Abstract
We conducted a qualitative content analysis of health science literature (N = 100) involving qualitative interviews or focus groups. Given recent data sharing mandates, our goal was to characterize the nature of relationships between the researchers and participants to inform ethical deliberations regarding qualitative data sharing and secondary analyses. Specifically, some researchers worry that data sharing might harm relationships, while others claim that data cannot be analyzed absent meaningful relationships with participants. We found little evidence of relationship building with participants. The majority of studies involve single encounters (95%), lasting less than 60 min (59%), with less than half of authors involved in primary data collection. Our findings suggest that relationships with participants might not pose a barrier to sharing some qualitative data collected in the health sciences and speak to the feasibility in principle of secondary analyses of these data.
Keywords: qualitative research, health sciences, relationships, data sharing, secondary analysis, research ethics
Background
Qualitative data sharing is rare in the United States (U.S.) (Mozersky et al., 2021; Yoon, 2014). Some countries, such as the UK and Australia, have more established infrastructure and services to support qualitative data sharing, yet overall it remains an uncommon practice (Bishop & Kuula-Luumi, 2017; Broom et al., 2009; Corti et al., 2016; Yardley et al., 2014). Despite this, qualitative researchers will need to prepare for increased qualitative data sharing in light of open science and changing funder and journal requirements (Foster & Deardorff, 2017; McKiernan et al., 2016; National Institutes of Health, 2020). For instance, the National Institutes of Health (NIH), the largest federal funding body of health research in the U.S., issued a new data sharing policy mandating data sharing as of 2023 regardless of whether data are qualitative or quantitative, including data that are not used in final publications (NOT-OD-21–013). The policy requires all NIH-funded investigators to submit Data Management and Sharing Plans to “integrate data sharing into the routine conduct of research” (National Institutes of Health, 2020). While researchers frequently share quantitative data, sharing qualitative data creates concerns and challenges, while bringing potential benefits.
Researchers from many disciplines – including anthropology, sociology, psychology, public health, medicine, nursing, implementation science, and bioethics – conduct qualitative research. There is no single context or discipline that characterizes all qualitative research or all of the possible methods used (i.e. interviews, focus groups, ethnography, participant observation) (Corti & Thompson, 2004). We acknowledge there is tremendous diversity in qualitative researchers’ epistemological and methodological stances. Below we first describe some key concerns and benefits regarding sharing qualitative data in general, followed by our rationale for focusing on the health sciences. This study is part of a larger NIH-funded project [R01HG009351] to develop guidelines for ethical and responsible qualitative data sharing and software to support health science researchers in deidentifying qualitative data (DuBois et al., 2018).
Concerns Regarding Qualitative Data Sharing
Some qualitative researchers have expressed concerns that the very idea of sharing qualitative data in a repository for others to analyze is inconsistent with the goals, purpose, and meaning of qualitative research (Broom et al., 2009). Within some qualitative approaches, such as ethnography, a key distinction is that these qualitative methods involve interactions and exchanges between participants and researchers – creating a relationship based on genuine rapport and closeness - which allows deeply personal and sensitive information to be disclosed (Broom et al., 2009; Carusi & Jirotka, 2009; Dickson-Swift et al., 2006; Guillemin & Heggen, 2009; Guishard, 2017). From this perspective, qualitative research is a process of “generating” data in conjunction with participants rather than simply “collecting” data, leading to data that are relational and embedded (Broom et al., 2009, p. 1164).
Some researchers believe that since they play an essential role in collecting and interpreting data based on their theoretical positioning and embeddedness, then sharing qualitative data for others to analyze simply makes no sense (Broom et al., 2009; Guishard, 2017; Kuula, 2010/2011; Parry & Mauthner, 2004). A related concern expressed by researchers is that participants would not agree to data sharing because information was shared within a relationship of trust and any form of data sharing would breach this participant trust (Guishard, 2017; Mozersky, Walsh, et al., 2020; Yardley et al., 2014).
According to this view of qualitative research, these relationships with, and knowledge of, participants give the primary researcher the necessary context and nuance to interpret the data in a way that those who were not present do not have (Broom et al., 2009). As a result, some researchers claim that secondary users could misinterpret the data, and data sharing is therefore neither feasible nor desirable (Broom et al., 2009; Yardley et al., 2014).
Data sharing mandates may be resisted if qualitative researchers are reticent to share due to concerns about negatively affecting existing relationships between researchers and participants (Mozersky, Walsh, et al., 2020; Mozersky et al., 2021). We conducted a survey of 425 qualitative researchers in the U.S. who gather health related or sensitive data (Mozersky et al., 2021). Only 4% of qualitative researchers had ever shared their data in a repository, and their top concerns regarding qualitative data sharing include the sensitivity of the data (85%) and breach of participant trust (82%).
