Abstract
Background: Amid the ongoing national crisis of opioid misuse in the United States, medical cannabis (MC) has emerged as a potential alternative for chronic pain conditions. This study was performed to understand which orthopedic conditions patients are seeking MC certification for.
Methods: This prospective study was conducted at the Department of Medical Cannabis, Rothman Orthopaedic Institute, Philadelphia, PA, USA. It included consecutive patients with chronic musculoskeletal noncancer pain who were certified for MC, following the Pennsylvania state certification process. Data collected included demographic data, diagnoses, anatomic site of pain, and Patient-Reported Outcomes Measurement Information System (PROMIS) global health scale. The outcome measures from the PROMIS global health scale were used to generate Global Physical Health (GPH) quality of life (QoL) T scores and Global Mental Health (GMH) QoL T scores.
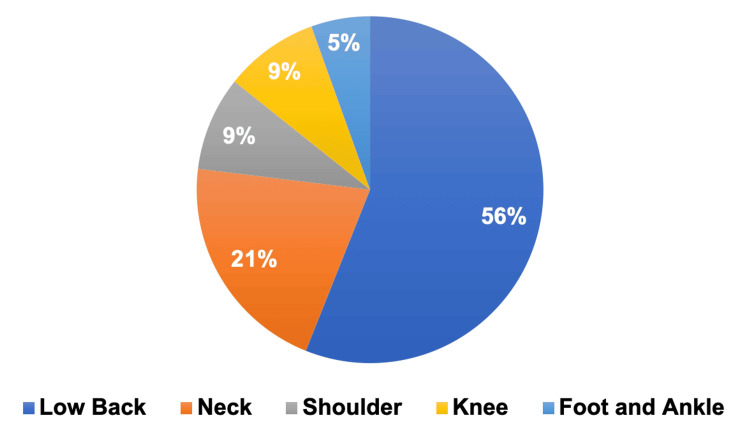
Results: A total of 78 patients were available for analysis following initial MC certification, with 50 (64%) being female and 28 (36%) male. The average age was 63 years with 60% of patients in the 65+ age group. Ethnically, 73 (92%) identified as White, and 70 (90%) were not of Hispanic or Latino origin. The most common reason for seeking MC certification was low back pain (56%), followed by neck pain (21%) and then extremity complaints. The mean GPH QoL T score was 43.71 with a standard deviation of ± 9.86 (p-value = 0.001), while the mean GMH QoL T score was 46.85 with a standard deviation of 8.28 (p-value = 0.0015).
Conclusion: MC cannabis certification was more often sought by women than men and most common for spinal complaints, specifically lower back followed by cervical spine concerns.. This cohort of patients had lower GPH QoL and GMH QoL T scores compared the US general population, representing a significant reduction in the overall physical and mental health.
Keywords: orthopaedic, medical cannabis certification, musculoskeletal conditions, orthopaedics, medical cannabis
Introduction
The United States faces a national crisis from opioid misuse [1]. The utilization of medical cannabis (MC) has emerged as an alternative option for pain relief, potentially alleviating the need for excessive opioid reliance. As of 2023, there are currently 38 states, three territories, and the District of Columbia where MC is legal [2]. As medical and recreational cannabis become increasingly legalized across the United States and in other nations, our understanding of MC continues to expand [3].
MC has shown to be effective in treating chronic noncancer pain, neuropathic pain, seizure disorders, and multiple sclerosis-related spasticities [4-7]. Several randomized control studies have shown a significant analgesic effect of cannabinoids without severe adverse effects [4]. MC has proven to be effective in alleviating orthopedic pain when compared to a placebo [8]. Subsequently, there is a growing interest within the orthopedic field regarding its potential as a treatment or supplementary approach for various painful musculoskeletal conditions [9].
The purpose of this study is to enhance understanding of orthopedic patients’ perspectives on MC by examining the specific orthopedic conditions for which they are pursuing MC certification. This research aims to provide insights into the demographic profiles of patients seeking MC certification. It also explores patients’ perceptions of their overall health including their physical and mental well-being, as assessed through a global health scale [10].
Materials and methods
This study was conducted at the Department of Medical Cannabis, Rothman Orthopaedic Institute, Philadelphia, PA, USA. Thomas Jefferson University Institutional Review Board (IRB) Committee approved full IRB approval for this project (approval number: 19D.159). All consecutive patients seeking initial MC certification with a diagnosis of chronic musculoskeletal noncancer pain between October 2022 and September 2023 were prospectively enrolled. Patients were enrolled and certified at a single academic practice.
