Abstract
A 67-year-old woman with a history of obesity, chronic low back pain, and recurrent episodes of major depression presents with mild depressive symptoms of more than 2 years’ duration, with worsening symptoms over the past 4 months. She was receiving sertraline at a stable dose of 100 mg per day until 3 months ago, when she initially presented for her worsening depressive symptoms. At that time, sertraline was tapered off, and treatment with extra-long extended-release bupropion (bupropion XL) was started at a dose of 150 mg daily and was increased to 300 mg daily 3 weeks later. Despite having taken the higher dose of bupropion XL for more than 2 months, the patient continues to have low mood, loss of interest in usual pleasurable activities, trouble falling asleep, wakefulness several times during the night, diminished energy, poor appetite, difficulty concentrating, and intrusive thoughts of being “better off dead,” but she does not have active suicidal thinking. Her nine-question Patient Health Questionnaire (PHQ-9) score is 17 (on a scale of 0 to 27, with higher scores indicating greater severity of depressive symptoms). How would you evaluate and treat this patient?
THE CLINICAL PROBLEM
Mood disorders, including major depression, persistent depressive disorder (also known as dysthymia), and subsyndromal depression are common among older adults1 and are associated with poor health outcomes and poor quality of life.2 Response to initial antidepressant treatment in clinical trials involving older persons varies from 35 to 73%.3–5 Factors related to poor response and treatment-resistant depression include chronic medical conditions, presence of cerebrovascular disease, coexisting anxiety, concomitant chronic dysthymia, substance abuse, and bereavement.
There is broad consensus for defining treatment-resistant depression across the lifespan as a lack of response to two or more adequate trials of antidepressants in a single episode.6,7 Although clinicians embrace a definition specifying treatment failure of at least two different classes of antidepressants, there is no current consensus on this nuance. A sufficient trial of a therapeutic dose is generally considered to be 8 weeks. Definitions of treatment-resistant depression are focused on lack of response to pharmacologic treatment and do not include lack of response to psychotherapy (recommended as initial treatment for mild-to-moderate depression8), electroconvulsive therapy (ECT), or transcranial magnetic stimulation (TMS). Diagnostic variation regarding treatment-resistant depression may affect accurate estimates of the prevalence of and prognosis for the condition and may lead to inconsistent treatment recommendations across guidelines.9 Levels of response are defined on the basis of guidelines: a decrease in symptom severity of 25% or less indicates nonresponse, a decrease of 26 to 49% indicates partial response, a decrease of 50% or greater indicates response, and the presence of no or very few symptoms indicates remission.10,11
STRATEGIES AND EVIDENCE
Evaluation of Treatment-Resistant Depression in Older Adults
Evaluation of treatment-resistant depression comprises confirmation of the diagnosis with validated tools and assessment of coexisting conditions (Fig. 1). The PHQ-9 is a validated tool for use in establishing a diagnosis of major depression and for tracking the progress of treatment; a score below 5 is typically the treatment goal.12 The Geriatric Depression Scale13 also is useful for tracking depressive symptoms in older adults.
Figure 1. Management of Treatment-Resistant Depression in Older Adults.
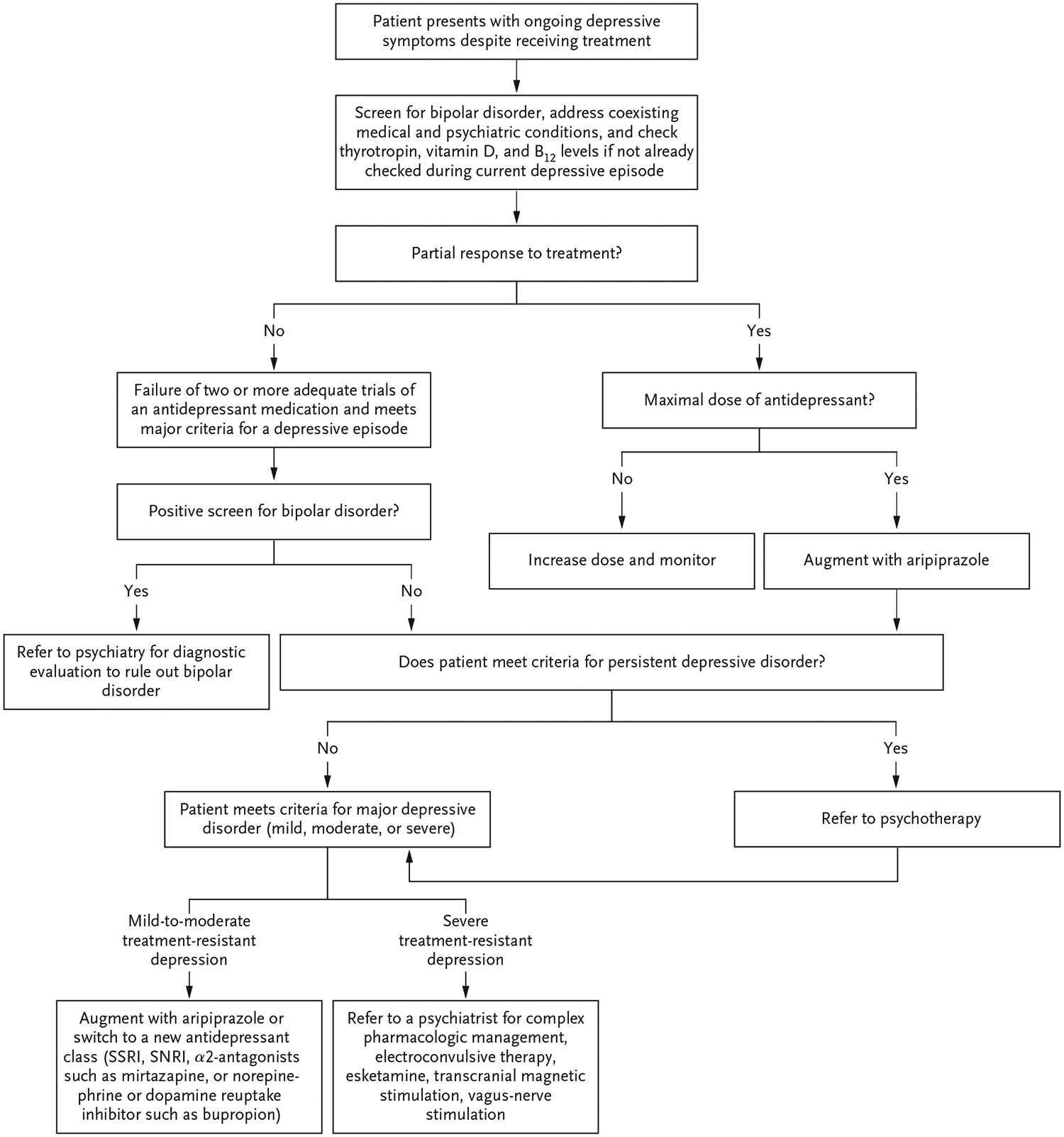
SNRI denotes serotonin–norepinephrine reuptake inhibitors, and SSRI selective serotonin-reuptake inhibitors.
Coexisting conditions that affect the diagnosis and management of depression include concomitant dysthymia, suicidal ideation, and other major psychiatric disorders and medical conditions. Dysthymia, defined as chronic (≥2 years) depressive symptoms that are insufficient to meet major depression criteria yet impair function,14 is associated with recurrent depressive episodes. For any depressive disorder, assessment of suicidal ideation is essential because of the increased prevalence of suicide among patients with this disorder and the need for specific further intervention. Screening tools such as the PHQ-9 include questions about suicide; however, further assessment of a patient who reports suicidal ideation should be undertaken as part of a clinical interview.
