Abstract
Objectives
This study reviewed existing recommendations for virtual mental healthcare services through the quadruple aim framework to create a set of recommendations on virtual healthcare delivery to guide the development of Canadian policies on virtual mental health services.
Design
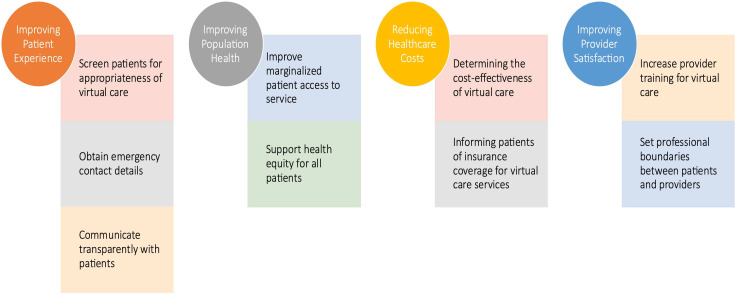
We conducted a systematic rapid review with qualitative content analysis of data from included manuscripts. The quadruple aim framework, consisting of improving patient experience and provider satisfaction, reducing costs and enhancing population health, was used to analyse and organise findings.
Methods
Searches were conducted using seven databases from 1 January 2010 to 22 July 2022. We used qualitative content analysis to generate themes.
Results
The search yielded 40 articles. Most articles (85%) discussed enhancing patient experiences, 55% addressed provider experiences and population health, and 25% focused on cost reduction. Identified themes included: screen patients for appropriateness of virtual care; obtain emergency contact details; communicate transparently with patients; improve marginalised patients’ access to care; support health equity for all patients; determine the cost-effectiveness of virtual care; inform patients of insurance coverage for virtual care services; increase provider training for virtual care and set professional boundaries between providers and patients.
Conclusions
This rapid review identified important considerations that can be used to advance virtual care policy to support people living with mental health conditions in a high-income country.
Keywords: MENTAL HEALTH, PSYCHIATRY, Health Services Accessibility, Primary Care
STRENGTHS AND LIMITATIONS OF THIS STUDY.
Extraction of data on virtual healthcare from a wide range of sources that were analysed using the quadruple aim framework.
Engagement of people with lived experience with mental illness in study design.
Recommendations for patient/provider experience and population health.
Omission of non-English resources and research discussing asynchronous care.
‘Rapid’ nature of review may have left some pertinent resources unexplored.
Introduction
Virtual delivery of ambulatory healthcare became widespread in high-income countries after the onset of the COVID-19 pandemic, and its adoption has been sustained, even as guidance recommending its use has evolved. ‘Virtual care’ can be defined as ‘any interaction between patients and/or members of their circle of care, occurring remotely, using any forms of communication or information technologies, with the aim of facilitating or maximising the quality and effectiveness of patient care’.1 In Canada, there was an overall 56-fold increase in the use of virtual care, comprising 71% of primary care visits in the first months of the COVID-19 pandemic.2 Similarly, in international settings, there has been a 38-fold increased volume of virtual care in healthcare, when compared with prepandemic use.3 Furthermore, this increased volume has persisted, years after the pandemic onset.4
Although there has been a steady return to in-person care due to vaccination and other public health measures decreasing the risk of severe COVID-19 disease, virtual delivery has become the default modality for many health concerns, particularly mental health. Mental health concerns are common; about 20% of people will have a mental health issue in any given year.5 In most settings, primary care is the first point of access for mental health services,6 and common mental illnesses such as anxiety and depression are the most frequent conditions for which people seek out primary care services.7 8 Virtual care has been reported to be as accurate from a diagnostic perspective for simple diagnoses not requiring in-person physical examinations,9 but there is limited evidence about the diagnostic accuracy or effectiveness virtual care delivery related to mental health conditions.
Despite the rapid and sustained proliferation of virtual care across healthcare settings, there has been no attempt to bring together existing recommendations and peer-reviewed guidelines for virtual care delivery of mental health services. The quadruple aim is an established health quality framework that includes the following pillars: improving patient and caregiver experiences, reducing costs, supporting population health and improving provider experiences.10 It has been used in health services research to determine the priorities of different populations within the healthcare setting,11 12 but to our knowledge, has not been used to understand virtual care recommendations in high-income settings. For this reason, we conducted a rapid review to identify recommendations for virtual delivery of mental health services to adults in high-income countries, using the quadruple aim to guide our analysis and synthesis of the results.
Methods
We used rapid review methodology to search for, review and organise mental health standards from international sources. A rapid review is a form of knowledge synthesis that accelerates the process of conducting a traditional systematic review through streamlining or omitting specific methods to produce evidence for stakeholders in a resource-efficient manner. We chose this over a traditional systematic or scoping review because we wanted to quickly generate evidence that could be used in a policy-making process to develop national standards for virtual delivery of mental health services in Canadian primary care; this manuscript reports results of the first phase of that rapid-cycle project,13 which subsequently went on to conduct focus groups and interviews and extensive policy review to generate a list of standards. We followed Cochrane Methods Rapid Reviews guidance14 as well as Tricco et al’s specific recommendations for conducting rapid reviews related to the COVID-19 pandemic.15 Our rapid literature review was conducted in line with the principles outlined in,16 as there is currently no dedicated reporting checklist specifically tailored for rapid reviews. In order to uphold a thorough and transparent reporting process, we aligned our reporting with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. We employed the PRISMA checklist17 to ensure all pertinent sections and topics were included and also reported the checklist for the abstract. (Checklist can be found in online supplemental appendices A and B).
bmjopen-2023-079244supp001.pdf (64.4KB, pdf)
bmjopen-2023-079244supp002.pdf (24.8KB, pdf)
Our overall aim was to identify recommendations for virtual delivery of mental health services to adults in high-income countries. Within the literature, virtual mental healthcare services are referred to using a variety of terms, including but not limited to: telemental health, telepsychiatry and psychiatric telehealth. In this manuscript, we use the term ‘virtual mental health services’, which we define as, ‘ …the use of telecommunications […such as telephones…] or videoconferencing technology to provide mental health services’.18
We initially focused on synchronous care, where the patient and provider are meeting in real time.19 We searched for peer-reviewed literature to identify guidance and recommendations for virtual mental health in primary care settings. We did not limit the search regarding specific mental health conditions. References had to make specific recommendations for virtual healthcare services in ambulatory settings such as psychiatry, family medicine and/or primary care. We intentionally kept the inclusion criteria broad and included resources that did not necessarily relate exclusively to primary care because our initial discussions and preliminary exploration of the literature suggested that we may miss relevant resources if we limited exclusively to primary care. We excluded resources focused exclusively on substance use disorder diagnosis and management. We excluded resources related exclusively to asynchronous care that is self-directed and mobile health (also known as ‘mhealth’) wearable technologies. In line with rapid review methodology, we did not conduct a risk of bias assessment of included studies. In addition, the search was limited to high-income countries to maximise the generalisability to the Canadian healthcare setting. Detailed inclusion/exclusion criteria are available in table 1.
