Highlights
-
•
Uterine transposition might represent a valid option for fertility preservation in women who require pelvic radiotherapy.
-
•
However, studies that assess its viability, effectiveness, and safety are required.
-
•
Menses and hormonal function are maintained after uterine transposition.
Keywords: Uterine transposition, Vulvar cancer, Pelvic radiotherapy, Fertility preservation
Abstract
Objective
To report the first uterine transposition for fertility preservation in a patient with vulvar cancer.
Case: A 26-year-old nulliparous patient with stage IIIB vulvar cancer, which was resected with adequate margins and bilateral inguinofemoral lymphadenectomy.
Laparoscopic transposition of the uterus to the upper abdomen, outside of the scope of radiation was performed to preserve fertility and ovarian function. After the end of radiotherapy, the uterus was repositioned into the pelvis.
Main Outcome Measure: Uterine and ovarian function preservation.
Result
The patient recovered her menstrual cycles spontaneously 1 month after the reimplantation and exhibited normal variation in ovarian hormones.
Twelve months after the surgery, the uterus was normal and there was no sign of recurrent disease.
Conclusion
Uterine transposition might represent a valid option for fertility preservation in women who require pelvic radiotherapy. However, studies that assess its viability, effectiveness, and safety are required.
1. Introduction
Advances in oncologic treatments and the increase in survival rates have brought new priorities to the forefront in the planning of treatment strategies. Aspects related to quality of life, particularly fertility preservation in young cancer patients, are among the most essential elements to be considered (Jeruss and Woodruff, 2009). For this reason, different fertility preservation strategies have been developed in the last few years (Oktay et al., 2018).
Pelvic radiotherapy is an essential component of treating various pelvic tumors, such as those affecting the rectum, anus, soft tissue sarcomas, and gynecologic cancers. However, pelvic radiation can lead to irreversible side effects like premature ovarian insufficiency, uterine fibrosis and endometrial injury (Wallace et al., 2005, Wo Jennifer and Viswanathan, 2009).Oocytes are extremely sensitive to radiotherapy, almost 50 % of oocytes may be damaged with a dose of 2 Gy, causing immediate and irreversible damage (Wallace et al., 2005, Wo Jennifer and Viswanathan, 2009). All these factors may lead to infertility, even with minimal doses of radiotherapy (Wallace et al., 2005, Wo Jennifer and Viswanathan, 2009). The only fertility preservation standardized options for these patients are embryo and oocyte cryopreservation as well as ovarian transposition to protect ovarian function (Oktay et al., 2018). However, none of these options enable patients to carry a pregnancy, leaving uterine surrogacy as the sole possibility. Surrogacy is addressed in the Assisted Reproductive Treatments national law but it is subjet to significant limitations in terms of access (Ley de Reproducción Asistida, 2013). Therefore, in such cases, oocyte and embryo cryopreservation used to be the only fertility preservation strategies available to safeguard future fertility or the possibility of having genetically related children (Oktay et al., 2018).
Uterine transposition (UT) was initially described by Ribeiro et al. in 2017 as a technique that enables the preservation of uterine and gonadal function in patients with rectal cancer requiring pelvic radiation (Ribeiro et al., 2017). Since this procedure began to be implemented, numerous international case reports have been published, and, more recently, three newborns have been reported in the international literature following UT (Baiocchi et al., 2018, Odetto et al., 2021, Baiocchi et al., 2021, Ribeiro et al., 2023, Lopez et al., 2023, Ribeiro et al., 2023).
The aim of this manuscript is to provide the first case report of UT in a patient with locally advanced vulvar cancer.
2. Case
The clinical case pertains to a 26-year-old nulliparous patient, with no pre-existing medical conditions but a prolonged history of vulvar itching. She was referred to our medical center due to a 3 cm vulvar ulcerated lesion on the left labia majora and a 1 cm lesion in the clitoris, with a fusion of labia minora and clinically palpable inguinofemoral nodes (Fig. 1A). The anatomical modifications observed in the vulva were indicative of vulvar lichen sclerosus. Biopsies confirmed a moderately differentiated vulvar squamous carcinoma that was non-HPV related, p16 negative, and p53 mutated. A pelvic MRI revealed a 17 mm lesion near the urethra and a second 32 mm lesion in the posterior region of the left labia majora. At the inguinofemoral level, pathological lymph nodes were identified on the left side, which were in contact with each other, forming a mass measuring 41 x 33 mm. No other inguinofemoral lymph nodes were identified, and there was no evidence of distant disease.
