Abstract
Introduction
Medication inventory management and error prevention are complex issues. Single interventions are insufficient to make improvement across the spectrum. A uniform system for dispensing and distributing medications can help reduce the risk of medication errors, improve efficiency, and minimize waste. This quality improvement project aims to: 1) decrease – the time from ordering medication to administration, including delay incidents, by > 70%; and 2) decrease the inpatient monthly total medication consumption by > 20% and ward medication stock items by > 70%, including decreasing returned items and loss from in-house expired medications by > 70%.
Methods
A Six-Sigma approach was applied to eliminate deficiencies throughout the medication management process. Failure mode effect analysis and staff surveys were used to evaluate implementation of automated dispensing cabinet (ADCs) and reengineered workflows for expensive, misused, and restricted medications.
Results
After the new processes were implemented, the turnaround time from ordering medication to administration was reduced by 83%, with zero delay incidents reported. Most nurses (64%) and pharmacists (67%) stated that implementation of ADCs increased their productivity by more than 40%. Monthly medication consumption was reduced by 24%, with an estimated annual saving of $4,100,000 USD. The number of returned items per month was reduced by 72%, and the estimated annual savings from loss of in-house expired medications was $750,000 USD.
Conclusions
This quality improvement project positively impacted stock control while reducing costs and turnaround time for inpatient medication dispensing. Medication delay incidents were reduced, and staff satisfaction levels were positive. Next steps are to reengineer narcotic, anesthesia, and refrigerated products’ management.
Keywords: Waste, inventory, medication error, Six-Sigma, FMEA, automation-satisfaction, safety, automated dispensing cabinets
INTRODUCTION
Delays in medication availability to the patient have been identified as a substantial component of medication error overall with the United States National Coordinating Council for Medication Error Reporting and Prevention, relating such events to procedures and systems, including prescribing, order communication, dispensing, and distribution.[1] Many studies have attempted to evaluate initiatives that include improving direct clinician-to-clinician communication for stat doses,[2[ electronic prescribing,[3] and clinical dashboards with visual indicators for overdue doses.[4]
Automation of the medication management process with more centralized control over the dispensing and distribution process has been suggested as having a positive impact on overall time required for medication delivery and management,[5] with the caveat that robust integration of prescribing, electronic medication administration records, and dispensing hardware and software must be planned to maintain patient safety[6] and to optimize the workflow down to administration and replenishment.[5,7–10]
In the literature, nursing responses to automation of medication management have been generally positive, with one study showing statements such as “I now spend less time waiting for medications that come from the pharmacy than before the automated dispensing cabinet (ADC) was implemented” scoring well in surveys.[10] In a Qatar hospital study[11], similar positive responses were found, with 87% of nurses agreeing that they were able to administer medication more efficiently with the ADC and a 91% overall satisfaction rate for ADC use.
Waste minimization can help with maintaining supply.[12] According to West et al[13], “medication wastage refers to any medication which expires or remains unused throughout the whole medicines supply chain (and) also refers to the unnecessary or inappropriate consumption of medications by patients, or the unjustified non-adherence to treatment guidelines by healthcare professionals.”
In terms of the cost of transitioning to an automated medication management process, Berdot et al[14] reported that initial costs have to be built into budget impact plans, and there is a fairly immediate return on investment from “gains in preparation time and fewer medication process errors. Detectability of medication errors is extremely difficult, and a baseline rate for error in traditional systems is hard to estimate. Reduction of medication error following implementation of ADCs has been reported to as 19% in the absence of effective integration with electronic prescribing systems and 50% or higher otherwise.[15–18]
METHODS
No formal consent was required from the ethics committee of the hospital. The project was approved by the hospital director. All patient data are automatically scrubbed from the metrics available in the Knowledge Portal.
Baseline Assessment
A failure mode effect analysis (FMEA) was performed for the existing medication management system in December 2019 and was extended into the period of introducing ADCs to allow for mitigation of identified risks that were carried forward into the new system and to allow for identification of new possible failure-modes related to the introduction of automation. This approach help identify where future improvement measures would need to be established, and risk priority numbers (RPNs) were calculated for the medication chain from central pharmacy through to the patient’s bedside. RPNs greater than 100 were considered for immediate remediation.19
Flow charts, Ishikawa fishbone diagrams, and root-cause analyses were used to explore issues of long turnaround times for inpatient medication dispensing (i.e., approximately 170 minutes [range: 140–210 mins]). These incidents included delayed dose administration versus facility targets for stat and routine orders of 30 minutes and less than 1 hour, respectively; medication unavailability requiring phone calls to the pharmacy; and workaround overstocking of nursing units, leading to medication wastage through use of expired, inappropriate, and uncounted medications.
