Abstract
Objective
To explore the effects of green spaces exposure on common psychiatric disorders.
Methods
PubMed, Embase, Web of Science and MEDLINE were screened and articles published prior to November 15, 2023 were included. Analyses were performed on common psychiatric disorders, categorized into depression, anxiety, dementia, schizophrenia, and attention deficit hyperactivity disorder (ADHD). And the subgroup analyses were conducted for depression, anxiety, dementia, and schizophrenia.
Results
In total, 2,0064 studies were retrieved, 59 of which were included in our study; 37 for depression, 14 for anxiety, 8 for dementia, 7 for schizophrenia and 5 for ADHD. Green spaces were found to benefit the moderation of psychiatric disorders (OR = 0.91, 95% CI: 0.89 to 0.92). Green spaces positively influence depression (OR = 0.89, 95% CI: 0.86 to 0.93), regardless of the cross-sectional or cohort studies. Green spaces can also help mitigate the risk of anxiety (OR = 0.94, 95%CI:0.92 to 0.96). As an important index for measuring green spaces, a higher normalized difference vegetation index (NDVI) level related to a lower level of depression (OR = 0.95, 95%CI:0.91 to 0.98) and anxiety (OR = 0.95, 95%:0.92 to 0.98). The protection was also found in dementia (OR = 0.95, 95% CI: 0.93 to 0.96), schizophrenia (OR = 0.74, 95% CI: 0.67 to 0.82), and ADHD (OR = 0.89, 95% CI: 0.86 to 0.92) results.
Conclusion
Green spaces decrease the risk of psychiatric disorders, including depression, anxiety, dementia, schizophrenia, and ADHD. Further studies on green spaces and psychiatric disorders are needed, and more green spaces should be considered in city planning.
Keywords: Common psychiatric disorders, Green spaces, NDVI, Mechanism
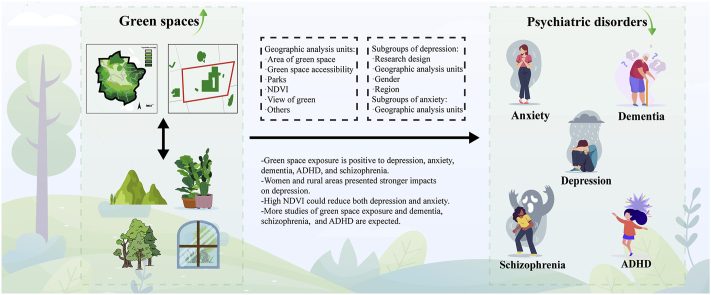
Graphical abstract
Highlights
-
•
Exposure to green spaces decrease the risk of common psychiatric disorders.
-
•
Increased NDVI may reduce the risk of depression and anxiety potentially.
-
•
Gender, study design, and geographical analytical units can affect correlation.
1. Introduction
Psychiatric disorders stress large burdens on society around the world. And as common psychiatric disorders, depression, anxiety, dementia, schizophrenia, and ADHD afflict an increasing number of individuals (Marshall, 2020; Posner et al., 2020; Prince et al., 2013). By 2030, depression is expected to become the main reason of death worldwide, imposing a large social burden (Hou et al., 2022). Some studies have indicated that up to 44% of the adult US population may suffer from anxiety (Kavelaars et al., 2023). The number of global dementia patients is predicted to reach to 65.7 million in 2030 (Prince et al., 2013). People with schizophrenia suffer from cognition function disturbance, abnormal behavior, and may sink into apathy, which bothered 1 in 100 individuals (Campeau et al., 2022). And as a neurodevelopmental disorder, ADHD held prevalence over 5%, especially found in children (Drechsler et al., 2020). The situations mentioned above point to the importance of exploring ways to reduce the incidence of psychiatric disorders.
Research has demonstrated the positive impact of being connected to nature on well-being and promoting pro-environmental behaviors (Lumber et al., 2017). It is said that exposure to greenness at youth could reduce odds of having a range of psychiatric disorders (Engemann et al., 2019). And an increasing number of researches have revealed that green spaces separately played a potential role in reducing depression, anxiety, dementia, schizophrenia, and ADHD. After searching a large number of articles, although most researchers are optimistic about the role of green space, we cannot rule out whether the effect of green space on psychiatric illness is disturbed by a variety of factors, including country development (Bloemsma et al., 2022; Mukherjee et al., 2017), gender (Donovan et al., 2019; Heo et al., 2021; Reklaitiene et al., 2014), related green space exposure indicators or the measurement of green space types (Astell-Burt et al., 2020, p. 145; Feng et al., 2022; Nishigaki et al., 2020). In addition, in the process of searching for articles, we also found a meta-analysis of the effects of green space on anxiety and depression (Liu et al., 2023), which is undeniably useful for improving our research, but it is worth mentioning that their research scope is relatively limited, analyzing the main indicators of green space exposure, i.e., the in-depth impact of NDVI and green space proportion on anxiety and depression, while we analyzed depression and anxiety on the basis of the general direction of psychiatric disorders, which are more macroscopic, including larger sample sizes, and exploring more confounding factors and the underlying mechanisms.
We conducted a meta-analysis to systematically study the relationships between green spaces and psychiatric illnesses mentioned above. And we conducted further subgroup analysis of the geographical analysis units to explore different possibilities between them. Moreover, the large and diverse sample size of depression also facilitated our subgroup analysis of study method, gender, region. We hope that this study will broaden the scope of research on the significance of green spaces toward alleviating common psychiatric illness and supply a scientific basis for the improved planning of green spaces construction.
2. Materials and method
2.1. Search strategy
The meta-analysis was conducted under the guidance of the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) statement guidelines. We screened PubMed, Embase, Web of science and MEDLINE databases for studies published before November 15, 2023. The search string is accessible in the Supplementary Material.
2.2. Selection criteria
Studies satisfying the following standards were included and considered to be of high quality: (1) The study must be observation research; (2) Newcastle-Ottawa scale (NOS) (Margulis et al., 2014) score and Joanna Briggs Institute (JBI) (Papalia et al., 2022) score respectively evaluate cohort and cross-sectional studies. Only when NOS score >7 or JBI score has “no” or “unclear” responses below two (score ≥7), the study can be included; (3) The study must have specific and appropriate standards to measure green spaces (e.g., NDVI, view, area, accessibility, numbers); (4) Psychiatric disorders including depression, anxiety, dementia, schizophrenia, and ADHD must be evaluated by scale, questionnaire or hospital diagnosis; (5) The study should not be meta-analyses, reviews, comments, books, or conference records; (6) Studies with original texts; (7) Study results should be shown in concrete Odds Ratio (OR), Risk Ratio (RR) Hazard Ratio (HR) or Prevalence Radio (PR).
2.3. Data collection
Studies included in the review provided the following information: author, publication year, region, sample size, age, study method, geographic analysis units, disease, adjusted OR with 95% confidence interval (CI) and NOS or JBI scores. The PR was similarly equal to the OR value and RR value could be converted into OR (Shor et al., 2017). Notably, several studies combined depression and anxiety as a total result, while others considered them separately or only one of them. Therefore, when encountering mixed studies, we chose separate values; otherwise, the values were combined. Studies of dementia, schizophrenia, and ADHD each has its own definite outcome.
2.4. Risk of bias assessment
Two investigators examined the quality of the included studies separately. Disagreements were intensively discussed, and finally, a unified outcome was presented. We used the NOS scores to measure cohort studies and the JBI scores to evaluate cross-sectional studies (Peng et al., 2022). We considered that a study with a NOS score >7 was of high quality or a JBI assessment that had “no” or “unclear” responses below two, indicated a low risk of bias (Papalia et al., 2022); otherwise, it would be low quality or high risk of bias.
2.5. Data analysis
We used Stata version 15 (College Station, TX, USA) to conduct the analysis. Heterogeneity was determined using the I2 statistic. A random-effects model was employed when I2 >50%, indicating substantial heterogeneity. Fixed effects model was chosen when I2 ≤50 (Zhou et al., 2021). The random-effects model was applied when the heterogeneity of outcomes exceeded 50%. Subgroup analyses were conducted and forest plots were presented. Begg's test (Begg & Mazumdar, 1994), trim and fill method (Duval & Tweedie, 2000), and funnel plots were used to detect publication bias. Finally, the sensitivity analysis was conducted by “leave-one-out”.
