Abstract
Background
Female sex workers (FSWs) have the highest HIV prevalence in Uganda. Pre exposure prophylaxis (PrEP) has been recommended as part of the HIV combination prevention strategy, with improved patient initiation, but continuation on the service is low. We evaluated PrEP continuation among FSWs and explored potential determinants of PrEP continuation within a public referral hospital in Urban Uganda.
Methods
An explanatory sequential mixed method study was conducted at Kiruddu National referral hospital in Uganda. Secondary data on social demographic characteristics and follow up outcomes of at least one year was collected for all FSWs who were initiated PrEP between May 2020 and April 2021.We used Kaplan–Meier survival analysis to evaluate continuation on PrEP from time of initiation and follow-up period. The capability, opportunity, and motivation to change behaviour model was used to explore perspectives and practices of FSWs (n = 24) and health care providers (n = 8) on continuation on PrEP among FSWs, using semi structured interviews. The qualitative data was deductively coded and analyzed thematically, categorizing the themes related to PrEP continuation as facilitators and barriers.
Results
Of the 292 FSWs initiated on PrEP during this period, 101 (34.6) % were active on PrEP, 137 (46.9%) were lost to follow-up, 45 (15.4%) were no longer eligible to continue PrEP, eight (2.7%) were transferred out and one (0.3%) had died. Median survival time on PrEP was 15 months (Interquartile range IQR, 3–21). The continuation rates on PrEP at six (6) and 12 months were, 61.1% and 53.1%, respectively. Facilitators of PrEP continuation included awareness of risk associated with sex work, integration of PrEP with other HIV prevention services, presence of PrEP Peer support and use of Drop-in centers. The barriers included low community awareness about PrEP, high mobility of sex workers, substance abuse, and the unfavorable daytime clinic schedules.
Conclusion
Continuation on PrEP remains low among FSWs. Interventions for PrEP continuation should address barriers such as low community awareness on PrEP, substance abuse and restrictive health facility policies for scale of the PrEP program among FSWs in Uganda. Integration of PrEP with other services and scale up of community PrEP delivery structures may improve its continuation.
Keywords: PrEP continuation, Female sex workers, barriers, facilitators, determinants, Uganda, COM-B
Background
Data from Sub-Saharan Africa (SSA) show that 15% of new HIV infections occur among female sex workers (FSWs) [1], a patten similar to that seen in Uganda where HIV studies show a high HIV prevalence among sex workers at 37% compared to 5.5% in the general population [2, 3]. Innovative and effective HIV prevention interventions such as Oral pre-exposure prophylaxis (PrEP) with Tenofovir disoproxil fumarate coformulated with Emtricitabine or Lamivudine is recommended globally for preventing HIV acquisition in high risk groups [4–6]. Uganda adopted oral PrEP as part of the combination prevention biomedical intervention. However, the scale up of the PrEP program remains sub-optimal[7]. Whereas the acceptance of PrEP among FSWs has previously been established [8], there is a dearth of knowledge about the continuation on PrEP services including its determinants (facilitators and barriers) among FSWs. According to the Uganda annual joint AIDS review report, 90% of the FSWs found eligible were initiated on PrEP during 2021/2022 [9] but the trends on PrEP continuation are unknown. Previous studies conducted in Uganda cited PrEP stigma and high mobility as potential barriers to uptake and continuation on PrEP among high risk populations [10]. To inform the national PrEP program on the current continuation rates among eligible FSWs, we evaluated PrEP continuation rates among FSWs in a public national referral hospital. In addition, we explored the potential facilitators and barriers to continuation on PrEP services among the FSWs using the Capacity, Opportunity, Motivation to change behavior (COM-B) model of the behavior change wheel [11–13].
Methodology
Study design.
This was a mixed methods explanatory sequential design [14], where we retrospectively collected and analysed quantitative data on the social demographic characteristics and follow up outcomes of FSWs enrolled on PrEP first and later collected qualitative data to better understand and explain the findings of the quantitative data. We used quantitative data to determine the discontinuation rates on PrEP among eligible FSWs at various time intervals and the predictors of PrEP discontinuation. The qualitative data was then used to contextualise the quantitative findings, understanding the potential facilitators and barriers to continuation on PrEP among FSWs.
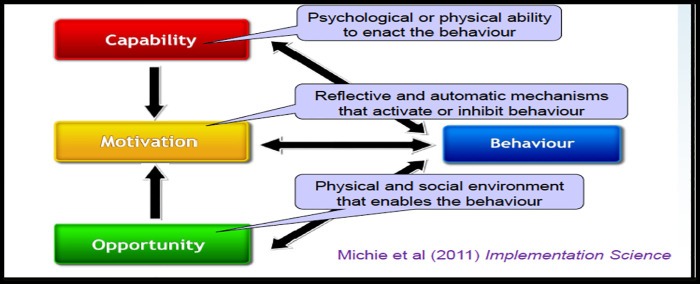
For the quantitative part, we collected data retrospectively on FSWs enrolled in PrEP at Kiruddu National referral hospital (KNRH) to map out the discontinuation rates and related factors. For the qualitative component, we purposively selected FSWs enrolled on PrEP and conducted semi structured interviews to explore their beliefs, understanding and perspectives on continuation on PrEP services. In addition, key informant interviews with health providers (HPs) at KNRH were conducted to share their experience and beliefs on continuation on PrEP services among eligible FSWs. We used the COM-B model, which postulates that for behavior change to occur, three conditions must be met: Capability, Opportunity, and Motivation (See Fig. 1) to explore the perspectives and practices of FSWs and health providers on continuation on PrEP among eligible FSWs.
Figure 1.
Illustration of the COM-B model
Study site.
The study was conducted at KNRH, a public tertiary level hospital located in the administrative division of Makindye of the Ugandan capital, Kampala. Makindye division is the largest of the five administrative divisions of Kampala with a high number of hotspots involved in sex work. KNRH provides HIV prevention care and treatment services at no cost to the patients including PrEP services to its catchment communities. At the time of this study a total number of 2,254 clients at substantial risk of HIV acquisition were active on PrEP, of whom 978 (43%) were FSWs. PrEP services at both health facility and community level are provided following the Uganda ministry of health guidelines. The PrEP services that include screening for eligibility, enrolment and follow up are offered by health providers including doctors, nurse counsellors, laboratory technicians, pharmacy technicians, data officers, and FSW PrEP peers with technical assistance by Makerere University Joint AIDS Program.