A study of nursing unit waiting times for medications was undertaken with a Pareto 80/20 analysis to identify where the project might best be applied during the pilot stage. This gave eight units to be targeted: pediatrics, neonatal intensive care (NICU), two medical wards, general intensive care (ICU), emergency department (ED), pediatric intensive care, and the transplant unit. The final selection of the General ICU for pilot testing was based on patient acuity, time criticality for medication delivery, the requirement for constant bedside nursing presence and the Pareto analysis.
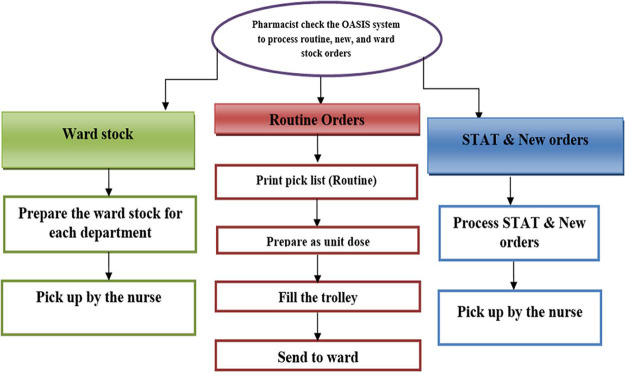
Pre-Automation Workflow
The pre-automation workflow is described in Figure 1. This workflow relies heavily on manual distribution systems, including traditional floor stock and medication carts (patient-specific medications in individual patient cassettes). The floor stock system is flexible, but the pharmacy has little control over inventory. A 24-hour unit-dose cart exchange system allows tighter inventory control than relying on whole-container floor stock, but there are limitations based on capacity for the central pharmacy to create and pick unit doses.20 Stat and new orders also require a nurse to visit the pharmacy, adding further potential delays for these medications. A major concern with this workflow included unregulated “borrowing” of patient-specific medications for other patients’ use.
Figure 1.
Overview of pre-automation workflow.
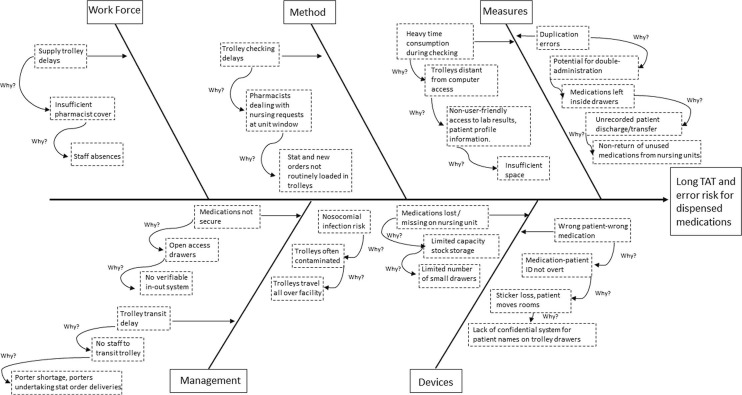
The Ishikawa diagram shows how the environment and information technology (IT) infrastructure made it difficult to ensure that medications were consistently dispensed with proper verification (Fig. 2). Floor stock medications were dispensed without being linked to a particular patient profile, making it extremely difficult to track use and misuse of medications (including allergy supervision and detection of errors and near misses). A lack of medication tracking through the organization led to understocking and overstocking, missing or inaccurate medication charges, and complicated manual documentation procedures. Substantial amounts of unit-dose medications were returned to the pharmacy from nursing units because medications were discontinued or patients were transferred and discharged. In nursing units, limited space within medication trolleys caused workarounds including dispensed medications to be stored on top of trolleys, with potential for mixing with other patients’ medications. The trolleys were not secure, and “whole package” quantities of medications (i.e., greater than that required for the prescribed medication regimen) were dispensed. This contributed to unused high-value medications being destroyed when returned to the pharmacy due to the lack of an efficient process for restocking them.
Figure 2.
Ishikawa fishbone diagram of the inpatient dispensing process pre automation. TAT: turnaround time.