Fig. 1A.
Vulvar ulcerated lesion.
During the treatment planning phase, the patient initiated a controlled ovarian stimulation protocol for oocyte cryopreservation. The selected protocol involved a short regimen with recombinant FSH 3000 IU and GnRH antagonist 0.25 mg per day, for 10 days. Finally, a dual trigger with 250 IU of HCG and 0.2 GnRH analogues was administered to optimize results. The patient exhibited an asymmetric response to stimulation and successfully cryopreserved 6 Metaphase II oocytes.
The treatment plan and the adverse effects were thoroughly discussed with the patient, who verbally expressed her desire to preserve fertility. Initially, the objective was to preserve fertility trough the cryopreservation of oocytes and the implementation of ovarian transposition during the oncologic surgery to protect ovarian function. However, this approach would not afford the patient to maintain the possibility of carrying a pregnancy. For this reason, after discussing the case with the tumor board at our institution, the patient was presented with the option to undergo uterine and ovarian transposition.
A comprehensive discussion was held with the patient and her family, outlining the risks and benefits of the treatment. The patient was informed that UT is considered an experimental approach. The initial treatment involved a radical vulvectomy with bilateral inguinofemoral lymphadenectomy (Fig. 1B) in December 2022. The final pathology report revealed a multi-focal, moderately differentiated squamous carcinoma that was non-HPV related. There were areas of invasion measuring 10 mm at the clitoris level and 14 mm in the left labia with negative margins. The left conglomerate inguinal lymph nodes were compromised with metastasis without extracapsular spread, and a right lymph node was compromised with a macro metastasis, indicating FIGO stage IIIB.
Fig. 1B.
Radical vulvectomy and Inguinofemoral lymph node resection.
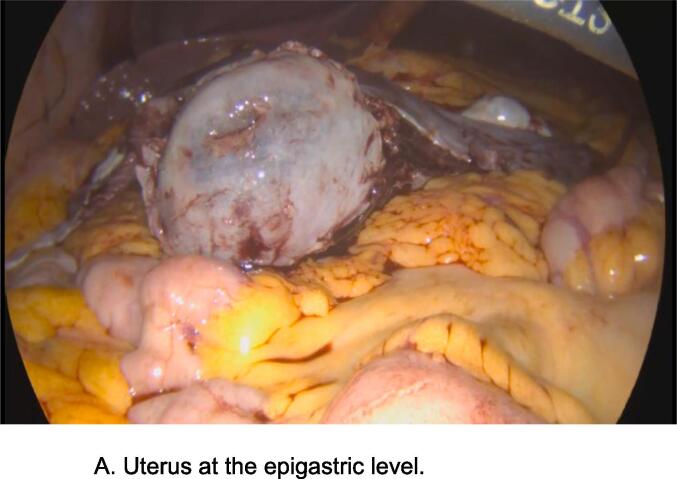
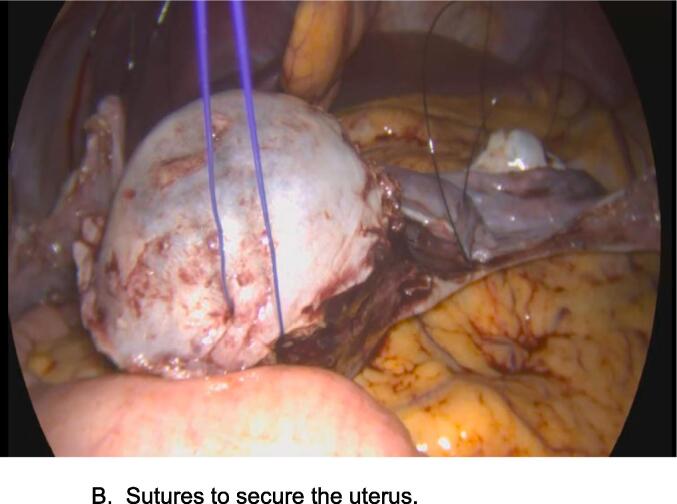
The UT was completed in January 2023. We briefly describe the procedure. Using a laparoscopic approach, the process begins with the sectioning of the round ligaments and the separation of the two sheets of the broad ligaments. A “window” is created to open the two sheets of the broad ligament ventral to the ureter. The infundibulopelvic (IP) ligament is dissected cranially until the intersection of the iliac arteries, preserving