All physicians participating in MC certification underwent a mandatory four-hour continuing medical education (CME) course and submitted applications to the Pennsylvania Department of Health to become accredited practitioners. All patients applying for MC certification were screened to ensure they met the requirements of being Pennsylvania residents and having one of the 23 state-approved medical conditions [11].
Patients eligible for MC underwent a thorough chart review aimed at identifying any history of severe mental health disorders. Those individuals found to have such a history were subsequently excluded. In addition, an evaluation of their prescription drug monitoring history was performed using Pennsylvania’s Prescription Drug Monitoring Program (PDMP). In the case that the patient was using opioids, the pain management team was involved to discuss reduction of opioid use to allow for introduction of MC to their regimen. During the certification visit, the chemical components of MC, routes of delivery methods, and optimal dosing parameters were discussed with each patient. Once certified, patients could obtain an MC identification card through the Pennsylvania Department of Health, allowing them to make purchases at state-approved cannabis dispensaries.
For all patients ultimately certified, patient demographics were obtained through the electronic medical records. At the initial visit, the Patient-Reported Outcomes Measurement Information System (PROMIS) global health scale and diagnosis of low back, neck, shoulder, and foot and ankle pain were collected. Due to the variability in the site of musculoskeletal pain, global pain outcome measures were used instead of site-specific disability measures. The PROMIS global health scale generated Global Physical Health (GPH) QoL T scores and Global Mental Health (GMH) quality of life (QoL) T scores [10].
Statistics for GPH and GMH were calculated using the Shapiro-Wilk test. The relationship of explanatory variables with GPH and GMH was tested using T-tests since the outcome variables were normally distributed. P values <0.05 in the analysis were considered statistically significant [10].
Results
This study included a total of 78 consecutive patients who were eligible and requested MC certification for a musculoskeletal pain diagnosis between October 2022 and September 2023. Of those patients, 28 (36%) were male and 50 (64%) were female. The average age of patients seeking MC certification was 63 years old (range 20-91 years), with the largest number of patients (60%) in the 65+ age group. Ethnically, 73 (92%) respondents identified as White, and 70 (90%) indicated that they were not of Hispanic or Latino origin (Table 1).
Table 1. Patient demographics.
*In the "Race" section, "Other" = one patient identified as African American and one patient identified as Arab
| Gender | N | % |
| Male | 28 | 36% |
| Female | 50 | 64% |
| Age | ||
| 18-34 | 4 | 5% |
| 35-49 | 9 | 11% |
| 50-64 | 18 | 23% |
| 65+ | 47 | 60% |
| Race | ||
| White | 73 | 94% |
| Other | 2 | 3% |
| Declined tosSpecify | 3 | 3% |
| Ethnicity | ||
| Hispanic or Latino | 0 | 0% |
| Not Hispanic or Latino | 70 | 90% |
| Declined to specify | 8 | 10% |
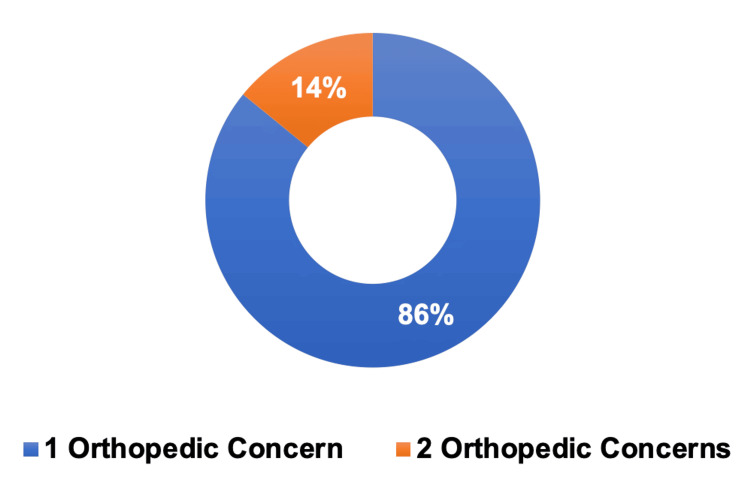
Among the 78 patients with orthopedic concerns, 51 (56%) sought MC certification for low back pain, 19 (21%) for neck pain, eight (9%) for shoulder pain, eight (9%) for knee pain, and five (5%) for foot and ankle pain (Figure 1). Of note, a portion of these patients presented multiple orthopedic concerns, as observed in 11 (14%) patients (Figure 2).