Intervention
We recognized that a uniform system for dispensing and distributing medications would help reduce the risk of medication administration errors. The hospital’s existing process is to dispense medications in the “most ready-to-administer form possible” to minimize opportunities for error during distribution and administration. This becomes crucial during emergent situations and may also decrease the risk of incorrect dosing (i.e., the units dispensed are either the correct total dose or an uncomplicated multiple of the prescribed dose).
The Ishikawa exercise made it clear that no single intervention would overcome all the problems in our medication chain. It was also clear that coordination with nursing, logistics, transport, IT, and medical staff was required for implementation of the planned interventions. The Lean Six-Sigma approach of Define-Measure-Analyze-Improve-Control (DMAIC) method was used because it focuses on eliminating defects (time, motion, and cost) throughout a process such as medication management. Processes introduced into the manufacturing industry in the 1980s have been adapted by healthcare to emphasize preventive error reduction, which aligns with FMEA and root-cause analysis of near-misses and actual incidents.[21] The fundamentals of DMAIC and FEMA for healthcare projects are well documented.[22–25]
Specific Aims
Beginning in January 2020, the planned interventions included:
Installation of ADCs;
Change in management of expensive and frequently misused medications; and
Implementation of a secondary approval process for restricted medications.
Primary aims by end of 2021 include:
Decrease turnaround time from ordering to administration of regular and stat medications by more than 70% (later, these would be patient-specific regular orders and stat orders, neither would be ADC stock items);
Decrease inpatient monthly medication consumption by more than 20%;
Decrease number of ward stock items by more than 70%;
Decrease number of returned items by more than 70%;
Decrease loss due to expired medications in both the central pharmacy and warehouse by more than 70%; and
Decrease number of delayed stat and regular prescription medication incidents to zero.
Secondary aims by end of 2021 include:
Improve percentage of effectively answered medication-related calls from nursing units handled by the pharmacy by more than 70%;
Monitor nursing and pharmacy staff satisfaction with the new medication management processes; and
Support acceptance and assurance with the solution through training and acting promptly on feedback.
Introduction of Automated Dispensing Cabinets (ADCs)
ADCs can provide secure medication storage on patient care units,10 enhance the efficiency of medication distribution, provide immediate access to medications, and reduce medication-dispensing errors.15 They also allow for more complete control of total in-facility medication stock by the pharmacy department.14
BD Pyxis MedStation ES ADCs were integrated to the facility’s Computerized Provider Order Entry (CPOE) system. The ADC installation plan used biometric-secured access (end-user fingerprint) with scheduled refills by the pharmacy department, with all dispensing and administration being linked to patient profiles. Knowledge Portal reports were used for monitoring the effectiveness of selected par levels of medications, via nursing overrides of profiles to obtain medications when facing stock-out situations, and to help identify potential medication diversion.
ADC single-access drawers and cubies allowed tighter control of medication withdrawal, the separation of Lookalike Soundalike (LASA) medications from each other, and the isolation of high-alert medications. ADC inventory management was devolved from pharmacists to pharmacy technicians. Pharmacists reviewed and checked each patient’s medication profile for appropriateness, potential medication interactions, allergies, and against patient laboratory results. Medications were sent to the nursing unit in their most ready-to-administer form, such as unit-dose packages, and oral syringes for liquid medications, both for dose control and to reduce waste of bulky items that could not be stored in the ADC.
Expensive and commonly misused medications were identified during planning, and during implementation these medications were secured via dispensing access being restricted to two senior pharmacists. Second approval for restricted medications was introduced via the CPOE and approved by the Pharmacy and Therapeutics Committee; restrictions were based on physician specialty, clinical indication, and medication cost.
Access to ADCs for both refilling and for administration was based on the completion of training delivered exclusively by authorized Pharmacy Informatics and Automation service trainers as per American Society of Hospital Pharmacists guidelines.26 Training covered (1) how to create orders, dispense, and return medications; and (2) how to enter expiry dates, assign and load medications, and create a picklist and delivery report. An ADC Support Team of trained pharmacy staff was created to resolve day-to-day problems and queries. Software, hardware, and interface issues were escalated to the Pharmacy Informatics and Automation Team.
As the project expanded across the selected nursing units there were issues of day-case and ED patients not appearing in the system; the ADC vendor had to be contacted to expand the integration of the ADCs with the Admission Discharge and Transfer system.
Another systemic issue was encountered during the later integration of the dialysis unit. As patients were being effectively discharged after each dialysis session, all “inpatient” medications were being removed from the ADC, and physicians were required to order discharge medications as a separate action. This was resolved by modification of the system, with an option for these regularly returning patients of “discharge with medications,” which automatically extends inpatient medications to outpatient status.
