Abstract
If the term “genetics” is a relatively recent proposition, introduced in 1905 by English biologist William Bateson, who rediscovered and spread in the scientific community Mendel’s principles of inheritance, since the dawn of human civilization the influence of heredity has been recognized, especially in agricultural crops and animal breeding. And, later, in familial dynasties. In this concise review, we outline the evolution of the idea of hereditary hearing loss, up to the current knowledge of molecular genetics and epigenetics.
Keywords: inheritance, genetics, epigenetics, hearing loss, deafness, deaf-mutism, consanguinity
1. Introduction
The interest in genetics is particularly lively due to the recent finding of a “genetic” contributory cause to COVID-19 deaths [1,2].
The term “genetics” is a relatively recent proposition, introduced in 1905 by English biologist William Bateson (1861–1926), who rediscovered and spread in the scientific community Mendel’s principles of inheritance. Since the dawn of human civilization, the influence of heredity has been recognized, especially in agricultural crops and animal breeding [3].
The word genetic comes from the French génétique, formed from the Greek genetikós, “which refers to gender”, and that is the genitive case, transferred from the grammatical field to the biological one. Gene, from the German Gen, taken from the root of the Greek ‘génesis’ (generation). Gènesis, from the Latin genĕsis, is derived from the Greek génesis, an action noun of the verb gígnomai, “I generate”, meaning “origin” [4,5]. Gen was coined in 1905 by Wilhelm Ludvig Johannsen (1857–1927), who also coined the term genotype and phenotype [6,7]; Darwin used the term pangenesis in 1868 [8,9], later revived by Hugo De Vries (1848–1935) as Intracellular Pangenesis [10,11].
2. Hybridists and Hereditarists
Numerous considerations on anomalies passed along generations have been made since ancient times. In the modern era, among others, Ulisse Aldrovandi (1522–1605) and Fortunio Liceti (1577–1657) stood out.
The interest in inheritance found spur at the end of the 16th century with the observations of Prosper Alpinus (or Prospero Alpini, 1553–1616, physician and botanist, prefect of the medical garden, Padova University), who observed a sexual difference in date palm plants. This observation became relevant in the foundation of the Linnaean taxonomy system. Carolus Linnaeus himself (or Carl von Linné, 1707–1778) started in the eighteenth century the theory of plant sexuality. From these studies and through the impulse given by the Enlightenment to agricultural sciences, the current of thought of the Vegetable Hybridists developed. The studies on hybridization were the starting point of Mendel’s research.
Another group of scientists (Hereditarists) followed the Preformationism theory, which was very popular in the first half of the eighteenth century. The fundamental principle was already proposed by Anaxagoras (496–428 b.C.) and Democritus (460–370 b.C.) and then accepted in the Corpus Hippocraticum. According to the manuscript, the seed derived from all the districts of the adult body and is made up of small particles, which were capable of reproducing the whole body though the formation of the embryo [12].
Table 1 shows the scholars who have most contributed to studies on heredity before Gregor Mendel (Hynčice 1822–Brno 1884).
Table 1.
The major exponents of the two main currents of thought on heredity before Mendel’s laws.
| Vegetable Hybridists | Hereditarists |
|---|---|
| Prospero Alpini (also known as Prosperus Alpinus, Prosper Alpinus, Prospero Alpinio) (Marostica 1553–Padua 1616) Adam Zaluziansky (Mnichov Hradiště 1558–Prague 1613) Nehemiah Grew (Atherstone 1641–London 1712) Rudolf Jakob Camerer (Tübingen 1665–Tübingen 1721) Carl von Linné (Råshult 1707–Uppsala 1778) Gottlieb Joseph Kölreuter (Sulz am Neckar 1733–Karlsruhe 1806) Thomas Andrew Knight (Wormsley 1759–London 1838) Augustin Sageret (Paris 1763–Paris 1851) Carl Friedrich von Gärtner (Göppingen 1772–Calw 1850) Henri Lecoq (Avesnes-sur-Helpe 1802–Clermont Ferrand 1871) Dominique Alexandre Godron (Hayange 1807–Nancy 1880) Charles-Victor Naudin (Autun 1815–Antibes 1899) Max Ernt Wichura (Neisse 1817–Berlin 1866) |
William Wollaston (Coton–Clanford 1660–London 1724) Pierre-Louis Moreau de Maupertuis (Saint-Malo 1698–Basilea 1759) Georges-Louis Leclerc de Buffon (Montbard 1707–Paris1788) Charles Darwin (Shrewsbury 1809–Downe 1882) Karl Wilhelm von Nägeli (Kilchberg 1817–Munich 1891) Herbert Spencer (Derby 1820–Brighton 1903) Francis Galton (Sparkbrook 1822–Haslemere 1911) Thomas Henry Huxley (Ealing 1825–Eastbourn 1895) |
3. Inheritance and Genetics in Humans
While most of the research was in the botanic field, among the Hereditarists there was also attention paid to human pathologies. In 1751, Pierre-Louis Moreau de Maupertuis (1698–1759) used the statistical analysis of the recurring polydactyly in the Ruhe family to demonstrate that (a) the phenomenon was not random but referred to a biological mechanism of character transmission that was still unknown; (b) the malformation was transmitted both maternally and paternally. The Preformationism idea was therefore amiss, in the ovistic and animalculistic versions. De Maupertuis suggested that the inheritance of characteristics was bound to “particles” in both germ cells. These particles would be responsible for the formation of different organs and structures in the baby [12]. Only in the second half of the 17th century hereditary diseases became the focus of some attention (see the Dissertatio Medica Inauguralis ‘Morbis Haereditariis’ by Johann Andreas Fischer at the Medical Faculty of Erfurt, January 1688. Frontispiece in Figure 1).
Figure 1.
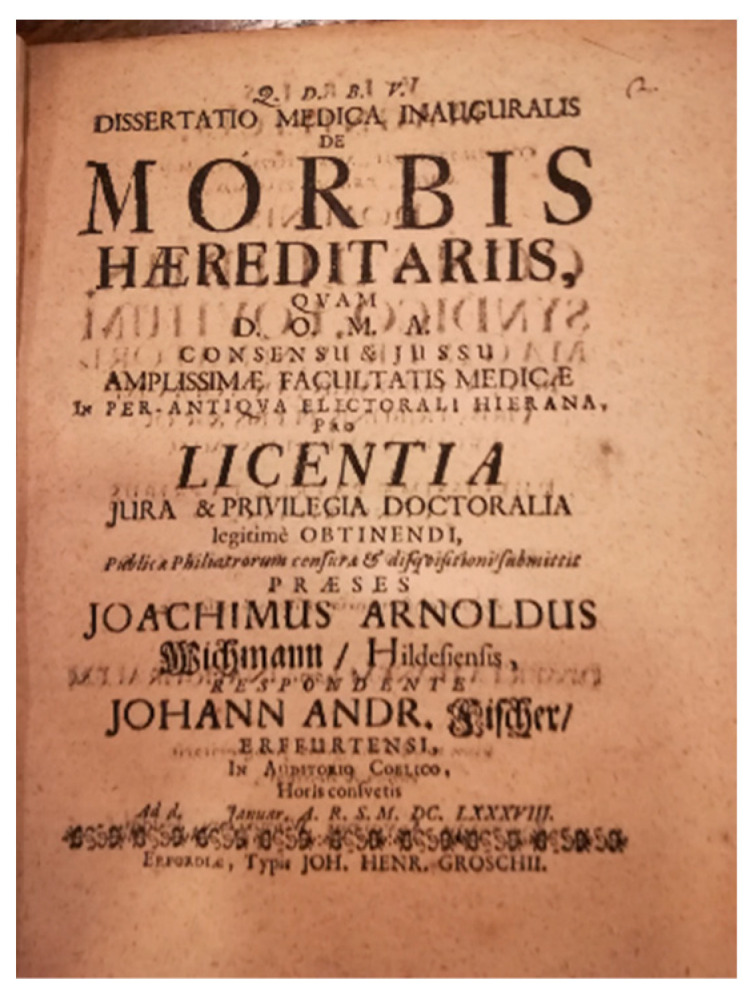
Frontispiece of Johann Andreas Fischer’s Dissertatio Medica Inauguralis de Morbis Haereditariis, 1688 (personal collection).