3. Results
3.1. Search results
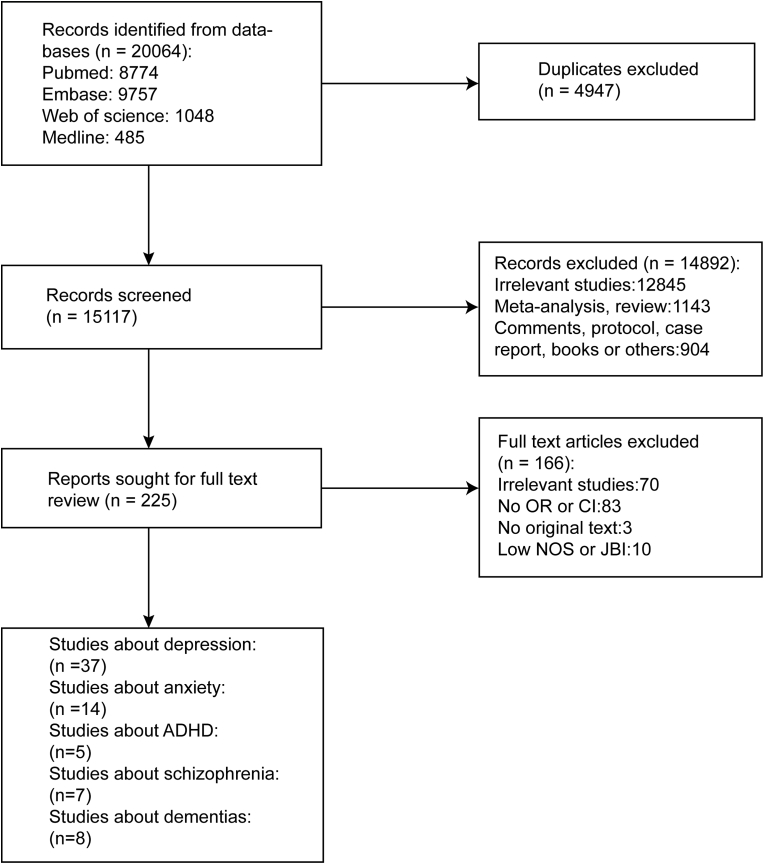
After thorough search and retrieval, 20,064 studies were included in our study, of which 15,117 remained after the removal of duplicate studies. A total of 14,892 studies were excluded after a review of titles and abstracts. 225 were further assessed by screening the full text. Finally, 59 articles were included in our study, among which 37 were on depression (Asri et al., 2021; Astell-Burt & Feng, 2019; Bezold et al., 2018a, 2018b; Bustamante et al., 2022; Dzhambov et al., 2021; Generaal et al., 2019; Gonzales-Inca et al., 2022; Heo et al., 2021; Hou et al., 2022; Hystad et al., 2019; Kim & Kim, 2017; Klompmaker et al., 2019; Lee & Lee, 2019; Maas et al., 2009; McEachan et al., 2016; Min, Kim, Kim, & Min, 2017; Nazif-Munoz et al., 2020; Nichani et al., 2017; Nieuwenhuijsen et al., 2022; Nishigaki et al., 2020; Pelgrims et al., 2021; Peng et al., 2022; Pouso et al., 2021; Rugel et al., 2019; Sarkar et al., 2018; Song et al., 2019; Sun et al., 2023; Tomita et al., 2017; Triebner et al., 2022; Tsai et al., 2023; Van den Berg et al., 2016; White et al., 2021; Zayas-Costa et al., 2021; Zhang et al., 2022, p. 811; Zhang et al., 2023; Zhou et al., 2022), 14 on anxiety (Astell-Burt & Feng, 2019; Bustamante et al., 2022; Dzhambov et al., 2021; Generaal et al., 2019; Heo et al., 2021; Hystad et al., 2019; Klompmaker et al., 2019; Maas et al., 2009; Mouly, Mishra, Hystad, Nieuwenhuijsen, & Knibbs, 2023; Nutsford et al., 2013; Pelgrims et al., 2021; Pouso et al., 2021; Triebner et al., 2022; White et al., 2021), 8 on dementia (Astell-Burt et al., 2020, 2023, p. 145, p. 82; Klompmaker et al., 2022; Paul et al., 2020; Rodriguez-Loureiro et al., 2022; Slawsky et al., 2022; Wu et al., 2020; Yuchi et al., 2020), 7 on schizophrenia (Chang et al., 2020; Engemann et al., 2018, 2019, 2020a, 2020b, 2020c; Rotenberg et al., 2022), 5 on ADHD (Donovan et al., 2019; Markevych et al., 2014; Thygesen et al., 2020; Yang et al., 2019; Yuchi et al., 2022) (see Fig. 1).
Fig. 1.
Flow diagram of the study selection process.
3.2. Study characteristics
The basic characteristics of the 59 selected studies are shown in Table S1. A majority of studies published in the last decade have paid attention to on the correlation between green spaces and common psychiatric illness, indicating a growing interest in this research area. The contained studies were from 21 countries. Most of the research was performed in developed countries, with only eleven in developing countries. The sample sizes covered a wide range, from 322 to 61, 662, 472. Exposure to green spaces was judged by more than one objective or subjective geographic analysis units’ data in the vast majority of studies of psychiatric disorders. There were studies on view of green (n = 5) (Dzhambov et al., 2021; Pelgrims et al., 2021; Pouso et al., 2021; Rugel et al., 2019; Zhang et al., 2023), NDVI (n = 31) (Asri et al., 2021; Bezold et al., 2018a; 2018b; Donovan et al., 2019; Engemann et al., 2018, 2019, 2020a, 2020b, 2020c; Gonzales-Inca et al., 2022; Hystad et al., 2019; Klompmaker et al., 2019; Markevych et al., 2014; McEachan et al., 2016; Mouly, Mishra, Hystad, Nieuwenhuijsen, & Knibbs, 2023; Nazif-Munoz et al., 2020; Nieuwenhuijsen et al., 2022; Paul et al., 2020; Peng et al., 2022; Rodriguez-Loureiro et al., 2022; Slawsky et al., 2022; Song et al., 2019; Sun et al., 2023; Thygesen et al., 2020; Triebner et al., 2022; Yang et al., 2019; Yuchi et al., 2022; Zhang et al., 2022, p. 811; Yuchi et al., 2020; Tomita et al., 2017; Sarkar et al., 2018), area of green space (n = 27) (Asri et al., 2021; Astell-Burt et al., 2020, p. 145; Astell-Burt et al., 2023, p. 82; Chang et al., 2020; Engemann et al., 2020b; Engemann et al., 2020c; Gonzales-Inca et al., 2022; Hou et al., 2022; Generaal et al., 2019; Maas et al., 2009; Nieuwenhuijsen et al., 2022; Nishigaki et al., 2020; Nutsford et al., 2013; Rotenberg et al., 2022; Rugel et al., 2019; Pelgrims et al., 2021; Sun et al., 2023; Tsai et al., 2023; Wu et al., 2020; Zayas-Costa et al., 2021; Zhang et al., 2023; White et al., 2021; Zhou et al., 2022; Kim & Kim, 2017; Lee and Lee, 2019; Min et al., 2017; Nichani et al., 2017), green spaces accessibility (n = 4) (Nieuwenhuijsen et al., 2022; Rugel et al., 2019; Wu et al., 2020; Zayas-Costa et al., 2021), parks (n = 4) (Bustamante et al., 2022; Klompmaker et al., 2022; Sun et al., 2023; Zayas-Costa et al., 2021), other exposure index (n = 5) (Chang et al., 2020; Gonzales-Inca et al., 2022; Heo et al., 2021; Peng et al., 2022; Zhang et al., 2022, p. 811) and others (n = 2) (Bustamante et al., 2022; Nutsford et al., 2013). In addition, for gender in depression, there were studies on male (n = 2) (Hou et al., 2022; Hystad et al., 2019) and female (n = 11) (Dzhambov et al., 2021; Heo et al., 2021; Hou et al., 2022; Hystad et al., 2019; McEachan et al., 2016; Nazif-Munoz et al., 2020; Nichani et al., 2017; Sarkar et al., 2018; Sun et al., 2023; Triebner et al., 2022; Tsai et al., 2023). For region in depression, there were studies on urban (n = 13) (Astell-Burt & Feng, 2019; Bustamante et al., 2022; Gonzales-Inca et al., 2022; Maas et al., 2009; Nichani et al., 2017; Nishigaki et al., 2020; Pelgrims et al., 2021; Peng et al., 2022; Rugel et al., 2019; Song et al., 2019; Sun et al., 2023; Tomita et al., 2017; Zhou et al., 2022) and rural areas (n = 4) (Bustamante et al., 2022; Nishigaki et al., 2020; Peng et al., 2022; Tomita et al., 2017).
3.3. Findings about associations between green spaces and psychiatric disorders
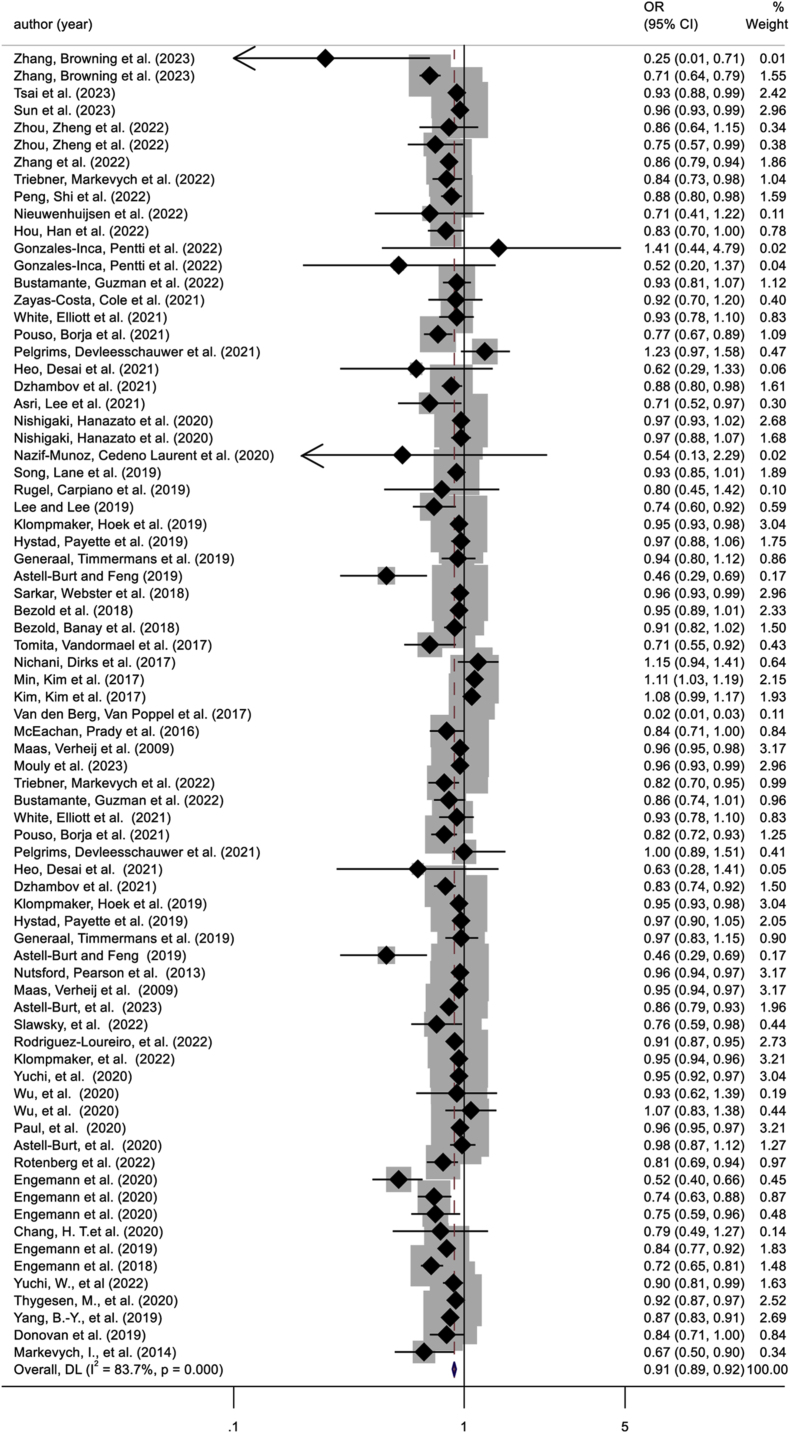
We collected data of psychiatric disorders which went through a series analysis. We firstly chose the fixed-effect model (I2 = 83.7%), but used the random-effect model for high heterogeneity at last. As Fig. 2 shows, generally, green spaces moderate the risk of having psychiatric disorders (OR = 0.91, 95% CI: 0.89 to 0.92). And then depression, anxiety, dementia, schizophrenia, and ADHD were performed to discover whether green spaces have diverse influences on each specific psychiatric disorder.
