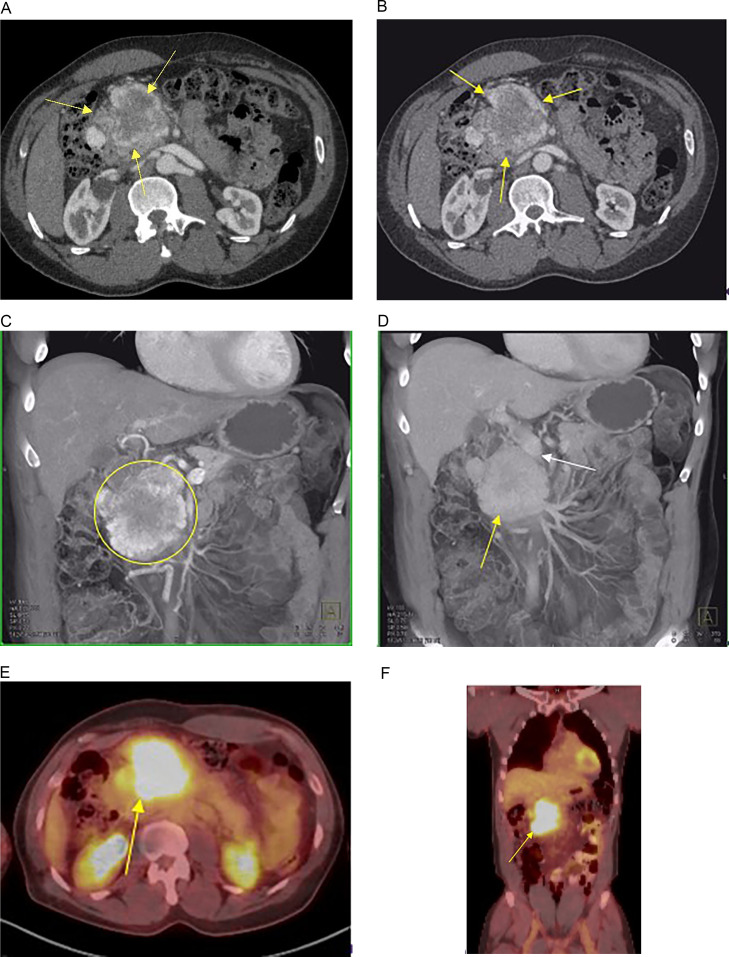
Fig. 1. A.
62-year-old male with a history of nausea, vomiting, and abdominal pain. CT scan of the abdomen and pelvis with IV contrast and PET/CT were done for evaluation and staging. (A and B) Axial CT scans demonstrate a 7.7 × 6.5 cm vascular mass in the head of the pancreas (yellow arrows). Several enhancing nodes are defined by the lateral tumor margin. (C and D) Volume rendering coronal views of the CT scan in arterial and venous phase imaging demonstrate the vascular mass in the head of the pancreas (yellow circle) (C), which washes out on the venous phase images (yellow arrow) (D). Involvement of the portal vein and SMV is noted (white arrow) (D). (E and F) PET/CT with axial and coronal merged display shows the avid uptake by the mass in the head of the pancreas (yellow arrows).
One week later, the patient underwent an endoscopic ultrasound-guided fine-needle aspiration (EUS-FNA) for biopsy of the mass. Pathology was consistent with a plasma cell neoplasm expressing kappa light chains and the BRAF V600E mutation. Sections of the biopsy showed sheets of atypical plasma cells with variations in size and occasionally conspicuous nucleoli. Immunostains exhibited atypical plasma cells positive for CD138 MUM-1 with aberrant expression of CD56. Kappa and lambda immunostains revealed a kappa light-chain-restricted population consistent with plasmacytoma, confirming the pancreatic plasmacytoma diagnosis.
Approximately three weeks later, to exclude systemic disease, a bone marrow biopsy, fluorine-18-fluorodeoxyglucose PET-CT scan (F-18 FDG PET-CT), and an M-spike quantitation were completed. The skeletal survey was negative for osseous lesions, and the PET-CT revealed a pancreatic mass consistent with pancreatic plasmacytoma as well as possible involvement in the mesentery and ascitic fluid (Figs. 1E and F). PET-CT findings included an intensely FDG-avid multilobulated mass centered in the head/uncinate process, consistent with biopsy-proven plasmacytoma, and an avid nodular opacity indistinct from the right posterior lateral contour of the mass. No evidence of FDG-avid osseous lesions above background activity was seen to suggest metabolically active MM. The M-spike quantitation showed a gamma M-spike of 0.37 g/dL. Additionally, the bone marrow biopsy was normocellular with no increased blasts or evidence of MM but revealed a small number of BRAF V600E clones, suggesting potential systemic involvement.
Given the concern for metastatic disease in the abdomen due to the possible mesenteric and ascitic fluid involvement seen on PET-CT, an exploratory laparoscopy was performed. No visible extrapancreatic disease in the abdomen was visualized, and washing was performed in the right upper quadrant. Although grossly normal, flow cytometry on the wash showed 3.5% kappa-restricted plasma cells.