Depressive symptoms also occur in other major psychiatric disorders that may not be recognized when a patient initially presents with recurrent depressive symptoms. Patients with recurrence of depressive symptoms may have a cyclic mood disorder such as bipolar disorder, and screening for past symptoms of mania15 should include inquiry about mood swings, episodes of high mood with increased energy and decreased need for sleep, and personal or family history of manic–depressive illness.14 People with schizoaffective disorder have psychotic symptoms, such as hallucinations or delusions, as well as symptoms of a mood disorder — either bipolar type (episodes of mania and sometimes depression) or depressive type (episodes of depression). A patient who appears to have psychotic symptoms could be having a depressive episode (major depression with psychotic features) or may have a depressed subtype of schizoaffective disorder.
Medical conditions and side effects of medication can masquerade as depressive symptoms, and coexisting psychiatric and medical conditions can contribute to treatment resistance. Common confounding psychiatric conditions include anxiety, dysthymia, and alcohol or substance use disorders. Common confounding medical conditions include coronary heart disease, congestive heart failure, diabetes, cancer, and neurologic conditions.16
TREATMENT
Patients with treatment-resistant depression generally benefit from consultation with a mental health clinician, preferably a psychiatrist, because decision making around medication is often indicated. Such collaborative care may involve either comanagement of care by a primary care provider and a psychiatrist or a psychotherapist (or both) or referral to a psychiatrist or psychotherapist for consultation or ongoing care.
In a comanagement model, the primary care clinician may seek to optimize medication management by means of dose escalation, a change in therapy to a new antidepressant, or augmentation of therapy with another agent, while concurrently referring the patient to psychotherapy. Improving Mood-Promoting Access to Collaborative Treatment (IMPACT) is an evidence-based care model in which a behavioral health specialist who is embedded with a primary care provider and supervised by a psychiatrist works in collaboration with a primary care clinician to manage geriatric depression with the use of antidepressant medication and psychotherapy.17 As compared with usual care, this model resulted in significant reductions in depressive symptoms at 3 months that were sustained at 6 months and 12 months.17 Similarly, in the Prevention of Suicide in Primary Care Elderly: Collaborative Trial (PROSPECT), depression care managers in primary care settings collaborated with clinicians, an approach that showed decreases in geriatric depression and suicidal ideation.18 Despite these positive outcomes, only approximately half the active-intervention groups both in a trial assessing the IMPACT model and in PROSPECT met the definitions of response at 12 months.17,18
Referral to a psychiatrist is indicated for more complex interventions (e.g., ECT, TMS, vagus-nerve stimulation, and ketamine or esketamine therapy) when depressive symptoms are severe or chronic or involve coexisting cognitive impairment, psychosis, or worsening suicidal thoughts. Referral of patients with treatment-resistant depression to a psychiatrist who specializes in geriatric medicine may also be helpful in determining whether treatment with certain psychoactive medications should be stopped. However, provision of treatment will continue to be affected by a limited psychiatry and behavioral health workforce, especially for care of older adults.19
Management of Mild-to-Moderate Treatment-Resistant Depression
Regardless of the clinical setting, management of mild-to-moderate treatment-resistant depression often involves consideration of a referral for psychotherapy and changes in medication. Psychotherapy is considered first-line treatment for major depression without psychotic or suicidal features and includes individual and group cognitive behavioral therapy, individual problem-solving therapy, and interpersonal therapy.8
Cognitive behavioral therapy targets current problems and symptoms and focuses on the relationship among behaviors, thoughts, and feelings and aims to change those patterns that reduce pleasure and interfere with a person’s ability to function at their best. Problem-solving therapy is a cognitive behavioral approach that focuses on addressable problems identified by the patient that contribute to depression. Interpersonal psychotherapy focuses on improving problematic relationships and circumstances that are most closely associated with the current depressive episode.