Fig. 2.
Forest plot of the studies of psychiatric disorders.
3.4. Studies of common psychiatric disorders
3.4.1. Exposure to green spaces and the risk of depression
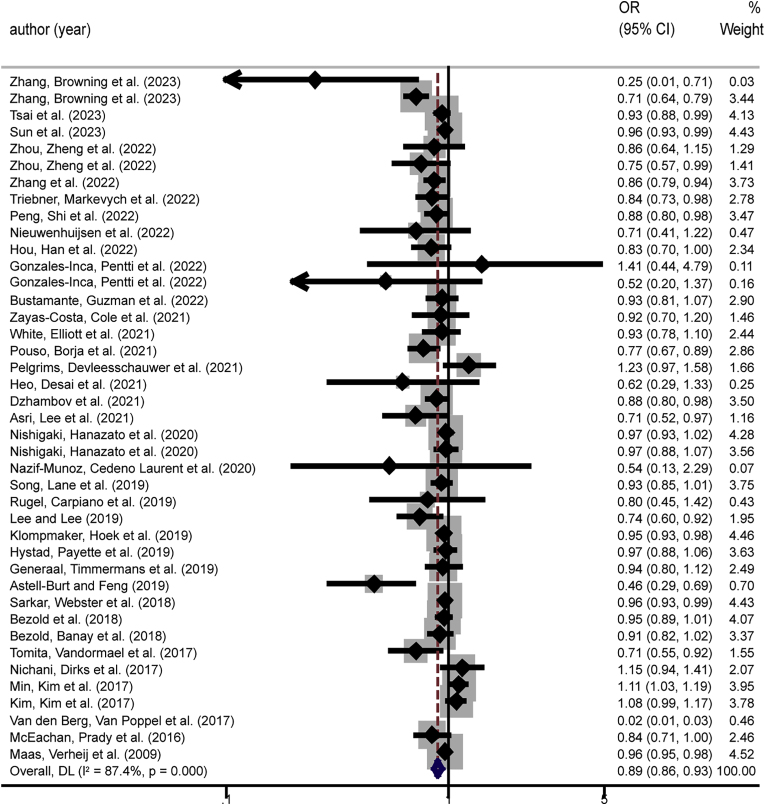
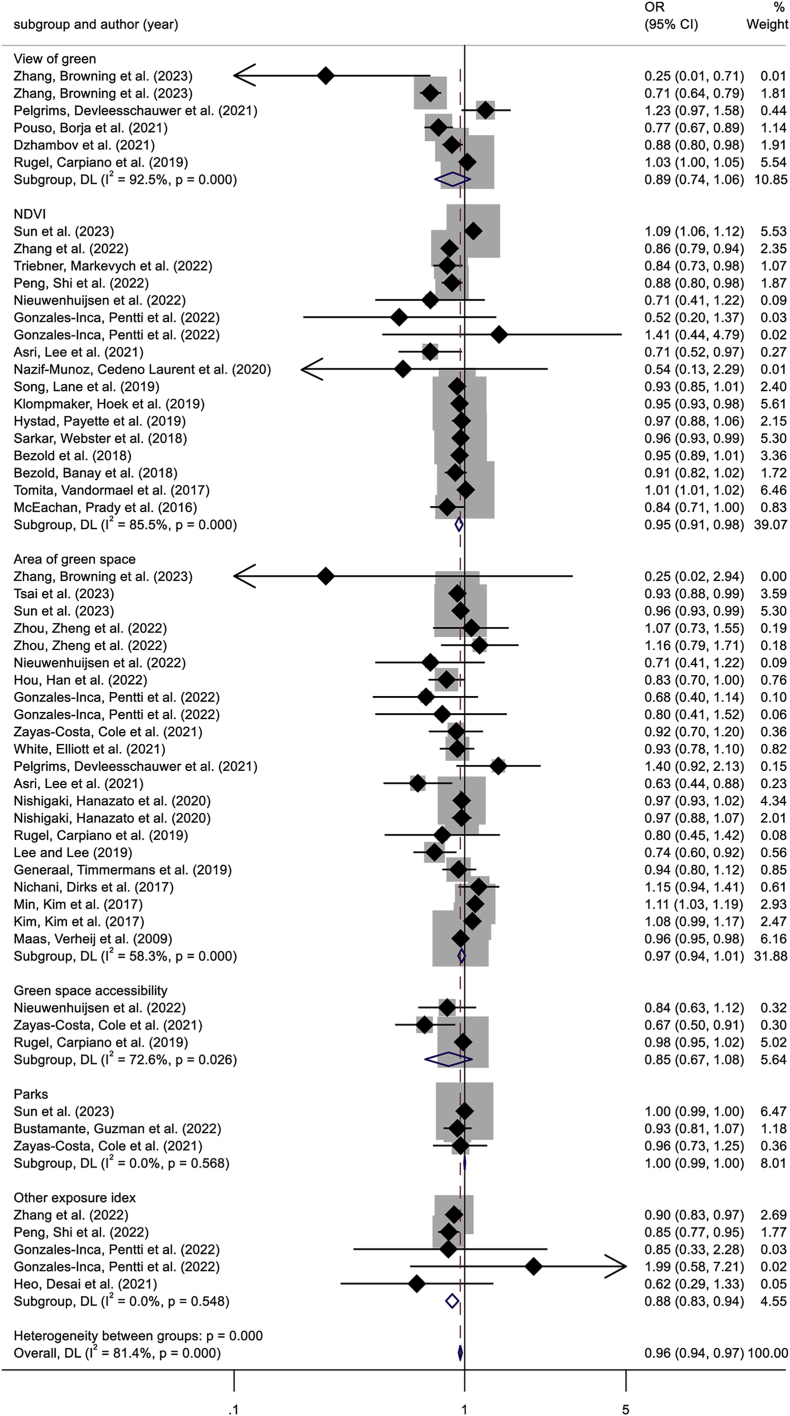
We used a fixed-effects model (I2 = 87.4%) at first and high heterogeneity was exhibited, so the random-effects model was finally employed. Judging by the overall findings of the analysis between green spaces and depression with the random effects model (I2 = 87.4%, p < 0.001), we demonstrated that green spaces alleviate the odds of depression (OR = 0.89, 95% CI: 0.86 to 0.93) (Fig. 3). Then we conducted subgroup analyses to further explore the correlation between them. Subgroups analysis revealed that the level of effect was related to certain factors, such as gender, region, and geographic analysis units (especially NDVI). Different study designs can also lead to variability in results.
Fig. 3.
Forest plot of the studies of depression.
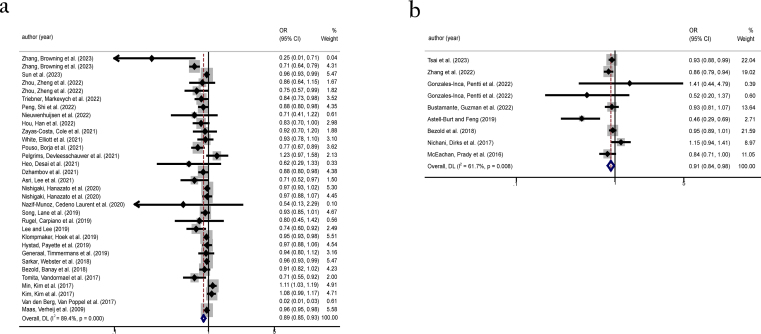
3.4.1.1. The relationship between green spaces and study method of depression
By analyzing cross-sectional studies, we demonstrated that green spaces are protective factors to depression (OR = 0.89, 95%CI:0.85 to 0.93). After employing the random effects model, heterogeneity was still substantial ( = 89.4%, p < 0.001) (Fig. S1a). The analysis of cohort studies also suggested that green spaces can mitigate the developing of depression (OR = 0.91, 95%CI:0.84 to 0.98). Substantial heterogeneity was also observed ( = 61.7%, p = 0.008) (Fig. S1b).
3.4.1.2. Various geographic analysis units show different connections with depression
The geographic analysis units were divided into view of green, NDVI, area of green space, green spaces accessibility, parks, and other exposure index. Most studies preferred to use area of green space (OR = 0.97, 95%CI:0.94 to 1.01) or NDVI (OR = 0.95, 95%CI:0.91 to 0.98) for measurement, and NDVI showed a higher correlation between green spaces and depression. Influences were also reflected in the subgroups of view of green (OR = 0.89, 95%CI:0.74 to 1.06) and green spaces accessibility (OR = 0.85, 95%CI:0.67 to 1.08), suggesting that the exposure to green spaces is positively related to depression (Fig. 4).
Fig. 4.
Subgroup analysis of different geographic units about depression.
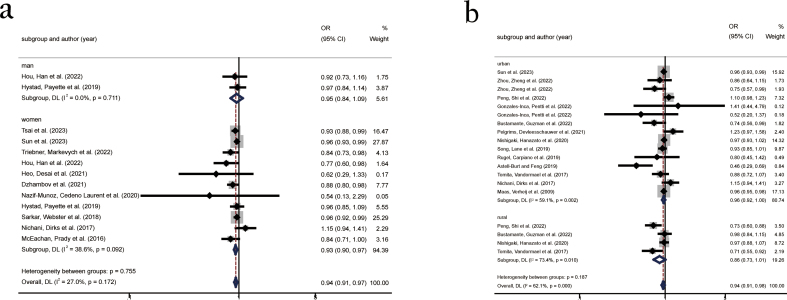
3.4.1.3. The association of gender difference and the risk of depression
Ten studies were classified into two groups: male and female. Two studies included data of both male and female, hence, they were included in both groups. Results indicated that the protective effects of green spaces on depression among male (OR = 0.95, 95%CI:0.84 to 1.09) were not as strong as that in female (OR = 0.93, 95%CI:0.90 to 0.97) (Fig. S2a).
3.4.1.4. The correlation between green spaces and depression in different regions
Thirteen studies were conducted research in urban areas (OR = 0.96, 95%CI:0.92 to 1.00) and four were conducted in rural areas (OR = 0.86, 95%:0.73 to 1.01) (Fig. S2b). The overall results were positive for both, but a higher OR was found for urban areas than rural areas.
