Abstract
Background
Endothelial cell injury is one of the important pathogenic mechanisms in thrombotic diseases, and also neutrophils are involved. MicroRNAs (miRNAs) have been demonstrated to act as essential players in endothelial cell injury, but the potential molecular processes are unknown. In this study, we used cellular tests to ascertain the protective effect of miR-328-3p on human umbilical vein endothelial cells (HUVECs) treated with oxygen-glucose deprivation (OGD).
Methods
In our study, an OGD-induced HUVECs model was established, and we constructed lentiviral vectors to establish stable HUVECs cell lines. miR-328-3p and Toll-like receptor 2 (TLR2) interacted, as demonstrated by the dual luciferase reporter assay. We used the CCK8, LDH release, and EdU assays to evaluate the proliferative capacity of each group of cells. To investigate the expression of TLR2, p-P65 NF-κB, P65 NF-κB, NLRP3, IL-1β, and IL-18, we employed Western blot and ELISA. Following OGD, each group’s cell supernatants were gathered and co-cultured with neutrophils. An immunofluorescence assay and Transwell assay have been performed to determine whether miR-328-3p/TLR2 interferes with neutrophil migration and neutrophil extracellular traps (NETs) formation.
Results
In OGD-treated HUVECs, the expression of miR-328-3p is downregulated. miR-328-3p directly targets TLR2, inhibits the NF-κB signaling pathway, and reverses the proliferative capacity of OGD-treated HUVECs, while inhibiting neutrophil migration and neutrophil extracellular trap formation.
Conclusions
miR-328-3p inhibits the NF-κB signaling pathway in OGD-treated HUVECs while inhibiting neutrophil migration and NETs formation, and ameliorating endothelial cell injury, which provides new ideas for the pathogenesis of thrombotic diseases.
1. Introduction
It is generally recognized that Virchow’s triad is the main factor contributing to thrombosis [1], in which vascular endothelial cell injury occupies an important position [2]. Many studies have shown that ischemia and hypoxia can trigger an inflammatory response, which is an essential pathological cause of endothelial cell injury. Ischemia and hypoxia activate multiple pathways that damage endothelial cells, while neutrophils accumulate at the site of injury [3], exacerbating the inflammatory response. Despite considerable progress in understanding the mechanisms of endothelial cell injury in thrombotic diseases, effective biomarkers to reverse ischemia-hypoxia-induced cell injury are still lacking. Therefore, it is crucial to focus on the inflammatory response-related mechanisms behind endothelial cell injury, which may facilitate the development of novel drugs.
Neutrophils are derived from hematopoietic stem cells of the bone marrow, which are chemotactic, phagocytic, and bactericidal and are important in nonspecific cellular immunity. Large extracellular reticular structures known as neutrophil extracellular traps (NETs) are released by neutrophils, in response to inflammatory stimuli or hypoxia, etc [4]. Dominated by chromatin DNA, they contain a variety of enzymes and proteins, especially Myeloperoxidase (MPO), Neutrophil Elastase (NE), Histone G, Histone H3 Citrulline (H3Cit), and neutrophil antimicrobial proteins [5]. Upon stimulation, neutrophils become active and have the ability to damage endothelium cells. In addition, NETs can be activated by activated endothelial cells, and NETs produce endothelial cytotoxicity. Neutrophil and endothelial cell activation form a vicious circle. Thus, neutrophil migration and the NETs formation are closely associated with the mechanism of endothelial cell injury.
MicroRNAs (miRNAs), which influence post-transcriptional gene regulation, consist of 18–25 nucleotides and are small, highly conserved non-coding RNAs. MiRNAs can bind to the 3’-UTR of target genes to inhibit the protein levels of target genes thereby regulating cell biological functions such as cell proliferation, differentiation, apoptosis, and disease progression [6]. For example, it was discovered that overexpressing miR-126 inhibited oxidative stress and inflammation in HUVECs, a process that primarily involves activation of the SIRT1/Nrf2 signaling pathway [7]. According to Zhang et al., when H9c2 cells are hypoxic, interfering with microRNA-495 prevents apoptosis via targeting NFIB [8]. It has recently been found that miR-328-3p affects the beginning and progression of diseases, particularly in a range of malignancies [9–11]. Nonetheless, it is still unclear how miR-328-3p prevents vascular endothelial cell damage in ischemia-hypoxic environments.
Toll-like receptors (TLRs) are single transmembrane non-catalytic proteins that have been implicated in a range of inflammations and diseases, primarily recognizing pathogens and participating in damage-associated molecular patterns of innate immunity [12]. It has been found that TLR2 is abundant in endothelial cells in a variety of tissues and is required for pro-inflammatory endothelial cell function. TLR2 is closely related to the occurrence of endothelial cell inflammation and injury [13, 14]. TLR2 dimerization can trigger the nuclear factor-kappa B (NF-κB) pathway, which specifically binds DNA and regulates protein transcription [15], which triggers the transcription of various target genes and controls and participates in cell cycle progression, inflammatory responses, and inhibition of cell adhesion and apoptosis [16]. More research is necessary to fully understand how miR-328-3p regulates vascular endothelial cell damage by influencing the NF-κB pathway via TLR2.
Therefore, to simulate the ischemic-hypoxic environment in vitro, the oxygen-glucose deprivation approach was employed in this study. We explored the protective role of miR-328-3p against inflammatory injury in HUVECs through the TLR2 /NF-κB signaling pathway, as well as the role of neutrophils in this process. The significance of miR-328-3p in vascular endothelial cells and novel insights into the cellular molecular mechanisms of thrombotic disorders are both supported by our findings.
2. Materials and methods
2.1 Cell culture
The medium used for cell culture was Dulbecco’s Modified Eagle Medium (DMEM, C11995500BT, Gibco, China), which was enhanced with 1% penicillin-streptomycin (15140–122, Gibco, USA) and 5% fetal bovine serum (FBS, A3160801, Gibco, UK). HUVECs (FH1122, STR 20170721–05, Fuheng Biology, Shanghai, China) were cultivated in an incubator with 5% CO2 and a temperature of 37°C. When the cells were fused to 80%, we digested and passaged them with 0.25% Trypsin-EDTA (25200–056, Gibco, Canada). Tests were performed after the cell traits were stabilized by 3 consecutive passages.
2.2 Cell transfection
Introduction of lentivirus (miR-328-3p mimic, miR-328-3p inhibitor, negative control mimic, and negative control inhibitor) (GenePharma, China) into cells and screening by Puromycin Solution (BL528A, Biosharp, China) to obtain stably expressing cell lines. The vector we used were all LV3 (H1/GFP&Puro) and the sequences are shown in Table 1.
