Abstract
We aimed to assess the prognostic role of the neutrophil/lymphocyte ratio (NLR) in community-acquired pneumonia (CAP) via a single-center retrospective cohort of hospitalized adult patients from 1/2009 to 12/2019. Patients were dichotomized into lower NLR (≤12) and higher NLR (>12). The primary outcome was mortality. ICU admission and hospital- and ICU-free days were secondary outcomes. The pneumonia severity index (PSI) and the NLR’s ability to predict outcomes was also tested. An NLR ≤12 was observed in 2513 (62.2%) patients and >12 in 1526 (37.8%). After adjusting for PSI, the NLR was not associated with hospital mortality (odds ratio [OR] 1.115; 95% confidence interval [CI] 0.774, 1.606; p = 0.559), but it was associated with a higher risk of ICU admission (OR 1.405; 95% CI 1.216, 1.624; p < 0.001). The PSI demonstrated acceptable discrimination for mortality (area under the receiver operating characteristic curve [AUC] 0.78; 95% CI 0.75, 0.82) which was not improved by adding the NLR (AUC 0.78; 95% CI 0.75, 0.82, p = 0.4476). The PSI’s performance in predicting ICU admission was also acceptable (AUC 0.75; 95% CI 0.74, 0.77) and improved by including the NLR (AUC 0.76, 95% CI 0.74, 0.77, p = 0.008), although with limited clinical significance. The NLR was not superior to the PSI for predicting mortality in hospitalized CAP patients.
Keywords: community-acquired pneumonia, CAP, neutrophil/lymphocyte ratio, NLR, mortality, prognostication
1. Introduction
Community-acquired pneumonia (CAP) is an acute infection of the lung parenchyma and one of the leading causes of hospitalization and mortality in the United States [1], with more than 1.5 million annual hospitalizations and about 100,000 deaths [2]. Risk stratification and prognostication provide useful information on the disease trajectory and guide management [3]. Although several prognostic tools for CAP have been evaluated, the pneumonia severity index (PSI), Confusion, Uremia, Respiratory rate, Blood pressure, being 65 years of age and older (CURB-65), and the ATS/IDSA are the most validated and remain commonly used in CAP, with satisfactory outcomes [4,5,6]. Evaluations of the prognostic value of biomarkers like NT-pro-BNP [7], C-reactive protein, and procalcitonin have been less satisfactory when used individually [8]. The neutrophil/lymphocyte ratio (NLR) (the ratio of absolute neutrophil count to absolute lymphocyte count), is an easily measurable index that is receiving growing interest as a useful prognostic biomarker in several stressful conditions including infections. In CAP, multiple studies have shown conflicting results on the prognostic value of the NLR alone or in addition to clinical severity scores [7,9,10,11,12]. The addition of the NLR to the PSI and CURB-65 in one study did not improve the prediction of mortality [12]. More recently, a systematic review demonstrated a comparable prognostic value of the NLR to the PSI, CURB-65, CRP, procalcitonin, neutrophil count, lymphocyte count, and white blood cell count [13]. However, only a few studies in the systematic review confirmed an association between the NLR and adverse outcomes utilizing a multivariate analysis, thus resulting in limited consideration of confounding factors on mortality. Also, most studies focused on mortality only as an outcome, with minimal evaluation of other clinical outcomes including need for invasive and non-invasive mechanical support and admission to the intensive care unit (ICU). Further, most studies were limited by sample size.
The aim of this study was to evaluate the prognostic value of the NLR in predicting the clinical outcomes of patients who are hospitalized with CAP.
2. Materials and Methods
The institutional review board (IRB) at the Mayo Clinic approved this research as low-risk, denoted by the IRB number 17-011140, with a waiver of the requirement for written informed consent.
2.1. Design, Setting, and Participants
This study had a retrospective cohort design. All adult patients admitted to the Mayo Clinic in Rochester, Minnesota, between January 2009 and December 2019 who had community-acquired pneumonia (CAP) underwent screening. The presence of CAP was determined using International Classification of Diseases 9 (481–486) and 10 (J13, J15, and J18) codes, coupled with note searches. Community-acquired pneumonia was defined as an acute infection of the lung parenchyma exhibiting clinical symptoms (cough, fever, pleuritic chest pain, and dyspnea) and a new radiographic infiltrate not being acquired in the hospital or healthcare setting [14].
