Abstract
Childhood trauma has been linked to schizophrenia, but underlying biological mechanisms remain elusive. This study explored the potential role of plasma oxytocin as a mediator in the relationship between childhood trauma and the psychopathology of schizophrenia. 160 patients with schizophrenia and 80 age- and sex-matched healthy controls were assessed for childhood trauma experiences using the Childhood Trauma Questionnaire and structured interviews. Psychopathology was evaluated using the Positive and Negative Syndrome Scale and plasma oxytocin levels were measured. Results showed that patients with schizophrenia had lower oxytocin levels and higher childhood trauma scores than healthy controls. There was a significant correlation between childhood trauma scores and psychopathology, with plasma oxytocin levels being inversely associated with psychopathology, except for positive symptoms. Hierarchical regression analysis indicated that both childhood trauma scores and plasma oxytocin levels significantly predicted psychopathology. Plasma oxytocin levels partially mediated the relationship between childhood trauma and schizophrenia psychopathology. This study underscores the potential role of oxytocin in bridging the gap between childhood trauma and schizophrenia.
Subject terms: Biomarkers, Developmental biology, Schizophrenia
Introduction
Childhood trauma is recognized as a factor indicating vulnerability to psychotic symptoms and schizophrenia1,2. Evidence indicates that patients with schizophrenia are more likely to report a history of childhood adversity or trauma than healthy controls are3. Research has consistently identified increased risks of developing psychotic disorders and schizophrenia in the context of various factors among individuals with the experience of child adversity or trauma4,5, though establishing direct causality remains complex. Patients with schizophrenia who experienced childhood trauma are typically younger age at schizophrenia onset6,7, have worse psychotic symptoms8,9, have more severe functional impairment10,11, respond to treatment more poorly12, and have an even higher risk of suicide13 than those who did not experience childhood trauma.
Despite the well-established relationship between childhood trauma and schizophrenia, the mechanisms underlying the association, particularly the biological mechanisms, are poorly understood. Few studies have explored the possible factors mediating this relationship, such as neurotransmitters and hormones. Oxytocin, a hormonal neuropeptide that regulates social cognition, social affiliation, stress, learning and memory14, has been reported to have a role in regulating the expression of schizophrenia15. Both human and animal studies have explored the role of oxytocin in the development of schizophrenia16, particularly its impact on social cognition. Studies examining the endogenous oxytocin levels of patients with schizophrenia have reported mixed findings, with some suggesting that the endogenous oxytocin levels in these patients are lower than those in the healthy population17. Oxytocin dysregulation has been demonstrated to be associated with several symptom domains of schizophrenia, particularly negative symptoms and social cognition. A negative correlation between endogenous oxytocin levels and negative symptoms has been reported in numerous studies18,19. Oxytocin is critical to the regulation of social cognition in schizophrenia, indicating that patients with higher endogenous oxytocin levels are associated with more effective recognition of facial emotions20 and social cues21. These findings elucidate the role of oxytocin in the pathophysiology of schizophrenia and have inspired growing research on the therapeutic potential of exogenous oxytocin; some clinical trials have reported encouraging results22,23, but the overall findings have been inconsistent. Several factors, such as dosage, route of administration, and individual variations in endogenous oxytocin levels and oxytocin receptor gene, can interfere with treatment efficacy16,24,25. Furthermore, it is plausible that individuals with inherently lower endogenous oxytocin levels and oxytocin receptor gene polymorphisms26,27, potentially due to factors like childhood trauma, may respond more effectively to intranasal oxytocin treatment. This suggests that intranasal oxytocin could be a viable therapeutic option for patients with schizophrenia, particularly those with a history of childhood trauma. However, further research is required to explore this hypothesis, determine the optimal target groups and treatment course, and gain a more thorough understanding of the mechanisms underpinning the relationship between schizophrenia and oxytocin28.
Childhood trauma can have wide-ranging impacts; while some forms involve physical harm, others primarily result in psychological or emotional impacts. These experiences can potentially affect the developing brain, leading to dysregulation in neurotransmitter systems and hormonal production, which may contribute to deficits in behavioral, cognitive, and emotional regulation29. Oxytocinergic dysfunction is one of the most studied hormonal disturbances. Most studies have identified an inverse relation between childhood trauma and endogenous oxytocin concentration30,31; however, a positive association has also been reported32,33. A previous systematic review concluded that reduced oxytocin levels were associated with the history of trauma, supporting the assumption that adversity in early life alters oxytocin homeostasis in the long term34. Polymorphism of the oxytocin receptor gene moderates the link between the incidence of childhood abuse and social relationships35, implying that childhood trauma may influence the oxytocinergic system through genetic mechanisms. The aforementioned evidence indicates that childhood trauma disrupts the oxytocinergic system, and this disruption may be associated with the progression of schizophrenia. Whether oxytocin mediates the path from childhood trauma to schizophrenia is unconfirmed.
This study explored the relationship between childhood trauma and the clinical symptoms of schizophrenia to investigate the role of plasma oxytocin in this association. New treatment modalities must be developed to address the insufficiency of existing therapies, particularly in alleviating negative symptoms and social cognitive deficits. The identification of key mediators is the first step toward developing new therapeutic agents. In accordance with the literature, we hypothesized the following: (1) patients with schizophrenia are more likely to have childhood trauma experiences and to have experienced more severe trauma compared with healthy controls, (2) patients with schizophrenia have lower plasma oxytocin levels than do healthy controls, (3) a positive correlation exists between the severity of childhood trauma and the severity of schizophrenia psychopathology, and (4) plasma oxytocin levels mediate the relationship between childhood trauma and the severity of schizophrenia psychopathology, with lower plasma oxytocin levels associated with more severe childhood trauma and psychopathology.
Methods
Participants and procedures
This cross-sectional study was conducted between August 2020 and April 2022. The study protocol was approved by the Joint Institutional Review Board of Taipei Medical University (Approval No. N202008006, dated August 19, 2020). All procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. All participants provided written informed consent. Patients with schizophrenia were recruited from the psychiatry outpatient clinic, and healthy controls were enrolled through advertisement. A total of 240 individuals joined the study: 160 patients with schizophrenia and 80 healthy controls matched by age and sex. All participants were aged 20–65 years and capable of providing written informed consent. The Structured Clinical Interview for DSM-536 was used as an interview guide by trained psychiatrists to assess diagnoses of any mental disorders for all participants. A patient with schizophrenia was included only if they (i) met the diagnosis criteria for schizophrenia and had been administered a stable dosage of antipsychotic treatment for at least 28 days and (ii) had no current or lifetime mental disorders except for schizophrenia spectrum disorder. Healthy controls were excluded if they or their first-degree relatives had a history of mental disorders. Any participant was excluded if they had a severe neurological disorder, epilepsy, intellectual disability, a neurocognitive disorder, history of substance use disorder, renal disease, or another severe, life-threatening medical condition. They were also excluded if they were pregnant, breastfeeding, or receiving hormonal therapy. No additional treatment was provided to any participant. The patients with schizophrenia received their treatment as usual after recruitment. All assessments were conducted in a private location. Blood tests were performed by nurses on the research team.
Childhood trauma
All participants were asked to complete the Childhood Trauma Questionnaire—Short Form (CTQ-SF37; to screen for and assess the severity of any childhood trauma. The CTQ-SF consists of 28 items and is scored on a 5-point scale. It measures five types of childhood trauma: emotional abuse, emotional neglect, physical abuse, physical neglect, and sexual abuse. The questionnaire has been translated into Chinese, with its reliability confirmed (Cronbach’s α = 0.57 to 0.90; intraclass coefficient = 0.67 to 0.8538. Participants who scored at or above the designated moderate exposure cutoff point on each subscale (specifically, ≥10 for physical abuse, ≥13 for emotional abuse, ≥8 for sexual abuse, ≥10 for physical neglect, and ≥15 for emotional neglect) were categorized as individuals with a documented history of childhood trauma exposure38. To enhance the validity of these self-reported scores, individual interviews were conducted with all participants. These interviews were carried out by trained psychiatrists following a structured protocol, where they delved deeper into the experiences indicated in the CTQ-SF. Participants were asked to elaborate on their responses, and the psychiatrists probed for specific details and examples of the reported experiences. This process was crucial to ascertain that the reported events met the criteria for childhood trauma as defined in our research context and to distinguish between actual trauma events and other negative, but non-traumatic, childhood experiences. For cross-validation, these detailed clarifications obtained during the interviews were used alongside the questionnaire responses.
Psychopathology
The Positive and Negative Syndrome Scale (PANSS) was used to evaluate the severity of the psychotic symptoms of patients with schizophrenia. The PANSS is a well-established and widely used scale consisting of 30 items and scored on a 7-point scale; it evaluates the positive, negative, and general psychopathological symptoms of schizophrenia39. Studies have demonstrated the robust psychometric properties of this instrument, including the favorable validity of the Chinese version40.