Data Analysis
Data were collected over a protracted period because the performance of medical devices and automation commonly lags in performance as the human agents learn to work with automation and the system is optimized to meet the organization’s demands.27 We anticipated an upturn in delayed medications followed by a downward trend as pharmacists and nurses “learned the system.”28 For this reason, most data were interpreted in time-sequence graphs to examine variation at an aggregate level and to allow for an overlay of linear trends.
RPN scores and staff surveys were used to evaluate the new processes at 3 months and during the project’s roll out. Turnaround time for non-ADC stat and routine medication orders were taken from ADC and non-ADC nursing units and amalgamated monthly.
The most complex aspect of data discovery was ascertaining the bound stock and waste per annum pre ADC, as manual inventory was time-consuming and possibly inaccurate. The process of converting each nursing unit one by one helped in this process, as an audit could be undertaken in each area as medications were transferred from floor stock in cupboards to the ADCs, and expired medications were removed. In this way an ongoing tally could be kept that more accurately assessed total bound stock pre-automation. Consumption of expensive and commonly misused medications was also calculated.
Telephone calls to all inpatient pharmacy lines received and answered or not answered were monitored by the IT department, before and during the project. Although we knew this would not directly reflect medication supply issues per se, as there are other telephone queries, we felt that as the bulk of calls to the department were supply related, and that any reduction in the volume of such calls would increase the likelihood of positively answered calls overall, this was an acceptable measure for the impact of ADC introduction, as we hoped to increase medication lines available in the nursing units and monitor stock successfully.
RESULTS
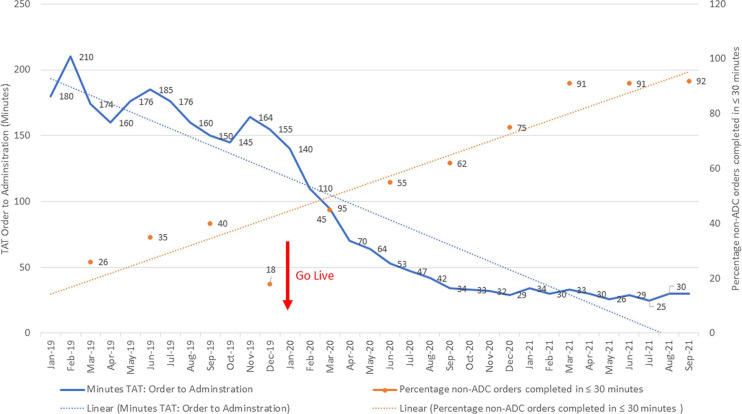
The top five RPN scores from the pre-intervention FEMA are shown in Table 1. All primary aims were met and went beyond the original targets. Medication turnaround time from order to administration was reduced by 83% with zero delay incidents reported. (See Fig. 3).
Table 1.
Top five RPN scoring activities in the inpatient pharmacy before introducing ADCs, with pre- and post-intervention scores
| Activity | Integrate pharmacy formulary–monitoring system | Order verification and approval | Emergency situation | Out of stock in nursing units for individual medications | LASA medication error |
|---|---|---|---|---|---|
| Potential failures | |||||
| Failure of integration | Physicians create incomplete order | Delay in unit receiving medication in acute situation | Medication administration delay | Incorrect selection of medication by administrating nurse | |
| Potential effects | |||||
| No control of process | Process of approval delayed | Failure to treat emergent patient event correctly | Failure of therapy | Incorrect medication may reach the patient | |
| Potential causes | |||||
| Unable to integrate | Physician unavailable to correct order | Nurses have to wait for pharmacy approvals and delivery of medications | Inventory miscount, pharmacy miss refill cycle Medication placed in wrong location | Wrong medication stocked or selected | |
| Current controls | |||||
| None | None | None | Manual reporting | LASA medications separated in pharmacy and inpatient units | |
| Pre-Intervention Scoresa | |||||
| Severity | 8 | 9 | 10 | 7 | 10 |
| Occurrence | 10 | 10 | 5 | 5 | 10 |
| Detection | 5 | 8 | 10 | 10 | 9 |
| RPN 1 score | 400 | 720 | 500 | 350 | 900 |
| Corrective actions undertaken | |||||
| Integrate ADCs with pharmacy formulary–monitoring system | CPOE alert screen for physician to complete entry | ADC override function allows staff to remove certain medications from the ADC prior to approvals of pharmacy | Scheduling refills with internal pharmacy timetabling Barcode scanning of all medications for unit vs. pharmacy dynamic inventory | Avoid placing LASA medications in matrix drawers in the ADC Use ADC modular “cubies” to isolate medications within the ADC. Barcode scanning of medications upon withdrawal for administration as confirmatory step Clinical advisory for user for LASA medications on ADC | |
| Action owner | |||||
| Pharmacy and ICT Team | Pharmacy and ICT Team | Pharmacy and ICT Team | Pharmacy | Pharmacy and nursing units | |
| Post-Intervention Scoresa | |||||
| Severity | 8 | 9 | 10 | 7 | 5 |
| Occurrence | 3 | 1 | 1 | 2 | 1 |
| Detection | 5 | 5 | 1 | 10 | 1 |
| RPN 2 score | 120 | 45 | 10 | 140 | 5 |
RPN score can range from 0-1000. It is calculated as a product of likely severity (scale of 0-10, where 0 is unlikely and 10 is likely to cause death or severe harm), likely occurrence (scale of 0-10, where 0 is almost never and 10 is extremely frequent), and difficulty of detection (scale of 0-10, where 0 is fully and immediately detectable and 10 is undetectable at point of care).