Evidence for the addition of psychotherapy to the management of treatment-resistant depression specifically is lacking. One small randomized, controlled trial involving 124 participants who had a partial response to escitalopram therapy showed no significant difference in remission when escitalopram treatment was augmented with interpersonal therapy (58%) as compared with depression care management that included support, psycho-education, and behavioral interventions (45%) (P = 0.14).20
Pharmacotherapy for Mild-to-Moderate Treatment-Resistant Depression
The appropriate dose of antidepressant medicine for older adults with depression is similar to that for younger adults, and older persons can receive what might be perceived as a high dose without negative side effects (Table 1).20 However, older patients are more prone to adverse effects associated with antidepressants, especially falls (Table 2).21 Given high reported rates of medication nonadherence in depression, establishment and maintenance of a therapeutic alliance to support adherence surveillance can improve outcomes in patients with depression.15
Table 1.
Antidepressant Medication in Older Adults.*
| Medication | Starting Daily Dose | Target Daily Dose | Comments |
|---|---|---|---|
| Selective serotonin-reuptake inhibitors (SSRIs) | As a class, SSRIs should be used with caution in patients with a history of falls21 | ||
| Citalopram | 10–20 mg | 20 mg | FDA recommends 20 mg as maximal daily dose in patients >60 yr of age owing to risk of prolongation of the QT interval on ECG |
| Escitalopram | 10 mg | 10–20 mg | Possible risk of QT prolongation22 |
| Fluoxetine | 10–20 mg | 10–40 mg | Drug interaction based on both CYP450 and protein binding; lack of QT prolongation in most studies22 |
| Fluvoxamine | — | 50–300 mg | Dose reduction recommended in older adults23; lack of QT prolongation in most studies22 |
| Paroxetine | 10–20 mg | 20–40 mg | Some concern about use in older adults owing to anticholinergic effects; lack of clinically significant QTc prolongation in all studies22 |
| Sertraline | 25–50 mg | 50–200 mg | Has mild dopaminergic activity, which may help with motivation; lack of QT prolongation in most studies22 |
| Serotonin-norepinephrine reuptake inhibitors | |||
| Desvenlafaxine | — | 50 mg | 25-mg dose is available for frail older adults or those with renal impairment |
| Duloxetine | — | 60 mg | May help with chronic pain; may increase fall risk among older adults21 |
| Levomilnacipran | 20 mg | 40–120 mg | Limited evidence for use in late-life depression |
| Venlafaxine XR | 75 mg | 75–300 mg | At doses >150 mg may have more noradrenergic effects |
| Other nontricyclic antidepressants | |||
| Bupropion SR | 100–150 mg | 150–400 mg | Avoid in patients with history of seizures and psychosis |
| Bupropion XL | 150 mg | 150–450 mg | Avoid in patients with history of seizures and psychosis |
| Mirtazapine | 7.5–15.0 mg | 15–45 mg | Good evidence for mirtazapine monotherapy in older adults with depression24; may increase risk of falls21 |
| Trazodone | 25–50 mg | 50–300 mg | Sedating effects often preclude use as monotherapy; may increase risk of falls21 |
| Vilazodone | 10 mg | 20–40 mg | Low potential for drug-drug interactions |
| Vortioxetine | 5 mg | 5–20 mg | Low potential for drug-drug interactions; limited data in patients ≥65 yr of age |
| Tricyclic antidepressants | |||
| Desipramine | 50 mg | Depends on plasma level | Monitor ECG; target plasma levels to achieve plasma level of 200–400 ng per millilter; monitor closely for anticholinergic side effects |
| Nortriptyline | 25 mg | Depends on plasma level | Monitor ECG; target plasma levels to achieve plasma level of 50–150 ng per millilter; monitor closely for anticholinergic side effects |
| Augmenting agents | |||
| Aripiprizole | 2.5 mg | 5–15 mg | Aripiprazole augmentation shown to be more efficacious with respect to psychological well-being than a switch to bupropion25 |
| Lithium | 150–300 mg | Depends on plasma level; target, 0.6 mmol per liter25 | Lithium augmentation efficacy for unipolar depression is well-documented; monitor renal function and be alert to potential drug-drug interactions |
| Methylphenidate | 5 mg | 5–40 mg | Combination of citalopram and methylphenidate shown to be superior in efficacy for major depression as compared with monotherapy with either agent26 |
| Pramipexole | 0.125 mg | 0.25–2.0 mg | May be helpful in depression associated with Parkinson’s disease; dose range for monotherapy or as augmenting agent in major depression is not well- established |
| Quetiapine SR | 50–150 mg | 100–300 mg | Limited data on use of quetiapine as an augmenting agent with SSRIs, tricyclic antidepressants, and atypical antidepressants27 |
CYP450 denotes cytochrome P450, ECG electrocardiogram, FDA Food and Drug Administration, QTc corrected QT interval, SR sustained release, XL extra-long extended release, and XR extended release.
