Abstract
Purpose
To compare a large cohort of patients who underwent remnant-sparing anterior cruciate ligament reconstruction (rACLR) with a matched group of patients who underwent anatomic single-bundle anterior cruciate ligament reconstruction (ACLR) with respect to clinical laxity, patient-reported outcomes, and functional testing.
Methods
Patients who underwent rACLR between January 2010 and December 2015 were matched according to age, sex, body mass index, and graft type to patients who underwent ACLR. The primary outcome measure was the ACL Quality of Life (ACL-QOL) score at final follow-up of 24 months. Secondary outcomes included functional tests and clinical laxity measurements at 6, 12, and 24 months postoperatively. Concurrent intra-articular pathology at the time of surgery and postoperative complications were also recorded. Statistical analyses included the dependent t test and the Wilcoxon signed rank test.
Results
A total of 210 rACLR patients were successfully matched to a corresponding cohort of 210 ACLR patients. There were no statistically significant differences in ACL Quality of Life (ACL-QOL) or functional testing results between the groups; however, scores in both groups showed a steady and statistically significant improvement over time. A statistically significant difference was noted with respect to the Lachman test findings, favoring the rACLR cohort (Z = –2.79, P = .005); no between-group difference was seen for the pivot-shift test (Z = –0.36, P = .72). The rACLR group had a significantly lower rate of concurrent meniscal and chondral injury. There was no difference in complications between the groups (Z = –0.49, P = .63).
Conclusions
There was no difference in patient-reported or functional testing outcomes in patients undergoing remnant-sparing compared with anatomic single-bundle ACLR. There was, however, a significantly lower rate of positive Lachman test findings after rACLR. Furthermore, the rate of concurrent meniscal and chondral pathology was lower in the rACLR group.
Level of Evidence
Level III, retrospective cohort study.
Partial tears of the anterior cruciate ligament (ACL) are a common presenting complaint in the field of sport medicine and are becoming increasingly recognized as a source of knee instability in the active patient population. Advances in medical imaging have allowed for improved visualization of knee ligaments, and partial tears have been identified in 5% to 28% of ACL injuries.1, 2, 3 Natural history studies have shown that 72% of partial ACL injuries contribute to activity-related instability, and nearly half progress to complete tears without surgical intervention.4, 5, 6 In light of these findings, many surgeons advocate early surgical treatment of symptomatic partial ACL injuries.
Despite substantial attention in the literature, the optimal approach for surgical treatment of partial ACL tears remains undefined. The surgical decision-making process centers on the remnant ACL fibers and whether it is best to remove this tissue or retain it and perform a “remnant-sparing” ACL reconstruction (rACLR). The latter technique can refer to either preservation of the native ACL stump or an intact ACL bundle(s) (also referred to as “selective bundle reconstruction”). The proposed advantages of rACLR include the presence of a mechanical strut during graft healing, accelerated graft revascularization and synovialization, and improved proprioception through maintenance of native mechanoreceptors.7, 8, 9, 10 The main disadvantages include challenging visualization of anatomic landmarks that may predispose to compromised tunnel positioning, the need for careful tunnel drilling to avoid damaging the remnant fibers, and formation of a cyclops lesion leading to an extension deficit.
A number of clinical studies have investigated outcomes after rACLR, and variable results have been reported. Some authors have shown decreased laxity and improved patient-reported outcomes with the remnant-sparing technique, whereas others have been unable to show a difference compared with standard ACL reconstruction (ACLR).3,11, 12, 13, 14, 15, 16 Many of these studies have been composed of small patient cohorts, and few have included an appropriate control group.
The purpose of this study was to compare a large cohort of patients who underwent rACLR with a matched group of patients who underwent anatomic single-bundle ACLR with respect to clinical laxity, patient-reported outcomes, and functional testing. We hypothesized that patients in the rACLR group would display improved overall outcomes with respect to patient-reported measures, knee laxity, and functional assessments.