Table 1. Sequences for lentivirus transfection.
| Name | Sequence (5’-3’) |
|---|---|
| miR-328-3p mimic | CTGGCCCTCTCTGCCCTTCCGT |
| negative control mimic | TTCTCCGAACGTGTCACGT |
| miR -328-3p inhibitor | ACGGAAGGGCAGAGAGAGGGCCAG |
| negative control inhibitor | TTCTCCGAACGTGTCACGT |
2.3 Oxygen-glucose deprivation (OGD) model
Glucose-free DMEM (D6540, Solarbio, China) was added after washing the cells once with 1 × phosphate buffered solution (PBS). To reach anaerobic conditions, groups of cells were placed in an anaerobic incubator for 30 min to reduce the oxygen concentration to 1%. We maintained conditions of 94% N2, 5% CO2, and 1% O2, and after 6h of oxygen-glucose deprivation, the basal medium was added in place of Glucose-free DMEM. For a full day, the cells were grown in standard conditions. A total of 6 groups were obtained: Normal, OGD-Normal, OGD-NC mimic, OGD-mimic, OGD-NC inhibitor, and OGD-inhibitor.
2.4 Cell Counting Kit-8 (CCK-8) assay
2×103 cells were inoculated in 96-well plates. After OGD, we used the cell Counting kit -8 kit (C0038, Beyotime Biotechnology, Shanghai, China) to detect cell proliferation. After adding reagents, place in an incubator at 37°C for 1.5 hours.
2.5 Lactate dehydrogenase (LDH) releases assay
Membrane integrity and cell viability can be determined by LDH release assays, and we use the LDH assay kit (A020-2-2, Nanjing Jiancheng Bioengineering Institute, China) to detect cellular damage. After OGD, we collected the cell supernatants, operated according to the kit instructions, and measured the absorbance value at 450nm using a microplate reader.
2.6 5-Ethynyl-2ʹ-deoxyuridine (EdU) assay
We inoculated each group of cells at 2×103 per well in a 96-well plate. After OGD, we added the EdU working solution (G1603, Servicebio, China) and then used 4% paraformaldehyde (BL539A, Biosharp, China) and 0.5% Triton (P0096, Beyotime Biotechnology, Shanghai, China) according to the instructions. We treated the cells with Apollo reaction solution for 30 min under light-avoidance conditions. After staining with Hoechst33342, 3 random fields were taken under a fluorescence microscope. The ratio of red fluorescence (EdU-stained cells) to blue fluorescence (Hoechst 33,342-stained cells) in the obtained image indicates the percentage of EdU-positive cells.
2.7 Dual-luciferase reporter assay
The Dual-luciferase reporter assay was employed to identify possible binding between miR-328-3p and the 3’-UTR of TLR2. Wild-type (WT) or mutant (MUT) TLR2 3’-UTR sequences were inserted into the vectors, and after transfection for a specific time, we measured luciferase activity and normalized it (Promega, USA). The difference between the WT and MUT 3’-UTR sequences is that the WT is base complementary paired with the miRNA, the MUT is not. The vector we used were all psiCHECK™-2-Vector (GenePharma, China) and the sequences are shown in Table 2.
Table 2. Sequences for dual-luciferase reporter assay.
| Name | Sequence (5’-3’) |
|---|---|
| hsa-TLR2-miR-328-3p-WT | ggttgacttcatggatgcagaacccatggatatagAGGGCCAactgtaatctgtagcaactggcttagt |
| hsa-TLR2-miR-328-3p-MUT | ggttgacttcatggatgcagaacccatggatatagTCCCGGTactgtaatctgtagcaactggcttagt |
2.8 Quantitative real-time PCR (qRT-PCR)
TRIzol (R0016, Beyotime Biotechnology, Shanghai, China) was used to extract total RNA from six groups of cells, and RNA concentration and purity were measured by UV spectrophotometer. To analyze miR-328-3p expression, we synthesized cDNA using the stem-loop method (B532453, Sangon Biotech, China). The real-time RT-PCR was performed using the microRNAs qPCR Kit (SYBR Green Method) (B639271, Sangon Biotech, China) according to the instructions, using U6 as Endogenous Reference Genes Primers. For the analysis of TLR2, TLR3, TLR4, TLR9, NF-κB, NLRP3, IL-1β, and IL-18, a PrimeScript™ RT reagent Kit with gDNA Eraser (Perfect Real Time) (Cat# RR047A, Takara, China) was used to synthesize cDNA. Using β-actin as the Endogenous Reference Genes Primers, cDNA was evaluated using TB Green® Premix Ex Taq™ II (Tli RNaseH Plus) (Cat# RR820A, Takara, China) for real-time RT-PCR. Each sample was replicated three times. We used the 2-ΔΔCt method to calculate qRT-PCR Ct values. All primers (Table 3) were ordered from Sangon Biotech.
Table 3. Primer sequences for qRT-qPCR.
| Gene | Forward 5’-3’ | Reverse 5’-3’ |
|---|---|---|
| miR-328-3p | AACAATCTGGCCCTCTCTGC | CAGTGCAGGGTCCGAGGT |
| U6 | CTCGCTTCGGCAGCACA | AACGCTTCACGAATTTGCGT |
| TLR2 | AAGCAGCATATTTTACTGCTGG | CCTGAAACAAACTTTCATCGGT |
| TLR3 | CCTGGTTTGTTAATTGGATTAACGA | TGAGGTGGAGTGTTGCAAAGG |
| TLR4 | TTTGGACAGTTTCCCACATTGA | AAGCATTCCCACCTTTGTTGG |
| TLR9 | TGGTGTTGAAGGACAGTTCTCTC | CACTCGGAGGTTTCCCAGC |
| P65 NF-κB | AACAGAGAGGATTTCGTTTCCG | TTTGACCTGAGGGTAAGACTTCT |
| NLRP3 | CGTGAGTCCCATTAAGATGGAGT | CCCGACAGTGGATATAGAACAGA |
| IL-1β | ATGATGGCTTATTACAGTGGCAA | GTCGGAGATTCGTAGCTGGA |
| IL-18 | GCTGAAGATGATGAAAACCTGG | CAAATAGAGGCCGATTTCCTTG |
| β-actin | CCTGGCACCCAGCACAAT | GGGCCGGACTCGTCATAC |
2.9 Protein extraction and Western blot analysis
We collected six sets of cell samples and lysed proteins with RIPA buffer (R0010, Solarbio, China) that contained Aprotinin and PMSF. Protein concentrations were determined by the BCA method, SDS-PAGE electrophoresis was performed using 7.5% and 12.5% separation gels (PG111, PG113, Epizyme Biotech, China), respectively, and the samples were transferred to PVDF membranes. Following blocking, we incubated the membranes with primary antibodies against TLR2 (Catalog No. 66645-1-Ig, Proteintech, China), P65 NF-κB (Catalog No. 10745-1-AP, Proteintech, China), p-P65 NF-κB (Cat.#: AF2006, Affinity Biosciences, China), NLRP3 (#M035175, abmart, China), IL-1β (Catalog No. 16806-1-AP, Proteintech, China), IL-18 (Catalog No. 60070-1-Ig, Proteintech, China), and β-actin (Catalog No. 20536-1-AP, Proteintech, China) at 4°C overnight. After washing in TBST, we incubated for 1 h using secondary HRP antibodies (Catalog No. SA00001-1, Catalog No. SA00001-2, Proteintech, China). The samples were exposed to a developer using ECL Plus reagent (P0018S, Beyotime Biotechnology, Shanghai, China). Grey-scale values were analyzed using Images-J to quantify protein expression levels based on band density.