The exclusion criteria were:
-
-
The absence of Minnesota research authorization;
-
-
Baseline conditions of human immune deficiency virus infection, interstitial lung disease, leukopenia, or neutropenia;
-
-
Diagnoses of hospital-acquired pneumonia, ventilator-associated pneumonia, or aspiration pneumonia;
-
-
Readmissions (only the earliest admission during the study period was included per individual);
-
-
Hospital stays under 24 h;
-
-
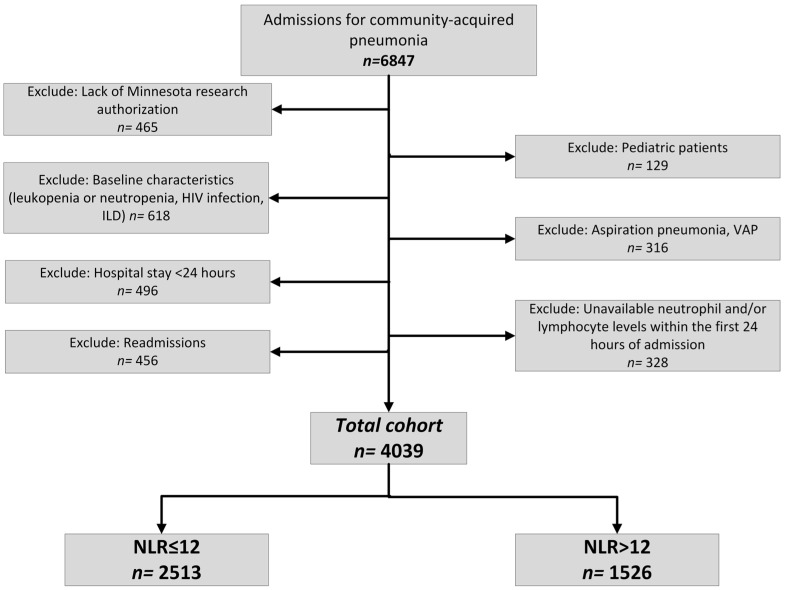
The absence of neutrophil or lymphocyte levels within the initial 24 h of admission (Figure 1).
Figure 1.
Flowchart of the identification of the patients in neutrophil/lymphocyte ratio analyses. HIV: human immunodeficiency virus, ILD: interstitial lung disease, NLR: neutrophil/lymphocyte ratio, VAP: ventilator-associated pneumonia.
2.2. Variable Definitions
The data were extracted by the Anesthesia Clinical Research Unit team using standardized and validated queries [15,16,17]. Extracted data included relevant demographic information, comorbidities (recorded as the presence of individual comorbidities alongside the Charlson Comorbidity Index [CCI]) [18], and disease severity indexes, evaluated via clinical scores. The medication exposure evaluation was limited to corticosteroids and vasopressors.
The white blood cell count, which measures the total number of leukocytes, is recorded as 109/L in our institution, with the institutional normal falling between 3.4 and 9.6 × 109/L. As per the differential components, the normal ranges for neutrophil and lymphocyte counts are considered to be 1.56 to 6.45 × 109/L and 0.95 to 3.07 × 109/L, respectively. Neutrophil and lymphocyte levels tested during the first 24 h of admission (the first one available if more than one result was available during the timeline) were recorded as continuous variables and used to calculate the neutrophil/lymphocyte ratio (NLR). Based on the literature, an a priori NLR cut-off of 12 was chosen (patients were compared as those whose NLR level was ≤12 vs. those >12) [13].
2.3. Outcomes
Primary outcomes included mortality during hospitalization and within six months of admission. Secondary outcomes encompassed the need for invasive and non-invasive mechanical ventilation (IMV) (NIMV), intensive care unit (ICU) admission, and hospital- and ICU-free days, calculated as days alive spent outside of the hospital or the ICU, respectively, within 28 days of admission, resulting in 0 for patients who died during the stay or had a length of stay of ≥28 days [19]. In a similar fashion, IMV-free days were also calculated and evaluated. The prediction of in-hospital mortality and the requirement for ICU admission using PSI-only and PSI combined with NLR were also calculated.
2.4. Statistical Analysis
The median, interquartile range (IQR) for continuous data and the numbers and frequencies for categorical variables were used to perform and present descriptive summary statistics. The chi-square test was used to examine categorical data, while the Mann–Whitney U test was used to evaluate continuous variables. The NLR ≤ 12 group was used as the reference for comparing the two groups. Results were reported using odds ratios (ORs), p values, estimates, and 95% confidence intervals (CIs). The analyses were adjusted for the baseline conditions and severity of the patients, measured by the PSI score using binary logistic regression and linear regression, depending on the characteristics of the outcomes of interest. As PSI already includes baseline characteristics such as age, gender, and certain comorbid conditions, no additional covariates were deemed necessary for the multivariable calculations comparing the NLR groups.
To better understand NLR’s association with outcomes, the following sensitivity analyses were conducted:
-
-
Evaluating the impact of increasing NLR as a continuous variable;
-
-
Classifying patients into four categories based on quartiles (quartile [Q] #1 NLR < 5.13, Q #2 NLR ≥ 5.13 and <9.26, Q #3 NLR ≥ 9.26 and <16.35, Q #4 NLR ≥ 16.35; Q #1 was the reference group);
-
-
Limiting the analyses to patients with neutrophilia (defined as having an absolute neutrophil count of >6.45 × 109, the institutional cut-off level);
-
-
Limiting the analyses to patients with lymphopenia (defined as having an absolute lymphocyte count of <0.95 × 109, the institutional cut-off level).