Benefits of Qualitative Data Sharing
Despite these concerns, there are also numerous benefits of qualitative data sharing, such as generating new research findings with existing data in cost-effective ways, reducing participant burden, training students in qualitative analysis through access to original and real data, and enhancing transparency in the qualitative research enterprise (Bishop, 2009; DuBois et al., 2018; Kirilova & Karcher, 2017). Sharing qualitative data also enables others to verify the quality of data analysis. This is not the same as ensuring reproducibility (Nosek, 2015) – a concept only suitable for quantitative data – and we are not suggesting that replicability and validity are the primary reasons to share qualitative data (Guishard, 2017). However, data sharing can promote transparency and help ensure that data and primary findings are trustworthy.
Despite researcher concerns that sharing data would breach participant trust, research participants themselves may want—and expect—their qualitative data to be shared. We conducted qualitative interviews with 30 research participants who had previously taken part in qualitative health research regarding sharing their sensitive qualitative health data, and our findings indicate that the vast majority of research participants (28/30) support data sharing so long as it is de-identified and shared with other researchers (Mozersky, Parsons, et al., 2020). Most participants (23/30) hoped their data would be shared and may have expected or assumed this was already happening. As one participant explained, “If I’m going for research, or someone is doing research on me and gathering information, then I actually want that information to be shared so everybody will know the information and everybody can put their dots together to come up with the solution” (Mozersky, Parsons, et al., 2020, p. 16).
Focus on Interviews and Focus Groups in the Health Sciences
Given the emerging call to share data (including qualitative data), we wanted to explore one posited barrier to data sharing: the nature of researcher-participant relationships in qualitative health science research. We conducted a content analysis of a representative sample of qualitative health science research to better understand the ways in which researcher-participant relationships were characterized or manifested in interview or focus group studies.
By conducting a qualitative content analysis of 100 randomly selected qualitative health science studies indexed in PubMed, we sought to determine what types of relationships, if any, are evident in qualitative health science research. Do qualitative health science researchers establish deep relationships with participants? Do they have pre-existing relationships with them that enable honest discussions? Do those who conduct data analysis also collect the data? This study aims to explore the nature of researcher-participant relationships in qualitative health science research to help inform ethical deliberations regarding qualitative data sharing and secondary analysis.
We focus on qualitative health science research because there is a substantial body of qualitative research conducted in the health sciences, and the recent NIH guidance will primarily affect those conducting health science qualitative research. For instance, 82% of initial research projects funded by The Patient Centered Outcomes Research Institute (PCORI) include qualitative methods, which support PCORI’s mission of ensuring patients have a voice in research (Vandermause et al., 2017). A majority of research projects awarded through the National Human Genome Research Institute’s “ethical, legal, and social implications” (ELSI) program also use qualitative or mixed methods (National Institutes of Health, 2015). Implementation science projects to implement evidence-based practices in the health sciences also frequently deploy both quantitative and qualitative methods, as mixed methods designs often provide a better understanding of research issues than a single methodological approach (Palinkas et al., 2015).
We focus on qualitative research that used an interview or focus group methodology, as these are commonly used methods in the health sciences and generate data that could be shared. A PubMed search for health sciences articles that used an interview or focus group methodology in the past year returned more than 1600 articles. This does not represent all possible qualitative methods that could be used, but reflects the aim of our overall project, which is to focus on two commonly used qualitative methods in health sciences.
Methods
In order to collect a representative sample of qualitative health science research involving interviews or focus groups published in the past year, we carried out a two-pronged sampling strategy. First, we searched PubMed for qualitative articles published in the past year (11/01/2019 to 10/31/2020) using the search terms: “qualitative” AND (“interview” OR “focus group”). This search returned 1641 articles. Then, using a random integer generator, we selected 50 random articles that met our search criteria (human subjects research, published in English, indexed in MEDLINE, using an interview or focus group methodology).
In order to ensure we were including qualitative research reported in the highest impact journals, we specifically targeted high impact journals in our second phase. We identified 50 qualitative research articles in top-ranked health sciences journals as indicated by impact factor. Using the Web of Science InCites Journal Citation Report, we searched the top-ranking journals in three clusters of disciplines: Nursing; Public, Occupational and Environmental Health; and Medicine, General and Internal (see Table 1).
Table 1.
Top-Ranking Health Sciences Journals That Publish Qualitative Research.
| Discipline | Journal | Impact Factor |
|---|---|---|
|
| ||
| Medicine | BMJ | 30.313 |
| Medicine | Annals of Internal Medicine | 21.317 |
| Medicine | JAMA Internal Medicine | 18.652 |
| Medicine | PLoS Medicine | 10.5 |
| Medicine | Mayo Clinic Proceedings | 6.942 |
| Public health | The Lancet Global Health | 21.597 |
| Public health | Tobacco Control | 6.726 |
| Public health | American Journal of Public Health | 6.464 |
| Public health | Environmental Health | 4.69 |
| Public health | American Journal of Preventive Medicine | 4.42 |
| Nursing | International Journal of Nursing Studies | 3.783 |
| Nursing | Nursing Outlook | 2.833 |
| Nursing | Birth-Issues in Perinatal Care | 2.705 |
| Nursing | Journal of Nursing Scholarship | 2.655 |
| Nursing | Nursing Ethics | 2.597 |
Using each journal’s Web site search function, we again used the search term: “qualitative” AND (“interview” OR “focus group) to find qualitative articles published in the past year (11/01/2019 to 10/31/2020). The journal was excluded if it did not publish at least one qualitative article in the past year, and as a result some of the highest-ranked journals in each discipline were not included on the list. For example, the New England Journal of Medicine and The Lancet were both excluded because they did not publish any qualitative research within the timeline of the search. Similarly, journals that focus exclusively on qualitative methods often have lower impact factors (<2) and thus were not within the five highest-ranking journals that publish qualitative research. However, these journals were present on the list generated during our first search from which we randomly selected 50 articles.