Oxytocin laboratory assessment
Given the challenges of directly measuring central oxytocin levels, we utilized plasma oxytocin levels in our study, informed by studies that identified a positive correlation between central and peripheral concentrations41. Phlebotomies were performed in the morning from 8am to 10am. All participants were instructed to abstain from tobacco, caffeine, and analgesics on the day of blood sampling to prevent interference with their plasma oxytocin levels42,43. The blood samples were maintained on ice until centrifugation at 3000 rpm for 15 min at 4 °C. Isolated plasma was then divided into 1-mL aliquots and stored at −80 °C immediately until the time of assay. Plasma oxytocin levels were determined using an enzyme immunosorbent assay kit (Catalog number: EKE-051-01, Phoenix Pharmaceuticals, Burlingame, CA, USA) with an oxytocin detection range of 0 to 100 ng/mL. Each plasma sample was assayed twice, and the mean of the two measurements was used in the analysis. We calculated the intra-assay coefficient of variation (CV) by assessing the variability in repeated measurements of the same sample within a single plate during a single run, using two random samples from each plate. The CV for each sample was determined by computing the standard deviation of the first and second results, then dividing this value by the duplicate mean, and finally multiplying by 100. The average CV of all these random samples was taken as the intra-assay CV. For the inter-assay CV, we gauged the variability in measurements of the same sample across different plates. We determined the plate means for the results of two random samples from different plates and then used these values to calculate the overall mean, standard deviation, and CV. The inter-assay and intra-assay coefficients of variation were both less than 5%, and no significant cross reactivity or interference between oxytocin and analogs was observed.
Covariates
Demographic characteristics, disease-specific variables, and cognitive function were added to the analysis as covariates, as they potentially influence the relationships between childhood trauma, oxytocin, and psychopathology. The inclusion of age and sex as confounders is based on their known influence on the onset, progression, and psychopathology of schizophrenia44,45, as well as their potential impact on plasma oxytocin levels46. Regarding disease-specific variables, the age of schizophrenia onset and illness duration were considered colliders of childhood trauma and plasma oxytocin levels47,48. Antipsychotics were recorded and converted into chlorpromazine-equivalent doses49, considering their established relevance in schizophrenia psychopathology and plasma oxytocin levels15,50. The Mini-Mental State Examination (MMSE) scores and years of education were included as confounders due to their potential impact on cognitive function, which may confound the relationship between childhood trauma and psychopathology51,52. The MMSE53 is a 21-item instrument with scores ranging from 0 to 30 to assess the following domains: orientation, registration and recall, attention and calculation, language, repetition, and the ability to follow written and verbal instructions. The decision to incorporate these covariates was informed by both empirical evidence and theoretical considerations, aiming to elucidate the complex interplay between these variables and the psychopathology of schizophrenia.
Statistical analysis
All collected data were transcribed in Microsoft Excel and then transferred to SPSS Statistics version 26.0 (IBM, Armonk, NY, USA) for coding and analysis. The normality of distributions was determined using the Kolmogorov–Smirnov test. The demographic characteristics, disease-specific variables, MMSE scores, plasma oxytocin levels, CTQ-SF scores, and PANSS scores are expressed as the mean (M) with standard deviation (SD). Independent sample t-tests were employed to compare continuous variables between the schizophrenia group and healthy controls, with Cohen’s d used to quantify effect size. The variables under comparison included demographic characteristics (age, sex, years of education, and MMSE score); plasma oxytocin levels; scores for each component of the CTQ-SF and the number of types of childhood trauma. Pearson’s chi-square test was applied to assess the categorical variable, namely, the prevalence of various types of childhood trauma among healthy controls and patients with schizophrenia, with effect sizes determined using Cramér’s V (φc). A series of one-way analyses of variance (ANOVAs) were employed to investigate the relationship between various types of childhood trauma and the severity of schizophrenia symptoms, as measured by the PANSS. Eta-squared (η2) was used to quantify the effect size for each ANOVA performed, providing a measure of the strength of the associations.
Pearson’s correlation coefficients were calculated to examine the correlations between psychopathology (measured by the PANSS total score, positive scale, negative scale, and general psychopathology scale) and other continuous variables, including plasma oxytocin levels, CTQ-SF score, demographic characteristics (sex, age, and years of education), disease-specific variables (age of schizophrenia onset, duration of illness, and antipsychotic dose), and MMSE score. Hierarchical regression analysis was used to investigate whether childhood trauma and plasma oxytocin levels accounted for unique variance in the psychopathology (measured by PANSS total score) of schizophrenia beyond that explained by other covariates (i.e., sex, age, years of education, age of schizophrenia onset, antipsychotic dose, and MMSE score). The covariates were included in the regression analysis model hierarchically in accordance with a time series. Finally, to explore the potential association between plasma oxytocin levels and the psychopathology (measured by PANSS total score) of schizophrenia, and how this might relate to childhood trauma, a mediation analysis was conducted using SPSS macro-PROCESS version 4.1 (model 4)54; after the data had been bias-corrected and percentile-method bootstrapped, with the data resampled 5,000 times. Exploratory analyses were performed to determine the best-fit model for the mediation analysis. The covariates incorporated into the mediation analysis were sex, age, years of education, age of schizophrenia onset, antipsychotic dose, and MMSE score. As the issue of multiple comparisons was present in this study, Bonferroni correction was applied to adjust the significance level. All probability values are reported at the two-tailed level for statistical significance at p < 0.05.
Results
Demographic characteristics, plasma oxytocin levels, childhood trauma, and psychopathology
The demographic characteristics and childhood trauma of the patients with schizophrenia and healthy controls are presented in Table 1. No significant differences between the two groups in terms of age and sex, but there was a significant difference in the years of education, with the schizophrenia group having lower years of education compared to the healthy group (t = −2.093, p = 0.038). All participants underwent the MMSE evaluation and were found to have normal cognitive function, with no intergroup differences being discovered. Figure 1 illustrates the distribution of plasma oxytocin levels in patients with schizophrenia compared to healthy controls. In comparison with the healthy controls, the patients with schizophrenia had significantly lower plasma oxytocin levels (t = −5.543, p < 0.001). The total scores in the CTQ-SF, as well as the scores in all the subscales, were higher for the patients with schizophrenia than for the healthy controls (p < 0.001). Comparison of the prevalence of different trauma types between healthy controls and patients with schizophrenia revealed a higher prevalence of all types of childhood trauma in the latter group: physical abuse (p < 0.001), emotional abuse (p = 0.004), sexual abuse (p = 0.008), physical neglect (p = 0.012), emotional neglect (p = 0.015), as well as a greater number of trauma types (p < 0.001). Table 1 provides information about the psychopathology and disease-specific variables of the patients with schizophrenia.
Table 1.
Demographic characteristics of patients with schizophrenia and healthy controls.
| Schizophrenia n = 160 | Healthy Controls n = 80 | Significance | |||||
|---|---|---|---|---|---|---|---|
| M | SD | M | SD | t/χ² | p | d/φc | |
| Age | 42.40 | 9.40 | 43.45 | 9.99 | −0.783 | 0.435 | −0.109 |
| Sex (male/female) | 96/64 | 46/34 | 0.710 | ||||
| Education years | 10.58 | 3.00 | 11.46 | 3.15 | −2.093 | 0.038 | −0.288 |
| MMSE score | 29.23 | 0.97 | 29.50 | 1.00 | −1.976 | 0.050 | −0.275 |
| Plasma oxytocin levels (ng/mL) | 14.34 | 3.07 | 17.26 | 4.49 | −5.543 | < 0.001 | −0.810 |
| CTQ-SF score | |||||||
| Total score | 60.59 | 14.18 | 38.00 | 4.32 | 13.917 | < 0.001 | 2.155 |
| Physical abuse | 13.59 | 5.00 | 7.16 | 1.66 | 11.175 | < 0.001a | 1.532 |
| Emotional abuse | 12.52 | 7.37 | 6.96 | 1.24 | 6.693 | < 0.001a | 0.917 |
| Sexual abuse | 6.98 | 3.25 | 5.19 | 0.55 | 4.881 | < 0 .001a | 0.669 |
| Physical neglect | 12.38 | 5.05 | 10.50 | 1.40 | 3.266 | 0.006a | 0.447 |
| Emotional neglect | 15.19 | 6.81 | 8.19 | 2.04 | 9.000 | < 0.001a | 1.230 |
| Positive for childhood trauma (n) | |||||||
| Physical abuse | 118 | 32 | 25.920 | < 0.001 | 0.329 | ||
| Emotional abuse | 71 | 20 | 8.505 | 0.004 | 0.188 | ||
| Sexual abuse | 39 | 8 | 6.998 | 0.008 | 0.171 | ||
| Physical neglect | 103 | 38 | 6.267 | 0.012 | 0.162 | ||
| Emotional neglect | 70 | 22 | 5.958 | 0.015 | 0.158 | ||
| Number of childhood trauma types | 2.51 | 1.90 | 1.50 | 1.35 | 4.725 | < 0.001 | 0.610 |
| Age of schizophrenia onset | 24.21 | 8.28 | |||||
| Duration of illness | 18.19 | 10.65 | |||||
| Antipsychotic dose (CPZ equiv. in mg) | 393.43 | 323.90 | |||||
| PANSS score | |||||||
| Total score | 76.22 | 17.22 | |||||
| Positive symptoms | 18.08 | 6.98 | |||||
| Negative symptoms | 19.91 | 8.05 | |||||
| General psychopathology | 33.99 | 7.54 | |||||
MMSE Mini-Mental Status Examination, CTQ-SF Childhood Trauma Questionnaire—Short Form, CPZ equiv. chlorpromazine equivalent doses, PANSS Positive and Negative Syndrome Scale.
aBonferroni-corrected p value.
Fig. 1.