Table 1.
Inclusion/exclusion criteria for review
| Inclusion | Exclusion |
|
|
Our search strategy was developed in collaboration with an information specialist at Unity Health Toronto on our team (CZ). We included English-language articles, from both peer-reviewed and grey literature, from any country on the World Bank list identified as high-income countries.17 We started with a systematic formalised database search of seven databases from 1 January 2010 to 22 July 2022: All Medline (via Ovid), PsycINFO (Ovid), Embase (Ovid), Scopus, Cochrane Central Register of Controlled Trials and Cochrane Database of Systematic Reviews (EBM Reviews Ovid) and CINAHL (EBSCO host). We limited our search to resources published on or after 1 January 2010 because we assessed that limiting to this more recent literature would provide insights more likely to be generalisable to contemporary technologies. Our team included clinicians, researchers, people with lived experience of mental illness, from multiple Canadian provinces and the UK. The information specialist (CZ) performed the database searches (online supplemental appendix C), compiled and deduplicated the results in EndNote.
bmjopen-2023-079244supp003.pdf (6.5MB, pdf)
Article selection process
We used Covidence review management software to enable reviewer pairs to screen articles. Title and abstract screening were conducted by two independent reviewers (LL and NE). If an abstract or summary was available, the reviewer conducted a brief full-text screening to assess eligibility. Any disagreement encountered in eligibility was resolved through discussion with a third reviewer (BO’N). Two independent reviewers (NE and AY) conducted full-text screening of each potentially relevant resource, and disagreements in eligibility were resolved through consensus with a third reviewer (BO’N).
Data extraction
Once full-text articles were identified from the database searches, two team members’ extracted data using a data extraction template which was tested and refined through team discussion and trialled with five previously identified resources. We extracted data related to author and year, authors’ location; specific setting in which the study was conducted/to which the guidelines or recommendations applied; study description; provider type; whether people with lived experience were involved in generation of recommendations; and the text of recommendations or guidance according to aspects of the quadruple aim (improving patient experience; improving population health; reducing costs; improving provider experience).10
Analysis and synthesis approach
We conducted directed content analysis of data extracted from included manuscripts.20 We used the quadruple aim as our initial categorisation matrix.21 Two authors (NE and AY) read included manuscripts and extracted excerpts of text from the manuscripts that were related to each aspect of the quadruple aim. This was completed independently in parallel, and then three authors (NE, AY and BO’N) met and reviewed the excerpts together. Then one author (NE) reviewed each excerpt and generated codes from the textual excerpts, and then combined these into subcategories. Then, NE and BO’N met to review the subcategories and combined them into the ‘themes’ that are represented in the results section of this manuscript. Throughout this process, we discussed the emerging ‘themes’ at two project meetings, where multiple authors discussed the analysis and proposed slight alterations to the phrases or words used to describe particular phenomena. For example, we replaced ‘special populations’, a description of a theme related to data extracted under quadruple aim 2 (‘improving population health’) with ‘equity-deserving groups’ in the first instance and then further modified this to ‘marginalised populations’.
Patient and public involvement
Two people with lived experience of mental health concerns (EA and another team member who chose not to be identified) were members of the study team and involved in a series of team meeting where we developed and approved the research question and search keywords. As themes were being developed, findings were regularly reviewed with the study team, which at that point included one person with lived experience of mental health concerns (EA) who provided substantive input on the final themes.
Results
The primary search strategy identified 2760 records (online supplemental appendix C). Of these, 106 full-text articles were screened and 40 articles met the eligibility criteria and were included in the analysis (figure 1).
Figure 1.
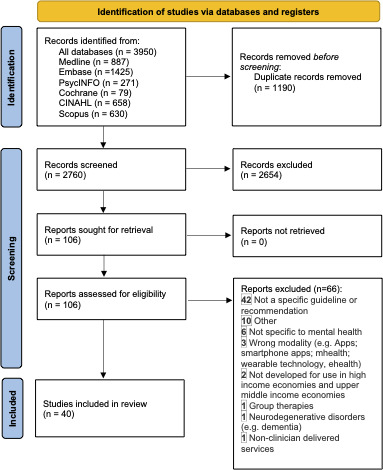
PRISMA flow diagram. PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
Included articles were published mostly in the USA (n=24; 60%), followed by other countries: Canada (n=2, 5%), South Africa (n=2, 5%), the UK (n=2, 5%), China (n=1, 2.5%), Poland (n=1, 2.5%), Australia (n=1, 2.5%) Switzerland (n=1, 2.5) and Qatar.1 Five articles (12.5%) did not specify a country of origin.
Most articles described the setting to which their recommendations or guidance applied in general terms as ‘virtual mental healthcare’ (n=29, 72.5%) or the ‘mental health sector’ (n=1, 2.5%) A few were more specific about the setting, such as a psychiatry clinic (n=2, 5%), geriatrics clinic (n=1, 2.5%), neuropsychology clinic (n=1, 2.5%) or a prison (n=1, 2.5%). One article described that it was applicable to ‘virtual mental healthcare during COVID-19 outbreaks’ (n=1, 2.5%). Two articles were focused on specific populations served by specialised clinics: one for people with bipolar disorder (n=1, 2.5%) and one for deaf patients (n=1, 2.5%).