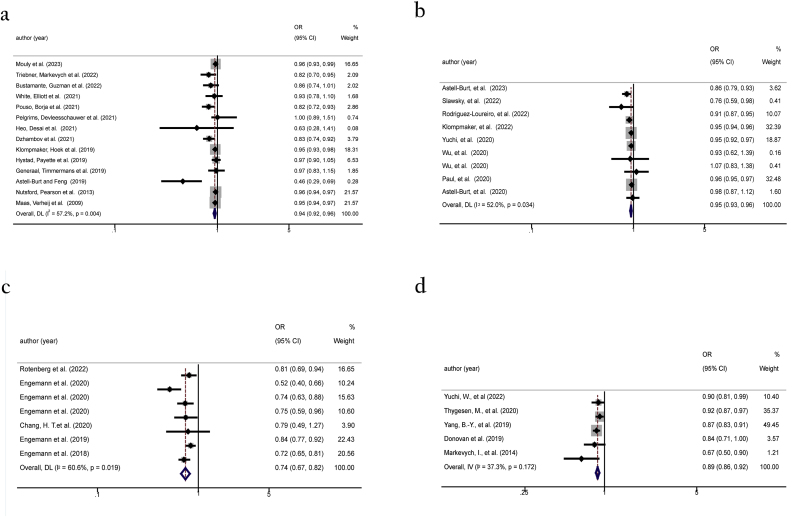
3.4.2. Exposure to green spaces and the risk of anxiety
We analyzed the association between green spaces and the odds of anxiety. The fixed-effects model (I2 = 57.2%) showed high heterogeneity, so the analysis of green spaces and anxiety was also presented in the random-effects model ( = 57.2%, p = 0.004) (Fig. 5a). Green spaces are discovered to alleviate the danger of anxiety (OR = 0.94, 95%CI:0.92 to 0.96) (Fig. 5a). Anxiety-related studies were stratified by geographic analysis units. Various geographic analysis units showed an insignificant relationship between green spaces and anxiety. However, in one of the geographic analysis units, the NDVI potentially played a significant role in the reduction of anxiety.
Fig. 5.
Forest plot of the studies of anxiety(a); Forest plot of the studies of dementia(b); Forest plot of the studies of schizophrenia (c); Forest plot of the studies of ADHD(d).
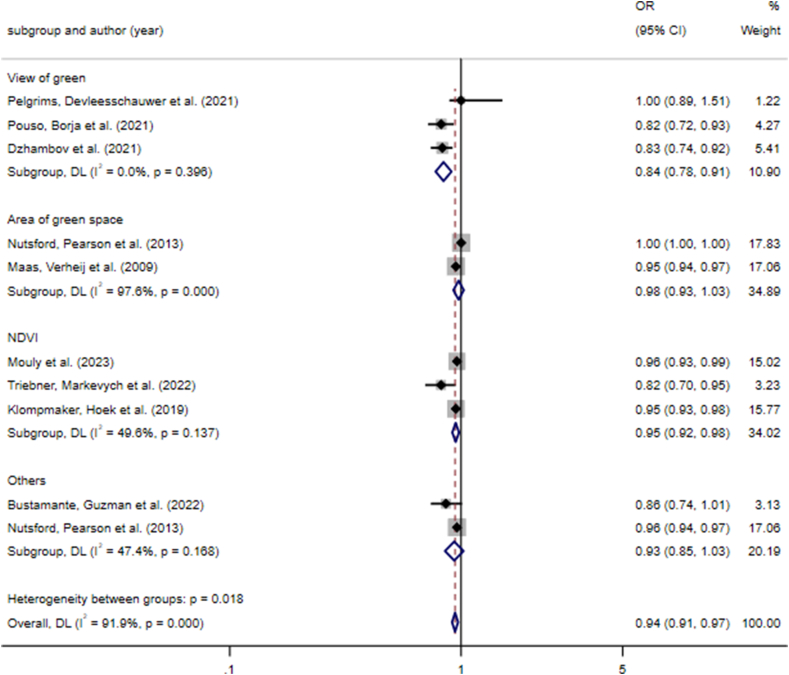
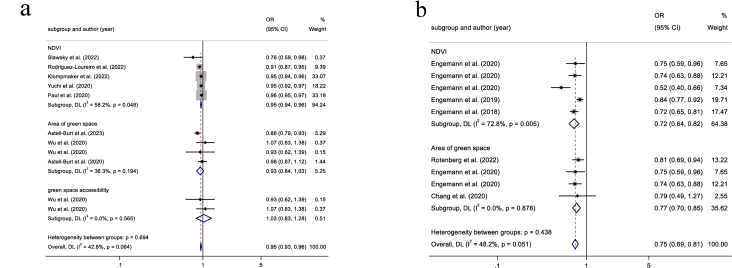
3.4.2.1. Various geographic analysis units show different connections with anxiety
For anxiety, geographic analysis units were divided into view of green, area of green space, NDVI and others. Among the last group, one was regarding the number of parks accessible to people and the other was regarding the distance to the nearest total green spaces. View of green (OR = 0.84, 95%CI:0.78 to 0.91), area of green space (OR = 0.98, 95%CI:0.93 to 1.03), NDVI (OR = 0.95, 95%:0.92 to 0.98), and others (OR = 0.93, 95%CI:0.85 to 1.03) completely supported the existing research conclusions (Fig. 6). Significant positive connections were revealed in all studies on NDVI.
Fig. 6.
Subgroup analysis of different geographic units about anxiety.
3.4.3. Exposure to green spaces and the risk of dementia
After analyzing the data from the eight existing relevant researches, we found green spaces can be a protective factor for dementia (OR = 0.95, 95% CI: 0.93 to 0.96). The fixed-effects model (I2 = 52.0%) was used initially, and we finally chose the random-effected model ( = 52.0%, p = 0.034) for significant heterogeneity (Fig. 5b).
3.4.3.1. Various geographic analysis units show different connections with dementia
For dementia, geographic analysis units were sorted into NDVI, and green space accessibility. Results of NDVI (OR = 0.95, 95% CI: 0.94 to 0.96) and area of green space (OR = 0.93, 95% CI: 0.84 to 1.03) showed consistency, but green space accessibility (OR = 1.03, 95% CI: 0.83 to 1.28) exhibited a variation (Fig. S3a).
3.4.4. Exposure to green spaces and the risk of schizophrenia and ADHD
We separately analyzed the relationship between exposure to green spaces and schizophrenia (OR = 0.74, 95% CI: 0.67 to 0.82) (Fig. 5c) and ADHD (OR = 0.89, 95% CI: 0.86 to 0.92) (Fig. 5d). The results of the above two mental diseases both supported exposure to green spaces was inversely associated with them. For schizophrenia, high heterogeneity (I2 = 52.0%) existed so we used the random-effects model ( = 60.6%, p = 0.019) to analyze. For ADHD, we just employed the fixed-effects model ( = 37.3%, p = 0.172) due to low heterogeneity.
Each article included in schizophrenia and ADHD supported their overall results, respectively. It was not controversially indicated green spaces played a beneficial role in schizophrenia and ADHD. But the insufficient number of studies make the results less persuasive.
3.4.4.1. Various geographic analysis units have different links to schizophrenia
For schizophrenia, geographic analysis units were categorized into NDVI (OR = 0.72, 95% CI: 0.64 to 0.82) and area of green space (OR = 0.77, 95% CI: 0.70 to 0.85), among which indicated the same direction (Fig. S3b).
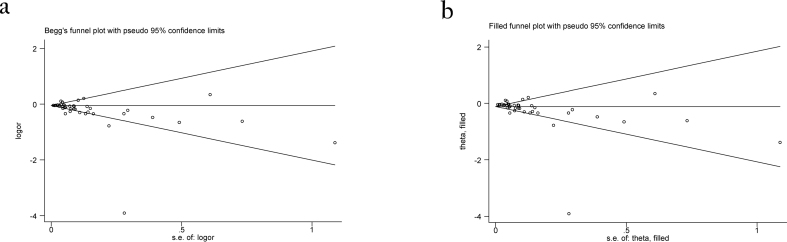
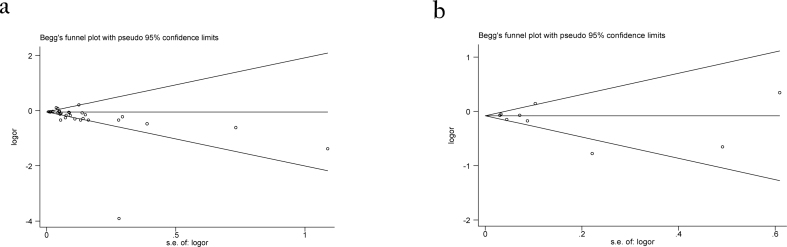
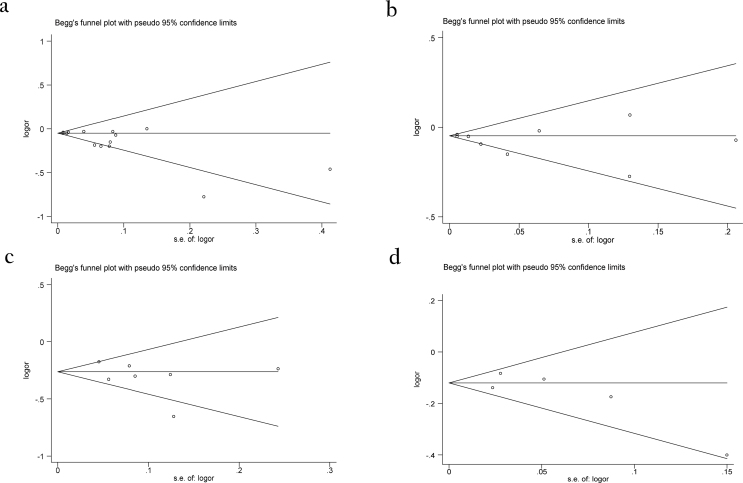
3.5. Publication bias
We use Begg's test to detect publication bias at first. Cohort studies of depression (p = 0.405) (Fig. S5b), dementia (p = 0.197) (Fig. S6b), schizophrenia (p = 0.267) (Fig. S6c) and ADHD (p = 0.312) (Fig. S6d) did not show publication bias, while anxiety (p = 0.01) (Fig. S6a), depression (p = 0.006) (Fig. S4a) and cross-sectional studies of depression (p = 0.015) (Fig. S5a) both had p-scores of less than 0.05 which were subject to publication bias. So, we conducted the trim-and-fill to examine the reliability of the results and found the outcomes of anxiety (OR = 2.56, 95%CI: 2.50 to 2.62) (Fig. S7b), depression (OR = 2.44, 95%CI: 2.36 to 2.53) (Fig. S4b) and cross-sectional studies of depression (OR = 2.43, 95%CI: 2.34 to 2.53) (Fig. S7a) with green spaces did not change.