Methods
An electronic patient database from a 4-surgeon (S.M.H., G.M.B., L.A.H., and M.K.) subspecialty sport medicine practice was retrospectively reviewed. All patients who underwent rACLR for symptomatic knee instability between January 2010 and December 2015 were identified. Patients were excluded if they required multiligament reconstruction, repair of a meniscal root or radial tear, treatment of chondral pathology, or revision ACLR. Patients were then matched according to sex, age (within 2 years), body mass index (BMI) (within 2), and graft type to patients who underwent anatomic single-bundle ACLR. Operative records were reviewed to collect surgical information including graft size, meniscal pathology and treatment, and chondral pathology. Clinical laxity was assessed preoperatively and postoperatively via standard Lachman and pivot-shift testing. Disease-specific patient-reported outcomes were assessed using the ACL Quality of Life (ACL-QOL) questionnaire. A battery of functional tests were conducted and recorded at 6, 12, and 24 months postoperatively.
Surgical Technique
Patients underwent either spinal or general anesthesia based on an assessment of risk factors as well as patient preference. Preoperative cefazolin was administered, and patients were positioned supine. A tourniquet was not used. An examination under anesthesia was performed to rule out multiligamentous injury and confirm the degree of ACL laxity per Lachman and pivot-shift testing.
A diagnostic arthroscopy was performed. Any chondral or meniscal pathology was documented and treated as necessary. Any remnant ACL fibers were evaluated, and a remnant-sparing technique was undertaken if a robust tibial stump comprising more than 50% of the native tissue was present and/or if the remnant ACL fibers remained attached at their native femoral origin. In all other cases, a standard single-bundle ACLR was performed.
All grafts were either hamstring autograft or non-irradiated fresh-frozen soft-tissue allograft. The tendon or tendons were passed through a fixed-loop suspensory fixation device (EndoButton; Smith & Nephew, London, England), and the ends were whipstitched with No. 2 FiberWire suture (Arthrex, Naples, FL). The diameter and length of the graft were measured. The femoral tunnel was drilled via an inside-out technique through an anteromedial portal. The graft was secured in the tibial tunnel with the use of a bioabsorbable screw (Genesys Matrix; ConMed, Largo, FL) with the knee in full extension.
Postoperative Assessments and Outcome Measures
Patients were permitted to bear weight as tolerated with crutches immediately postoperatively. A brace was not used. In the event of a concurrent meniscal repair, knee flexion was restricted to 90° until 6 weeks postoperatively. A phase-based rehabilitation approach was used, whereby dynamic plyometrics were initiated after 3 months, controlled pivoting activities were started after 6 months, and return to sport was permitted after 9 to 12 months in most cases. Clinical assessments and laxity tests were performed independently by one of the primary surgeons and a physiotherapist at 6, 12, and 24 months. The physiotherapist but not the surgeon was blinded to the procedure performed. Range of motion was measured via a goniometer. Lachman and pivot-shift tests were graded according to the International Knee Documentation Committee (IKDC) standard, and a positive test finding was defined as grade I or greater. Concurrent functional testing with a physiotherapist took place at 6, 12, and 24 months postoperatively. Functional tests included the single-leg half ball balance, 1-legged hop for distance, triple hop for distance, triple crossover hop for distance, and 1-legged 6-m timed hop. Patients completed the ACL-QOL questionnaire preoperatively and at 6, 12, and 24 months postoperatively.17 Failure of the surgical reconstruction was defined as laxity examination finding greater than II and/or symptomatic instability necessitating revision ACLR. Complications including infection, thromboembolic events, and knee stiffness were recorded to enable a between-group comparison.
Statistical Analysis
Demographic data for the rACLR and ACLR groups were compared using the paired t test to assess for between-group differences. ACL-QOL scores of the 2 groups were compared preoperatively and at 6, 12, and 24 months postoperatively using a 1-way analysis of variance. Objective functional testing measures were compared between the rACLR and ACLR groups at 6, 12, and 24 months postoperatively using a 1-way analysis of variance. The sample size calculation was based on a projected ACL-QOL outcome score of 75.0 (standard deviation, 20) at 24-month follow-up. The minimal clinically important difference was calculated as 10 points, with power = 0.90 and significance of P < .05. This calculation resulted in a requirement of 131 patients per group to assess for a difference in the primary outcome. Matching of the 2 cohorts occurred retrospectively, with 210 patients per group, for a total of 420 patients included in the analysis.18, 19, 20 The Wilcoxon signed rank test was used to determine whether there were differences between the rACLR and ACLR groups in the Lachman and pivot-shift laxity measures at 24 months postoperatively. The Wilcoxon signed rank test was also used to compare the rACLR and ACLR groups in terms of rates of surgical failure, as well as rates of meniscal and chondral pathology at the time of surgery. Time from injury to surgery was compared between the groups using the paired t test. All statistical analysis was completed using SPSS software (version 26; IBM, Armonk, NY).