With respect to the type of healthcare professional to which recommendations or guidance applied, 14 articles described this as for ‘clinicians/healthcare professionals’ in general (n=14, 35%). Eight articles were for psychologists (n=8, 20%). Four were focused on ‘mental health clinicians/practitioners/providers (10%). Three were for physicians (7.5%) and three for psychiatrists (7.5%). Two articles were for psychotherapists (5%), two for nurse practitioners (5%) and two for primary care providers (5%). One article was for counsellors (2.5%), one for neuropsychologists (2.5%) and one for social workers (2.5%). One article did not have any description of the type of healthcare provider to which it was applicable (2.5%) (in total, this adds to >40 articles because several articles described multiple types of healthcare providers).
Online supplemental appendix D shows the extracted data from all included studies. None of the included manuscripts reported that they had any patient or caregiver involvement in the development of guidelines or recommendations, so we did not include this in the table.
bmjopen-2023-079244supp004.pdf (168.8KB, pdf)
The themes extracted for each quadruple aim are summarised in figure 2.
Figure 2.
Recommendations from reviewed literature in context of quadruple aim domains.
Quadruple aim 1: improving patient and caregiver experience
34 articles (85%) were found to have information related to quadruple aim 1. From data extracted related to this aim, we identified three themes:
Screen patients for appropriateness of virtual care (n=30, 75%).
Obtain emergency contact details (n=5, 12.5%).
Communicate transparently with patients (n=8, 20%).
Screen patients for appropriateness of virtual care
22 (52.5%) articles described the importance of, or methods for, assessing before virtual appointments to evaluate whether virtual care is a viable, useful method of care delivery for a patient’s particular needs.22–43 For example, one article described the importance of establishing a ’relationship’ between healthcare providers and patients to assess virtual care appropriateness23; another three articles noted that patients generally have a positive view of psychological screening assessments conducted prior to a virtual visit.24–27
Three articles (7.5%) listed criteria that providers should assess prior to a first virtual visit including: healthcare services the patient requires, resources available to providers and what is required for sustainable longitudinal care.28–30 One article suggested providers should also assess how their patients perceive their conditions,31 and four (n=7.5%) recommended asking what patients wish to gain from their appointment(s).32–35
Two articles (5%) noted that providers should assess potential risks of using virtual care for each patient, and whether providers and patients have appropriate technology for virtual appointments and patients’ cognitive capacity to consent to virtual care.36 37 Three articles (7.5%) recommended providers should assess if patients have a safe environment to attend a virtual healthcare appointment.36 38 39 One article noted that sensory deficiencies, particularly visual and auditory, can impede patient capacity to engage in videocalls.40 Three articles (7.5%) noted that the most important consideration is whether patients want a virtual appointment or not.32 41–43
Obtain emergency contact details
Three articles (7.5%) mentioned the importance of emergency contacts for verifying the patient’s location, both to assess whether care could be provided in the context of licensure in that particular jurisdiction (for state licensure requirements) and for having knowledge on where to dispatch emergency services if a crisis were to happen during a virtual appointment.44–46 Two articles (5%) discussed the need for providers to engage in safety planning, such as what to do in case of self-harm, with their patient and document the plan, including emergency contacts, immediately after an initial appointment.47 48
Communicate transparently with patients
Eight articles (20%) emphasised the need for transparent communication between patients and providers. One article stated generally that ethical and professional standards of care and practice should be maintained by psychologists throughout appointments.41 Five articles described that whether patients want to continue with virtual care after initially using it should be assessed on an ongoing basis, and the modality changed if requested.49–53 Two articles (5%) highlighted the importance of healthcare providers explicitly informing patients of the steps they take ensure confidentiality of their sessions.54 55
Quadruple aim 2: improving population health
27 articles (67.5%) had information related to quadruple aim 2. Two major themes were identified:
Improve marginalised patients’ access to care (n=22, 52%).
Support health equity for all patients (n=8, 20%).
Improve marginalised patients’ access to care
22 included articles (52%) focused on improving marginalised patients’ access to care, noting that technology has the potential to expand patient access to mental health services. Fourteen of these articles (35%) stated that virtual mental health services can facilitate patients’ access to necessary services that they might not otherwise have, such as those living in rural areas where many lack access included articles (52%) focused on improving accessibility, noting that technology has the potential to expand patient access to mental health services. Fourteen articles (35%) also stated that virtual mental health services can facilitate patients' access to necessary services that they might not otherwise have, such as those living in rural areas where many lack access to in-person mental health therapy, or for individuals living with limited mobility or disability.22 25 28 30 36 38 39 41 46 47 52 55–57
Three articles (7.5%) noted virtual care could be useful for people who have diagnoses or for whom symptoms of their diagnoses might preclude attending in-person visits,37 42 including the provision of psychotherapy and education for patients with severe personality disorders.53 Four articles (10%) noted that using telepsychiatry to deliver mental health treatments could alleviate the provider shortage, having a direct impact on access to care.24 26 44 51 Stigma was also highlighted by one of the articles as a barrier to receiving care and that virtual modalities might ease access to care by reducing stigma experienced by patients accessing virtual services, through not having to go to a public place such as a hospital or clinic.35
Support health equity for all patients
Another theme explored was supporting marginalised populations, those for whom access to (in-person) mental healthcare is limited for some reason, in achieving health equity. For example, one article (2.5%) noted that virtual modalities can aid in providing deaf communities in the USA with services that are linguistically and culturally appropriate.50
One article (2.5%) highlighted the ability of telepsychiatry to minimise health inequalities and contribute to health equality by reaching communities who would otherwise go unserved.56 Another discussed problems related to the ‘digital divide’ and how telepsychiatry cannot reach its therapeutic and equity-promoting potential if patients in need do not have access to or know how to use the internet.43
Three articles (7.5%) described how virtual modalities could support the availability of mental health services through facilitating care from existing providers into new settings such as prisons26 27 29 and one noted that a population of veterans preferred virtual mental healthcare due to stigma surrounding mental health within that community.35 One article (2.5%) noted the importance of tailoring safety plans to specific situations such as geographical or jurisdictional area,45 since there might be unique challenges related to specific marginalised populations.