the gonadal vessels but followed by the section of the utero sacral ligaments. Following the dissection of the vesicouterine septum, the surgery proceeds similarly to a laparoscopic hysterectomy. The uterine vessels are then coagulated and sectioned medially to the ureter. Subsequently, the vagina is sectioned and sutured to move the uterus and the ovaries out of the pelvis. To protect the uterus and ovaries from radiation exposure, the sigmoidal and descending colon must be repositioned cranially to allow complete dissection of the gonadal vessels up to their origin. The full dissection of the IP ligament allows the movement of the uterus and ovaries to the upper abdomen. The uterus is positioned at the epigastric level (Fig. 2A). In this case, the uterine cervix was not exteriorized to the umbilical scar because reaching the umbilicus without tension on the gonadal vessels for correct fixation was not feasible. Consequently, the patient promptly initiated GnRH analogs to suppress ovarian function and menstrual cycles until the uterine reposition could occur. Then, two 2–0 polypropylene transabdominal sutures are passed approximately 2 cm distally to the costal margins and sutured to the ends of the round ligaments, ovaries, and IPs securing them to the anterior abdomen wall (Fig. 2B).
Fig. 2A.
Uterus at the epigastric level.
Fig. 2B.
Sutures to secure the uterus.
The patient was discharged from the hospital four days after surgery, following a Doppler ultrasound that confirmed the proper vascular function of gonadal vessels and an adequate uterine and adnexal perfusion. As a prophylaxis for deep venous thrombosis and to prevent thrombosis of gonadal vessels, she used subcutaneous enoxaparin (40 mg) for 28 days.. Fifteen days after the procedure, the transparietal sutures were removed, and the patient resumed her usual activities. Sexual intercourse was contraindicated for 60 days.
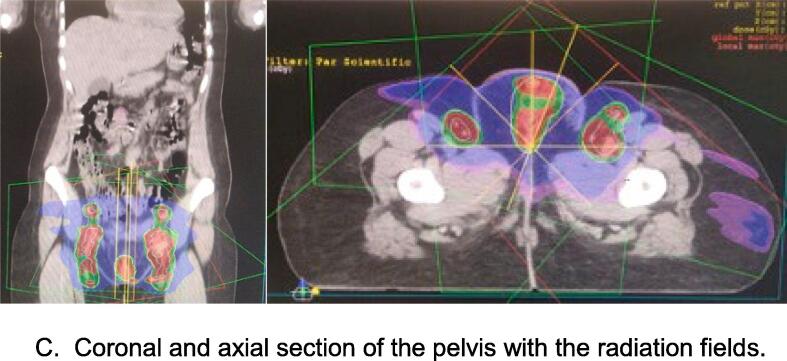
Adjuvant radiotherapy commenced 49 days after the uterine transposition. The treatment involved a radiation dose of 60 Gy (30 fractions) of 2 Gy per day, tergeting to the vulva and inguinofemoral and pelvic nodes up to the iliac bifurcation using intensity-modulated radiotherapy techniques (Fig. 2C). The treatment was successfully completed in 6.5 weeks, with a need for a split because of radio dermatitis at the inguinal level.
Fig. 2C.
Coronal and axial section of the pelvis with the radiation fields.
