Abstract
Objective:
Acute lung injury (ALI), including its more severe sub-category, acute respiratory distress syndrome (ARDS), is a critical illness associated with considerable morbidity and mortality. The authors’ objective was to summarize data on the prevalence of depressive, posttraumatic stress disorder (PTSD), and other anxiety syndromes amongst survivors of ALI/ARDS, potential risk factors for these syndromes, and their relationships to quality of life.
Methods:
The authors conducted a systematic literature review using Medline, EMBASE, Cochrane Library, CINAHL, and PsycINFO. Eligible studies reported data on psychiatric morbidity at least once following intensive care treatment of ALI/ARDS.
Results:
Ten observational studies met inclusion criteria (total n=331). Using questionnaires, the point prevalence of “clinically significant” symptoms of depression ranged from 17-43% (4 studies); PTSD, 21-35% (4 studies); and non-specific anxiety, 23-48% (3 studies). Studies varied in terms of instruments used, thresholds for clinical significance, baseline psychiatric history exclusions, and timing of assessments (range 1 month to 8 years). Psychiatrist-diagnosed PTSD prevalences at hospital discharge, 5 years, and 8 years were 44%, 25%, and 24%, respectively. Three studies prospectively assessed risk factors for post-ALI/ARDS PTSD and depressive symptoms; significant predictors included longer durations of mechanical ventilation, ICU stay, and sedation. All four studies that examined relationships between psychiatric symptoms and quality of life found significant negative associations.
Conclusions:
The prevalence of psychiatric morbidity in patients surviving ALI/ARDS appears high. Future research should incorporate more in-depth diagnostic and risk factor assessments for prevention and monitoring purposes.
Keywords: respiratory distress syndrome, acute; depression; stress disorder, posttraumatic; anxiety; critical care; outcome assessment (health care)
INTRODUCTION
Acute lung injury (ALI), including its more severe sub-category, acute respiratory distress syndrome (ARDS), is a common critical illness with important physical and mental health consequences for survivors. There are an estimated 190,600 cases of ALI and 141,500 cases of ARDS annually in the US (1). The incidence of this illness increases with age. The syndrome is defined by acute onset of severe hypoxemia and bilateral pulmonary infiltrates on chest x-ray in the setting of various pulmonary (e.g. pneumonia, aspiration) or non-pulmonary (e.g. sepsis, pancreatitis, trauma, blood transfusion) risk factors. ALI/ARDS usually results in respiratory failure necessitating mechanical ventilation in the intensive care unit (ICU), with an average ICU length of stay of 11 days (2). Due to advances in critical care treatment, the short-term mortality of ALI/ARDS has decreased from approximately 70% to 40% (1-3), and research has begun to focus on survivors’ recovery, which occurs over subsequent months and years. Researchers have examined survivors’ quality of life, physical and cognitive function, and mental health (4-6). Several studies have shown persistent physical and cognitive impairments in large proportions of ALI/ARDS survivors (6). The authors’ objective was to systematically review the prevalence of psychiatric syndromes in ALI/ARDS survivors [specifically depression, posttraumatic stress disorder (PTSD), and other anxiety syndromes], potential risk factors for these syndromes, and their relationships to quality of life (QOL).
METHODS
Search Strategy
To identify studies eligible for systematic review, we searched Medline (1966-2007), EMBASE (1974-2007), CINAHL (1982-2007), the Cochrane Library (2007, Issue 1), and PsycInfo (1967-2007) as of April 6, 2007. The following search strategy was used, with all terms mapped to the appropriate MeSH/EMTREE subject headings and “exploded”: (“mental disorders” OR “psychometrics”) AND (“respiratory distress syndrome, adult” OR “critical care” OR “critical illness” OR “intensive care units” OR “sepsis”). Also, the following terms were included as text words: (“depress*” OR “stress” OR “anxi*”) AND (“respiratory distress syndrome” OR “ARDS” OR “acute lung injury” OR “ALI”). The search was limited to English-language articles. Articles dealing with neonatal or pediatric intensive care were excluded.
Study Selection
Two authors (D.S.D. and S.V.D.) independently and sequentially reviewed citations, abstracts, and full text articles to select eligible studies. All citations or abstracts selected by either author were included in the next step of the selection process. At each step, the authors calculated interobserver agreement using percent agreement and the kappa statistic (7). Disagreement regarding eligibility of full text articles was resolved by consensus among all authors.
Articles were selected for review if they met the following criteria: 1) the study population was comprised of adult ALI/ARDS survivors, and 2) psychiatric assessments occurred following ICU discharge. Studies that reported only QOL data were excluded, as were case reports and review articles.
Data Abstraction
For each eligible study, two authors (D.S.D. and S.V.D.) independently abstracted information regarding study cohorts, psychiatric measures, quality of life, and potential risk factors. The authors calculated interobserver agreement for data abstraction using percent agreement and the kappa statistic. Authors of eligible studies were contacted directly for additional information, when necessary.