4. The Inheritance of Hearing Loss and Deafness
Apart from some sporadic descriptions, perhaps the first finding of a fairly large series of familial deafness was that of the island of Martha’s Vineyard [13]. For almost three centuries, a high rate of hereditary deafness appeared in the population of Martha’s Vineyard, an island in Dukes Country, southern Massachusetts, separated from Cape Cod by Vineyard Sound. In 1642, a group of migrants arrived from the county of Kent, in the south of England. The ancestor of most of the deaf was Jonathan Lambert, who moved there with his wife—who was not deaf—in 1694. When the migration virtually ceased, the endogamous community that was created contained a high incidence of hereditary deafness that persisted for over 200 years. Due to the isolation, a village sign language was developed, and it was once widely used in the island from the early 18th century to 1952. Martha’s Vineyard Sign Language was used by both deaf and hearing people in the community.
The GJB2 gene was causing deafness in Martha’s Vineyard. Today, we know hundreds of hereditary types of hearing loss (see Hereditary Hearing Loss Homepage) [14].
5. The Birth of Otology
«Until the beginning of the 19th century, there were almost no measuring tools to determine and quantify the degree of hearing disability» [15]. In the first part of the 19th century, new examination techniques became available, such as the otoscope with magnification and overall, functional hearing tests became possible. In 1802, Christian Heinrich Wolke (1741–1825) created the first ‘Akuometer’, and the main concepts of audiometry evolved. These innovations, together with the development of more adequate pathological knowledge, and therefore the possibility of a better diagnostic and therapeutic framework, and the improvement of surgical techniques allowed for the birth of new specialists dedicated to the treatment of otological pathologies, with the establishment of specialized hospitals (usually together with eye diseases).
The most significant contributions are those of the German, French, English, and Italian schools, as is reported in Table 2.
Table 2.
The major exponents of the birth and development of otology in the nineteenth century.
| French School | German School |
|---|---|
| Antoine Saissy (1756–1822) Jean Marc Gaspard Itard (1775–1838) Gilbert Breschet (1784–1845) Pierre-Marie Flourens (1794–1867) Nicholas Deleau the Younger (1797–1862) Prosper Menière (1798–1862) Marcellin Emile Hubert-Valleroux (1812–1884) Alexandre Louis Paul Blanchet (1819–1867) |
Ernst Heinrich Weber (1795–1878) Emil Huschke (1797–1858) Wilhelm Kramer (1801–1875) Eduard Schmalz (1801–1871) Carl Gustav Lincke (1804–1849) Gabriel Gustav Valentin (1810–1883) Hermann von Helmholtz (1821–1894) Ernst Reissner (1824–1878) Anton Friedrich von Tröltsch (1828–1867) Otto Friedrich Karl Deiters (1834–1863) Ádám Politzer (1835–1920) Hermann Schwartze (1837–1910) |
| English school | Italian school |
| William Robert Wilde (1773–1860) John Cunningham Saunders (1773–1810) William Wright (1773–1860) Samuel Akery (1785–1845) Henry Jones Shrapnell (1792–1834) James Yearsley (1805–1869) Joseph Toynbee (1815–1866) |
Carlo Giovanni Brugnone (1741–1816) Alfonso Corti (1822–1876) Demetrio Bargellini (1823–1899) Giuseppe Gradenigo (1859–1926) Vittorio Grazzi (1849–1929) Vincenzo Cozzolino (1853–1911) |
6. Deaf-Mutism
During the 19th century, there was a great debate on congenital deafness and consequent mutism. The prevalence was around 0.05–0.10% in Europe and a little less in the United States of America [16]. The existence of risk factors that influenced the frequency of deaf-mutism was already a topic of debate at that time [17]. However, Albert Eulenburg (1840–1917) notably addressed the issue of consanguinity while studying populations residing in mountainous regions, emphasizing the problem of «close proximity of life and due to the often-deficient exchange with the outside world». The inquiry considered consanguinity as a potential risk factor, exploring the idea that «among those who enter into marriage, no other individual dispositions yet exist; inheritance, etc., for the procreation of deaf and dumb children» [16].
By the end of the century, there was already a debated awareness of the existence of risk factors influencing the prevalence of deaf-mutism. However, clear causes of congenital deaf-mutism remained elusive.
7. Consanguinity
Various authors examined the incidence of deaf-mutes in consanguineous marriages [18,19,20,21,22,23].
In Germany, Richard Liebreich and Georg von Mayr reported a higher incidence of deaf-mutism among Jews compared to Christians (with a ratio ranging from 1:2 to 1:4). Additionally, albeit with a smaller difference, they noted a higher incidence among Protestants compared to Catholics [21,24]. These variations were linked to the prevalence of consanguineous marriages among Jews and the allowance of such marriages among Protestants, in contrast to the prohibition among Catholics. Schmaltz (1884) observed an increase in the frequency of deaf-mutism corresponding to the number of consanguineous spouses.
Eulenberg, recognizing the complexities involved, asserted that «the question of the inheritance of congenital deaf-mutism is not truly resolved with all certainty through statistics». He considered possibilities such as direct and indirect hereditary transmission: «much more frequently, an indirect hereditary transmission of deaf-mutism can be demonstrated, either in the sense that the infirmity appears in ancestors and descendants, or monsters in the various lateral lines»; further on he writes «in addition to the above-mentioned more or less probable causes of congenital deaf-mutism, various authors also adduce a whole series of factors, especially important ones, such as the drunkenness of the parents, their mental illnesses, the large age difference, violent emotional excitations during pregnancy, etc., without it having until now been possible with statistics or accurate direct observations to even demonstrate the probability of an etiological link between these conditions and congenital deaf-mutism» [16]. The question raised is whether consanguinity is the risk factor or the fact that «among those who enter into marriage no other individual dispositions yet exist; inheritance, etc. for the procreation of deaf and dumb children» [16].
An important indicator sufficient to raise suspicion of a congenital form of deaf-mutism was the presence of other conditions in relatives, such as additional cases of deaf-mutism or specific ocular diseases such as retinitis pigmentosasyndactyly, epilepsy, chorea, and cleft lip [21].
8. Heredity of Deafness
Wilde (1853) [25], Liebreich (1861) [19], and Uchermann (1869) [23] had found evidence that hearing impairment and deafness could be hereditary. Wilde wrote in 1853: «That diseases of the ear are hereditary there is little doubt; and next to the congenitally deaf and dumb, I believe that nervous deafness is the most frequent form in which the disease is transmitted; but whether arising from some congenital peculiarity of the auditory nerve, which only becomes developed in after life, I cannot say. I know many cases in which mothers and daughters are deaf. I have also known several members of the same family and its collateral branches deaf of one ear. In the upper ranks of society, the disease is much more frequent in females than males» [25].
An indirect familiar connection was described by different authors, with no clear direct inheritance [24,26]. A more frequent familiarity in the collateral line rather than the vertical line was described, besides that of a hypothetic recessive transmission.