After finding the five highest-ranking journals in each category that published qualitative research, we had 125 articles. To ensure a representative category of articles from each of the three disciplines, we included all 14 qualitative articles from Medicine, 18 (randomly out of 25) from Public Health, and 18 (randomly out of 86) from Nursing (see Figure 1). Our final set consisted of 100 qualitative health science articles comprising 50 randomly selected articles from the general health science literature and 50 selected articles from high impact journals in three fields (see Supplemental Appendix 1 for a list of all articles).
Figure 1.
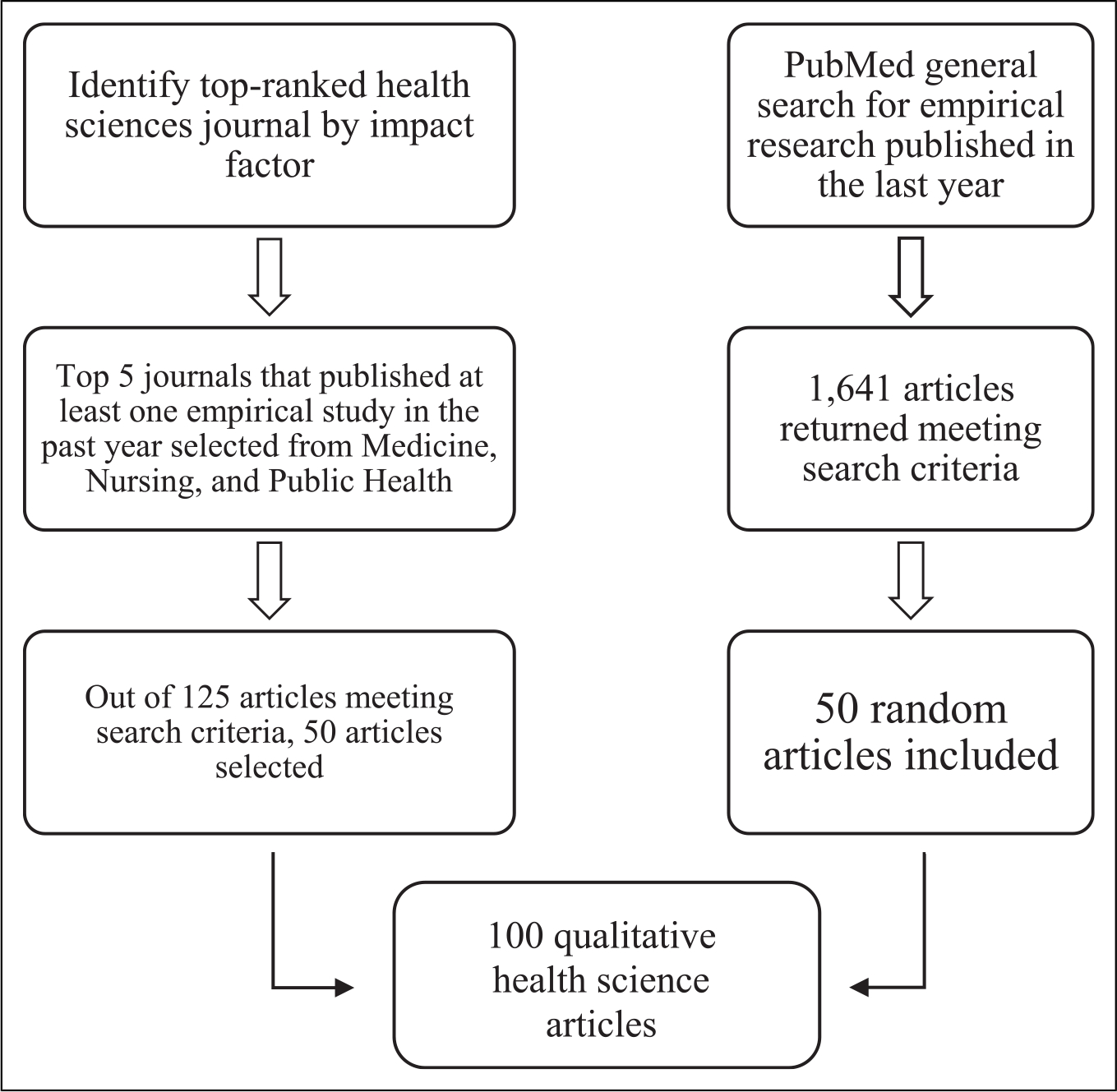
Inclusion flowcharts for qualitative health sciences research.