Due to the low likelihood that radiation would be definitive, the patient was treated systemically for high-risk MM with daratumumab plus lenalidomide, bortezomib, and dexamethasone (D-RVd). However, after the first 2 treatment cycles, a CT scan of the abdomen and pelvis with IV contrast showed minimal response to D-RVd treatment, and the mass continued to obstruct the SMV. Consequently, D-RVd treatment was put on hold, and the patient is proceeding with radiation therapy. The patient's most recent gamma M-spike decreased and is at 0.10 g/dL.
Discussion
Here we report a case of solitary plasmacytoma of the pancreas, an extremely rare form of pancreatic cancer. Plasmacytoma, a cancer of plasma cells, can occur anywhere in the body as solitary or multiple masses and is most commonly seen in bone marrow [4]. This cancer is prevalent in African Americans and has a male predominance and a mean age of presentation of 55 years old [4]. If these plasma cell neoplasms occur in organs outside of the bone marrow, they are referred to as extramedullary plasmacytomas, and most frequently arise in the upper respiratory tract, liver, spleen, or stomach [4,5]. Although rare, these tumors may be found in the pancreas, accounting for only 2.3% of extramedullary plasmacytoma cases [6,7]. Furthermore, approximately 80% of these tumors occur in the pancreatic head [2] and can be primary or secondary to MM, depending on blood serum markers or bone marrow involvement [8]. Solitary plasmacytomas of the pancreas are associated with poor prognoses, especially in patients over the age of 50 with a tumor size above 4 cm [7].
Imaging plays an essential role in identifying the lesion location and guiding the biopsy of solitary plasmacytomas [2]. Dual-phase CT is the primary modality of choice because of the ability to assess vascularity [8]. In our case, the patient underwent CT imaging, which revealed a heterogeneous exophytic lobulated solid mass in the region of the pancreatic head/uncinate process measuring 7.7 × 7.2 × 6.5 cm, which was confirmed to be plasmacytoma after an EUS-FNA-guided biopsy and pathological analysis. Commonly established CT characteristics are described as a well-defined, focal, multilobulated solid mass with homogeneous IV contrast enhancement and hypodense in relation to the pancreatic parenchyma [2]. These generally nonspecific radiological features make pancreatic plasmacytomas challenging to differentiate from other pancreatic tumors that show IV contrast enhancement, such as PNETs and adenocarcinomas, especially in patients without a history of MM and related disease [9]. Lesion enhancement is another common feature of pancreatic plasmacytomas rendering differentiation from PNETs difficult [10]. On CT, PNETs are described as well-defined, hypervascular lesions with heterogenous enhancement [1]. Considering the heterogeneous, exophytic appearance and prominent vascularity of the mass in our patient, imaging findings diverged from those found in previous pancreatic plasmacytoma case reports and were consistent with a PNET. Also, because the mass did not obstruct the biliary tree and elicit the most common pancreatic plasmacytoma symptom, jaundice, it was challenging to determine a preprocedural diagnosis.
In addition to CT, PET-CT can help determine the lesion's probability of malignancy by revealing the presence of hypermetabolism [11]. The PET-CT findings, in this case, were an intensely FDG-avid multilobulated mass centered in the head/uncinate process, consistent with biopsy-proven plasmacytoma, and an avid nodular opacity indistinct from the right posterior lateral contour of the mass. Slight FDG-avid small ascites and soft tissue nodularities in the mesentery/left posterior peritoneum were seen with no evidence of FDG-avid osseous lesions above background activity to suggest metabolically active MM. However, due to possible carcinomatosis and lymph node involvement revealed by PET-CT and BRAF V600E clones seen in the bone marrow biopsy, the patient was treated with D-RVd and radiation. Though uncommon, BRAF V600E mutations have been reported in MM cases [12].
To our knowledge, there is no standardized treatment for solitary plasmacytoma of the pancreas. However, since these tumors have radiosensitive and chemosensitive properties, a combination of surgery, chemotherapy, or radiation is generally used [7]. In cases such as ours, where the tumor is large and has a high risk of systemic involvement, surgeries are not often performed [1]. Rather, chemotherapy treatments such as D-RVd are used, which can increase the duration of progression of plasmacytoma to MM but cannot decrease the incidence of progression to MM [1]. Furthermore, for the treatment of extramedullary plasmacytomas, Mignot et al. [13] reported that lenalidomide-dexamethasone treatment in combination with radiation therapy improved MM-free survival and progression-free survival. Generally, the course of treatment in cases where the tumor is not secondary to MM are associated with more favorable outcomes.
It is important to acknowledge the difficulty of diagnosing pancreatic plasmacytoma in a patient without a history of MM. There are only approximately 25 reported cases of pancreatic involvement in the English-language literature [14] and according to a 2015 study, only 8 case reports of pancreatic plasmacytoma were not associated with MM [9]. Given this cancer's potential to progress to MM (15% of extramedullary plasmacytoma cases), efficient and prompt diagnosis is essential for favorable patient outcomes [15].