Quadruple aim 3: reducing costs
10 articles (25%) had information related to quadruple aim 3. Two major themes were identified:
Determine the cost-effectiveness of virtual care (n=7, 17.5%).
Informing patients of insurance coverage for virtual care services (n=3, 7.5%).
Determine the cost-effectiveness of virtual care
Seven articles (17.5%) discussed whether virtual care could be cost-effective. One (2.5%) described telemedicine as more cost-effective compared with in-person appointments, because it reduces patient-level costs related to time and travel for attending appointments.36 Another article (2.5%) reported that online psychotherapy could lower healthcare expenses for clients, therapists and society since it is reportedly cost-effective, although they did not provide specific figures.38 Two articles suggested that virtual care could somehow reduce long waiting lists for face-to-face therapy, because a single therapist may be able to see more patients, and that this could result in greater cost effectiveness with more patients served for the same number of staff.38 50
In one article (2.5%), virtual mental healthcare was linked to lower healthcare expenditures per capita because more patients with mental illnesses could receive more effective care which could result in fewer hospitalisations.27 Two articles (5%) on peer support interventions for social isolation and depression reported that virtual delivery required less clinician time, lowering per capita healthcare costs.36 51 Another article about a telepsychiatry programme in prisons in the USA described between US$12 000 and US$1 million in cost savings after the implementation of remote programmes.58 A review of virtual care visits across several countries reported a lower no-show rate than in-person visits.42
Inform patients of insurance coverage for virtual care services
Three articles (7.5%) noted the importance for patients to know what virtual care services were and were not covered in their specific setting; one of these articles also noted the importance for providers to understand how virtual care is dealt with in their compensation model.55 A review article of international literature from during the COVID-19 pandemic described the importance of patients having access to clear information about what their insurance covers regarding virtual mental healthcare,43 since this often differs from what in-person services are covered. One article from Poland noted in that country, virtual visits are paid the same as in-person visits, as long as they are not being used inappropriately in place of a needed in-person assessment.59
Quadruple aim 4: improving provider experience
22 articles (55%) had information related to quadruple aim 4. We identified two major themes:
Increase provider training for virtual care (n=10, 25%).
Set professional boundaries between providers and patients (n=15, 37.5%).
Increase provider training for virtual care
Ten articles (22.5%) focused on providing training for virtual care. Seven articles (17.5%) recommended that staff receive proper training and adopt an understanding and individualised communication approach.22 23 27 41–43 52 Two articles (5%) reported that providers should strengthen their communication skills by enrolling in training courses or programmes.57 60 Another article (2.5%) noted the importance of physical comfort for providers, to avoid weariness and issues related to prolonged computer use.40
Set professional boundaries between providers and patients
Fifteen articles (37.5%) described the importance of scheduling and anticipated response times related to appointment booking and requests for urgent and or/asynchronous care. Eight articles (20%) noted that because virtual care can theoretically be provided at any time of day, it is essential for patients to have unambiguous information about the provider or service’s working hours.28–30 38 44 48 59 60 Five articles (12.5%) recommended that providers and patients set a contract around an ‘anticipated response time’ related to when a patient reaches out to a provider, when they should expect a response, at the start of their clinical relationship.33 34 38 46 49 Four articles (10%) described the importance of a personalised and empathetic communication style was emphasised across multiple articles.27 43 54 60 One article (2.5%) recommended providers avoid discussions about aspects related to life outside the clinical setting.60
Discussion
Our rapid review found that articles describing mental health-based virtual services and standards offered a wide range of recommendations for practitioners. Our team condensed these recommendations into nine independent guidelines that can be used to inform Canadian policy as well as future research on the logistics of virtual healthcare services.
We used the quadruple aim to extract data and then conducted directed content analysis using those extracted data. Our content analysis approach identified several important concepts related to virtual care for mental health, such as the extent to which it can enhance health equity, and the importance of establishing agreements or understanding between patients and providers about the expected time between a patient contacting a healthcare provider and their response. We found that many articles included in our manuscript were vague with respect to what discipline they related to (eg, 14 articles reported that they were targeting ‘clinicians’ or ‘healthcare professionals’ in general).
Overall, we found that there were fewer articles addressing the extent to which virtual care could reduce costs, in comparison with the number of articles reporting recommendations about improving patient and caregiver experience, improving population health or improving provider experiences. One article noted that although much research seems to portray a positive view of the cost-effectiveness of telehealth, less research is available evaluating the cost-effectiveness of virtual mental health.61
Various other quadruple aim-based health services studies have shared similar findings. For example, in one article assessing the quadruple aim in the context of patient portals, researchers reported that providers had worries about implementing this new technology into their practices and how this may challenge provider boundaries, particularly if patients expected that this new technology would require providers to respond to their messages constantly and immediately.12 Other articles evaluating the potential of virtual mental health services post-COVID-19 have also focused on themes not unlike our results, such as the importance of developing and providing sufficient virtual mental health training for healthcare providers.62 63 One article63 emphasised that whatever virtual mental health guidelines and standards are developed should be customised for different disciplines.
The quadruple aim suggests that healthcare systems and institutions should work to improve population health and the ‘patient experience of care’,10 among other things. Surprisingly, although almost all of our included manuscripts reporting standards for virtual mental healthcare provided recommendations related to improving either population health or patient experience, only one article reported patient inclusion or feedback within their work.45 Instead, they reported what researchers and providers believed to be best for their patients, based on their own experiences. Although other research has been done assessing patients’ opinions on virtual health services,64 65 or satisfaction after using these services,66 very little has been published reporting patients’ opinions on virtual mental health services. Additionally, while we focused our search on ‘synchronous’ delivery of virtual mental health services, many included articles also described the importance of and recommendations for asynchronous virtual mental healthcare such as emails and text messages between patients and providers. Our team previously examined what virtual mental health services are included in provincial health coverage in Canadian settings and determined that in almost all cases, only synchronous care was included67; the emphasis we identified in this review on asynchronous care suggests that there is interest in a more diverse basket of services being available. Future research in this area should explore patients’ experiences with and the effectiveness of all virtual care modalities.