Study participants and Sample size.
For the quantitative component of the study, we used a retrospective cohort study research design to collect quantitative data on the social demographic characteristics and follow up outcomes of FSWs who received PrEP services at KNRH between May 2020 and April 2021 and to allow for at least one year follow-up.
For the qualitative component we purposively selected a subset of 24 FSWs who were initiated on PrEP at KNRH, ≥ 18 years of age, about to return for PrEP refills and had been part of the quantitative study. To ensure diversity, both FSWs receiving PrEP refills at the facility and community based drop-in centres were included in the study. We recruited eight (8) health providers of different cadres (medical doctor, nurses, and Community-based FSW PrEP Peers) from the HIV outpatient clinic who participated in the provision of PrEP services at KNRH for at least one year.
Telephone calls were made to FSWs who were eligible to participate in the study and whose PrEP refill appointments were within two weeks. Health providers were approached physically at the facility and requested to participate in the study. The participants were recruited into the study until no new information was being obtained. In addition, the data provided was captured real time to know when data saturation was reached.
Data collection.
For the quantitative component, secondary data was obtained from PrEP facility registers and the Health Management Information System (HMIS) AIDS Control Program (ACP) 027 that contain follow-up visit information. A data abstraction tool was developed to capture data of all FSWs who were initiated PrEP between May 2020 and April 2021 with their follow-up outcomes of at least one year as of April 2022. The baseline characteristics captured included age, date of PrEP initiation, education level, occupation, religion, PrEP continuation status, marital status, and place of residence and site of PrEP refills. The continuation on PrEP status was classified on whether the client was active on PrEP, lost to follow-up, transferred out, advised to stop PrEP by a health provider or died. Reasons for stopping PrEP by the health provider and transfer out were also captured. The extracted data was entered using Microsoft Access and later exported to Microsoft Excel for cleaning and coding. The data was analyzed with Stata version MP 14.0.
The qualitative study aimed to get a wider context of the possible enablers and barriers to continuation on PrEP services among FSWS. In-depth interviews with FSWs enrolled on PrEP and health providers involved in the provision of PrEP services were conducted. The pretested interview guides were developed based on the domains of the COM-B model and were administered by trained research assistants. 24 in-depth interviews were conducted with FSWs and eight Key informant interviews with health providers. Both sets of interviews lasted approximately 45 mins to one hour. We explored individual knowledge and beliefs about PrEP for HIV prevention, factors that influence decision to initiate on PrEP, how to receive the PrEP, the importance of PrEP and continuation on PrEP services. In addition, we generated individual lived experiences and perceptions of the proposed interventions to ensure continuation on PrEP services.
Written informed consent was obtained from all participants to join the study. For participants who could not read or write, informed consent was obtained in presence of an impartial witness. The interviews for health providers (HPs) were all conducted in English, audio recorded and later transcribed verbatim while those with FSWs were conducted in Luganda, the most spoken local language, audio recorded transcribed verbatim in Luganda and later translated in English.
Data analysis.
Analysis of quantitative data involved the use of Kaplan–Meier survival analysis to evaluate discontinuation on PrEP from time of initiation, one month after initiation and every 3 months thereafter. The outcome variable was lost to follow-up, constructed as the time between initiation on PrEP and lost to follow-up (failure) as of April 2022. Lost to follow up was defined as no PrEP refill within one month after scheduled appointment.
Censoring was considered for individuals who continued PrEP, those who were no longer eligible for PrEP and stopped, transferred out and died within the study period. Our analysis considered the following as independent variables: age groups, education level, religion, marital status, residence, and site of PrEP refills. The Kaplan-Meier method was used to plot survival curves that served to test the proportional hazard assumption. We used the Cox’s Regression Hazards model to assess the association of the independent variables and PrEP discontinuation at 95% confidence interval. Stepwise analysis was used where covariates that had P-value ≤ 0.25 in bivariate cox regression analysis were selected for multivariable cox regression analysis. All the covariates with P-value ≤ 0.05 were considered to have statistically significant association with PrEP discontinuation during multivariable cox proportional regression analysis.
Analysis of the qualitative data involved de-identification of interview scripts which were later analyzed by the research team. The team comprised of a behavioral social scientist (HW) and public health specialist (SK) who analyzed data using a thematic content analysis [15, 16] guided by the six domains (physical/psychological capability, social/physical opportunity and reflective/automatic motivation) of the COM-B framework. The team developed a codebook by sampling some of the transcripts from the data. Each researcher independently identified preliminary codes and sub-themes using a deductive approach. Once a codebook was developed and the team agreed on recurring themes, HW reviewed all transcripts for completeness and later coded in Atlas ti qualitative analysis software version 22. The obtained themes were mapped to the COM-B domains and constructs and the data separated into facilitators and barriers that relate to continuation on PrEP services.
Results
Quantitative study.
Participant socio-demographic and baseline characteristics.
Between April 2020 and May 2021, a total of 292 FSWs were initiated on PrEP at KNRH with the baseline median age of 26 years, IQR, 22–30. (SD, ± 5.76). Majority (90.75%) received their PrEP refills from the community and were single (59.93%). (See Table 1).
Table 1.