Finally, C-statistics was used to examine the NLR and PSI’s predictive ability for mortality and ICU admission. This included creating a receiver operating characteristic (ROC) curve and determining the area under the curve (AUC), as well as the 95% CI The potential contribution of NLR to the PSI was also evaluated. The ROC curves for both approaches were compared using DeLong’s test [20]. A two-sided p-value of 0.05 was considered significant. IBM SPSS v27.0 (IBM Statistical Package for Social Sciences Statistics for Windows, Armonk, NY, USA) and MedCalc Statistical Software v19.1 (MedCalc Software bv, Ostend, Belgium) were used to perform the calculations.
3. Results
Following the application of exclusion criteria, 4039 patients out of the initial 6847 were included in the cohort (Figure 1).
3.1. Comparison of Patients with an NLR ≤ 12 vs. >12
The primary analysis compared 2513 patients with NLR ≤ 12 and 1526 with NLR > 12. Table 1 illustrates the distribution of baseline characteristics across both groups. Although there were some differences in the distribution of specific comorbidities, the baseline comorbidity burdens were generally well-balanced, as indicated by a comparable CCI (median [IQR] = 7 [5,10] and 7 [5,9] for NLR ≤ 12 and >12 groups, respectively, p = 0.541).
Table 1.
Demographics and clinical characteristics of patients.
| Variables | Total (n = 4039) | NLR ≤ 12 (n = 2513) | NLR > 12 (n = 1526) | p, OR (95% CI) |
|---|---|---|---|---|
| Age, median (IQR) | 78 (65, 88) | 77 (65, 88) | 80 (67, 88) | 0.003 |
| Sex, Male, no. (%) | 2172 (53.8%) | 1293 (51.5%) | 879 (57.6%) | <0.001, 1.28 (1.13, 1.46) |
| Race, no. (%) | 0.038 | |||
| White | 3805 (94.2%) | 2349 (93.5%) | 1456 (95.4%) | |
| Asian | 42 (1.0%) | 31 (1.2%) | 11 (0.7%) | |
| African American | 64 (1.6%) | 50 (2.0%) | 14 (0.9%) | |
| Others | 128 (3.2%) | 83 (3.3%) | 45 (2.9%) | |
| Ethnicity, no. (%) | 0.401 | |||
| Non-Hispanic | 3897 (96.5%) | 2423 (96.4%) | 1474 (96.6%) | |
| Hispanic | 65 (1.6%) | 45 (1.8%) | 20 (1.3%) | |
| Unknown/Other | 77 (1.9%) | 45 (1.8%) | 32 (2.1%) | |
| Comorbidities, no. (%) | ||||
| Congestive heart failure | 1118 (27.7%) | 703 (28.0%) | 415 (27.2%) | 0.592, 0.96 (0.83, 1.11) |
| COPD | 1310 (32.4%) | 740 (29.4%) | 570 (37.4%) | <0.001, 1.43 (1.25, 1.63) |
| Diabetes | 1220 (30.2%) | 790 (31.4%) | 430 (28.2%) | 0.029, 0.86 (0.74, 0.98) |
| Chronic kidney disease | 1159 (28.7%) | 724 (28.8%) | 435 (28.5%) | 0.836, 0.99 (0.86, 1.13) |
| Malignancy | 938 (23.5%) | 576 (22.9%) | 372 (24.4%) | 0.290, 1.08 (0.93, 1.26) |
| Neutrophil/lymphocyte ratio, median, (IQR) | 9.26 (5.13, 16.35) | 6.09 (3.80, 8.67) | 19.71 (14.86, 27.88) | |
| Clinical Severity Scores | ||||
| Pneumonia Severity Index, median (IQR) | 113 (87, 141) | 109 (83, 136) | 119 (93, 148) | <0.001 |
| CURB 65 | 3 (2, 3) | 3 (2, 3) | 3 (2, 4) | <0.001 |
| APACHE III | 65 (52, 80) | 64 (51, 79) | 66 (53, 81) | 0.013 |
| Need for vasopressor during hospitalization, no. (%) | 888 (22.0%) | 512 (20.4%) | 376 (24.6%) | 0.002, 1.28 (1.10, 1.49) |
APACHE: Acute Physiology and Chronic Health Evaluation, CI: confidence interval, COPD: Chronic Obstructive Pulmonary Disease, NLR: neutrophil/lymphocyte ratio, IQR: interquartile range, OR: odds ratio.