Figure 1. Orthopedic conditions.
Breakdown of orthopedic conditions for patients seeking medical cannabis certification: low back pain (n = 51), neck pain (n = 19), shoulder pain (n = 8), knee pain (n = 8), and foot and ankle pain (n = 5).
Figure 2. Number of patients with one versus two orthopedic conditions .
One orthopedic concern (n = 67), two orthopedic concerns (n = 11).
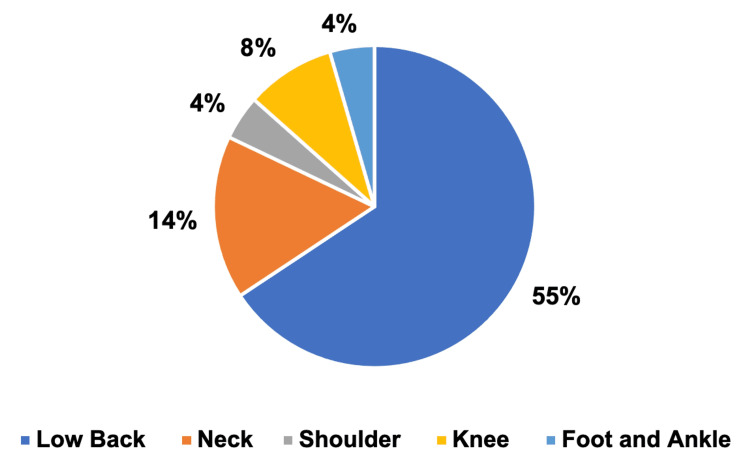
Among those with a single orthopedic concern, the largest group consisted of 44 (55%) patients with low back pain, while the smallest group had 3 (4%) patients with foot and ankle pain (Figure 3).
Figure 3. Patients with one orthopedic concern.
Low back pain = 44, neck pain = 11, shoulder pain = 3, knee pain = 6, foot and ankle pain = 3
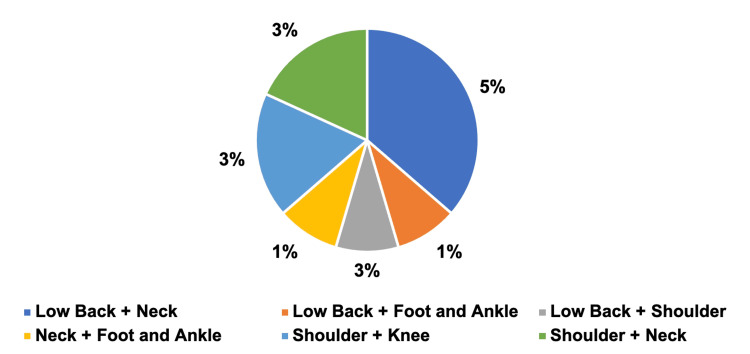
For patients with two orthopedic concerns, the most prevalent combination was low back pain and neck pain, with four (5%) patients, while the lowest prevalent combination was observed in low back pain and foot and ankle pain, neck pain and foot and ankle pain, and shoulder pain and neck pain, each with one patient (Figure 4).
Figure 4. Patient with two orthopedic concerns.