RESULTS
Search Results and Study Characteristics
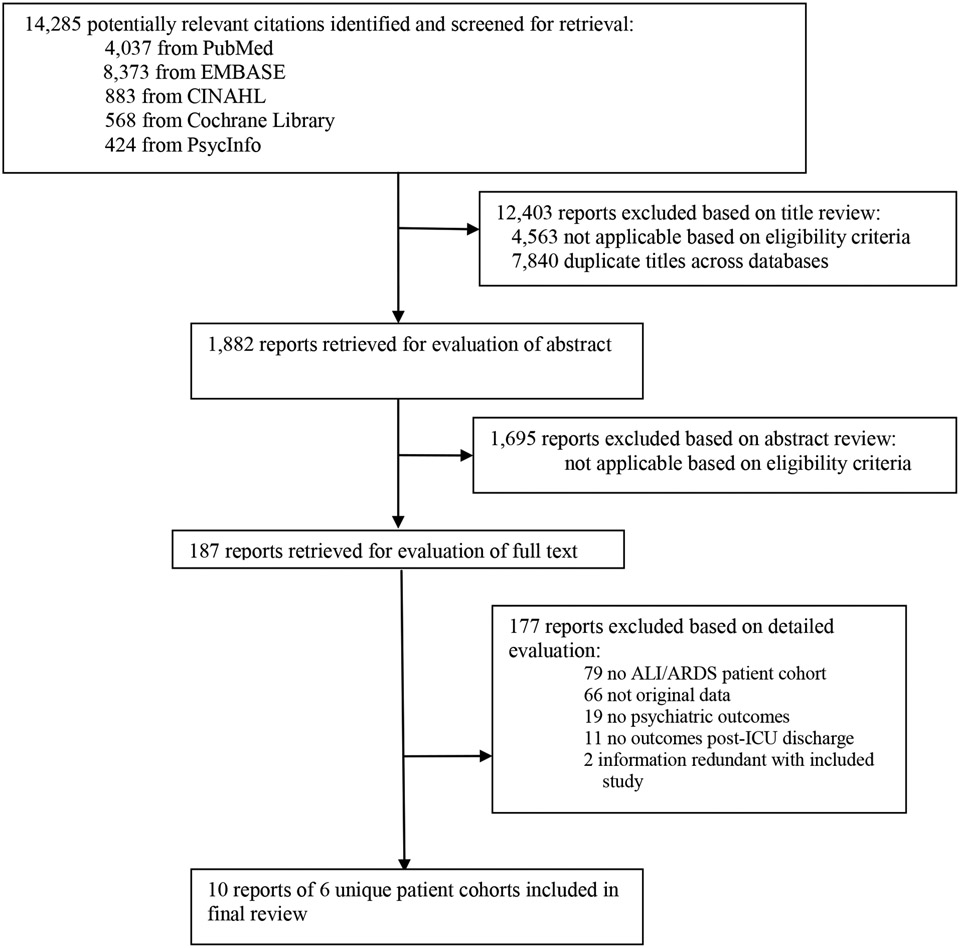
The authors reviewed 14,285 citations, 1,882 abstracts and 187 full-text articles (Figure 1). Ten articles describing six unique cohorts of ALI/ARDS survivors were eligible for data abstraction [twelve articles were originally identified, but two of them (8-9) were not included in this review, since these articles presented a summary of depression and anxiety data which were presented, in greater detail, in a subsequent article (10)]. The percent agreement (and kappa statistic) for each stage of the study selection and data abstraction process were: citation review, 91% (κ = 0.54); abstract review 98% (κ = 0.84); full text review 99% (κ = 0.89); and data abstraction, 99.5% (κ = 0.98). Of the ten studies reviewed, six were retrospective cohort studies (11-16), two were prospective cohort studies (10, 17), and two were cross-sectional studies (18-19). Six of the studies were conducted in the US (10-13, 17, 18), and four were conducted in Germany (14-16, 19).
Figure 1. Flow Diagram of Literature Search Results.
Abbreviations: ALI, acute lung injury; ARDS, acute respiratory distress syndrome
Table 1 shows baseline descriptive data for the ten studies, ordered by timing of follow-up assessments. Follow-up periods ranged from approximately 1 month (11) to a median of 96 months (16). These studies reported on 321 unique patients. Six of the studies excluded subjects with a history of psychiatric illness (variably defined - 10, 14-17, 19). None of the studies addressed baseline personality characteristics.
Table 1.
Study cohort characteristics, ordered by follow-up time
| Mean (Standard Deviation) or Median | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Study | Study type | N Enrolled | Inclusion (I) and exclusion (E) criteria | Sex (%) | Age in years |
Days in hospital |
Days in ICU |
Days of mechanical ventilation |
Apache II/[III] score |
LIS | Follow-up in months |
|
Shaw et al. 2001 11 |
Retrospective cohort | 20 | I: ventilated for at least 48 hours, ARDS E: none |
- | - | - | - | - | - | - | 1-1.5A |
|
Hopkins et al. 2004,10 2005 17 |
Prospective Cohort | 74 | I: >16 years of age, intubated, ARDS E: history of TBI, history of CNS disease, psychotic disorder, prior cognitive disability |
♂: 45% ♀: 55% |
46 (16) | 39 (22) | 34 (20) | 28 (19) | 18.1 (6.6) | - | 12, 24 |
|
Weinert et al. 1997 12 |
Retrospective cohort | 24 | I: >18 years of age, acute lung injury E: recent transplant recipient, clinically significant prior lung disease |
♂: 67% ♀: 33% |
40 (12) | - | - | 24 | - | 2.4 (0.5) | 19 (10), 15 |
|
Christie et al. 2006 18 |
Cross-sectional | 79 | I: ALI/ARDS E: none |
♂:15% ♀: 85% |
43 (13) | 57 (41) | - | - | - | - | 28 |
|
Schelling et al. 1998 14, B |
Retrospective cohort | 80 | I: >16 years of age, ARDS E: discharge <6 months before start of study, preexisting neurologic disease, preexisting psychiatric disease, history of cerebral trauma or surgery, history of CPR |
- | - | - | - | - | - | - | 48 |
|
Stoll et al. 1999 15, B |
Retrospective cohort | 52 | I: >16 years of age, ARDS E: same as Schelling et al. 1998C |
♂: 50% ♀: 50% |
37 | - | 30 | 27 | 22.5 | 3.25 | 60 |
|
Deja et al. 2006 19 |
Cross-sectional | 65 | I: >1 year from ICU discharge E: history of mental disease (as reported by patient or collateral informant) |
♂: 54% ♀: 46% |
39 (15) | - | 47 (32) | 30 (22) | 16 (6) | 3.2 (0.5) | 57 (32) |
|
Kapfhammer et al. 2004 16, B |
Retrospective cohort | 46 | I: >16 years of age, ARDS E: same as Schelling et al. 1998C |
♂: 52% ♀: 48% |
37 | - | - | 27 | 22.5 | 3.3 | 96 |
Abbreviations (in alphabetical order): ARDS = acute respiratory distress syndrome; ALI = acute lung injury; CNS = central nervous system; CPR = cardiopulmonary resuscitation; ICU = intensive care unit; LIS = Lung Injury Scale; TBI = traumatic brain injury; "-" = not reported.
range, not mean or median.
