Abstract
Purpose
Sarcopenia is a pathological change characterized by muscle loss in older people. According to the reports, there is controversy on the relationship between dyslipidemia and sarcopenia. Therefore, this meta-analysis aimed to explore the association between sarcopenia and dyslipidemia.
Methods
We searched the Cochrane Library, Web of Science, PubMed, China National Knowledge Infrastructure (CNKI), Wan Fang, China Science and Technology Journal Database (VIP Database) for case‒control studies to extract data on the odds ratio (OR) between sarcopenia and dyslipidemia and the MD(mean difference) of TC, LDL-C, HDL-C, TG, and TG/HDL-C between sarcopenia and nonsarcopenia. The JBI(Joanna Briggs) guidelines were used to evaluate the quality. Excel 2021, Review Manager 5.3 and Stata 16.0 were used for the statistical analysis.
Results
Twenty studies were included in the meta-analysis, 19 of which were evaluated as good quality. The overall OR of the relationship between sarcopenia and dyslipidemia was 1.47, and the MD values of TC, LDL-C, HDL-C, TG, and TG/HDL-C were 1.10, 1.95, 1.27, 30.13, and 0.16 respectively. In female, compared with the non-sarcopnia, the MD of TC, LDL-C, HDL-C, TG of sarcopenia were − 1.67,2.21,1.02,-3.18 respectively. In male, the MD of TC, LDL-C, HDL-C, TG between sarcopenia and non-sarcopenia were − 0.51, 1.41, 5.77, -0.67. The OR between sarcopenia and dyslipidemia of the non-China region was 4.38, and it was 0.9 in China. In the group(> 60), MD of TC between sarcopenia and non-sarcopenia was 2.63, while it was 1.54 in the group(20–60).
Conclusion
Dyslipidemia was associated with sarcopenia in the elderly, which was affected by sex, region and age.
Keywords: Sarcopenia, Dyslipidemia, TC, HDL-C, LDL-C, TG
Introduction
Sarcopenia is defined as the loss of muscle mass and strength which is a comprehensive, progressive pathological change characterized by a reduction in skeletal muscle and a decrease in physical activity in older people.There are differences in body composition and diagnostic methods among people in different regions. The Asia criteria of sarcopenia is (1) grip strength: Male < 28 kg, female < 18 kg (2) 6-meter walking test < 1.0 m/second (3) Simplified Physical Function Assessment (SPPB) ≤ 9 points (4) 5 sit up tests for ≥ 12 s (5) Dual energy X-ray method: male < 7.0 kg/m2, female < 5.4 kg/m2. The European criteria of sarcopenia was: (1) Grip strength: Male < 27 kg Female < 16 kg (2) 6-meter walking test < 0.8 m/second (3) Simplified Physical Function Assessment (SPPB) ≤ 8 points (4) 5 sit up tests for ≥ 15 s. (6) Muscle mass:<7.0 kg/m2 < 5.5 kg/m2. A study [1] from Europe reported that the prevalence of sarcopenia varied from 10% to 27% of people (≥ 60) worldwide, and the prevalence of severe sarcopenia ranged from 2% to 9%. In addition, the prevalence of sarcopenia in older people in Shanghai was 22.9%. Recently, some studies found that the prevalence of dyslipidemia in the elderly was 53.65%, and there was approximately 40% dyslipidemia globally [2]. It was inllustrated that higher TG can elevate the level of ROS, GDF-8, SIR1 and then decrease the synthesis of muscle and ROS is a risk factor of the cardiocascular disease [3].
Some studies have indicated that the association between sarcopenia and dyslipidemia is controversial. To date, data from a study [4] illustrated that the LDL-C of females with sarcopenia was 3.1 mg/dL more than that of non-sarcopenic individuals, and a study by Zhang et al. [5] found that dyslipidemia was associated with increased odds of sarcopenia(OR = 1.506, 95% CI: 1.112 ~ 2.140). However, a study [6] including 1543 older individuals indicated that compared with non-sarcopenic people, the levels of VLDL-C (0.49 ± 0.18 mmol/L), TG (1.57 ± 0.92 mmol/L), and TG/HDL-C (1.26 ± 1.10 mmol/L) in sarcopenic people were significantly lower (P < 0.05). Moreover, a study performed by Yushu Guo [7] demonstrated that there was no significant difference in HDL-C and LDL-C between sarcopenia and non-sarcopenia people. These studies showed a controversial relationship between dyslipidemia and sarcopenia, which prompted us to conduct a meta-analysis to explore the relationship. The results would shed more light on the prevention and treatment of sarcopenia and improving the health condition of older people.
Methods
This research was conducted according to the Preferred Reporting Items for Meta-Analysis (PRISMA) guidelines.
Literature search
Web of Science, PubMed, Cochrane Library, China National Knowledge Infrastructure (CNKI), Wan Fang, China Science and Technology Journal Database (VIP Database) were searched studies demonstrating the association between sarcopenia and dyslipidemia published through August 2023. Our search terms included “sarcopenia (MeSH)” OR “muscle (reduce OR loss)” AND “dyslipidemia (MeSH)” OR “(abnormal OR high) AND (blood fat OR lipid)” OR “TC” OR “LDL-C” OR “HDL-C” OR “TG” OR “TG/HDL-C.”
Selection criteria
The inclusion criteria were as follows: (1) literature published in English or Chinese; (2) topic of studies relevant to the relationship between sarcopenia and dyslipidemia; (3) the variables of the studies including “TG”, “TC”, “HDL-C”, “LDL-C”; and “OR” of sarcopenia and dyslipidemia” (4) applicable data can be extracted.