Low back pain + neck pain = 4, low back pain + foot and ankle pain = 1, low back pain + shoulder pain = 1, neck pain + foot and ankle pain = 1, shoulder pain + knee pain = 2, and shoulder pain + neck pain = 2
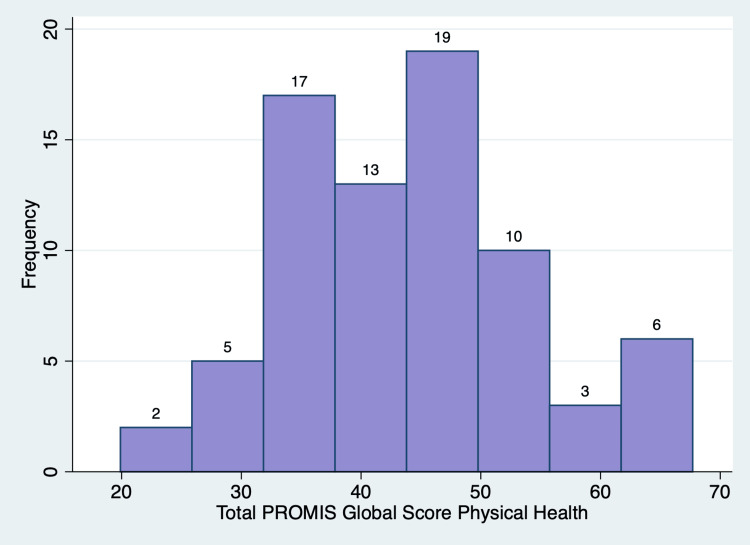
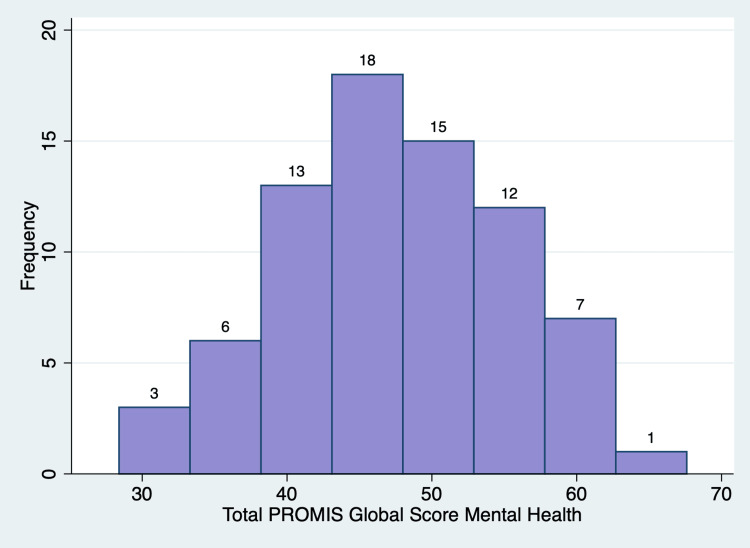
PROMIS outcome measures generates T-scores, which are standardized scores with a mean of 50 and a standard deviation of 10 based on a reference population (US general population) [12]. There was a range of responses for each of the items in the PROMIS global health scale (Table 2). For the GPH QoL, the mean T score was 43.71 ± 9.86 (p-value = 0.001), with 56 (72%) patients having lower than the standard T score of 50 (Figure 5). For the GMH QoL, the mean T score was 46.85 ± 8.28 (p-value = 0.0015), with 46 (59%) patients having lower than the standard T score of 50 (Figure 6). Of note, one patient did not fill out a global health survey, while two patients left questions 7, 8, and 10 blank. Thus, these responses were omitted. A posthoc power analysis showed that 78 patients provide 99.68% power to detect one-point change in the PROMIS global health scale (α = 0.05).
Table 2. Patient-Reported Outcomes Measurement Information System (PROMIS) global health scale .
| Poor (N) | (%) | Fair (N) | (%) | Good (N) | (%) | Very Good (N) | (%) | Excellent (N) | (%) | |||||||||||
| 1. In general, would you say your health is… | 2 | 3% | 23 | 30% | 26 | 34% | 22 | 29% | 4 | 5% | ||||||||||
| 2. In general, would you say your quality of life is… | 2 | 3% | 25 | 32% | 24 | 31% | 21 | 27% | 5 | 6% | ||||||||||
| 3. In general, how would you rate your physical health? | 6 | 9% | 29 | 38% | 28 | 36% | 11 | 14% | 3 | 4% | ||||||||||
| 4. In general, how would you rate your mental health, including your mood and your ability to think? | 2 | 3% | 8 | 10% | 29 | 38% | 25 | 32% | 13 | 17% | ||||||||||
| 5. In general, how would you rate your satisfaction with your social activities and relationships? | 5 | 6% | 11 | 14% | 22 | 29% | 27 | 35% | 12 | 16% | ||||||||||
| 9. In general, please rate how well you carry out your usual social activities and roles. | 5 | 6% | 19 | 25% | 25 | 32% | 22 | 29% | 5 | 6% | ||||||||||
| Not At All | A Little | Moderately | Mostly | Completely | ||||||||||||||||
| 6. To what extent are you able to carry out your everyday physical activities such as walking, climbing stairs? | 3 | 4% | 21 | 27% | 28 | 36% | 20 | 26% | 5 | 6% | ||||||||||
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | |||||||||||
| 7. How would you rate your pain on average? | 0 | 0% | 0 | 0% | 3 | 4% | 13 | 17% | 9 | 12% | 13 | 17% | 17 | 22% | 11 | 14% | 7 | 13% | 3 | 4% |
| None | Mild | Moderate | Severe | Very Severe | ||||||||||||||||
| 8. How would you rate your fatigue on average? | 4 | 5% | 18 | 23% | 42 | 55% | 9 | 12% | 2 | 3% | ||||||||||
| Never | Rarely | Sometimes | Often | Always | ||||||||||||||||
| 10. How often have you been bothered by emotional problems such as feeling anxious, depressed? | 9 | 12% | 24 | 31% | 31 | 40% | 8 | 10% | 2 | 3% | ||||||||||
Figure 5. Normal distribution of the Patient-Reported Outcomes Measurement Information System (PROMIS) Global Physical Health T score.