2.10 Extraction of neutrophils
Peripheral whole blood was taken from healthy adults and anticoagulated with EDTA. Neutrophils were isolated using Polymorphprep (AS1114683, Oslo, Norway) and centrifuged at 500g for 30 minutes, following the isolation procedure as instructed. Carefully extract neutrophils, wash twice with PBS resuspension, and centrifuge at 400g for 10 minutes. Add erythrocyte lysis solution (R1010, Solarbio, China) and lyse at 4°C for 15 minutes, centrifuge and discard supernatant until no red color is present in the precipitate. We use a cell counter to count the number of cells. Healthy adults were recruited from March 1 to April 1, 2023, and all received written informed consent. The first affiliated Hospital of Gannan Medical University’s Institutional Review Board and Ethics Committee approved the study (Ganzhou China, ethical approval No. LLSC-2023022801).
2.11 Transwell migration assay
We inoculated each group of cells in 24-well plates and collected cell supernatants after OGD. After centrifugation, we added the supernatant into a new 24-well plate and then placed transwell chambers with a membrane pore size of 8 μm. Neutrophils were diluted to 106 cells per ml and 200 μl was aspirated and added to the upper chamber. After 12 hours, the cytosol of the lower chamber was collected and counted using a cell counter.
2.12 Cell immunofluorescence
The number of neutrophils was set at 4×106 cells per ml, and 100 μl of each well was inoculated into 24-well plates with Polylysine slides. We collected cell cultures from each group after OGD. After centrifugation, we collected 400 μl of supernatants and added them to 24-well plates that were seeded with neutrophils and incubated in a 5% CO2, 37°C incubator. After overnight incubation, 4% paraformaldehyde was added slowly along the plate wall in each well. After permeabilizing by 0.5% Triton at room temperature, we blocked the non-specific antigen with the Goat Blocking Buffer. We mixed equal amounts of H3Cit (ab5013, Abcam) and MPO (Catalog No. 66177-1-Ig, Proteintech, China) primary antibodies, and added the primary antibody mixture to each well. After incubating at 4°C overnight, we added the secondary antibody (Catalog No. SA00013-1, Catalog No. SA00013-4, Proteintech, China) and incubated it for 1 hour in a wet box protected from light. Finally, stained with DAPI solution and observed by fluorescence microscope.
2.13 Enzyme-linked immunosorbent assay (ELISA)
We collected the supernatant after the different treatments. The instructions for the ELISA assay were followed in order to measure the levels of IL-1β (KE00021, Proteintech, China), IL-18 (KE00193, Proteintech, China), MPO (KE00171. Proteintech, China), and NE (JL12352, Jonln, China).
2.14 Statistical analysis
We use means ± standard deviation (SD) to present all data. To compare data between the two independent groups, we employ Student’s t-test. SPSS 21.0 statistical software (IBM, USA) and GraphPad Prism 8.0 (La Jolla, USA) were used to analyze the experimental data and picture processing. A statistically significant difference was defined as P<0.05.
3. Result
3.1 In HUVECs treated with OGD, overexpression of miR-328-3p reverses damage
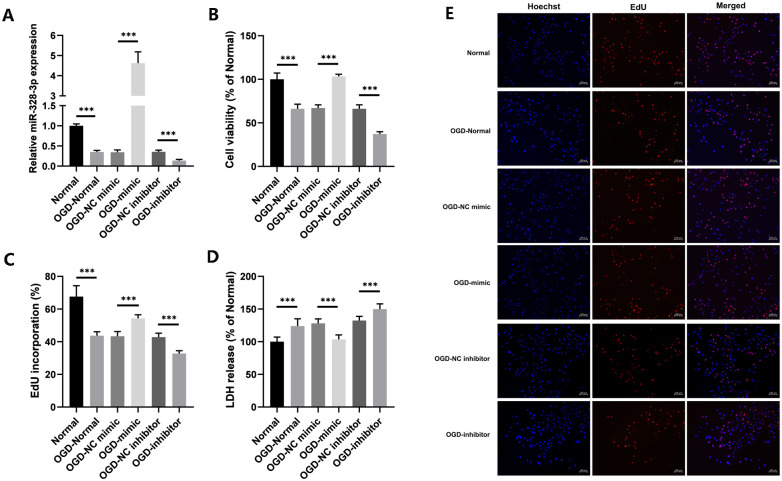
According to the qRT-PCR results, OGD-treated HUVECs expressed less miR-328-3p than normal culture did, indicating that OGD treatment significantly reduced the expression of miR-328-3p. Following transfection, the qRT-PCR findings demonstrated a substantial change in the expression of miR-328-3p between the OGD-mimic and OGD-inhibitor groups and the OGD-NC mimic and OGD-NC inhibitor groups (Fig 1A). CCK8, LDH release, and EdU assays were used to assess the cell proliferative capacity in each group. The results of CCK8 and EdU assay showed that OGD treatment was able to reduce cell viability compared to the Normal group. The OGD-mimic group’s ability for cell proliferation was higher than that of the OGD-NC mimic group; in contrast, the OGD-inhibitor group displayed the opposite trend (Fig 1B, 1C and 1E). The LDH release assay showed that OGD treatment could promote cellular LDH release. The percentage of LDH release in the OGD-mimic or OGD-inhibitor groups was significantly reduced or increased compared to the OGD-NC mimic or OGD-NC inhibitor groups (Fig 1D). In conclusion, following OGD treatment, miR-328-3p expression was decreased in HUVECs. In the meantime, HUVECs damage was reversed and cell viability was increased by miR-328-3p overexpression.