Table 2.
Somatic Treatment Approaches to Treatment-Resistant Depression in Older Adults.
| Treatment | Comments |
|---|---|
| Augmentation of antidepressant therapy in patients with partial response to treatment | |
| Low-dose second-generation antipsychotic agents | The strongest evidence is for aripiprazole25; quetiapine is another option if the patient is willing to live with potential sedating effects, although the strength of evidence is low. |
| Second-generation antidepressants | Certain non-SSRI and non-SNRI antidepressants can be used for augmentation; bupropion may be considered in patients with fatigue, weight gain, or sexual dysfunction, and there is evidence of efficacy in late-life treatment-resistant depression29; augmentation with mirtazapine is a reasonable option for patients with insomnia, anxiety, or weight loss but may increase risk of falls.21 |
| Lithium | Low-dose lithium targeting blood levels between 0.3 mmol and 0.6 mmol per liter may also be considered30; monitor renal function and be alert to potential drug-drug interactions. |
| Thyroid medications | Triiodothyronine has shown limited evidence as an augmenting agent.31 |
| Medications and other treatments to consider switching to in patients with no or minimal response * | |
| Tricyclic antidepressants | Tricyclic antidepressants with low anticholinergic burden (e.g., nortriptyline and desipramine) may be useful; careful monitoring of blood levels and ECG is warranted. |
| Monoamine oxidase inhibitors | Usually administered as monotherapy; has a washout period. Dietary restrictions are necessary with tyramine. Transdermal selegiline may be an option owing to minimal dietary restrictions, but data from older adults with depression are limited.32 |
| Psychedelics | Esketamine (inhaled formulation) is approved for treatment of depression, and older adults may have improvements in mood similar to those in younger adults.33 Ketamine (administered intravenously) has been shown to reduce depression. The evidence base is slim for psilocybin, although it may improve cognitive flexibility (the ability to switch between different cognitive operations in response to changing environmental demands) in patients with depression.34 |
| Neurostimulation | There is substantial literature supportive of the efficacy and safety of electroconvulsive therapy in older adults; evidence exists for the use of transcranial magnetic stimulation in older adults with depression.35 Data on the use of vagus-nerve stimulation in older adults are limited.36 |
Given the lack of evidence for switching in the context of treatment-resistant depression, the recommendations shown are based on evidence from the treatment of older patients with depression. SNRI denotes serotonin–norepinephrine reuptake inhibitor.
The evidence base for the pharmacologic treatment of treatment-resistant depression is limited and involves strategies of switching or augmenting antidepressants. One large, multisite platform trial, Sequenced Treatment Alternatives to Relieve Depression (STAR*D), involved a series of randomized, controlled treatment trials involving 3671 adult outpatients with nonpsychotic major depressive disorder who were candidates for medication (citalopram) as a first treatment step.37 Remission at step 1 in the trial was 36.8%; only 106 adults 65 years of age or older received citalopram monotherapy, and remission of symptoms in that subgroup occurred in 31.1%.38 Given the small number of older patients with depression included in the STAR★D trial, we can only extrapolate findings from subsequent steps to older adults. In step 2, patients who did not have remission were randomly assigned to switch to one of three antidepressants (i.e., bupropion, sertraline, or venlafaxine), switch to cognitive behavioral therapy, or continue to receive citalopram therapy with augmentation (bupropion, buspirone, or cognitive behavioral therapy). Overall remission with these interventions was observed in 30.6% of the patients, with none of the medication switch regimens being clearly superior.37 Overall cumulative remission after multiple steps was observed in 67%.
Although switching from one antidepressant class to another is an approach that is common clinical practice, there is little evidence to support it.28 Nevertheless, there is guideline-based support for switching antidepressants from a selective serotonin-reuptake inhibitors (SSRI) to either the serotonin–norepinephrine reuptake inhibitor (SNRI) venlafaxine or the monoamine oxidase inhibitor (MAOI) tranylcypromine in nongeriatric patients with depression.10 A small study assessing the use of venlafaxine as compared with paroxetine in older patients who did not have a response to other treatments showed that 60% of the patients who received venlafaxine and 33% of those who received paroxetine had remission of symptoms after 8 weeks of treatment.39 A 1996 study involving older adults with depression who did not have a response to an initial trial of nortriptyline showed that 63.6% of the participants had a response to phenelzine (an MAOI) at 6 weeks.40 SSRIs and SNRIs are the most commonly prescribed classes of antidepressants; however, because MAOIs are prescribed less frequently than SSRIs and SNRIs in both geriatric and nongeriatric patients, treatment with an MAOI in an older adult should be managed by a geriatric psychiatrist.