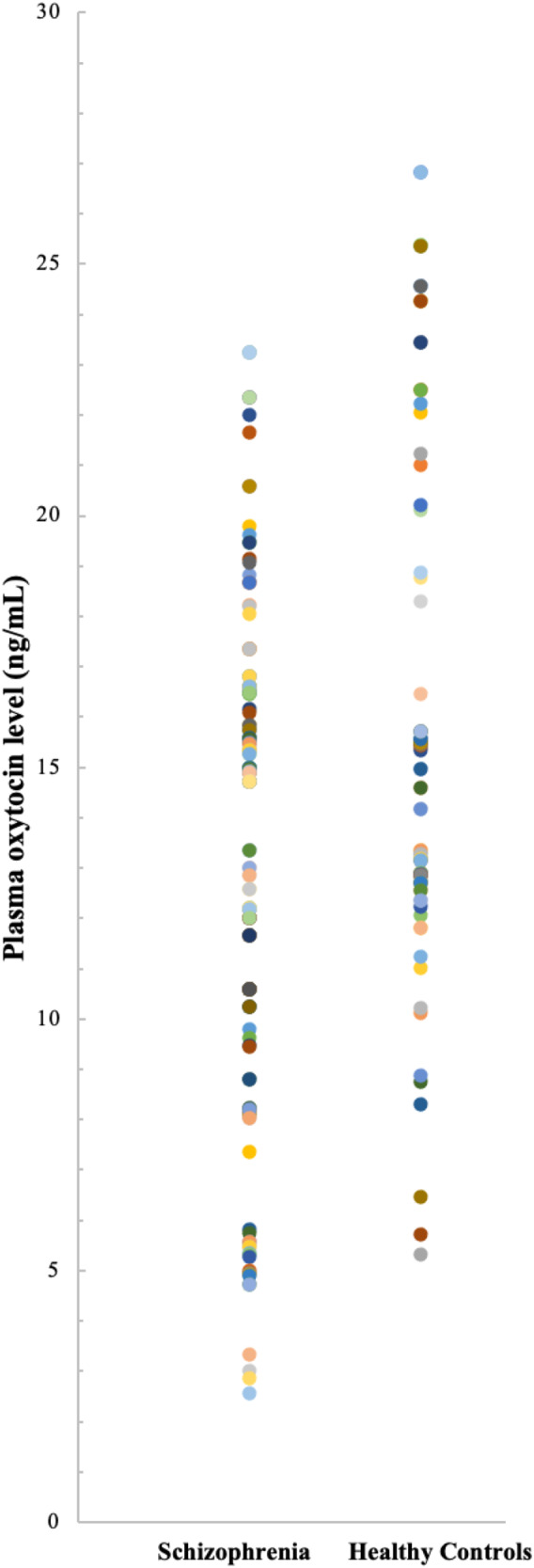
Distribution of plasma oxytocin levels between patients with schizophrenia and healthy controls.
Table 2 revealed significant associations between childhood trauma and PANSS scores among patients with schizophrenia. Patients who reported experiencing any form of childhood trauma—and who scored at or above the designated moderate exposure cutoff points on each subscale of the CTQ-SF, thus categorized as individuals with a documented history of childhood trauma exposure—consistently had higher PANSS total scores. This indicates more severe psychopathology compared to those without such childhood trauma history. Specifically, emotional abuse and emotional neglect were associated with the highest increases in PANSS total scores, as well as in scores for negative symptoms and general psychopathology. The effect sizes, as indicated by η2, ranged from moderate to large across different types of childhood trauma, with emotional neglect showing the most substantial impact on all measured aspects of the PANSS subdomains.
Table 2.
Comparison of psychopathology among patients with schizophrenia based on various childhood trauma types.
| PANSS | ||||||||
|---|---|---|---|---|---|---|---|---|
| Total score | Positive symptoms | Negative symptoms | General psychopathology | |||||
| M | SD | M | SD | M | SD | M | SD | |
| Physical abuse | ||||||||
| Yes (n = 118) | 81.50 | 14.79 | 19.07 | 6.51 | 21.89 | 7.82 | 36.08 | 6.83 |
| No (n = 42) | 61.38 | 14.84 | 15.31 | 7.55 | 14.33 | 5.79 | 28.12 | 6.27 |
| F(1, 158) = 57.219; p < 0.001; η2 = 0.266 | F(1, 158) = 9.466; p = 0.002; η2 = 0.057 | F(1, 158) = 32.750; p < 0.001; η2 = 0.172 | F(1, 158) = 43.914; p < 0.001; η2 = 0.217 | |||||
| Emotional abuse | ||||||||
| Yes (n = 71) | 89.77 | 8.98 | 20.73 | 6.32 | 24.59 | 7.78 | 39.51 | 5.35 |
| No (n = 89) | 65.40 | 14.32 | 15.97 | 6.78 | 16.17 | 6.09 | 29.60 | 5.98 |
| F(1, 158) = 156.345; p < 0.001; η2 = 0.497 | F(1, 158) = 20.715; p < 0.001; η2 = 0.116 | F(1, 158) = 59.031; p < 0.001; η2 = 0.272 | F(1, 158) = 118.865; p < 0.001; η2 = 0.429 | |||||
| Sexual abuse | ||||||||
| Yes (n = 39) | 89.05 | 9.69 | 20.41 | 6.90 | 24.67 | 7.98 | 38.85 | 5.16 |
| No (n = 121) | 72.08 | 17.10 | 17.33 | 6.86 | 18.37 | 7.48 | 32.43 | 7.53 |
| F(1, 158) = 34.701; p < 0.001; η2 = 0.180 | F(1, 158) = 5.924; p = 0.016; η2 = 0.036 | F(1, 158) = 20.218; p < 0.001; η2 = 0.113 | F(1, 158) = 24.525; p < 0.001; η2 = 0.134 | |||||
| Physical neglect | ||||||||
| Yes (n = 103) | 82.54 | 15.76 | 19.14 | 6.88 | 22.23 | 8.47 | 36.63 | 7.14 |
| No (n = 57) | 64.79 | 13.54 | 16.18 | 6.80 | 15.70 | 5.04 | 29.23 | 5.71 |
| F(1, 158) = 51.344; p < 0.001; η2 = 0.245 | F(1, 158) = 6.850; p = 0.010; η2 = 0.042 | F(1, 158) = 28.308; p < 0.001; η2 = 0.152 | F(1, 158) = 45.223; p < 0.001; η2 = 0.223 | |||||
| Emotional neglect | ||||||||
| Yes (n = 70) | 90.16 | 9.25 | 20.57 | 6.55 | 25.07 | 7.99 | 39.54 | 5.37 |
| No (n = 90) | 65.38 | 13.85 | 16.14 | 6.71 | 15.89 | 5.38 | 29.68 | 6.01 |
| F(1, 158) = 166.212; p < 0.001; η2 = 0.513 | F(1, 158) = 17.497; p < 0.001; η2 = 0.100 | F(1, 158) = 75.137; p < 0.001; η2 = 0.322 | F(1, 158) = 116.320; p < 0.001; η2 = 0.424 | |||||
Correlations between psychopathology and other variables
Correlation analysis within the schizophrenia cohort, as detailed in Table 3, indicated a significant correlation between the total CTQ-SF score and the total PANSS score (r = 0.699, p < 0.001). Additionally, all scores for the CTQ-SF subscales were significantly correlated with the total PANSS score and the scores for its subdomains scores, except for positive symptoms. Besides, the higher number of childhood trauma types experienced, the greater severity of schizophrenia psychopathology, measured by the total PANSS score (r = 0.738, p < 0.001) and the scores for its subdomains, namely positive symptoms (r = 0.843, p < 0.001), negative symptoms (r = 0.951, p < 0.001), and general psychopathology (r = 0.845, p < 0.001). Plasma oxytocin levels were inversely correlated with the total PANSS score (r = −0.688, p < 0.001) and the scores for its subdomains, except for positive symptoms.
Table 3.
Pearson’s correlation coefficients between childhood trauma and psychopathology in patients with schizophrenia.