Results
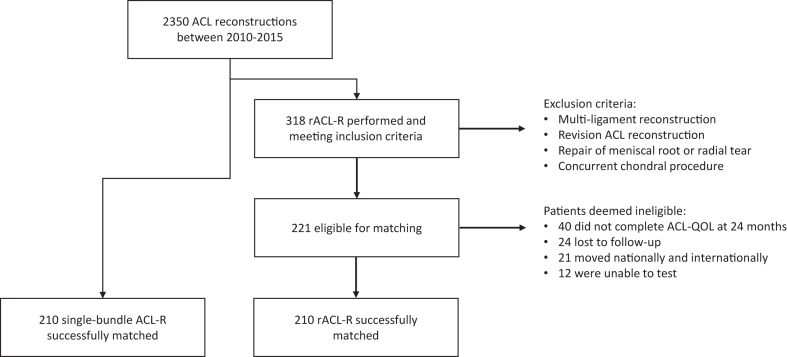
Between January 2010 and December 2015, a total of 2,350 ACLRs were performed. Of these surgical procedures, 318 met the criteria for inclusion in the rACLR group. A total of 221 patients completed final follow-up at 24 months (40 did not complete the ACL-QOL questionnaire, 24 were lost to follow-up, 21 moved nationally or internationally, and 12 were unable to complete functional testing). Two hundred ten patients were successfully matched by age, sex, BMI, and graft type to ACLR patients meeting the inclusion criteria (Fig 1).
Fig 1.
Subject enrollment flowchart. (ACL, anterior cruciate ligament; ACL-QOL, ACL Quality of Life; ACL-R, anterior cruciate ligament reconstruction; rACL-R, remnant-sparing anterior cruciate ligament reconstruction.)
The demographic and injury data for both cohorts are presented in Table 1. The Beighton score was used as a measure of generalized ligamentous laxity, and a score of 4 of 9 was considered positive. No statistically significant differences were noted between the groups with respect to sex, BMI, or Beighton score. A statistically significant difference was noted between the groups with respect to age; however, this is unlikely to represent clinical significance given that patients were matched by age within 2 years. The time from injury to surgery was significantly greater in the ACLR group. No differences were noted between the groups with respect to graft type (autograft vs allograft); however, the graft diameter was significantly smaller in the rACLR cohort. Statistically significant differences were noted in favor of the rACLR group with respect to decreased rates of meniscal and chondral injury. No differences were noted in rates of meniscal repair or resection.
Table 1.
Demographic and Injury Data of rACLR and ACLR Cohorts
| rACLR | ACLR | t or Z Statistic | P Value | |
|---|---|---|---|---|
| Mean age (SD), yr | 34.00 (10.90) | 34.11 (10.81) | t = –2.267 | .024∗ |
| Sex: M/F, n | 110/100 | 110/100 | — | — |
| Mean BMI (SD) | 25.03 (3.40) | 25.06 (3.06) | t = –0.357 | .721 |
| Mean Beighton score (SD) | 3.04 (2.48) | 3.30 (2.52) | t = –1.231 | .220 |
| Mean time from injury to surgery (SD), d | 327.1 (107) | 448.9 (112) | t = 2.81 | .005∗ |
| Graft: autograft/allograft, n | 174/36 | 174/36 | — | — |
| Mean graft diameter in mm (SD) | 7.30 (0.82) | 7.70 (0.72) | t = –5.587 | .001∗ |
| Meniscal injury, n (%) | 110 (52.5) | 135 (64.3) | Z = –2.62 | .009∗ |
| Meniscal resection, n (%) | 60 (28.6) | 76 (36.2) | Z = –1.77 | .08 |
| Meniscal repair, n (%) | 51 (24.2) | 54 (25.67) | Z = –0.35 | .73 |
| Chondral injury, n (%) | 62 (30.0) | 80 (38.1) | Z = –2.04 | .04∗ |
ACLR, anterior cruciate ligament reconstruction; rACLR, remnant-sparing anterior cruciate ligament reconstruction; BMI, body mass index; F, female; M, male; SD, standard deviation.