Table 2 outlines the distribution of the primary outcomes and the results of the multivariable analysis. The odds of ICU admission were higher in patients with NLR > 12 (n = 710, 46.5%) compared to those with NLR ≤ 12 (n = 869, 34.6%) (adjusted OR [95% CI] = 1.41 [1.22, 1.62]).
Table 2.
Primary and secondary outcomes based on NLR levels.
| Variables | Total (n = 4039) | NLR ≤ 12 (n = 2513) | NLR > 12 (n = 1526) | Univariate Analysis | Multivariate Analysis * | ||
|---|---|---|---|---|---|---|---|
| Odds Ratio (95% CI) | p Value | Odds Ratio (95% CI) | p Value | ||||
| Hospital mortality, no. (%) | 128 (3.2%) | 69 (2.7%) | 59 (3.9%) | 1.43 (1.00, 2.03) | 0.049 | 1.12 (0.77, 1.61) | 0.559 |
| Mortality at 6 months, no. (%) | 638 (15.8%) | 375 (14.9%) | 263 (%17.2) | 1.19 (1.00, 1.41) | 0.051 | 0.99 (0.83, 1.19) | 0.923 |
| Need for invasive mechanical ventilation, no. (%) | 704 (17.4%) | 406 (16.2%) | 298 (19.5%) | 1.26 (1.07, 1.49) | 0.006 | 1.08 (0.91,1.28) | 0.395 |
| Need for invasive and non-invasive mechanical ventilation, no. (%) | 1348 (33.4%) | 789 (31.4%) | 559 (36.6%) | 1.26 (1.11, 1.44) | <0.001 | 1.08 (0.93,1.24) | 0.312 |
| ICU admission | 1579 (39.1%) | 869 (34.6%) | 710 (46.5%) | 1.65 (1.45, 1.87) | <0.001 | 1.41 (1.22, 1.62) | <0.001 |
| p value | Estimate (95% CI) | p value | |||||
| Hospital-free days, median (IQR) | 24.01 (21.04, 25.44) | 24.13 (21.38, 25.65) | 23.78 (20.23, 25.29) | <0.001 | −0.34 (−0.72, 0.04) | 0.081 | |
| Invasive ventilator-free days, median (IQR) | 26.29 (23.67, 27.27) | 26.19 (23.19, 27.28) | 26.40 (23.97, 27.19) | 0.510 | 0.96 (−0.31, 2.23) | 0.139 | |
CI: confidence interval, ICU: intensive care unit, IQR: interquartile range, NLR: neutrophil/lymphocyte ratio. * Data were analyzed using multivariable regression models adjusting for pneumonia severity index. NLR ≤ 12 was the reference.
3.2. Sensitivity Analyses
3.2.1. Evaluation of the Impact of the NLR as a Continuous Variable
Upon analyzing the relationship between an increasing NLR and various outcomes without categorization, we observed a rise in the odds of both hospital mortality and ICU admission as the NLR increased (adjusted OR [95% CI] = 1.01 [1.00, 1.02], p = 0.047 and adjusted OR [95% CI] = 1.02 [1.01, 1.02], p < 0.001 for hospital mortality and ICU admission, respectively). Additionally, higher NLR levels were associated with a significant decrease in the number of hospital-free days (adjusted estimate [95% CI] = −0.02 [−0.04, −0.01]). Although univariate analyses suggested a significant association between the NLR and mortality within six months after admission, as well as the need for mechanical ventilation, these associations did not remain significant after adjusting for the PSI (adjusted OR [95% CI] = 1.0 [1.0, 1.01], p = 0.693 and adjusted OR [95% CI] = 1.0 [1.0, 1.01], p = 0.198 for mortality at six months and the requirement for mechanical ventilation, respectively).
3.2.2. Four-Group Comparison Based on NLR Quartiles
Supplementary Table S1 and Table 3 illustrate the distribution of baseline characteristics and outcomes among the four groups of patients based on NLR levels. Similar to the primary analyses, the need for ICU admission was significantly different in patients belonging to Q#3 (n = 405, 40.1%) and Q#4 (n = 492 (48.7%) compared to Q#1 (n = 319, 31.6%) (adjusted OR [95% CI] = 1.38 [1.16, 1.69] and 1.64 [1.34, 2.01] for Q#3 and Q#4, respectively).
Table 3.