All authors were involved in initial codebook development. We used a combination of inductive and deductive coding strategies. Deductive coding allowed us to examine traditional markers of relationship-building between participants and researchers. We operationalized markers of relationship-building to include the following: whether participants were known to researchers before the research, length of interaction, type of interaction (i.e. face to face, telephone), number of interactions with participants, number of authors, and which of these authors collected and analyzed data. Inductive coding allowed us to identify unanticipated ways of relationship-building between participants and researchers.
We analyzed relationship evidence across all facets of the research, from design, to participant recruitment, to data collection and analysis:
Study design and recruitment: How did the researchers recruit their participants? Did researchers have pre-existing relationships with participants?
Data collection: How did the researchers gather data? Were there multiple points of contact between researchers and participants? How long did the engagement with participants last?
Data transcription and analysis: Were research team members who conducted the interviews or transcription process also involved in data analysis? Were participants engaged in the data interpretation process?
During the first phase of coding, two coders (AF and JM) blind coded two articles, discussed and resolved differences in coding, and made changes to the codebook. The two repeated this process until codes were consistently applied to the articles without major discrepancies between the raters. The primary coder (AF) proceeded to code half of the articles, at which point another blind coding check was conducted with the second coder (JM) to ensure ongoing agreement and consistent application of codes. Coders resolved differences in coding during consensus meetings and revised the codebook accordingly.
Results
Characterizing Interview and Focus Group Methods
Sixty-five percent of the studies used interviews, 18% used focus groups, and 17% used both focus groups and interviews (see Table 2). Fifty-four percent of the studies utilized a face-to-face approach to collect data, while the remaining studies used telephone or web-based video conferencing only or did not report whether their data collection was in-person or remote. We found only one study that involved a combination of participant observation in addition to single encounter semi-structured interviews (Rubio-Navarro et al., 2020). One additional study reported using participant observation as part of a larger ethnographic project, but explicitly noted that researchers did not know those who took part in qualitative interviews (Lalla et al., 2020). A mixed methods approach was reported in 26% of the studies.
Table 2.
Characteristics of Interviews and Focus Groups of Included Articles.
| Study Method | Interview Only N = 65(%) |
Focus Group Only N = 18 (%) |
Both Interview and Focus Group N = 17(%) |
Subtotals |
|---|---|---|---|---|
|
| ||||
| Face-to-Face | 31 (48) | 15 (83) | 8 (47) | 54 |
| Telephone or virtual | 8 (12) | 0 (0) | 1 (6) | 9 |
| Combination: Face-to-face and telephone or virtual | 17 (26) | 0 (0) | 3 (18) | 20 |
| Unreported | 9 (14) | 3 (17) | 5 (29) | 17 |
Note.
- Studies that used both interviews and focus groups as methods appeared to do so with separate samples of participants. That is, these were not repeated engagements with the same participants.
- We found only one study that involved participant observation in addition to single encounter semi-structured interviews.
- These studies were conducted prior to the COVID-19 pandemic, which forced much of qualitative research to be conducted via telephone or virtual platforms.
Eighty percent of the studies were international, 16% were in the United States, and 4% studied both international and United States locations. Thirty percent were completed at a single site or institution, 23% were conducted at multiple sites, and 47% focused on a generalized population or broader community. The majority of studies (59%) had 5 or more authors, 39% had 2–4 authors, with only 2% of studies being single-authored. The articles characterized their recruitment approaches as “purposive” (81%), “snowball” (18%), “convenience” (10%), or some other approach (such as random sampling) (4%). Some studies used multiple recruitment methods.
Characterizing Researcher-Participant Interactions
We analyzed each study for evidence of multiple contact with participants or longitudinal design and the duration of each researcher-participant encounter. Only 5% of studies noted multiple points of contact with participants (e.g., multiple interviews over the course of a year), while the remainder involved a single encounter with participants. Seventy-seven articles reported the duration of interviews or focus groups (all of which were one-time encounters with participants), and 60% of these encounters with participants were less than 60 min, with about 10% lasting less than 30 min (see Table 3).
Table 3.
Duration of Single-Encounter Interviews and Focus Groups.
| Duration | N = 77 (%) |
|---|---|
|
| |
| Less than 30 min | 7 (9) |
| 30–60 min | 39 (50) |
| 60–90 min | 22 (29) |
| More than 90 min | 9 (12) |
Note. Of the remaining 23 articles, 5 involved more than one encounter, and 18 did not report an interview or focus group duration.
We identified what percentage of authors conducted the interviews or moderated the focus groups to better understand the involvement of researchers with participants during the primary data collection phase. Of the 72 studies that reported this information, the majority of studies (61%) involved fewer than half of authors in direct data collection. One-third of articles involved fewer than 30% of authors. Individuals who collected data included first author, second author, multiple authors, researchers, trained research assistants, nurses, or dedicated interviewers. These proportions of authors involved in data collection may actually be an over-estimate, as it was not always possible to confirm that an interviewer or focus group moderator was also an author on the paper. For example, one study with 4 authors reported that interviews were conducted by “three female research assistants” (Binka et al., 2019), but it is unclear if these assistants are listed as authors. We erred on the side of inclusion when it was not possible to confirm.