Many articles praised the potential of virtual mental healthcare to improve the care for marginalised populations, such as those living rurally, or who may have limitations due to mobility.64 Others cautioned that other parts of the population may be easily left behind in a provirtual mental healthcare era; some of these populations include patients with low internet access or poor technological literacy.68–70 Throughout high-income country settings, virtual delivery of mental health services has become a core part of the health system; although there were some questions of whether there would be a diminution of the use of virtual care as the public health concerns related to the COVID-19 pandemic resolved, it is apparent that virtual modalities are a core aspect of the ‘new normal’.3 A key takeaway from this research is the need for high-quality guidelines to support and guide for virtual mental healthcare; these could be used to guide development of provider training and influence policy decisions about resource allocation. Above all, we found that research on the implications for virtual care has emphasised the need for it to be effective, safe for participants, timely, efficient, patient-centred and equitable.
Our work expands on other resources developed by provincial, territorial and federal healthcare associations on how to incorporate virtual care into mental healthcare-based settings and could be used to further guide policy development on virtual mental healthcare. For example, in parallel to this project, Ontario Health—a provincial healthcare association—developed and released a guidance reference document on using virtual care for treating depression and anxiety.71 This document summarised literature reviews on virtual care and cognitive–behavioural therapy as well as the needs of First Nations, Métis, Inuit and other Indigenous peoples. While there were numerous similarities to the themes we found, particularly those emphasising the need for patient screening and privacy policies, there was little guidance regarding training healthcare providers to deliver virtual care, setting professional boundaries with patients or assessing the cost-effectiveness of virtual health services.68 In general, the guidance from provincial medical associations tended to also be somewhat vague (we reviewed these documents as part of our project, available at: https://pcmhstandards.ca/policy-overview/). Several guidance documents focused more on describing the potential usefulness of virtual healthcare for improving health equity.72 73 Others did not provide an outline of what is needed for effective delivery of virtual mental healthcare services.74 75
Strengths and limitations
Our approach has some limitations. This review is a ‘rapid review’, which has been previously described as a ‘…type of knowledge synthesis in which components of the systematic review process are simplified or omitted to produce information in a short period of time’.76 As such, while this review was well suited for establishing a knowledge base regarding virtual care delivery guidelines, it is possible that our literature search was not fully comprehensive. Although this may have resulted in missing some relevant articles, we believe the value of having completed this in a relatively timely manner to guide policy development outweighs that downside. Our use of the ‘quadruple aim’ as a framework for data collection from included articles may have impacted the interpretation of the content analysis, but we believe this provided an important direction that grounded our process in essential health services aims. In addition, despite our best efforts, the timeline of this review took longer than expected in order to prioritise resources to the completion of the entire grant project instead of to one individual article.
Strengths include our engagement of individuals with lived experience of mental illness throughout the review process, including in establishing the research question and reviewing emerging concepts and themes through the content analysis process. Our search identified relevant results and by conducting a rapid review as opposed to a systematic or scoping review, we have been able to incorporate these findings into a process for developing national standards for virtual mental health services in Canadian primary care,13 which will become important policy guidance for Canadian healthcare. We used rigorous methods throughout and advanced knowledge in an area that had not previously been thoroughly examined.
Conclusion
Changes in the delivery of primary care brought about by the public health response to the COVID-19 pandemic have necessitated an analysis of how virtual mental healthcare is delivered, and what recommendations exist to support and refine its delivery. This review described the extent to which existing recommendations in high-income settings fulfil domains within the quadruple aim, and generated new knowledge about concepts within these domains that can be used to guide policy development. This review has occurred at an opportune time to address a burgeoning gap in knowledge, contributing to current understanding of the research and guidelines relied on by providers to deliver virtual care in high-income countries before, during and after the implementation of COVID-19 restrictions.
Supplementary Material
Footnotes
Twitter: @h_atherton
Presented at: Presented at North American Primary Care Research Group Conference in San Francisco, CA, United States on 2 November 2023 and preliminary results published in the following conference proceeding document: O’Neill B, Langford L, Selby P, Salvalaggio G, Ziegler C, Anderson E, Atherton H. Guidance for virtual mental health services: a rapid review of guidelines and recommendations from high income countries. Ann Fam Med. 2023 Nov 1;21(Suppl 3).
Contributors: BO'N conceived of the overall project and obtained funding. CZ designed and implemented the search strategy. LL, NE and AY reviewed search results and selected articles for inclusion and extracted data. NE and AY conducted analysis. BO'N, NE, AY wrote the first draft of this manuscript. NE, AY, MKa, KW, SRM, HA, GS, LL, SS, CZ, TDA, PS, MKe, EA and BO'N substantively contributed to discussions about data analysis and interpretation during the review process. NE, AY, MKa, KW, SRM, HA, GS, LL, SS, CZ, TDA, PS, MKe, EA and BO'N substantively reviewed and edited the manuscript for intellectual content prior to submission. BO'N accepts full responsibility for the work and/or the conduct of the study as guarantor, had access to the data, and controlled the decision to publish.
Funding: This study is supported by the Canadian Institutes of Health Research (478439).
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting, or dissemination plans of this research. Refer to the Methods section for further details.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
All data relevant to the study are included in the article or uploaded as online supplemental information.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study was approved by the Unity Health Toronto Research Ethics Board, approval #22-262.