Fig 1. miR-328-3p expression is down-regulated and promotes cell proliferation in OGD-treated HUVECs.
A. qRT-qPCR was used to detect the expression of miR-328-3p in OGD-treated cells in each group. B. Cell viability of each group was detected by CCK8 assay. C and E. EdU assays were performed to measure the effect of miR-328-3p on the proliferation of OGD-treated HUVECs. D. Detection of LDH release from OGD-treated cells in each group. Data are presented as the mean ± SD (n = 3). ***P < 0.001.
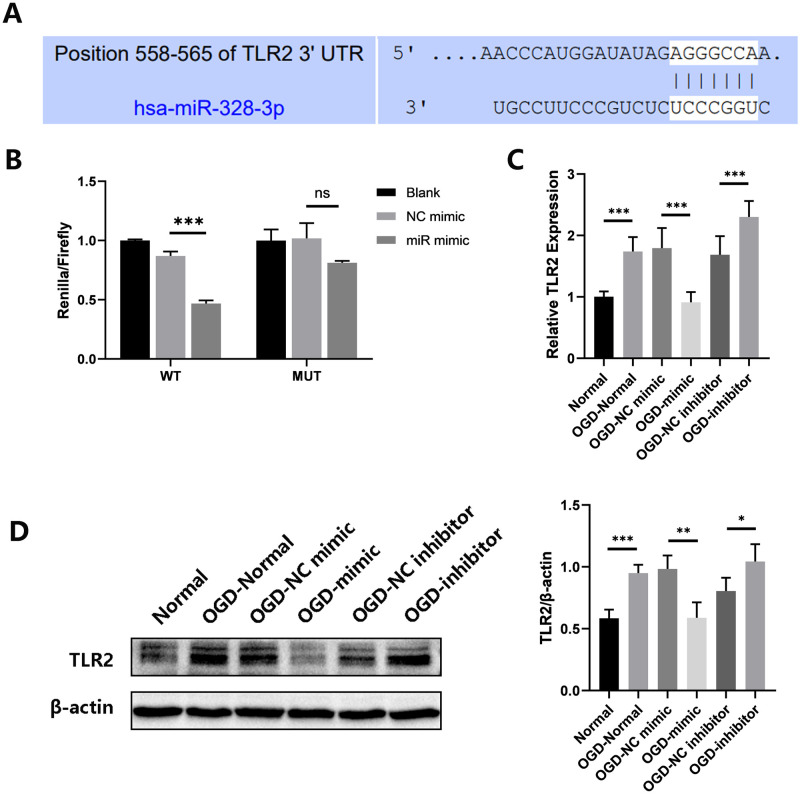
3.2 The miR-328-3p targets TLR2 in HUVECs treated with OGD and affects NF-κB signaling pathway expression as well as inflammation-related molecules
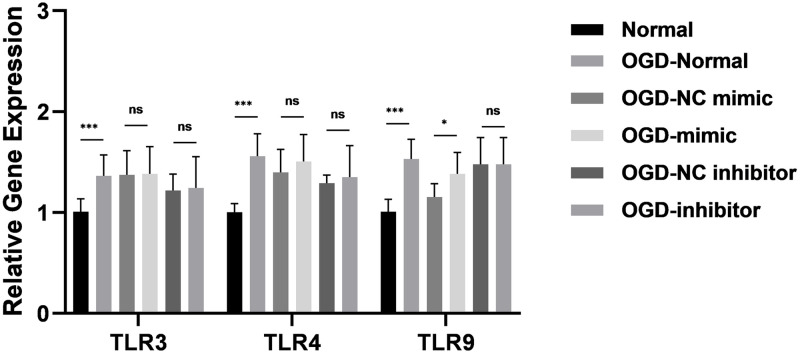
TargetScan was used to determine whether TLR2 is a potential target of miR-328-3p (Fig 2A). The Dual-luciferase reporter assay can detect whether miRNA and target protein are potentially bound. We discovered that miR-328-3p binds to the 3’-UTR of TLR2, and the 3’-UTR of TLR2 is a potential binding site for miR-328-3p (Fig 2B). OGD-treated HUVECs also showed dramatically elevated the protein and mRNA levels of TLR2, as demonstrated by Western blotting and qRT-qPCR. The TLR2 expression was markedly reduced or enhanced in the OGD-mimic group or OGD-inhibitor group compared with the OGD-NC mimic group or OGD-NC inhibitor group (Fig 2C and 2D). In addition, under the influence of OGD and miR-328-3p, we examined the expression of TLR3, TLR4, and TLR9 by qRT-PCR experiments. It was found that OGD treatment could affect the expression of TLR3, TLR4, and TLR9 in HUVECs. However, there was no correlation trend of TLR3, TLR4, and TLR9 expression in HUVECs overexpressing and interfering with miR-328-3p (Fig 3). Based on the above experiments, we detected the protein expression of NF-κB and inflammation-related molecules. The OGD-Normal group had higher levels of p-P65 NF-κB, NLRP3, IL-1β, and IL-18 expression than the Normal group, according to the results of Western blotting. However, protein expression was reduced or enhanced in the OGD-mimic group or OGD-inhibitor group compared to the OGD-NC mimic group or OGD-NC inhibitor group (Fig 4A). The qRT-qPCR results showed the same trend (Fig 4B). According to the results above, miR-328-3p binds TLR2 and suppresses TLR2 expression in OGD-treated HUVECs while influencing the expression of NF-κB signaling pathway and inflammation-related molecules.
Fig 2. miR-328-3p targets TLR2 and down-regulates TLR2 expression after OGD treatment.
A. 3’-UTR of TLR2 mRNA was predicted to be targeted by miR-328-3p. B. Dual-luciferase reporter assay detects the binding of TLR2 and miR-328-3p (n = 3). C. qRT-qPCR analyzed the mRNA expression level of TLR2 in each group (n = 3). D. Western blotting analyzed the protein expression level of TLR2 in each group (n = 4). Data are presented as the mean ± SD. **P < 0.01; ***P < 0.001; ns, no significance.
Fig 3. OGD treatment up-regulates the expression of TLR3, TLR4, and TLR9, but is not associated with miR-328-3p.
qRT-qPCR analyzed the mRNA expression level of TLR3, TLR4, and TLR9 in each group (n = 3). Data are presented as the mean ± SD. **P < 0.01; ***P < 0.001; ns, no significance.
Fig 4. miR-328-3p affects the expression of NF-κB signaling pathway and inflammation-related molecules after OGD treatment.