There is evidence supporting augmentation strategies for use in patients with treatment-resistant depression (Table 2). The use of lithium as an augmenting agent is recommended in two treatment guidelines.10,15 A meta-analysis of 10 prospective trials involving mostly nongeriatric participants showed that lithium augmentation was superior to placebo in the treatment of unipolar major depression, with 41.2% of the patients in the lithium group having a response, as compared with 14.4% of those in the placebo group.41 In the STAR★D trial, augmentation with lithium in patients who had not had a response to two adequate trials of antidepressant agents resulted in remission in an additional 15.9% of those patients; however, the mean lithium blood level was only 0.6 mmol per liter (therapeutic range, 0.6 to 1.2), which may have accounted for the modest effect.42 When considering the use of lithium in older adults, clinicians should be aware of potential drug–drug interactions. The evidence for augmentation with second-generation antipsychotic agents is stronger than that for lithium, with results of randomized clinical trials favoring augmentation with quetiapine, aripiprazole, olanzapine, and risperidone in nongeriatric adults.43 The recommended doses in patients with unipolar depression are lower than those used in the treatment of patients with schizophrenia,28 with one guideline recommending aripiprazole at an initial dose of 2 mg to 5 mg per day and a maximum final dose of 15 mg per day.10 In treatment-resistant depression in older patients, a trial of augmentation with aripiprazole (target dose, 10 mg per day) as compared with placebo showed greater remission with aripiprazole (in 44% of the patients vs. 28%), although akathisia (in 26.7% of the patients), increased dream activity (in 26.7%), and weight gain (in 19.8%) were commonly reported side effects.25
Augmentation with triiodothyronine (T3) has a modest evidence base, mostly among older adults receiving T3 augmentation of treatment with tricyclic antidepressants.43 A review of eight trials of varying quality involving augmentation with T3 showed that a pooled percentage of 56.8% of the patients who received augmentation had remission, as compared with 23.5% who received placebo; the number needed to treat (for response) was 4.3.44 However, when analyses were restricted to randomized, controlled trials, there was no difference between augmentation with T3 and placebo.44 In the STAR★D trial, T3 augmentation of citalopram therapy led to remission in an additional 24.7% of the patients.42
The choice of augmentation with an antidepressant can be tailored to the patient’s symptoms.45 For patients in an anergic or amotivated state, clinicians should consider switching to or augmenting treatment with an activating agent such as an SNRI or bupropion.7 Insomnia, diminished appetite, or weight loss may indicate the use of mirtazapine, which has been associated with sedation, increased appetite, and weight gain.45
Treatment of Severe Treatment-Resistant Major Depression in Older Adults
Older patients with severe treatment-resistant depression are usually referred to a psychiatrist who typically would recommend trials of medications such as those shown in Table 2. Other approaches to treatment include ECT, esketamine, and TMS. Evidence for the use of ECT comes from the uncontrolled, observational Prolonging Remission in Depressed Elderly trial, in which 240 adults 60 years of age or older with treatment-resistant depression were treated with ECT to the right side of the brain combined with venlafaxine therapy.46 This intervention resulted in remission in 63% of the patients with severe depression and in 75% of those with moderately severe depression. A randomized, controlled trial of intranasal esketamine plus antidepressant therapy as compared with intranasal placebo plus antidepressant therapy in patients 65 years of age or older with treatment-resistant depression showed no improvement associated with esketamine.47,48 With regard to TMS, a recent systematic review including seven randomized, controlled trials and seven uncontrolled trials of TMS in geriatric depression showed substantial variation in clinical response, with remission occurring in 6.7 to 54.3% of the patients.49 Data are limited with regard to the effects of intravenous ketamine or psilocybin for treatment of older adults with treatment-resistant depression.
AREAS OF UNCERTAINTY
There is little evidence with regard to how long an older adult with depression should continue treatment with an antidepressant once remission is reached. Further studies, including longer term clinical trials, are needed to guide maintenance treatment, especially for patients with a history of recurrence of severe depression. In addition, more evidence is needed with regard to antidepressant augmentation and switching strategies. The use of brain imaging and genetic markers in the management of treatment-resistant depression in older patients also requires more study.
GUIDELINES
Although no guidelines have been developed solely for the evaluation and management of treatment-resistant depression in older adults, there are published guidelines regarding treatment-resistant depression in adults and guidelines for management of late-life depression more broadly. Both U.S.8,15,50 and non-U.S.51–54 guidelines mention treatment approaches for use in patients with treatment-resistant depression. Recommendations in this article are generally consistent with these guidelines.