Baseline characteristics of study Participants.
| Variable | Total N = 292, % | Event n = 137 ,46.92 | Censored n = 155, 53.08 | P-Value |
|---|---|---|---|---|
| Age | ||||
| Median age (age group), SD | 26 (22–30), ± 5.76 | 25(21–29), ± 5.72 | 27(23–30), ± 5.72 | |
| Age group | ||||
| <25 | 113, 38.7 | 62, 45.3 | 51, 32.9 | 0.09 |
| 25–29 | 100, 34.3 | 41, 29.9 | 59, 38.1 | |
| ≥30 | 79, 27.1 | 34, 24.8 | 45, 29.0 | |
| Education level | ||||
| None | 83, 28.4 | 41, 29.9 | 42, 27.1 | 0.70 |
| Primary | 106, 36.3 | 49, 35.8 | 57, 36.8 | |
| Secondary | 97, 33.2 | 43, 31.4 | 54, 34.8 | |
| Tertiary | 6, 2.1 | 4, 2.9 | 2, 1.3 | |
| Religion | ||||
| Christian | 230, 78.8 | 115, 83.9 | 115, 74.2 | 0.04 |
| Islam | 62, 21.2 | 22, 16.1 | 40, 25.8 | |
| Marital status | ||||
| Single | 175, 59.9 | 89, 64.9 | 86, 55.5 | 0.55 |
| Married | 19, 6.5 | 8, 5.8 | 11, 7.1 | |
| Separated | 85, 29.1 | 35, 25.6 | 50, 32.3 | |
| Divorced | 9, 3.1 | 3, 2.2 | 6, 3.9 | |
| Widowed | 4, 1.4 | 2, 1.5 | 2, 1.3 | |
| Area of Residence | ||||
| Central | 35, 12.0 | 22, 16.06 | 13, 8.4 | 0.33 |
| Kawempe | 55, 18.8 | 26, 18.98 | 29, 18.7 | |
| Kyadondo | 15, 5.1 | 7, 5.11 | 8, 5.2 | |
| Makindye | 50, 17.1 | 24, 17.52 | 26, 16.8 | |
| Nakawa | 32, 11.0 | 11, 8.03 | 21, 13.6 | |
| Rubaga | 105, 36.0 | 47, 34.31 | 58, 37.4 | |
| Site of PrEP refills | ||||
| Facility | 27, 9.25 | 11, 8.0 | 16, 10.3 | 0.50 |
| Community | 265, 90.75 | 126, 92.0 | 139, 89.7 | |
PrEP - Pre-Exposure Prophylaxis; SD - Standard deviation
PrEP discontinuation among Female Sex Workers.
Among the 292 FSWs who were initiated on PrEP during this period, 101 (34.6%) were still active on PrEP, 137 (46.9%) were lost to follow-up, 45 (15.4%) were stopped due to contraindications to PrEP, 8 (2.7%) were transferred out and one (0.3%) had died. Among those who stopped PrEP 42 (93.3%) were no longer at risk of HIV infection and three (6.7%) were due to other contra-indications to PrEP including low creatinine (< 60 mls/min), Hepatitis B positive, and unwillingness to continue PrEP by the client.
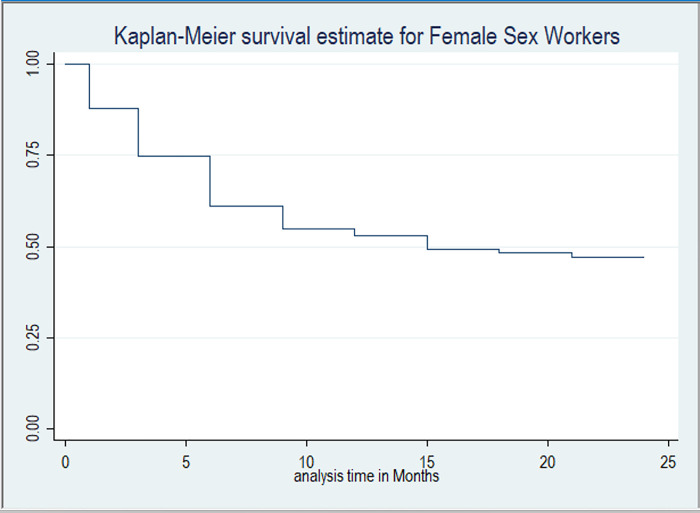
Figure 2 shows the Kaplan Meier survival estimate for continuation on PrEP among FSWs at Kiruddu National referral hospital. The overall median survival time on PrEP was 15 months (IQR,3–21). The continuation rates on PrEP at one, three, six, nine, 12, 15, 18, 21 and 24 months were 88.0%, 74.7%, 61.1%, 54.9%, 53.1%, 49.3%, 48.4%, 47.1% and 47.0% respectively.
Figure 2.
Kaplan-Meier survival curve for Female Sex Workers
Factors associated with PrEP discontinuation among FSWs.
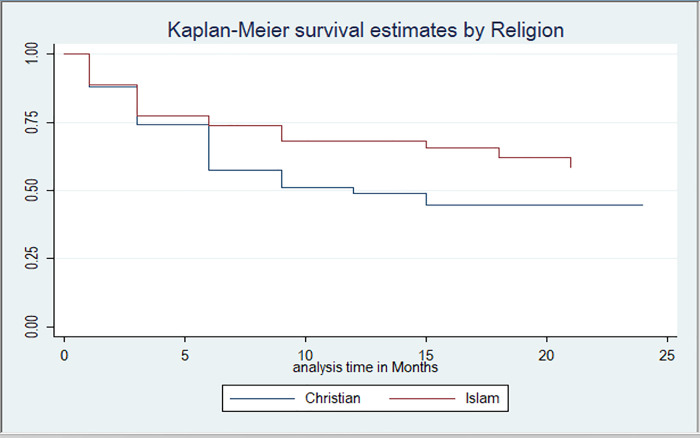
FSWs who were Christians had higher hazard rates of discontinuation at 56% compared to those that were Islam by religion (P-Value, 0.05, AHR = 1.56, 95% CI: 0.987, 2.467). (Table 2). There was no statistical relationship between PrEP discontinuation and age-group and education level. There was significant difference in discontinuation among FSWs by religion: Christians, Islam (Log Rank Test P-Value 0.039) (Fig. 3).
Table 2.
Multivariable Cox Proportional Hazards Model.
| Variable | UHR | P-Value | 95% CI | AHR | P-Value | 95% CI |
|---|---|---|---|---|---|---|
| Age group | ||||||
| <25 | Ref | Ref | ||||
| 25–29 | 0.747 | 0.15 | 0.503–1.109 | 0.735 | 0.14 | 0.491–1.101 |
| >30 | 0.823 | 0.36 | 0.541–1.251 | 0.787 | 0.27 | 0.516–1.206 |
| Religion | ||||||
| Islam | Ref | Ref | ||||
| Christian | 1.561 | 0.06 | 0.988–2.466 | 1.560 | 0.05 | 0.987–2.467 |
| Education level | ||||||
| None | Ref | Ref | ||||
| Primary | 1.037 | 0.87 | 0.684–1.571 | 1.052 | 0.81 | 0.693–1.596 |
| Secondary | 0.92 | 0.71 | 0.601–1.417 | 0.988 | 0.96 | 0.638–1.529 |
| Tertiary | 1.93 | 0.21 | 0.690–5.414 | 2.062 | 0.17 | 0.729–5.832 |
UHR - Unadjusted hazard ratio; CI - Confidence interval; Ref - Reference category.