Duplicate publications, reviews, case reports, literature not published in English or Chinese, literature with inconsistent experimental subjects, inappropriate methods or not including the variables this research needs or necessary data were excluded. Disagreements were resolved by discussion with all investigators.
Data extraction and confirmation
First author, publication year, sample size, odds ratio of sarcopenia and dyslipidemia, the mean values of TC, LDL-C, HDL-C, TG, TG/HDL-C in sarcopenia and non-sarcopenia people, location, gender, age and the criteria of sarcopenia and dyslipidemia were collected in the eligible literature with a standardized diagram.
Literature quality evaluation
Two reviewers (Bingqing Bi and Xinying Dong) evaluated the included literature to illustrate the validity of any findings investigated through the JBI(Joanna Briggs) [8] guidelines. The scoring criteria are as follows: ① 0 points: not meeting the requirements; ② 1 point: mentioned but not described in detail; ③ 2 points: detailed, comprehensive, and accurate description.When two reviewers have different opinions on the same article, we will discuss and propose solutions with Shugang Li.
Statistical analysis
Excel 2021 was used for unit conversion of TC and LDL-C. HDL-C and TG from mol/L to mg/dl. Meta-analysis of the OR(Odds Ratio) between sarcopenia and dyslipidemia and the MD(Mean Difference) between TC, LDL-C, HDL-C, TG, TG/HDL-C and sarcopenia were performed by Review Manager 5.3. When I² was higher than 50%, the random effect model was used; when I² was less than 50%, the fixed effect model was performed. Subgroup analysis was carried out to explore the cause of heterogeneity. In addition, a funnel plot of the OR was conducted to assess whether there was publication bias in the research results, and a sensitivity analysis with Stata 16.0 was performed to evaluate the reliability of the results.
Results
Study selection
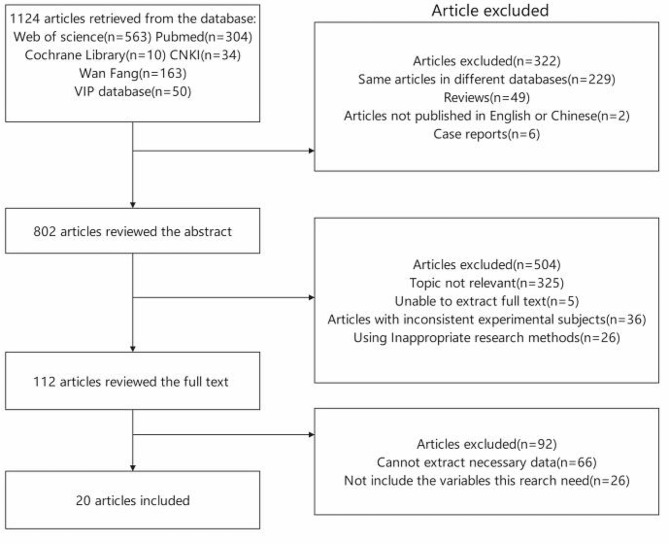
The search process identified 1124 articles from 6 databases. Among them, 529 same articles in different databases, 49 reviews, 2 studies not published in English or Chinese, and 6 case reports were excluded by skimming the title. After reading the abstracts, the main reasons for exclusion were that the topic of the paper was not relevant to the association between sarcopenia and dyslipidemia, research was unable to extract full text, studies with inconsistent experimental subjects and inappropriate methods were used. Moreover, studies in which the necessary data could not be extracted and the variables this research needed were not included were excluded. Ultimately, twenty original case‒control studies [5, 6, 7, 9–25] met the inclusion criteria. The article selection process is shown in Fig. 1.
Fig. 1.
Flow chart of the selection process
Study characteristics
The characteristics of studies are presented in Table 1, including the first author, country, age and the indicators this research includes. The studies were performed in America, China, Korea and Syrian Arab Republic, and only one subject was under 60 years old. However, the odds ratio of sarcopenia and dyslipidemia, the average values of TC, TG, HDL-C, LDL-C, and TG/HDL-C in sarcopenia and nonsarcopenia people and the sample size were manifested in the forest plot (Figures 2, 3, 4, 5, 6 and 7; Table 3).
Table 1.