Statistically significant.
There was a significant difference in the total number of patients with positive Lachman test findings after rACLR (18 of 210) compared with ACLR (40 of 210) (IKDC grade I or greater) at 24 months postoperatively (Z = –2.79, P = .005). In contrast, there was no significant difference in the total number of patients with positive pivot-shift test findings after rACLR (12 of 210) compared with ACLR (14 of 210) (Z = –0.36, P = .72). A total of 7 rACLR and 10 ACLR patients had both positive Lachman test and positive pivot-shift test findings. Only 1 patient in the ACLR group had a Lachman test graded as II; all other patients with “positive” clinical laxity test findings were graded as I.
The ACL-QOL scores preoperatively and at 6, 12, and 24 months postoperatively are presented in Table 2. Statistically significant improvements between preoperative and postoperative ACL-QOL scores were observed in both cohorts, and the scores showed statistically significant improvements over time (out to 24 months postoperatively). However, no statistically significant differences in ACL-QOL scores were detected between the rACLR and ACLR groups.
Table 2.
Mean ACL-QOL Scores Preoperatively and at 6, 12, and 24 Months Postoperatively in rACLR and ACLR Cohorts
| Time | ACL-QOL Score |
|
|---|---|---|
| rACLR | ACLR | |
| Preoperatively | 27.87 (12.33) (n = 163) | 31.45 (14.15) (n = 155) |
| Postoperatively | ||
| 6 mo | 57.37 (18.60) (n = 173) | 60.17 (16.64) (n = 170) |
| 12 mo | 72.56 (17.92) (n = 173) | 74.41 (16.60) (n = 165) |
| 24 mo | 78.51 (17.96) (n = 210) | 80.46 (17.40) (n = 210) |
NOTE. Data are presented as mean (standard deviation).
ACL-QOL, ACL Quality of Life; ACLR, anterior cruciate ligament reconstruction; n, total number; rACLR, remnant-sparing anterior cruciate ligament reconstruction.
Descriptive data for the functional tests at 6, 12, and 24 months postoperatively are listed in Table 3. There were no statistically significant differences between the rACLR and ACLR groups in the battery of functional tests at any time point. However, both groups showed continued improvements in their testing results over time, with statistically significant improvements noted between 6 and 24 months. No statistically significant improvements were observed between 6 and 12 months or between 12 and 24 months. The patients who received autografts in both groups significantly outperformed those who received allografts in nearly all tests at all time points. No difference in performance was noted between allograft patients in the rACLR and ACLR cohorts.
Table 3.
Mean Functional Testing Data at 6, 12, and 24 Months Postoperatively in rACLR and ACLR Groups Stratified by Autograft and Allograft
| Functional Test | 6 mo |
12 mo |
24 mo |
|||
|---|---|---|---|---|---|---|
| rACLR | ACLR | rACLR | ACLR | rACLR | ACLR | |
| Single-leg balance, s | ||||||
| Autograft | 23.41 (8.58) | 23.73 (9.03) | 25.42 (7.73) | 24.60 (8.92) | 24.40 (8.39) | 23.92 (8.93) |
| Allograft | 19.64 (10.40) | 16.58 (10.40) | 18.40 (11.24) | 20.00 (9.91) | 17.59 (10.17) | 20.54 (10.01) |
| Hop for distance, m | ||||||
| Autograft | 1.30 (0.35) | 1.30 (0.33) | 1.44 (0.31) | 1.39 (0.35) | 1.46 (0.31) | 1.46 (0.31) |
| Allograft | 1.11 (0.29) | 1.05 (0.27) | 1.21 (0.32) | 1.18 (0.26) | 1.18 (0.29) | 1.22 (0.27) |
| Timed hop, s | ||||||
| Autograft | 2.85 (1.00) | 2.82 (0.78) | 2.55 (0.70) | 1.39 (0.35) | 2.54 (0.80) | 2.47 (0.64) |
| Allograft | 3.31 (0.92) | 3.40 (1.05) | 3.09 (0.80) | 1.18 (0.26) | 3.01 (0.70) | 3.10 (0.82) |
| Triple hop, m | ||||||
| Autograft | 3.88 (0.99) | 3.88 (0.99) | 4.23 (0.92) | 4.13 (1.03) | 4.29 (0.92) | 4.21 (1.02) |
| Allograft | 3.30 (0.83) | 2.94 (0.83) | 3.47 (0.63) | 3.46 (0.77) | 3.43 (0.71) | 3.42 (0.84) |
| Crossover hop, m | ||||||
| Autograft | 3.44 (0.96) | 3.34 (1.00) | 3.77 (0.92) | 3.69 (1.02) | 3.77 (0.93) | 3.74 (0.98) |
| Allograft | 2.82 (0.88) | 2.54 (0.64) | 3.07 (0.64) | 3.03 (0.74) | 3.01 (0.73) | 2.94 (0.78) |
NOTE. Data are presented as mean (standard deviation).