Measures of Psychiatric Symptoms and QOL
Two hundred seventy-seven subjects completed at least one depression measure, and 208 and 253 subjects completed at least one PTSD and anxiety measure, respectively. Six of the studies utilized in-person assessments (10-11, 14-17); three, mailed questionnaires (12, 13, 19); and one, a telephone interview (18). Two studies used a semi-structured diagnostic interview administered by a psychiatrist, the Structured Clinical Interview for DSM-IV (SCID) (15-16). The remaining studies used only questionnaires to assess psychopathology (Table 2).
Table 2.
Measurements of psychiatric symptoms/syndromes, ordered by follow-up time
| Mean (standard deviation) or median (interquartile difference) | |||||||
|---|---|---|---|---|---|---|---|
| Psychiatric Condition | Study | Instrument | Follow-up in months | N at follow-up | Mean/median | Cut-off score | Point prevalence |
| Depression | Hopkins et al. 2004 10, A | BDI | 12 | 66 | 9 (10) | 17 | 17% |
| Weinert et al. 1997 12 | CES-D | 19 (10), 15 | 24 | 20 (15) | 16 | 43% | |
| Hopkins et al. 2005 17, A | BDI | 24 | 62 | 10 (11) | 17 | 23% | |
| Christie et al. 2006 18 | ZDRS | 28 | 79 | - | - | 34% | |
| Deja et al. 2006 19 | SCL90r depression | 57 (32) | 62 | 55 (10) | - | - | |
| Kapfhammer et al. 2004 16, C | MADRS | 96 | 46 | 2 (17) | - | - | |
| SCID MDD | 96 | 46 | - | - | 4% | ||
| PTSD | Kapfhammer et al. 2004 16, C | PTSS-10 | 26 | - | - | ||
| SCID PTSD | 0 [d/c] | 46 | - | - | 44% | ||
| Shaw et al. 2001 11 | IES | 1-1.5D | 20 | 22 (15) | 30 | 35% | |
| Schelling et al. 1998 14, C | PTSS-10 | 48 | 80 | - | 35 | 28% | |
| Deja et al. 2006 19 | PTSS-10 | 57 (32) | 62 | 28 (14) | 35 | 29% | |
| Stoll et al. 1999 15, C | PTSS-10 | 60 | 52 | - | 35 | 21% | |
| SCID PTSD | 25% | ||||||
| Kapfhammer et al. 2004 16, C | PTSS-10 | 25 | - | - | |||
| SCID PTSD | 96 | 46 | - | - | 24% | ||
| Anxiety | Hopkins et al. 2004 10 2005 17 | BAI | 12 | 66 | 10 (10) | 17 | 24% |
| BAI | 24 | 62 | 10 (10) | 17 | 23% | ||
| Christie et al. 2006 18 | BAI | 28 | 79 | - | 17 | 48% | |
| Deja et al. 2006 19 | SCL90r anxiety | 57 (32) | 62 | 58 (9) | - | - | |
| Kapfhammer et al. 2004 16, C | STAS-S | 96 | 46 | 40 (32) | - | - | |
Abbreviations (in alphabetical order): BAI = Beck Anxiety Inventory; BDI = Beck Depression Inventory; CES-D = Center for Epidemiologic Studies Depression Scale; d/c = hospital discharge; IES = Impact of Events Scale; MADRS = Montgomery Asberg Depression Rating Scale; MDD = major depressive disorder; PTSD = post-traumatic stress disorder; PTSS-10 = Posttraumatic Symptom Scale-10; SCID =Structured Clinical Interview for DSM-IV; SCL90r = Symptom Checklist 90r; STAS-S = Spielberger State-Trait Anxiety Scale – state score; ZDRS = Zung Depression Rating Scale; "-" = not reported.
The two studies by Hopkins et al. (10, 17) reported data on the same cohort but at different follow-up times.
Point prevalence in Nelson et al. (13) is for 20/24 subjects in the cohort.
Stoll et al. (15) and Kapfhammer et al. (16) reported data on subgroups from the same cohort as Schelling et al. (15) but at different follow-up times.
range, not mean or median.
Seven studies measured QOL with the Medical Outcomes Study Short Form-36 (SF-36) (10, 12-14, 16, 17, 19); one also used the Sickness Impact Profile (SIP) (13).
Prevalence of Psychiatric Symptoms/Disorders and QOL
The point prevalence of questionnaire-ascertained clinically significant depressive symptoms ranged from 17% (10) to 43% (12), with a median prevalence of 28% (Table 2). Only one study employed the SCID to ascertain major depressive disorder (MDD) (16), the point prevalence was 4% at a median of 8 years. The point prevalence of significant posttraumatic stress symptoms using questionnaires ranged from 21% (15) to 35% (11), with a median of 28% (14). The point prevalence of SCID PTSD was 44% at hospital discharge (16), 25% at 5 years (15), and 24% at 8 years (16). The point prevalence of significant anxiety symptoms utilizing questionnaires ranged from 23% (17) to 48% (18), with a median of 24% (16).
Table 3 displays QOL results, ordered by follow-up time. The scores for most QOL domains were higher at subsequent follow-up times.
Table 3.