References
- 1.Shaw J, Jamieson T, Agarwal P, et al. Virtual care policy recommendations for patient-centred primary care: findings of a consensus policy dialogue using a nominal group technique. J Telemed Telecare 2018;24:608–15. 10.1177/1357633X17730444 [DOI] [PubMed] [Google Scholar]
- 2.Glazier RH, Green ME, Wu FC, et al. Shifts in office and virtual primary care during the early COVID-19 pandemic in Ontario, Canada. CMAJ 2021;193:E200–10. 10.1503/cmaj.202303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bestsennyy O, Gilbert G, Harris A, et al. Telehealth: A quarter-Trilliondollar post-COVID-19 reality? 2020. Available: https://www.mckinsey.com/~/media/McKinsey/Industries/Healthcare Systems and Services/Our Insights/Telehealth A quarter trillion dollar post COVID 19reality/Telehealth-A-quarter-trilliondollar-post-COVID-19-reality.pdf
- 4.Husain MO, Gratzer D, Husain MI, et al. Mental Illness in the Post-pandemic World: Digital Psychiatry and the Future. Front Psychol 2021;12:567426. 10.3389/fpsyg.2021.567426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Canadian Mental Health Association . Fast facts about mental illness. 2021. Available: https://cmha.ca/brochure/fast-facts-about-mental-illness/
- 6.College of Family Physicians of Canada . Family physicians’ response to the COVID-19 pandemic: results of the May 2021 CFPC members survey on COVID-19. 2021. Available: https://www.cfpc.ca/CFPC/media/Resources/Research/COVID-19-Summary-May2021-ENG.pdf
- 7.Stephenson E, Butt DA, Gronsbell J, et al. Changes in the top 25 reasons for primary care visits during the COVID-19 pandemic in a high-COVID region of Canada. PLoS One 2021;16:e0255992. 10.1371/journal.pone.0255992 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stephenson E, O’Neill B, Gronsbell J, et al. Changes in family medicine visits across sociodemographic groups after the onset of the COVID-19 pandemic in Ontario: a retrospective cohort study. CMAJ Open 2021;9:E651–8. 10.9778/cmajo.20210005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hammersley V, Donaghy E, Parker R, et al. Comparing the content and quality of video, telephone, and face-to-face consultations: a non-randomised, quasi-experimental, exploratory study in UK primary care. Br J Gen Pract 2019;69:e595–604. 10.3399/bjgp19X704573 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bodenheimer T, Sinsky C. From triple to quadruple aim: care of the patient requires care of the provider. Ann Fam Med 2014;12:573–6. 10.1370/afm.1713 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Avdagovska M, Menon D, Stafinski T. Capturing the Impact of Patient Portals Based on the Quadruple Aim and Benefits Evaluation Frameworks: Scoping Review. J Med Internet Res 2020;22:e24568. 10.2196/24568 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Arnetz BB, Goetz CM, Arnetz JE, et al. Enhancing healthcare efficiency to achieve the Quadruple Aim: an exploratory study. BMC Res Notes 2020;13. 10.1186/s13104-020-05199-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Canadian standards for virtual delivery of mental health services in primary care. 2023. Available: https://pcmhstandards.ca/ [Accessed 20 Dec 2023].
- 14.Garritty C, Gartlehner G, Nussbaumer-Streit B, et al. Cochrane Rapid Reviews Methods Group offers evidence-informed guidance to conduct rapid reviews. J Clin Epidemiol 2021;130:13–22. 10.1016/j.jclinepi.2020.10.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tricco AC, Garritty CM, Boulos L, et al. Rapid review methods more challenging during COVID-19: commentary with a focus on 8 knowledge synthesis steps. J Clin Epidemiol 2020;126:177–83. 10.1016/j.jclinepi.2020.06.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Stevens A, Garritty C, Hersi M, et al. Developing PRISMA-RR, a reporting guideline for rapid reviews of primary studies (protocol). 2018. Available: https://www.equator-network.org/wp-content/uploads/2018/02/PRISMA-RR-protocol.pdf
- 17.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Int J Surg 2021;88:105906. 10.1016/j.ijsu.2021.105906 [DOI] [PubMed] [Google Scholar]
- 18.National Institute of Mental Health . What is Telemental health? n.d. Available: https://www.nimh.nih.gov/health/publications/what-is-telemental-health
- 19.Health Resources & Services Administration . Telehealth for direct-to-consumer care. Health Resources & Services Administration. n.d. Available: https://telehealth.hhs.gov/providers/best-practice-guides/direct-to-consumer [Google Scholar]
- 20.Hsieh H-F, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res 2005;15:1277–88. 10.1177/1049732305276687 [DOI] [PubMed] [Google Scholar]
- 21.Elo S, Kyngäs H. The qualitative content analysis process. J Adv Nurs 2008;62:107–15. 10.1111/j.1365-2648.2007.04569.x [DOI] [PubMed] [Google Scholar]
- 22.DE Weger E, Macinnes D, Enser J, et al. Implementing video conferencing in mental health practice. J Psychiatr Ment Health Nurs 2013;20:448–54. 10.1111/j.1365-2850.2012.01947.x [DOI] [PubMed] [Google Scholar]
- 23.Rabe M. Telehealth in South Africa: A guide for healthcare practitioners in primary care. South African Family Practice 2022;64:e1–6. 10.4102/safp.v64i1.5533 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Johnson GR. Toward uniform competency standards in telepsychology: A proposed framework for Canadian psychologists. Canadian Psychology / Psychologie Canadienne;55:291–302. 10.1037/a0038002 [DOI] [Google Scholar]
- 25.Luxton DD, Pruitt LD, Osenbach JE. Best practices for remote psychological assessment via telehealth technologies. Professional Psychology: Research and Practice 2014;45:27–35. 10.1037/a0034547 [DOI] [Google Scholar]
- 26.Saeed SA, Pastis I. Using telehealth to enhance access to evidence-based care. Psychiatr Times 2018;35:9–22. [Google Scholar]