ADC: automated dispensing cabinet; CPOE: Computerized Provider Order Entry; ICT: Information and Communication Technology; LASA: Lookalike Soundalike; RPN: risk priority number.
Figure 3.
Average TAT from ordering to administration for non-ADC items: stat and patient-specific regular orders, with corresponding non-ADC items dispensed within 30 minutes. ADC: automated dispensing cabinet; TAT: turnaround time.
In terms of our primary aims:
Monthly medication consumption was reduced by 24%.
Overall, medication held as ward stock was reduced by 81%.
The number of returned items per month was reduced by 72%.
The estimated annual cost saving from total expired medications (floor, inpatient pharmacy, and warehouse stock) was approximately $750,000 USD, a 57% reduction. This gave a substantial estimated annual saving of ≈ $4,100,000 USD.
Reported medication delay incidents for both routine and stat orders fell from 7 to 0 by August 2020.
For our secondary aims we found that:
The number of successfully processed telephone calls to the pharmacy improved by 160% by mid-2021. This was primarily due to a substantial reduction in “missing medication” calls.
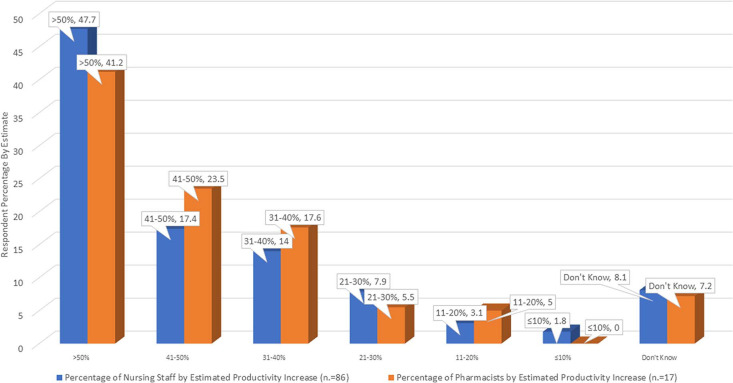
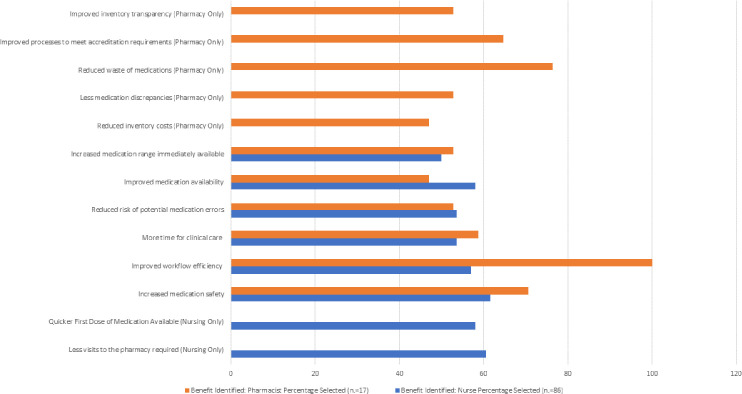
64% of nurses and 67% of pharmacists stated that ADC introduction increased their productivity by > 40%. (See Fig. 4).