| PANSS | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total score | Positive symptoms | Negative symptoms | General psychopathology | |||||||||
| r | r2 | pa | r | r2 | pa | r | r2 | pa | r | r2 | pa | |
| CTQ-SF score | ||||||||||||
| Total score | 0.699 | 0.489 | < 0.001 | 0.253 | 0.064 | 0.069 | 0.603 | 0.364 | < 0.001 | 0.639 | 0.408 | < 0.001 |
| Physical abuse | 0.654 | 0.428 | < 0.001 | 0.263 | 0.069 | 0.054 | 0.562 | 0.316 | < 0.001 | 0.581 | 0.338 | < 0.001 |
| Emotional abuse | 0.667 | 0.445 | < 0.001 | 0.230 | 0.053 | 0.192 | 0.559 | 0.312 | < 0.001 | 0.630 | 0.397 | < 0.001 |
| Sexual abuse | 0.302 | 0.091 | 0.006 | 0.015 | 0.000 | 1.000 | 0.357 | 0.127 | < 0.001 | 0.261 | 0.068 | 0.044 |
| Physical neglect | 0.588 | 0.346 | < 0.001 | 0.212 | 0.045 | 0.399 | 0.518 | 0.268 | < 0.001 | 0.540 | 0.292 | < 0.001 |
| Emotional neglect | 0.705 | 0.497 | < 0.001 | 0.282 | 0.080 | 0.057 | 0.582 | 0.339 | < 0.001 | 0.643 | 0.413 | < 0.001 |
| Number of childhood trauma types | 0.738 | 0.544 | < 0.001 | 0.843 | 0.710 | < 0.001 | 0.951 | 0.904 | < 0.001 | 0.845 | 0.714 | < 0.001 |
| Sex | −0.066 | 0.004 | 1.000 | −0.063 | 0.004 | 1.000 | −0.005 | 0.000 | 1.000 | −0.093 | 0.009 | 0.976 |
| Age | −0.085 | 0.007 | 1.000 | 0.029 | 0.000 | 1.000 | −0.097 | 0.009 | 0.888 | −0.104 | 0.011 | 0.768 |
| Education years | −0.136 | 0.018 | 0.348 | −0.032 | 0.001 | 1.000 | −0.107 | 0.011 | 0.708 | −0.133 | 0.018 | 0.376 |
| Age of schizophrenia onset | −0.160 | 0.026 | 0.172 | 0.009 | 0.000 | 1.000 | −0.203 | 0.041 | 0.040 | −0.162 | 0.026 | 0.164 |
| Duration of illness | 0.049 | 0.002 | 1.000 | 0.018 | 0.000 | 1.000 | 0.072 | 0.005 | 1.000 | 0.034 | 0.001 | 1.000 |
| Antipsychotic dose | 0.080 | 0.006 | 1.000 | 0.100 | 0.010 | 0.836 | 0.006 | 0.000 | 1.000 | 0.049 | 0.002 | 1.000 |
| MMSE score | −0.121 | 0.015 | 0.512 | 0.112 | 0.013 | 0.636 | −0.223 | 0.050 | 0.020 | −0.147 | 0.022 | 0.256 |
| Plasma oxytocin levels | −0.688 | 0.473 | < 0.001 | −0.161 | 0.026 | 0.168 | −0.646 | 0.417 | < 0 .001 | −0.647 | 0.419 | < 0.001 |
MMSE Mini-Mental Status Examination, CTQ-SF Childhood Trauma Questionnaire—Short Form, PANSS Positive and Negative Syndrome Scale.
aBonferroni-corrected p value.
Age of schizophrenia onset was discovered to have a negative association with the total PANSS score, negative symptoms, and general psychopathology; however, after applying the Bonferroni correction, this association remained significant only for negative symptoms (r = −0.203, p = 0.040), indicating that earlier onset is associated with more severe negative symptoms. Regarding the other variables, the correlations were nonsignificant except for a negative association between the MMSE score and negative symptoms (r = −0.223, p = 0.020).
Hierarchical regression analysis of predictors of psychopathology
The results of the hierarchical regression analysis are provided in Table 4. The variables were included in succeeding steps: (a) model 1 predicted psychopathology from only sex and age, (b) CTQ-SF score was added for model 2, (c) educational years was added for model 3, (d) age of schizophrenia onset was added for model 4, (e) antipsychotic dose and MMSE score was added for model 5, and (f) plasma oxytocin levels were added for model 6. The result of model 2 revealed that the CTQ-SF score served as a significant predictor of psychopathology, explaining 47.7% of the variation (ΔR2 = 0.477, p < 0.001). The result of model 6 demonstrated that oxytocin levels accounted for an additional 6.1% change in the prediction of psychopathology (ΔR2 = 0.052, p < 0.001). Additional hierarchical regression analyses predicting the PANSS subdomains scores were presented in Supplementary Table S1.
Table 4.
Hierarchical regression analysis of predictors of psychopathology (measured by PANSS total score) in patients with schizophrenia.
| R | R2 | ∆R2 | p | B | SE B | β | t | p | |
|---|---|---|---|---|---|---|---|---|---|
| Model 1 | 0.116 | 0.013 | 0.344 | ||||||
| Sex | −2.795 | 2.806 | −0.080 | −0.996 | 0.321 | ||||
| Age | −0.177 | 0.147 | −0.096 | −1.205 | 0.230 | ||||
| Model 2 | 0.701 | 0.491 | 0.477 | < 0.001 | |||||
| Sex | −1.683 | 2.025 | −0.048 | −0.831 | 0.407 | ||||
| Age | −0.028 | 0.106 | −0.015 | −0.261 | 0.795 | ||||
| CTQ-SF score | 0.496 | 0.041 | 0.696 | 12.091 | < 0.001 | ||||
| Model 3 | 0.707 | 0.499 | 0.009 | 0.102 | |||||
| Sex | −1.627 | 2.014 | −0.046 | −0.808 | 0.421 | ||||
| Age | −0.058 | 0.107 | −0.032 | −0.538 | 0.591 | ||||
| CTQ-SF score | 0.490 | 0.041 | 0.688 | 11.979 | < 0.001 | ||||
| Education years | −0.547 | 0.332 | −0.095 | −1.645 | 0.102 | ||||
| Model 4 | 0.711 | 0.506 | 0.007 | 0.153 | |||||
| Sex | −2.120 | 2.036 | −0.061 | −1.041 | 0.299 | ||||
| Age | −0.022 | 0.110 | −0.012 | −0.204 | 0.839 | ||||
| CTQ-SF score | 0.482 | 0.041 | 0.676 | 11.700 | < 0.001 | ||||
| Education years | −0.610 | 0.334 | −0.106 | −1.825 | 0.070 | ||||
| Age of schizophrenia onset | −0.182 | 0.126 | −0.087 | −1.436 | 0.153 | ||||
| Model 5 | 0.719 | 0.516 | 0.010 | 0.198 | |||||
| Sex | −2.077 | 2.037 | −0.059 | −1.020 | 0.310 | ||||
| Age | −0.016 | 0.110 | −0.008 | −0.142 | 0.888 | ||||
| CTQ-SF score | 0.477 | 0.041 | 0.670 | 11.582 | < 0.001 | ||||
| Education years | −0.652 | 0.336 | −0.113 | −1.939 | 0.054 | ||||
| Age of schizophrenia onset | −0.213 | 0.129 | −0.102 | −1.653 | 0.100 | ||||
| Antipsychotic dose | 0.005 | 0.003 | 0.101 | 1.745 | 0.083 | ||||
| MMSE score | −0.536 | 1.030 | −0.030 | −0.521 | 0.603 | ||||
| Model 6 | 0.754 | 0.569 | 0.052 | < 0.001 | |||||
| Sex | −2.015 | 1.931 | −0.057 | −1.043 | 0.298 | ||||
| Age | −0.030 | 0.104 | −0.016 | −0.290 | 0.772 | ||||
| CTQ-SF score | 0.294 | 0.058 | 0.413 | 5.078 | < 0.001 | ||||
| Education years | −0.351 | 0.326 | −0.061 | −1.074 | 0.285 | ||||
| Age of schizophrenia onset | −0.174 | 0.122 | −0.083 | −1.418 | 0.158 | ||||
| Antipsychotic dose | 0.005 | 0.003 | 0.095 | 1.732 | 0.085 | ||||
| MMSE score | 0.244 | 0.993 | 0.014 | 0.246 | 0.806 | ||||
| Plasma oxytocin levels | −62.896 | 14.733 | −0.359 | −4.269 | < 0.001 |
MMSE Mini-Mental Status Examination, CTQ-SF Childhood Trauma Questionnaire—Short Form, PANSS Positive and Negative Syndrome Scale.
Mediation effect of plasma oxytocin
Mediation analysis results, presented in Table 5, demonstrated a significant regression coefficient between childhood trauma and plasma oxytocin levels (p < 0.001), and between plasma oxytocin levels and the psychopathology of schizophrenia (p < 0.001). The bootstrapped unstandardized indirect effect was significant (β = 0.183, SE = 0.044, 95% confidence interval [CI] [0.102, 0.272]), indicating that plasma oxytocin levels partially mediate the effect of childhood trauma on the schizophrenia psychopathology. The regression coefficients remained robust when controlling for covariates presented in the study such as age, sex, years of education, MMSE score, age of schizophrenia onset, and antipsychotic dosage. The overall mediation model was significant (R2 = 0.517, F = 23.195, p < 0.001). Furthermore, additional analyses were conducted and presented in Supplementary Tables S2 and S3, where the correlations between PANSS scores and the number of childhood trauma types were examined, as well as their implications in hierarchical regression and mediation analysis. These analyses corroborated the initial findings that using total CTQ-SF scores, underscoring the robustness of the results. All exploratory analyses conducted to determine the best-fit model for the mediation analysis are presented in Supplementary Table S4.
Table 5.
Mediation effect of plasma oxytocin levels on the relationship between childhood trauma and psychopathology (measured by PANSS total score) in patients with schizophrenia.
 | ||||||
|---|---|---|---|---|---|---|
| Model summary | ||||||
| R | R2 | MSE | F | p | ||
| Model 4 | 0.719 | 0.517 | 150.014 | 23.195 | < 0.001 | |
| Covariates: sex, age, year of education, MMSE score, age of schizophrenia onset, antipsychotic dose. | ||||||
| Mediation Estimates | ||||||
|---|---|---|---|---|---|---|
| Effect | Estimate | SE | 95% CI | % Mediation | ||
| Indirect | 0.183 | 0.044 | [0.102, 0.272] | 38.36 | ||
| Direct | 0.294 | 0.058 | [0.180, 0.409] | 61.64 | ||
| Total | 0.477 | 0.041 | [0.400, 0.559] | 100.00 | ||
| Path Estimates | ||||||
|---|---|---|---|---|---|---|
| Estimate | SE | t | pa | |||
| CTQ-SF score | → | Oxytocin levels | −0.003 | 0.001 | −13.522 | < 0.001 |
| Oxytocin levels | → | PANSS total score | −62.896 | 14.733 | −4.269 | < 0.001 |
| CTQ-SF score | → | PANSS total score | 0.295 | 0.058 | 5.079 | < 0.001 |
MMSE Mini-Mental Status Examination, CTQ-SF Childhood Trauma Questionnaire—Short Form, PANSS Positive and Negative Syndrome Scale.
aBonferroni-corrected p value.