Characteristics of studies
| No. | Research | Country | Age/years | The indicators this research include | Diagnostic criteria of sarcopenia |
Diagnostic criteria of dyslipidemia |
|---|---|---|---|---|---|---|
| 1 | S. J. Baek [4] | Korea | ≧ 65 | 2,3,4,5,6,7,9 | Asia criteria1a | Criteria5 |
| 2 | Yuan Zhang [5] | China | ≧ 60 | 1,8 | Asia criteria1a | Critertia1 |
| 3 | Jiaojiao Li [6] | China | ≧ 60 | 2,3,4,5,9 | Asia criteria1a | Criteria3 |
| 4 | Hanyi Zou [9] | China | ≧ 60 | 1,8 | Asia criteria1a | Criteria2 |
| 5 | Peipei Han [10] | China | ≧ 60 | 1,8 | Asia criteria1a | Criteria4 |
| 6 | Yu Wang [11] | China | ≧ 60 | 2,3,4,5,9 | Asia criteria2d | Criteria3 |
| 7 | Rui Cheng [12] | China | ≧ 60 | 1,8 | Asia criteria1a | Criteria4 |
| 8 | Lijuan Wang [13] | China | ≧ 60 | 2,3,4,5 | Asia criteria1a | Criteria4 |
| 9 | Hee-Sook Lim [14] | America | ≧ 60 | 1,8 | Europena criteriab | Criteria6 |
| 10 | Yourui Xu [15] | China | ≧ 60 | 2,5 | Asia criteria1a | Criteria2 |
| 11 | Ruirui Hao [16] | China | ≧ 60 | 2,3,4,9 | Asia criteria3e | Criteria3 |
| 12 | Nan Wang [17] | China | ≧ 60 | 2,3,4,5,6,9 | Asia criteria1a | Criteria2 |
| 13 | Xuelian Zhang [18] | China | ≧ 60 | 2,3,4,5 | Asia criteria1a | Criteria3 |
| 14 | Syed Shahid Habib [19] | Syrian Arab Republic | ≧ 60 | 2,4,5 | Syrian Arab Republic’s criteriac | Criteria6 |
| 15 | Yanping Du [20] | China | ≧ 65 | 2,3,4,5,7,9 | Asia criteria1a | Criteria1 |
| 16 | Ana Coto Montes [21] | Korea | ≧ 60 | 1,2,3,4,5,7,8,9, | Asia criteria1a | Criteria6 |
| 17 | Seong-Joon Park [22] | Korea | ≧ 60 | 4,5 | Asia criteria1a | Criteria7 |
| 18 | Jun-Hyuk Lee [23] | Korea | ≧ 60 | 2,3,4,5 | Asia criteria1a | Criteria8 |
| 19 | K Sanada [24] | Japan | ≧ 60 | 4,5,6 | Asia criteria1a | Ctiteria6 |
| 20 | Qifan Zhou [25] | China | 20–60 | 2,9 | Asia criteria1a | Criteria2 |
Indicators:1:Overall OR,2:Overall TC MD,3:Overall LDL-C MD,4:Overall HDL-C MD,5:Overall TG MD,6:Overall TG/HDL-C, 7:Subgroup analysis of gender, 8:Subgroup analysis of area, 9:Subgroup analysis of age
a(i) skeletal muscle mass index (BIA) of the limbs: <7.0 kg/m2 for men < 5.7 kg/m2 for women; (ii) assessment of physical function: 6-meter stride < 1.0 m/s or SPPB score ≤ 9 or standing test ≥ 12 s; (iii) grip strength: <28 kg for men and < 18 kg for women; if ① and ② or③ were satisfied, the diagnosis of sarcopenia was made;
bMuscle mass decreased by dual energy X-ray absorptiometry (DXA)was divided by body weight and calculated as a percentage. When the calculated value was less than 1 standard deviation (SD), it was classified as sarcopenia.
cAuthors analyzed appendicular lean mass (ALM) and hand grip strength test (HGS). Total and percent lean mass and TLM/ ht2 were calculated. ALM is the sum of arm and leg lean mass, and ALM/ht2 was also calculated. The sarcopenia was defined when the ALM/ht2 was less than 7.46.
dSkeletal muscle mass index (SMI) = Skeletal muscle mass/body weight ×100%, Sarcopenia is defined as a condition where the standard deviation is 2 times lower than that of the young control group (18–39 years old) of the same sex
eThe calculation of skeletal muscle index (SMI) based on imaging to determine the presence of sarcopenia is calculated by dividing the total muscle area by the square of height. The threshold for diagnosing sarcopenia is less than 42.6 cm2/m2 for males and less than 30.6 cm2/m2 for females
Critertia1:TC ≥ 6.2 mmol/L、HDL-C ≥ 4.1 mmol/L、HDL-C ≤ 1.0 mmol/L、TG ≥ 2.3 mmol/L or use lipid-lowering drugs
Criteria2: TC ≥ 6.2 mmol/L、HDL-C ≥ 4.1 mmol/L、HDL-C ≤ 1.0 mmol/L、TG ≥ 2.3 mmol/L
Criteria3:LDL-C ≥ 3.37mmol/L, HDL-C<1.04mmol/L, TC ≥ 5.18mmol/L,TG ≥ 1.7mmol/L
Criteria4:TG ≥ 2.26 mmol/L, TC ≥ 6.22mmol/L, LDL -C ≥ 4.14 mmol/L, HDL-C ≤ 1.04mmol/L
Criteria5:TG > 400 mg/dL, HDL-C ≤ 160 mg/dL, TG/HDL-C>4
Criteria6: TG > 150 mg/dL, HDL-C < 40 mg/dL
Criteria7:TG > 150 mg/dL,HDL-C < 40 mg/dL for males or < 50 mg/dL for females or use of dyslipidemia medication
Criteria8: HDL-C < 40 mg/dL
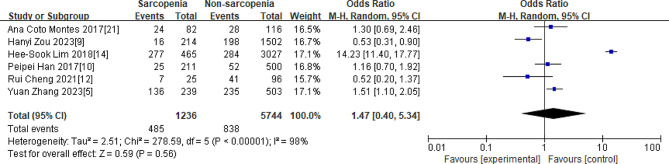
Fig. 2.
Overall OR of the relationship between sarcopenia and dyslipidemia
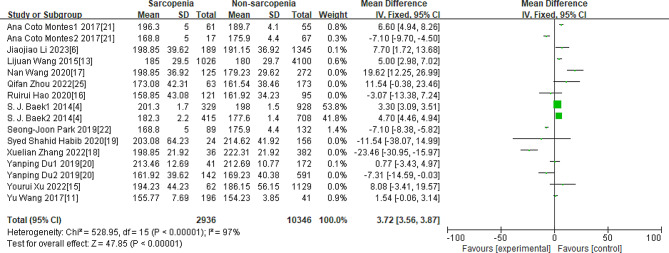
Fig. 3.