We also created a code called “relationship evidence” to inductively assess whether researchers had pre-existing relationships with their participants which may be important for recruitment and the success of the study. Of the 68 articles that addressed this issue, 84% explicitly indicated there was no prior relationship with the participants. Examples of how we characterized “no relationship” include: “the researcher introduced herself to the participants” or “the researcher had no prior relationship with the participants.” If participants were recruited via a listserv or social media, the study was coded as “no relationships.” One study identified this lack of researcher-participant relationship as follows:
Two non-medical researchers (RA/JW), experienced in qualitative interviewing, separately conducted the interviews and were accompanied on the home visit by a research nurse. The researchers and nurse were not known to the participants (Walburn et al., 2020, p. 91).
The remaining 16% of studies that included relationship evidence indicated some form of pre-existing relationship between the researcher(s) and participants.
Researchers’ Data Transcription and Analysis Practices
To better understand the researchers’ relationship to their data during data analysis, we analyzed the transcription practices of each study. While transcription itself is not a marker of relationship to a participant, it is a marker of relationship to the data. Even if one did not conduct the interviews or focus groups initially, one can arguably obtain a deeper sense of the encounter by listening to the audio recordings of the interview or focus group during transcription. Of the 89 articles that reported transcription practices, 55% reported transcription in the passive voice (i.e. “the interviews were audio-recorded and transcribed verbatim”). Nineteen percent reported utilizing a transcription service or professional transcriber, and a research team member transcribed the interview or focus group data in 26% of the studies. Only 7% of these 89 studies specifically noted that the same person who conducted the interview or focus group also personally transcribed the data.
We also looked for evidence of whether researchers offered some form of member checking to participants during the data analysis phase, a process by which data or results are returned to participants to check for accuracy and resonance with their experience, which can be a form of relationship-building (Birt et al., 2016). Only 15% of studies reported or offered any form of member checking, and participants did not necessarily participate or provide feedback to the researchers even when given the opportunity, which suggests a lack of relationship-building with participants.
Discussion
Overall, our results suggest that there is considerable distance between the researcher or research team and the research participant across all stages of qualitative health science research involving interviews or focus groups. We did not find evidence of pre-existing or long-lasting relationships between researchers and participants in a representative sample of qualitative health sciences literature. Notably, in the 68 studies that reported this information, 84% had clear indication that there was no prior relationship with the participants. This inductive finding was surprising, as we were not expecting to see such clear indication of a lack of relationship. Some authors noted that this critical distance was actually beneficial to the study, as participants were perhaps more comfortable speaking openly with a stranger (Moukarzel et al., 2020).
The majority (95%) of qualitative research encounters are single instances, with only 5% of studies reporting multiple contact points with participants. We found only one example of a study that used participant observation in addition to qualitative interviews. Additionally, these one-time encounters are generally brief: 60% of the studies that reported an interview or focus group duration lasted less than 60 min.
The vast majority of studies (98%) had two or more authors, with 59% of the studies having 5 or more authors. This “team science” approach is more common in health sciences such as implementation science research and public health research than in anthropology or sociology (Stokols et al., 2008), which further reduces the likelihood that all authors have a relationship to all participants. Of the 72 studies that reported the number of authors involved in conducting interviews or moderating focus groups, the majority of studies (61%) involved fewer than half of authors in direct data collection. One-third of articles involved fewer than 30% of authors, although as we note above this may actually be an overestimate. However, we assume that all individuals listed as authors are involved in data interpretation in some manner and therefore, our findings suggest that many authors involved in data analysis, interpretation, or discussion of results are not involved in data collection and thus appear to have no relationship with the research participants.
Some research teams may purposefully separate the tasks of data collection and analysis. One article mentioned an intentional separation of individuals who moderated focus groups from those who were coding data to “reduce investigator bias” (Sim et al., 2020, p. 173). This raises an interesting question of whether there are benefits to coding data in the absence of a relationship to participants.
Importantly, participants themselves may have a different understanding of the researcher-participant relationship than researchers. According to one study (Kuula, 2010/2011), qualitative research participants perceived their relationship with researchers as more of an institutional arrangement rather than a personal or private relationship with the individual researcher. As noted earlier, research participants may themselves support qualitative data sharing as a way to enhance their contribution to science, and trust researchers and institutions to properly handle data sharing (Kuula, 2010/2011; Mozersky, Parsons, et al., 2020).