Primary and secondary outcomes of patients according to their neutrophil/lymphocyte ratio levels *.
| Variables | Quartile #1 (n = 1010) | Quartile #2 (n = 1010) | Quartile #3 (n = 1009) | Quartile #4 (n = 1010) | Univariable Analysis | Multivariable Analysis ** | ||
|---|---|---|---|---|---|---|---|---|
| p Value | Odds Ratio (95% CI) | p Value | ||||||
| Hospital mortality, no. (%) | 24 (2.4) | 27 (2.7) | 34 (3.4) | 43 (4.3) | 0.075 | Q#2 | 1.09 (0.62, 1.93) | 0.763 |
| Q#3 | 1.3 (0.76, 2.23) | 0.343 | ||||||
| Q#4 | 1.28 (0.76, 2.16) | 0.352 | ||||||
| Mortality at 6 months, no. (%) | 162 (16) | 144 (14.3) | 152 (15.1) | 180 (17.8) | 0.147 | Q#2 | 0.83 (0.64, 1.07) | 0.149 |
| Q#3 | 0.84 (0.66, 1.08) | 0.185 | ||||||
| Q#4 | 0.86 (0.68, 1.1) | 0.238 | ||||||
| Need for invasive mechanical ventilation, no. (%) | 152 (15) | 165 (16.3) | 185 (18.3) | 202 (20) | 0.018 | Q#2 | 1.07 (0.84, 1.37) | 0.581 |
| Q#3 | 1.19 (0.93, 1.51) | 0.164 | ||||||
| Q#4 | 1.12 (0.88, 1.43) | 0.341 | ||||||
| Need for invasive and non-invasive mechanical ventilation, no. (%) | 300 (29.7) | 324 (32.1) | 346 (34.3) | 378 (37.4) | 0.002 | Q#2 | 1.08 (0.89, 1.32) | 0.422 |
| Q#3 | 1.15 (0.95, 1.4) | 0.158 | ||||||
| Q#4 | 1.12 (0.92, 1.37) | 0.254 | ||||||
| ICU admission | 319 (31.6) | 363 (35.9) | 405 (40.1) | 492 (48.7) | <0.001 | Q#2 | 1.19 (0.97, 1.46) | 0.090 |
| Q#3 | 1.38 (1.13, 1.69) | 0.002 | ||||||
| Q#4 | 1.64 (1.34, 2.01) | <0.001 | ||||||
| p value | Estimate (95% CI) | p value | ||||||
| Hospital-free days, median (IQR) | 24.3 (22.06, 25.88) | 24.01 (21.12, 25.48) | 23.98 (21, 25.41) | 23.55 (19.96, 25.23) | <0.001 | Q#2 | −0.41 (−0.93, 0.11) | 0.120 |
| Q#3 | −0.43 (−0.95, 0.09) | 0.104 | ||||||
| Q#4 | −0.63 (−1.15, −0.11) | 0.017 | ||||||
CI: confidence interval, ICU: intensive care unit, IQR: interquartile range, Q: quartile. * Neutrophil-lymphocyte ratio levels per quartiles: Quartile #1, <5.13; Quartile #2, ≥5.13 and <9.26; Quartile #3, ≥9.26 and <16.35; Quartile #4, ≥16.35. ** Data were analyzed using multivariable regression models adjusting for pneumonia severity index. Quartile #1 was the reference.
3.2.3. Analysis among Patients with Neutrophilia
Supplementary Tables S2 and S3 depict the distribution of baseline characteristics and outcomes for the comparative analysis among the 2989 patients with neutrophilia.
3.2.4. Analysis among Patients with Lymphopenia
Supplementary Tables S4 and S5 showcase the distribution of baseline characteristics and outcomes for the comparative analysis among the 1905 patients with lymphopenia.
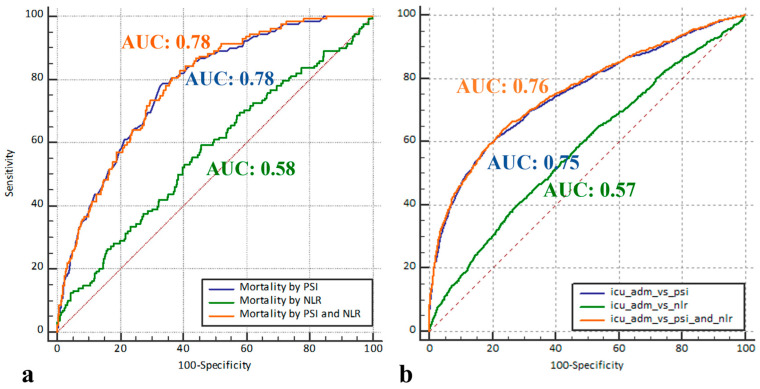
3.3. Discriminatory Performance
Supplementary Table S6 presents the distribution of baseline characteristics between patients who died during their hospital stay and those who were discharged alive. The distinguishing capacity of the NLR for patients who died during hospitalization was poor (AUC [95% CI] = 0.57 [0.52, 0.62]). The discriminatory capacity of the PSI for patients who died during hospitalization was acceptable (AUC [95% CI] = 0.78 [0.75, 0.82]) and did not considerably improve with the addition of the NLR (AUC [95% CI] = 0.78 [0.75, 0.82]) (Figure 2a), with a negligible difference between the AUC for PSI versus PSI and NLR of 0.0025 (95% CI: −0.0039, 0.0089, p = 448).
Figure 2.