Overall MD of the average TC value between sarcopenia and nonsarcopenia people
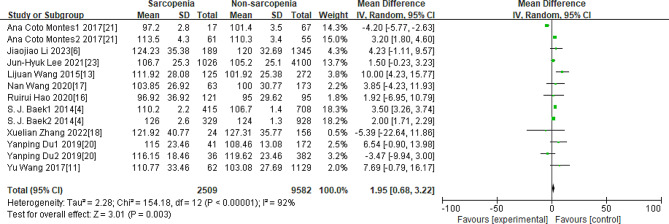
Fig. 4.
Overall MD of the average LDL-C value between sarcopenia and nonsarcopenia people
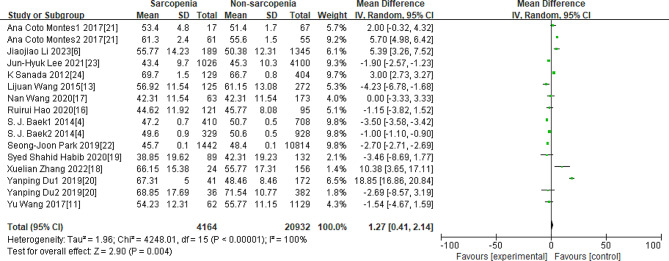
Fig. 5.
Overall MD of the average HDL-C value between sarcopenia and nonsarcopenia people
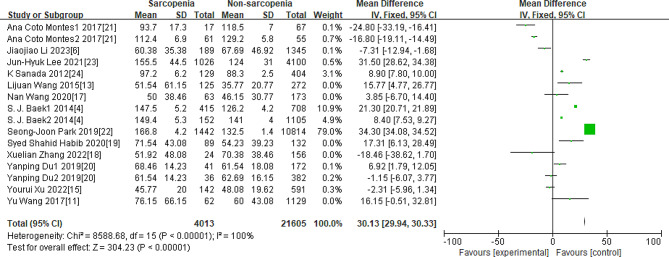
Fig. 6.
Overall MD of the average TG value between sarcopenia and nonsarcopenia people
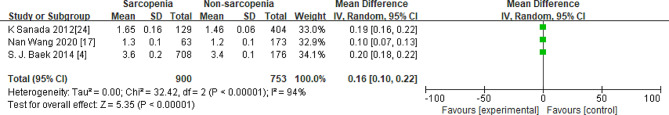
Fig. 7.
Overall MD of the average TG/HDL-C value between sarcopenia and nonsarcopenia people
Table 3.
Subgroup analysis by gender, region and age
| Factor | Indicator of the meta- analysis |
Number of the research |
Effect Variable | The result of the meta-analysis | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 95% CI | I²(%) | Z | P | 95% CI | I²(%) | Z | P | ||||
| Female | Male | ||||||||||
| Gender | TC | 3 | MD |
-1.67 [-7.36,4.01] |
97% | 0.58 | < 0.00001 |
-0.51 [-8.76,7.75] |
98% | 0.12 | < 0.00001 |
| LDL-C | 3 | MD |
2.21 [0.78,3.63] |
63% | 3.04 | < 0.00001 |
1.41 [-4.98,7.79] |
97% | 1.69 | < 0.00001 | |
| HDL-C | 3 | MD |
1.02 [-4.57,6.61] |
99% | 0.36 | < 0.00001 |
5.77 [-8.13,19.66] |
100% | 3.47 | < 0.00001 | |
| TG | 3 | MD |
-3.18 [-21.63, 15.28] |
100% | 0.34 | < 0.00001 |
-0.67 [-11.49,10.14] |
100% | 0.12 | < 0.00001 | |
| China | Non-China | ||||||||||
| Region |
Total rate of the dyslipidemia |
6 | OR |
0.90 [0.52,1.56] |
98% | 0.59 | <0.00001 |
4.38 [0.41,5.34] |
78% | 0.38 | 0.004 |
| More than 60 years | Less than 60 years | ||||||||||
| Age | TC | 11 | MD |
2.63 [0.92,4.35] |
98% | 6.13 | < 0.00001 |
1.54 [-0.89, 4.12] |
----- | 1.25 | 0.0002 |
Methodological quality assessment
Joanna Briggs was conducted to evaluate the quality of the studies we included, and the results of the assessment are listed in Table 2. The fact that the score of 19 studies was more than 15 indicated that the quality of the studies we included was relatively better. The score of the study by Qifan Zhou were ≤ 1 in the aspect, including study population, the inclusion and exclusion criteria, sample features etc(② ③ ④ ⑥ ⑦ ⑧ ⑩, Table 2).
Table 2.