Figure 6. Normal distribution of the Patient-Reported Outcomes Measurement Information System (PROMIS) Global Mental Health T score.
Discussion
This study revealed that patients sought MC certification for a range of musculoskeletal pain conditions, with the most being common lower back pain. This trend is consistent with existing literature as low back pain ranks as the primary cause of years lived with disability in both developed and developing nations, and it holds the sixth position in terms of the overall disease burden [13-15]. Following closely, neck pain was the second most common condition reported. Most patients presented with a single orthopedic concern, but 14% patients presented with dual primary musculoskeletal pain diagnoses, and among this subset, low back pain was still the most prevalent diagnosis.
When examining patient demographics, a larger proportion of women were seeking MC certification compared to men. This observation reflects existing studies, which emphasizes the higher prevalence of chronic back pain among women [16] and the greater likelihood of women to seek medical care for such conditions [13]. Chronic back pain also increases linearly from the third decade of life on, which is observed in the trend of a growing number of patients pursuing MC certification as their age increased [16].
The PROMIS global health survey measures an individual’s physical and mental well-being to provide a self-assessment of individuals’ overall health [10]. A higher PROMIS T-score indicates a greater representation of the measured concept [17]. The US general population has a T score mean of 50 and a standard deviation of 10 [12]. An individual with T-scores of 60 for the GPH or GMH scales is one standard deviation healthier than the general population [17]. Patients seeking MC certification had overall lower GPH QoL T scores and GMH QoL T scores with p-values less than 0.05, indicating a significant reduction in both overall physical and mental health compared to the US general population. The patients’ musculoskeletal pain likely contributes to the lower T scores. Importantly, these scores are a baseline measurement as future studies will include this outcome measure to track and examine the effects of MC on patients' self-reported assessments of their overall health.
The existing literature is controversial regarding the impact of MC on opioid use among individuals with chronic pain. While certain studies have demonstrated a reduction in opioid consumption with MC, others have reported no discernible change or even an increase in prescription drug usage [8,18-24]. However, there is a notable lack of research examining the influence of MC on opioid consumption, particularly in the context of chronic musculoskeletal pain [8,24-26]. This study emphasizes the need to further research MC in the realm of chronic musculoskeletal pain. There are limited studies that delineate the patient profiles seeking MC certification. This study clearly shows that patients of both genders and all age groups are considering MC as a component of their pain management strategy for a diverse array of orthopedic conditions.
This study has several limitations. The relatively small number of surveyed patients limits the statistical power of our findings. The patient group is not generalizable evidenced by over 90% of patients identifying as non-Hispanic and Latino and over 90% identifying as White compared to the general US population (58.9% non-Hispanic and Latino and 75.5% White) [27]. Another limitation is the unmeasured variables that cannot be accounted for when studying the relationship between musculoskeletal pain and patients' self-reported assessments of their overall health. These variables could include concurrent medication use, physical activity, and other lifestyle factors.
Future studies should incorporate follow-up assessments for patients with MC certifications to investigate the different types of cannabis products (whole flowers, oil cartridges, concentrates, tinctures, etc.) they are utilizing, aiming to identify the most effective options. In addition, assessing PROMIS global health scale outcome measures over time could provide valuable insights into the efficacy of MC. Given the limited data available regarding the side effects of various medical cannabis types, it would be insightful to explore the possible adverse effects experienced by patients.