Workflow efficiency was the highest scoring item of the benefits of automation for pharmacy staff. Nursing staff scored medication safety as the most important benefit (see Fig. 5).
The nursing and pharmacist surveys showed good internal consistency, and reliability for the applied scale (Cronbach alpha for all items, 0.9709; range, 0.9625–0.9744).
Figure 4.
Estimates of productivity increase post ADC implementation by discipline. ADC, automated dispensing cabinet.
Figure 5.
Key benefits experienced from using ADCs by discipline: “All that Apply” selected. ADC: automated dispensing cabinet.
DISCUSSION
Change is not always successful and sometimes difficult to measure. We feel that we have managed, in a unique way, to triangulate the question of the project’s success or failure with definitive cost and product savings, safety measures including RPN, and with a comprehensive satisfaction survey across the two key disciplines in medication management: pharmacy and nursing. To our knowledge, this theoretical framework for monitoring the effectiveness of a change process for inpatient medication management, and the degree of triangulation of the central issues of waste, safety, and efficiency that it creates, has not been previously applied.
The growing body of evidence on ADCs that are integrated into pharmacy stock management systems largely mirrors our experience. At the outset of the project, we selected metrics to indicate successful change (i.e., reduced turnaround time or cost savings targets) rather than established metrics (e.g., reducing RPN by half through each cycle of change29 and establishing a downward trend for stock-outs and overrides30). Setting 70% reduction in turnaround time as a target was derived from pre-automation data, where we found a mean average time of 170 minutes (range, 140–210). The initial target of 50 minutes or less for each transaction, with a stretch target of 30 minutes or less, was set as an achievable goal to put us en route to our final target of 30 minutes or less. As the results show, we achieved an 83% reduction, with almost all transactions taking 30 minutes or less within 14 months of introducing the ADCs.
The decision on what to set for achievable cost reduction was also set, in retrospect, somewhat conservatively. We suggest that the question of bound stock within an organization—and therefore vulnerable to expiry loss, overordering, and apparent loss—is highly variable between facilities and is related to issues of transparency of stock, inventory constraints, and infrastructure. Conversations with peers at other facilities indicated that the wastage from stock totally from incorrect use, expiry, and other losses could be as high as 80%. Although this information was anecdotal, it was drawn from experienced pharmacists. An expectation of 70% reduction was therefore applied to the number of ward stock items, returned items, and for loss due to expired medications in both the central pharmacy and warehouse.
There was anticipation that savings in medication and costs would be achieved, but the team and the organization were surprised by the volume of medications expiring in the pre-change system. As discussed earlier, ascertaining the bound stock and waste per annum pre ADC was time-consuming, and possibly inaccurate. The process of auditing each nursing unit one by one had not been done before, so a lot of discovery occurred during this stringent process. As discussed above, we had set out our targets for cost-savings based on the organization’s wider goals of budget control across the facility and through conversations with our peers from other facilities who commonly gave us anecdotal but well-informed estimates of medication loss from expiry. Our cost savings of 57% per annum from total expired medications was substantial. One study published after our project was completed of central pharmacy automation in an outpatient department in Saudi Arabia reported an even more substantial reduction in waste, though this was limited to a subset of medications rather than a full inventory assessment.31 We showed a monthly medication consumption reduction of 24%, and a reduction of bound wards stock of 81%. The societal costs of unused, or inappropriately dispensed or used, medications include harm to social healthcare budgets and have an environmental opportunity cost in the raw materials and resources used in the production of pharmaceuticals.
Limitations
Narcotics and fridge items were excluded from the study owing to local regulations and lack of integration with refrigerators. The operating room (OR) was excluded owing to differing medication management needs, and the NICU was excluded as it was undergoing renovation. We believe the findings of the study are broadly applicable to the NICU, but the OR will require more specialist medication dispensing units. Local regulations for narcotic management are changing quickly.
A more extensive overhaul of the system could have been undertaken, but our budget horizons are necessarily limited, and the savings in medication costs and the ability for our plan to be modular (with hardware being firmware-updatable and capable of further integration) means we are in a reasonable position for further expansion.
The project was undertaken partly during the 2019 coronavirus disease (COVID-19) pandemic, which was disruptive to the organization and may have slowed the improvements in turnaround time (the slope in turnaround time reduction does not follow the linear trend established between January and March 2020). The average patient census of the hospital remained largely unchanged, but several units received higher acuity nonroutine patients and changed their role.