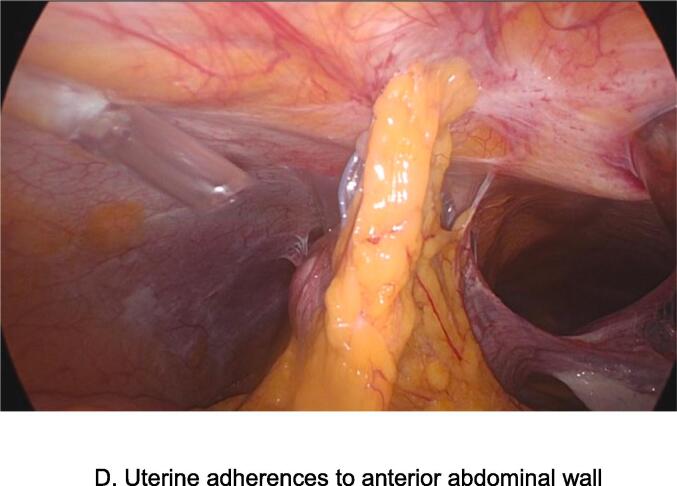
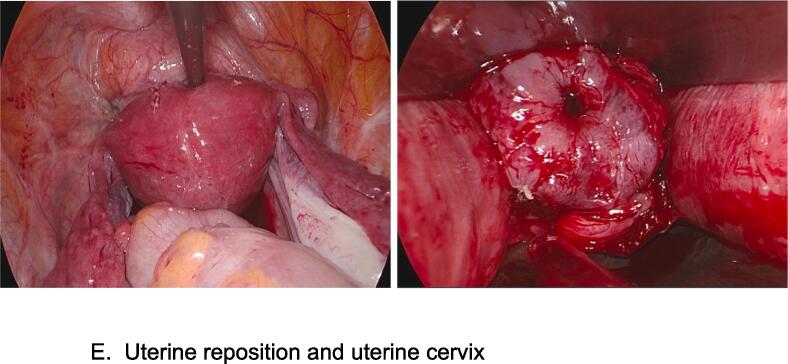
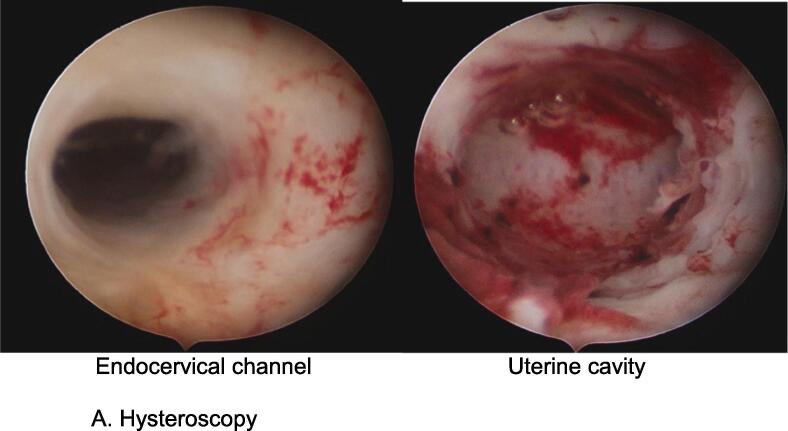
The uterine repositioning was performed after 133 days of the transposition in May 2023. Following the re-implantation, the treatment with GnRH analogs was concluded. The reposition was accomplished through laparoscopic adhesiolysis, allowing the uterine movement and its descent back into the pelvis (Fig. 2D). A vaginal probe was introduced to identify and dissect the vaginal vault. The vagina was then sectioned using monopolar energy, and the uterine cervix was inserted at the vaginal level and sutured transvaginally with absorbable sutures. The round ligaments were sutured in their remaining lateral portions, and the broad ligaments were reconstructed, restoring the normal anatomy of the pelvis (Fig. 2E). Once the uterine anatomy was reestablished, a hysteroscopy was performed to rule out uterine synechiae (Fig. 3A). The patient was discharged from the hospital two days after the procedure. However, ten days later, she was readmitted due to pelvic pain, vaginal bleeding, and fever. An urgent CT scan revealed a 5 cm collection on the left side of the vaginal suture. To treat this complication, a vaginal drainage was done under general anesthesia (Fig. 3B). The patient was released from the hospital three days later with antibiotics and experienced a smooth recovery.
Fig. 2D.
Uterine adherences to anterior abdominal wall.
Fig. 2E.
Uterine reposition and uterine cervix.
Fig. 3A.
Hysteroscopy.
Fig. 3B.
Collection on the left side of the vaginal suture and vaginal derangement.
She spontaneously recovered her menstrual cycles spontaneously and resumed sexual intercourse. In September 2023, an MRI was conducted, revealing no evidence of local or regional relapse. She continues her follow-up with oncofertility and gynecologic oncology teams, with her last visit was in December 2023. She does not plan to get pregnant until two years after completing treatment.
3. Discussion
Despite substantial advancements in fertility preservation for cancer patients, pelvic radiotherapy continues to pose a challenge when it comes to achieving pregnancy. We present the first case of UT in a vulvar cancer patient, providing a solution that preserves fertility and allows for a natural pregnancy without the necessity of in vitro fertilization, nor surrogacy.