Measurements of quality of life, ordered by follow-up time
| Mean (standard deviation) or median (interquartile difference) | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Quality of Life Measures | |||||||||||||
| SF-36 Domain and Summary Scores | SIP domain scores | ||||||||||||
| Study | Follow-up in Months |
PF | RP | BP | GH | V | SF | RE | MH | PCS | MCS | Ph | Ps |
| Hopkins et al. 2004 10, A | 0 [d/c] | 23 (26) | 6 (20) | 55 (30) | 50 (20) | 31 (21) | 26 (25) | 68 (45) | 65 (23) | - | - | - | - |
| 12 | 55 (31) | 39 (41) | 58 (31) | 52 (26) | 51 (24) | 71 (31) | 74 (39) | 72 (23) | - | - | - | - | |
| Weinert et al. 1997 12 | 19 (10), 15 | 55 (38) | 42 (45) | 53 (31) | 51 (30) | 48 (27) | 57 (37) | 61 (44) | 62 (24) | 38 | 45 | - | - |
| Hopkins et al. 2005 17, A | 24 | 58 (32) | 53 (44) | 60 (30) | 54 (27) | 53 (26) | 72 (29) | 69 (41) | 66 (24) | - | - | - | - |
| Schelling et al. 1998 14, B | 48 | 63 (29) | 50 (43) | 60 (33) | 56 (25) | 49 (24) | 74 (30) | 66 (45) | 65 (21) | - | - | - | - |
| Deja et al. 2006 19 | 57 (32) | 73 (23) | 68 (39) | 64 (29) | 56 (23) | 51 (15) | 76 (21) | 76 (31) | 66 (15) | 44 (12) | 48 (9) | - | - |
| Kapfhammer et al. 2004 16, B | 96 | 83 (41) | 75 (100) | 63 (59) | 60 (30) | 50 (25) | 88 (37) | 100 (67) | 74 (29) | - | - | - | - |
Abbreviations: SF-36 = Medical Outcomes Study Short Form – 36; PF = Physical Functioning; RP = Role Physical; BP = Bodily Pain; GH = General Health; V = Vitality; SF = Social Functioning; RE = Role Emotional;
MH = Mental Health; PCS = Physical Component Summary; MCS = Mental Component Summary; SIP = Sickness Impact Profile; Ph = Physical Component Score; Ps = Psychosocial Component Score; "-" = not reported.
Potential Risk Factors for Psychiatric Symptoms
Only three studies prospectively assessed potential risk factors for psychiatric morbidity after ALI/ARDS (12, 13, 16) (Table 4). Durations of sedation, mechanical ventilation, and ICU stay each predicted later depressive and PTSD symptoms.
Table 4.
Prospectively-assessed potential risk factors for later depressive and/or post-traumatic stress symptoms/disorder
| Test value | ||||
|---|---|---|---|---|
| Study | Measure of Association | Potential risk factor | depressive symptoms | post-traumatic stress symptoms/disorder |
|
Weinert et al. 1997 12 |
Spearman Correlation | a) Days of mechanical ventilation b) Months since ALI |
a) 0.32 (p = 0.13) b) −0.40 (p = 0.05) |
- |
|
Nelson et al. 2000 13, A |
Pearson Correlation | a) Days in ICU b) Days of mechanical ventilation c) Apache III Score d) Days of sedation e) Days of neuromuscular blockade |
a) 0.26 (p = 0.01) b) 0.34 (p = 0.01) c) 0.01 (p = 0.64) d) 0.30 (p = 0.01) e) 0.06 (p = 0.24) |
a) 0.28 (p = 0.01) b) 0.28 (p = 0.02) c) 0.03 (p = 0.46) d) 0.32 (p = 0.01) e) 0.20 (p = 0.04) |
|
Kapfhammer et al. 2004 16 |
Kruskal-Wallis ANOVA of ranks test (H) for continuous variables, Fisher’s exact test for discrete variables | a) Days in ICU b) Age c) Sex d) Premorbid psychopathology C e) Apache II score f) LIS |
- | a) H = 7.37, df = 2 (p < 0.04)
B b) n.s. c) n.s. d) n.s. e) n.s. f) n.s. |
Abbreviations: ALI = acute lung injury; ANOVA = analysis of variance; df = degrees of freedom; ICU = intensive care unit; "-" = not reported.
The instrument used to detect symptoms of PTSD was a non-validated questionnaire derived by the study authors from the DSM-IV criteria for PTSD; specific symptoms included feeling irritable or tense, difficulty concentrating, memory problems, feeling fearful or anxious, feeling angry, lack of sleep, and bad memories or dreams about the hospitalization. These authors noted higher CES-D scores in 4 patients with a known diagnosis of depression or antidepressant treatment (mean = 29) versus the remaining 16 patients (mean = 22); however, the difference was not statistically significant. This study involved the same sample as Weinert et al. 12
Patients with PTSD at follow-up spent a median 70 days in the ICU; those with “sub-PTSD” or no PTSD spent a median of 28 days in the ICU.
Only 1 of these patients had a pre-ARDS history of major depression, and only 2 had a history of alcohol abuse; premorbid psychopathology was assessed retrospectively.
Three studies reported that recall of ICU-related pain, breathing difficulties, nightmares, and anxiety was associated with PTSD symptoms (14, 15, 19), and one study also reported that recall of limited social support was also associated with PTSD symptoms (19). In each case, these potential risk factors were assessed retrospectively, at the time of the PTSD assessments.
Associations of Psychiatric Symptoms/Syndromes and QOL
Four studies assessed relationships between psychiatric symptoms/syndromes and QOL (SF-36) (10, 12, 16, 19) (Table 5). Symptoms of depression, non-specific anxiety, and PTSD were associated with lower QOL in each case. Psychiatric symptoms/syndromes were more strongly associated with mental health QOL domains (vitality, social functioning, role-emotional, and mental health) than physical domains (physical functioning, role-physical, bodily pain, and general health), though relationships with physical domains were also substantial. In one small study (12), depressive symptoms were very strongly associated with a diminished mental component score (Spearman correlation = −0.94).