Politzer wrote in 1882 that «the most frequent causes of congenital deafness are: hereditary, including direct transmission from the parents as well as indirect transmission from forefathers and marriage between blood relatives» [27]. This assertion stemmed from the research of Arthur Hartmann, who conducted studies in Berlin’s schools for deaf children [28]. Hartmann differentiated between the direct transmission of deafness from parent to child and indirect transmission, in which he observed a high incidence of consanguinity [23].
Giuseppe Gradenigo reported in 1887 not only the difference between “chronic catarrhal otitis media” and “otosclerosis”, but probably was the first to report on possible hereditary origin «I must claim priority, for having, as early as 1887, asserted the very clear distinction between the two affections, and highlighted the degenerative hereditary nature of otosclerosis in contrast to the exogenous, inflammatory nature of chronic catarrhal otitis» [29].
In the second edition of his Lehrbuch der Ohrhenheilkunde, published in 1887, Politzer clearly stated that deafness could be attributed to inheritance. He distinguished between direct or dominant inheritance and indirect or recessive inheritance, drawing on the research of another German author, Arthur Hartmann.
Holger Mygind [30], Uchermann, and Hartmann were among the early advocates for considering heredity as a significant factor. According to these authors, the consanguinity of parents only reinforces inheritance when it is present. Gradenigo (1903) asserted that «heredity has a great influence in the production of congenital deaf-mutism» and the presence of other cases of deaf-mutism in the family or retinitis pigmentosa serves as criteria supporting the congenital form [17]. Gradenigo also emphasized that «in the case of ear diseases in general, the existence of other cases of deafness in the family is a valuable factor in differential diagnosis» [31].
The first descriptions of syndromes involving hearing impairment or deafness emerged in the 19th century. Examples include Usher syndrome [21,32,33], branchio-oto-renal syndrome [34], Pendred syndrome [35], Treacher Collins syndrome [36,37], and osteogenesis imperfecta tarda [38]. While most hereditary hearing impairments are non-syndromic, more attention has been given to syndromic hearing disorders due to their distinguishable associated characteristics. Similarly, congenital forms of deafness have historically received more focus than late-onset hearing impairments.
9. The Audiometer and the Audiogram Phenotype
With the introduction of the audiometer in the late 1930s, describing and distinguishing non-syndromic forms of hearing impairment became more accessible. In 1955, Fisch described a relation between audiometric patterns and the etiology of perceptive deafness. He noted that «a flat audiogram suggests rubella, a saucer-shaped audiogram kernicterus, a gently sloping audiogram with the high tones affected more than the low is often seen in dominant deafness, and a sharply sloping audiogram with a residual island of hearing in the low tones suggests autosomal recessive deafness» [39].
Fraser (1970) reported on a substantial sample of 3534 individuals who had been “profoundly deaf from childhood,” describing numerous syndromic cases and focusing on causes based on “family history” [40]. He discussed the limited impact of discouraging deaf individuals from marrying each other in reducing the prevalence of genetically determined and recessive deafness. Fraser highlighted that such deafness is often not inherited from one generation to the next due to its association with numerous different genes. More frequently, the transmission of deafness from parent to child occurs when one of the parents has dominant deafness, regardless of whether the marriage partner is hearing or deaf [40].
Konigsmark (1971) emphasized the aid of five characteristics in the differential diagnosis of about 70 types of hereditary deafness in humans («(1) The mode of genetic transmission, (2) the characteristics of the deafness, (3) the age of onset, (4) the sonic frequencies involved and (5) the associated abnormalities»). These characteristics include the mode of genetic transmission, the characteristics of deafness, the age of onset, the sonic frequencies involved, and associated abnormalities [41]. The book “Genetic and Metabolic Deafness” by Bruce W. Konigsmark and Robert J. Gorlin, published in 1976 [42], along with subsequent editions, as well as McKusick’s “Mendelian Inheritance in Man” [43,44] and its online version [45], have been crucial reference sources for clinicians for decades.
10. Molecular Genetics and Epigenetics
The development of genetics, briefly reported in Table 3, was fundamental to identify new causes of hearing loss.
Table 3.
The main stages of research that led to the discovery of the DNA double helix (1953).
| Period | Discoveries |
|---|---|
| 1866 | Ernst Heinrich Haeckel (Potsdam 1834–Jena 1919), in 1866, proposed that the nucleus contained the factors responsible for the transmission of hereditary traits. |
| 1869 | Johann Friedrich Miescher (Basel 1844–Davos 1895) identified in 1869, inside the nuclei of human white blood cells, ‘nuclein’, the molecule now known as DNA |
| 1870s | Walther Flemming (Schwerin 1843–Kiel 1905) in the 1870s described the morphology of a fibrous structure within the nucleus of cells, named ‘chromatin’, now known as chromosomes. By observing this chromatin, Flemming correctly worked out how chromosomes separate during cell division, also known as mitosis. |
| since 1879 | Ludwig Karl Martin Leonhard Albrecht Kossel (Rostock 1853–Heidelberg 1927) made great progress in understanding the basic building blocks of nuclein. Kossel isolated the five nucleotide bases that are the building blocks of DNA and RNA: adenine, cytosine, guanine, thymine, and uracil. In 1881, Kossel identified nuclein as a nucleic acid and provided its present chemical name, deoxyribonucleic acid (DNA). |
| since the 1880s | Theodor Boveri (Bamberg 1862–Würzburg 1915) first presented the idea that the genetic material passed down from parent to child is within the chromosomes. |
| since 1905 | Walter Stanborough Sutton (Utica 1877–Kansas City 1916) expanded on Theodor’s observation. He found it was possible to distinguish individual chromosomes undergoing meiosis in the testes of the grasshopper and identified the sex chromosome. |
| since 1905 | Phoebus Aaron Theodor Levene (Sagor 1869–New York 1940), and his student J. A. Mandel, described a linear complex with a phosphoric acid and a base forming a subunit they called a mononucleotide, with two or more mononucleotides bound together to form what they called a polyphosphoric acid, or polynucleotide. |
| since 1910 | Thomas H. Morgan (Lexington 1866–Pasadena 1945) and his students (Alfred Sturtevant, Calvin Bridges, Hermann Muller, and others), provided the proof for the chromosomal theory of heredity, genetic linkage, and chromosomal crossing over and non-disjunction. |
| 1928 | Frederick Griffith (Prescott 1879–London 1941) performed important studies on Bacterial transformation. |
| 1944 | Oswald Avery (Halifax 1877–Nashville1955). In 1944, he and his colleagues Maclyn McCarty and Colin MacLeod reported that the transforming substance, the genetic material of the cell, was DNA. |
| 1950 | Erwin Chargaff (Černivci 1905–New York 2002) found that in DNA, the ratios of adenine (A) to thymine (T) and guanine (G) to cytosine (C) are equal. |
| 1951–1952 | Maurice Hugh Frederick Wilkins (Pongaroa 1916–London 2004) and Rosalind Franklin (Kensington 1920–Chelsea 1958), at King’s College London, used X-ray diffraction to study the structure of DNA in solution. They found that DNA could take two forms: crystalline or A form, and paracrystalline or B form, as «big helix with several chains, phosphates on outside, phosphate–phosphate interhelical bonds, disrupted by water». |
| 1953 | J. D. Watson, F. H. C. Crick. Molecular structure of nucleic acids. A Structure for Deoxyribose Nucleic Acid. Nature 4356 April 25: 737-38, 1953 M. H. F. Wilkins, A. R. Stokes, H. R. Wilson. Molecular Structure of Deoxypentose Nucleic Acids. Nature 4356 April 25: 738-40, 1953 |
Since the mid-1900s, extensive efforts have been dedicated to comprehending the origins of both syndromic and non-syndromic hearing loss and identifying connections with specific audiological traits. In the last three decades, remarkable advances in molecular genetics have significantly contributed to our understanding of the causes and pathology of hearing impairment.