- 27.Shore JH. Best Practices in Tele-Teaming: Managing Virtual Teams in the Delivery of Care in Telepsychiatry. Curr Psychiatry Rep 2019;21:1–8. 10.1007/s11920-019-1052-x [DOI] [PubMed] [Google Scholar]
- 28.Shore JH, Yellowlees P, Caudill R, et al. Best Practices in Videoconferencing-Based Telemental Health April 2018. Telemedicine and E-Health 2018;24:827–32. 10.1089/tmj.2018.0237 [DOI] [PubMed] [Google Scholar]
- 29.Liem A, Sit HF, Arjadi R, et al. Ethical standards for telemental health must be maintained during the COVID-19 pandemic. Asian J Psychiatr 2020;53:102218. 10.1016/j.ajp.2020.102218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sasangohar F, Bradshaw MR, Carlson MM, et al. Adapting an Outpatient Psychiatric Clinic to Telehealth During the COVID-19 Pandemic: A Practice Perspective. J Med Internet Res 2020;22:e22523. 10.2196/22523 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Duane J-N, Blanch-Hartigan D, Sanders JJ, et al. Environmental Considerations for Effective Telehealth Encounters: A Narrative Review and Implications for Best Practice. Telemedicine and E-Health 2022;28:309–16. 10.1089/tmj.2021.0074 [DOI] [PubMed] [Google Scholar]
- 32.Summer G, Adelman DS, Fant C. COVID-19 and telehealth: How to complete a successful telehealth visit. Nurse Pract 2021;46:43–7. 10.1097/01.NPR.0000751808.74986.82 [DOI] [PubMed] [Google Scholar]
- 33.Turvey C, Coleman M, Dennison O, et al. ATA Practice Guidelines for Video-Based Online Mental Health Services. Telemedicine and E-Health 2013;19:722–30. 10.1089/tmj.2013.9989 [DOI] [PubMed] [Google Scholar]
- 34.Webb C, Orwig J. Expanding our Reach: Telehealth and Licensure Implications for Psychologists. J Clin Psychol Med Settings 2015;22:243–50. 10.1007/s10880-015-9440-9 [DOI] [PubMed] [Google Scholar]
- 35.Pompeo-Fargnoli A, Lapa A, Pellegrino C. Telemental health and student veterans: A practice perspective through voices from the field. Journal of Technology in Human Services 2020;38:271–87. 10.1080/15228835.2019.1674764 [DOI] [Google Scholar]
- 36.Goldin D, Maltseva T, Scaccianoce M, et al. Cultural and Practical Implications for Psychiatric Telehealth Services: A Response to COVID-19. J Transcult Nurs 2021;32:186–90. 10.1177/1043659620973069 [DOI] [PubMed] [Google Scholar]
- 37.Haydon HM, Smith AC, Snoswell CL, et al. Addressing concerns and adapting psychological techniques for videoconsultations: a practical guide. Clinical Psychologist 2021;25:179–86. 10.1080/13284207.2021.1916904 [DOI] [Google Scholar]
- 38.Stoll J, Müller JA, Trachsel M. Ethical Issues in Online Psychotherapy: A Narrative Review. Front Psychiatry 2019;10:993. 10.3389/fpsyt.2019.00993 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yellowlees P, Shore J, Roberts L. Practice Guidelines for Videoconferencing-Based Telemental Health – October 2009. Telemedicine and E-Health 2010;16:1074–89. 10.1089/tmj.2010.0148 [DOI] [PubMed] [Google Scholar]
- 40.Chipps J, Ramlall S, Mars M. Practice guidelines for videoconference-based telepsychiatry in South Africa. Afr J Psych 2012;15. 10.4314/ajpsy.v15i4.35 [DOI] [PubMed] [Google Scholar]
- 41.Joint Task Force for the Development of Telepsychology Guidelines for Psychologists . Guidelines for the practice of telepsychology. Am Psychol 2013;68:791–800. 10.1037/a0035001 [DOI] [PubMed] [Google Scholar]
- 42.Hilty DM, Sunderji N, Suo S, et al. Telepsychiatry and other technologies for integrated care: evidence base, best practice models and competencies. Int Rev Psychiatry 2018;30:292–309. 10.1080/09540261.2019.1571483 [DOI] [PubMed] [Google Scholar]
- 43.Abraham A, Jithesh A, Doraiswamy S, et al. Telemental Health Use in the COVID-19 Pandemic: A Scoping Review and Evidence Gap Mapping. Front Psychiatry 2021;12:748069. 10.3389/fpsyt.2021.748069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Luxton DD, O’Brien K, McCann RA, et al. Home-Based Telemental Healthcare Safety Planning: What You Need to Know. Telemedicine and E-Health 2012;18:629–33. 10.1089/tmj.2012.0004 [DOI] [PubMed] [Google Scholar]
- 45.Luxton DD, O’Brien K, Pruitt LD, et al. Suicide risk management during clinical telepractice. Int J Psychiatry Med 2014;48:19–31. 10.2190/PM.48.1.c [DOI] [PubMed] [Google Scholar]
- 46.Barnett JE, Kolmes K. The practice of tele-mental health: Ethical, legal, and clinical issues for practitioners. Practice Innovations 2016;1:53–66. 10.1037/pri0000014 [DOI] [Google Scholar]
- 47.Palomares RS, Bufka LF, Baker DC. Critical Concerns When Incorporating Telepractice in Outpatient Settings and Private Practice. J Child Adolesc Psychopharmacol 2016;26:252–9. 10.1089/cap.2015.0013 [DOI] [PubMed] [Google Scholar]
- 48.Smith K, Ostinelli E, Macdonald O, et al. COVID-19 and Telepsychiatry: Development of Evidence-Based Guidance for Clinicians. JMIR Ment Health 2020;7:e21108. 10.2196/21108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Van Daele T, Karekla M, Kassianos AP, et al. Recommendations for policy and practice of telepsychotherapy and e-mental health in Europe and beyond. Journal of Psychotherapy Integration 2020;30:160–73. 10.1037/int0000218 [DOI] [Google Scholar]
- 50.Crowe TV. Is Telemental Health Services a Viable Alternative to Traditional Psychotherapy for Deaf Individuals? Community Ment Health J 2017;53:154–62. 10.1007/s10597-016-0025-3 [DOI] [PubMed] [Google Scholar]
- 51.Gorenko JA, Moran C, Flynn M, et al. Social Isolation and Psychological Distress Among Older Adults Related to COVID-19: A Narrative Review of Remotely-Delivered Interventions and Recommendations. J Appl Gerontol 2021;40:3–13. 10.1177/0733464820958550 [DOI] [PubMed] [Google Scholar]
- 52.Grosch MC, Gottlieb MC, Cullum CM. Initial practice recommendations for teleneuropsychology. Clin Neuropsychol 2011;25:1119–33. 10.1080/13854046.2011.609840 [DOI] [PubMed] [Google Scholar]