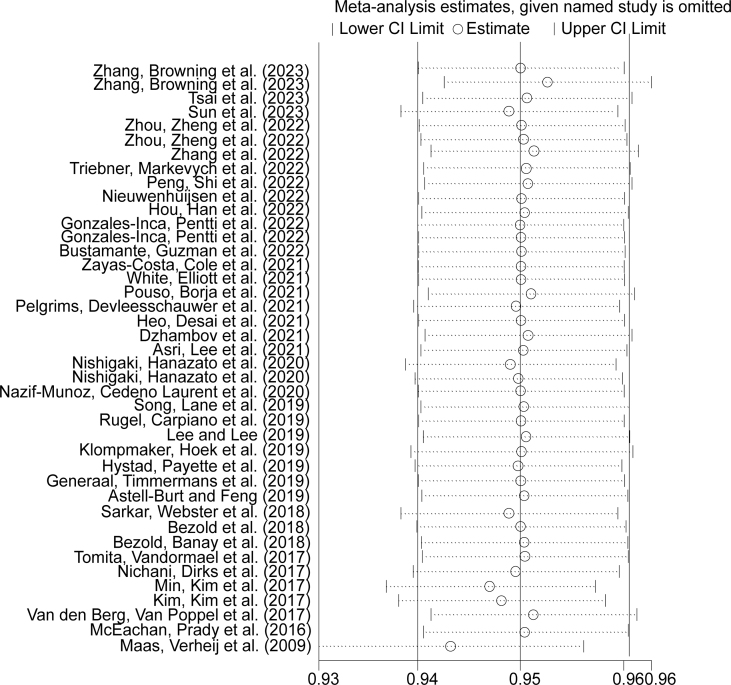
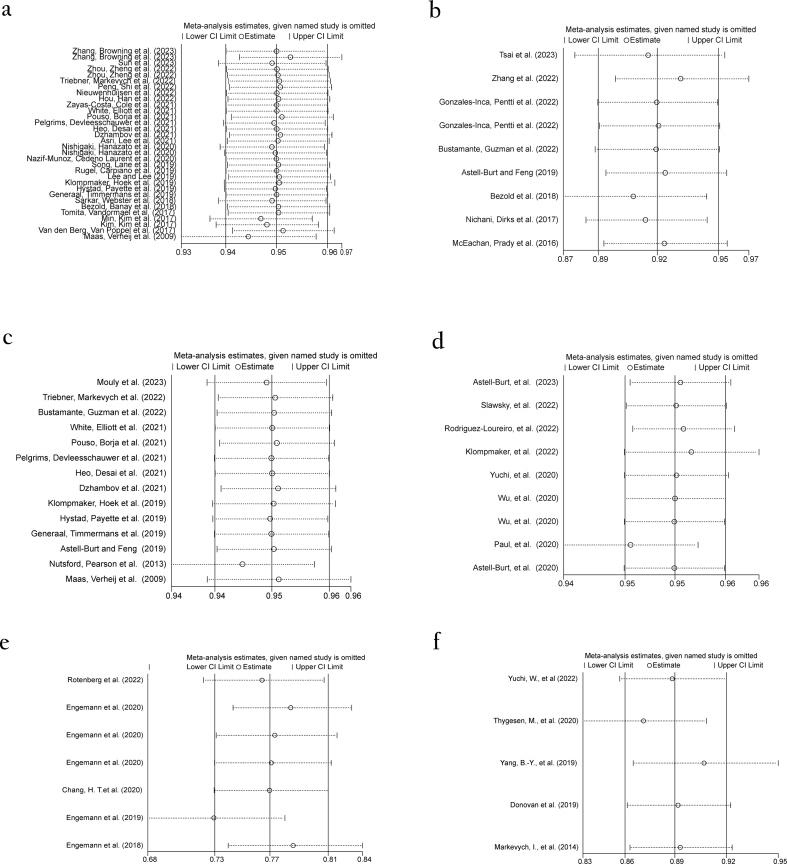
3.6. Sensitivity analysis
We chose “leave-one-out” method to conduct sensitivity analysis of depression (Fig. S8), cross-sectional studies in depression, cohort studies in depression, anxiety, dementia, schizophrenia, and ADHD (Fig. S9). No obvious changes of outcomes between green spaces and psychiatric disorders were observed after omitting any single study.
4. Discussion
Using 59 studies, the meta-analysis analyzed the existing scientific evidence to determine whether green spaces can alleviate psychiatric disorders. We confirmed that positive influences can be found between green spaces and psychiatric disorders. Referring to subgroups analysis, the results were more pronounced for the NDVI.
Regarding depression, it was interesting to find that the difference in results between male and female may be attributed to the fact that female had considerably poorer mental health outcomes for depression than male (Kim & Kim, 2017). Moreover, we noticed that effects of greenness exposure on depression during and after pregnancy appeared to be different. A decreased risk of depression during pregnancy was correlated to NDVI (McEachan et al., 2016). Previous studies have confirmed that depression is more common in urban environments (Blazer et al., 1985), and the factors influencing the effect of urban green spaces on depression are complex (Lauwers et al., 2021). Some studies showed plentiful trees in urban region as well as suitable numbers of grassland in rural region were both related to the decreased probability of depression (Nishigaki et al., 2020). Additionally, Cross-sectional and cohort studies of depression showed differences on data. The diversity came from the difference in quantity or time span. At a 5-years follow-up, scientists discovered a great correlation between green spaces and depression but less association over a 14-year period (Gonzales-Inca et al., 2022). This indicates that the follow-up duration also affected the results.
Although the general association between green spaces and anxiety is not as strong as that between green spaces and depression, a protective effect can still be revealed. Associating green spaces with anxiety may be related to green spaces in the neighborhood or within walking distance of a home (Nutsford et al., 2013). One reason suggested from Astell-Burt et al. is that greenness may provide people chances to recover from tiredness and promote the interpersonal communication. Additionally, biodiversity may also have beneficial effects (Astell-Burt & Feng, 2019).
Consistent with some of the existing results (Astell-Burt et al., 2020, p. 145; Paul et al., 2020; Rodriguez-Loureiro et al., 2022), our results generally indicated positive correlation between the exposure of greenness and dementia. But it should be noted that in some studies, moderate levels of green spaces reduce the risk of dementia to a greater extent than other levels (Slawsky et al., 2022). And there are also related studies that have been proposed high available green spaces was not associated with low dementia (Wu et al., 2020). About schizophrenia, scientists demonstrated that residing in more greenness correlated with a decreased odd of developing schizophrenia. Green space exposure during childhood is associated with schizophrenia risk on a dose-response basis (Engemann et al., 2018). Then more in-depth researches from Engemann et al. were conduct and found that gene did not disturb the association between green spaces and schizophrenia (Engemann et al., 2020a). Furthermore, higher vegetation density had been revealed associated with lower danger of schizophrenia in urban (Engemann et al., 2020c). Articles of ADHD also supported that increased hyperactivity problems were related with less green spaces. And the growth of exposure to minimum green spaces of children appeared to offer the maximum protection (Donovan et al., 2019). Notely, researches from Markevych et al. pointed out that based on sex stratification, only men exhibited statistically significant associations with ADHD (Markevych et al., 2014). However, limited articles cannot fully substantiate the benefits of green spaces to schizophrenia and ADHD, and a better knowledge of the role of greenness factors in reducing them requires more studies.
Heterogeneity was exhibited in studies of depression, anxiety, dementia, and schizophrenia. This may lead to the effect of high heterogeneity on the statistical power of meta-analysis, as well as the reliability and direction of the summary effect. There are differences in the measurement methods, sample sizes, types of green spaces, and sample characteristics (like age, gender) in studies. We can also speculate from subgroups analysis that studies design and geographic analysis units can be major sources of high heterogeneity, among which cross-sectional studies, view of green, NDVI, green space accessibility showed instability. This may because the way to view of green various, and NDVI were divided into a wide range of buffers and radius, and green spaces accessibility including distance or accessibility. We attempted to use the buffer radius for grouping but did not find a suitable classification method. Thus, the scattered distributions of different buffer radii were arranged in the existing subgroups. Some scientists estimated a buffer radius of 100 m around individuals’ homes and found no significant associations (Gonzales-Inca et al., 2022). This indicates that different buffer radii may have different effects on depression, which is expected to broaden the range of tacks in the future. Besides, difference in region can also be one of the reasons. Studies of ADHD were not classified into subgroups as they only assess green by NDVI.
When exploring the relationship between green spaces and psychiatric disorders, scientists are also trying to explore the relevant mechanisms behind it. The mainstream claim that green spaces alleviate psychiatric disorders by reducing the exposure to environmental air pollution (Bloemsma et al., 2022; Triebner et al., 2022). Green spaces can decrease PM10 in the air remarkably and minimize exposure to PM2.5 and NO2 in pregnant women (Nieuwenhuijsen et al., 2017). One study from Thygesen et al. revealed that areas with more green spaces tend to have less pollution, which may benefit from the filtration deposition of plants (Thygesen et al., 2020). The same assertion is reflected in some of other articles. What's more, Bloemsma et al. said that the differentiation of mental health between urban and rural areas is also possible to provide an explanation (Bloemsma et al., 2022). This is also consistent with the results of the regional subgroup analysis of depression in our article, which can provide ideas for the future targeted construction of urban and rural health. There are also a number of studies demonstrated noise reduction may also contribute to the outcomes (Thygesen et al., 2020; Yang et al., 2019). Green spaces can play a role as a “wall”, which can minimize noise by diffraction, absorption, or destructive interference of sound waves (Van Renterghem et al., 2015). Some studies provided evidence that physical exercise, diabetes, social support and psychiatric distress may be the mediators (Astell-Burt et al., 2023, p. 82). Among these factors, stress, and social cohesion influence the outcomes primarily (De Vries, Van Dillen, Groenewegen, & Spreeuwenberg, 2013). However, many studies have not yet found a clear link. Learning from a related meta-analysis for dementia, they indicated a non-linear relationship between green spaces and dementia, but potential mechanisms could not be found due to the limitations (Zagnoli et al., 2022). Rotenberg et al. said the cause of schizophrenic symptoms may be influenced by environment but the mechanism remains unclear (Rotenberg et al., 2022). Exploration in the mechanism is still much needed in the future.