CONCLUSIONS AND RECOMMENDATIONS
With regard to the patient described in the vignette, I would begin with a review of her current depressive symptoms and investigate possible coexisting conditions, such as anxiety and dysthymia. Her chronic depressive symptoms appear to have been exacerbated by worsening lower back pain, causing her to curtail many of her activities; therefore, I would refer her for problem-solving therapy to develop strategies to motivate her to engage in physical therapy and help her identify enjoyable activities in which she can participate and thereby improve her mood. I would also continue to monitor her suicidal ideation. Owing to her moderately severe symptoms (PHQ-9 score of 17), ongoing use of pharmacotherapy is warranted. Because she has had two unsuccessful trials of antidepressants, I would switch treatment to an SNRI such as duloxetine at a dose of 30 mg daily, with a plan to increase to 60 mg daily after a week. Duloxetine may relieve some of her chronic low back pain, and it is unlikely to cause weight gain. Ideally, management of her depression would occur in the context of a collaborative care model that would involve visits every 2 weeks, measurement-based monitoring of symptoms and severity, and a goal of remission. If her depression does not remit after 8 weeks of treatment with duloxetine at the 60-mg dose, I would step up care with augmentation using a second-generation antipsychotic such as aripiprazole. Should her condition deteriorate to include severe symptoms or active suicidal ideation, I would refer her for ECT.
Key Clinical Points.
Treatment-Resistant Depression in Older Adults
Treatment-resistant depression is common in older adults with depression and is associated with several biologic, psychological, and social factors, as well as with adverse clinical and functional outcomes.
A commonly accepted definition of treatment-resistant depression is a lack of improvement despite adequate trials of two different classes of antidepressants for at least 8 weeks.
Assessment of treatment-resistant depression includes screening for coexisting medical and psychiatric conditions.
Measurement-based collaborative care with the use of validated instruments (e.g., the nine-item Patient Health Questionnaire) is recommended for the management of depression, with continuous monitoring and adjustment of treatment until remission is reached and sustained.
The best evidence for a pharmacologic approach to the management of treatment-resistant depression rests on augmentation strategies, such as the use of second-generation antipsychotic agents, lithium, or another antidepressant agent, or a switch to a different class of agent.
Referral for a psychiatric evaluation for consideration of electroconvulsive therapy or other treatment is recommended for patients with severe depression, worsening suicidal ideation, psychosis, or coexisting cognitive impairment.
Acknowledgments
I thank Neha Jain, M.D., associate professor of psychiatry, and Shakaib Khan, M.D., assistant professor of psychiatry, at the University of Connecticut School of Medicine, for their review of and input regarding an earlier version of the manuscript.
Footnotes
This Journal feature begins with a case vignette highlighting a common clinical problem. Evidence supporting various strategies is then presented, followed by a review of formal guidelines, when they exist. The article ends with the author’s clinical recommendations.
Disclosure forms provided by the author are available with the full text of this article at NEJM.org.
References
- 1.Steffens DC, Fisher GG, Langa KM, Potter GG, Plassman BL. Prevalence of depression among older Americans: the Aging, Demographics and Memory Study. Int Psychogeriatr 2009; 21: 879–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Defrancesco M, Pechlaner R, Kiechl S, et al. What characterizes depression in old age? Results from the Bruneck Study. Pharmacopsychiatry 2018; 51: 153–60. [DOI] [PubMed] [Google Scholar]
- 3.Culang ME, Sneed JR, Keilp JG, et al. Change in cognitive functioning following acute antidepressant treatment in late-life depression. Am J Geriatr Psychiatry 2009; 17: 881–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schatzberg A, Roose S. A double-blind, placebo-controlled study of venlafaxine and fluoxetine in geriatric outpatients with major depression. Am J Geriatr Psychiatry 2006; 14: 361–70. [DOI] [PubMed] [Google Scholar]
- 5.Newhouse PA, Krishnan KR, Doraiswamy PM, Richter EM, Batzar ED, Clary CM. A double-blind comparison of sertraline and fluoxetine in depressed elderly outpatients. J Clin Psychiatry 2000; 61: 559–68. [DOI] [PubMed] [Google Scholar]
- 6.Gaynes BN, Lux L, Gartlehner G, et al. Defining treatment-resistant depression. Depress Anxiety 2020; 37: 134–45. [DOI] [PubMed] [Google Scholar]
- 7.Lenze EJ, Mulsant BH, Roose SP, et al. Antidepressant augmentation versus switch in treatment-resistant geriatric depression. N Engl J Med 2023; 388: 1067–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.American Psychological Association. Clinical practice guideline for the treatment of depression across three age cohorts. February 2019 (https://www.apa.org/depression-guideline/guideline.pdf).