Linkage analyses in affected families have allowed researchers to successfully map the loci associated with hearing loss. Investigations of homozygosity have made it possible to identify autosomal recessive genes in consanguineous families. The first non-syndromic hearing loss locus was mapped in 1988 through the study of families with X-linked inheritance (DFNX2) [46,47]. It led to the identification of the POU3F4 gene in 1995 [48]. The first autosomal dominant locus (DFNA1) was linked to chromosome 5q31 in 1992 [49], and, a few years later, the DIAPH1 gene was identified [50]. The first autosomal recessive locus (DFNB1) was mapped in 1994 [51].
The first pathogenic variants of the GJB2 gene, encoding the protein connexin 26, the mutation of which are the cause of most forms of non-syndromic congenital deafness, was discovered in 1997 [52]. The identification of the GJB2 gene revolutionized the clinical approach to hearing loss, particularly for “isolated” deafness, which constituted the majority of cases labeled as “deafness of unknown cause.” Next-generation sequencing technologies have significantly improved the diagnostic rate for genetic hearing loss, allowing the detection of novel variants in known deafness-related genes and the identification of new genes associated with hearing disease.
Among the factors that cause syndromic and non-syndromic deafness, several mutations, which are in hundreds of genes, have been identified. Nowadays, approximately 206 non-syndromic hearing loss loci are known (78 autosomal dominant loci, 121 autosomal recessive loci, 7 X-linked loci, and one Y-linked locus). A total of 125 non-syndromic hearing loss-associated genes have been reported [14]. Finally, more than 400 syndromes that have hearing loss in their phenotypic presentation have been identified and described [53].
Scientists subsequently have turned their attention to epigenetics, a term coined by Conrad Waddington in 1942. Epigenetics is a branch of biology which studies heritable changes in gene expression that occur without alterations of the DNA sequence [54,55], regulating gene function through DNA and histone modifications, non-coding RNA expression, and chromatin remodeling. Five years after James Watson and Francis Crick first published the 3D structure of the DNA double helix [56]. In 1958, David Ledbetter Nanney [57] published a paper in which he used the term epigenetics to distinguish between different types of cellular control systems, trying to explain the relationships between genotype and phenotype [58,59]. Epigenetic regulation plays a vital role in maintaining genome stability, normal embryo development, and cell differentiation, and abnormalities can lead to various diseases, such as cancer [60] or type 2 diabetes.
Researchers in epigenetics and genetics collaborate closely to uncover the fundamental mechanisms of complex diseases, identifying novel therapeutic targets and prognostic indicators [61,62,63,64,65].
The significance of epigenetics in ear development is evident in human genetic disorders caused by mutations in genes involved in chromatin remodeling, DNA methylation, and histone modification. It is able to impact processes such as neurodevelopment [66], the development of external ear defects, and hearing loss. Vincent Michael Riccardi was probably the first scientist to consider the role of epigenetics in the genetic expression of genetic disorders in cranio-facial malformation hearing loss [67].
Epigenetic regulation influences various stages of cochlear hair cell (HC) life, such as differentiation, proliferation, and survival [68]. It contributes to HC regeneration, playing a critical role in ototoxic drug-induced hearing loss, noise-induced hearing loss, and D-gal-induced mimicking of presbycusis. Researchers are exploring compounds to regulate epigenetic modification as a potential avenue for alleviating acquired hearing loss. Epigenetic regulation is also crucial for inner ear HC regeneration, which offers an opportunity for hearing loss therapy [69,70].
Notably, environmental conditions, such as aging, lifestyle, infections, toxic exposure, and concurrent pathologies, can alter the epigenetic status, as reported by Gemmati and Collaborators [71]. Epigenetic markers may serve as indicators of disease, or contribute to the development of pathological conditions [72,73]. Inherited predispositions or gene mutations can shape an individual’s epigenetic landscape, potentially leading to various pathologies, including cancer, neurological diseases, pregnancy loss, and delayed wound healing [74,75,76]. Metal overload and epigenetic changes may also affect the cochlea or the sensorial epithelium, playing a role in various forms of sensorineural hearing loss. [77,78]. These facts were observed by the same group, describing how iron homeostasis genes predispose to one of the most difficult and complex forms of hearing loss, i.e., idiopathic sudden sensorineural hearing loss [79].
11. A Look at the Future: The “Omics Sciences” and Artificial Intelligence
Recently, there has been a lot of discussion about “Omics Sciences”, such as genomics, transcriptomics, proteomics, or metabolomics, and on the possible advantage of artificial intelligence (AI) for a better understanding of the causes and treatment of hearing loss [80]. The suffix “-omics” is used to address the objects of study in fields, such as the genome, proteome, transcriptome, or metabolome, respectively.
We will try to briefly summarize the state of the art of “Omics Sciences”.
11.1. Genomics
Genomics is the discipline that studies the genome of living beings. It deals with the structure, content, function, and evolution of the genome, utilizing bioinformatics to process and visualize the enormous amount of data that is produced [81].
Genomic technologies have transformed medicine in the post-genome era, promising personalized and precise healthcare based on DNA sequencing. The existing literature on this subject is extensive, with numerous reports continuously emerging, presenting new discoveries for a better understanding of various alterations [82,83] and potential gene therapies [84].
Before and immediately after the completion of the Human Genome Project, the primary obstacle to advancing precision medicine was the generation of DNA sequencing and genetic variant data. This challenge was particularly significant in the study of genetic hearing loss. The classification of genetic variants posed a major challenge in the post-genome era.
Richard Smith’s group evaluated and classified 876,139 hearing loss genetic variants; around 8100 variants were found to be pathogenic or likely pathogenic, 172,000 variants benign or likely benign, and more than 695,000 variants of uncertain significance [85]. The authors observed that over 96% of the coding variants were both rare and novel. They noted that the pathogenicity was influenced by factors such as minor allele frequency thresholds, variant effects, and protein domain considerations. The mutational landscape revealed intricate gene-specific variability, underscoring the importance of comprehending these nuances for enhanced accuracy in variant interpretation. This understanding is foundational for improving clinical decision-making and advancing our knowledge of deafness biology and treatment [86].
11.2. Proteomics
Proteomics is defined as the science that explores the interactions, function, composition, and structures of proteins and their cellular activities [87]. A proteome is a set of proteins produced in an organism, system, or biological context. Proteomics has proven effective in studying the inner ear. This approach aids in elucidating basic and pathologic mechanisms, diagnosing diseases, and treating hearing disorders [88,89,90,91,92,93]. Notably, recent research has highlighted the role of sophisticated glutamatergic ribbon synapses with afferent neurons to transmit auditory information to the brain. Furthermore, the multi-C2 domain protein otoferlin has been analyzed, linking defects in the coding Otof gene to auditory synaptopathy [94].
11.3. Transcriptomics
Transcriptomics, utilizing technologies such as bulk microarrays and RNA sequencing (RNA-Seq), provides a comprehensive view of the transcriptional landscape of auditory research [95,96]. Single-cell RNA-seq (scRNA-seq) technology has significantly contributed to the study of inner ear hearing, offering accurate transcriptome information for hair cell regeneration and hearing recovery. It also provides dimensional insights into the auditory organ, complementing other technologies mentioned above and holding potential for future clinical applications.