Through the analysis of the above five common psychiatric disorders, we suggested that people can promote the development of public health by improving green space facilities in the future, and through our research, green space construction is more important in the urban environment, which provides ideas for the development of urbanization in the future. There are already many approaches or policy internationally to promote the development of green spaces in cities. In Denmark, approximately one quarter of health policies include references to the significance of promoting the utilization of green spaces (Schipperijn et al., 2010). A pattern named 3-30-300 green space rule is recommended, which requires that every citizen should be able to see at least three trees from their home, have 30 percent tree canopy cover in their neighborhood and not live more than 300 m away from the nearest park or green space (Nieuwenhuijsen et al., 2022). Small Public Urban Green Spaces (SPUGS) is also a promoted form of green spaces in cities (Peschardt et al., 2012). Some cities also built pocket park (Dong, Guo, Guo, & Cai, 2024). As the scarcity of urban land, green spaces of small scale demonstrate its potential. The development of green spaces still present challenges. We can draw from experience and look forward to more innovation and progress. Furthermore, we should continue striving to address inequality of urban green space (UGS) distribution (Wu & Kim, 2021) and environmental injustice (Wolch et al., 2014), thereby enabling the green space to better realize its benefits. Economic development will be a positive factor, and it is significant to prioritize not only the quantity but also the quality of green spaces (Wu & Kim, 2021).
Our meta-analysis holds some strengths as follows. First, we use extensive search string for the outcomes, and we conducted the exploration on four big databases, thus, this can provide a large sample source for our study. Second, our study consisted of five common psychiatric disorders. We started with an overview of all the diseases, and then analyze each disease individually, which providing a more comprehensive view on psychiatry. Thirdly, subgroups were employed in certain diseases, which demonstrate different influencing factors in detail. Admittedly, we also had many limitations and a wide space to improve the quality and rigor. Insufficient research has constrained our exploration of factors which may also have effect, like ethnicity, age, etc. We cannot adequately eliminate the interference caused by factors such as sample size, age, and geographic location. Besides, the mechanisms of some psychiatric disorders are still needed more in-depth discussion. The limited articles of schizophrenia and ADHD make our results less convincing. And our meta-analysis did not include grey literature, and involved studies in English only. When including studies, we did not strictly limit participant characteristics. The included articles encompassed studies targeting elderly individuals as well as studies focusing on pregnant women. These can all lead to bias.
5. Conclusion
Our meta-analysis revealed that green space is linked to lower odds of depression, anxiety, dementia, schizophrenia, and ADHD. Women and rural areas may benefit more from it. A high NDVI could be the major impact factor. Our meta-analysis encourages the local authorities and policymakers to attach greater importance to green infrastructure construction and urges the public to spend more time enjoying greenery. In the future, further studies are expected to explore the roles of gender, geographical locations, ethnicity, quality of greenness, potential mechanisms, as well as specific investigations into dementia, schizophrenia, and ADHD.
Ethical statement
I certify that this manuscript is original and has not been published and will not be submitted elsewhere for publication while being considered by SSM - Population Health. And the study is not split up into several parts to increase the quantity of submissions and submitted to various journals or to one journal over time. No data have been fabricated or manipulated (including images) to support your conclusions. No data, text, or theories by others are presented as if they were our own.
The submission has been received explicitly from all co-authors. And authors whose names appear on the submission have contributed sufficiently to the scientific work and therefore share collective responsibility and accountability for the results.
CRediT authorship contribution statement
Yimin Zhang: Writing – original draft, Software, Investigation. Tongyan Wu: Writing – original draft, Validation, Formal analysis. Hao Yu: Writing – review & editing, Validation, Methodology. Jianfei Fu: Software, Funding acquisition, Conceptualization. Jin Xu: Supervision, Conceptualization. Liya Liu: Validation, Supervision. Chunlan Tang: Writing – review & editing, Validation. Zhen Li: Writing – review & editing, Supervision, Project administration.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
This work was supported by the National Natural Science Foundation of China (grant numbers 81703189); Ningbo Natural Science Foundation (grant numbers 2018A610237 and 202003N4113); Natural Science Foundation of Zhejiang Province (grant numbers LY21B070002 and ZCLY24H2601); and the KC Wong Magna Fund of Ningbo University.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ssmph.2024.101630.
Appendix A. Supplementary data
The following are the Supplementary data to this article.
figs1.
Forest plot of the cross-sectional studies (a) and cohort studies (b) of depression.
figs2.
Subgroup analysis on studies for depression adjusted for gender (a) and region (b).
figs3.
Subgroups analysis on studies for dementia and schizophrenia adjusted for various geographic analysis units.
figs4.
Funnel plot for the studies of depression (a); publication bias of studies about depression (trimmed and filled funnel plot) (b).
figs5.
Funnel plot for the cross-sectional studies of depression (a); Funnel plot for the cohort studies of depression (b).
figs6.
Funnel plot for the studies of anxiety (a); Funnel plot for the studies of dementia (b); Funnel plot for the studies of schizophrenia (c); Funnel plot for the studies of ADHD (d).
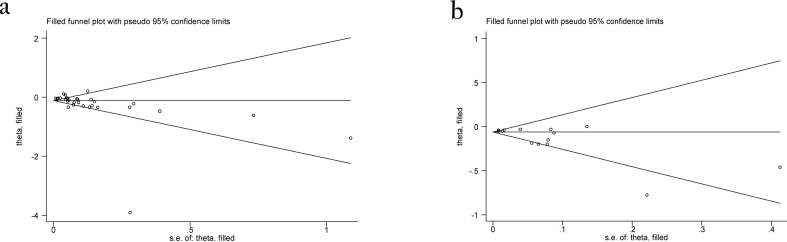
figs7.
Publication bias of cross-sectional studies about depression (trimmed and filled funnel plot) (a); Publication bias of studies about anxiety (trimmed and filled funnel plot) (b).
figs8.
Sensitivity analysis of studies about depression.
figs9.
Sensitivity analysis of studies about cross-sectional studies (a) and cohort studies of depression (b), anxiety (c), dementia (d), schizophrenia (e) and ADHD (f).
Data availability
Data will be made available on request.
References
- Asri A.K., Lee H.Y., Pan W.C., Tsai H.J., Chang H.T., Lung S.C.C., et al. Is green space exposure beneficial in a developing country? Landscape and Urban Planning. 2021;215 [Google Scholar]
- Astell-Burt T., Feng X.Q. Association of urban green space with mental health and general health among adults in Australia. JAMA Network Open. 2019;2 doi: 10.1001/jamanetworkopen.2019.8209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Astell-Burt T., Navakatikyan M.A., Feng X.Q. Urban green space, tree canopy and 11-year risk of dementia in a cohort of 109,688 Australians. Environment International. 2020;145 doi: 10.1016/j.envint.2020.106102. [DOI] [PubMed] [Google Scholar]
- Astell-Burt T., Navakatikyan M.A., Feng X.Q. Why might urban tree canopy reduce dementia risk? A causal mediation analysis of 109,688 adults with 11 years of hospital and mortality records. Health & Place. 2023;82 doi: 10.1016/j.healthplace.2023.103028. [DOI] [PubMed] [Google Scholar]
- Begg C.B., Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50:1088–1101. [PubMed] [Google Scholar]
- Bezold C.P., Banay R.F., Coull B.A., Hart J.E., James P., Kubzansky L.D., et al. The association between natural environments and depressive symptoms in adolescents living in the United States. Journal of Adolescent Health. 2018;62:488–495. doi: 10.1016/j.jadohealth.2017.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bezold C.P., Banay R.F., Coull B.A., Hart J.E., James P., Kubzansky L.D., et al. The relationship between surrounding greenness in childhood and adolescence and depressive symptoms in adolescence and early adulthood. Annals of Epidemiology. 2018;28:213–219. doi: 10.1016/j.annepidem.2018.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blazer D., George L.K., Landerman R., Pennybacker M., Melville M.L., Woodbury M., et al. Psychiatric disorders. A rural/urban comparison. Archives of General Psychiatry. 1985;42:651–656. doi: 10.1001/archpsyc.1985.01790300013002. [DOI] [PubMed] [Google Scholar]
- Bloemsma L.D., Wijga A.H., Klompmaker J.O., Hoek G., Janssen N.A.H., Lebret E., et al. Green space, air pollution, traffic noise and mental wellbeing throughout adolescence: Findings from the PIAMA study. Environment International. 2022;163 doi: 10.1016/j.envint.2022.107197. [DOI] [PubMed] [Google Scholar]
- Bustamante G., Guzman V., Kobayashi L.C., Finlay J. Mental health and well-being in times of COVID-19: A mixed-methods study of the role of neighborhood parks, outdoor spaces, and nature among US older adults. Health & Place. 2022;76 doi: 10.1016/j.healthplace.2022.102813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campeau A., Mills R.H., Stevens T., Rossitto L.A., Meehan M., Dorrestein P., et al. Multi-omics of human plasma reveals molecular features of dysregulated inflammation and accelerated aging in schizophrenia. Molecular Psychiatry. 2022;27:1217–1225. doi: 10.1038/s41380-021-01339-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang H.T., Wu C.D., Wang J.D., Chen P.S., Wang Y.J., Su H.J. Green space structures and schizophrenia incidence in Taiwan: Is there an association? Environmental Research Letters. 2020;15 [Google Scholar]
- De Vries S., Van Dillen S.M., Groenewegen P.P., Spreeuwenberg P. Streetscape greenery and health: Stress, social cohesion and physical activity as mediators. Social Science & Medicine. 2013;94:26–33. doi: 10.1016/j.socscimed.2013.06.030. [DOI] [PubMed] [Google Scholar]
- Donovan G.H., Michael Y.L., Gatziolis D., Mannetje A., Douwes J. Association between exposure to the natural environment, rurality, and attention-deficit hyperactivity disorder in children in New Zealand: A linkage study. The lancet. Planetary health. 2019;3:e226–e234. doi: 10.1016/S2542-5196(19)30070-1. [DOI] [PubMed] [Google Scholar]
- Dong J., Guo R., Guo F., Cai J. Potential evaluation and implementation strategy for pocket park construction in high-density urban areas: A case study in dalian, China. Frontiers of Architectural Research. 2024 In press. [Google Scholar]