Results of methodological quality assessment using the JBI
| Number | Research | ① | ② | ③ | ④ | ⑤ | ⑥ | ⑦ | ⑧ | ⑨ | ⑩ | Overall |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Ana Coto Montes | 2 | 2 | 2 | 1 | 2 | 2 | 1 | 2 | 2 | 1 | 17 |
| 2 | Hanyi Zou | 2 | 1 | 2 | 1 | 1 | 1 | 1 | 2 | 2 | 1 | 14 |
| 3 | Hee-Sook Lim | 2 | 2 | 2 | 2 | 2 | 2 | 1 | 2 | 1 | 1 | 17 |
| 4 | Jiaojiao Li | 1 | 2 | 2 | 1 | 2 | 2 | 1 | 2 | 2 | 2 | 17 |
| 5 | Jun-Hyuk Lee | 2 | 2 | 2 | 2 | 2 | 2 | 1 | 2 | 2 | 1 | 18 |
| 6 | K Sanada | 2 | 2 | 2 | 1 | 1 | 2 | 1 | 1 | 2 | 2 | 16 |
| 7 | Lijuan Wang | 2 | 1 | 2 | 1 | 2 | 2 | 1 | 1 | 1 | 2 | 15 |
| 8 | Nan Wang | 1 | 2 | 2 | 1 | 2 | 2 | 1 | 2 | 1 | 1 | 15 |
| 9 | Peipei Han | 2 | 2 | 2 | 2 | 1 | 2 | 1 | 2 | 2 | 2 | 18 |
| 10 | Qifan Zhou | 2 | 1 | 1 | 1 | 2 | 0 | 1 | 1 | 2 | 1 | 12 |
| 11 | Rui Cheng | 2 | 2 | 2 | 2 | 2 | 2 | 1 | 2 | 2 | 2 | 19 |
| 12 | Ruirui Hao | 2 | 2 | 2 | 1 | 1 | 1 | 1 | 1 | 2 | 2 | 15 |
| 13 | S. J. Baek | 2 | 2 | 2 | 2 | 2 | 1 | 1 | 2 | 2 | 2 | 18 |
| 14 | Seong-Joon Park | 2 | 2 | 2 | 2 | 2 | 2 | 1 | 2 | 2 | 2 | 19 |
| 15 | Syed Shahid Habib | 2 | 2 | 2 | 2 | 2 | 1 | 1 | 2 | 1 | 2 | 17 |
| 16 | Xuelian Zhang | 2 | 1 | 2 | 2 | 2 | 1 | 1 | 2 | 1 | 1 | 15 |
| 17 | Yanping Du | 1 | 2 | 2 | 2 | 2 | 1 | 1 | 2 | 1 | 1 | 15 |
| 18 | Yourui Xu | 2 | 2 | 2 | 2 | 2 | 1 | 1 | 2 | 1 | 2 | 17 |
| 19 | Yu Wang | 2 | 2 | 2 | 2 | 2 | 1 | 1 | 2 | 1 | 2 | 17 |
| 20 | Yuan Zhang | 2 | 2 | 2 | 2 | 1 | 2 | 1 | 1 | 2 | 2 | 17 |
Evaluation criteria:① Is the research purpose clear? Is the basis for setting the question sufficient?②How was the study population selected (whether the study subjects were randomly selected, and whether stratified sampling was adopted to improve sample representativeness)?③Does clearly describe the inclusion and exclusion criteria for the sample?④Does clearly describe the sample features?⑤Does the tool for collecting data have reliability and validity (If using an investigator survey, how is the repeatability of the survey results)?⑥What are the measures to verify the authenticity of the information?⑦Does consider ethical issues?⑧Is the statistical method correct?⑨Are the statements of the research results appropriate and accurate? Are the results distinguished from the inference, and are the results faithful to the data rather than the inference?⑩Have you provided a clear explanation of the research value?
0 points: Not meeting the requirements; 1 point: mentioned but not described in detail; 2 points: Detailed, comprehensive, and accurate description
Association between Sarcopenia and dyslipidemia
Overall OR of the relationship between Sarcopenia and dyslipidemia
As shown in Fig. 2, the overall OR of the relationship between sarcopenia and dyslipidemia was 1.47[0.40,5.34], Z = 0.59, P = 0.56.
Overall MD of TC, LDL-C, HDL-C, TG, and TG/HDL-C values between the Sarcopenia and non-sarcopenia
As Figs. 3, 4, 5, 6 and 7 were shown, the overall Mean Difference of the average TC, LDL-C, HDL-C, TG, TG/HDL-C value was 3.72[3.56,3.87](P < 0. 00001), 1.95[0.68,3.22](P = 0.003), 1.27[0.41,2.14](P = 0.004), 30.13[29.93,30.33](P < 0. 00001), 0.16[0.10,0.22](P < 0. 00001). The heterogeneity of the TC, LDL-C, HDL-C, TG, TG/HDL-C were significantly. Therefore, subgroup analysis was performed to analyze the origin of the heterogeneity.
Note for Figs. 3–7: Some studies only had the average values of TC, LDL-C, HDL-C, and TG in females and males, so we also included them in our research. The number “1” represents females, and the number “2” represents males. The unit of “mmol/L” was converted to “mg/dL”.
Subgroup analysis of gender, region and age
Subgroup analysis of sex, region and age is shown in Table 3. In female, compared with the non-sarcopnia, the MD of TC, LDL-C, HDL-C, TG of sarcopenia were − 1.67,2.21,1.02,-3.18 respectively. In male, the MD of TC, LDL-C, HDL-C, TG between sarcopenia and non-sarcopenia were − 0.51, 1.41, 5.77, -0.67. The OR between sarcopenia and dyslipidemia of the non-China region was 4.38, and it was 0.9 in China. In the group(> 60), MD of TC between sarcopenia and non-sarcopenia was 2.63, while it was 1.54 in the group(20–60).
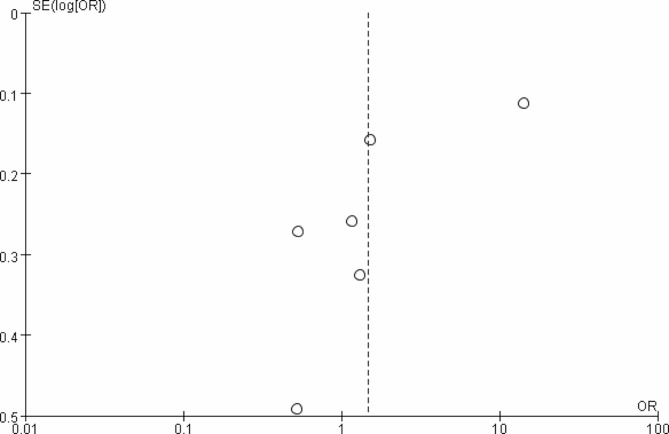
Publication bias
The publication bias was presented in Fig. 8, which showed the asymmetry distribution of the articles. No significant bias was observed in this research.