Table 5.
Associations of Psychiatric Symptoms/Syndromes with Quality of Life
| Study | Measure of Association |
Instrument | Test value | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| SF-36 Domain | ||||||||||||
| PF | PR | BP | GH | V | SF | ER | MH | PCS | MCS | |||
|
Hopkins et al. 2004 10 |
Pearson Correlation | BDI | −0.29 p = 0.020 |
−0.46 p < 0.001 |
−0.56 p < 0.001 |
−0.59 p < 0.001 |
− 0.57 p < 0.001 |
− 0.56 p < 0.001 |
− 0.65 p < 0.001 |
− 0.76 p < 0.001 |
- | - |
| BAI | −0.30 p = 0.013 |
−0.45 p < 0.001 |
−0.58 p < 0.001 |
−0.51 p < 0.001 |
−0.57 p < 0.001 |
−0.56 p < 0.001 |
−0.45 p < 0.001 |
−0.59 p < 0.001 |
- | - | ||
|
Weinert et al. 1997 12 |
Spearman correlation | CES-D | - | - | - | - | - | - | - | - | −0.17 p = 0.43 |
−0.94 p < 0.0001 |
|
Deja et al. 2006 19 |
ANOVA (F) | PTSS-10 | 36.8 p = 0.0001 |
17.9 p = 0.0001 |
35.8 p = 0.0001 |
37.5 p = 0.0001 |
63.8 p = 0.0001 |
37.6 p = 0.0001 |
31.3 p = 0.0001 |
54.1 p = 0.0001 |
34.4 p = 0.0001 |
48.9 p = 0.0001 |
|
Kapfhammer et al. 2004 16 |
Kruskal-Wallis ANOVA of ranks test (H) | SCID PTSD | 9.2 p = 0.44 |
6.4 p = 0.13 |
9.9 p = 0.34 |
12.1 p = 0.002 |
11.82 p = 0.06 |
10.75 p = 0.005 |
5.32 p = 0.07 |
11.92 p = 0.003 |
- | - |
Abbreviations (in alphabetical order): ANOVA = analysis of variance; BAI = Beck Anxiety Inventory; BDI = Beck Depression Inventory; CES-D = Center for Epidemiologic Studies Depression scale; PTSD = post-traumatic stress disorder; PTSS-10 = Posttraumatic Symptom Scale-10; SCID = Structured Clinical Interview for DSM-IV; SF-36 = Medical Outcomes Study Short Form-36; "-" = not reported.
SF-36 abbreviations: PF = Physical Functioning; PR = Role Physical; BP = Bodily Pain; GH = General Health; V = Vitality; SF = Social Functioning; ER = Role Emotional; MH = Mental Health; MCS = Mental Component Summary; PCS = Physical Component Summary.
DISCUSSION
This systematic review of psychiatric morbidity in ALI/ARDS survivors highlights three important issues. First, the point prevalences of substantial symptoms of depression, PTSD, and non-specific anxiety are quite high at a year or more after ALI/ARDS. Across studies, the median point prevalence of each syndrome was >20%, substantially higher than the 6.7% and 3.5% one-year prevalences of MDD and PTSD, respectively, in a recent study of US adults that utilized structured interviews (20). To our knowledge, there are no general population estimates of psychiatric disorder prevalences using the questionnaires discussed in this review. Nevertheless, it is interesting to note that the point prevalences of substantial depressive and PTSD symptoms in ALI/ARDS survivors are higher than those in survivors of myocardial infarction [depression 9% at 12 months (21) and PTSD 9.8% at 6 months (23)] , and as high as those in survivors of coronary artery bypass graft surgery[depression 38% at a mean of 5.2 years (22)]; the latter studies used some of the same questionnaires, with similar cut-off scores for case definition (21-23). Second, durations of sedation, mechanical ventilation, and ICU LOS may be risk factors for subsequent depression and/or PTSD after ALI/ARDS. Third, the presence of psychiatric symptoms is associated with lower QOL in ALI/ARDS survivors.
There are limitations to the existing literature. First, most studies relied exclusively on questionnaires to estimate the burden of psychopathology in ALI/ARDS survivors. Most psychiatric questionnaires are designed as screening instruments or measures of symptom severity in patients with known disorders (24). Only two studies utilized expert clinicians and semi-structured diagnostic interviews (15-16), and one of these only included the PTSD section of the SCID (15). Of the questionnaires employed, only the PTSS-10 has been validated specifically in ARDS survivors (15). The Beck Anxiety Inventory, the only measure of non-specific anxiety in the eligible studies (10, 17, 18), appears more sensitive to panic than other anxiety syndromes (25-26); consequently, the prevalence of significant generalized anxiety symptoms, for example, may be underestimated in our review. The studies that used the Beck Depression Inventory (BDI) employed a cut-off score of 17 (10, 17), which indicates “moderate or greater” depression but may be high as a screening threshold (27). The Center for Epidemiologic Studies Depression Scale (CES-D), used to measure depression in one of the studies (12), may lack specificity for depression (28-29). Also, the studies that used the CES-D employed the standard cut-off score of 16, which may be low (30). Thus, threshold choices likely account for some of the variability in depression prevalences across studies. The only study to utilize clinicians in diagnosing MDD found a point prevalence of 4% at a median of 8 years post-ARDS (16); it seems likely, based on questionnaire results, that the point prevalence of clinician-diagnosed MDD would be substantially higher in the first two years after ALI/ARDS. Future studies of psychopathology in ALI/ARDS survivors should utilize expert clinicians to conduct broad diagnostic interviews, to establish prevalence rates and to evaluate the psychometric properties of existing questionnaires in this population.