ACLR, anterior cruciate ligament reconstruction; rACLR, remnant-sparing anterior cruciate ligament reconstruction.
Descriptive data for the complications in both the rACLR and ACLR groups are listed in Table 4. No significant difference between the rACLR and ACLR groups was noted with respect to any of the reported complications including graft rupture or knee stiffness (Z = –0.49, P = .63).
Table 4.
Number of Complications After Surgery in rACLR and ACLR Groups
| Complication | rACLR, n | ACLR, n |
|---|---|---|
| ACL graft failure | 3 | 4 |
| Saphenous nerve injury∗ | 29 | 35 |
| Infection† | ||
| Superficial | 3 | 5 |
| Deep | — | 2 |
| DVT | 2 | 2 |
| Meniscal tear | 6 | 8 |
| Stiffness‡ | 3 | 7 |
ACL, anterior cruciate ligament; ACLR, anterior cruciate ligament reconstruction; DVT, deep venous thrombosis; rACLR, remnant-sparing anterior cruciate ligament reconstruction.
Saphenous nerve injury was classified as any numbness greater than 2 cm2 inferior to the incision for graft harvest and/or tibial tunnel drilling.
Superficial infections were treated with a course of antibiotics, whereas deep infections required repeated surgery for irrigation and debridement.
Stiffness was defined as a greater than 5° loss of knee flexion or extension compared with the nonoperative limb.
Discussion
This study revealed no differences in ACL-QOL scores or functional testing scores between matched cohorts of patients undergoing anatomic single-bundle ACLR and patients undergoing rACLR. No between-group differences were observed in the pivot-shift test findings; however, the rACLR group had fewer positive Lachman examination findings compared with the ACLR group, and this difference was statistically significant. The rACLR group also had fewer injuries to the menisci and articular cartilage as detected during intraoperative diagnostic arthroscopy. There were no between-group differences in graft failure, knee stiffness, or other surgical complications.
The literature to date has yielded variable results with respect to patient-reported outcomes after rACLR. A 2016 meta-analysis by Tie et al.10 evaluated 6 randomized controlled trials that compared outcomes of rACLR (190 patients) and anatomic single-bundle ACLR (188 patients). The authors showed no difference in Lysholm or IKDC scores between the groups. In contrast, subsequent meta-analyses have shown a statistically significant difference in Lysholm scores favoring patients undergoing rACLR but no difference in IKDC scores.16,21, 22, 23 A recent prospective trial randomized patients undergoing single-bundle ACLR with hamstring autograft to either the remnant preservation group or remnant debridement group.24 Of 49 randomized patients, 86% were available for telephone follow-up at 10 years. The authors found no difference between the groups with respect to return to work or sport or perceived knee function.24 Our study showed no statistically significant difference in ACL-QOL scores between the groups at any time point from 6 to 24 months postoperatively. These results further strengthen the body of evidence that shows no difference in patient-reported outcomes with rACLR techniques.