Fig. 8.
Bias analysis
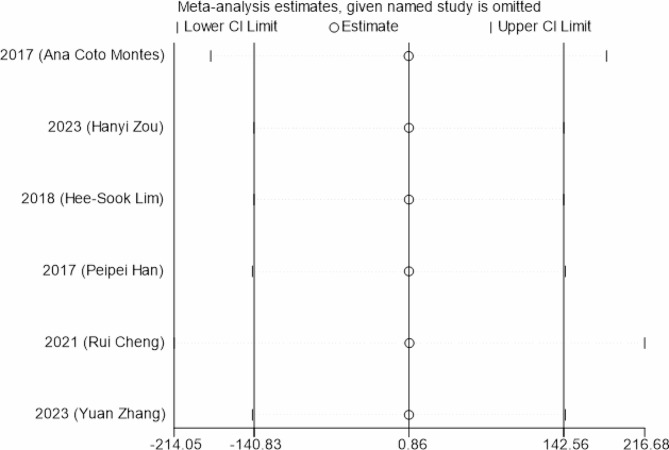
Sensitivity analysis
From Fig. 9, it was shown that the value of the sensitivity analysis was relatively concentrated, which demonstrated the reliability of the results.
Fig. 9.
Sensitivity analysis
Discussion
The results of the present study showed that sarcopenia was positively associated with dyslipidemia. The overall OR was 1.47[0.40,5.34], and the total mean differences in TC, LDL-C, HDL-C, TG, and TG/HDL-C were 1.10[-0.50,2.71], 1.95[0.68,3.22], 1.27[0.41,2.14], 30.13[29.93,30.33], and 0.16[0.10,0.22] respectively, indicating that there was a difference in lipids between sarcopenia and non-sarcopenia patients.These results provided references for the prevention and control of sarcopenia.
In female, compared with the non-sarcopnia, the MD of TC, LDL-C, HDL-C, TG of sarcopenia were − 1.67,2.21,1.02,-3.18 respectively. In male, the MD of TC, LDL-C, HDL-C, TG between sarcopenia and non-sarcopenia were − 0.51, 1.41, 5.77, -0.67. It seemed that the difference between genders could be interpreted for many reasons, especially different hormone level [26]. With aging, the decrease in androgen levels led to less synthesis of skeletal muscle proteins. Correspondingly, the decreasing estrogen level may be associated with the rise of TNF-α, IL-6 and other inflammatory factors and then reduce the mass of the muscle [27]and the decrease of estrogen levels leads to mitochondrial dysfunction and muscle loss, mitochondrial division in satellite cells [28], the loss of energy can cause the electron transport chain (ETC) out of control, leading to low oxidative phosphorylation metabolism and mitochondrial phagocytosis efficiency, and increase oxidative stress, then decline the synthesis of muscle [29]. A study by Xiaoling Luo [30] stated that the decrease in estrogen levels affects the activity of multi-chain lipase and reduces the synthesis of HDL-C. Another study indicated that after menopause, women’s estrogen levels decreased and their inhibitory effect on liver enzymes weakened, leading to an increase in TG levels [31]. In addition, testosterone can affect the activity of tricarboxylic acid cycle enzymes, promote free fatty acids to enter the tricarboxylic acid cycle for oxidation, and reduce cholesterol synthesis [32]. Therefore, it could be inferred that the difference between androgen and estrogen affected the MD values of LDL-C, TG, HDL-C, and TG in females and males.
A study [33] indicated that the increase in lipids was proportional to the mass intake of red meat, fast food, such as clips [34], and sugary drinks, which is a habit of regions such as Europe and Korea [35]. The OR between sarcopenia and dyslipidemia of the non-China region was 4.38, and it was 0.9 in China. Compared with the non-China region, the Chinese relatively preferred the food made from wheat, flour, fruits and vegetables, which was in reverse ratio of increased lipid and European people ate the red meat more.
It was reported that C-reactive protein (CRP) was associated with degenerative changes, so CRP may be a driving factor of sarcopenia [36]. In the group(> 60), MD of TC between sarcopenia and non-sarcopenia was 2.63, while it was 1.54 in the group(20–60). In addition, compared with that of non-sarcopenic elderly people, the leptin level of sarcopenic elderly people was evidently increased [37].
It must be acknowledged that limitations existed in this meta-analysis.First, the diagnostic criteria of sarcopenia was different between Asia and Europe, which may be the origin of the heterogeneity. Second, the subgroup analysis of small metabolic molecules, such as P3NP, IL-6, TNF-α, and FGF-21, was not conducted as a result of the limited original studies. Moreover, all the included studies were case‒control studies, and the causality relationship could not be inferred.
Conclusion
Dyslipidemia was associated with sarcopenia in the elderly, and sex, region and age were the influencing factors. Subsequent studies were proposed to elucidate the relationship between sarcopenia and dyslipidemia to explore the mechanism of the relationship between them.
Acknowledgements
Not applicable.
Author contributions
Bingqing Bi: designed and extracted the data, evaluated the quality of the literature and wrote the manuscript. Xinying Dong: designed and evaluated the quality of the literature and participated in the discussion. Shugang Li and Hao Wu: designed and controlled the quality of the manuscript and revised the manuscript. Meilin Yan, Zhuo Zhao and Ruitong Liu: data extraction.
Funding
This work was supported by the Beijing High Level Public Health Technical Talents Training Plan (2022-1-005, Key Discipline Member-02-44).
Data availability
The datasets used during the present study are available from the corresponding author on reasonable request.
Declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
Not applicable(This paper is a secondary literature analysis based on other original articles. The original articles we analyzed passed the ethical review, but the analysis in this paper does not need ethical review again.)