11.4. Metabolomics
Metabolomics, reflecting both genetic traits and environmental influences, plays a crucial role in understanding various forms of hearing impairment [97]. Recent studies have reported consistent data on the predictive role of serum metabolic profiles in sudden hearing loss [98], noise-induced hearing loss [99], and the identification of markers for ototoxicity [97,100]. Metabolomic investigations may pave the way for improved diagnostic strategies, personalized interventions, and targeted treatments, ultimately enhancing the clinical management of individuals affected by different causes of hearing loss [101,102].
11.5. Artificial Intelligence
Artificial Intelligence (AI) is not merely a topic of discussion, as the development of this technology is progressively expanding its possible applications [80]. AI is actively reshaping healthcare delivery. Specifically, deep learning (DL) and reinforcement learning (RL) methods are becoming indispensable factors in otolaryngology and communication sciences. While AI systems excel in specific areas like image and speech recognition, there is acknowledgment that the human brain still outperforms AI in many daily tasks [80]. The potential of AI to revolutionize healthcare, particularly in the field of otolaryngology, is increasingly recognized, with DL and RL methods playing crucial roles in achieving human-level or super-human AI systems [103]. To date, AI seems to be able to play an important role not only in the diagnosis of some complex forms disease [104,105,106] but also in sign language recognition and translation [107,108].
The enormous amount of data that can be obtained from “Omics Sciences” can be integrated and analyzed by artificial intelligence and the resulting digital transformation of systems science. But this is a story still largely to be written [109].
Author Contributions
Conceptualization, A.M.; methodology, A.M. and A.C.; software, A.C. and V.M.D.P.F.; validation, A.M. and A.C.; formal analysis, A.M., A.C. and V.M.D.P.F.; investigation, A.M. and V.M.D.P.F.; resources, A.M., A.C. and V.M.D.P.F.; data curation, A.M., A.C. and V.M.D.P.F.; writing—original draft preparation, A.M., A.C. and V.M.D.P.F.; writing—review and editing, A.M., A.C. and V.M.D.P.F.; visualization, A.M., A.C. and V.M.D.P.F.; supervision, A.M.; project administration, A.M. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data sharing not applicable.
Conflicts of Interest
The authors declare no conflicts of interest.
Funding Statement
This research received no external funding.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Zeberg H., Pääbo S. The major genetic risk factor for severe COVID-19 is inherited from Neanderthals. Nature. 2020;587:610–612. doi: 10.1038/s41586-020-2818-3. [DOI] [PubMed] [Google Scholar]
- 2.Breno M., Noris N., Rubis N., Parvanova A.I., Martinetti D., Gamba S., Liguori L., Mele C., Piras R., Orisio S., et al. A GWAS in the pandemic epicenter highlights the severe COVID-19 risk locus introgressed by Neanderthals. iScience. 2023;26:107629. doi: 10.1016/j.isci.2023.107629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Genetics|History, Biology, Timeline, & Facts|Britannica. [(accessed on 5 November 2023)]. Available online: https://www.britannica.com/science/genetics.
- 4.Devoto G. Avviamento Alla Etimologia Italiana: Dizionario Etimologico. 3rd ed. Le Monnier; Firenze, Italy: 1968. [Google Scholar]
- 5.Montanari F. Vocabolario Della Lingua Greca. Loescher; Torino, Italy: 1995. [Google Scholar]
- 6.Johannsen W. Elemente der Exakten Erblichkeitslehre. Fischer; Jena, Germany: 1909. [Google Scholar]
- 7.Roll-Hansen N. The Genotype Theory of Wilhelm Johannsen and its Relation to Plant Breeding and the Study of Evolution. Centaurus. 1979;22:201–235. doi: 10.1111/j.1600-0498.1979.tb00589.x. [DOI] [Google Scholar]
- 8.Darwin C. The Variation of Animals and Plants under Domestication. John Murray; London, UK: 1868. [Google Scholar]
- 9.Liu Y. A new perspective on Darwin’s Pangenesis. Biol. Rev. Camb. Philos. Soc. 2008;83:141–149. doi: 10.1111/j.1469-185X.2008.00036.x. [DOI] [PubMed] [Google Scholar]
- 10.Vries H. De Intracellular Pangenesis. Gustav Fischer; Jena, Germany: 1889. [Google Scholar]
- 11.Stamhuis I.H., Meijer O.G., Zevenhuizen E.J. Hugo de Vries on heredity, 1889–1903. Statistics, Mendelian laws, pangenes, mutations. Isis. Int. Rev. Devoted Hist. Sci. Its Cult. Influ. 1999;90:238–267. doi: 10.1086/384323. [DOI] [PubMed] [Google Scholar]
- 12.Di Trocchio F. Storia Della Scienza. Treccani; Roma, Italy: 2003. L’Ottocento: Biologia. Studi sull’ereditarietà. [Google Scholar]
- 13.Enerstvedt R. The Legacy of the Past: Those Who Are Gone but Have Not Left. Basis-Tryk; Dronninglund, Denmark: 1996. [Google Scholar]
- 14.Van Camp G., Smith R.J.H. Hereditary Hearing Loss Homepage. [(accessed on 14 September 2021)]. Available online: https://hereditaryhearingloss.org.
- 15.Mudry A. The History of Otology: A Tribute to Adam Politzer. Wayenborgh; Peribebuy, Paragauy: 2015. [Google Scholar]
- 16.Eulenburg A. Real-Encyklopädie der Gesammten Heilkunde: Medizinisch-Chirurgisches Handwörterbuch für Praktische Ärzte. Volume 12 Urban & Schwarzenberg; Wien und Leipzig, Germany: 1890. [Google Scholar]
- 17.Cozza A., Di Pasquale Fiasca V.M., Martini A. Congenital Deafness and Deaf-Mutism: A Historical Perspective. Children. 2024;11:51. doi: 10.3390/children11010051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ménière P. Du mariage entre parents, considéré comme cause de la surdimutité congénitale. Gaz. Méd. 1856;3:303–306. [Google Scholar]
- 19.Liebreich R. Abkunft aus Ehen unter Blutsverwandten als Grund von Retinitis Pigmentosa. Deutsche Klinik; Berlin, Germany: 1861. [Google Scholar]
- 20.Boudin J.C.M. Dangers des Unions Consanguines et Nécessité des Croisements dans L’espèce Humaine et Parmi les Animaux. Baillière; Paris, France: 1862. [Google Scholar]