A. The protein expression levels of p-P65 NF-κB, NLRP3, IL-1β, and IL-18 were analyzed by Western blotting in each group (n = 4). B. The mRNA expression levels of P65 NF-κB, NLRP3, IL-1β, and IL-18 in each group were analyzed by qRT-qPCR (n = 3). Data are presented as the mean ± SD. *P < 0.05; **P < 0.01; ***P < 0.001.
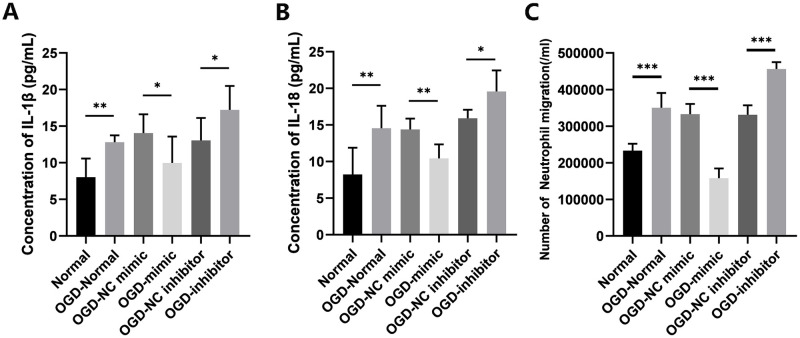
3.3 Overexpression of miR-328-3p attenuates neutrophil migration after OGD treatment
It is established that IL-1β and IL-18 mediate neutrophil recruitment [17] and amplify inflammatory responses. In order to investigate the impact of miR-328-3p overexpression on neutrophils under OGD induction, we used ELISA to identify IL-1β and IL-18 secretion in the cell supernatants after OGD treatment. The OGD-Normal group released more IL-1β and IL-18 than the Normal group, and the results are identical to the Western blotting results. However, compared with the OGD-NC mimic group or OGD-NC inhibitor group, the release was reduced or enhanced in the OGD-mimic group or OGD-inhibitor group (Fig 5A and 5B). After neutrophil isolation and purification, neutrophil transwell co-culture experiments confirmed that OGD-treated cell supernatants were able to increase neutrophil migration compared to normal culture. The OGD-mimic group showed a much lower number of cell migrations than the OGD-NC mimic group, whereas the OGD-inhibitor group showed the opposite trend (Fig 5C). Therefore, our study revealed that upregulation of miR-328-3p could prevent neutrophil migration by lowering IL-1β and IL-18 secretion in OGD-treated HUVECs, a process that may affect the NF-κB signaling pathway.
Fig 5. Overexpression of miR-328-3p inhibits IL-1β and IL-18 release and neutrophil migration after OGD treatment.
A. Supernatant IL-1β levels were measured via ELISA. B. Supernatant IL-18 levels were measured via ELISA. C. Neutrophil migration counts. Data are presented as the mean ± SD (n = 3). *P < 0.05; **P < 0.01; ***P < 0.001.
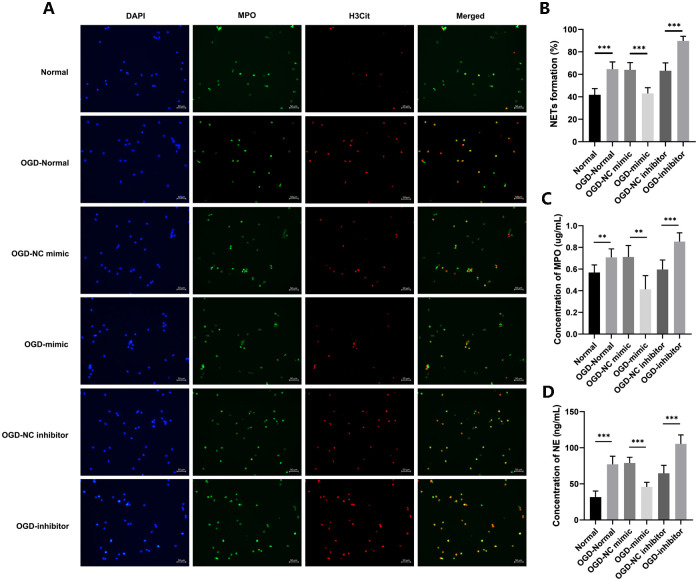
3.4 Overexpression of miR-328-3p improves neutrophil extracellular traps formation after OGD treatment
H3Cit, MPO, and NE are proteins that are released by neutrophils and are important in the composition of neutrophil extracellular traps [18]. We extracted cell supernatants from each group after OGD, co-cultured them with neutrophils, and localized NETs by immunofluorescence staining for H3Cit and MPO. We used Image J to calculate the number of cells co-localized with H3Cit and MPO as a percentage of the number of DAPI-stained cells. The results showed that the OGD-Normal group had more co-localization of H3Cit and MPO than the Normal group. We draw the conclusion that, in contrast to the Normal group, more NETs were created in the OGD-Normal group. Meanwhile, the proportion of NETs was reduced in the OGD-mimic group compared to the OGD-NC mimic group, while the OGD-inhibitor group showed the opposite trend (Fig 6A and 6B). To further analyze the levels of NETs, we used ELISA to detect the levels of MPO and NE in the supernatants of co-cultured cells. According to the experimental findings, the OGD-Normal group had greater MPO and NE levels than the Normal group. However, compared with the OGD-NC mimic group or the OGD-NC inhibitor group, the release was reduced or enhanced in the OGD-mimic group or the OGD-inhibitor group (Fig 6C and 6D). We have found that miR-328-3p regulates the NETs formation by affecting inflammatory factors released by OGD-treated HUVECs.
Fig 6. Overexpression of miR-328-3p inhibits NETs formation after OGD treatment.
A. Localization of NETs by immunofluorescence staining for H3Cit and MPO. B. Percentage of the number of cells co-localized by H3Cit and MPO in the number of DAPI-stained cells. C and D. ELISA assay for determination of MPO and NE levels in supernatants. Data are presented as the mean ± SD (n = 3). **P < 0.01; ***P < 0.001.