The literature is equally inconclusive when comparing clinical laxity in rACLR and ACLR patients. In the previously mentioned meta-analysis by Tie et al.,10 no between-group differences in KT-1000 (MEDmetric, San Diego, CA), Lachman, or pivot-shift test findings were identified. However, Wang et al.21 showed improved side-to-side laxity using the KT-1000/KT-2000 device (MEDmetric) or Rolimeter (Aircast, Vista, CA) in their rACLR cohort. The authors did not find a difference in Lachman or pivot-shift test results between the groups. Our study showed a significant difference in Lachman test findings favoring the rACLR cohort (P = .005) and no-between group difference in pivot-shift test findings. Reduced graft laxity in rACLR patients may be due to enhanced synovialization and revascularization of the ACL graft, leading to more native biomechanical properties. A study by Kondo et al.25 showed that preservation of more than 50% of the native ACL fibers significantly reduced anterior translation on KT-2000 testing. The lack of difference noted on pivot-shift testing may be explained by the inherent challenge of performing this test accurately in non-anesthetized patients owing to guarding or reflex muscle contraction. Alternatively, this may correlate to the preferential reconstruction of either the anteromedial or posterolateral ACL bundle depending on the condition of the native ACL. Further research into selective bundle reconstruction may shed some light on this interesting topic.
This study compared functional outcomes in patients undergoing rACLR and single-bundle ACLR and revealed no difference in performance on dynamic hop and balance testing between the groups. In a clinical study of proprioception, Adachi et al.14 assessed joint position sense using a Cybex dynamometer (Rosemont, IL) and showed better results in patients who underwent rACLR compared with those who underwent standard ACLR. A recent systematic review investigated the effect of remnant-sparing techniques on proprioception in ACLR.26 The authors identified 4 studies, of which 3 assessed proprioception via a reproduction of passive positioning, and all of them revealed better results in the rACLR group. Reproduction of active positioning was assessed by 1 study and was also noted to be superior in the rACLR group.26 The lack of difference in testing results between the groups in our study may suggest that the proprioceptive advantages of rACLR do not directly translate to dynamic functional testing. However, this study was not powered for functional testing results, and thus, not all patients had complete data at all time points. Given that the proprioceptive advantages of the native ACL fibers would be most significant in the early postoperative period, a more detailed investigation of functional testing at the 6-month postoperative time point would be valuable.
An interesting finding of this study was that the rACLR group had lower rates of both meniscal injury and chondral injury at the time of surgery compared with the ACLR cohort. Although this may be related to a slightly shorter time from injury to surgery in the rACLR group, other factors such as a less traumatic initial injury and stability conferred by the intact ACL fibers likely also contribute to protecting the menisci and chondral surfaces. However, given that nearly 50% of partial ACL injuries progress to complete tears, this finding lends support to early surgical treatment of partial ACL tears to prevent secondary injury. This is of particular relevance in the young and active patient cohort who may not be experiencing functional instability. These patients may benefit from early surgical reconstruction to limit meniscal and chondral injury and thereby reduce the risk of osteoarthritis.
Limitations
One limitation of this study was the retrospective nature and inherent biases of this design. Furthermore, given that the primary outcome measure was the ACL-QOL score at 24 months postoperatively, the intermediate follow-up at 6 and 12 months postoperatively was not completed for all outcome measures in all patients. It is thus possible that differences between the cohorts at earlier time points were not detected
Conclusions
There was no difference in patient-reported or functional testing outcomes in patients undergoing remnant-sparing compared with anatomic single-bundle ACLR. There was, however, a significantly lower rate of positive Lachman test findings after rACLR. Furthermore, the rate of concurrent meniscal and chondral pathology was lower in the rACLR group.