- 21.Knapp H., Moos S. Archiv für Augen und Ohrenheilkunde. Wood; Ney York, NY, USA: 1870. [Google Scholar]
- 22.Hartmann A. Taubstummenheit und Taubstummenbildung nach den Vorhandenen Quellen, Sowie Nach e Igenen Beobochtungen und Erfahrungen. Enke; Stuttgart, Germany: 1880. [Google Scholar]
- 23.Uchermann V. Sordità e Sordomutismo. Ricerche Sperimentali. Versione con Proemio di Giulio Ferrari. Tipografia S. Bernardino; Siena, Italy: 1899. [Google Scholar]
- 24.Schmaltz H. Die Taubstummenim Königreich Sachsen. Breitkopf & Härtel; Leipzig, Germany: 1884. [Google Scholar]
- 25.Wilde W.R.W. Practical Observations on Aural Surgery and the Nature and Treatment of Diseases of the Ear. Churchill; Dublin, Ireland: 1853. [PMC free article] [PubMed] [Google Scholar]
- 26.Lent, Statistik der Taubstummen des Reg-Bez. DuMont Schauberg; Köln, Germany: 1869. [Google Scholar]
- 27.Politzer A. Lehrbuch der Ohrenheilkunde fur Practische Arzte und Studirende. Enke; Stuttgart, Germany: 1882. [Google Scholar]
- 28.Reardon W. Genetic deafness. J. Med. Genet. 1992;29:521–526. doi: 10.1136/jmg.29.8.521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gradenigo G. Sur la pathogénie de l’otite sclérosante et de l’Ankylose stapedio-vestibulaire. Boll. Mal Orecch. 1887;5:136. [Google Scholar]
- 30.Mygind H. Deaf-Mutism. Rebman; London, UK: 1894. [Google Scholar]
- 31.Gradenigo G. Monographies Oto-Rhino-Laryngologiques Internationales. 3, Legrand; Paris, France: 1921. La Surdite Familiale. [Google Scholar]
- 32.Uchermann V. De Dovstumme i Norge. Cammermeyer; Christiana, Norway: 1869. [Google Scholar]
- 33.Von Graefe A. Vereinzelte Beobachtungen und Bemerkungen: Exceptionelles Verhalten des Gesichtfeldes bei Pigmententartung der Netzhaut. Arch. Opthalmol. 1858;4:250–253. [Google Scholar]
- 34.Paget J. Cases of branchial fistulae in the external ears. Med. Chir. Trans. 1878;61:41–50. doi: 10.1177/095952877806100105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pendred V. Deaf-mutism and goitre. Lancet. 1856;2:532. doi: 10.1016/S0140-6736(01)74403-0. [DOI] [Google Scholar]
- 36.Berry G. Note on a congenital defect (coloboma?) of the lower lid. Lond. Ophthalmol. Hosp. Rep. 1899;21:255–257. [Google Scholar]
- 37.Treacher Collins E. Case with symmetrical notches in the outer-part of each lower lid and defective development of the malar bone. Trans. Ophthalmol. Soc. UK. 1990;20:190–192. [Google Scholar]
- 38.Dent C. Case of fragilitas ossium. Trans. Med. Soc. Lond. 1897;20:339–342. [Google Scholar]
- 39.Fisch L. The aetiology of congenital deafness and audiometric patterns. J. Laryngol. Otol. 1955;69:479–493. doi: 10.1017/S0022215100050969. [DOI] [PubMed] [Google Scholar]
- 40.Fraser G. Sensorineural Hearing Loss. Churchill; London, UK: 1970. The causes of profound deafness in childhood; pp. 3–35. [DOI] [PubMed] [Google Scholar]
- 41.Konigsmark B.W. Syndromal approaches to the nosology of hereditary deafness. Birth Defects Orig. Artic. Ser. 1971;7:2–17. [PubMed] [Google Scholar]
- 42.Konigsmark B., Gorlin R. Genetic and Metabolic Deafness. W. B. Saunders Company; Philadelphia, PA, USA: 1976. [Google Scholar]
- 43.McKusick V. Mendelian Inheritance in Man: Catalogs of Autosomal Dominant, Autosomal Recessive and X-Linked Phenotypes. Johns Hopkins University Press; Baltimore, MD, USA: 1966. [Google Scholar]
- 44.McKusick V. Mendelian Inheritance in Man: A Catalog of Human Genes and Genetic Disorders. Johns Hopkins University Press; Baltimore, MD, USA: 1994. [Google Scholar]
- 45.Hamosh A., Scott A.F., Amberger J., Valle D., McKusick V.A. Online Mendelian Inheritance in Man (OMIM) Hum. Mutat. 2000;15:57–61. doi: 10.1002/(SICI)1098-1004(200001)15:1<57::AID-HUMU12>3.0.CO;2-G. [DOI] [PubMed] [Google Scholar]
- 46.Brunner H.G., van Bennekom C.A., Lambermon E., Oei T.L., Cremers C.W.R.J., Wieringa B., Ropers H.-H. The gene for X-linked progressive mixed deafness with perilymphatic gusher during stapes surgery (DFN3) is linked to PGK. Qual. Life Res. 1988;80:337–340. doi: 10.1007/BF00273647. [DOI] [PubMed] [Google Scholar]
- 47.Wallis C., Ballo R., Wallis G., Beighton P., Goldblatt J. X-linked mixed deafness with stapes fixation in a Mauritian kindred: Linkage to Xq probe pDP34. Genomics. 1988;3:299–301. doi: 10.1016/0888-7543(88)90119-X. [DOI] [PubMed] [Google Scholar]
- 48.De Kok Y.J., van der Maarel S.M., Bitner-Glindzicz M., Huber I., Monaco A.P., Malcolm S., Pembrey M.E., Ropers H.H., Cremers F.P. Association between X-linked mixed deafness and mutations in the POU domain gene POU3F4. Science. 1995;267:685–688. doi: 10.1126/science.7839145. [DOI] [PubMed] [Google Scholar]
- 49.Leon P.E., Raventos H., Lynch E., Morrow J., King M.-C. The gene for an inherited form of deafness maps to chromosome 5q31. Proc. Natl. Acad. Sci. USA. 1992;89:5181–5184. doi: 10.1073/pnas.89.11.5181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lynch E.D., Lee M.K., Morrow J.E., Welcsh P.L., León P.E., King M.-C. Nonsyndromic Deafness DFNA1 Associated with Mutation of a Human Homolog of the Drosophila Gene diaphanous. Science. 1997;278:1315–1318. doi: 10.1126/science.278.5341.1315. [DOI] [PubMed] [Google Scholar]
- 51.Guilford P., Ben Arab S., Blanchard S., Levilliers J., Weissenbach J., Belkahia A., Petit C. A non–syndromic form of neurosensory, recessive deafness maps to the pericentromeric region of chromosome 13q. Nat. Genet. 1994;6:24–28. doi: 10.1038/ng0194-24. [DOI] [PubMed] [Google Scholar]
- 52.Kelsell D.P., Dunlop J., Stevens H.P., Lench N., Liang J.N., Parry G., Mueller R.F., Leigh I.M. Connexin 26 mutations in hereditary non-syndromic sensorineural deafness. Nat. Cell Biol. 1997;387:80–83. doi: 10.1038/387080a0. [DOI] [PubMed] [Google Scholar]
- 53.Online Mendelian Inheritance in Man, OMIM®; McKusick-Nathans Institute of Genetic Medicine, Johns Hopkins University: Baltimore, MD, USA. [(accessed on 1 January 2024)]. Available online: http://omim.org.