Figure 3.
Kaplan-Meier survival curve for Sex Workers by Religion. (Log Rank Test: 0.039)
Integration of quantitative and qualitative findings.
The qualitative results below provide perspective to the perceived facilitators among health providers and FSWs on the continuation of PrEP among FSWs. The barriers and facilitators were presented along the domains of the COM-B model and explain why some FSWs stop or continue with PrEP services. Both barriers and facilitators emerged from the domains of the COM-B model including psychological capability, physical capability, physical opportunity, social opportunity, reflective motivation an automatic reflection. (Table 3).
Table 3.
Facilitators and barriers to continuation on PrEP services in the Hospital as related to the COM-Bdomains.
| C | Facilitators | Example quotes | Barriers | Example quotes |
|---|---|---|---|---|
| Psychological capability |
FSWs:Awareness that sex work is associated with a high risk of HIV acquisition. Fear of death due HIV disease Experience of having friends who stopped PrEP and acquired HIV. HP: Healthcare providers have adequate knowledge of PrEP screening, initiation, and continuation. |
“What I understand by PrEP is, it is a medicine, that I use that can help prevent HIV/AIDs because as a sex worker, I have many sex partners.”FSW 013. And most people say, “That girl is spoilt, she is a prostitute but in spite of that, she is HIV negative” but why is it so? Because of PrEP. And I tell them the same thing” FSW 020 PrEP is the use of ARVs to prevent the likely hood of HIV infection among high-risk HIV negative individuals. So, PrEP is taken as long as one continues to be at risk of contracting HIV. HP 001-Counsellor In this line of work (sex work) ,you have to encourage your self to continue with PrEP, to avoid acquisition of HIV and death.” FSW 001 “When FSWs come here, we are able to offer PrEP, in addition, we also assess for other diseases, we offer general treatment, and this keeps them interested to come back” HP 002- Clinician. |
FSWs Misconceptions about PrEP medicine Inadequate knowledge on how to manage side effects associated with PrEP. Inadequate community awareness about PrEP services. Poor health worker attitudes towards FSWs, |
“Sometimes the medicine I think stopped me from giving birth. I want to have a child, but it is not happening’ FSW 015. “May be, the doctors need to further sensitize the people in the community about PrEP so that they can also be educated about it and begin to take it. They should go to different communities sensitizing people so that they can also start their medication.” FSW 003. |
| Physical capability | None. | None. | ||
| Physical opportunity |
FSWs Presence of health education ,support and monitoring by health providers Supportive infrastructure at both facility and community including the PrEP Peer leaders. Integration of other services during the PrEP refill visits. Availability of PrEP drugs. Easy accessibility of PrEP services. HPs: Flexibility of work ensures clients retention |
“I will thank the management of drop-in centers (DICs) because, you may be stressed over a man who had sex with you, beaten you and not paid you, you come here, you are counselled, given something to eat and bed to rest”.FSW 006. “The medicines are available and sometimes they bring us the medicine when we fail to come. “ FSW 001 HPs “Then we have flexi hours clinics. So, those who are unable to come for refills during the weekdays can be refilled on Saturday or the evening” HP 001- Counsellor “Like I said that we work with CBOs and Peer leaders. All clients who are initiated at that facility are attached to Peers who are key to their follow-up”HP 006- Counsellor |
FSWs Substance abuse/Alcohol consumption The daytime clinic schedules are not in sync with the daily routines of sex work. Insufficient commodities at the facility such as PrEP drugs and HIV testing kits Increased workload by health providers. Limited Privacy at the hospital. Restrictive health facility policies such as dress code. High mobility from one place to another The busy work schedules . The burden of swallowing the pill every day. Long distance to facility or community refill points, long waiting times at the clinic due to routine assessments HPs: Time consuming data collection tools Stock out of supplies such as rapid testing kits, drugs for sexually transmitted infection (STI) treatment and PrEP, discourages FSWs from returning. This also limits MMDs in PrEP programming. |
“The other thing that’s so common among the sex workers, they want to sleep during the day. We want everything (clinical) to be done in the night, yet the doctors are readily available during the day.”FSW 009 “Most times what hinders me from coming is transport, we need more drop in centers.” FSW 020 “I started drinking alcohol because the kind of work I do. You may get a customer who first wants you to get drank. People are different so you may find one who wants to first have fun with you before going to bed”. FSW 010. “When you tell them to wait for the drugs at the pharmacy, some of them leave without the drugs. So that one is also affecting us.”HW 001- Consellor. The increasing number of clients on PrEP services with no increase in the healthcare work force impairs implementation of retention on PrEP strategies with fidelity” HP 004. “We have challenges of commodity stock outs. Sometimes we have limited stocks and that affects our retention since we cannot dispense multi month refills which demoralizes the client” HP 001. “Stock-out of commodities such as testing kits (Determine) deters health providers from reaching out to clients for their refills since you cannot perform PrEP refills before retesting the clients” HP 008. |
| Social opportunity |
FSWs: Disclosure to a trusted relative/friend. Peer attachment at facility or community HPs: Task shift to peers based at the facility who carry out some tasks when the health providers are overwhelmed with workload. |
“…..But some friends encourage me and tell me to be strong because life is mine, take the medicine, after all you are not taking it for HIV. When God gives you marriage, you will stop this job. But just take your medicine.” FSW 006. The Peer model we use to mobilize them in the hospitals makes at least refilling PrEP easier. You find that you are alone, and you have over 300 clients to refill, it may be very hard follow and refill these clients especially when some of them don’t want to come back to hospital. So, the peer network and DICs have helped a lot ’.’ HP 005-Clinician |
Nil | Nil |
| Reflective motivation |
FSWs Confidence and trust in the ability of health providers to manage any PrEP side effects. Understanding that indeed PrEP prevents HIV acquisition if continued with by FSW. HPs: Regular reports on retention keep health providers updated. |
HPs “We have systems like weekly, monthly and quarterly reports. All those reports I think are the systems that enable retention”.HP 006. “The doctors often call and check on us, we have that kind of relationship, they can even call you to remind you that your refill time is close and ask about any problems encountered with PrEP. This has helped us to always pick the medicine in time and since I am in this business (Sex work), the message that HIV/AIDS has no cure often rings a bell in my mind and it is me that has the power to prevent it”. FSW 009. |
FSWs Attitudes of some health providers may discourage FSWs from coming for PrEP refills |
“just the attention sex workers get when they enter the hospital drives them away instead. Everyone would be looking at them and they would feel out of place ” FSW 004. |
| Automatic motivation |
FSWs Desire to establish a family. |
FSWs ’ I must swallow PrEP because I am an Orphan and I still want to raise my children” FSW 024. |
Nil | Nil |
FSWs - Female sex workers; PrEP - Pre-exposure prophylaxis; HIV - Human immunodeficiency virus; ARVs - Antiretroviral Drugs; HPs - Health Providers; MMD - Multi-Month Dispensing; HCW - Health Care Worker, DICs - Drop in centers; CBOs - Community-based organizations,STI- Sexually transmitted infections.