Consent for publication
Not applicable.
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Bingqing Bi and Xinying Dong contributed equally.
Contributor Information
Shugang Li, Email: lishugang@ccmu.edu.cn.
Hao Wu, Email: wushunzhe@ccmu.edu.cn.
References
- 1.Petermann-Rocha F, Balntzi V, Gray SR, et al. Global prevalence of Sarcopenia and severe Sarcopenia: a systematic review and meta‐analysis[J] J Cachexia Sarcopenia Muscle. 2022;13(1):86–99. doi: 10.1002/jcsm.12783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Huang QX, Wen YT, Huang J et al. Prevalence of dyslipidemia and its influencing factors among elderly community residents [J]. Chinese General Practice, 2023, 26(28):3520–3525. http://kns.cnki.net/kcms/detail/13.1222.R20230625.1511.035.html.
- 3.Yang X. Study on the intervention effect and mechanism of n3 polyunsaturated fatty acids and wheat oligopeptides on Sarcopenia based on proteomics. DongNan Univ. 2021 doi: 10.27014/d.cnki.gdnau.2021.003966. [DOI] [Google Scholar]
- 4.Baek SJ, Nam GE, Han KD, et al. Sarcopenia and sarcopenic obesity and their association with dyslipidemia in Korean elderly men: the 2008–2010 Korea National Health and Nutrition Examination Survey[J] J Endocrinol Investig. 2014;37(3):247–60. doi: 10.1007/s40618-013-0011-3. [DOI] [PubMed] [Google Scholar]
- 5.Zhang Y, Han ZF. Risk factors for Sarcopenia among elderly individuals: a case–control study[J] J Prev Med. 2023;35(06):461–4. doi: 10.19485/j.cnki.issn2096-5087.2023.06.001. [DOI] [Google Scholar]
- 6.Li JJ, Chen Y, Zhang H, et al. Association between blood lipid profile and sarcopenia in elderly people in one community in Suzhou[J] Chin J Multiple Organ Dis Elder. 2023;22(01):6–11. doi: 10.11915/i.issn.1671-5403.2023.01.002. [DOI] [Google Scholar]
- 7.Guo YS, Xue Q, Weu YN, et al. Prevalence and risk factors of Sarcopenia in obese Elderly Adults[J] Chin Gen Pract. 2021;24(24):3048–53. doi: 10.12114/i.issn.1007-9572.2021.00.530. [DOI] [Google Scholar]
- 8.Grammatopoulos T, Hunter JWS, Munn Z, Stone JC, Barker TH. Reporting quality and risk of bias in JBI systematic reviews evaluating the effectiveness of interventions: a methodological review protocol. JBI Evid Synth. 2023;21(3):584–91. doi: 10.11124/JBIES-22-00317. [DOI] [PubMed] [Google Scholar]
- 9.Zou HY, Wang YH, Gao M. Prevalence and influencing factors of Sarcopenia in community elderly[J] Clin Res. 2023;37(03):246–50. doi: 10.3969/.1ssn.1003-9198.2023.03.009. [DOI] [Google Scholar]
- 10.Han PP, Yu HR, Ma YX, et al. The increased risk of Sarcopenia in patients with cardiovascular risk factors in Suburb-Dwelling older Chinese using the AWGS definition[J] Sci Rep. 2017;7(1):9592. doi: 10.1038/s41598-017-08488-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wang Y, Jiang MX, Xu Q, et al. Correlation of Sarcopenia and metabolic risk factors[J] J Med Postgraduates. 2017;30(2):181–5. doi: 10.16571/i.cnki.1008-8199.2017.02.015. [DOI] [Google Scholar]
- 12.Cheng R, Wang J, Zhang KY, et al. Assessment of risk factors associated with sarcopenia under according toAsian Working Group for Sarcopenia 2019 Consensus[J] J HeBei Med Univ. 2021;42(12):1421–5. doi: 10.3969/i.issn.1007-3205.2021.12.012. [DOI] [Google Scholar]
- 13.Wang LJ, Wang MF, Li XL, et al. Correlation between sarconenic obesity and dyslipidemia in the voung and middle aged adults [J] Chin J Health Manage. 2015;8(3):186–90. doi: 10.3760/cmajisn.1674-0815.2015.03.009. [DOI] [Google Scholar]
- 14.Lim H-S, Park Y-H, Suh K, et al. Association between Sarcopenia, Sarcopenic Obesity, and Chronic Disease in Korean Elderly[J] J Bone Metabolism. 2018;25(3):187. doi: 10.11005/jbm.2018.25.3.187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Xu YR, Cai WW, Chen Y, et al. Correlation between Sarcopenia and nutritional status among elderly population in some communities of Shanghai[J] Chin J Clininal Healthc. 2022;25(5):605–9. doi: 10.3969/J.issn.1672-6790.2022.05.006. [DOI] [Google Scholar]
- 16.Hao RR, Wang H, Wang HY, et al. Analysis of risk factors or serile srcopunin and its relationship with NAFID[J] J Clin Experimental Med. 2020;19(15):1588–91. doi: 10.3969/1.issn.1671-4695.2020.15.006. [DOI] [Google Scholar]
- 17.Wang N, Wei YN, Liu J, et al. Related factors for Sarcopenia in Elderly Hospitalized patients with Chronic Diseases[J] Chin Genenral Pract. 2020;23(5):611–6. doi: 10.12114/j.issn.1007-9572.2020.00.006. [DOI] [Google Scholar]
- 18.Zhang XL, Sha M, Yang DY, et al. Prevalence and influencing factors of Sarcopenia in the middle agedand elderly of Bai ethnic group in Gusheng village,Dali city[J] J Community Med. 2022;20(9):479–84. doi: 10.19790/j.cnki.JCM.2022.09.02. [DOI] [Google Scholar]