- 54.Waddington C.H. The epigenotype. Int. J. Epidemiol. 2012;41:10–13. doi: 10.1093/ije/dyr184. [DOI] [PubMed] [Google Scholar]
- 55.Dupont C., Armant D.R., Brenner C.A. Epigenetics: Definition, mechanisms and clinical perspective. Semin. Reprod. Med. 2009;27:351–357. doi: 10.1055/s-0029-1237423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Watson J.D., Crick F.H.C. Molecular Structure of Nucleic Acids: A Structure for Deoxyribose Nucleic Acid. Nature. 1953;171:737–738. doi: 10.1038/171737a0. [DOI] [PubMed] [Google Scholar]
- 57.Nanney D.L. Epigenetic control systems. Proc. Natl. Acad. Sci. USA. 1958;44:712–717. doi: 10.1073/pnas.44.7.712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Deans C., Maggert K.A. What Do You Mean, “Epigenetic”? Genetics. 2015;199:887–896. doi: 10.1534/genetics.114.173492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Henikoff S., Matzke M. Exploring and explaining epigenetic effects. Trends Genet. 1997;13:293–295. doi: 10.1016/S0168-9525(97)01219-5. [DOI] [PubMed] [Google Scholar]
- 60.Egger G., Liang G., Aparicio A., Jones P. Epigenetics in human disease and prospects for epigenetic therapy. Nature. 2004;429:457–463. doi: 10.1038/nature02625. [DOI] [PubMed] [Google Scholar]
- 61.Gemmati D., Longo G., Gallo I., Silva J.A., Secchiero P., Zauli G., Hanau S., Passaro A., Pellegatti P., Pizzicotti S., et al. Host genetics impact on SARS-CoV-2 vaccine-induced immunoglobulin levels and dynamics: The role of TP53, ABO, APOE, ACE2, HLA-A, and CRP genes. Front. Genet. 2022;13:1028081. doi: 10.3389/fgene.2022.1028081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Boison D., Rho J.M. Epigenetics and epilepsy prevention: The therapeutic potential of adenosine and metabolic therapies. Neuropharm. 2020;167:107741. doi: 10.1016/j.neuropharm.2019.107741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Tisato V., Zauli G., Rimondi E., Gianesini S., Brunelli L., Menegatti E., Zamboni P., Secchiero P. Inhibitory effect of natural anti-inflammatory compounds on cytokines released by chronic venous disease patient-derived endothelial cells. Mediat. Inflamm. 2013;2013:423407. doi: 10.1155/2013/423407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Obri A., Serra D., Herrero L., Mera P. The role of epigenetics in the development of obesity. Biochem. Pharmacol. 2020;177:113973. doi: 10.1016/j.bcp.2020.113973. [DOI] [PubMed] [Google Scholar]
- 65.Shamsi M.B., Firoz A.S., Imam S.N., Alzaman N., Samman M.A. Epigenetics of human diseases and scope in future therapeutics. J. Taibah. Univ. Med. Sci. 2017;12:205–211. doi: 10.1016/j.jtumed.2017.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Davis K.N., Qu P.P., Ma S., Lin L., Plastini M., Dahl N., Plazzi G., Pizza F., O’Hara R., Wong W.H., et al. Mutations in human DNA methyltransferase DNMT1 induce specific genome-wide epigenomic and transcriptomic changes in neurodevelopment. Hum. Mol. Genet. 2023;17:3105–3120. doi: 10.1093/hmg/ddad123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Riccardi V.M. Cell--cell interaction as an epigenetic determinant in the expression of mutant neural crest cells. Birth Defects Orig. Artic. Ser. 1979;15:89–98. [PubMed] [Google Scholar]
- 68.Xiao Y., Li D. The role of epigenetic modifications in sensory hair cell development, survival, and regulation. Front. Cell. Neurosci. 2023;14:1210279. doi: 10.3389/fncel.2023.1210279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Nguyen J.D., Llamas J., Shi T., Crump J.G., Groves A.K., Segil N. DNA methylation in the mouse cochlea promotes maturation of supporting cells and contributes to the failure of hair cell regeneration. Proc. Natl. Acad. Sci. USA. 2023;15:e2300839120. doi: 10.1073/pnas.2300839120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Zou S., Zheng Q., Sun Y., Fu X., Zhou W., He Z. Editorial: Hearing loss: From pathogenesis to treatment, volume II. Front. Cell. Neurosci. 2023;23:1309592. doi: 10.3389/fncel.2023.1309592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Tisato V., Castiglione A., Ciorba A., Aimoni C., Silva J.A., Gallo I., D’Aversa E., Salvatori F., Bianchini C., Pelucchi S., et al. LINE-1 global DNA methylation, iron homeostasis genes, sex and age in sudden sensorineural hearing loss (SSNHL) Hum. Genom. 2023;14:112. doi: 10.1186/s40246-023-00562-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Gemmati D., Tisato V. Chapter 15—Genetics and epigenetics of the one-carbon metabolism pathway in autism spectrum disorder: Role of a sex-specific brain epigenome. In: Legato M.J., Feldberg D., Glezerman M., editors. Sex, Gender, and Epigenetics. Academic Press; Cambridge, UK: 2023. pp. 181–191. [Google Scholar]
- 73.Gemmati D., Tisato V. Principles of Gender-Specific Medicine. Academic Press; Cambridge, UK: 2023. Chapter 24—Genomic and epigenomic signature at the branch-point among genome, phenome, and sexome in health and disease: A multiomics approach; pp. 393–408. [Google Scholar]
- 74.Tisato V., Silva J.A., Longo G., Gallo I., Singh A.V., Milani D., Gemmati D. Genetics and epigenetics of one-carbon metabolism pathway in autism spectrum disorder: A sex-specific brain epigenome? Genes. 2021;12:782. doi: 10.3390/genes12050782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Zhou Q., Xiong Y., Qu B., Bao A., Zhang Y. DNA methylation and recurrent pregnancy loss: A mysterious compass? Front. Immunol. 2021;12:738962. doi: 10.3389/fimmu.2021.738962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Gemmati D., Tognazzo S., Serino M.L., Fogato L., Carandina S., De Palma M., Izzo M., De Mattei M., Ongaro A., Scapoli G.L., et al. Factor XIII V34L polymorphism modulates the risk of chronic venous leg ulcer progression and extension. Wound Repair. Regen. 2004;12:512–517. doi: 10.1111/j.1067-1927.2004.012503.x. [DOI] [PubMed] [Google Scholar]
- 77.Seker Yildiz K., Durmus K., Donmez G., Arslan S., Altuntas E.E. Studying the association between sudden hearing loss and DNA N-methyltransferase 1 (DNMT1) genetic polymorphism. J. Int. Adv. Otol. 2017;13:313–317. doi: 10.5152/iao.2017.2723. [DOI] [PubMed] [Google Scholar]
- 78.Ma P.W., Wang W.L., Chen J.W., Yuan H., Lu P.H., Gao W., Ding X.-R., Lun Y.-Q., Liang R., He Z.-H., et al. Treatment with the ferroptosis inhibitor ferrostatin-1 attenuates noise-induced hearing loss by suppressing ferroptosis and apoptosis. Oxid. Med. Cell. Longev. 2022;2022:3373828. doi: 10.1155/2022/3373828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Gemmati D., Castiglione A., Vigliano M., Ciorba A., Aimoni C. Handbook of Hearing Disorders Research. Nova Science Publishers; New York, NY, USA: 2015. Sudden sensorineural hearing loss and polymorphisms in iron homeostasis genes; pp. 77–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Wilson B.S., Tucci D.L., Moses D.A., Chang E.F., Young N.M., Zeng F.-G., Lesica N.A., Bur A.M., Kavookjian H., Mussatto C., et al. Harnessing the Power of Artificial Intelligence in Otolaryngology and the Communication Sciences. J. Assoc. Res. Otolaryngol. 2022;23:319–349. doi: 10.1007/s10162-022-00846-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.National Human Genome Research Institute. A Brief Guide to Genomics. [(accessed on 10 January 2024)]; Available online: https://www.genome.gov.