Qualitative Study
Participants.
A total of 24 FSWs aged ≥ 18 years receiving PrEP services at KNRH and eight (8) health providers offering PrEP services at KNRH participated in the study. The health providers included doctors (1), nurses (4), and two community health providers (PrEP Peers). Cumulatively, 24 in-depth interviews were conducted with FSWs and eight (8) Key informant interviews with health providers. Table 3 shows the perspectives of the health providers and FSWs as mapped on the COM-B model.
Perceived facilitators to continuation on PrEP services.
Psychological Capability.
FSWs expressed their understanding that sex work is associated with a high risk of HIV acquisition, which motivated them to continue PrEP services.
“What I understand by PrEP is, it is a medicine, that I use that can help prevent HIV/AIDs because as a sex worker, I have many sex partners.” FSW 013.
In addition, majority of the FSWs expressed the fear of death as an enabler to continue using PrEP.
“In this line of work (sex work), you have to encourage yourself to continue with PrEP, to avoid acquisition of HIV and death.” FSW 001.
Also, health providers had adequate knowledge on PrEP screening, eligibility criteria, and follow-up guidelines for PrEP which enabled the provision of appropriate information to PrEP recipients. In addition, they reported that most times, evaluation for PrEP services was also integrated with screening and management for other medical conditions such as sexually transmitted diseases which further enhanced continuation on PrEP services.
“PrEP is the use of ARVs to prevent the likely hood of HIV infection among high-risk HIV negative individuals. So, PrEP is taken as long as one continues to be at risk of contracting HIV.” HP 001-Counsellor
“When FSWs come here, we are able to offer PrEP, in addition, we also assess for other diseases, we offer general treatment, and this keeps them interested to come back” HP 002- Clinician.
Physical Opportunity.
Both health providers and FSWs acknowledged the role played by the supportive community structures in ensuring continuation on PrEP services. The presence of PrEP peer leaders at both the facility and established drop-in centers managed by the community-based organizations (CBOs) was a major facilitator. The peers supported in client mobilization, screening, and follow-up. In addition, the drop-in centers bring PrEP services closer to the target population including PrEP refills.
“I thank the management of drop-in centers (DICs) because, you may be stressed over a man who had sex with you, beaten you and not paid you, you come here, you are counselled, given something to eat, get your PrEP and bed to rest”. FSW 006.
“Like I said that we work with CBOs and peer leaders. All clients who are initiated at that facility are attached to peers who are key to their follow-up.” HP 006 -Counsellor.
Social Opportunity.
The health providers and FSWs believe that engagement of FSWs as peer supporters for continuation on PrEP services enables task shifting and relieves workload from the health providers. But also, the FSWs trust their peers to reach them in the community to provide PrEP refills.
“The peer model we use to mobilize FSWs in the hospital makes refilling PrEP easier. You find that you are alone, and you have over 300 clients to refill, it may be very hard to follow-up and refill these clients especially when some of them do not want to come back to hospital. So, the peer network and DICs have helped a lot “HP 005-Clinician.
“Sometimes the Peers bring us the medicine. when you fail to come back to the hospital. ” FSW 001.
Reflective Motivation.
Confidence and trust in the ability of the health providers to manage any side effects due to PrEP motivated FSWs to continue PrEP services.
“The doctors often call and check on us, we have that kind of relationship, they can even call you to remind you that your refill time is close and ask about any problems encountered with PrEP “. FSW 009.
Also, when FSWs are knowledgeable about the ability of PrEP to avert HIV acquisition, all of them are motivated to continue with PrEP services FSW 009.
“And most people say, “that girl is spoilt, she is a prostitute but in spite of that, she is HIV negative” but why is it so? This is because of PrEP” FSW 020.
Automatic reflection.
Most FSWs without children expressed their desire to establish a family as a motivator to continue PrEP services by being healthy while the ones with children wanted to stay negative to take care of their children.
“I must swallow PrEP because I am an orphan and still want to raise my children” FSW 024.
Female sex workers and health providers reported barriers to continuation on PrEP.
Psychological capacity.
Female sex workers lack adequate knowledge on PrEP medicine such as possible side effects were a barrier to continuation on PrEP services.
“Sometimes, I think the PrEP medicines stopped me from getting pregnant. I want to have a child, but it is not happening’ FSW 015.
Many FSWs felt there was inadequate community awareness about PrEP services. This requires them to give explanations to prospective customers, friends and family about PrEP and its benefits. The situation is worsened by the packaging that is like that of ARVs.
“Many people don’t know about PrEP, when they see the drug container, they may think they are antiretroviral therapy.” FSW 011.
“May be, the doctors need to further sensitize the people in the community about PrEP so that they can also be educated about it and begin to take it. They should go to different communities sensitizing people so that they can also benefit from the medication.” FSW 003.