Disclosure
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests: L.A.H. receives speaking and lecture fees from ConMed and Smith & Nephew. All other authors (M.K., S.M.H., G.M.B., M.R.L., S.K.) declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Supplementary Data
References
- 1.Zantop T., Brucker P.U., Vidal A., Zelle B.A., Fu F.H. Intraarticular rupture pattern of the ACL. Clin Orthop Relat Res. 2007;454:48–53. doi: 10.1097/BLO.0b013e31802ca45b. [DOI] [PubMed] [Google Scholar]
- 2.Sonnery-Cottet B., Colombet P. Partial tears of the anterior cruciate ligament. Orthop Traumatol Surg Res. 2016;102:S59–S67. doi: 10.1016/j.otsr.2015.06.032. (suppl) [DOI] [PubMed] [Google Scholar]
- 3.Ochi M., Adachi N., Deie M., Kanaya A. Anterior cruciate ligament augmentation procedure with a 1-incision technique: Anteromedial bundle or posterolateral bundle reconstruction. Arthroscopy. 2006;22:463.e1–463.e5. doi: 10.1016/j.arthro.2005.06.034. [DOI] [PubMed] [Google Scholar]
- 4.Noyes F.R., Mooar L.A., Moorman C.T., III, McGinniss G.H. Partial tears of the anterior cruciate ligament. Progression to complete ligament deficiency. J Bone Joint Surg Br. 1989;71:825–833. doi: 10.1302/0301-620X.71B5.2584255. [DOI] [PubMed] [Google Scholar]
- 5.Fritschy D., Panoussopoulos A., Wallensten R., Peter R. Can we predict the outcome of a partial rupture of the anterior cruciate ligament? A prospective study of 43 cases. Knee Surg Sports Traumatol Arthrosc. 1997;5:2–5. doi: 10.1007/s001670050015. [DOI] [PubMed] [Google Scholar]
- 6.Buckley S.L., Barrack R.L., Alexander A.H. The natural history of conservatively treated partial anterior cruciate ligament tears. Am J Sports Med. 1989;17:221–225. doi: 10.1177/036354658901700212. [DOI] [PubMed] [Google Scholar]
- 7.Takahashi T., Kondo E., Yasuda K., et al. Effects of remnant tissue preservation on the tendon graft in anterior cruciate ligament reconstruction: A biomechanical and histological study. Am J Sports Med. 2016;44:1708–1716. doi: 10.1177/0363546516643809. [DOI] [PubMed] [Google Scholar]
- 8.Choi S., Kim M.K., Kwon Y.S., Kang H. Clinical and arthroscopic outcome of single bundle anterior cruciate ligament reconstruction: Comparison of remnant preservation versus conventional technique. Knee. 2017;24:1025–1032. doi: 10.1016/j.knee.2017.05.012. [DOI] [PubMed] [Google Scholar]
- 9.Adachi N., Ochi M., Uchio Y., Iwasa J., Ryoke K., Kuriwaka M. Mechanoreceptors in the anterior cruciate ligament contribute to the joint position sense. Acta Orthop Scand. 2002;73:330–334. doi: 10.1080/000164702320155356. [DOI] [PubMed] [Google Scholar]
- 10.Tie K., Chen L., Hu D., Wang H. The difference in clinical outcome of single-bundle anterior cruciate ligament reconstructions with and without remnant preservation: A meta-analysis. Knee. 2016;23:566–574. doi: 10.1016/j.knee.2015.07.010. [DOI] [PubMed] [Google Scholar]
- 11.Abat F., Gelber P.E., Erquicia J.I., Pelfort X., Tey M., Monllau J.C. Promising short-term results following selective bundle reconstruction in partial anterior cruciate ligament tears. Knee. 2013;20:332–338. doi: 10.1016/j.knee.2013.05.006. [DOI] [PubMed] [Google Scholar]
- 12.Pujol N., Colombet P., Potel J.F., et al. Anterior cruciate ligament reconstruction in partial tear: Selective anteromedial bundle reconstruction conserving the posterolateral remnant versus single-bundle anatomic ACL reconstruction: Preliminary 1-year results of a prospective randomized study. Orthop Traumatol Surg Res. 2012;98(suppl):S171–S177. doi: 10.1016/j.otsr.2012.09.007. [DOI] [PubMed] [Google Scholar]
- 13.Sonnery-Cottet B., Panisset J.C., Colombet P., et al. Partial ACL reconstruction with preservation of the posterolateral bundle. Orthop Traumatol Surg Res. 2012;98(suppl):S165–S170. doi: 10.1016/j.otsr.2012.10.001. [DOI] [PubMed] [Google Scholar]