Conclusions
While MC certification was sought out by patients of both genders and all age groups, it was more frequently sought by women than men and in older ages. The most common complaints pertained to the spine, specifically the lower back followed by cervical spine concerns. This cohort of patients exhibited lower GPH QoL and GMH QoL T scores in comparison to the US general population with p-values lower than 0.05, indicating a significant reduction in both overall physical health and mental health.
Acknowledgments
This study was supported through funding from the Rothman Orthopaedic Institute Foundation for Opioid Research & Education in Philadelphia, PA, USA.
The authors have declared that no competing interests exist.
Author Contributions
Concept and design: Juliet Chung, Asif M. Ilyas, Ari Greis
Acquisition, analysis, or interpretation of data: Juliet Chung, Asif M. Ilyas, Ari Greis, Yusuf Mahmoud, Sina Ramtin, Gianna Uhler
Drafting of the manuscript: Juliet Chung, Asif M. Ilyas, Yusuf Mahmoud, Sina Ramtin, Gianna Uhler
Critical review of the manuscript for important intellectual content: Juliet Chung, Asif M. Ilyas, Ari Greis
Supervision: Asif M. Ilyas, Ari Greis
Human Ethics
Consent was obtained or waived by all participants in this study. Thomas Jefferson University IRB Committee issued approval 19D.159
Animal Ethics
Animal subjects: All authors have confirmed that this study did not involve animal subjects or tissue.
References
- 1.The opioid crisis: the surgeon's role. Goldberg RF. Adv Surg. 2019;53:305–325. doi: 10.1016/j.yasu.2019.04.015. [DOI] [PubMed] [Google Scholar]
- 2.National Conference of State Legislatures State Medical Marijuana Laws. [ Oct; 2023 ]. 2023. https://www.ncsl.org/health/state-medical-cannabis-laws https://www.ncsl.org/health/state-medical-cannabis-laws
- 3.Medical cannabis in hand surgery: a review of the current evidence. Yang A, Townsend CB, Ilyas AM. J Hand Surg Am. 2023;48:292–300. doi: 10.1016/j.jhsa.2022.11.008. [DOI] [PubMed] [Google Scholar]
- 4.Cannabinoids for the treatment of chronic non-cancer pain: an updated systematic review of randomized controlled trials. Lynch ME, Ware MA. J Neuroimmune Pharmacol. 2015;10:293–301. doi: 10.1007/s11481-015-9600-6. [DOI] [PubMed] [Google Scholar]
- 5.Cannabis and cannabinoids for chronic pain. Romero-Sandoval EA, Kolano AL, Alvarado-Vázquez PA. Curr Rheumatol Rep. 2017;19:67. doi: 10.1007/s11926-017-0693-1. [DOI] [PubMed] [Google Scholar]
- 6.Medical marijuana for treatment of chronic pain and other medical and psychiatric problems: a clinical review. Hill KP. JAMA. 2015;313:2474–2483. doi: 10.1001/jama.2015.6199. [DOI] [PubMed] [Google Scholar]
- 7.Therapeutic potential of cannabis, cannabidiol, and cannabinoid-based pharmaceuticals. Legare CA, Raup-Konsavage WM, Vrana KE. Pharmacology. 2022;107:131–149. doi: 10.1159/000521683. [DOI] [PubMed] [Google Scholar]
- 8.Cannabis for pain in orthopedics: a systematic review focusing on study methodology. Madden K, George A, van der Hoek NJ, Borim FM, Mammen G, Bhandari M. Can J Surg. 2019;62:369–380. doi: 10.1503/cjs.001018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Medicinal cannabis in orthopaedic practice. Kleeman-Forsthuber LT, Dennis DA, Jennings JM. J Am Acad Orthop Surg. 2020;28:268–277. doi: 10.5435/JAAOS-D-19-00438. [DOI] [PubMed] [Google Scholar]
- 10.Patient-Reported Outcomes Measurement Information System. [ Oct; 2023 ]. 2017. http://www.healthmeasures.net/images/PROMIS/manuals/PROMIS_Global_Scoring_Manual.pdf http://www.healthmeasures.net/images/PROMIS/manuals/PROMIS_Global_Scoring_Manual.pdf
- 11.Getting medical marijuana. [ Oct; 2023 ]. 2023. https://www.pa.gov/guides/pennsylvania-medical-marijuana-program/ https://www.pa.gov/guides/pennsylvania-medical-marijuana-program/