The standard fertility preservation methods offered to these patients are oocyte cryopreservation and ovarian transposition before radiotherapy (Oktay et al., 2018). However, the feasibility of utilizing in vitro fertilization techniques may be limited in in regions with limited resources (Baiocchi et al., 2022).The prospect of achieving pregnancy without relying on in vitro fertilization methods renders it viable in resource-limited areas or those with legal restrictions, making it a promising alternative for these specific regions.
Religious considerations are also pertinent, as some patients may reject assisted fertilization methods (Sallam and Sallam, 2016). In this context, UT emerges as a promising alternative especially given that the reported pregnancies resulting from this technique have occurred spontaneously (Ribeiro et al., 2023, Lopez et al., 2023, Ribeiro et al., 2023).
The decision to offer UT to the patient was based on two key factors. Firstly, it provided a comprehensive approach to preserving both reproductive and hormonal function in a single procedure. Secondly, the decision was supported by an increasing number of successful cases reported in international literature (Ribeiro et al., 2017, Baiocchi et al., 2018, Odetto et al., 2021, Baiocchi et al., 2021, Ribeiro et al., 2023).
These aspects have been demonstrated in published manuscripts on UT, highlighting the preservation of uterine and gonadal function. Notably, there have been three documented cases in the literature where patients successfully achieved pregnancy and delivered term newborns without compromising the standard oncologic treatment (Ribeiro et al., 2023). However, further evaluation is essential to assess oncologic security and the uterine viability for conception in the coming years. The first prospective study of addressing this viability is currently underway (NCT 03040921). This prospective nonrandomized multicenter phase I study, aims to assess the feasibility of performing UT before chemoradiation for rectal cancer followed by uterine reimplantation after the treatment. Patients diagnosed with pelvic cancer requiring pelvic radiation will be offered the option to undergo UT before the radiation therapy with the subsequent repositioning of the uterus in its natural position after the treatment. The primary outcome measure will focus on uterine preservation after transposition to the upper abdomen and replacement in the pelvis. The secondary outcome measure will be morbidity and cancer recurrence. The study has completed the recruitment of patients and is currently in the phase of results analyses. A second study of the same research group initiated in 2020 aims to evaluate fertility rates and oncologic outcomes.
Although UT may no longer be considered an experimental approach, the option of oocyte or embryo cryopreservation should always be offered to patients who would benefit from a UT. This provides the opportunity to have genetically related children even if the ovaries lose their function while the uterus remains viable (Ribeiro et al., 2023).
Regarding the UT and the oncologic prognostic of the patient, several relevant aspects need consideration. UT does not impact the rates of pelvic, uterine, or ovarian recurrence due to the specific biological behavior of vulvar cancer.
Conversely, studies on minimally invasive surgery have indicated that radiotherapy can be promptly initiated after the procedure with minimal to no risk of complications (Ribeiro et al., 2017). For patients undergoing radical vulvectomy, it is generally recommended to initiate radiotherapy 4 to 6 weeks after the procedure to allow proper wound healing. The same time lapse is required to get the adequate vaginal wound healing (Baiocchi et al., 2021). However, in this case, the initiation of adjuvant radiotherapy had to be delayed due to the need to do radiotherapy in another center because of not having IMRT available.
The main limitation of our manuscript is that this is a single case report.
Nevertheless, reflects accumulated experience of the technique applied universally.
We highlight that this is the first case report of a UT related to vulvar cancer and the first hysteroscopic evaluation during the uterine reposition procedure. Additionally, we emphasize the feasibility to perform the technique in different centers and by different groups of surgeons.
In conclusion, UT can be regarded as a viable fertility preservation option similar to other techniques available, offering new opportunities and hope for young cancer patients. Despite the increasing scientific evidence and promising outcomes, we strongly recommend that cases be thoroughly discussed in multidisciplinary meetings and are subjected to local/regional Institutional review boards. The future results of ongoing prospective studies designed to explore this technique will be of paramount relevance.