- Drechsler R., Brem S., Brandeis D., Grünblatt E., Berger G., Walitza S. Adhd: Current concepts and treatments in children and adolescents. Neuropediatrics. 2020;51:315–335. doi: 10.1055/s-0040-1701658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duval S., Tweedie R. Trim and fill: A simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics. 2000;56:455–463. doi: 10.1111/j.0006-341x.2000.00455.x. [DOI] [PubMed] [Google Scholar]
- Dzhambov A.M., Lercher P., Browning M.H.E.M., Stoyanov D., Petrova N., Novakov S., et al. Does greenery experienced indoors and outdoors provide an escape and support mental health during the COVID-19 quarantine? Environmental Research. 2021;196 doi: 10.1016/j.envres.2020.110420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Engemann K., Pedersen C.B., Agerbo E., Arge L., Borglum A.D., Erikstrup C., et al. Association between childhood green space, genetic liability, and the incidence of schizophrenia. Schizophrenia Bulletin. 2020;46:1629–1637. doi: 10.1093/schbul/sbaa058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Engemann K., Pedersen C.B., Arge L., Tsirogiannis C., Mortensen P.B., Svenning J.C. Childhood exposure to green space – A novel risk-decreasing mechanism for schizophrenia? Schizophrenia Research. 2018;199:142–148. doi: 10.1016/j.schres.2018.03.026. [DOI] [PubMed] [Google Scholar]
- Engemann K., Pedersen C.B., Arge L., Tsirogiannis C., Mortensen P.B., Svenning J.C. Residential green space in childhood is associated with lower risk of psychiatric disorders from adolescence into adulthood. Proceedings of the National Academy of Sciences of the United States of America. 2019;116:5188–5193. doi: 10.1073/pnas.1807504116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Engemann K., Svenning J.C., Arge L., Brandt J., Erikstrup C., Geels C., et al. Associations between growing up in natural environments and subsequent psychiatric disorders in Denmark. Environmental Research. 2020;188 doi: 10.1016/j.envres.2020.109788. 109788. [DOI] [PubMed] [Google Scholar]
- Engemann K., Svenning J.C., Arge L., Brandt J., Geels C., Mortensen P.B., et al. Natural surroundings in childhood are associated with lower schizophrenia rates. Schizophrenia Research. 2020;216:488–495. doi: 10.1016/j.schres.2019.10.012. [DOI] [PubMed] [Google Scholar]
- Feng X., Toms R., Astell-Burt T. The nexus between urban green space, housing type, and mental health. Social Psychiatry and Psychiatric Epidemiology. 2022;57:1917–1923. doi: 10.1007/s00127-022-02266-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Generaal E., Timmermans E.J., Dekkers J.E.C., Smit J.H., Penninx B.W.J.H. Not urbanization level but socioeconomic, physical and social neighbourhood characteristics are associated with presence and severity of depressive and anxiety disorders. Psychological Medicine. 2019;49:149–161. doi: 10.1017/S0033291718000612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzales-Inca C., Pentti J., Stenholm S., Suominen S., Vahtera J., Käyhkö N. Residential greenness and risks of depression: Longitudinal associations with different greenness indicators and spatial scales in a Finnish population cohort. Health & Place. 2022;74 doi: 10.1016/j.healthplace.2022.102760. [DOI] [PubMed] [Google Scholar]
- Heo S., Desai M.U., Lowe S.R., Bell M.L. Impact of changed use of greenspace during COVID-19 pandemic on depression and anxiety. International Journal of Environmental Research and Public Health. 2021;18:5842. doi: 10.3390/ijerph18115842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hou F., Han X., Wang Q., Zhou S., Zhang J., Shen G., et al. Cross-sectional associations between living and built environments and depression symptoms among Chinese older adults. International Journal of Environmental Research and Public Health. 2022;19:5819. doi: 10.3390/ijerph19105819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hystad P., Payette Y., Noisel N., Boileau C. Green space associations with mental health and cognitive function: Results from the Quebec CARTaGENE cohort. Environmental Epidemiology. 2019;3 doi: 10.1097/EE9.0000000000000040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kavelaars R., Ward H., Mackie D.S., Modi K.M., Mohandas A. The burden of anxiety among a nationally representative US adult population. Journal of Affective Disorders. 2023;336:81–91. doi: 10.1016/j.jad.2023.04.069. [DOI] [PubMed] [Google Scholar]
- Kim J., Kim H. Demographic and environmental factors associated with mental health: A cross-sectional study. International Journal of Environmental Research and Public Health. 2017;14:431. doi: 10.3390/ijerph14040431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klompmaker J.O., Hoek G., Bloemsma L.D., Wijga A.H., van den Brink C., Brunekreef B., et al. Associations of combined exposures to surrounding green, air pollution and traffic noise on mental health. Environment International. 2019;129:525–537. doi: 10.1016/j.envint.2019.05.040. [DOI] [PubMed] [Google Scholar]
- Klompmaker J.O., Laden F., Browning M.H.E.M., Dominici F., Jimenez M.P., Ogletree S.S., et al. Associations of greenness, parks, and blue space with neurodegenerative disease hospitalizations among older US adults. JAMA Network Open. 2022;5 doi: 10.1001/jamanetworkopen.2022.47664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lauwers L., Leone M., Guyot M., Pelgrims I., Remmen R., Van den Broeck K., et al. Exploring how the urban neighborhood environment influences mental well-being using walking interviews. Health & Place. 2021;67 doi: 10.1016/j.healthplace.2020.102497. [DOI] [PubMed] [Google Scholar]
- Lee H.J., Lee D.K. Do sociodemographic factors and urban green space affect mental health outcomes among the urban elderly population? International Journal of Environmental Research and Public Health. 2019;16:789. doi: 10.3390/ijerph16050789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Z., Chen X., Cui H., Ma Y., Gao N., Li X., et al. Green space exposure on depression and anxiety outcomes: A meta-analysis. Environmental Research. 2023;231 doi: 10.1016/j.envres.2023.116303. [DOI] [PubMed] [Google Scholar]
- Lumber R., Richardson M., Sheffield D. Beyond knowing nature: Contact, emotion, compassion, meaning, and beauty are pathways to nature connection. PLoS One. 2017;12 doi: 10.1371/journal.pone.0177186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maas J., Verheij R.A., de Vries S., Spreeuwenberg P., Schellevis F.G., Groenewegen P.P. Morbidity is related to a green living environment. Journal of Epidemiology & Community Health. 2009;63:967–973. doi: 10.1136/jech.2008.079038. [DOI] [PubMed] [Google Scholar]
- Margulis A.V., Pladevall M., Riera-Guardia N., Varas-Lorenzo C., Hazell L., Berkman N.D., et al. Quality assessment of observational studies in a drug-safety systematic review, comparison of two tools: The newcastle-ottawa scale and the RTI item bank. Clinical Epidemiology. 2014;6:359–368. doi: 10.2147/CLEP.S66677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Markevych I., Tiesler C.M.T., Fuertes E., Romanos M., Dadvand P., Nieuwenhuijsen M.J., et al. Access to urban green spaces and behavioural problems in children: Results from the GINIplus and LISAplus studies. Environment International. 2014;71:29–35. doi: 10.1016/j.envint.2014.06.002. [DOI] [PubMed] [Google Scholar]
- Marshall M. The hidden links between mental disorders. Nature. 2020;581:19–21. doi: 10.1038/d41586-020-00922-8. [DOI] [PubMed] [Google Scholar]
- McEachan R.R., Prady S.L., Smith G., Fairley L., Cabieses B., Gidlow C., et al. The association between green space and depressive symptoms in pregnant women: Moderating roles of socioeconomic status and physical activity. Journal of Epidemiology & Community Health. 2016;70:253–259. doi: 10.1136/jech-2015-205954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Min K.B., Kim H.J., Kim H.J., Min J.Y. Parks and green areas and the risk for depression and suicidal indicators. International Journal of Public Health. 2017;62:647–656. doi: 10.1007/s00038-017-0958-5. [DOI] [PubMed] [Google Scholar]
- Mouly T.A., Mishra G.D., Hystad P., Nieuwenhuijsen M., Knibbs L.D. Residential greenspace and anxiety symptoms among Australian women living in major cities: A longitudinal analysis. Environment International. 2023;179 doi: 10.1016/j.envint.2023.108110. [DOI] [PubMed] [Google Scholar]
- Mukherjee D., Safraj S., Tayyab M., Shivashankar R., Patel S.A., Narayanan G., et al. Park availability and major depression in individuals with chronic conditions: Is there an association in urban India? Health & Place. 2017;47:54–62. doi: 10.1016/j.healthplace.2017.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nazif-Munoz J.I., Laurent J.G.C., Browning M., Spengler J., Alvarez H.A.O. Green, Brown, and gray: Associations between different measurements of land patterns and depression among nursing students in el paso, Texas. International Journal of Environmental Research and Public Health. 2020;17:8146. doi: 10.3390/ijerph17218146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nichani V., Dirks K., Burns B., Bird A., Grant C. Green space and depression during pregnancy: Results from the growing Up in New Zealand study. International Journal of Environmental Research and Public Health. 2017;14:1083. doi: 10.3390/ijerph14091083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nieuwenhuijsen M.J., Dadvand P., Márquez S., Bartoll X., Barboza E.P., Cirach M., et al. The evaluation of the 3-30-300 green space rule and mental health. Environmental Research. 2022;215 doi: 10.1016/j.envres.2022.114387. [DOI] [PubMed] [Google Scholar]
- Nieuwenhuijsen M.J., Khreis H., Triguero-Mas M., Gascon M., Dadvand P. Fifty shades of green: Pathway to healthy urban living. Epidemiology. 2017;28:63–71. doi: 10.1097/EDE.0000000000000549. [DOI] [PubMed] [Google Scholar]
- Nishigaki M., Hanazato M., Koga C., Kondo K. What types of greenspaces are associated with depression in urban and rural older adults? A multilevel cross-sectional study from jages. International Journal of Environmental Research and Public Health. 2020;17 doi: 10.3390/ijerph17249276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nutsford D., Pearson A.L., Kingham S. An ecological study investigating the association between access to urban green space and mental health. Public Health. 2013;127:1005–1011. doi: 10.1016/j.puhe.2013.08.016. [DOI] [PubMed] [Google Scholar]
- Papalia G.F., Petrucci G., Russo F., Ambrosio L., Vadalà G., Iavicoli S., et al. COVID-19 pandemic increases the impact of low back pain: A systematic review and metanalysis. International Journal of Environmental Research and Public Health. 2022;19:4599. doi: 10.3390/ijerph19084599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paul L.A., Hystad P., Burnett R.T., Kwong J.C., Crouse D.L., van Donkelaar A., et al. Urban green space and the risks of dementia and stroke. Environmental Research. 2020;186 doi: 10.1016/j.envres.2020.109520. [DOI] [PubMed] [Google Scholar]