Unique Context of Qualitative Health Science Research
Assumptions about the importance of relationships for data collection and analyses reflect the epistemological standpoint, described in the introduction, that qualitative data is generated and collected within relationships of trust and genuine rapport (Broom et al., 2009). Traditional social science disciplines such as anthropology or sociology frequently employ extensive fieldwork or ethnographic methods, often by a single researcher, that involves building deep relationships with particular communities over time (Bosk, 1979; Fadiman, 1997; Geertz, 1973). In addition, such researchers may not even conduct, let alone transcribe interviews; their raw data may be field notes based on participant observation, which can be highly personal (Barbour, 2000). Concerns about the implications of data sharing in these contexts may be warranted, as deep and richly descriptive data such as field notes may be highly personal, subjective, and difficult to de-identify.
Yet in some contexts, such as the health sciences, qualitative research may be conducted with more specific goals. Multi-disciplinary team science is common in the health sciences, and qualitative methods are frequently employed to explore a particular health experience or topic during a single interview or focus group, to triangulate quantitative findings in mixed methods research, or to help inform the development of quantitative measures (Barbour, 2000). Projects in the health sciences are also frequently grant funded, with finite end dates when researchers need to move onto new funded projects, leaving little time to return to past projects for further analyses or to foster lasting relationships with past participants.
Overall, our findings suggest that deep or ongoing relationship-building between researchers and participants may not be commonly present in qualitative interview or focus group health science research studies. In the health sciences, qualitative data are often not collected by a single individual in the context of a close or established relationship with a participant. The assumption that there is a single individual who is best placed to interpret this data due to their context-specific knowledge of their participants and the relationship established does not appear to be the case based on our findings (Kuula, 2010/2011). These circumscribed and time-limited relationships may be more common in qualitative health science research where researchers often conduct mixed methods studies, utilize single interviews or focus groups to explore a discreet health topic or issue, or consider population-based issues in a public health context, with participants who are previously unknown to them (Barbour, 2000).
While we do not address every concern to secondary data sharing, this absence of ongoing personal relationships addresses one crucial concern and speaks to the feasibility (in principle) of secondary analysis of qualitative health science research data. It is likely that much qualitative health science data could be shared and potentially used for secondary analysis more readily than critics claim. Qualitative health science research may be especially well suited to data sharing, as it is often grant funded with finite end dates (Barbour, 2000), and funding agencies such as the NIH will require compliance with data sharing requirements.
Limitations
Our content analysis focused on a particular type of qualitative research – involving interviews or focus groups – within the health sciences. Our findings are thus not representative of all qualitative research or methods, but a specific form of qualitative research conducted within health sciences. Our findings do not represent other qualitative disciplinary or methodological approaches that may involve building relationships. However, in light of the large volume of qualitative interviews and focus groups conducted in the health sciences, our findings contribute to debates regarding ethical and appropriate data sharing in this particular context.
Further, because we sought to identify a portion of qualitative articles from journals with the highest impact factors in medicine, nursing, and public health, qualitative health science research published in prominent qualitative journals with lower impact factors were excluded from the second phase of our search strategy. However, these journals were included in the first phase, as any qualitative health science articles utilizing a focus group or interview, indexed in PubMed, and published between 11/01/2019 and 10/31/2020 were included for randomization in the first phase of our search strategy.
We also encountered challenges when trying to determine the exact roles of those who collected data or whether researchers had pre-existing relationships with participants, as this information was not always readily available in journal articles. The Consolidated Criteria for Reporting Qualitative Research (COREQ) contains 32 items that authors are encouraged to report when publishing qualitative research (Tong et al., 2007). According to COREQ, information that should be included when reporting include: which authors collected data, whether a relationship was established with participants prior to the study, and how many coders coded data. Not all studies reported this information, which suggests that authors are not necessarily following COREQ criteria when publishing qualitative findings. However, we were able to assess how many individuals collected data in 72% of articles, and 68% of studies reported information regarding whether there was a pre-existing relationship, which enables us to draw strong conclusions about the nature of researcher-participant relationships.
Future Research
While our findings suggest that researcher-participant relationships do not pose an insurmountable barrier to data sharing for secondary analysis, more research needs to be done to develop criteria for responsible data sharing and secondary analysis. For instance, if data are shared more broadly for secondary analyses, researchers may need to guard against “entrenchment”, that is, over-reliance on a single or limited data set to answer questions and failure to obtain more diverse data (Beskow, 2018 unpublished). It is also essential to ensure that data contain adequate contextual details to enable others to analyze data.
Going forward it is also essential that consent forms include permission for data sharing, and in particular avoid promising to destroy data which prohibits any sharing in future. In our survey of qualitative researchers, lack of permission to share data was the top concern (87%), but importantly 80% of these researchers said that knowing participants agreed to data sharing would increase their willingness to share (Mozersky, Walsh, et al., 2020). It is important to ensure consent forms convey information regarding data sharing in a way that is understandable and acceptable to participants.
Notably, the NIH data sharing policy does not specify what types of data should be shared, but our larger project has focused on sharing de-identified qualitative transcripts, as opposed to field notes, audio, video, or photographic images which present greater challenges for de-identification. As data sharing increases, guidance on responsible sharing of these materials will also be needed.