Physical opportunities.
The majority of FSWs noted substance abuse as a key hindrance of retention on PrEP. The drugs such as alcohol interfere with their adherence to health worker instructions and subsequently impair continuation on PrEP services.
“I started drinking alcohol because of the kind of work I do. You may get a customer who first wants you to get drank. People are different so you may find one who wants to first have fun with you before sex.” FSW 010.
Both FSWs and health providers agreed that the increased workload at facility and long waiting time were structural barriers to continuation on PrEP services.
“The increasing number of clients on PrEP services with no increase in the healthcare work force impairs implementation of retention on PrEP strategies with fidelity” HP 004.
Moreover, majority of the FSWs expressed the lack of privacy and restrictive health facility policies such as dress code, centralized drug picking points (Pharmacy) as barriers found at the health facility.
“When you tell them to wait for the drugs at the pharmacy, some of them leave without the drugs. This affects retention efforts.” HP 001-consellor.
All health providers agreed that stock out of key commodities such as PrEP drugs and rapid HIV testing kits hinders their efforts to retain clients on PrEP services. This interferes with the conduct of standard follow-up activities such as repeat HIV testing and supply of multi month PrEP refills.
“We have challenges of commodity stock outs. Sometimes we have limited stocks and that affects our retention since we cannot dispense multi month refills which demoralizes the client.” HP 001.
“Stock-out of commodities such as rapid HIV testing kits deters health providers from reaching out to clients for their refills since you cannot perform PrEP refills before retesting the clients.” HP 008.
Female sex workers described long distances to facility or community refill points that increase transport expenses. They expressed the desire to have integrated services brought nearer to them through establishment of more community structures given their mobile nature and increase of multi-month refills to reduce hospital visits.
“Most times what hinders me from coming is transport. We move from one place to another; we therefore need more drop-in centers.” FSW 020
“I wish they (health providers) would put in place more community places within those far to reach areas and supply PREP, condoms and other prevention services. They should supply condoms, family planning injectable, and lubricants to the sex workers.” FSW 019
Reflective motivation.
Female sex workers felt that the attitudes of some health providers discouraged them from coming for PrEP refills. There was therefore a call for more safe spaces to offer services to the FSWs.
“Just the attention sex workers get when they enter the hospital drives them away. Everyone would be looking at them and they would feel out of place. We need places where we are more accepted”. FSW 004
DISCUSSION
This explanatory sequential mixed methods study explored the trends on continuation on PrEP services among eligible FSWs as well as the barriers and facilitators of continuation on PrEP, using the COM-B model. There was high discontinuation of PrEP among FSWs with more than half-discontinuing PrEP within 15 months of initiation. However, in our cohort, early continuation on PrEP was high at 88.0% and 74.7% at one and three months respectively suggesting that the gaps are in the current strategies for long term continuation on PrEP among FSWs in Uganda. Similar high PrEP discontinuations among FSWs have been observed in other studies in sub-Saharan Africa[17, 18]. Therefore, our results suggest that there is need for more research on population specific interventions to sustain PrEP use overtime which is a critical issue in PrEP implementation[19].
Social demographic factors such as age and sex have been shown to affect continuation on PrEP services. In some studies, young users and being female were more likely to discontinue PrEP [20–22] compared to their adult and male counterparts respectively. Our study shades light on the possible role of religious beliefs and practices on persistence on PrEP services and hence the need for PrEP providers to explore PrEP recipient beliefs and address any concerns through comprehensive counselling. However, we did not find any significant association between age and continuation on PrEP services potentially because most of the study population was young.
Our qualitative study results emphasize the importance of improving PrEP knowledge among FSWs to ensure continuation on PrEP services. Understanding the use of PrEP, the side effects associated with PrEP would address stigma associated with PrEP use and mitigate PrEP discontinuations due to side effects as evidenced in South Africa [23]. In addition, PrEP programs should improve community awareness about PrEP services and address PrEP misconceptions such as PrEP recipients being mistaken for being on HIV treatment due to similarity in drug packaging [21]. Therefore, PrEP programs need to emphasize mass sensitization campaigns on PrEP for improved uptake, reduced stigmatization, and long-term continuation.
Consistence with evidence elsewhere [23, 24], our findings show that awareness of the risk associated with sex work was an enabler to continuation on PrEP services. Therefore, empowering people to accurately perceive their individual risk of HIV acquisition would lead to higher rates of PrEP continuation. Health providers should offer comprehensive education and counselling on sexual risk behavior to increase awareness and knowledge among female sex workers for long term continuation on PrEP services.
The presence of female sex worker Peers at both facility and community level was reported to enhance continuation on PrEP among FSWs and reduced workload on the health providers. The community health providers such as FSW Peers who are living through a similar experience provide psychosocial support, follow-up clients, deliver PrEP and improve client knowledge on PrEP [25].The Peers can in addition help to dispel myths, address misconceptions and provide accurate information about the benefits and importance of PrEP for female sex worker. This proactive Peer navigation has been shown to improve retention in HIV care and PrEP services and should be scaled up as we address the gap in persistence on PrEP among eligible populations [26–28].
In addition, both healthcare providers and FSWs emphasized the need for decentralized PrEP delivery through community structures such as the drop-in centers and community pharmacies to increase accessibility and continuation on PrEP services. Decentralization of PrEP delivery models enhances person centeredness and is key in demedicalisation of the services[29]. Through demedicalisation, facility level barriers to continuation on PrEP services shared by health providers and FSWs such as the increased workload, FSW adherence to a particular dress code, long waiting time during clinic visits and the frequent clinic visits also observed in other sub-Saharan countries such as Kenya [30] can be addressed.
Sex work is associated with high mobility [31] and our study results further emphasize its impact on FSWs adherence to PrEP refill schedules. Majority of the FSWs acknowledged that this occupational context of their work significantly influenced continuation on PrEP patterns. The findings underscore the quick adoption of six-month PrEP refills by the PrEP programs to reduce clinic visit frequency. Multi month drug refills as seen in HIV programs in SSA have improved retention in care among people living with HIV [32, 33] and the same approach could benefit PrEP programs. Also, the adoption of other PrEP options such as long acting cabotegravir in the PrEP program would address the pill burden barrier [34] and reduce clinic visits in this highly mobile population.