4. Discussion
Patients with thrombotic diseases have severe burdens due to high rates of morbidity and mortality [19]. The surface of blood vessels is covered by endothelium, which separates blood from the vessel wall and sustains endovascular homeostasis [20]. When endothelial dysfunction or injury occurs, a variety of adverse consequences occur, such as increased inflammation, decreased vasodilation, and increased thrombosis, all of which contribute to the progression of thrombotic diseases [21]. It has been found that miRNAs have the potential to be used as therapeutic targets for cardiovascular diseases, as well as for use as novel biomarkers [22]. Notably, miR-328-3p can affect cancer progression [10, 11], and miR-328-3p also has a unique role in inflammation regulation. miR-328-3p is closely related to the progression of osteoarthritis [23], human pulmonary artery endothelial cell function [24], and airway inflammation [25]. Meanwhile, miR-328-3p was able to improve endothelial injury and inflammation. For example, miR-328-3p protected vascular endothelial cells from oxidized LDL-induced injury [26]. The above results led us to consider whether miR-328-3p has a protective effect against endothelial injury and is a potential target for endothelial injury. Therefore, we found that miR-328-3p was lowly expressed in HUVECs treated with OGD for the first time. The harmful effects of OGD were reversed and cell growth was encouraged by increased miR-328-3p expression. According to our findings, miR-328-3p might be crucial in defending endothelium cells while thrombotic illnesses are developing.
Upon endothelial activation, endothelial cells and neutrophils promote neutrophil recruitment through ligand-receptor interactions, and these interactions are critical for thrombus formation [27]. Cytokines released by endothelial cells (e.g., ROS, IL-8, and IL-1β) can accelerate NETs formation [28]. Meanwhile, enzymes with proteolytic activity released by NETs, such as elastase, metalloproteinase, protein hydrolase 3, and histone G, can increase the blood vessel’s permeability by destroying the connections between endothelial cells [29]. Together, endothelial cell damage and NETs formation influence the progression of thrombotic disease. Consistent with these studies, our study found that OGD-treated cell supernatants promoted the formation of NETs in the middle by immunofluorescence localization of H3Cit and MPO, as evidenced by ELISA experiments detecting MPO and NE. However, miR-328-3p overexpression showed the reverse result. Therefore, we suggest that the NF-κB signaling pathway may be affected, which would result in decreasing inflammatory factor IL-1β and IL-18 release and reducing neutrophil migration and NETs formation.
Using a dual-luciferase reporter assay, we were able to determine that miR-328-3p directly binds to TLR2 in order to study its impact on endothelial injury and inflammation in OGD-treated endothelium. The expression of TLR2 was increased in OGD-induced HUVECs. In the OGD-mimic group, we found decreased TLR2 expression. TLR2 is one of the TLRs, and we also examined the expression of other TLRs such as TLR3, TLR4, and TLR9 (which are more studied in HUVECs [30–32]). The experimental results revealed that OGD treatment could affect the expression of TLR3, TLR4, and TLR9 in HUVECs, which again corroborated that TLRs are associated with inflammatory responses. However, after OGD treatment, there was no correlation trend of TLR3, TLR4, and TLR9 expression in HUVECs overexpressing and interfering with miR-328-3p. The above experiments prove the rationality of studying TLR2 under our experimental conditions. Meanwhile, NF-κB, as a downstream molecule of TLR2, is an inflammatory signaling pathway that acts as a crucial player in immune responses and cellular inflammatory responses. Inflammatory stimuli (e.g., IL-1β, ROS, LPS, TNFα, and thrombin) can activate NF-κB. Innate immunity and inflammation are caused by cellular genes being transcribed by NF-κB dimers, which bind DNA in the nucleus [33]. During acute inflammation, NF-κB promotes neutrophil apoptosis to counteract the body’s inflammatory response [34, 35]. Through NF-κB activation, TLR2 can further activate Nod-like receptor protein-3 (NLRP3) [36, 37]. We learned that NLRP3 can regulate neutrophil migration and NETs activation by affecting caspase-1 causing the activation and cleavage of IL-18 and IL-1β [38, 39]. Our findings support earlier research showing that miR-328-3p targeted TLR2 to activate the NF-κB signaling pathway during OGD treatment. MiR-328-3p overexpression inhibited the NF-κB signaling pathway, decreased NLRP3 expression, IL-1β and IL-18 release, ameliorated cell injury, and the formation of NETs.
In addition to affecting endothelial cells, the critical role of NETs in thrombosis has been demonstrated. It has been discovered that NETs serve as the structural basis for thrombus development [39–41] and are crucial in immune thrombosis [42]. NETs are abundant in venous, arterial, and cancer-related thrombi [43–45]. In recent clinical studies, it has been shown that patients with DVT have significantly altered serum or plasma levels of NETs biomarkers, such as H3Cit and cell-free DNA (cfDNA), and that these might be predictive of DVT in conjunction with D-dimer [46, 47]. Thus, NETs not only provide different ideas for the pathogenesis of thrombotic diseases but also provide new potential references and directions for the prediction and diagnosis of thrombotic diseases. Our study used the oxygen-glucose deprivation method, which is a simulation of in vitro thrombogenic environment and ischemic hypoxic injury. MiR-328-3p had a protective role against HUVECs treated with OGD, and via the NF-κB signaling pathway, it influenced the release of inflammatory factors and NETs. In summary, our study is valuable for understanding the mechanism of endothelial injury in thrombosis, which is favorable for the development of biomarkers and novel drugs.
However, the current study still has some limitations. Both TLR2 and TLR4 are involved in noninfectious injury, and future studies of the role of TLR4 in OGD-treated HUVECs may provide valuable insights. We need to show that miR-328-3p functions in vivo and clarify the precise mechanism by which NETs promote thrombosis, as we have only looked into the role and mechanism of miR-328-3p in cellular tests.
5. Conclusions
To summarize, our study revealed that miR-328-3p expression was downregulated in OGD-treated HUVECs and miR-328-3p overexpression reversed the proliferative capacity of OGD-treated HUVECs. Mechanistically, miR-328-3p affects the NF-κB signaling pathway by directly targeting TLR2. After OGD treatment, miR-328-3p overexpression may have anti-inflammatory effects by reducing inflammatory factors and NETs formation.
Supporting information
(PDF)
Data Availability
All relevant data are within the manuscript and its Supporting information files.