Although it can be difficult to validate surveys, we were able to structure the tool’s responses in such a way that its internal consistency could be tested. The sample size was representative.
CONCLUSIONS
Addressing harm related to patient safety caused by medication delay is one of the key factors likely to improve medication distribution and improve patient experiences. The fact that medication costs are rising at a fast rate means that projects such as ours should be supported by organizations for tertiary healthcare delivery to be sustainable.
The potential for automation to improve safety and efficiency in the outpatient setting, by adapting the lessons of inpatient change processes such as our Six-Sigma project, has been seen in some other recent regional studies.31,32 A systematic approach to medication cost containment necessitates specific and extensive data on medication procurement, actual medication usage, and waste trends in healthcare systems. Any projects looking at system change in medication management need to evidence change through accurate quantitative data. Traditional inventory systems cannot achieve this.
The particular strengths of the project are that the transparency and dynamic inventory achieved through automation8 allowed for calculation of return on investment, which quantitatively strengthened the case for further conversion to automation and workflow reworks in budget impact meetings.18 The largely positive responses to the staff survey indicate that sustainability is likely to be achieved, as a key reason for the success or failure of automation in healthcare is the degree of successful integration with human systems.5,10,11,15,28,31
Footnotes
Source of Support: None. Conflict of Interest: None.
References
- 1.National Coordinating Council for Medication Error Reporting and Prevention (NCCMERP); About medication errors: what is a medication error?www.nccmerp.org/about-medication-errors Accessed Jan 21, 2023. [Google Scholar]
- 2. Nagar S, Davey N. Reducing avoidable time delays in immediate medication administration—learning from a failed intervention. BMJ Qual Improv Rep. 2015;4:u206468.w2612. doi: 10.1136/bmjquality.u206468.w2612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Matthews P, Wangrangsimakul T, Borthwick M, et al. Electronic prescribing: reducing delay to first dose of antibiotics for patients in intensive care. BMJ Qual Improv Rep. 2013;2:u202241.w1120. doi: 10.1136/bmjquality.u202241.w1120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Coleman J, Hodson J, Brooks HL, Rosser D. Missed medication doses in hospitalised patients: a descriptive account of quality improvement measures and time series analysis Int J Qual Health Care 2013. 25 564–572 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ahtiainen H, Kallio M, Airaksinen M, Holmström A. Safety, time and cost evaluation of automated and semi-automated drug distribution systems in hospitals: a systematic review Eur J Hosp Pharm 2020. 27 253–262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. McCarthy B, Ferker M. Implementation and optimization of automated dispensing cabinet technology Am J Health Syst Pharm 2016. 73 1531–1536 [DOI] [PubMed] [Google Scholar]
- 7. O’Neil D, Miller A, Cronin D, Hatfield C. A comparison of automated dispensing cabinet optimization methods Am J Health Syst Pharm 2016. 73 975–980 [DOI] [PubMed] [Google Scholar]
- 8. Nanni A, Rana T, Schenkat D. Screening for expired medications in automated dispensing cabinets Am J Health Syst Pharm 2020. 77 2107–2111 [DOI] [PubMed] [Google Scholar]
- 9.Institute for Safe Medication Practice; 2019. Guidelines for the Safe Use of Automated Dispensing Cabinets.www.ismp.org/resources/guidelines-safe-use-automated-dispensing-cabinets?check_logged_in=1 Feb 7. Accessed Jan 19, 2023. [Google Scholar]
- 10. Wang Y, Tsan C, Chen M. Implementation of an automated dispensing cabinet system and its impact on drug administration: longitudinal study. JMIR Form Res. 2021;5:e24542. doi: 10.2196/24542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Zaidan M, Rustom F, Kassem N, et al. Nurses’ perceptions of and satisfaction with the use of automated dispensing cabinets at the Heart and Cancer Centers in Qatar: a cross-sectional study. BMC Nurs. 2016;15:4. doi: 10.1186/s12912-015-0121-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Smale E, Egberts T, Heerdink E, et al. Waste-minimising measures to achieve sustainable supply and use of medication In: Sustainable Chemistry and Pharmacy 2021. 20 100400 [Google Scholar]