- Pelgrims I., Devleesschauwer B., Guyot M., Keune H., Nawrot T.S., Remmen R., et al. Association between urban environment and mental health in Brussels, Belgium. BMC Public Health. 2021;21:635. doi: 10.1186/s12889-021-10557-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peng W., Shi H., Li M., Li X., Liu T., Wang Y. Association of residential greenness with geriatric depression among the elderly covered by long-term care insurance in Shanghai. Environmental Science and Pollution Research International. 2022;29:12054–12064. doi: 10.1007/s11356-021-16585-5. [DOI] [PubMed] [Google Scholar]
- Peschardt K.K., Schipperijn J., Stigsdotter U.K. Use of small public urban green spaces (SPUGS) Urban Forestry and Urban Greening. 2012;11:235–244. [Google Scholar]
- Posner J., Polanczyk G.V., Sonuga-Barke E. Attention-deficit hyperactivity disorder. Lancet. 2020;395:450–462. doi: 10.1016/S0140-6736(19)33004-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pouso S., Borja Á., Fleming L.E., Gómez-Baggethun E., White M.P., Uyarra M.C. Contact with blue-green spaces during the COVID-19 pandemic lockdown beneficial for mental health. Science of the Total Environment. 2021;756 doi: 10.1016/j.scitotenv.2020.143984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prince M., Bryce R., Albanese E., Wimo A., Ribeiro W., Ferri C.P. The global prevalence of dementia: A systematic review and metaanalysis. Alzheimers Dement. 2013;9:63–75.e2. doi: 10.1016/j.jalz.2012.11.007. [DOI] [PubMed] [Google Scholar]
- Reklaitiene R., Grazuleviciene R., Dedele A., Virviciute D., Vensloviene J., Tamosiunas A., et al. The relationship of green space, depressive symptoms and perceived general health in urban population. Scandinavian Journal of Public Health. 2014;42:669–676. doi: 10.1177/1403494814544494. [DOI] [PubMed] [Google Scholar]
- Rodriguez-Loureiro L., Gadeyne S., Bauwelinck M., Lefebvre W., Vanpoucke C., Casas L. Long-term exposure to residential greenness and neurodegenerative disease mortality among older adults: A 13-year follow-up cohort study. Environmental Health. 2022;21:49. doi: 10.1186/s12940-022-00863-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rotenberg M., Tuck A., Anderson K.K., McKenzie K. Green space and the incidence of schizophrenia in Toronto, Canada. Canadian Journal of Psychiatry. 2022;67:238–240. doi: 10.1177/07067437221076722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rugel E.J., Carpiano R.M., Henderson S.B., Brauer M. Exposure to natural space, sense of community belonging, and adverse mental health outcomes across an urban region. Environmental Research. 2019;171:365–377. doi: 10.1016/j.envres.2019.01.034. [DOI] [PubMed] [Google Scholar]
- Sarkar C., Webster C., Gallacher J. Residential greenness and prevalence of major depressive disorders: A cross-sectional, observational, associational study of 94 879 adult UK biobank participants. The Lancet Planetary Health. 2018;2:e162–e173. doi: 10.1016/S2542-5196(18)30051-2. [DOI] [PubMed] [Google Scholar]
- Schipperijn J., Ekholm O., Stigsdotter U.K., Toftager M., Bentsen P., Kamper-Jørgensen F., et al. Factors influencing the use of green space: Results from a Danish national representative survey. Landscape and Urban Planning. 2010;95:130–137. [Google Scholar]
- Shor E., Roelfs D., Vang Z.M. The "Hispanic mortality paradox" revisited: Meta-analysis and meta-regression of life-course differentials in Latin American and Caribbean immigrants' mortality. Social Science & Medicine. 2017;186:20–33. doi: 10.1016/j.socscimed.2017.05.049. [DOI] [PubMed] [Google Scholar]
- Slawsky E.D., Hajat A., Rhew I.C., Russette H., Semmens E.O., Kaufman J.D., et al. Neighborhood greenspace exposure as a protective factor in dementia risk among U.S. Adults 75years or older: A cohort study. Environmental Health: A Global Access Science Source. 2022;21:14. doi: 10.1186/s12940-022-00830-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song H., Lane K.J., Kim H., Kim H., Byun G., Le M., et al. Association between urban greenness and depressive symptoms: Evaluation of greenness using various indicators. International Journal of Environmental Research and Public Health. 2019;16:173. doi: 10.3390/ijerph16020173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun Y., Molitor J., Benmarhnia T., Avila C., Chiu V., Slezak J., et al. Association between urban green space and postpartum depression, and the role of physical activity: A retrospective cohort study in southern California. Lancet regional health. Americas. 2023;21 doi: 10.1016/j.lana.2023.100462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thygesen M., Engemann K., Holst G.J., Hansen B., Geels C., Brandt J., et al. The association between residential green space in childhood and development of attention deficit hyperactivity disorder: A population-based cohort study. Environmental Health Perspectives. 2020;128 doi: 10.1289/EHP6729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomita A., Vandormael A.M., Cuadros D., Di Minin E., Heikinheimo V., Tanser F., et al. Green environment and incident depression in South Africa: A geospatial analysis and mental health implications in a resource-limited setting. The Lancet Planetary Health. 2017;1:e152–e162. doi: 10.1016/S2542-5196(17)30063-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Triebner K., Markevych I., Bertelsen R.J., Sved Skottvoll B., Hustad S., Forsberg B., et al. Lifelong exposure to residential greenspace and the premenstrual syndrome: A population-based study of northern European women. Environment International. 2022;158 doi: 10.1016/j.envint.2021.106975. [DOI] [PubMed] [Google Scholar]
- Tsai W.L., Nash M.S., Rosenbaum D.J., Prince S.E., D'Aloisio A.A., Mehaffey M.H., et al. Association of redlining and natural environment with depressive symptoms in women in the sister study. Environmental Health Perspectives. 2023;131 doi: 10.1289/EHP12212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van den Berg M., Van Poppel M., Van Kamp I., Andrusaityte S., Balseviciene B., Cirach M., et al. Visiting green space is associated with mental health and vitality: A cross-sectional study in four european cities. Health & Place. 2016;38:8–15. doi: 10.1016/j.healthplace.2016.01.003. [DOI] [PubMed] [Google Scholar]
- Van Renterghem T., Forssén J., Attenborough K., Jean P., Defrance J., Hornikx M., et al. Using natural means to reduce surface transport noise during propagation outdoors. Applied Acoustics. 2015;92:86–101. [Google Scholar]
- White M.P., Elliott L.R., Grellier J., Economou T., Bell S., Bratman G.N., et al. Associations between green/blue spaces and mental health across 18 countries. Scientific Reports. 2021;11:8903. doi: 10.1038/s41598-021-87675-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolch J.R., Byrne J., Newell J.P. Urban green space, public health, and environmental justice: The challenge of making cities ‘just green enough’. Landscape and Urban Planning. 2014;125:234–244. [Google Scholar]
- Wu Y.T., Brayne C., Liu Z., Huang Y., Sosa A.L., Acosta D., et al. Neighbourhood environment and dementia in older people from high-, middle- and low-income countries: Results from two population-based cohort studies. BMC Public Health. 2020;20:1330. doi: 10.1186/s12889-020-09435-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu L., Kim S.K. Does socioeconomic development lead to more equal distribution of green space? Evidence from Chinese cities. Science of the Total Environment. 2021;757 doi: 10.1016/j.scitotenv.2020.143780. [DOI] [PubMed] [Google Scholar]
- Yang B.Y., Zeng X.W., Markevych I., Bloom M.S., Heinrich J., Knibbs L.D., et al. Association between greenness surrounding schools and kindergartens and attention-deficit/hyperactivity disorder in children in China. JAMA Network Open. 2019;2 doi: 10.1001/jamanetworkopen.2019.17862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuchi W., Brauer M., Czekajlo A., Davies H.W., Davis Z., Guhn M., et al. Neighborhood environmental exposures and incidence of attention deficit/hyperactivity disorder: A population-based cohort study. Environment International. 2022;161 doi: 10.1016/j.envint.2022.107120. [DOI] [PubMed] [Google Scholar]
- Yuchi W., Sbihi H., Davies H., Tamburic L., Brauer M. Road proximity, air pollution, noise, green space and neurologic disease incidence: A population-based cohort study. Environmental Health: A Global Access Science Source. 2020;19:8. doi: 10.1186/s12940-020-0565-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zagnoli F., Filippini T., Jimenez M.P., Wise L.A., Hatch E.E., Vinceti M. Is greenness associated with dementia? A systematic review and dose-response meta-analysis. Current Environment Health Representative. 2022;9:574–590. doi: 10.1007/s40572-022-00365-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zayas-Costa M., Cole H.V.S., Anguelovski I., Connolly J.J.T., Bartoll X., Triguero-Mas M. Mental health outcomes in Barcelona: The interplay between gentrification and greenspace. International Journal of Environmental Research and Public Health. 2021;18:9314. doi: 10.3390/ijerph18179314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang J., Browning M., Liu J., Cheng Y., Zhao B., Dadvand P. Is indoor and outdoor greenery associated with fewer depressive symptoms during COVID-19 lockdowns? A mechanistic study in Shanghai, China. Building and Environment. 2023;227 doi: 10.1016/j.buildenv.2022.109799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang X.H., Wei F., Yu Z.B., Guo F.J., Wang J.B., Jin M.J., et al. Association of residential greenness and incident depression: Investigating the mediation and interaction effects of particulate matter. Science of the Total Environment. 2022;811 doi: 10.1016/j.scitotenv.2021.152372. [DOI] [PubMed] [Google Scholar]
- Zhou X.J., Qin Z., Lu J., Hong J.G. Efficacy and safety of salmeterol/fluticasone compared with montelukast alone (or add-on therapy to fluticasone) in the treatment of bronchial asthma in children and adolescents: A systematic review and meta-analysis. Chinese Medical Journal. 2021;134:2954–2961. doi: 10.1097/CM9.0000000000001853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou R., Zheng Y.J., Yun J.Y., Wang H.M. The effects of urban green space on depressive symptoms of mid-aged and elderly urban residents in China: Evidence from the China health and retirement longitudinal study. International Journal of Environmental Research and Public Health. 2022;19:717. doi: 10.3390/ijerph19020717. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data will be made available on request.