An additional barrier that remains to be addressed is how to protect participant confidentiality when sharing qualitative data. To that end, in the next phase of our project, we are exploring which identifiers are commonly reported in qualitative health science research and which identifiers may need to be anonymized when sharing qualitative data. This complements our larger project to develop guidelines for ethical and responsible qualitative data sharing and software to support health science qualitative researchers in de-identifying qualitative data (DuBois et al., 2018).
Conclusion
Even though questions remain about what responsible and ethical secondary analysis should look like in qualitative health science research, our study shows that one supposed barrier—the need for close relationships between researcher and participant in order to collect and accurately interpret data—should not be a barrier to sharing some qualitative health science data for secondary analyses. These findings are important given the recent NIH mandate requiring data sharing which will primarily impact health science researchers.
Supplementary Material
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by grants from the U.S. National Institutes of Health [R01HG009351 and UL1TR002345].
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Supplemental Material
Supplemental material for this article is available online.
References
- Barbour RS (2000). The role of qualitative research in broadening the èvidence base’ for clinical practice. Journal of Evaluation in Clinical Practice, 6(2), 155–163. 10.1046/j.1365-2753.2000.00213.x [DOI] [PubMed] [Google Scholar]
- Beskow L (2018). Challenges in sharing and re-using qualitative data: Context matters. American Society for Bioethics and Humanities Annual Meeting. [Google Scholar]
- Binka C, Nyarko SH, Awusabo-Asare K, & Doku DT (2019). Barriers to the uptake of cervical cancer screening and treatment among rural women in Ghana. BioMedical Research International. 10.1155/2019/6320938 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birt L, Scott S, Cavers D, Campbell C, & Walter F (2016). Member checking: A tool to enhance trustworthiness or merely a nod to validation? Qualitative Health Research, 26(13), 1802–1811. 10.1177/1049732316654870 [DOI] [PubMed] [Google Scholar]
- Bishop L (2009). Ethical sharing and reuse of qualitative data. Australian Journal of Social Issues, 44(3), 255–272. [Google Scholar]
- Bishop L, & Kuula-Luumi A (2017). Revisiting qualitative data reuse. SAGE Open, 7(1), 21582440166. 10.1177/2158244016685136 [DOI] [Google Scholar]
- Bosk C (1979). Forgive and remember: Managing medical failure (2nd ed.). The University of Chicago Press. [Google Scholar]
- Broom A, Cheshire L, & Emmison M (2009). Qualitative researchers’ understandings of their practice and the implications for data archiving and sharing. Sociology, 43(6), 1163–1180. 10.1177/0038038509345704 [DOI] [Google Scholar]
- Carusi A, & Jirotka M (2009). From data archive to ethical labyrinth. Qualitative Research, 9, 285–298. 10.1177/1468794109105032 [DOI] [Google Scholar]
- Corti L, Fielding N, & Bishop L (2016). Editorial for special edition, digital representations. SAGE Open, 6(4), 1–3. 10.1177/2158244016678911 [DOI] [Google Scholar]
- Corti L, & Thompson P (2004). Secondary analysis of archived data. In Seale CG, Gubrium JF, & Silverman D (Eds.), Qualitative research practice (pp. 297–313). Sage Publications Ltd. [Google Scholar]
- Dickson-Swift V, James EL, Kippen S, & Liamputtong P (2006). Blurring boundaries in qualitative health research on sensitive topics. Qualitative Health Research, 16(6), 853–871. 10.1177/1049732306287526 [DOI] [PubMed] [Google Scholar]
- DuBois JM, Strait M, & Walsh H (2018). Is it time to share qualitative research data? Qualitative Psychology, 5(3), 380–393. 10.1037/qup0000076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fadiman A (1997). The spirit catches you and you fall down: A Hmong child, her American doctors, and the collision of two cultures. Farrar, Straus and Giroux. [DOI] [PubMed] [Google Scholar]
- Foster ED, & Deardorff A (2017). Open science framework (OSF). Journal of the Medical Library Association, 105(2), 203–206. 10.5195/jmla.2017.88 [DOI] [Google Scholar]
- Geertz C (1973). The interpretation of cultures. Basic Books. [Google Scholar]
- Guillemin M, & Heggen K (2009). Rapport and respect: Negotiating ethical relations between researcher and participant. Medicine, Health Care, and Philosophy, 12(3), 291–299. 10.1007/s11019-008-9165-8 [DOI] [PubMed] [Google Scholar]
- Guishard MA (2017). Now’s not the time! Qualitative data repositories on tricky ground. Comment on DuBois et al. (2017). Qualitative Psychology. 10.1037/qup0000085 [DOI] [Google Scholar]
- Kirilova D, & Karcher S (2017). Rethinking data sharing and human participant protection in social science research: Applications from the qualitative realm. Data Science Journal, 16(43), 1–7. 10.5334/dsj-2017-043 [DOI] [Google Scholar]