- 9.Gabriel FC, Stein AT, de Melo DO, et al. Recommendations for the pharmacological treatment of treatment-resistant depression: a systematic review protocol. PLoS One 2022; 17(4): e0267323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bauer M, Pfennig A, Severus E, Whybrow PC, et al. World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for biological treatment of unipolar depressive disorders, part 1: update 2013 on the acute and continuation treatment of unipolar depressive disorders. World J Biol Psychiatry 2013; 14: 334–85. [DOI] [PubMed] [Google Scholar]
- 11.Coley RY, Boggs JM, Beck A, Hartzler AL, Simon GE. Defining success in measurement-based care for depression: a comparison of common metrics. Psychiatr Serv 2020; 71: 312–8. [DOI] [PubMed] [Google Scholar]
- 12.Spitzer RL, Kroenke K, Williams JBW. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. JAMA 1999; 282: 1737–44. [DOI] [PubMed] [Google Scholar]
- 13.Sheikh JI, Yesavage JA. Geriatric Depression Scale (GDS): recent evidence and development of a shorter version. In: Brink TL, ed. Clinical gerontology: a guide to assessment and intervention. New York: Hawthorn Press, 1986: 165–73. [Google Scholar]
- 14.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Washington, DC: American Psychiatric Association, 2022. [Google Scholar]
- 15.American Psychiatric Association. Practice guideline for the treatment of patients with major depressive disorder. 3rd ed. October 2010 (https://psychiatryonline.org/pb/assets/raw/sitewide/practice_guidelines/guidelines/mdd.pdf). [PubMed]
- 16.Subramanian S, Oughli HA, Gebara MA, Palanca BJA, Lenze EJ. Treatment-resistant late-life depression: a review of clinical features, neuropsychology, neuro-biology, and treatment. Psychiatr Clin North Am 2023; 46: 371–89. [DOI] [PubMed] [Google Scholar]
- 17.Unützer J, Katon W, Callahan CM, et al. Collaborative care management of late-life depression in the primary care setting: a randomized controlled trial. JAMA 2002; 288: 2836–45. [DOI] [PubMed] [Google Scholar]
- 18.Bruce ML, Ten Have TR, Reynolds CF III, et al. Reducing suicidal ideation and depressive symptoms in depressed older primary care patients: a randomized controlled trial. JAMA 2004; 291: 1081–91. [DOI] [PubMed] [Google Scholar]
- 19.Institute of Medicine. The mental health and substance use workforce for older adults: in whose hands? Washington, DC: National Academies Press, 2012. [PubMed] [Google Scholar]
- 20.Reynolds CF III, Dew MA, Martire LM, et al. Treating depression to remission in older adults: a controlled evaluation of combined escitalopram with interpersonal psychotherapy versus escitalopram with depression care management. Int J Geriatr Psychiatry 2010; 25: 1134–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sobieraj DM, Martinez BK, Hernandez AV, et al. Adverse effects of pharmacologic treatments of major depression in older adults. J Am Geriatr Soc 2019; 67: 1571–81. [DOI] [PubMed] [Google Scholar]
- 22.Funk KA, Bostwick JR. A comparison of the risk of QT prolongation among SSRIs. Ann Pharmacother 2013; 47: 1330–41. [DOI] [PubMed] [Google Scholar]
- 23.Orlando R, De Martin S, Andrighetto L, Floreani M, Palatini P. Fluvoxamine pharmacokinetics in healthy elderly subjects and elderly patients with chronic heart failure. Br J Clin Pharmacol 2010; 69: 279–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Schatzberg AF, Kremer C, Rodrigues HE, Murphy GM Jr, Mirtazapine vs. Paroxetine Study Group. Double-blind, randomized comparison of mirtazapine and paroxetine in elderly depressed patients. Am J Geriatr Psychiatry 2002; 10: 541–50. [PubMed] [Google Scholar]
- 25.Lenze EJ, Mulsant BH, Blumberger DM, et al. Efficacy, safety, and tolerability of augmentation pharmacotherapy with aripiprazole for treatment-resistant depression in late life: a randomised, double-blind, placebo-controlled trial. Lancet 2015; 386: 2404–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lavretsky H, Reinlieb M, St Cyr N, Siddarth P, Ercoli LM, Senturk D. Citalopram, methylphenidate, or their combination in geriatric depression: a randomized, double-blind, placebo-controlled trial. Am J Psychiatry 2015; 172: 561–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hashimi H, Andersen M, Sessa M. Predictors of quetiapine extended-release formulation add-on in older patients exposed to antidepressant drugs: a Danish register-based cohort study. Int J Geriatr Psychiatry 2020; 35: 1156–62. [DOI] [PubMed] [Google Scholar]
- 28.Dold M, Kasper S. Evidence-based pharmacotherapy of treatment-resistant unipolar depression. Int J Psychiatry Clin Pract 2017; 21: 13–23. [DOI] [PubMed] [Google Scholar]
- 29.Dew MA, Whyte EM, Lenze EJ, et al. Recovery from major depression in older adults receiving augmentation of antidepressant pharmacotherapy. Am J Psychiatry 2007; 164: 892–9. [DOI] [PubMed] [Google Scholar]
- 30.Kok RM, Vink D, Heeren TJ, Nolen WA. Lithium augmentation compared with phenelzine in treatment-resistant depression in the elderly: an open, randomized, controlled trial. J Clin Psychiatry 2007; 68: 1177–85. [DOI] [PubMed] [Google Scholar]
- 31.Cooper-Kazaz R, Lerer B. Efficacy and safety of triiodothyronine supplementation in patients with major depressive disorder treated with specific serotonin reuptake inhibitors. Int J Neuropsychopharmacol 2008; 11: 685–99. [DOI] [PubMed] [Google Scholar]