CRediT authorship contribution statement
Joel Laufer: Writing – review & editing, Writing – original draft, Conceptualization. Santiago Scasso: Writing – original draft. Dana Kimelman: Writing – review & editing. Clara Olmedo: Writing – original draft. Valeria Bentancor: Writing – original draft. Anne Soust: Writing – original draft. Gonzalo Sotero: Writing – original draft. Reitan Ribeiro: Writing – review & editing, Conceptualization.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
The authors thank Professor Claudio Sosa, Dr. Mariana Gilardoni and all members of the Hospital staff, for their deep involvement that ensured the success of the procedure. Adiottionally, we thank Peluffo Giguens Foundation and his President, Alejandro Barrere for the logistical support that ensured the success of the procedure.
Consent
Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
References
- Baiocchi G., Mantoan H., Chen M.J., Faloppa C.C. Uterine transposition after radical trachelectomy. Gynecol Oncol. 2018;150(2):387–388. doi: 10.1016/j.ygyno.2018.05.009. [DOI] [PubMed] [Google Scholar]
- Baiocchi G., Vieira M., Moretti-Marques R., et al. Uterine transposition for gynecological cancers. Int J Gynecol Cancer. 2021;31(3):442–446. doi: 10.1136/ijgc-2020-001780. [DOI] [PubMed] [Google Scholar]
- Baiocchi G., Tsunoda A.T., Guitmann G., et al. Brazilian Society of Surgical Oncology consensus on fertility-sparing surgery for cervical cancer. J Surg Oncol. 2022;126(1):37–47. doi: 10.1002/jso.26899. [DOI] [PubMed] [Google Scholar]
- Jeruss J.S., Woodruff T.K. Preservation of fertility in patients with cancer. N Engl J Med. 2009;360(9):902–911. doi: 10.1056/NEJMra0801454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ley de Reproducción Asistida 16.167. https://www.impo.com.uy/reproduccion-humana-asistida/19167-2013.
- Lopez A., Perez Villena J.F., Guevara Jabiles A., Davila K., Sernaque Quintana R., Ribeiro R. Uterine transposition and successful pregnancy in a patient with rectal cancer. Int J Gynecol Cancer. 2023;33(8):1310–1315. doi: 10.1136/ijgc-2023-004661. [DOI] [PubMed] [Google Scholar]
- Odetto D., Saadi J.M., Chacon C.B., Wernicke A., Ribeiro R. Uterine transposition after radical trachelectomy. Int J Gynecol Cancer. 2021;31(10):1374–1379. doi: 10.1136/ijgc-2021-002944. [DOI] [PubMed] [Google Scholar]
- Oktay K., Harvey B.E., Partridge A.H., et al. Fertility preservation in patients with cancer: ASCO clinical practice guideline update. J Clin Oncol. 2018;36(19):1994–2001. doi: 10.1200/JCO.2018.78.1914. [DOI] [PubMed] [Google Scholar]
- Ribeiro R., Rebolho J.C., Tsumanuma F.K., Brandalize G.G., Trippia C.H., Saab K.A. Uterine transposition: technique and a case report. Fertil Steril. 2017;108(2):320–324. doi: 10.1016/j.fertnstert.2017.06.016. [DOI] [PubMed] [Google Scholar]
- Ribeiro R., Anselmi M.C., Schneider G.A., et al. First live birth after uterine transposition. Fertil Steril. 2023;120(1):188–193. doi: 10.1016/j.fertnstert.2023.02.033. [DOI] [PubMed] [Google Scholar]
- Ribeiro R., Baiocchi G., Moretti-Marques R., Linhares J.C., Costa C.N., Pareja R. Uterine transposition for fertility and ovarian function preservation after radiotherapy. Int J Gynecol Cancer. 2023;33(12):1837–1842. doi: 10.1136/ijgc-2023-004723. [DOI] [PubMed] [Google Scholar]
- Sallam H.N., Sallam N.H. Religious aspects of assisted reproduction. Facts Views vis Obgyn. 2016;8(1):33–48. [PMC free article] [PubMed] [Google Scholar]
- Wallace W.H.B., Thomson A.B., Saran F., et al. Predicting age of ovarian failure after radiation to a field that includes the ovaries. Int J RadiatOncol Biol Phys. 2005;62:738–744. doi: 10.1016/j.ijrobp.2004.11.038. [DOI] [PubMed] [Google Scholar]
- Wo Jennifer Y., Viswanathan A.N. The impact of radiotherapy on fertility, pregnancy, and neonatal outcomes of female cancer patients. Int J Radiat Oncol Biol Phys. 2009;73:1304–1312. doi: 10.1016/j.ijrobp.2008.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]