Funding Statement
his work was supported by the National Natural Science Foundation of China (No. 82160375); Natural Science Foundation of Jiangxi Province (No. 20202BABL206035); Science and Technology Planning Project of Jiangxi Provincial Health Commission in 2023 (NO. 202312146); Science and Technology Program of Jiangxi Provincial Administration of Traditional Chinese Medicine (Project No. 2021A374); and Ganzhou City Science and Technology Plan Project (NO. 2023LNS26841). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Kyrle PA, Eichinger S. Deep vein thrombosis. Lancet. 2005. 365(9465): 1163–74. doi: 10.1016/S0140-6736(05)71880-8 [DOI] [PubMed] [Google Scholar]
- 2.Mammen EF. Pathogenesis of venous thrombosis. Chest. 1992. 102(6 Suppl): 640S–644S. doi: 10.1378/chest.102.6_supplement.640s [DOI] [PubMed] [Google Scholar]
- 3.Malone PC, Agutter PS. To what extent might deep venous thrombosis and chronic venous insufficiency share a common etiology. Int Angiol. 2009. 28(4): 254–68. [PubMed] [Google Scholar]
- 4.Papayannopoulos V. Neutrophil extracellular traps in immunity and disease. Nat Rev Immunol. 2018. 18(2): 134–147. doi: 10.1038/nri.2017.105 [DOI] [PubMed] [Google Scholar]
- 5.Brinkmann V, Reichard U, Goosmann C, et al. Neutrophil extracellular traps kill bacteria. Science. 2004. 303(5663): 1532–5. doi: 10.1126/science.1092385 [DOI] [PubMed] [Google Scholar]
- 6.Li X, Wei Y, Wang Z. microRNA-21 and hypertension. Hypertens Res. 2018. 41(9): 649–661. doi: 10.1038/s41440-018-0071-z [DOI] [PubMed] [Google Scholar]
- 7.Li J, Yang C, Wang Y. miR‑126 overexpression attenuates oxygen‑glucose deprivation/reperfusion injury by inhibiting oxidative stress and inflammatory response via the activation of SIRT1/Nrf2 signaling pathway in human umbilical vein endothelial cells. Mol Med Rep. 2021. 23(2). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhang WQ, Feng L, Wang HJ, et al. Inhibition of microRNA-495 inhibits hypoxia-induced apoptosis in H9c2 cells via targeting NFIB. Eur Rev Med Pharmacol Sci. 2021. 25(1): 335–343. doi: 10.26355/eurrev_202101_24399 [DOI] [PubMed] [Google Scholar]
- 9.Lu J, Lin J, Zhou Y, Ye K, Fang C. MiR-328-3p inhibits lung adenocarcinoma-genesis by downregulation PYCR1. Biochem Biophys Res Commun. 2021. 550: 99–106. doi: 10.1016/j.bbrc.2021.02.029 [DOI] [PubMed] [Google Scholar]
- 10.Ma H, Liu C, Zhang S, et al. miR-328-3p promotes migration and invasion by targeting H2AFX in head and neck squamous cell carcinoma. J Cancer. 2021. 12(21): 6519–6530. doi: 10.7150/jca.60743 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Xiao Z, Zheng YB, Dao WX, et al. MicroRNA-328-3p facilitates the progression of gastric cancer via KEAP1/NRF2 axis. Free Radic Res. 2021. 55(6): 720–730. doi: 10.1080/10715762.2021.1923705 [DOI] [PubMed] [Google Scholar]
- 12.Wang Y, Ge P, Zhu Y. TLR2 and TLR4 in the brain injury caused by cerebral ischemia and reperfusion. Mediators Inflamm. 2013. 2013: 124614. doi: 10.1155/2013/124614 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wang F, Wang Z, Pu J, et al. Oscillating flow promotes inflammation through the TLR2-TAK1-IKK2 signalling pathway in human umbilical vein endothelial cell (HUVECs). Life Sci. 2019. 224: 212–221. doi: 10.1016/j.lfs.2019.03.033 [DOI] [PubMed] [Google Scholar]
- 14.Zhu H, Dai R, Fu H, Meng Q. MMP-9 Upregulation is Attenuated by the Monoclonal TLR2 Antagonist T2.5 After Oxygen-Glucose Deprivation and Reoxygenation in Rat Brain Microvascular Endothelial Cells. J Stroke Cerebrovasc Dis. 2019. 28(1): 97–106. doi: 10.1016/j.jstrokecerebrovasdis.2018.09.014 [DOI] [PubMed] [Google Scholar]
- 15.Khan S, Shafiei MS, Longoria C, Schoggins JW, Savani RC, Zaki H. SARS-CoV-2 spike protein induces inflammation via TLR2-dependent activation of the NF-κB pathway. Elife. 2021. 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Malaponte G, Signorelli SS, Bevelacqua V, et al. Increased Levels of NF-kB-Dependent Markers in Cancer-Associated Deep Venous Thrombosis. PLoS One. 2015. 10(7): e0132496. doi: 10.1371/journal.pone.0132496 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jorgensen I., Lopez J.P., Laufer S.A., Miao E.A., 2016. IL-1β, IL-18, and eicosanoids promote neutrophil recruitment to pore-induced intracellular traps following pyroptosis. Eur. J. Immunol. 46, 2761–2766. doi: 10.1002/eji.201646647 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kolaczkowska E., Kubes P., 2013. Neutrophil recruitment and function in health and inflammation. Nat. Rev. Immunol. 13, 159–175. doi: 10.1038/nri3399 [DOI] [PubMed] [Google Scholar]
- 19.Koupenova M, Kehrel BE, Corkrey HA, Freedman JE. Thrombosis and platelets: an update. Eur Heart J. 2017. 38(11): 785–791. doi: 10.1093/eurheartj/ehw550 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zheng D, Liu J, Piao H, Zhu Z, Wei R, Liu K. ROS-triggered endothelial cell death mechanisms: Focus on pyroptosis, parthanatos, and ferroptosis. Front Immunol. 2022. 13: 1039241. doi: 10.3389/fimmu.2022.1039241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhang X, Zheng Y, Wang Z, et al. Melatonin as a therapeutic agent for alleviating endothelial dysfunction in cardiovascular diseases: Emphasis on oxidative stress. Biomed Pharmacother. 2023. 167: 115475. doi: 10.1016/j.biopha.2023.115475 [DOI] [PubMed] [Google Scholar]
- 22.Barwari T, Joshi A, Mayr M. MicroRNAs in Cardiovascular Disease. J Am Coll Cardiol. 2016. 68(23): 2577–2584. doi: 10.1016/j.jacc.2016.09.945 [DOI] [PubMed] [Google Scholar]