- 32.Alexopoulos GS. Pharmacotherapy for late-life depression. J Clin Psychiatry 2011; 72(1): e04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ochs-Ross R, Wajs E, Daly EJ, et al. Comparison of long-term efficacy and safety of esketamine nasal spray plus oral antidepressant in younger versus older patients with treatment-resistant depression: post-hoc analysis of SUSTAIN-2, a long-term open-label phase 3 safety and efficacy study. Am J Geriatr Psychiatry 2022; 30: 541–56. [DOI] [PubMed] [Google Scholar]
- 34.Doss MK, Považan M, Rosenberg MD, et al. Psilocybin therapy increases cognitive and neural flexibility in patients with major depressive disorder. Transl Psychiatry 2021; 11: 574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kaster TS, Daskalakis ZJ, Noda Y, et al. Efficacy, tolerability, and cognitive effects of deep transcranial magnetic stimulation for late-life depression: a prospective randomized controlled trial. Neuropsychopharmacology 2018; 43: 2231–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.McDonald WM. Neuromodulation treatments for geriatric mood and cognitive disorders. Am J Geriatr Psychiatry 2016; 24: 1130–41. [DOI] [PubMed] [Google Scholar]
- 37.Rush AJ, Trivedi MH, Wisniewski SR, et al. Acute and longer-term outcomes in depressed outpatients requiring one or several treatment steps: a STAR★D report. Am J Psychiatry 2006;163:1905–17. [DOI] [PubMed] [Google Scholar]
- 38.Steiner AJ, Recacho J, Vanle B, et al. Quality of life, functioning, and depressive symptom severity in older adults with major depressive disorder treated with citalopram in the STAR★D study. J Clin Psychiatry 2017; 78: 897–903. [DOI] [PubMed] [Google Scholar]
- 39.Mazeh D, Shahal B, Aviv A, Zemishlani H, Barak Y. A randomized, single-blind, comparison of venlafaxine with paroxetine in elderly patients suffering from resistant depression. Int Clin Psychopharmacol 2007; 22: 371–5. [DOI] [PubMed] [Google Scholar]
- 40.Flint AJ, Rifat SL. The effect of sequential antidepressant treatment on geriatric depression. J Affect Disord 1996; 36: 95–105. [DOI] [PubMed] [Google Scholar]
- 41.Crossley NA, Bauer M. Acceleration and augmentation of antidepressants with lithium for depressive disorders: two meta-analyses of randomized, placebo-controlled trials. J Clin Psychiatry 2007; 68: 935–40. [DOI] [PubMed] [Google Scholar]
- 42.Nierenberg AA, Fava M, Trivedi MH, et al. A comparison of lithium and T(3) augmentation following two failed medication treatments for depression: a STAR★D report. Am J Psychiatry 2006; 163: 1519–30. [DOI] [PubMed] [Google Scholar]
- 43.Voineskos D, Daskalakis ZJ, Blumberger DM. Management of treatment-resistant depression: challenges and strategies. Neuropsychiatr Dis Treat 2020; 16: 221–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Aronson R, Offman HJ, Joffe RT, Naylor CD. Triiodothyronine augmentation in the treatment of refractory depression: a meta-analysis. Arch Gen Psychiatry 1996; 53: 842–8. [DOI] [PubMed] [Google Scholar]
- 45.Watanabe N, Omori IM, Nakagawa A, et al. Mirtazapine versus other antidepressive agents for depression. Cochrane Database Syst Rev 2011; (12): CD006528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Østergaard SD, Speed MS, Kellner CH, et al. Electroconvulsive therapy (ECT) for moderate-severity major depression among the elderly: data from the PRIDE study. J Affect Disord 2020; 274: 1134–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ochs-Ross R, Daly EJ, Zhang Y, et al. Efficacy and safety of esketamine nasal spray plus an oral antidepressant in elderly patients with treatment-resistant depression-TRANSFORM-3. Am J Geriatr Psychiatry 2020; 28: 121–41. [DOI] [PubMed] [Google Scholar]
- 48.Di Vincenzo JD, Siegel A, Lipsitz O, et al. The effectiveness, safety and tolerability of ketamine for depression in adolescents and older adults: a systematic review. J Psychiatr Res 2021; 137: 232–41. [DOI] [PubMed] [Google Scholar]
- 49.Cappon D, den Boer T, Jordan C, Yu W, Metzger E, Pascual-Leone A. Transcranial magnetic stimulation (TMS) for geriatric depression. Ageing Res Rev 2022; 74: 101531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Alexopoulos GS, Katz IR, Reynolds CF III, Carpenter D, Docherty JP, Expert Consensus Panel for Pharmacotherapy of Depressive Disorders in Older Patients. The expert consensus guideline series: pharmacotherapy of depressive disorders in older patients. Postgrad Med 2001; Spec No Pharmacotherapy: 1–86. [PubMed] [Google Scholar]
- 51.Ijaz S, Davies P, Williams CJ, Kessler D, Lewis G, Wiles N. Psychological therapies for treatment-resistant depression in adults. Cochrane Database Syst Rev 2018; 5(5): CD010558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Davies P, Ijaz S, Williams CJ, Kessler D, Lewis G, Wiles N. Pharmacological interventions for treatment-resistant depression in adults. Cochrane Database Syst Rev 2019; 12(12): CD010557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Bennabi D, Charpeaud T, Yrondi A, et al. Clinical guidelines for the management of treatment-resistant depression: French recommendations from experts, the French Association for Biological Psychiatry and Neuropsychopharmacology and the fondation FondaMental. BMC Psychiatry 2019; 19: 262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Baba H, Kito S, Nukariya K, et al. Guidelines for diagnosis and treatment of depression in older adults: a report from the Japanese Society of mood disorders. Psychiatry Clin Neurosci 2022; 76: 222–34. [DOI] [PubMed] [Google Scholar]