- 82.Cho S.H., Yun Y., Lee D.H., Cha J.H., Lee S.M., Lee J., Suh M.H., Lee J.H., Oh S.H., Park M.K., et al. Novel autosomal dominant TMC1 variants linked to hearing loss: Insight into protein-lipid interactions. BMC Med. Genom. 2023;16:320. doi: 10.1186/s12920-023-01766-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Sethukumar P., Mandavia R., Yildirim O., Hazell G., Devakumar H., Ahmed M., Stragier E., Duran M.J., Schilder A.G.M., Mehta N. Cataloging Existing Hearing Loss Cohort Data to Guide the Development of Precision Medicine for Sensorineural Hearing Loss: A Systematic Review of Hearing Repositories. J. Int. Adv. Otol. 2023;19:420–425. doi: 10.5152/iao.2023.22690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Liu X., Wen J., Liu X., Chen A., Li S., Liu J., Sun J., Gong W., Kang X., Feng Z., et al. Gene regulation analysis of patient-derived iPSCs and its CRISPR-corrected control provides a new tool for studying perturbations of ELMOD3 c.512A>G mutation during the development of inherited hearing loss. PLoS ONE. 2023;18:e0288640. doi: 10.1371/journal.pone.0288640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Azaiez H., Booth K.T., Ephraim S.S., Crone B., Black-Ziegelbein E.A., Marini R.J., Shearer A.E., Sloan-Heggen C.M., Kolbe D., Casavant T., et al. Genomic Landscape and Mutational Signatures of Deafness-Associated Genes. Am. J. Hum. Genet. 2018;103:484–497. doi: 10.1016/j.ajhg.2018.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Hahn R., Avraham K.B. Gene Therapy for Inherited Hearing Loss: Updates and Remaining Challenges. Audiol. Res. 2023;13:952–966. doi: 10.3390/audiolres13060083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Wilkins M.R., Sanchez J.C., Gooley A.A., Appel R.D., Humphery-Smith I., Hochstrasser D.F., Williams K.L. Progress with proteome projects: Why all proteins expressed by a genome should be identified and how to do it. Biotechnol. Genet. Eng. Rev. 1996;13:19–50. doi: 10.1080/02648725.1996.10647923. [DOI] [PubMed] [Google Scholar]
- 88.Thalmann I. Proteomics and the inner ear. Dis. Markers. 2001;17:476738. doi: 10.1155/2001/476738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Jamesdaniel S., Salvi R., Coling D. Auditory proteomics: Methods, accomplishments and challenges. Brain Res. 2009;1277:24–36. doi: 10.1016/j.brainres.2009.02.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Chance M.R., Chang J., Liu S., Gokulrangan G., Chen D.H., Lindsay A., Geng R., Zheng Q.Y., Alagramam K. Proteomics, bioinformatics and targeted gene expression analysis reveals up-regulation of cochlin and identifies other potential biomarkers in the mouse model for deafness in Usher syndrome type 1F. Hum. Mol. Genet. 2010;19:1515–1527. doi: 10.1093/hmg/ddq025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Dossena S., Nofziger C., Lang F., Valenti G., Paulmichl M. The ESF meeting on “The proteomics, epigenetics and pharmacogenetics of pendrin”. Cell. Physiol. Biochem. 2011;28:377–784. doi: 10.1159/000335101. [DOI] [PubMed] [Google Scholar]
- 92.Mateo Sánchez S., Freeman S.D., Delacroix L., Malgrange B. The role of post-translational modifications in hearing and deafness. Cell. Mol. Life Sci. 2016;73:3521–3533. doi: 10.1007/s00018-016-2257-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Zheng Q.Y., Rozanas C.R., Thalmann I., Chance M.R., Alagramam K.N. Inner ear proteomics of mouse models for deafness, a discovery strategy. Brain Res. 2006;1091:113–121. doi: 10.1016/j.brainres.2006.02.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Cepeda A.P., Ninov M., Neef J., Parfentev I., Kusch K., Reisinger E., Jahn R., Moser T., Urlaub H. Proteomic analysis reveals the composition of glutamatergic organelles of auditory inner hair cell. Mol. Cell. Proteom. 2023;23:100704. doi: 10.1016/j.mcpro.2023.100704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Street K., Risso D., Fletcher R.B., Das D., Ngai J., Yosef N., Purdom E., Dudoit S. Slingshot: Cell lineage and pseudotime inference for single-cell transcriptomics. BMC Genom. 2018;19:477. doi: 10.1186/s12864-018-4772-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Ma X., Guo J., Tian M., Fu Y., Jiang P., Zhang Y., Chai R. Advance and Application of Single-cell Transcriptomics in Auditory Research. Neurosci. Bull. 2023 doi: 10.1007/s12264-023-01149-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Malesci R., Lombardi M., Abenante V., Fratestefano F., Del Vecchio V., Fetoni A.R., Troisi J. A Systematic Review on Metabolomics Analysis in Hearing Impairment: Is It a Possible Tool in Understanding Auditory Pathologies? Int. J. Mol. Sci. 2023;24:15188. doi: 10.3390/ijms242015188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Wang X., Gao Y., Jiang R. Diagnostic and Predictive Values of Serum Metabolic Profiles in Sudden Sensorineural Hearing Loss Patients. Front. Mol. Biosci. 2022;9:982561. doi: 10.3389/fmolb.2022.982561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Miao L., Zhang J., Yin L., Pu Y. Metabolomics Analysis Reveals Alterations in Cochlear Metabolic Profiling in Mice with Noise-Induced Hearing Loss. BioMed. Res. Int. 2022;2022:9548316. doi: 10.1155/2022/9548316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Pierre P.V., Haglöf J., Linder B., Engskog M.K.R., Arvidsson T., Pettersson C., Fransson A., Laurell G. Cisplatin-Induced Metabolome Changes in Serum: An Experimental Approach to Identify Markers for Ototoxicity. Acta. Oto-Laryngol. 2017;137:1024–1030. doi: 10.1080/00016489.2017.1325006. [DOI] [PubMed] [Google Scholar]
- 101.Ishibashi R., Hirayama K., Watanabe S., Okano K., Kuroda Y., Baba Y., Kanayama T., Ito C., Kasahara K., Aiba S., et al. Imeglimin-mediated glycemic control in maternally inherited deafness and diabetes. Diabetes Investig. 2023;14:1419–1422. doi: 10.1111/jdi.14085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Vila-Sanjurjo A., Mallo N., Atkins J.F., Elson J.L., Smith P.M. Our current understanding of the toxicity of altered mito-ribosomal fidelity during mitochondrial protein synthesis: What can it tell us about human disease? Front. Physiol. 2023;14:1082953. doi: 10.3389/fphys.2023.1082953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Matsuo Y., LeCun Y., Sahani M., Precup D., Silver D., Sugiyama M., Uchibe E., Morimoto J. Deep learning, reinforcement learning, and world models. Neural. Netw. 2022;152:267–275. doi: 10.1016/j.neunet.2022.03.037. [DOI] [PubMed] [Google Scholar]
- 104.Huang X., Tang F., Hua Y., Li X. In silico prediction of drug-induced ototoxicity using machine learning and deep learning methods. Chem. Biol. Drug. Des. 2021;98:248–257. doi: 10.1111/cbdd.13894. [DOI] [PubMed] [Google Scholar]
- 105.Liu X., Teng L., Zuo W., Zhong S., Xu Y., Sun J. Deafness gene screening based on a multilevel cascaded BPNN model. BMC Bioinform. 2023;24:56. doi: 10.1186/s12859-023-05182-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Jin F.Q., Huang O., Kleindienst Robler S., Morton S., Platt A., Egger J.R., Emmett S.D., Palmeri M.L. A Hybrid Deep Learning Approach to Identify Preventable Childhood Hearing Loss. Ear Heart. 2023;44:1262–1270. doi: 10.1097/AUD.0000000000001380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Parton B.S. Sign language recognition and translation: A multidisciplined approach from the field of artificial intelligence. J. Deaf. Stud. Deaf. Educ. 2006;11:94–101. doi: 10.1093/deafed/enj003. [DOI] [PubMed] [Google Scholar]
- 108.Wen F., Zhang Z., He T., Lee C. AI enabled sign language recognition and VR space bidirectional communication using triboelectric smart glove. Nat. Commun. 2021;12:5378. doi: 10.1038/s41467-021-25637-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Lin B., Ma Y., Wu S. Multi-Omics and Artificial Intelligence-Guided Data Integration in Chronic Liver Disease: Prospects and Challenges for Precision Medicine. OMICS. 2022;26:415–421. doi: 10.1089/omi.2022.0079. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing not applicable.