The study results showed how critical it is to integrate of PrEP services with other health care services such as family planning, substance use treatment, sexually transmitted treatment (STI) treatment, HIV testing and mental health support to enhance continuation on PrEP. The intersection of substance use and failure to return for PrEP refills reported by the FSWs emphasizes the importance of extra resources to enhance service integration in HIV clinics and primary care settings. PrEP programs should adopt the integrated approach to holistically address the needs of the clients, improves service access and utilization as evidenced elsewhere [35, 36].
Poor attitude of health providers towards FSWs and inconvenient clinic operation hours that impair access to prevention services were major barriers to continuation on PrEP services in this population. Most FSWs reported working during the night and rest during the day. However, health providers continued to schedule daytime appointments due to the inflexible clinic policies. Such discriminatory treatment of FSWs that may even involve denial of treatment after gender based violence and hostility from public sector health providers has also been found in studies conducted in Uganda, Kenya ,Zimbabwe and South Africa [37–39]. To address this problem, training and sensitization of public health care workers should constitute some of the multilevel interventions [38] aimed at ensuring the delivery of non-discriminatory, private and safe heath care services.
Strengths and Limitations.
The use of multiple sources of data in the qualitative component (Health care providers, Female Sex Workers) and use of the COM-B model to guide data collection and analysis was a strength for the study [40].
The study was conducted in a single public health hospital offering PrEP services according to the Uganda national guidelines in an urban setting. Since the clinic is found in a national referral hospital, which receives clients from all over the country, we believe that the study findings are generalizable to other low-income countries.
Conclusion
PrEP continuation rates remain low among FSWs. Integration of PrEP with other services, improved health provider knowledge on PrEP and scale up of community PrEP delivery structures will facilitate continuation on PrEP. In addition, interventions should address barriers to PrEP continuation such low community awareness on PrEP, substance abuse and health facility level barriers for the scale of the PrEP program among FSWs in Uganda.
Acknowledgements.
We appreciate the research assistants, the staff and administration of both Kiruddu National referral hospital and Makerere University Joint AIDS Program who supported this study.
Funding.
The reported research was supported by the Fogarty International Center of the National Institutes of Health under Award Number D43TW010037.
Abbreviations
- ART
Antiretroviral therapy
- FSW
Female sex worker
- HIV
Human Immune virus
- KNRH
Kiruddu national referral hospital
- MJAP
Makerere university Joint AIDS Program
- MOH
Ministry of health
- UAC
Uganda AIDS commission
- PrEP
Pre exposure prophylaxis
- PEP
Post exposure prophylaxis
- PLHIV
People living with HIV
- CDC
Center for disease control and prevention
- WHO
World health Organization
- HP
Health provider
Footnotes
Competing interests.
The authors declare that they have no competing interests.
Ethics approval and consent to participate.
The study was approved by The AIDS Support Organization (TASO) institutional review board (IRB) number TASO- 2022–190 and Uganda National council of science and technology (UNCST) number HS2771ES. We obtained written permission from Kiruddu national referral hospital to access clients’ medical records for the quantitative component and written informed consent was obtained from participants involved in the qualitative study after provision of comprehensive information about the study. For participants who could not read or write, informed consent was obtained in presence of an impartial witness. All study participants were adults above 18 years of age. The steps taken to maintain participants’ confidentiality included replacing names with unique study identification numbers and always keeping participant data (audio recordings and the abstracted database) on password-protected computers. Principles expressed in the Declaration of Helsinki were followed in the conduct of this study.
Availability of data and materials.
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Contributor Information
Samuel Kawuma, Makerere University Joint AIDS Program.
Rogers Katwesigye, Makerere University Joint AIDS Program.
Happy Walusaga, Makerere University Joint AIDS Program.
Praise Akatukunda, Makerere University Joint AIDS Program.
Joan Nangendo, Infectious Diseases Research Collaboration.
Charles Kabugo, Kiruddu National Referral Hospital.
Moses R. Kamya, Infectious Diseases Research Collaboration
Fred C. Semitala, Makerere University Joint AIDS Program
References
- 1._UNAIDS, Special analysis,2022 2022. [Google Scholar]
- 2.MOH. Uganda Population Based HIV Impact Assessment 2020. [cited 2023 March 17]; Available from: https://www.mediacentre.go.ug/media/release-preliminary-results-2020-uganda-population-based-hiv-impact-assessment.
- 3.UAC, Synthesis,Consolidation and Building Consensus on Key and Priority Population Size Estimation numbers in Uganda. 2019.
- 4.WHO, Consolidated guidelines on the use of antiretroviral drugs for treating and preventing HIV infection. 2016: Geneva, Switzerland. [PubMed]
- 5.Thigpen M.C., et al. , Antiretroviral preexposure prophylaxis for heterosexual HIV transmission in Botswana. New England journal of medicine, 2012. 367(5): p. 423–434. [DOI] [PubMed] [Google Scholar]
- 6.Baeten J.M., et al. , Antiretroviral prophylaxis for HIV prevention in heterosexual men and women. New England journal of medicine, 2012. 367(5): p. 399–410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ahmed N., Pike C., and Bekker L.G., Scaling up pre-exposure prophylaxis in sub-Saharan Africa. Curr Opin Infect Dis, 2019. 32(1): p. 24–30. [DOI] [PubMed] [Google Scholar]
- 8.Witte S.S., et al. , PrEP acceptability and initiation among women engaged in sex work in Uganda: Implications for HIV prevention. EClinicalMedicine, 2022. 44: p. 101278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Joint Annual AIDS Review Report. 2022.