- 53.de Siqueira Rotenberg L, Nascimento C, Cohab Khafif T, et al. Psychological therapies and psychoeducational recommendations for bipolar disorder treatment during COVID-19 pandemic. Bipolar Disord 2020;22:644–6. 10.1111/bdi.12981 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Adams SM, Rice MJ, Jones SL, et al. TeleMental Health: Standards, Reimbursement, and Interstate Practice [Formula: see text]. J Am Psychiatr Nurses Assoc 2018;24:295–305. 10.1177/1078390318763963 [DOI] [PubMed] [Google Scholar]
- 55.McCord C, Bernhard P, Walsh M, et al. A consolidated model for telepsychology practice. J Clin Psychol 2020;76:1060–82. 10.1002/jclp.22954 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Sabin JE, Skimming K. A framework of ethics for telepsychiatry practice. Int Rev Psychiatry 2015;27:490–5. 10.3109/09540261.2015.1094034 [DOI] [PubMed] [Google Scholar]
- 57.Xiang Y-T, Zhao N, Zhao Y-J, et al. An overview of the expert consensus on the mental health treatment and services for major psychiatric disorders during COVID-19 outbreak: China’s experiences. Int J Biol Sci 2020;16:2265–70. 10.7150/ijbs.47419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Batastini AB, Jones ACT, Lester ME, et al. Initiation of a multidisciplinary telemental health clinic for rural justice-involved populations: Rationale, recommendations, and lessons learned. J Community Psychol 2020;48:2156–73. 10.1002/jcop.22424 [DOI] [PubMed] [Google Scholar]
- 59.Krzystanek M, Matuszczyk M, Krupka-Matuszczyk I, et al. Letter to Editor. Polish recommendations for conducting online visits in psychiatric care. Psychiatr Pol 2020;54:391–4. 10.12740/PP/120067 [DOI] [PubMed] [Google Scholar]
- 60.Drum KB, Littleton HL. Therapeutic boundaries in telepsychology: Unique issues and best practice recommendations. Prof Psychol Res Pr 2014;45:309–15. 10.1037/a0036127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Hilty DM, Serhal E, Crawford A. A Telehealth and Telepsychiatry Economic Cost Analysis Framework: Scoping Review. Telemedicine and E-Health 2023;29:23–37. 10.1089/tmj.2022.0016 [DOI] [PubMed] [Google Scholar]
- 62.Palesy D, Forrest G, Crowley ME. Education guidelines, frameworks and resources for building virtual care capacity: An integrative review. J Telemed Telecare 2023;29:222–43. 10.1177/1357633X221149230 [DOI] [PubMed] [Google Scholar]
- 63.Thomas EE, Haydon HM, Mehrotra A, et al. Building on the momentum: Sustaining telehealth beyond COVID-19. J Telemed Telecare 2022;28:301–8. 10.1177/1357633X20960638 [DOI] [PubMed] [Google Scholar]
- 64.Gordon HS, Solanki P, Bokhour BG, et al. “I’m Not Feeling Like I’m Part of the Conversation” Patients’ Perspectives on Communicating in Clinical Video Telehealth Visits. J GEN INTERN MED 2020;35:1751–8. 10.1007/s11606-020-05673-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Yellowlees P, Richard Chan S, Burke Parish M. The hybrid doctor-patient relationship in the age of technology - Telepsychiatry consultations and the use of virtual space. Int Rev Psychiatry 2015;27:476–89. 10.3109/09540261.2015.1082987 [DOI] [PubMed] [Google Scholar]
- 66.Serhal E, Kirvan A, Sanches M, et al. Client Satisfaction and Experience With Telepsychiatry: Development and Validation of a Survey Using Clinical Quality Domains. J Med Internet Res 2020;22:e19198. 10.2196/19198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Yusuf A, O’Neill B. Access to virtual mental-health care uneven across Canada. healthy debate. 2023. Available: https://healthydebate.ca/2023/05/topic/access-mental-health-care-uneven/
- 68.O’Keefe M, White K, Jennings JC. Asynchronous telepsychiatry: A systematic review. J Telemed Telecare 2021;27:137–45. 10.1177/1357633X19867189 [DOI] [PubMed] [Google Scholar]
- 69.Rodriguez JA, Betancourt JR, Sequist TD, et al. Differences in the use of telephone and video telemedicine visits during the COVID-19 pandemic. Am J Manag Care 2021;27:21–6. 10.37765/ajmc.2021.88573 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Sachs JW, Graven P, Gold JA, et al. Disparities in telephone and video telehealth engagement during the COVID-19 pandemic. JAMIA Open 2021;4:ooab056. 10.1093/jamiaopen/ooab056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Ontario Health . Clinically appropriate use of virtual care for depression and Anxiety- related conditions | guidance reference document. 2023. Available: https://www.ontariohealth.ca/sites/ontariohealth/files/DepressionAnxietyRelatedConditionsVirtualCareGuidance.pdf
- 72.College of Physicians and Surgeons of Saskatchewan . Virtual care. 2021. Available: https://www.cps.sk.ca/imis/CPSS/For_Physicians/Patient_Care/Virtual_Care/CPSS/For_Physicians/Patient_Care/Virtual_Care.aspx?hkey=534927ea-eb4b-4ec2-ba89-d09928e2bd07
- 73.College of Physicians and Surgeons of British Columbia . Virtual care. 2013. Available: https://www.cpsbc.ca/files/pdf/PSG-Virtual-Care.pdf
- 74.College of Physicians and Surgeons of Alberta . Virtual care | standard of practice. 2014. Available: https://cpsa.ca/physicians/standards-of-practice/virtual-care/
- 75.Northwest Territories, Health and Social Services Authority Telehealth. n.d. Available: https://www.nthssa.ca/en/services/telehealth
- 76.Tricco AC, Antony J, Zarin W, et al. A scoping review of rapid review methods. BMC Med 2015;13:224. 10.1186/s12916-015-0465-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.The World Bank . World Bank country and lending groups. n.d. Available: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519#High_income
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2023-079244supp001.pdf (64.4KB, pdf)
bmjopen-2023-079244supp002.pdf (24.8KB, pdf)
bmjopen-2023-079244supp003.pdf (6.5MB, pdf)
bmjopen-2023-079244supp004.pdf (168.8KB, pdf)
Data Availability Statement
All data relevant to the study are included in the article or uploaded as online supplemental information.