Second, additional research is required to understand risk factors for psychopathology in ALI/ARDS survivors. Although some studies attempted to exclude patients with prior psychopathology (14-15, 19), presumably to determine the independent effect of ALI/ARDS on first incidence of psychopathology, these studies appeared to use limited information (e.g., chart reviews or brief interviews of patients or collateral informants), not direct lifetime diagnostic interviews, to determine who should be excluded. As reported in Kapfhammer et al. (16), such screening was not entirely successful, as a few patients with pre-ARDS histories of alcohol abuse or depression were included in a cohort that was meant to exclude such patients (14-16). In addition, successfully excluding patients with pre-ALI/ARDS psychopathology is problematic in that it prevents estimation of the extent to which pre-ALI/ARDS psychopathology serves as a risk factor for post-ALI/ARDS psychopathology. An additional potential risk factor for post-ALI/ARDS psychopathology, not assessed in any of the studies, is pre-ALI/ARDS personality vulnerabilities, such as high neuroticism (negative affectivity). High neuroticism and prior anxiety and depressive disorders are potent predictors of depression and PTSD in the context of stress (31-34). Future studies should explicitly assess these variables as potential risk factors. Regarding the potential risk factors identified in this review (durations of sedation, mechanical ventilation, and ICU stay), it remains unclear whether these correlated characteristics are themselves causally related to post-ALI/ARDS psychopathology, or if these factors reflect clinicians’ management of anxiety and/or agitated delirium in the ICU (e.g., increased use of sedation could lead to prolonged mechanical ventilation and ICU stays). ICU clinical management, or anxiety or agitated delirium in the ICU, may be the causal risk factor(s) or markers of risk for post-ALI/ARDS psychopathology. Clarification of these issues is an important goal for future research that could facilitate prevention (e.g., via minimization of GABA-ergic sedative agents in the ICU) and identification of patients at high risk for psychiatric morbidity (for monitoring and early intervention).
Currently, there is much speculation regarding the possible cause(s) of depressive and/or PTSD symptoms in survivors of critical illnesses like ALI/ARDS. One potential “neurobiologic” etiology of both depression and PTSD in this patient population is systemic inflammation associated with ALI/ARDS and its risk factors. There is some evidence that inflammatory cytokines may play a role in the development of general medical illness-related psychopathology. For example, elevated serum levels of IL-6 are associated with depression in patients with cancer (35). Also, administration of an anti-inflammatory glucocorticoid, hydrocortisone, may be associated with a decrease in the incidence of PTSD in survivors of septic shock (36) or cardiac surgery (37). There are certainly other, more “narrative” explanations for post-ALI/ARDS psychopathology. For example, patients may develop PTSD symptoms as a result of extremely frightening memories, such as those of severe dyspnea and/or delirium-related psychotic experiences, perhaps shaped by coincident invasive procedures (16, 38). Finally, loss can be substantial in patients who survive ALI/ARDS. Many patients leave the ICU with deficits in physical and cognitive function, leading to a delayed return to work; in addition, family lives can be disrupted by prolonged hospitalizations and recovery periods. Such stress could be an “understandable” cause of depression/demoralization. To our knowledge, no studies have attempted to develop a comprehensive model of post-ALI/ARDS psychopathology; it is possible that these and other potential etiologic factors play a role.
Several potential limitations of this systematic review should be noted. First, it is unclear whether the results of this review are specific to ALI/ARDS survivors versus survivors of critical illness in general. We know of no studies comparing PTSD and/or depressive symptoms in survivors of ALI/ARDS to a control group of ICU survivors without ALI/ARDS. Certain aspects of ALI/ARDS (e.g. systemic inflammation, severity of illness, and prolonged ICU stays) may add risk for psychopathology in survivors. Nevertheless, it remains unclear to what extent risk factors for ALI/ARDS (e.g., sepsis) are associated with equivalent psychopathology in survivors who did not have ALI/ARDS. These are important areas for future research. Second, confidence regarding the identified potential risk factors should be tempered, given the methodological issues described above, the small number of studies, and the small sample sizes. Third, despite a comprehensive search of 14,285 citations, potentially eligible studies may have been missed due to inconsistent indexing in the electronic citation databases.
In conclusion, ALI/ARDS survivors appear to have high prevalences of significant depressive, PTSD, and other anxiety symptoms which adversely affect QOL. Longer durations of sedation, mechanical ventilation, and ICU stay may be risk factors for these psychiatric outcomes in ALI/ARDS survivors, although the causal mechanisms are not fully elucidated at this time. Future studies should include more rigorous diagnostic evaluations and risk factor assessments (e.g. premorbid personality traits and prior psychiatric history). In the meantime, clinicians should recognize that psychiatric illness is common in ALI/ARDS survivors, necessitating comprehensive evaluations and treatment.
ACKNOWLEDGEMENTS
The authors thank Jason D. Christie, M.D., Ramona O. Hopkins, Ph.D., Gustav Schelling, M.D., Richard J. Shaw, M.D., and Craig R. Weinert, M.D., M.P.H., for providing additional data for this review.
Dr. Needham is supported by a Clinician-Scientist Award from the Canadian Institutes of Health Research and by the National Institutes of Health (Acute Lung Injury SCCOR Grant # P050 HL 73994). Dr. Bienvenu is supported by a Career Development Award from the National Institutes of Health (K23 MH64543).
Abbreviations ( in alphabetical order):
- ALI
acute lung injury
- ARDS
acute respiratory distress syndrome
- BAI
Beck Anxiety Inventory
- BDI
Beck Depression Inventory
- CES-D
Center for Epidemiologic Studies Depression scale
- ICU
intensive care unit
- IES
Impact of Events Scale
- LOS
length of stay
- MADRS
Montgomery-Asberg Depression Rating Scale
- MDD
major depressive disorder
- PTSD
posttraumatic stress disorder
- PTSS-10
Posttraumatic Symptom Scale-10
- QOL
quality of life
- SCID
Structured Clinical Interview for DSM-IV
- SCL90r
Symptom Checklist 90r
- SF-36
Medical Outcomes Study Short Form-36
- SIP
Sickness Impact Profile
- STAS-S
Spielberger State-Trait Anxiety Scale-State
- US
United States
Contributor Information
Dimitry S. Davydow, Department of Psychiatry and Behavioral Sciences, Johns Hopkins University School of Medicine, Baltimore, USA..