- 23.Yang J, Zhang M, Yang D, et al. m(6)A-mediated upregulation of AC008 promotes osteoarthritis progression through the miR-328-3p‒AQP1/ANKH axis. Exp Mol Med. 2021. 53(11): 1723–1734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hong L, Ma X, Liu J, Luo Y, Lin J, Shen Y, et al. Circular RNA-HIPK3 regulates human pulmonary artery endothelial cells function and vessel growth by regulating microRNA-328-3p/STAT3 axis. Pulm Circ. 2021; 11:20458940211000234. doi: 10.1177/20458940211000234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cao X, Wang K, Zhu H. Yanghepingchuan granule improves airway inflammation by inhibiting autophagy via miRNA328-3p/high mobility group box 1/Toll-like receptor 4 targeting of the pathway of signaling in rat models of asthma. J Thorac Dis. 2023; 15:6251–64. doi: 10.21037/jtd-23-1262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Qin X, Guo J. MicroRNA-328-3p Protects Vascular Endothelial Cells Against Oxidized Low-Density Lipoprotein Induced Injury via Targeting Forkhead Box Protein O4 (FOXO4) in Atherosclerosis. Med Sci Monit. 2020; 26:e921877. doi: 10.12659/MSM.921877 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Brill A, Fuchs TA, Chauhan AK, et al. von Willebrand factor-mediated platelet adhesion is critical for deep vein thrombosis in mouse models. Blood. 2011. 117(4): 1400–7. doi: 10.1182/blood-2010-05-287623 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zapponi K, Orsi FA, Cunha J, et al. Neutrophil activation and circulating neutrophil extracellular traps are increased in venous thromboembolism patients for at least one year after the clinical event. J Thromb Thrombolysis. 2022. 53(1): 30–42. doi: 10.1007/s11239-021-02526-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yao M, Ma J, Wu D, et al. Neutrophil extracellular traps mediate deep vein thrombosis: from mechanism to therapy. Front Immunol. 2023. 14: 1198952. doi: 10.3389/fimmu.2023.1198952 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Guo Z, Chen L, Zhu Y, Zhang Y, He S, Qin J, et al. Double-stranded RNA-induced TLR3 activation inhibits angiogenesis and triggers apoptosis of human hepatocellular carcinoma cells. Oncol Rep. 2012; 27:396–402. doi: 10.3892/or.2011.1538 [DOI] [PubMed] [Google Scholar]
- 31.Liu X, Lu B, Fu J, Zhu X, Song E, Song Y. Amorphous silica nanoparticles induce inflammation via activation of NLRP3 inflammasome and HMGB1/TLR4/MYD88/NF-kb signaling pathway in HUVEC cells. J Hazard Mater. 2021; 404:124050. doi: 10.1016/j.jhazmat.2020.124050 [DOI] [PubMed] [Google Scholar]
- 32.Li Y, Ou K, Wang Y, Luo L, Chen Z, Wu J. TLR9 agonist suppresses choroidal neovascularization by restricting endothelial cell motility via ERK/c-Jun pathway. Microvasc Res. 2022; 141:104338. doi: 10.1016/j.mvr.2022.104338 [DOI] [PubMed] [Google Scholar]
- 33.Millar MW, Fazal F, Rahman A. Therapeutic Targeting of NF-κB in Acute Lung Injury: A Double-Edged Sword. Cells. 2022. 11(20): 3317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lawrence T, Gilroy DW, Colville-Nash PR, Willoughby DA. Possible new role for NF-kappaB in the resolution of inflammation. Nat Med. 2001. 7(12): 1291–7. doi: 10.1038/nm1201-1291 [DOI] [PubMed] [Google Scholar]
- 35.Greten FR, Arkan MC, Bollrath J, et al. NF-kappaB is a negative regulator of IL-1beta secretion as revealed by genetic and pharmacological inhibition of IKKbeta. Cell. 2007. 130(5): 918–31. doi: 10.1016/j.cell.2007.07.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Jang HM, Park JY, Lee YJ, et al. TLR2 and the NLRP3 inflammasome mediate IL-1β production in Prevotella nigrescens-infected dendritic cells. Int J Med Sci. 2021. 18(2): 432–440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tian L, Yan J, Li K, et al. Ozone exposure promotes pyroptosis in rat lungs via the TLR2/4-NF-κB-NLRP3 signaling pathway. Toxicology. 2021. 450: 152668. [DOI] [PubMed] [Google Scholar]
- 38.Saxena A, Chen W, Su Y, et al. IL-1 induces proinflammatory leukocyte infiltration and regulates fibroblast phenotype in the infarcted myocardium. J Immunol. 2013. 191(9): 4838–48. doi: 10.4049/jimmunol.1300725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yadav V, Chi L, Zhao R, et al. Ectonucleotidase tri(di)phosphohydrolase-1 (ENTPD-1) disrupts inflammasome/interleukin 1β-driven venous thrombosis. J Clin Invest. 2019. 129(7): 2872–2877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Brill A, Fuchs TA, Savchenko AS, et al. Neutrophil extracellular traps promote deep vein thrombosis in mice. J Thromb Haemost. 2012. 10(1): 136–44. doi: 10.1111/j.1538-7836.2011.04544.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Yago T, Liu Z, Ahamed J, McEver RP. Cooperative PSGL-1 and CXCR2 signaling in neutrophils promotes deep vein thrombosis in mice. Blood. 2018. 132(13): 1426–1437. doi: 10.1182/blood-2018-05-850859 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kimball AS, Obi AT, Diaz JA, Henke PK. The Emerging Role of NETs in Venous Thrombosis and Immunothrombosis. Front Immunol. 2016. 7: 236. doi: 10.3389/fimmu.2016.00236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Thålin C, Hisada Y, Lundström S, Mackman N, Wallén H. Neutrophil Extracellular Traps: Villains and Targets in Arterial, Venous, and Cancer-Associated Thrombosis. Arterioscler Thromb Vasc Biol. 2019. 39(9): 1724–1738. doi: 10.1161/ATVBAHA.119.312463 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Dyer MR, Chen Q, Haldeman S, et al. Deep vein thrombosis in mice is regulated by platelet HMGB1 through release of neutrophil-extracellular traps and DNA. Sci Rep. 2018. 8(1): 2068. doi: 10.1038/s41598-018-20479-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Leal AC, Mizurini DM, Gomes T, et al. Tumor-Derived Exosomes Induce the Formation of Neutrophil Extracellular Traps: Implications For The Establishment of Cancer-Associated Thrombosis. Sci Rep. 2017. 7(1): 6438. doi: 10.1038/s41598-017-06893-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Liu L, Zhang W, Su Y, Chen Y, Cao X, Wu J. The impact of neutrophil extracellular traps on deep venous thrombosis in patients with traumatic fractures. Clin Chim Acta. 2021. 519: 231–238. doi: 10.1016/j.cca.2021.04.021 [DOI] [PubMed] [Google Scholar]
- 47.Li Y, Jiang Q, Zhou X, et al. A prospective marker for the prediction of postoperative deep venous thrombosis: Neutrophil extracellular traps. Front Cell Dev Biol. 2022. 10: 1071550. doi: 10.3389/fcell.2022.1071550 [DOI] [PMC free article] [PubMed] [Google Scholar]