- 14.Adachi N., Ochi M., Uchio Y., Sumen Y. Anterior cruciate ligament augmentation under arthroscopy. A minimum 2-year follow-up in 40 patients. Arch Orthop Trauma Surg. 2000;120:128–133. doi: 10.1007/s004020050028. [DOI] [PubMed] [Google Scholar]
- 15.Song G.Y., Zhang H., Zhang J., et al. The anterior cruciate ligament remnant: To leave it or not? Arthroscopy. 2013;29:1253–1262. doi: 10.1016/j.arthro.2013.03.078. [DOI] [PubMed] [Google Scholar]
- 16.Hu J., Qu J., Xu D., Zhang T., Zhou J., Lu H. Clinical outcomes of remnant preserving augmentation in anterior cruciate ligament reconstruction: A systematic review. Knee Surg Sports Traumatol Arthrosc. 2014;22:1976–1985. doi: 10.1007/s00167-013-2749-8. [DOI] [PubMed] [Google Scholar]
- 17.Mohtadi N. Development and validation of the quality of life outcome measure (questionnaire) for chronic anterior cruciate ligament deficiency. Am J Sports Med. 1998;26:350–359. doi: 10.1177/03635465980260030201. [DOI] [PubMed] [Google Scholar]
- 18.Lafave M.R., Hiemstra L., Kerslake S., Heard M., Buchko G. Validity, reliability, and responsiveness of the Anterior Cruciate Ligament Quality of Life measure: A continuation of its overall validation. Clin J Sport Med. 2017;27:57–63. doi: 10.1097/JSM.0000000000000292. [DOI] [PubMed] [Google Scholar]
- 19.Mohtadi N., Chan D., Barber R., Oddone Paolucci E. A randomized clinical trial comparing patellar tendon, hamstring tendon, and double-bundle ACL reconstructions: Patient-reported and clinical outcomes at a minimal 2-year follow-up. Clin J Sport Med. 2015;25:321–331. doi: 10.1097/JSM.0000000000000165. [DOI] [PubMed] [Google Scholar]
- 20.Marien M., Lafave M.R., Hiemstra L.A., Heard S.M., Buchko G.M., Kerslake S. Validity, responsiveness, and reliability of the ACL-QOL in an adolescent population. J Pediatr Orthop. 2021;41:e917–e922. doi: 10.1097/BPO.0000000000001964. [DOI] [PubMed] [Google Scholar]
- 21.Wang H., Liu Z., Li Y., et al. Is remnant preservation in anterior cruciate ligament reconstruction superior to the standard technique? A systematic review and meta-analysis. Biomed Res Int. 2019;2019 doi: 10.1155/2019/1652901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wang H.D., Wang F.S., Gao S.J., Zhang Y.Z. Remnant preservation technique versus standard technique for anterior cruciate ligament reconstruction: A meta-analysis of randomized controlled trials. J Orthop Surg Res. 2018;13:231. doi: 10.1186/s13018-018-0937-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ma T., Zeng C., Pan J., Zhao C., Fang H., Cai D. Remnant preservation in anterior cruciate ligament reconstruction versus standard techniques: A meta-analysis of randomized controlled trials. J Sports Med Phys Fitness. 2017;57:1014–1022. doi: 10.23736/S0022-4707.16.06832-8. [DOI] [PubMed] [Google Scholar]
- 24.Annear P.T., Rohr E.J., Hille D.M., Gohil S., Ebert J.R. No clinical difference in 10-year outcomes between standard and minimal graft debridement techniques in patients undergoing anterior cruciate ligament reconstruction using autologous hamstrings: A randomized controlled trial. Knee Surg Sports Traumatol Arthrosc. 2019;27:516–523. doi: 10.1007/s00167-018-5146-5. [DOI] [PubMed] [Google Scholar]
- 25.Kondo E., Yasuda K., Onodera J., Kawaguchi Y., Kitamura N. Effects of remnant tissue preservation on clinical and arthroscopic results after anatomic double-bundle anterior cruciate ligament reconstruction. Am J Sports Med. 2015;43:1882–1892. doi: 10.1177/0363546515587713. [DOI] [PubMed] [Google Scholar]
- 26.Cho E., Chen J., Xu C., Zhao J. Remnant preservation may improve proprioception after anterior cruciate ligament reconstruction. J Orthop Traumatol. 2022;23:22. doi: 10.1186/s10195-022-00641-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.