Receiver operating characteristic curves for pneumonia severity index (PSI) only, neutrophil/lymphocyte ratio (NLR) only, and PSI combined with NLR in detecting (a) in-hospital mortality (the area under the receiver operating characteristic curve (AUC) was 0.78 (95% CI, 0.75–0.82) for PSI only and PSI combined with NLR approaches, while it was 0.57 (95% CI, 0.52–0.62) for NLR only) and (b) the requirement for intensive care unit admission (the AUC was 0.75 (95% CI, 0.74–0.77), 0.58 (95% CI, 0.56–0.6), and 0.76 (95% CI: 0.74–0.77) for PSI only, NLR only, and PSI combined with NLR, respectively). ICU: intensive care unit.
The discriminatory capacity of the NLR for patients requiring an ICU admission was poor (AUC [95% CI] = 0.58 [0.56, 0.6]). The distinguishing capacity of the PSI for patients requiring an ICU stay was acceptable (AUC [95% CI] = 0.75 [0.74, 0.77]) and significantly improved with the addition of the NLR (AUC [95% CI] = 0.76 [0.74, 0.77]) (Figure 2b), with a difference between the AUC for PSI versus PSI and NLR of 0.0041 (95% CI: 0.001, 0.007, p = 0.008).
4. Discussion
In this large single-center retrospective cohort of hospitalized patients with community-acquired pneumonia, we found that a higher NLR (>12) was not associated with an increased odds for in-hospital mortality and 6-month mortality. Notably, there was a significant difference in the severity of illness as measured by the PSI, CURB-65, and APACHE III scores between the subgroups (NLR ≤ 12 and >12), and a significant association with mortality following univariate analysis. However, after adjusting for baseline comorbid conditions and the severity of illness using the PSI, the association between a higher NLR and mortality became insignificant. Additional adjusted analysis with the NLR as a continuous variable revealed a barely significant association between the NLR and in-hospital mortality. On assessment of secondary outcomes, a higher NLR was only found to be associated with an increased odds of ICU admission in this cohort, while no association was observed with other secondary outcomes including the need for invasive and non-invasive mechanical ventilation. Further adjusted analysis with the NLR as a continuous variable also revealed a significant association with ICU admission and hospital-free days, but no association with other secondary outcomes. These findings were consistent on additional sensitivity analysis evaluating outcomes in NLR quartiles, with an increasing odds of ICU admission in the third and fourth quartiles. Interestingly, the increased odds of ICU admission were only observed in the subset of patients with a high NLR and co-existing lymphopenia compared to patients with concomitant neutrophilia. Additionally, an increased odds for a need of both invasive and non-invasive mechanical ventilation were noted in this lymphopenic subgroup. Potential explanations include the presence of other confounding factors like the increasing use of non-invasive mechanical support for high-risk extubation patients such as COPD. Finally, in this cohort, the discriminatory capacity of the NLR in predicting both mortality and ICU admission was inferior to the PSI. Moreover, the addition of the NLR to the PSI did not improve the prediction of the mortality model. The improvement with the addition of the NLR to the PSI for predicting ICU admission, albeit statistically significant, was very small and not clinically meaningful.
The utility of the NLR in predicting adverse outcomes in CAP has been previously reported in other studies [7,8,10,11,21,22]. However, these studies reported conflicting results and were limited by sample size. Further, only a few studies confirmed an association between the NLR and mortality by multivariate analysis. In a recent systematic review of nine studies (n = 3340), the association between a higher NLR and mortality was observed to be significant. An NLR cut-off value >10 in this systematic review was found to predict mortality compared to the PSI, CURB-65, and other biomarkers including C-reactive protein, lymphocytes, neutrophils, and WBC [13]. A higher sensitivity and specificity were observed at a cut-off value between 11.2 and 13.4. In contrast, our results demonstrated a barely significant association between an elevated NLR and mortality, and also a poor discriminatory ability of the NLR in predicting mortality compared to the PSI. Although the results of a retrospective study by Postma et al., the largest study included in the systematic review (n = 1549), reported a significant association between the NLR and mortality based on bivariate analysis, this was absent in the subsequent multivariate analysis. In addition, the lack of improvement in the PSI model with the addition of the NLR, as seen in our study, was similarly observed in the large study by Postma et al. [12]. Therefore, our result in this larger cohort further limits the clinical applicability of utilizing the NLR as a prognostic tool for mortality, alone or in combination with severity scores, in CAP. Further studies, including prospective studies and an updated systematic review will be needed.
In comparison with other prior studies evaluating the prognostic value of the NLR in CAP, our study further found a significant association between the NLR and need for ICU admission, an important outcome that is rarely assessed. In addition, other outcomes, including the need for mechanical ventilation, hospital-free days, and ventilator-free days, were all assessed. Moreover, our study explored the outcomes in subset of patients with neutrophilia versus lymphopenia, with significant associations observed in the lymphopenia group.