Discussion
The results of this study indicated that any childhood trauma experienced by the participants was more severe on average in the patients with schizophrenia than in the healthy controls, as reflected in the significant difference between CTQ-SF scores and in the prevalence of positive responses for various types of childhood trauma. The patients with schizophrenia also had lower oxytocin levels, which is consistent with our hypothesis and supports the idea that oxytocinergic system dysfunction is associated with schizophrenia. We further investigated the link between childhood trauma and psychopathology severity in patients with schizophrenia, determining a positive correlation between these two variables; plasma oxytocin levels were inversely correlated with both factors. To provide new insights into these associations, we examined the role of oxytocin through mediation analysis. After controlling for covariates, oxytocin was found to exert a partial mediation effect on the relationship between childhood trauma and the psychopathology of schizophrenia.
Our findings align with the existing literature indicating that patients with schizophrenia experience more severe childhood trauma, which is substantiated by both the higher CTQ-SF total scores and the increased prevalence of all trauma types in this population, with the existence of potential threshold and dose–response effects55–58. This observed gradation in childhood trauma severity and its association with the spectrum of schizophrenia symptoms highlight the intricacy of trauma’s impact on the disorder. Our findings reveal that a categorical approach to assessing childhood trauma—classifying individuals based on whether their experiences meet a certain threshold of severity—aligns with heightened positive symptoms in schizophrenia. In contrast, our correlation analysis did not show a direct relationship between the continuous severity of childhood trauma and positive symptoms. Our results may suggest that while childhood trauma, in general, is associated with an exacerbation of psychopathology, the specific relationship with positive symptoms may become more pronounced only after surpassing a certain threshold of trauma severity. This nuanced effect is in line with the notion that various trauma subtypes may influence the development of schizophrenia to differing extents, highlighting the potential for threshold effects in the trauma-psychopathology nexus, as supported by a meta-analysis indicating that all trauma subtypes may confer a substantial risk of psychosis4. The significant correlation between the number of childhood trauma types and the severity of psychopathology in our schizophrenia cohort further reinforces the concept of a dose-response relationship, where a greater number of trauma experiences correlates with more severe symptoms of the disorder59,60. Such severity may trigger a series of neurobiological changes, including HPA axis dysregulation, genetic vulnerabilities, and epigenetic modifications, contributing to the altered brain structure and function observed in schizophrenia61.
The interplay between childhood trauma and schizophrenia is multifaceted, with research suggesting that the dissociative states stemming from adversity could amplify cognitive deficits. Such deficits may blur the distinction between internal thoughts and external reality, potentially leading to hallucinations. These hallucinations may manifest as a variation of posttraumatic intrusive memories62 or emerge from errors in source monitoring63,64. Notably, auditory verbal hallucinations have been linked to these cognitive challenges in discerning internal from external auditory information, a difficulty that may be exacerbated by dissociative states induced by childhood trauma65–67, and potentially related to oxytocinergic system dysfunctions68. Furthermore, delusions, particularly those connected to trauma-induced negative beliefs, can arise from a compromised ability to form secure attachments due to childhood negligence, fostering distrust and paranoia. This attachment failure and the ensuing paranoia may be moderated by genetic factors, including polymorphisms in the oxytocin receptor gene69,70. Moreover, attachment style has been implicated in the development of negative symptoms71,72, with poor attachment possibly leading to interpersonal dysfunction. This dysfunction has been hypothesized as an adaptive deactivation of the attachment system in response to the fear of rejection or threat73, further complicating the clinical presentation of schizophrenia. These findings are consistent with evidence linking various trauma subtypes to schizophrenia, particularly to negative symptoms and general psychopathology. However, our results indicate that the association with positive symptoms is less pronounced, a finding that diverges from some studies emphasizing the childhood trauma-positive symptom connection58,74, yet aligns with others that have found a stronger link between childhood trauma, especially neglectful trauma, and negative symptoms75–77.
Building on this, the nuances in the relationships between specific childhood trauma types and schizophrenia symptoms become evident. Although sexual abuse was found to have a weaker association with schizophrenia in our study, it is essential to consider the broader context of research. For instance, the literature presents mixed evidence on sexual abuse’s connection with schizophrenia, with some studies indicating a particular association with positive symptoms, while others do not find a strong link to negative symptoms78–81. This variability suggests that positive and negative symptoms may emerge through distinct pathways related to the impact of sexual abuse. Furthermore, the potential for underreporting of sexual abuse due to stigma, guilt, or embarrassment82, as well as the dissociative amnesia83, introduces additional challenges in assessing the true strength of these associations. Such complexities underscore the need for a careful examination of how different childhood trauma experiences contribute to the heterogeneity of schizophrenia’s symptomatology.
Our study contributes to the growing body of literature that posits the oxytocinergic system as a potential mediator in the pathway from childhood trauma to the development of schizophrenia. This study introduces a potential new explanation for the trajectory from childhood trauma to schizophrenia, with oxytocin possibly playing a significant role. However, the intricate mechanisms through which childhood trauma disrupts the oxytocinergic system are still an area of active exploration. The disruption of early attachment processes, which are intricately linked to oxytocin regulation, appears to be a contributing factor to the emergence of negative symptoms and general psychopathology84–86. The resulting alteration in oxytocin levels might influence key neural pathways, including those involving oxytocin’s interaction with dopaminergic pathways, regulation of the amygdala, and adjustment of social information processing87, which provide potential explanations for our observations. Indeed, oxytocin dysregulation could exacerbate social cognitive deficits, potentially leading to enhanced paranoia, social withdrawal, and comorbid affective disorders, as evidenced by our findings and supported by recent studies27,88,89. This proposition aligns with our observation that oxytocin levels are associated with various symptom domains of schizophrenia.
Furthermore, initial molecular insights suggest that the impact of childhood trauma may extend to the genetic regulation of oxytocin production and receptor expression90, potentially via epigenetic modifications like DNA methylation91 or single nucleotide polymorphisms92, both of which can induce stress-related pathology93. This genetic vulnerability, compounded by adverse environmental exposures, may contribute to a ‘gene × environment’ interplay that underpins the schizophrenia phenotype. While oxytocin’s role in this complex interplay is significant, it is likely not the sole mediator. Our study echoes the broader schizophrenia research that implicates factors such as chronic stress and systemic inflammation as additional contributing elements to the psychopathology61,94. As such, our findings underscore the need for a multifactorial approach to understand the full scope of schizophrenia’s etiology and pathophysiology, considering both neurobiological and environmental influences.
To our knowledge, this is the first study to explore oxytocin’s mediating role in the relationship between childhood trauma and schizophrenia. However, the findings must be interpreted cautiously due to the study’s limitations. The retrospective nature of the CTQ-SF raises concerns about recall bias and potential underreporting of childhood trauma95, although prior research supports the validity of retrospective reporting96. We attempted to minimize bias by conducting interviews to clarify and validate participant responses. Nevertheless, future research employing mediation analyses and a prospective design would be invaluable in confirming the mediating role of oxytocin. Oxytocin levels are subject to various influences, such as stress, inflammation, circadian rhythm, nicotine use97, and reproductive status46, which could act as uncontrolled confounders. We have attempted to control for some of these by excluding nicotine use, pregnancy, breastfeeding, hormonal therapy, and menstruation from our participant criteria. We requested that participants refrain from tobacco use on the day of blood sampling. We also ensured that blood sampling did not occur during menstruation. Additionally, the potential influence of antipsychotic medication on oxytocin levels should be considered. Furthermore, while we standardized antipsychotic dosages to chlorpromazine-equivalent doses, the lack of differentiation between antipsychotic types is a limitation given their distinct effects on oxytocin levels. Subsequent studies should differentiate between antipsychotic classes to better understand their impact on oxytocin and schizophrenia. Furthermore, assessing oxytocin levels both before and after antipsychotic treatment would be instrumental in better understanding the dynamic between medication and oxytocin regulation in schizophrenia. Moreover, while peripheral oxytocin levels correlate with central levels41, they are not a perfect substitute. Direct measurements of central oxytocin remain impractical, posing a challenge for accurately assessing its role in schizophrenia. Additionally, our study specifically included participants with schizophrenia who had been on stable medication for at least 28 days to minimize the confounding effects of fluctuating medication levels on oxytocin levels and psychopathology. While this approach was aimed at strengthening the internal validity of our findings, it may also have inadvertently introduced a selection bias. By selecting more clinically stable participants, our findings may not fully represent the broader schizophrenia population, particularly those not on consistent medication regimens or those with additional comorbidities. This could potentially limit the generalizability of our results to all cases of schizophrenia. The cross-sectional design also means we cannot establish causal links or account for variations in trauma timing98. Despite these limitations, we constructed mediation models based on the assumption of oxytocin’s stability over time, aiming to elucidate its relationship with psychopathology of schizophrenia. Future longitudinal studies are necessary to confirm these relationships over time. Our study underscores the significance of oxytocin in understanding the biological impact of childhood trauma on schizophrenia, highlighting the need for further investigation into the genetic factors that may affect oxytocin regulation following trauma. Identifying specific genetic variants linked to schizophrenia susceptibility could provide valuable insights for therapeutic interventions. Future clinical trials might consider including individuals with a history of childhood trauma or those with suboptimal oxytocin levels to discern who might benefit most from oxytocin supplementation.