Sanjay V. Desai, Division of Pulmonary and Critical Care Medicine, Johns Hopkins University School of Medicine, Baltimore, USA.
Dale M. Needham, Division of Pulmonary and Critical Care Medicine, Johns Hopkins University School of Medicine, Baltimore, USA.
O. Joseph Bienvenu, Department of Psychiatry and Behavioral Sciences, Johns Hopkins University School of Medicine, Baltimore, USA.
REFERENCES
- 1.Rubenfeld GD, Caldwell E, Peabody E, Weaver J, Martin DP, Neff M, Stern EJ, Hudson LD. Incidence and outcomes of acute lung injury. N Engl J Med 2005;353:1685–1693. [DOI] [PubMed] [Google Scholar]
- 2.Fan E, Needham DM, Stewart TE. Ventilatory management of acute lung injury and acute respiratory distress syndrome. JAMA 2005;294:2889–2896. [DOI] [PubMed] [Google Scholar]
- 3.Milberg JA, Davis DR, Steinberg KP, Hudson LD. Improved survival of patients with acute respiratory distress syndrome (ARDS): 1983-1993. JAMA 1995;273:306–309. [PubMed] [Google Scholar]
- 4.Dowdy DW, Eid MP, Dennison CR, Mendez-Tellez PA, Herridge MS, Guallar E, Pronovost PJ, Needham DM. Quality of life after acute respiratory distress syndrome: a meta-analysis. Intensive Care Med 2006;32:1115–1124. [DOI] [PubMed] [Google Scholar]
- 5.Herridge MS, Cheung AM, Tansey CM, Matte-Martyn A, Diaz-Granados N, Al-Saidi F, Cooper AB, Guest CB, Mazer CD, Mehta S, Stewart TE, Barr A, Cook D, Slutsky AS. One-year outcomes in survivors of the acute respiratory distress syndrome. N Eng J Med 2003;348:683–693. [DOI] [PubMed] [Google Scholar]
- 6.Hopkins RO, Herridge MS. Quality of life, emotional abnormalities, and cognitive dysfunction in survivors of acute lung injury/acute respiratory distress syndrome. Clin Chest Med 2006;27:679–689. [DOI] [PubMed] [Google Scholar]
- 7.Viera AJ, Garrett JM. Understanding interobserver agreement: the kappa statistic. Fam Med 2005;37:360–363. [PubMed] [Google Scholar]
- 8.Hopkins RO, Weaver LK, Pope D, Orme JF Jr., Bigler ED, Larson-Lohr V. Neuropsychological sequelae and impaired health status in survivors of severe acute respiratory distress syndrome. Am J Respir Crit Care Med 1999;160:50–56. [DOI] [PubMed] [Google Scholar]
- 9.Orme JF Jr., Romney JS, Hopkins RO, Pope D, Chan KJ, Thomsen G, Crapo RO, Weaver LK. Pulmonary function and health-related quality of life in survivors of acute respiratory distress syndrome. Am J Respir Crit Care Med 2003;167:690–694. [DOI] [PubMed] [Google Scholar]
- 10.Hopkins RO, Weaver LK, Chan KJ, Orme JF Jr. Quality of life, cognitive, and emotional function following acute respiratory distress syndrome. J Int Neuropsychol Soc 2004;10:1005–1017. [DOI] [PubMed] [Google Scholar]
- 11.Shaw RJ, Harvey JE, Nelson KL, Gunary R, Kruk H, Steiner H. Linguistic analysis to assess medically related posttraumatic stress symptoms. Psychosomatics 2001;42:35–40. [DOI] [PubMed] [Google Scholar]
- 12.Weinert CR, Gross CR, Kangas JR, Bury CL, Marinelli WA. Health-related quality of life after acute lung injury. Am J Respir Crit Care Med 1997;156:1120–1128. [DOI] [PubMed] [Google Scholar]
- 13.Nelson BJ, Weinert CR, Bury CL, Marinelli WA, Gross CR. Intensive care unit drug use and subsequent quality of life in acute lung injury patients. Crit Care Med 2000;28:3626–3630. [DOI] [PubMed] [Google Scholar]
- 14.Schelling G, Stoll C, Haller M, Briegel J, Manert W, Hummel T, Lenhart A, Heyduck M, Polasek J, Meier M, Preuss U, Bullinger M, Schuffer W, Peter K. Health-related quality of life and posttraumatic stress disorder in survivors of the acute respiratory distress syndrome. Crit Care Med 1998;26:651–659. [DOI] [PubMed] [Google Scholar]
- 15.Stoll C, Kapfhammer HP, Rothenhausler HB, Haller M, Briegel J, Schmidt M, Krauseneck T, Durst K, Schelling G. Sensitivity and specificity of a screening test to document traumatic experiences and diagnose post-traumatic stress disorder in ARDS patients after intensive care treatment. Intensive Care Med 1999;25:697–704. [DOI] [PubMed] [Google Scholar]
- 16.Kapfhammer HP, Rothenhausler HB, Krauseneck T, Stoll C, Schelling G. Posttraumatic stress disorder and health-related quality of life in long-term survivors of acute respiratory distress syndrome. Am J Psychiatry 2004;161:45–52. [DOI] [PubMed] [Google Scholar]
- 17.Hopkins RO, Weaver LK, Collinridge D, Parkinson RB, Chan KJ, Orme JF Jr. Two-year cognitive, emotional, and quality-of-life outcomes in acute respiratory distress syndrome. Am J Respir Crit Care Med 2005;171:340–347. [DOI] [PubMed] [Google Scholar]
- 18.Christie JD, Biester RC, Taichman DB, Shull WH Jr., Hansen-Flaschen J, Shea JA, Hopkins RO. Formulation and validation of a telephone battery to assess cognitive function in acute respiratory distress syndrome survivors. J Crit Care 2006;21:125–132. [DOI] [PubMed] [Google Scholar]