- Kuula A (2010/2011). Methodological and ethical dilemmas of archiving qualitative data. Iassist Quarterly, 34/35(3–4/1–2), 12–17. http://www.iassistdata.org/sites/default/files/iqvol34_35.pdf [Google Scholar]
- Lalla AT, Ginsbach KF, Penney N, Shamsudin A, & Oka R (2020). Exploring sources of insecurity for Ethiopian Oromo and Somali women who have given birth in Kakuma Refugee camp: A qualitative study. Plos Medicine, 17(3), e1003066. 10.1371/journal.pmed.1003066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKiernan EC, Bourne PE, Brown CT, Buck S, Kenall A, Lin J, McDougall D, Nosek BA, Ram K, Soderberg CK, Spies JR, Thaney K, Updegrove A, Woo KH, & Yarkoni T (2016). How open science helps researchers succeed. eLife, 5, e16800. 10.7554/eLife.16800 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moukarzel S, Mamas C, Farhat A, Abi Abboud A, & Daly AJ (2020). A qualitative examination of barriers against effective medical education and practices related to breastfeeding promotion and support in Lebanon. Medical Education Online, 25(1), 1723950. 10.1080/10872981.2020.1723950 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mozersky J, McIntosh T, Walsh H, Parsons M, Goodman M, & DuBois J (2021). Barriers and facilitators to qualitative data sharing: A survey of qualitative researchers. Plos One, 16(12), e0261719. 10.1371/journal.pone.0261719 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mozersky J, Parsons M, Walsh H, Baldwin K, McIntosh T, & DuBois JM (2020). Research participant views regarding qualitative data sharing. Ethics & Human Research, 42(2), 13–27. 10.1002/eahr.500044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mozersky J, Walsh H, Parsons M, McIntosh T, Baldwin K, & DuBois JM (2020). Are we ready to share qualitative research data? Knowledge and preparedness among qualitative researchers, IRB members, and data repository curators. Iassist Quarterly, 43(4), 1–23. 10.29173/iq952 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institutes of Health. (2015). The ethical, legal and social implications (ELSI) research program. https://www.genome.gov/page.cfm?pageID=17515632#beginSearch
- National Institutes of Health. (2020). NIH data sharing policy and implementation guidance. https://grants.nih.gov/grants/policy/data_sharing/data_sharing_guidance.htm
- Nosek BA (2015). Estimating the reproducibility of psychological science. Science, 349(6251), aac4716. 10.1126/science.aac4716 [DOI] [PubMed] [Google Scholar]
- Palinkas LA, Horwitz SM, Green CA, Wisdom JP, Duan N, & Hoagwood K (2015). Purposeful sampling for qualitative data collection and analysis in mixed method implementation research. Administration and Policy in Mental Health, 42(5), 533–544. 10.1007/s10488-013-0528-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parry O, & Mauthner NS (2004). Whose data are they anyway? Practical, legal and ethical issues in archiving qualitative research data. Sociology, 38(1), 139–152. [Google Scholar]
- Rubio-Navarro A, García-Capilla DJ, Torralba-Madrid MJ, & Rutty J (2020). Decision-making in an emergency department: A nursing accountability model. Nursing Ethics, 27(2), 567–586. 10.1177/0969733019851542 [DOI] [PubMed] [Google Scholar]
- Sim MA, Lee SH, Phan PH, & Lateef A (2020). Quality improvement at an acute medical unit in an asian academic center: A mixed methods study of nursing work dynamics. Nursing Outlook, 68(2), 169–183. 10.1016/j.outlook.2019.09.002 [DOI] [PubMed] [Google Scholar]
- Stokols D, Hall KL, Taylor BK, & Moser RP (2008). The science of team science: Overview of the field and introduction to the supplement. American Journal of Preventive Medicine, 35(2), S77–S89. 10.1016/j.amepre.2008.05.002 [DOI] [PubMed] [Google Scholar]
- Tong A, Sainsbury P, & Craig J (2007) (In press). Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. International Journal for Quality in Health Care, 19(6), 349–357. 10.1093/intqhc/mzm042 [DOI] [PubMed] [Google Scholar]
- Vandermause R, Barg FK, Esmail L, Edmundson L, Girard S, & Perfetti AR (2017). Qualitative methods in patient-centered outcomes research. Qualitative Health Research, 27(3), 434–443. [DOI] [PubMed] [Google Scholar]
- Walburn J, Anderson R, & Morgan M (2020). Forms, interactions, and responses to social support: A qualitative study of support and adherence to photoprotection amongst patients with xeroderma pigmentosum. British Journal of Health Psychology, 25(1), 89–106. 10.1111/bjhp.12396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yardley SJ, Watts KM, Pearson J, & Richardson JC (2014). Ethical issues in the reuse of qualitative data: Perspectives from literature, practice, and participants. Qualitative Health Research, 24 (1), 102–113. 10.1177/1049732313518373 [DOI] [PubMed] [Google Scholar]
- Yoon A (2014). Making a square fit into a circle”: Researchers’ experiences reusing qualitative data. Proceedings of the American Society for Information Science and Technology, 51(1), 1–4. 10.1002/meet.2014.14505101140 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