Conclusion
Childhood trauma is recognized a major risk factor in the development of schizophrenia. In this cross-sectional study, we delved into the underlying mechanisms, examining the role of oxytocin in mediating the effects of childhood trauma on the development of schizophrenia. Consistent with prior research, our findings confirm a positive correlation between childhood trauma and the severity of schizophrenia, as well as an inverse correlation between oxytocin levels and these variables. Significantly, our findings suggest that oxytocin partially mediates the relationship between childhood trauma and the clinical manifestations of schizophrenia, indicating the childhood trauma may potentially led to oxytocin dysregulation, which in turn could increase the clinical severity of schizophrenia. These insights reinforce the crucial need for preventive measures, early recognition, and targeted interventions in schizophrenia, particularly in individuals with a history of childhood trauma. The potential of oxytocin as a therapeutic avenue for alleviating symptoms offers a promising direction for future clinical research and treatment strategies in schizophrenia.
Supplementary information
Acknowledgements
The authors gratefully acknowledge Prof. Ming-Chyi Huang for providing the Chinese Version of Childhood Trauma Questionnaire-Short Form. This manuscript was edited by Wallace Academic Editing. This study was supported by Wan-Fang Hospital, Taipei Medical University (grant numbers 111-wf-eva-21, 112-wf-eva-31, TMU111-AE1-B22) in Taipei City, Taiwan; the National Science and Technology Council (grant numbers MOST110-2314-B-038-072-MY3, MOST110-2314-B-038-073, and MOST111-2314-B-038-065-MY3) in Taipei City, Taiwan; and the Higher Education Sprout Project by the Ministry of Education (grant number DP2-TMU-112-N-08) in Taipei City, Taiwan. The funding sponsors had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, and in the decision to publish the results.
Author contributions
Yuan-Jung Chen: Data curation, Formal analysis, Writing—original draft, Writing—review & editing. Mong-Liang Lu: Conceptualization, Investigation, Formal analysis, Validation, Resources, Supervision. Yi-Hang Chiu: Investigation, Validation, Resources, Supervision. Chenyi Chen: Methodology, Validation, Resources, Supervision. Vitor Hugo Jesus Santos: Validation, Writing—review & editing. Kah Kheng Goh: Conceptualization, Methodology, Formal analysis, Investigation, Data curation, Validation, Writing—original draft, Writing—review & editing, Visualization, Funding acquisition.
Data availability
Supplementary information is available for this paper. The datasets generated during and/or analyzed during this study are available from the corresponding author upon reasonable request.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
The online version contains supplementary material available at 10.1038/s41537-024-00433-9.
References
- 1.Trotta A, Murray RM, Fisher HL. The impact of childhood adversity on the persistence of psychotic symptoms: a systematic review and meta-analysis. Psychol. Med. 2015;45:2481–2498. doi: 10.1017/S0033291715000574. [DOI] [PubMed] [Google Scholar]
- 2.Read J, van Os J, Morrison AP, Ross CA. Childhood trauma, psychosis and schizophrenia: a literature review with theoretical and clinical implications. Acta Psychiatr. Scand. 2005;112:330–350. doi: 10.1111/j.1600-0447.2005.00634.x. [DOI] [PubMed] [Google Scholar]
- 3.Matheson SL, Shepherd AM, Pinchbeck RM, Laurens KR, Carr VJ. Childhood adversity in schizophrenia: a systematic meta-analysis. Psychol. Med. 2013;43:225–238. doi: 10.1017/S0033291712000785. [DOI] [PubMed] [Google Scholar]
- 4.Varese F, et al. Childhood adversities increase the risk of psychosis: a meta-analysis of patient-control, prospective- and cross-sectional cohort studies. Schizophr. Bull. 2012;38:661–671. doi: 10.1093/schbul/sbs050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Morgan C, et al. Threat, hostility and violence in childhood and later psychotic disorder: population-based case-control study. Br. J. Psychiatry. 2020;217:575–582. doi: 10.1192/bjp.2020.133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.İngeç C, Evren Kılıçaslan E. The effect of childhood trauma on age of onset in patients with schizophrenia. Int. J. Soc. Psychiatry. 2020;66:763–769. doi: 10.1177/0020764020943629. [DOI] [PubMed] [Google Scholar]
- 7.Li XB, et al. Childhood trauma associates with clinical features of schizophrenia in a sample of Chinese inpatients. Psychiatry Res. 2015;228:702–707. doi: 10.1016/j.psychres.2015.06.001. [DOI] [PubMed] [Google Scholar]
- 8.Akbey ZY, Yildiz M, Gündüz N. Is there any association between childhood traumatic experiences, dissociation and psychotic symptoms in schziophrenic patients? Psychiatry Investig. 2019;16:346–354. doi: 10.30773/pi.2019.02.10.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bailey T, et al. Childhood trauma is associated with severity of hallucinations and delusions in psychotic disorders: a systematic review and meta-analysis. Schizophr. Bull. 2018;44:1111–1122. doi: 10.1093/schbul/sbx161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hjelseng IV, et al. Childhood trauma is associated with poorer social functioning in severe mental disorders both during an active illness phase and in remission. Schizophr. Res. 2022;243:241–246. doi: 10.1016/j.schres.2020.03.015. [DOI] [PubMed] [Google Scholar]
- 11.Aas M, et al. A systematic review of cognitive function in first-episode psychosis, including a discussion on childhood trauma, stress, and inflammation. Front. Psychiatry. 2014;4:182. doi: 10.3389/fpsyt.2013.00182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Misiak B, Frydecka D. A history of childhood trauma and response to treatment with antipsychotics in first-episode schizophrenia patients: preliminary results. J. Nerv. Ment. Dis. 2016;204:787–792. doi: 10.1097/NMD.0000000000000567. [DOI] [PubMed] [Google Scholar]
- 13.Mohammadzadeh A, Azadi S, King S, Khosravani V, Sharifi Bastan F. Childhood trauma and the likelihood of increased suicidal risk in schizophrenia. Psychiatry Res. 2019;275:100–107. doi: 10.1016/j.psychres.2019.03.023. [DOI] [PubMed] [Google Scholar]
- 14.Froemke RC, Young LJ. Oxytocin, neural plasticity, and social behavior. Annu. Rev. Neurosci. 2021;44:359–381. doi: 10.1146/annurev-neuro-102320-102847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rich ME, Caldwell HK. A role for oxytocin in the etiology and treatment of schizophrenia. Front. Endocrinol. (Lausanne) 2015;6:90. doi: 10.3389/fendo.2015.00090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Goh KK, Chen CH, Lane HY. Oxytocin in schizophrenia: pathophysiology and implications for future treatment. Int. J. Mol. Sci. 2021;22:2146. doi: 10.3390/ijms22042146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ferreira AC, Osório FL. Peripheral oxytocin concentrations in psychiatric disorders—a systematic review and methanalysis: Further evidence. Prog. Neuropsychopharmacol. Biol. Psychiatry. 2022;117:110561. doi: 10.1016/j.pnpbp.2022.110561. [DOI] [PubMed] [Google Scholar]
- 18.Strauss GP, et al. Plasma oxytocin levels predict olfactory identification and negative symptoms in individuals with schizophrenia. Schizophr. Res. 2015;162:57–61. doi: 10.1016/j.schres.2014.12.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kéri S, Kiss I, Kelemen O. Sharing secrets: oxytocin and trust in schizophrenia. Soc. Neurosci. 2009;4:287–293. doi: 10.1080/17470910802319710. [DOI] [PubMed] [Google Scholar]
- 20.Goldman M, Marlow-O’Connor M, Torres I, Carter CS. Diminished plasma oxytocin in schizophrenic patients with neuroendocrine dysfunction and emotional deficits. Schizophr. Res. 2008;98:247–255. doi: 10.1016/j.schres.2007.09.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Strauss GP, et al. Plasma oxytocin levels predict social cue recognition in individuals with schizophrenia. Schizophr. Res. 2015;162:47–51. doi: 10.1016/j.schres.2015.01.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.De Coster L, Lin L, Mathalon DH, Woolley JD. Neural and behavioral effects of oxytocin administration during theory of mind in schizophrenia and controls: a randomized control trial. Neuropsychopharmacology. 2019;44:1925–1931. doi: 10.1038/s41386-019-0417-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Modabbernia A, et al. Intranasal oxytocin as an adjunct to risperidone in patients with schizophrenia : an 8-week, randomized, double-blind, placebo-controlled study. CNS Drugs. 2013;27:57–65. doi: 10.1007/s40263-012-0022-1. [DOI] [PubMed] [Google Scholar]
- 24.Zheng W, et al. Adjunctive intranasal oxytocin for schizophrenia: A meta-analysis of randomized, double-blind, placebo-controlled trials. Schizophr. Res. 2019;206:13–20. doi: 10.1016/j.schres.2018.12.007. [DOI] [PubMed] [Google Scholar]
- 25.Feifel D, Shilling PD, MacDonald K. A review of oxytocin’s effects on the positive, negative, and cognitive domains of schizophrenia. Biol. Psychiatry. 2016;79:222–233. doi: 10.1016/j.biopsych.2015.07.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Erdozain AM, Peñagarikano O. Oxytocin as treatment for social cognition, not there yet. Front. Psychiatry. 2019;10:930. doi: 10.3389/fpsyt.2019.00930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Goh, K. K., Kanahara, N., Chiu, Y. H. & Lu, M. L. The impact of childhood trauma exposure on social functioning in schizophrenia: the moderated mediation role of oxytocin and oxytocin receptor gene polymorphisms. Psychol. Med. 1–13. 10.1017/s003329172300274x (2023). [DOI] [PubMed]
- 28.Bradley ER, Woolley JD. Oxytocin effects in schizophrenia: reconciling mixed findings and moving forward. Neurosci. Biobehav. Rev. 2017;80:36–56. doi: 10.1016/j.neubiorev.2017.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.De Bellis MD, Zisk A. The biological effects of childhood trauma. Child Adolesc. Psychiatr. Clin. N. Am. 2014;23:185–222. doi: 10.1016/j.chc.2014.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Opacka-Juffry J, Mohiyeddini C. Experience of stress in childhood negatively correlates with plasma oxytocin concentration in adult men. Stress. 2012;15:1–10. doi: 10.3109/10253890.2011.560309. [DOI] [PubMed] [Google Scholar]
- 31.Heim C, et al. Lower CSF oxytocin concentrations in women with a history of childhood abuse. Mol. Psychiatry. 2009;14:954–958. doi: 10.1038/mp.2008.112. [DOI] [PubMed] [Google Scholar]
- 32.Seltzer LJ, Ziegler T, Connolly MJ, Prososki AR, Pollak SD. Stress-induced elevation of oxytocin in maltreated children: evolution, neurodevelopment, and social behavior. Child Dev. 2014;85:501–512. doi: 10.1111/cdev.12136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mizuki R, Fujiwara T. Association of oxytocin level and less severe forms of childhood maltreatment history among healthy Japanese adults involved with child care. Front. Behav. Neurosci. 2015;9:138. doi: 10.3389/fnbeh.2015.00138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Donadon MF, Martin-Santos R, Osório FL. The associations between oxytocin and trauma in humans: a systematic review. Front. Pharmacol. 2018;9:154. doi: 10.3389/fphar.2018.00154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ebbert AM, Infurna FJ, Luthar SS, Lemery-Chalfant K, Corbin WR. Examining the link between emotional childhood abuse and social relationships in midlife: the moderating role of the oxytocin receptor gene. Child Abuse Negl. 2019;98:104151. doi: 10.1016/j.chiabu.2019.104151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.First, M. B., Williams, J. B., Karg, R. S. & Spitzer, R. L. SCID-5-CV: Structured Clinical Interview for DSM-5 Disorders: Clinician Version (American Psychiatric Association Publishing, 2016).