- 19.Habib SS, Alkahtani S, Alhussain M et al. Sarcopenia coexisting with high adiposity exacerbates insulin resistance and dyslipidemia in Saudi adult Men[J]. Diabetes, metabolic syndrome and obesity: targets and therapy, 2020(13): 3089–97. 10.2147/DMSO.S260382. [DOI] [PMC free article] [PubMed]
- 20.Du YP, Wang X, Xie H, et al. Sex differences in the prevalence and adverse outcomes of Sarcopenia and sarcopenic obesity in community dwelling elderly in East China using the AWGS criteria[J] BMC Endocr Disorders. 2019;19(1):109. doi: 10.1186/s12902-019-0432-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Coto Montes A, Boga JA, Bermejo Millo C, et al. Potential early biomarkers of Sarcopenia among independent older adults[J] Maturitas. 2017;104:117–22. doi: 10.1016/j.maturitas.2017.08.009. [DOI] [PubMed] [Google Scholar]
- 22.Park S-J, Ryu S-Y, Park J, et al. Association of Sarcopenia with metabolic syndrome in Korean Population using 2009–2010 Korea National Health and Nutrition Examination Survey[J] Metab Syndr Relat Disord. 2019;17(10):494–9. doi: 10.1089/met.2019.0059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lee J-H, Lee HS, Cho A-R, et al. Relationship between muscle mass index and LDL cholesterol target levels: analysis of two studies of the Korean population[J] Atherosclerosis. 2021;325(10):1–7. doi: 10.1016/j.atherosclerosis.2021.01.016. [DOI] [PubMed] [Google Scholar]
- 24.Sanada K, Iemitsu M, Murakami H, et al. Adverse effects of coexistence of Sarcopenia and metabolic syndrome in Japanese women[J] Eur J Clin Nutr. 2012;66(10):1093–8. doi: 10.1038/ejcn.2012.43. [DOI] [PubMed] [Google Scholar]
- 25.Zhou QF, Yin LX, Zhang HL et al. Establishment and yalidation of a predictive modelfor sarcopenia in young and middle-aged patientswith maintenance hemodialysis[J]. Journal of Clinical Medicine in Practice, 2022, 26(05):44–47 + 53. 10.7619/jcmp.20214338.
- 26.Liao YX, Peng Z, Chen L, et al. Prospective views for whey protein and/or resistance training against age-related Sarcopenia[J]. Aging Dis. 2018;9(6):1–17. 10.14336/AD.2018.0325. [DOI] [PMC free article] [PubMed]
- 27.Huang XJ, Luo TJ. Research progress on risk factors and pathogenesis of sarcopenia[J] Practical Geriatr. 2020;34(01):81–5. doi: 10.3969/j.Issn.1003-9198.2020.01.024. [DOI] [Google Scholar]
- 28.Wu YB, Zhu JH,Song WD, et al. The relationship hetween estrogen level and blood lipid.blood glucose and blood homocysteine in postmenopausal women[J] Chin J Lab Diagn. 2023;33(07):1248–51. [Google Scholar]
- 29.Li KJ, Wu CC,Xiang YJ, et al. Analysis of the relationship between estrogen levels and blood homocysteine, blood lipids. In postmenopausal female patients with coronary heart disease [J]. Volume 14. Prevention and Treatment of Cardio-Cerebral-Vascular Disease; 2014. pp. 222–4. 03.
- 30.Luo XL, Zhang L. Wu LH.The effects of low estrogen levels on blood pressure, blood lipids, and bone density in postmenopausal women[J] Maternal Child Health Care China. 2018;33(24):5877–9. [Google Scholar]
- 31.Shen XB, Xiong SM, Liu FW et al. Correlation of serum androgen levels with lipid metabolism in middle-aged andelderly men in Zunyi, Guizhou [J]. National Joumnal of Andrology,2018,24(04):311–6. 10.13263/j.cnki.nja.2018.04.004. [PubMed]
- 32.Chen J, Wang MY,Zhu PW, et al. Correlations between partial androgen deficiency and glucose and lipidprofiles in middle-aged and elder men [J] Chin J Public Health. 2018;34(06):871–3. [Google Scholar]
- 33.Chen XC, Kong CQ, Xu L, et al. Osteosarcopenic obesity syndrome: diagnosis, treatment and related influencing factors[J] Chin J Tissue Eng Res. 2020;24(11):1777–82. doi: 10.3969/j.issn.2095-4344.2432. [DOI] [Google Scholar]
- 34.El-kassas G, Ziade F. Exploration of the risk factors of generalized and Central Obesity among adolescents in North Lebanon. J Environ Public Health[J] 2017;2017:1–13. doi: 10.1155/2017/2879075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mozaffarian D, Hao T, Rimm EB, et al. Changes in diet and lifestyle and long-term weight gain in women and men[J] N Engl J Med. 2011;364(25):2392–404. doi: 10.1056/NEJMoa1014296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lin TP, Yue JR. Exploring the pathogenesis of Sarcopenia from serum inflammatory markers[J] Practical Geriatr. 2019;33(09):833–5. doi: 10.3969/j.issn.1003-9198.2019.09.001. [DOI] [Google Scholar]
- 37.Xu LR, Zhang JX. Research progress on the differential role of adipokines in sarcopenia[J] Military Med Joint Logistics. 2023;37(03):267–71. doi: 10.13730/j.issn.2097-2148.2023.03.018. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used during the present study are available from the corresponding author on reasonable request.