The strengths of our study compared to prior similar studies include the large sample size (the largest sample size to our knowledge), the multivariable analysis adjusting for the severity of illness and comorbidities, the exploration of other clinical outcomes in addition to mortality, and the sensitivity analysis evaluating specific subgroups. As this was a single-center cohort study, findings reported are reflective of characteristics observed in a large academic center. Other limitations include the potential bias existing within the dataset, missing data, the lack of microbiological data, and other unmeasured confounders.
5. Conclusions
In this study, the neutrophil/lymphocyte ratio was not superior to the pneumonia severity index for predicting in-hospital mortality in patients who were hospitalized with community-acquired pneumonia. This limits its applicability as a prognostic enrichment tool, but additional studies are needed for assessing its use as a predictive enrichment tool.
Supplementary Materials
The following supporting information can be downloaded at https://www.mdpi.com/article/10.3390/biomedicines12020260/s1: Table S1: Demographics and clinical characteristics of patients according to their neutrophil/lymphocyte ratio levels; Table S2: Demographics and clinical characteristics of patients who had neutrophilia; Table S3: Primary and secondary outcomes of patients who had neutrophilia based on NLR; Table S4: Demographics and clinical characteristics of patients who had lymphopenia; Table S5: Primary and secondary outcomes of patients who had lymphopenia based on NLR; Table S6: Demographics and clinical characteristics of patients according to their in-hospital mortality status.
Author Contributions
Conceptualization, A.T., F.W.W., O.G. and Y.E.O.; methodology, A.T. and Y.E.O.; software, A.T.; validation, A.T. and Y.E.O.; formal analysis, A.T.; investigation, A.T. and Y.E.O.; resources, A.T., O.G. and Y.E.O.; data curation, Y.E.O.; writing—original draft preparation, A.T. and F.W.W.; writing—review and editing, O.G. and Y.E.O.; visualization, A.T.; supervision, O.G. and Y.E.O.; funding acquisition, Y.E.O. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The institutional review board (IRB) at the Mayo Clinic approved this research as low-risk, denoted by the IRB number 17-011140, approval date: 20 December 2017, with a waiver of the requirement for written informed consent.
Informed Consent Statement
Patient consent was waived due to the study being conducted on deidentified retrospective data.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author, A.T., upon reasonable request.
Conflicts of Interest
The authors declare no conflicts of interest.
Funding Statement
This research was supported by the National Institute of Health, grant number K23HL168212; the Robert D. and Patricia E. Kern Center for the Science of Health Care Delivery, Mayo Clinic; and the Robert A. Winn Diversity in Clinical Trials Career Development Award.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Hayes B.H., Haberling D.L., Kennedy J.L., Varma J.K., Fry A.M., Vora N.M. Burden of pneumonia-associated hospitalizations: United States, 2001–2014. Chest. 2018;153:427–437. doi: 10.1016/j.chest.2017.09.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ramírez P., Ferrer M., Martí V., Reyes S., Martínez R., Menéndez R., Ewig S., Torres A. Inflammatory biomarkers and prediction for intensive care unit admission in severe community-acquired pneumonia. Crit. Care Med. 2011;39:2211–2217. doi: 10.1097/CCM.0b013e3182257445. [DOI] [PubMed] [Google Scholar]
- 3.Moons K.G., Altman D.G., Vergouwe Y., Royston P. Prognosis and prognostic research: Application and impact of prognostic models in clinical practice. BMJ. 2009;338:b606. doi: 10.1136/bmj.b606. [DOI] [PubMed] [Google Scholar]
- 4.Aujesky D., Fine M.J. The pneumonia severity index: A decade after the initial derivation and validation. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2008;47((Suppl. S3)):S133–S139. doi: 10.1086/591394. [DOI] [PubMed] [Google Scholar]
- 5.Mandell L.A., Wunderink R.G., Anzueto A., Bartlett J.G., Campbell G.D., Dean N.C., Dowell S.F., File T.M., Jr., Musher D.M., Niederman M.S., et al. Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2007;44((Suppl. S2)):S27–S72. doi: 10.1086/511159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ewig S., Ruiz M., Mensa J., Marcos M.A., Martinez J.A., Arancibia F., Niederman M.S., Torres A. Severe community-acquired pneumonia. Assessment of severity criteria. Am. J. Respir. Crit. Care Med. 1998;158:1102–1108. doi: 10.1164/ajrccm.158.4.9803114. [DOI] [PubMed] [Google Scholar]