- 37.Bernstein DP, et al. Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse Neglect. 2003;27:169–190. doi: 10.1016/s0145-2134(02)00541-0. [DOI] [PubMed] [Google Scholar]
- 38.Cheng Y-C, Chen C-H, Chou K-R, Kuo P-H, Huang M-C. Reliability and factor structure of the chinese version of childhood trauma questionnaire-short form in patients with substance use disorder. Taiwanese J. Psychiatry. 2018;32:52–62. [Google Scholar]
- 39.Kay SR, Fiszbein A, Opler LA. The Positive and Negative Syndrome Scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13:261–276. doi: 10.1093/schbul/13.2.261. [DOI] [PubMed] [Google Scholar]
- 40.Cheng JJ, Ho H, Chang C-J, Lan S-Y, Hwu H-G. Positive and Negative Syndrome Scale (PANSS): establishment and reliability study of a Mandarin Chinese language version. Taiwanese J. Psychiatry. 1996;10:251–258. [Google Scholar]
- 41.Valstad M, et al. The correlation between central and peripheral oxytocin concentrations: a systematic review and meta-analysis. Neurosci. Biobehav. Rev. 2017;78:117–124. doi: 10.1016/j.neubiorev.2017.04.017. [DOI] [PubMed] [Google Scholar]
- 42.Wu L, et al. Caffeine inhibits hypothalamic A(1)R to excite oxytocin neuron and ameliorate dietary obesity in mice. Nat. Commun. 2017;8:15904. doi: 10.1038/ncomms15904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zhang KM, et al. Nicotine enhances GABAergic inhibition of oxytocin mRNA-expressing neuron in the hypothalamic paraventricular nucleus in vitro in rats. Neurosci. Lett. 2017;638:5–11. doi: 10.1016/j.neulet.2016.12.005. [DOI] [PubMed] [Google Scholar]
- 44.Häfner H, Maurer K, Löffler W, Riecher-Rössler A. The influence of age and sex on the onset and early course of schizophrenia. Br. J. Psychiatry. 1993;162:80–86. doi: 10.1192/bjp.162.1.80. [DOI] [PubMed] [Google Scholar]
- 45.Castle D, Sham P, Murray R. Differences in distribution of ages of onset in males and females with schizophrenia. Schizophr. Res. 1998;33:179–183. doi: 10.1016/s0920-9964(98)00070-x. [DOI] [PubMed] [Google Scholar]
- 46.Marazziti D, et al. Sex-related differences in plasma oxytocin levels in humans. Clin. Pract. Epidemiol. Ment. Health. 2019;15:58–63. doi: 10.2174/1745017901915010058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hogg B, et al. Psychological trauma as a transdiagnostic risk factor for mental disorder: an umbrella meta-analysis. Eur. Arch. Psychiatry Clin. Neurosci. 2023;273:397–410. doi: 10.1007/s00406-022-01495-5. [DOI] [PubMed] [Google Scholar]
- 48.Rubin LH, et al. Peripheral oxytocin and vasopressin are associated with clinical symptom severity and cognitive functioning in midlife women with chronic schizophrenia. Schizophr. Res. 2018;195:409–411. doi: 10.1016/j.schres.2017.09.041. [DOI] [PubMed] [Google Scholar]
- 49.Woods SW. Chlorpromazine equivalent doses for the newer atypical antipsychotics. J. Clin. Psychiatry. 2003;64:663–667. doi: 10.4088/jcp.v64n0607. [DOI] [PubMed] [Google Scholar]
- 50.Kiss A, Osacka J. The effect of amisulpride, olanzapine, quetiapine, and aripiprazole single administration on c-Fos expression in vasopressinergic and oxytocinergic neurons of the rat hypothalamic paraventricular nucleus. Neuropeptides. 2021;87:102148. doi: 10.1016/j.npep.2021.102148. [DOI] [PubMed] [Google Scholar]
- 51.Ong HL, et al. Performance of Mini-Mental State Examination (MMSE) in long-stay patients with schizophrenia or schizoaffective disorders in a psychiatric institute. Psychiatry Res. 2016;241:256–262. doi: 10.1016/j.psychres.2016.04.116. [DOI] [PubMed] [Google Scholar]
- 52.Talreja BT, Shah S, Kataria L. Cognitive function in schizophrenia and its association with socio-demographics factors. Ind. Psychiatry J. 2013;22:47–53. doi: 10.4103/0972-6748.123619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”: a practical method for grading the cognitive state of patients for the clinician. J. Psychiatric Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 54.Hayes, A. F. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-based Approach 3rd edn, 732 (Guilford publications, 2022).