Conclusion
Solitary plasmacytomas of the pancreas are a rare pancreatic neoplasm. Although they appear similar to other pancreatic tumors, they should be considered in the differential diagnosis in patients presenting with a heterogenous or homogenous multilobulated, hypodense, vascular, solid mass in the head of the pancreas, even in patients without a history of MM.
Patient consent
The patient reported in the manuscript signed the informed consent/authorization for participation in research, which includes the permission to use data collected in future research projects such as the presented case details and images used in this manuscript.
Footnotes
Competing Interests: The authors declare the following financial interests/personal relationships which may be considered as potential competing interests: Edmund M. Weisberg, MS, MBE, and Ryan C. Rizk, MS, have no competing financial interests or personal relationships that could have appeared to influence the work reported in this paper. Elliot K. Fishman, MD, receives grant funding from GE Healthcare and Siemens, and is a founder and stockholder, HipGraphics.
References
- 1.Lu T, Pu H, Zhao G. Primary pancreatic plasmacytoma: a rare case report. BMC Gastroenterol;17(1):167. [DOI] [PMC free article] [PubMed]
- 2.Lopes da Silva R. Pancreatic involvement by plasma cell neoplasms. J Gastrointest Cancer. 2012;43(2):157–167. doi: 10.1007/s12029-011-9314-9. [DOI] [PubMed] [Google Scholar]
- 3.Hefferman A. Plasmacytoma of pancreas and duodenum causing acute intestinal obstruction. Lancet. 1947;1(6461):910. doi: 10.1016/s0140-6736(47)91368-8. [DOI] [PubMed] [Google Scholar]
- 4.Iqbal QUA, Plasmacytoma Majid HJ. StatPearls Publishing; Treasure Island (FL): 2023. In: statpearls [Internet] [Google Scholar]
- 5.Alshomar KM, Altariqi SM, Alrikabi AC, Alkatan HM, Al-Faky YH. Primary extramedullary plasmacytoma of the eyelid conjunctiva - A case report and review of the literature. Ann Med Surg (Lond) 2020;55:1–4. doi: 10.1016/j.amsu.2020.04.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Paydas S. Pancreatic plasmacytoma: a rare but important entity for gastroenterologists, oncologists and hematologists. J Oncol Sci. 2019;5(3):109–111. [Google Scholar]
- 7.Le M, Surapaneni BK, Jain V, Vinayek R, Dutta SK. Pancreatic extramedullary plasmacytoma presenting as a pancreatic mass. Clin Med Insights Gastroenterol. 2018;11 doi: 10.1177/1179552218801603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hatem M, So B, Gray R, Wong J. Plasmocytoma presented as pancreatic head mass. Radiol Case Rep. 2015;10(4):81–87. doi: 10.1016/j.radcr.2015.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Utsumi T, Sasajima J, Goto T, Fujibayashi S, Dokoshi T, Sakatani A, et al. The detection of pancreatic and retroperitoneal plasmacytoma helped to diagnose multiple myeloma: a case report. Medicine (Baltimore) 2015;94(27):e914. doi: 10.1097/MD.0000000000000914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Akyuz F, Sahin D, Akyuz U, Vatansever S. Rare pancreas tumor mimicking adenocarcinoma: extramedullary plasmacytoma. World J Gastrointest Endosc. 2014;6(3):99–100. doi: 10.4253/wjge.v6.i3.99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhang D, Cao D, Shen D, Mulmi Shrestha S, Yin Y. Extramedullary plasmacytoma occurring in ileocecum: a case report and literature review. Medicine (Baltimore) 2017;96(51):e9313. doi: 10.1097/MD.0000000000009313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lehners N, Andrulis M, Capper D, von Deimling A, Ho AD, Goldschmidt H, et al. BRAF V600E mutations in multiple myeloma: clinical and therapeutic implications. Blood. 2012;120(21):4040. [Google Scholar]
- 13.Mignot F, Schernberg A, Arsène-Henry A, Vignon M, Bouscary D, Kirova Y. Solitary plasmacytoma treated by lenalidomide-dexamethasone in combination with radiation therapy: clinical outcomes. Int J Radiat Oncol Biol Phys. 2020;106(3):589–596. doi: 10.1016/j.ijrobp.2019.10.043. [DOI] [PubMed] [Google Scholar]
- 14.Smith A, Hal H, Frauenhoffer E. Extramedullary plasmacytoma of the pancreas: a rare entity. Case Rep Radiol. 2012;2012 doi: 10.1155/2012/798264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.International Myeloma Working Group Criteria for the classification of monoclonal gammopathies, multiple myeloma and related disorders: a report of the International Myeloma Working Group. Br J Haematol. 2003;121(5):749–757. [PubMed] [Google Scholar]