- 7.Ozmen I., Karakurt Z., Salturk C., Kargin F., Takir H.B., Aksoy E., Sari R., Celik E., Tuncay E.A., Yildirim E., et al. Can N-terminal pro B-type natriuretic peptide, neutrophil-to-lymphocyte ratio, C-reactive protein help to predict short and long term mortality? Bratisl. Lek. Listy. 2016;117:587–594. doi: 10.4149/BLL_2016_114. [DOI] [PubMed] [Google Scholar]
- 8.Yang T., Wan C., Wang H., Qin J., Chen L., Shen Y., Wen F. The prognostic and risk-stratified value of neutrophil–lymphocyte count ratio in Chinese patients with community-acquired pneumonia. Eur. J. Inflamm. 2017;15:22–27. doi: 10.1177/1721727X17702150. [DOI] [Google Scholar]
- 9.Kaya Y., Taş N., Çanakçı E., Cebeci Z., Özbilen M., Keskin H., Yıldırım B.B. Relationship of neutrophil-to-lymphocyte ratio with presence and severity of pneumonia. J. Clin. Anal. Med. 2018;9:452–457. [Google Scholar]
- 10.de Jager C.P., Wever P.C., Gemen E.F., Kusters R., van Gageldonk-Lafeber A.B., van der Poll T., Laheij R.J. The neutrophil-lymphocyte count ratio in patients with community-acquired pneumonia. PLoS ONE. 2012;7:e46561. doi: 10.1371/journal.pone.0046561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cataudella E., Giraffa C.M., Di Marca S., Pulvirenti A., Alaimo S., Pisano M., Terranova V., Corriere T., Ronsisvalle M.L., Di Quattro R., et al. Neutrophil-To-Lymphocyte Ratio: An Emerging Marker Predicting Prognosis in Elderly Adults with Community-Acquired Pneumonia. J. Am. Geriatr. Soc. 2017;65:1796–1801. doi: 10.1111/jgs.14894. [DOI] [PubMed] [Google Scholar]
- 12.Postma D.F., van Werkhoven C.H., Schuurman J., van Elden L.J., Oosterheert J.J., Bonten M.J. Prognostic value of the neutrophil/lymphocyte ratio in patients hospitalized with community-acquired pneumonia. Adults. 2016:155. [Google Scholar]
- 13.Kuikel S., Pathak N., Poudel S., Thapa S., Bhattarai S.L., Chaudhary G., Pandey K.R. Neutrophil-lymphocyte ratio as a predictor of adverse outcome in patients with community-acquired pneumonia: A systematic review. Health Sci. Rep. 2022;5:e630. doi: 10.1002/hsr2.630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Odeyemi Y.E., Lal A., Barreto E.F., LeMahieu A.M., Yadav H., Gajic O., Schulte P. Early machine learning prediction of hospitalized patients at low risk of respiratory deterioration or mortality in community-acquired pneumonia: Derivation and validation of a multivariable model. Biomol. Biomed. 2023 doi: 10.17305/bb.2023.9754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Herasevich V., Kor D.J., Li M., Pickering B.W. ICU data mart: A non-iT approach. A team of clinicians, researchers and informatics personnel at the Mayo Clinic have taken a homegrown approach to building an ICU data mart. Health. Inf. 2011;28:42–45. [PubMed] [Google Scholar]
- 16.Clinic M. Mayo Data Explorer. 2021. [Google Scholar]
- 17.Clinic M. Advanced Text Explorer. 2021. [Google Scholar]
- 18.Charlson M.E., Pompei P., Ales K.L., MacKenzie C.R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic. Dis. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 19.Schoenfeld D.A., Bernard G.R. Statistical evaluation of ventilator-free days as an efficacy measure in clinical trials of treatments for acute respiratory distress syndrome. Crit. Care Med. 2002;30:1772–1777. doi: 10.1097/00003246-200208000-00016. [DOI] [PubMed] [Google Scholar]
- 20.DeLong E.R., DeLong D.M., Clarke-Pearson D.L. Comparing the areas under two or more correlated receiver operating characteristic curves: A nonparametric approach. Biometrics. 1988;44:837–845. doi: 10.2307/2531595. [DOI] [PubMed] [Google Scholar]
- 21.Avci S., Perincek G. The alveolar-arterial gradient, pneumonia severity scores and inflammatory markers to predict 30-day mortality in pneumonia. Am. J. Emerg. Med. 2020;38:1796–1801. doi: 10.1016/j.ajem.2020.05.048. [DOI] [PubMed] [Google Scholar]
- 22.Curbelo J., Luquero Bueno S., Galván-Román J.M., Ortega-Gómez M., Rajas O., Fernández-Jiménez G., Vega-Piris L., Rodríguez-Salvanes F., Arnalich B., Díaz A., et al. Inflammation biomarkers in blood as mortality predictors in community-acquired pneumonia admitted patients: Importance of comparison with neutrophil count percentage or neutrophil-lymphocyte ratio. PLoS ONE. 2017;12:e0173947. doi: 10.1371/journal.pone.0173947. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are available from the corresponding author, A.T., upon reasonable request.