- 55.Mall S, et al. The relationship between childhood trauma and schizophrenia in the Genomics of Schizophrenia in the Xhosa people (SAX) study in South Africa. Psychol. Med. 2020;50:1570–1577. doi: 10.1017/S0033291719001703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kelleher I, et al. Childhood trauma and psychosis in a prospective cohort study: cause, effect, and directionality. Am. J. Psychiatry. 2013;170:734–741. doi: 10.1176/appi.ajp.2012.12091169. [DOI] [PubMed] [Google Scholar]
- 57.De-Nardin EMS, Muratori CA, Ribeiro IS, Huguete RB, Salgado JV. Childhood trauma is associated with onset of symptoms, functioning and cognition in patients with schizophrenia. Trends Psychiatry Psychother. 2022;44:e20190081. doi: 10.47626/2237-6089-2019-0081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Liu J, et al. Adverse childhood experiences and positive psychotic symptoms: a nationally representative study in Singapore. Child Abuse Negl. 2022;131:105778. doi: 10.1016/j.chiabu.2022.105778. [DOI] [PubMed] [Google Scholar]
- 59.Croft J, et al. Association of Trauma Type, Age of Exposure, and Frequency in Childhood and Adolescence With Psychotic Experiences in Early Adulthood. JAMA Psychiatry. 2019;76:79–86. doi: 10.1001/jamapsychiatry.2018.3155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Pruessner M, et al. Impact of childhood trauma on positive and negative symptom remission in first episode psychosis. Schizophr Res. 2021;231:82–89. doi: 10.1016/j.schres.2021.02.023. [DOI] [PubMed] [Google Scholar]
- 61.Popovic D, et al. Childhood trauma in schizophrenia: current findings and research perspectives. Front. Neurosci. 2019;13:274–274. doi: 10.3389/fnins.2019.00274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Garety PA, Kuipers E, Fowler D, Freeman D, Bebbington PE. A cognitive model of the positive symptoms of psychosis. Psychol. Med. 2001;31:189–195. doi: 10.1017/s0033291701003312. [DOI] [PubMed] [Google Scholar]
- 63.Brookwell ML, Bentall RP, Varese F. Externalizing biases and hallucinations in source-monitoring, self-monitoring and signal detection studies: a meta-analytic review. Psychol. Med. 2013;43:2465–2475. doi: 10.1017/S0033291712002760. [DOI] [PubMed] [Google Scholar]
- 64.Waters F, Woodward T, Allen P, Aleman A, Sommer I. Self-recognition deficits in schizophrenia patients with auditory hallucinations: a meta-analysis of the literature. Schizophr Bull. 2012;38:741–750. doi: 10.1093/schbul/sbq144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Perona-Garcelán S, et al. Dissociative experiences as mediators between childhood trauma and auditory hallucinations. J. Trauma Stress. 2012;25:323–329. doi: 10.1002/jts.21693. [DOI] [PubMed] [Google Scholar]
- 66.Varese F, Barkus E, Bentall RP. Dissociation mediates the relationship between childhood trauma and hallucination-proneness. Psychol. Med. 2012;42:1025–1036. doi: 10.1017/S0033291711001826. [DOI] [PubMed] [Google Scholar]
- 67.Varese F, Udachina A, Myin‐Germeys I, Oorschot M, Bentall RP. The relationship between dissociation and auditory verbal hallucinations in the flow of daily life of patients with psychosis. Psychosis. 2011;3:14–28. [Google Scholar]
- 68.Lee H, King AP, Li Y, Seng JS. Oxytocin receptor gene, post-traumatic stress disorder and dissociation in a community sample of European American women. BJPsych Open. 2022;8:e104. doi: 10.1192/bjo.2022.74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Sitko K, Bentall RP, Shevlin M, O’Sullivan N, Sellwood W. Associations between specific psychotic symptoms and specific childhood adversities are mediated by attachment styles: an analysis of the National Comorbidity Survey. Psychiatry Res. 2014;217:202–209. doi: 10.1016/j.psychres.2014.03.019. [DOI] [PubMed] [Google Scholar]
- 70.Zheng S, et al. Oxytocin Receptor Gene (OXTR) and Childhood Adversity Influence Trust. Psychoneuroendocrinology. 2020;121:104840. doi: 10.1016/j.psyneuen.2020.104840. [DOI] [PubMed] [Google Scholar]
- 71.van Dam DS, Korver-Nieberg N, Velthorst E, Meijer CJ, de Haan L. Childhood maltreatment, adult attachment and psychotic symptomatology: a study in patients, siblings and controls. Soc. Psychiatry Psychiatr. Epidemiol. 2014;49:1759–1767. doi: 10.1007/s00127-014-0894-0. [DOI] [PubMed] [Google Scholar]
- 72.Degnan A, Berry K, Humphrey C, Bucci S. The role of attachment and dissociation in the relationship between childhood interpersonal trauma and negative symptoms in psychosis. Clin. Psychol. Psychother. 2022;29:1692–1706. doi: 10.1002/cpp.2731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Liotti, G. & Gumley, A. In Psychosis, Trauma and Dissociation: Emerging Perspectives on Severe Psychopathology 117–133 (Wiley Blackwell, 2008).
- 74.Bentall RP, Wickham S, Shevlin M, Varese F. Do specific early-life adversities lead to specific symptoms of psychosis? A study from the 2007 the Adult Psychiatric Morbidity Survey. Schizophr. Bull. 2012;38:734–740. doi: 10.1093/schbul/sbs049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Pruessner M, et al. Gender differences in childhood trauma in first episode psychosis: Association with symptom severity over two years. Schizophr. Res. 2019;205:30–37. doi: 10.1016/j.schres.2018.06.043. [DOI] [PubMed] [Google Scholar]
- 76.Struck N, et al. Childhood maltreatment and adult mental disorders—the prevalence of different types of maltreatment and associations with age of onset and severity of symptoms. Psychiatry Res. 2020;293:113398. doi: 10.1016/j.psychres.2020.113398. [DOI] [PubMed] [Google Scholar]
- 77.Mansueto, G. et al. Childhood adversity, symptoms, and cortisol in first episode psychosis: a cross-sectional, secondary, observational analysis of a subsample of FEP patients. Nord. J. Psychiatry77, 432–439 (2023). [DOI] [PubMed]
- 78.Hailes HP, Yu R, Danese A, Fazel S. Long-term outcomes of childhood sexual abuse: an umbrella review. Lancet Psychiatry. 2019;6:830–839. doi: 10.1016/S2215-0366(19)30286-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Werbeloff N, et al. Childhood sexual abuse in patients with severe mental Illness: demographic, clinical and functional correlates. Acta Psychiatr. Scand. 2021;143:495–502. doi: 10.1111/acps.13302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Read J, Agar K, Argyle N, Aderhold V. Sexual and physical abuse during childhood and adulthood as predictors of hallucinations, delusions and thought disorder. Psychol. Psychother. 2003;76:1–22. doi: 10.1348/14760830260569210. [DOI] [PubMed] [Google Scholar]
- 81.Chae S, Sim M, Lim M, Na J, Kim D. Multivariate analysis of relationship between childhood trauma and psychotic symptoms in patients with schizophrenia. Psychiatry Investig. 2015;12:397–401. doi: 10.4306/pi.2015.12.3.397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Friedman T, Tin NN. Childhood sexual abuse and the development of schizophrenia. Postgrad. Med. J. 2007;83:507–508. doi: 10.1136/pgmj.2006.054577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Khosravi M, Bakhshani NM, Kamangar N. Dissociation as a causal pathway from sexual abuse to positive symptoms in the spectrum of psychotic disorders. BMC Psychiatry. 2021;21:266. doi: 10.1186/s12888-021-03290-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Scatliffe N, Casavant S, Vittner D, Cong X. Oxytocin and early parent-infant interactions: a systematic review. Int. J. Nurs. Sci. 2019;6:445–453. doi: 10.1016/j.ijnss.2019.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Sharma SR, Gonda X, Dome P, Tarazi FI. What’s Love Got to do with it: Role of oxytocin in trauma, attachment and resilience. Pharmacol. Ther. 2020;214:107602. doi: 10.1016/j.pharmthera.2020.107602. [DOI] [PubMed] [Google Scholar]
- 86.Ludmer JA, et al. Association between maternal childhood maltreatment and mother-infant attachment disorganization: moderation by maternal oxytocin receptor gene and cortisol secretion. Horm. Behav. 2018;102:23–33. doi: 10.1016/j.yhbeh.2018.04.006. [DOI] [PubMed] [Google Scholar]
- 87.Ellenbogen MA. Oxytocin and facial emotion recognition. Curr. Top. Behav. Neurosci. 2018;35:349–374. doi: 10.1007/7854_2017_20. [DOI] [PubMed] [Google Scholar]
- 88.Millan MJ, Bales KL. Towards improved animal models for evaluating social cognition and its disruption in schizophrenia: the CNTRICS initiative. Neurosci. Biobehav. Rev. 2013;37:2166–2180. doi: 10.1016/j.neubiorev.2013.09.012. [DOI] [PubMed] [Google Scholar]
- 89.Goh KK, Lu ML. Relationship between the domains of theory of mind, social dysfunction, and oxytocin in schizophrenia. J. Psychiatr. Res. 2022;155:420–429. doi: 10.1016/j.jpsychires.2022.09.013. [DOI] [PubMed] [Google Scholar]
- 90.Uhrig S, et al. Reduced oxytocin receptor gene expression and binding sites in different brain regions in schizophrenia: a post-mortem study. Schizophr. Res. 2016;177:59–66. doi: 10.1016/j.schres.2016.04.019. [DOI] [PubMed] [Google Scholar]
- 91.Ramo-Fernández L, et al. Associations between childhood maltreatment and DNA methylation of the oxytocin receptor gene in immune cells of mother-newborn dyads. Transl. Psychiatry. 2021;11:449. doi: 10.1038/s41398-021-01546-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Julian MM, et al. Associations between oxytocin receptor gene (OXTR) polymorphisms, childhood trauma, and parenting behavior. Dev. Psychol. 2019;55:2135–2146. doi: 10.1037/dev0000783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Kraaijenvanger EJ, et al. Epigenetic variability in the human oxytocin receptor (OXTR) gene: a possible pathway from early life experiences to psychopathologies. Neurosci. Biobehav. Rev. 2019;96:127–142. doi: 10.1016/j.neubiorev.2018.11.016. [DOI] [PubMed] [Google Scholar]
- 94.Wang L, et al. The mediating effect of brain-derived neurotrophic factor levels on childhood trauma and psychiatric symptoms in patients with first-episode schizophrenia. Aust. N. Z. J. Psychiatry. 2022;56:828–835. doi: 10.1177/00048674211031478. [DOI] [PubMed] [Google Scholar]
- 95.Baldwin JR, Reuben A, Newbury JB, Danese A. Agreement between prospective and retrospective measures of childhood maltreatment: a systematic review and meta-analysis. JAMA Psychiatry. 2019;76:584–593. doi: 10.1001/jamapsychiatry.2019.0097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Scott KM, McLaughlin KA, Smith DA, Ellis PM. Childhood maltreatment and DSM-IV adult mental disorders: comparison of prospective and retrospective findings. Br. J. Psychiatry. 2012;200:469–475. doi: 10.1192/bjp.bp.111.103267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Zanos P, et al. Region-specific up-regulation of oxytocin receptor binding in the brain of mice following chronic nicotine administration. Neurosci. Lett. 2015;600:33–37. doi: 10.1016/j.neulet.2015.05.054. [DOI] [PubMed] [Google Scholar]
- 98.Teicher MH, Samson JA, Anderson CM, Ohashi K. The effects of childhood maltreatment on brain structure, function and connectivity. Nat. Rev. Neurosci. 2016;17:652–666. doi: 10.1038/nrn.2016.111. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Supplementary information is available for this paper. The datasets generated during and/or analyzed during this study are available from the corresponding author upon reasonable request.