- 13. West L, Diack L, Cordina M, Stewart D. Applying the Delphi technique to define ‘medication wastage’ Eur J Hosp Pharm 2015. 22 274–279 [Google Scholar]
- 14. Berdot S, Blanc C, Chevalier D, et al. Impact of drug storage systems: a quasi-experimental study with and without an automated-drug dispensing cabinet Int J Qual Health Care 2019. 31 225–230 [DOI] [PubMed] [Google Scholar]
- 15. Cottney A. Improving the safety and efficiency of nurse medication rounds through the introduction of an automated dispensing cabinet. BMJ Qual Improv Rep. 2014;3:u204237.w1843. doi: 10.1136/bmjquality.u204237.w1843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Cheung K, Bouvy M, De Smet P. Medication errors: the importance of safe dispensing Br J Clin Pharmacol 2009. 67 676–680 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Cousein E, Mareville J, Lerooy A, et al. Effect of automated drug distribution systems on medication error rates in a short-stay geriatric unit J Eval Clin Pract 2014. 20 678–684 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Bonnabry P, François O. Return on investment: a practical calculation tool to convince your institution Eur J Hosp Pharm 2020. 27 111–113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Prado-Mel E, Mejías Trueba M, Reyes González I, et al. Failure mode effect analysis for safety improvement in the automatic drug dispensing systems [in Spanish] J Healthc Qual Res 2021. 36 81–90 [DOI] [PubMed] [Google Scholar]
- 20. Svirsko A, Norman B, Hostetler S, Parry B. Optimizing the medication distribution process for inpatient units. J Med Syst. 2022;46:32. doi: 10.1007/s10916-022-01822-2. [DOI] [PubMed] [Google Scholar]
- 21. Niñerola A, Sánchez-Rebull M, Hernández-Lara A. Quality improvement in healthcare: Six Sigma systematic review Health Policy 2020. 124 438–445 [DOI] [PubMed] [Google Scholar]
- 22. DelliFraine J, Wang Z, McCaughey D, et al. The use of six sigma in health care management: are we using it to its full potential? Qual Manag Health Care 2014. 23 240–253 [DOI] [PubMed] [Google Scholar]
- 23. van den Heuvel J, Does RJMM, Bisgaard, S. Dutch hospital implements six sigma Six Sigma Forum Magazine 2005. 11–14 [Google Scholar]
- 24. Bryman A. The research question in social research: what is its role? Int J Soc Res Methodol 2007. 101, 5–20 [Google Scholar]
- 25.Stamatis D. Failure Mode and Effects Analysis: FMEA from Theory to Execution. Milwaukee, WI: ASQC Quality Press; 1995. [Google Scholar]
- 26. Cello R, Conley M, Cooley T, et al. ASHP Guidelines on the Safe Use of Automated Dispensing Cabinets Am J Health Syst Pharm 2022. 79 e71–e82 [DOI] [PubMed] [Google Scholar]
- 27. Tarricone R, Callea G, Ogorevc M, Prevolnik Rupel V. Improving the methods for the economic evaluation of medical devices Health Econ 2017. 26(suppl 1): 70–92 [DOI] [PubMed] [Google Scholar]
- 28. Craswell A, Bennett K, Dalgliesh B, et al. The impact of automated medicine dispensing units on nursing workflow: a cross-sectional study. Int J Nurs Stud. 2020;111:103773. doi: 10.1016/j.ijnurstu.2020.103773. [DOI] [PubMed] [Google Scholar]
- 29.Institute for Healthcare Improvement; Risk Priority Number (from Failure Modes and Effects Analysis) Institute for Healthcare Improvement.www.ihi.org/resources/Pages/Measures/RiskPriorityNumberfromFailureModesandEffectsAnalysis.aspx Accessed Jul 1, 2023. [Google Scholar]
- 30.American Society of Hospital Pharmacists; Practice Resource for Automated Dispensing Cabinet Overrides.www.ashp.org/-/media/assets/pharmacy-practice/resource-centers/patient-safety/patient-safety-practice-resource-for-automated-dispensing-cabinet-overrides.ashx Accessed Jul 1, 2023. [Google Scholar]
- 31. Al Nemari M, Waterson J. The introduction of robotics to an outpatient dispensing and medication management process in Saudi Arabia: retrospective review of a pharmacy-led multidisciplinary Six Sigma performance improvement project. JMIR Hum Factors. 2022;9:e37905. doi: 10.2196/37905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Momattin H, Arafa S, Momattin S, et al. Robotic pharmacy implementation and outcomes in Saudi Arabia: a 21-month usability study. JMIR Hum Factors. 2021;8:e28381. doi: 10.2196/28381. [DOI] [PMC free article] [PubMed] [Google Scholar]