- 10.Ddaaki W., et al. , Qualitative assessment of barriers and facilitators of PrEP use before and after rollout of a PrEP program for priority populations in South-central Uganda. AIDS and Behavior, 2021. 25: p. 3547–3562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Michie S., Van Stralen M.M., and West R., The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implementation science, 2011. 6(1): p. 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Timlin D., McCormack J.M., and Simpson E.E., Using the COM-B model to identify barriers and facilitators towards adoption of a diet associated with cognitive function (MIND diet). Public Health Nutrition, 2021. 24(7): p. 1657–1670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Boyd J., et al. , Utility of the COM-B model in identifying facilitators and barriers to maintaining a healthy postnatal lifestyle following a diagnosis of gestational diabetes: a qualitative study. BMJ open, 2020. 10(8): p. e037318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Creswell J.W. and Poth C.N., Qualitative inquiry and research design: Choosing among five approaches. 2016: Sage publications. [Google Scholar]
- 15.Boyatzis R.E., Transforming qualitative information: Thematic analysis and code development. 1998: sage. [Google Scholar]
- 16.Braun V. and Clarke V., Using thematic analysis in psychology. Qualitative research in psychology, 2006. 3(2): p. 77–101. [Google Scholar]
- 17.Rao A., et al. , Persistence on oral pre-exposure prophylaxis (PrEP) among female sex workers in eThekwini, South Africa, 2016–2020. PLoS One, 2022. 17(3): p. e0265434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rugira E., Biracyaza E., and Umubyeyi A., Uptake and Persistence on HIV Pre-Exposure Prophylaxis Among Female Sex Workers and Men Having Sex with Men in Kigali, Rwanda: A Retrospective Cross-Sectional Study Design. Patient preference and adherence, 2023: p. 2353–2364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Spinelli M.A. and Buchbinder S.P., Pre-exposure prophylaxis persistence is a critical issue in PrEP implementation. 2020, Oxford University Press US. p. 583–585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Spinelli M.A., et al. Missed visits associated with future preexposure prophylaxis (PrEP) discontinuation among PrEP users in a municipal primary care health network. in Open forum infectious diseases. 2019. Oxford University Press US. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kagaayi J., et al. , Uptake and retention on HIV pre‐exposure prophylaxis among key and priority populations in South‐Central Uganda. Journal of the International AIDS Society, 2020. 23(8): p. e25588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Huang Y.-L.A., et al. , Persistence with human immunodeficiency virus pre-exposure prophylaxis in the United States, 2012–2017. Clinical Infectious Diseases, 2021. 72(3): p. 379–385. [DOI] [PubMed] [Google Scholar]
- 23.Pillay D., et al. , Factors influencing uptake, continuation, and discontinuation of oral PrEP among clients at sex worker and MSM facilities in South Africa. PloS one, 2020. 15(4): p. e0228620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mayanja Y., et al. , Oral pre‐exposure prophylaxis preference, uptake, adherence and continuation among adolescent girls and young women in Kampala, Uganda: a prospective cohort study. Journal of the International AIDS Society, 2022. 25(5): p. e25909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Edwards A.J., et al. , Impact of community health worker intervention on PrEP knowledge and use in Rakai, Uganda: A mixed methods, implementation science evaluation. International journal of STD & AIDS, 2022. 33(11): p. 995–1004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Spinelli M.A., et al. , A panel management and patient navigation intervention is associated with earlier PrEP initiation in a safety-net primary care health system. Journal of acquired immune deficiency syndromes (1999), 2018. 79(3): p. 347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Oldenburg C.E., et al. , Engagement with peer health educators is associated with willingness to use pre-exposure prophylaxis among male sex workers in Ho Chi Minh City, Vietnam. AIDS Patient Care and STDs, 2014. 28(3): p. 109–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Young L.E., et al. , PrEP Chicago: A randomized controlled peer change agent intervention to promote the adoption of pre-exposure prophylaxis for HIV prevention among young Black men who have sex with men. Clinical Trials, 2018. 15(1): p. 44–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Janamnuaysook R., et al. , Demedicalisation of HIV interventions to end HIV in the Asia–Pacific. Sexual Health, 2021. 18(1): p. 13–20. [DOI] [PubMed] [Google Scholar]
- 30.Ongolly F.K., et al. , “I just decided to stop:” Understanding PrEP discontinuation among individuals initiating PrEP in HIV care centers in Kenya. Journal of acquired immune deficiency syndromes (1999), 2021. 87(1): p. e150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Scorgie F., et al. , Socio-demographic characteristics and behavioral risk factors of female sex workers in sub-saharan Africa: a systematic review. AIDS and Behavior, 2012. 16: p. 920–933. [DOI] [PubMed] [Google Scholar]
- 32.Mody A., et al. , Improved retention with 6-month clinic return intervals for stable human immunodeficiency virus-infected patients in Zambia. Clinical Infectious Diseases, 2018. 66(2): p. 237–243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Keene C.M., et al. , ‘Only twice a year’: a qualitative exploration of 6-month antiretroviral treatment refills in adherence clubs for people living with HIV in Khayelitsha, South Africa. BMJ open, 2020. 10(7): p. e037545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ssuna B., et al. , Factors associated with willingness to use oral pre-exposure prophylaxis (PrEP) in a fisher-folk community in peri-urban Kampala, Uganda. BMC public health, 2022. 22(1): p. 468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ramchandani M.S., et al. , A De-medicalized Model to Provide PrEP in a Sexual Health Clinic. JAIDS Journal of Acquired Immune Deficiency Syndromes, 2022: p. 10.1097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ndawula P., et al. , P4. 105 Intergrating HIV Counselling and Testing Activities with STI Services Increases Acess and Utilisation to HIV/AIDS Care and Support Services. Sexually Transmitted Infections, 2013. 89(Suppl 1): p. A320–A321. [Google Scholar]
- 37.Wanyenze R.K., et al. , “When they know that you are a sex worker, you will be the last person to be treated”: perceptions and experiences of female sex workers in accessing HIV services in Uganda. BMC international health and human rights, 2017. 17(1): p. 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Muwonge T.R., et al. , Health care worker perspectives of HIV Pre-exposure prophylaxis service delivery in central Uganda. Frontiers in Public Health, 2022. 10: p. 658826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Scorgie F., et al. , ‘We are despised in the hospitals’: sex workers’ experiences of accessing health care in four African countries. Culture, health & sexuality, 2013. 15(4): p. 450–465. [DOI] [PubMed] [Google Scholar]
- 40.Patton M.Q., Qualitative research & evaluation methods: Integrating theory and practice. 2014: Sage publications. [Google Scholar]