- 12.Development and validation of an interpretive guide for PROMIS scores. Rothrock NE, Amtmann D, Cook KF. J Patient Rep Outcomes. 2020;4:16. doi: 10.1186/s41687-020-0181-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Non-specific low back pain. Maher C, Underwood M, Buchbinder R. Lancet. 2017;389:736–747. doi: 10.1016/S0140-6736(16)30970-9. [DOI] [PubMed] [Google Scholar]
- 14.Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;386:743–800. doi: 10.1016/S0140-6736(15)60692-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.The global burden of low back pain: estimates from the Global Burden of Disease 2010 study. Hoy D, March L, Brooks P, et al. Ann Rheum Dis. 2014;73:968–974. doi: 10.1136/annrheumdis-2013-204428. [DOI] [PubMed] [Google Scholar]
- 16.Prevalence of chronic low back pain: systematic review. Meucci RD, Fassa AG, Faria NM. Rev Saude Publica. 2015;49:1. doi: 10.1590/S0034-8910.2015049005874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Global Health Scoring Manual. [ Oct; 2023 ]. 2021. https://www.healthmeasures.net/images/PROMIS/manuals/Scoring_Manual_Only/PROMIS_Global_Health_Scoring_Manual.pdf. https://www.healthmeasures.net/images/PROMIS/manuals/Scoring_Manual_Only/PROMIS_Global_Health_Scoring_Manual.pdf.
- 18.Medical cannabis use is associated with decreased opiate medication use in a retrospective cross-sectional survey of patients with chronic pain. Boehnke KF, Litinas E, Clauw DJ. J Pain. 2016;17:739–744. doi: 10.1016/j.jpain.2016.03.002. [DOI] [PubMed] [Google Scholar]
- 19.Cannabis as a substitute for opioid-based pain medication: patient self-report. Reiman A, Welty M, Solomon P. Cannabis Cannabinoid Res. 2017;2:160–166. doi: 10.1089/can.2017.0012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.The effect of medicinal cannabis on pain and quality-of-life outcomes in chronic pain: a prospective open-label study. Haroutounian S, Ratz Y, Ginosar Y, Furmanov K, Saifi F, Meidan R, Davidson E. Clin J Pain. 2016;32:1036–1043. doi: 10.1097/AJP.0000000000000364. [DOI] [PubMed] [Google Scholar]
- 21.Medical cannabis access, use, and substitution for prescription opioids and other substances: a survey of authorized medical cannabis patients. Lucas P, Walsh Z. Int J Drug Policy. 2017;42:30–35. doi: 10.1016/j.drugpo.2017.01.011. [DOI] [PubMed] [Google Scholar]
- 22.Medical marijuana users are more likely to use prescription drugs medically and nonmedically. Caputi TL, Humphreys K. J Addict Med. 2018;12:295–299. doi: 10.1097/ADM.0000000000000405. [DOI] [PubMed] [Google Scholar]
- 23.Effect of cannabis use in people with chronic non-cancer pain prescribed opioids: findings from a 4-year prospective cohort study. Campbell G, Hall WD, Peacock A, et al. Lancet Public Health. 2018;3:0–50. doi: 10.1016/S2468-2667(18)30110-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Medical cannabis use reduces opioid prescriptions in patients with chronic back pain. Greis A, Renslo B, Wilson-Poe AR, Liu C, Radakrishnan A, Ilyas AM. Cureus. 2022;14:0. doi: 10.7759/cureus.21452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Preliminary assessment of the efficacy, tolerability and safety of a cannabis-based medicine (Sativex) in the treatment of pain caused by rheumatoid arthritis. Blake DR, Robson P, Ho M, Jubb RW, McCabe CS. Rheumatology (Oxford) 2006;45:50–52. doi: 10.1093/rheumatology/kei183. [DOI] [PubMed] [Google Scholar]
- 26.The impact of medical cannabis on intermittent and chronic opioid users with back pain: how cannabis diminished prescription opioid usage. Takakuwa KM, Hergenrather JY, Shofer FS, Schears RM. Cannabis Cannabinoid Res. 2020;5:263–270. doi: 10.1089/can.2019.0039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.QuickFacts: United States. [ Oct; 2023 ]. 2022. https://www.census.gov/quickfacts/fact/table/US/PST045222 https://www.census.gov/quickfacts/fact/table/US/PST045222