- 19.Deja M, Denke C, Webber-Carstens S, Schroder J, Pille CE, Hokema F, Falke KJ, Kaisers U. Social support during intensive care unit stay may improve mental impairment and consequently health-related quality of life in survivors of severe acute respiratory distress syndrome. Crit Care 2006;10:R147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kessler RC, Chui WT, Demler O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey replication. Arch Gen Psychiatry 2005;62:617–627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Legault SE, Joffe RT, Armstrong PW. Psychiatric morbidity during the early phase of coronary care for myocardial infarction: association with cardiac diagnosis and outcome. Can J Psychiatr 1992;37:316–325. [DOI] [PubMed] [Google Scholar]
- 22.Blumenthal JA, Lett HS, Babyak MA, White W, Smith PK, Mark DB, Jones R, Mathew JP, Newman MF, and for the NORG Investigators. Depression as a risk factor for mortality after coronary artery bypass surgery. Lancet 2003;362:604–609. [DOI] [PubMed] [Google Scholar]
- 23.Shemesh E, Rudnick A, Kaluski E, Milovanov O, Salah A, Alon D, Dinur I, Blatt A, Metzkort M, Golik A, Verd Z, Cotter G. A prospective study of posttraumatic stress and nonadherence in survivors of a myocardial infarction. Gen Hosp Psychiatry 2001;23:215–222. [DOI] [PubMed] [Google Scholar]
- 24.Rush AJ Jr., Pincus HA, First MB, Blacker D, Endicott J, Keith SJ, Phillips KA, Ryan ND, Smith GR Jr., Tsuang MT, Widiger TA, Zarin DA. Handbook of psychiatric measures. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- 25.Cox BJ, Cohen E, Direnfeld DM, Swinson RP. Does the Beck Anxiety Inventory measure anything beyond panic attack symptoms? Behavior Research and Therapy 1996;34:949–954. [DOI] [PubMed] [Google Scholar]
- 26.Leyfer OT, Ruberg JL, Woodruff-Borden J. Examination of the utility of the Beck Anxiety Inventory and its factors as a screener for anxiety disorders. J Anxiety Disord 2006;20:444–458. [DOI] [PubMed] [Google Scholar]
- 27.Lasa L, Ayuso-Mateos JL, Vazquez-Barquero JL, Diez-Manrique FJ, Dowrick CF. The use of the Beck Depression Inventory to screen for depression in the general population: a preliminary analysis. J Affect Disord 2000;57:261–265. [DOI] [PubMed] [Google Scholar]
- 28.Fechner-Bates S, Coyne JC, Schwenk TL. The relationship of self-reported distress to depressive disorders and other psychopathology. J Consult Clin Psychol 1994;62:550–559. [DOI] [PubMed] [Google Scholar]
- 29.McQuaid JR, Stein MB, McCahill M, Laffaye C, Rivel W. Use of brief psychiatric screening measures in a primary care sample. Depress Anxiety 2000;12:21-29. [DOI] [PubMed] [Google Scholar]
- 30.Lyness JM, Noel TK, Cox C, King DA, Conwell Y, Caine ED. Screening for depression in elderly primary care patients: a comparison of the Center for Epidemiologic Studies-Depression Scale and the Geriatric Depression Scale. Arch Intern Med 1997;157:449–454. [PubMed] [Google Scholar]
- 31.Kendler KS, Kuhn J, Prescott CA. The interrelationship of neuroticism, sex, and stressful life events in the prediction of episodes of major depression. Am J Psychiatry 2004;161:631–636. [DOI] [PubMed] [Google Scholar]
- 32.Kendler KS, Gardner CO, Prescott CA. Toward a comprehensive developmental model for major depression in men. Am J Psychiatry 2006;163:115–124. [DOI] [PubMed] [Google Scholar]
- 33.Bienvenu OJ, Stein MB. Personality and anxiety disorders: a review. J Personal Disord 2003;17:139–151. [DOI] [PubMed] [Google Scholar]
- 34.Brewin CR, Andrews B, Valentine JD. Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. J Consult Clin Psychol 2000;68:748–766. [DOI] [PubMed] [Google Scholar]
- 35.Musselman DL, Miller AH, Porter MR, Manatunga A, Gao F, Penna S, Pearce BD, Landry J, Glover S, McDaniel JS, Nemeroff CB. Higher than normal plasma interleukin-6 concentrations in cancer patients with depression: preliminary findings. Am J Psychiatry 2001;158:1252–1257. [DOI] [PubMed] [Google Scholar]
- 36.Schelling G, Briegel J, Roozendaal B, Stoll C, Rothenhausler HB, Kapfhammer HP. The effect of stress doses of hydrocortisone during septic shock on posttraumatic stress disorder in survivors. Biol Psychiatry 2001;50:978–985. [DOI] [PubMed] [Google Scholar]
- 37.Schelling G, Kilger E, Roozendaal B, De Quervain DJ, Briegel J, Dagge A, Rothenhausler HB, Krauseneck T, Nollert G, Kapfhammer HP. Stress doses of hydrocortisone, traumatic memories, and symptoms of posttraumatic stress disorder in patients after cardiac surgery: a randomized study. Biol Psychiatry 2004;55:627–633. [DOI] [PubMed] [Google Scholar]
- 38.Jones C, Griffiths RD, Humphris G, Skirrow PM. Memories, delusions, and the development of acute posttraumatic stress disorder-related symptoms after intensive care. Crit Care Med 2001;29:573–580. [DOI] [PubMed] [Google Scholar]